Abstract
Several factors that underlie health inequality have been studied and defined as the social determinants of health (SDHs). The main SDHs are gender, socioeconomic status (SES), and ethnicity. In this study, disparity was analyzed in the context of vascular diseases (VDs) such as Peripheral Artery Disease (PAD), Chronic Venous Disease (CVD), Abdominal Arterial Aneurysm (AAA), and Carotid Stenosis (CS). This article aims to provide a comprehensive overview of the published evidence of the SDHs in VDs. For this purpose, Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used. Published articles using the Scopus and ScienceDirect databases were searched. The criteria for the articles’ inclusion/exclusion were decided using a modified PICOTS framework. For the selected articles, the data sheets were organized in such a way to extract all data of potential relevance. Our findings showed that in VDs, gender, SES, and ethnicity are very important, with some specific problems for VDs analyzed. In conclusion, having detected the presence of SDHs that act negatively on VDs, a model based on action items for the SDHs associated with VDs was proposed.
1. Introduction
A series of factors are studied that underlie health inequalities, that is, the social determinants of health (SDHs) (CSDH 2008; Solar and Irwin 2010). The SDHs are all of those factors that are intertwined with the well-being of individuals and are elements that impact the probability of having good health and stand at the origin of the pervasive inequalities of our society (Solar and Irwin 2010).
From a theoretical point of view to date, there are three different approaches to SDHs: (1) psychological and sociological points of view; (2) social implications of disease/political economy of health; and (3) eco-social theory and related multilevel considerations. All three theories aim to explain what is behind the SDHs. In this regard, Krieger (2001) stated that the theory of the distribution of disease requires a complex approach and is therefore multicausal in biological, social, and economic systems (Morin 2007).
The first theoretical approach focuses on the psychosocial dimension based on the concept that a feeling of unequal personal status may lead to stress affecting health (Raphael 2006). This approach was introduced by Cassel (1976), who argued that the social context acts on individuals with some neuroendocrine consequences and increases the vulnerability to disease. Wilkinson and Pickett (2006) related the altered neuroendocrine pattern to the health capacity of people’s perception and experience of their role in social systems and thus the experience to live in social contexts with inequality issues that force people to compare their social positions, property, and circumstances of life with those of others, generating feelings of disgrace and uselessness, along with the chronic stress that undermines health.
The second approach correlates the state of health with the social and economic dimensions (Solar and Irwin 2010). This approach follows the neo-materialist vision, without excluding negative psychosocial effects that generate income inequality (CSDH 2008). In particular, the correlations between income inequality and health are analyzed, considering them as causal and structural elements of inequality, reducing instead the relevance of the perceptions of inequality. Therefore, the effect of income inequality on health has very serious consequences. In this regard, “Income inequality has risen during the past four decades within many societies, prompting some scholars to raise the alarm concerning the corrosive effects of inequality on social cohesion” (Berkman et al. 2014, p. 126). This relationship is known as reverse causation, i.e., the loss of income and/or wealth due to illness. Specifically, “reverse causation refers to ways in which ill health may lead to lower income—for example, when sickness causes a loss of income and/or medical care costs deplete one’s wealth. Reverse causation—the ways in which health can influence economic resources—is contrasted with the ways in which economic resources can influence health” (Braveman 2023, p. 20).
The third approach is the most recent and concerns the ecological vision of SDHs (Krieger 2001); it uses multilevel frameworks, through the integration between social, biological, economic, and historical variables, with a type of ecological orientation to propose a new vision of the determinants in terms of the distribution of diseases and social inequalities. According to Krieger, interdisciplinary approaches aim to analyze the actual and changing patterns of health in the world’s population, illness, and well-being related to several sciences, with all levels of complexity, such as biology, ecology, and sociology etc., connecting the ecosystem as a whole. Krieger describes the way to incorporate biological issues into the ecosystem and societies and states that every element of human existence cannot be understood if separated from the historical and sociological contexts (CSDH 2008).
Thus, SDHs are characterized by the fact that great importance is given to the socioeconomic and political contexts, i.e., the following are considered essential: macroeconomic policies, the organization of the labor market, and social values; factors which in turn affect the main tools for the protection of collective health, namely: the welfare state and health policies (Cardano et al. 2020).
In these contexts, it is known the structural mechanisms are rooted, i.e., those phenomena that increase and/or create social stratification and therefore sanction the social position of each individual. Indeed, these mechanisms are able to determine the state of health of communities on the basis of their position within the distribution of power, prestige, and barriers to use resources (Ottersen et al. 2014).
Therefore, according to the model proposed by the Commission on Social Determinants of Health (CSDH 2008): socioeconomic status, structural mechanisms, and social status constitute the so-called structural determinants, which are the main sources of health inequity (Costa 2023).
Among the SDHs, however, those that most involve health problems are gender, socioeconomic status (SES), and ethnic origin (Cardano et al. 2020). These three types of SDHs act both as structural determinants and as factors and in interaction with stratification variables that can modify health outcomes (Marmot 2014). Gender issues are today one of the main sources of discrimination that excludes or hinders access to care, and therefore, to the protection of health (Marmot 2015). Ethnicity and the related process of marginalization affect health, so the most disadvantaged ethnic groups have a worse state of health than that recorded for privileged groups or for the average population (Mackenbach 2012).
Thus, today, more than ever, there is a need for health professionals not only to know SDHs, but also to have expertise in how to manage them. This is the reason why the concept of cultural competency in medicine (CCIM) was born. In this regard, “CCIM has increasingly been seen as a panacea for how to provide quality and effective health care for all patients” (Moreira 2021, p. 76).
From a definitional point of view, the following definition was used: Cultural competence is defined by specific attitudes, behaviors, and policies integrated in a system, or among professionals exposed to cross-cultural events, considering also the ability to function effectively as a person or an organization within the context of the cultural beliefs, behaviors, and needs presented by consumers and their communities (Cross 1989).
Disparities also occur in biomedical fields such as vascular surgery (VS) (Haider et al. 2007; Moreira 2021). Despite significant improvements in VS techniques for the most common types of vascular diseases (VDs), such as Peripheral Artery Disease (PAD), Chronic Venous Disease (CVD), Abdominal Arterial Aneurysm (AAA), and Carotid Stenosis (CS), there are ethnic, socioeconomic, and gender disparities in most of the major outcomes of vascular procedures (Moreira 2021). Thus, “These findings are a call to action and highlight the urgent need for ongoing efforts to recruit and train a diverse VS workforce that will have the ability to identify and address these distinct social and cultural challenges that contribute to disparities in vascular surgical care” (ibid. p. 79).
VDs have an important prevalence, especially in western populations, and is a leading cause of morbidity and mortality among affected patients, with an important burden of social issues (Barnes 1995; Blais et al. 2020). In fact, it is estimated that 30% of the adult global population suffers from PAD, a chronic arterial disease of the lower limbs that causes affected patients to have claudication, rest pain, and even tissue loss with gangrene (Federman et al. 1998). Abdominal aortic aneurysm (AAA), a pathological dilation of the abdominal aorta, have a global prevalence of 2% to 8% of patients in developed countries and can cause threatening rupture with mortality rates up to 80% (Marcaccio and Schermerhorn 2021). CVD refers to pathological alterations of the veins of lower limbs that cause important symptoms and signs, such as varicose veins or venous leg ulcers, in affected patients and has a global prevalence up to 77% in the general adult population (Serra et al. 2016). Moderate CS and severe CS have a global pooled prevalence of 4.2% and 1.7%, respectively, and the latter has an annual risk of stroke of 2–5%. (de Weerd et al. 2009).
The issues of disparities, inclusion, and equity in treatment and health care outcomes among patients with vascular disease are a topic of interest in VS (Morrissey et al. 2007) and need to be further investigated.
Based on what has been reported, the question research of this review is as follows: in the literature, how have the health determinants been analyzed and therefore the social factors that affect the main VDs?
2. Materials and Methods
In the present study, PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020) guidelines was used (Page et al. 2021).
2.1. Search Strategy
Articles published on Scopus and ScienceDirect databases without a time limit were searched. Table 1 lists the keywords used for the search of the papers. these databases were considered because of the large number of indexed journals and the high coverage of relevant health sciences disciplines. The search of the database was extended to the title, keywords, and abstracts. No country or date restrictions were used in the search, but only publications written in English were included. Specifically, PubMed was not searched, and this goes along with the focus of the study conducted on non-biological aspects.

Table 1.
Databases, search strategy, and number of articles extracted.
2.2. Inclusion and Exclusion Criteria
The criteria for an article’s inclusion/exclusion were decided using a modified PICOTS framework (Samson and Schoelles 2012) (Table 2).

Table 2.
Criteria for articles’ inclusion/exclusion according to a modified PICOTS.
The parameter “Patients” was adapted to “Source”, “Setting” was adapted to “Study type”, and “Language” was included.
2.3. Study Selection
Using the inclusion and exclusion criteria, three authors built a list of all titles found, following the database search procedure, subsequently building an initial classification of the articles. These were then subjected to the analysis of the abstracts, from which the full texts were analyzed. Then, the author searched the references of the articles selected earlier to identify other relevant studies. Any differences of opinion on the inclusion of a document were resolved through discussion until the working group reached a consensus.
2.4. Data Extraction
For the selected articles, the data sheets were organized in such a way to extract all data of potential relevance. Two authors performed the filtering, and one author reviewed the results to ensure the accuracy of the selection. The extracted form contained the following elements: reference, title, journal, publication year, type of study, aim/research questions, SDHs studies, specific VDs (AAA, PAD, CVD, and CS) included, and key findings. Missing data were filled in, when possible, by mail correspondence with the study authors. Results are presented narratively and qualitatively (rather than quantitatively), a synthesis resulting in a good choice for showing the main overall results of the 22 included studies.
3. Results
3.1. Selected Studies
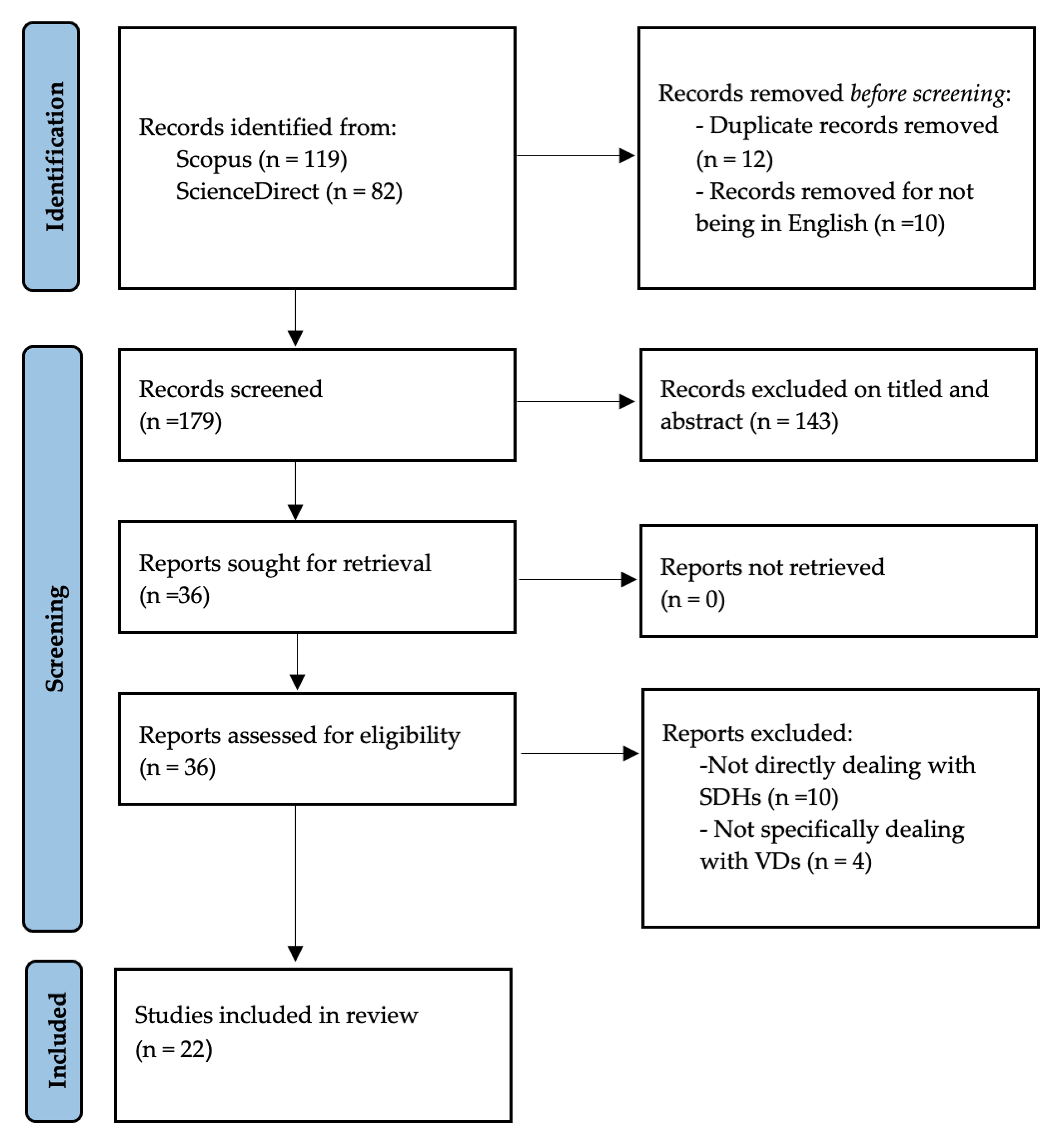
The initial search identified 201 articles (Figure 1). After a review of titles and abstracts, the authors pointed out 36 that reduced to 22 articles after a full text reading.
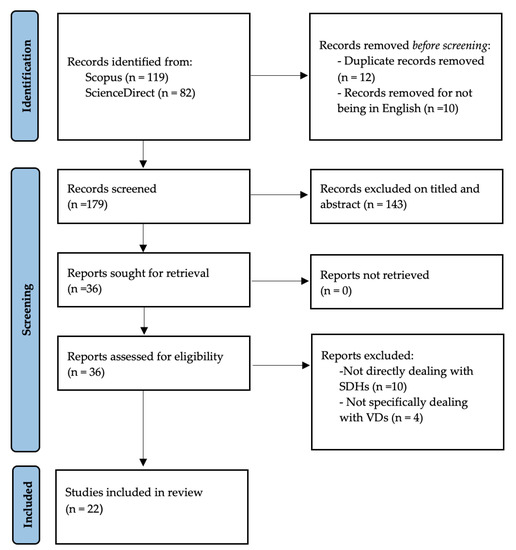
Figure 1.
Prisma 2020 Flow Diagram.
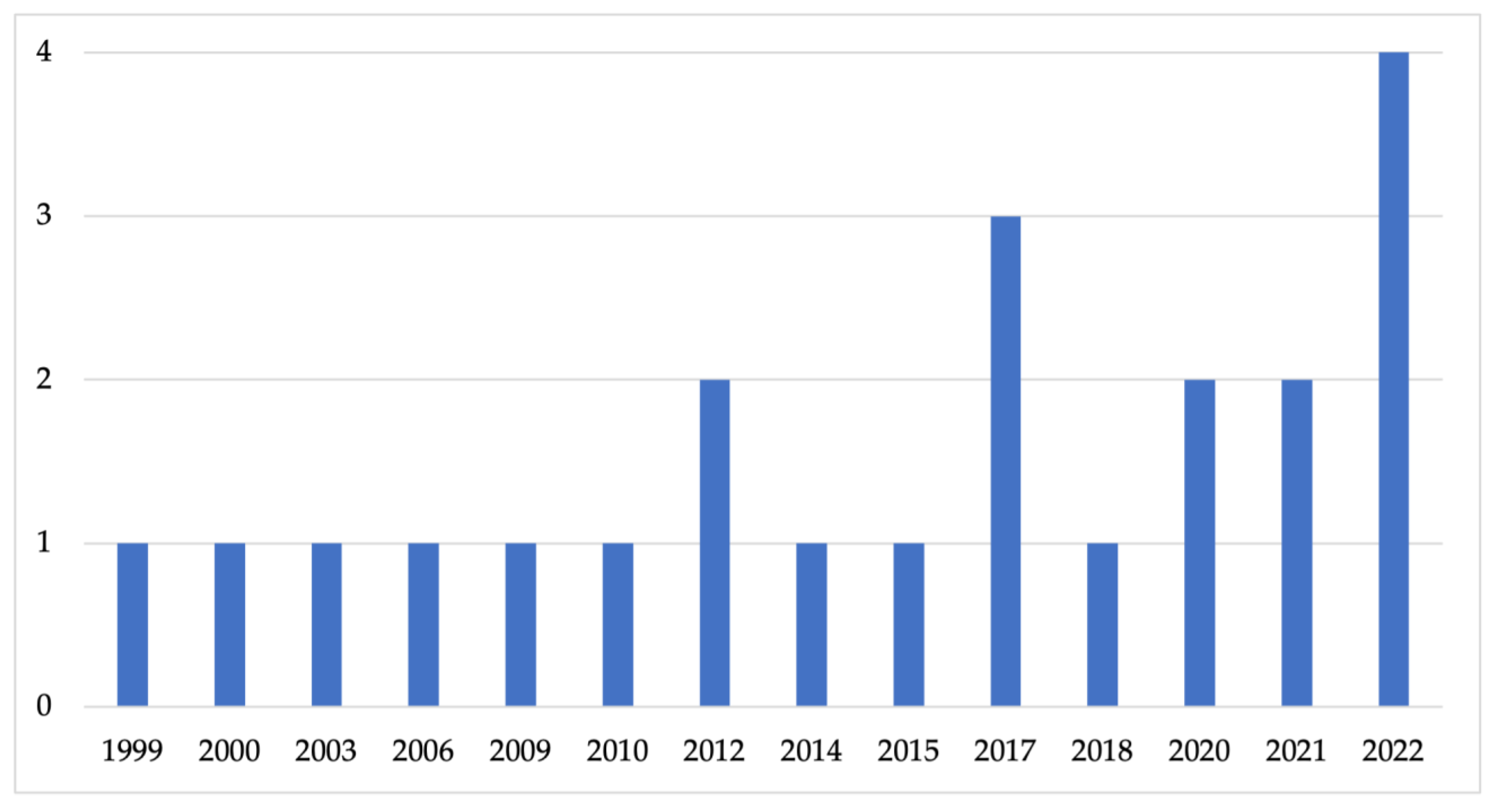
3.2. Temporal Extension
In the included set, the authors found 22 studies with an important temporal extension between 1999 and 2022. The years with the most articles were 2012–2020–2021 with two articles each, 2017 with three articles, and 2022 with four articles. In Figure 2, the authors report the publication years.
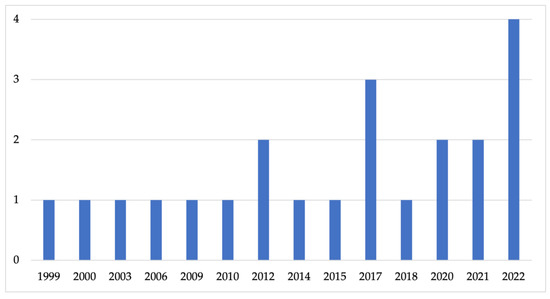
Figure 2.
Publication years.
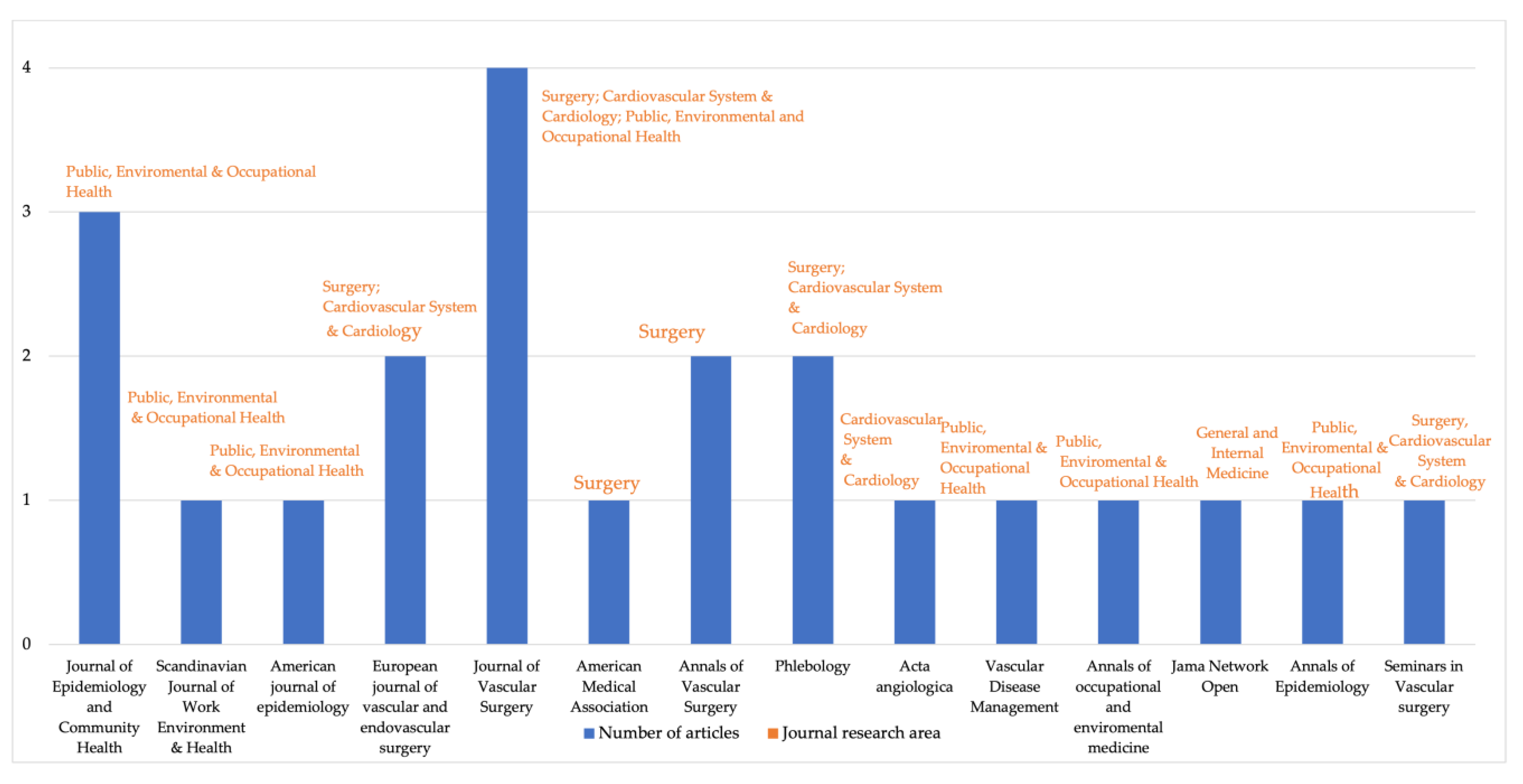
3.3. Journal List
The 22 papers included in our study appeared in different journals. The most frequently included journals were Journal of Vascular Surgery with four papers, Journal of Epidemiology and Community Health with three papers, European Journal of Vascular and Endovascular Surgery, Annals of Vascular Surgery, and Phlebology with two articles for each of these latter journals. Regarding the subject area of the included journals, 10 of the journals were vascular surgery journals, and five were epidemiology journals. Included papers were published in journals of different research areas (Figure 3).
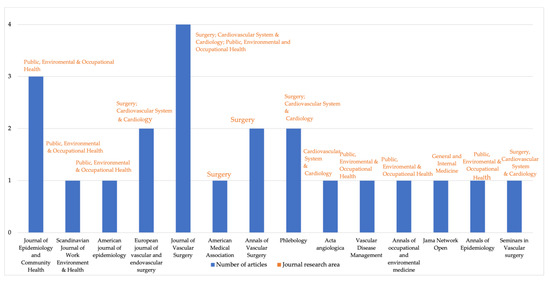
Figure 3.
Journal list.
3.4. Articles and Types of Vascular Disease
Of the 22 included articles, eight exclusively analysed AAA, two dealt with CS, eight studied CVD, three focused on the PAD, and only one paper dealt with PAD, CS, and AAA (Table 3).

Table 3.
Number of studies for each type of vascular disease (total of articles: 22).
3.5. General Characteristics of the Included Studies
The 22 articles included in this systematic review were analysed considering different characteristics, as shown in Table 4.

Table 4.
General characteristics of the included studies.
3.6. Abdominal Arterial Aneurysm and Social Determinants of Health
Nine studies out of 22 analyzed the relationship between AAA and SDHs, and the most important related issues are reported hereinafter.
3.6.1. Abdominal Arterial Aneurysm and Ethnicity
Ethnicity is widely analyzed among SDHs in AAA (Osborne et al. 2009, 2010; Sandiford et al. 2012; Jacomelli et al. 2017; Li et al. 2022). In particular, ethnicity is an important SDH in the AAA due to three reasons (Osborne et al. 2009, 2010): (1) patients with different ethnicities, for example, black patients, often receive hospital care with worse outcomes than white patients, especially in health facilities that have a prevalence of accesses of white patients (Sandiford et al. 2012; Jacomelli et al. 2017; Li et al. 2022). This happens because fewer resources are made available to black patients for their care (Osborne et al. 2009; Li et al. 2022). Often, black patients are operated on by less experienced surgeons, and the degree of surgical experience and skill plays an essential role in the survival of patients undergoing surgery in general (Sandiford et al. 2012); (2) patients of different ethnicities may have negative postoperative outcomes with a higher incidence when they are in healthcare facilities with a prevalence of white patients (Osborne et al. 2010; Sandiford et al. 2012); in fact, the various authors point out, that this constitutes a real form of discrimination (Osborne et al. 2009, 2010; Sandiford et al. 2012; Jacomelli et al. 2017; Li et al. 2022); (3) these forms of inequity, in part, according to some authors (Osborne et al. 2009; Osborne et al. 2010) are also linked to the stage of the disease, with a greater impact on black patients than on white ones (Li et al. 2022). According to some of the included studies (Sandiford et al. 2012; Jacomelli et al. 2017; Li et al. 2022), African American patients primarily undergo AAA repair at a rate of 70% compared to white patients; moreover, black patients have a higher incidence of ruptured aneurysms than whites. All studies included correlated gender with ethnicity and the incidence of AAA (Osborne et al. 2009, 2010; Sandiford et al. 2012; Jacomelli et al. 2017; Li et al. 2022), with the almost unequivocal result according to which women with AAA tend, on average, to present the onset of the disease at a later age compared to men, although black women have a greater number of comorbidities although AAA in women are smaller, but with a higher mortality compared with men (Jacomelli et al. 2017; Li et al. 2022).
3.6.2. Abdominal Arterial Aneurysm and Gender
Regarding the relationship between gender and AAA, it should be remembered that there are gender-based differences in the epidemiology of AAA (Ohrlander et al. 2012; Barshes and Minc 2021; Li et al. 2022) both in terms of prevalence (two to six times more frequent in men than in women) (Jacomelli et al. 2017) and in the modality of manifestation of the disease: in women, aneurysms are smaller than in men, and therefore there is less risk of rupture in women (Ramkumar et al. 2020; Li et al. 2022); another gender difference also concerns the treatment of AAA since women have a lower probability of undergoing surgery (Barshes and Minc 2021).
3.6.3. Abdominal Arterial Aneurysm and SES
Several included studies have shown that SES is a variable that negatively impacts and is therefore particularly harmful to patients with AAA (Osborne et al. 2009, 2010; Ohrlander et al. 2012; Zommorodi et al. 2018; Barshes and Minc 2021). Low SES is strongly correlated with a higher risk of AAA manifestation; moreover, it would also seem to influence the postoperative phase with worse outcomes. Several authors, in fact, consider a low SES as a real risk factor (Barshes and Minc 2021). Furthermore, the SES has a considerable impact on access to health services that deal with the pre-inter-and postoperative phases of AAA (Zommorodi et al. 2018; Barshes and Minc 2021). Some authors have found a correlation between the incidence of AAA and SES as well as with lifestyle and therefore any addiction to substances and/or sedentary lifestyle; (Osborne et al. 2009, 2010; Ohrlander et al. 2012) the social environment in which patients are placed: the type of home, its location, access to transport, type of work; and again the SES has been correlated, as already mentioned, to the access to health services (Barshes and Minc 2021).
3.7. Carotid Stenosis and the Social Determinants of Health
Three studies analyzed the relationship between CS and SDHs.
As can be seen, the number of studies (Barshes and Minc 2021; Hsu et al. 2022; Camelo et al. 2022) dealing with CS are few. However, from the analysis of the data of these three papers, it is clear that there are racial and ethnic disparities (Barshes and Minc 2021; Hsu et al. 2022; Camelo et al. 2022).
3.7.1. Carotid Stenosis and Ethnicity
The articles, despite their differences, showed that black patients had higher incidence and prevalence of CS than white patients (Barshes and Minc 2021). The included studies also show that there are racial disparities in the case of CS, which also concerns Latinas, Latinas, or Latinas and women (Camelo et al. 2022). The results of the analysis showed lower rates of CS in white patients who had received care in “minority” hospitals, adding to the idea that the variability in hospital quality and use of the procedure may partly explain the ethnic disparities (Hsu et al. 2022). Camelo et al. (2022), regarding ethnicity, demonstrated how the experience of ethnic discrimination experienced by individuals is correlated with high blood pressure and is therefore an important vascular risk factor, despite, as underlined by the authors, this association between discrimination and CS is underexamined. Therefore, all three included studies highlight how ethical limits access to health services regarding housing, education, employment, and income.
3.7.2. Carotid Stenosis and SES
As for AAA, also in CS, an important role is attributed to the SES (Barshes and Minc 2021) in the incidence and prevalence of the disease. In fact, it is argued that a low SES increases the risk of developing stenosis, both for incorrect eating habits and for the reduced possibility of access to the main prevention and diagnostic tests of CS (Hsu et al. 2022). This increases stress and situations that are risky for health (Barshes and Minc 2021; Hsu et al. 2022; Camelo et al. 2022). In conclusion, a recent study by Hsu et al. (2022) showed how the size of the hospital, in terms of beds related to insurance coverage, residence, and other clinical factors, and the intervention rates for CS, are significantly lower.
3.8. Peripheral Artery Disease and Social Determinants of Health
Four studies that analyzed the relationship between PAD and SDHs were found, and the main related issues can be found below.
3.8.1. Peripheral Artery Disease and Ethnicity
The analysis of the articles included shows the presence of real forms of ethnic stigma (Barshes and Minc 2021; Brathwaite et al. 2021; Demsas et al. 2022) in the treatment of PAD in general. Both papers dealing with ethnicity and PAD, in this regard, report that there are forms of diversity between ethnic groups and the epidemiology of PAD (Barshes and Minc 2021; Brathwaite et al. 2021; Demsas et al. 2022). More specifically, it is argued that black patients with PAD usually develop more comorbidities at a younger age and with greater severity (Demsas et al. 2022). In particular, it is reported that the prevalence of PAD in the black population is higher than that in the white one, with an incidence 1.6 times (Brathwaite et al. 2021) higher in black patients than in white patients; as regards, instead, amputation, black patients have an incidence that goes from two to four times higher than that for whites (Barshes and Minc 2021; Demsas et al. 2022). Regarding ethnicity and PAD, it was also found that black patients are more likely to undergo limb amputation with PAD, compared to whites, with a nearly doubled rate (Barshes and Minc 2021). Latinos, in the case of PAD, also have higher incidence and rates of amputations for PAD (Barshes and Minc 2021; Brathwaite et al. 2021). Furthermore, studies suggest an important correlation between ethnicity and rurality (Barshes and Minc 2021; Demsas et al. 2022), the latter being capable of significantly increasing the probability of amputation among the ethnicities considered most at risk. Rurality, according to the authors, is a risk factor compared to those who live in urban contexts, as there are greater logistical limitations (Barshes and Minc 2021; Demsas et al. 2022).
3.8.2. Peripheral Artery Disease and SES
Another important SDH (social determinant of health) analyzed regarding PAD concerns SES (Barshes and Minc 2021; Demsas et al. 2022). The association between SES and PAD is considered particularly multifactorial. In particular, it is argued that the correlation between PAD and SES in the United States, analyzed by studying the risk of hospitalization for PAD, is more than double in the sample with an average income <USD 12,000 compared to a sample with an average income equal to USD 25,000 (Demsas et al. 2022). Moreover, the SES, based on an analysis of the risk of hospitalization for PAD, was double that in subjects with a low level of education (Barshes and Minc 2021; Demsas et al. 2022). The authors underline that SES is highly limited as a type of variable because, especially in countries in which insurance is required for access to care, the financial barrier prevents timely prevention, diagnosis, and treatment (Demsas et al. 2022). The SES is therefore closely correlated with ethnicity, with ethnic minorities among the population groups with lower income and education Barshes and Minc 2021; Brathwaite et al. 2021; Demsas et al. 2022).
3.8.3. Peripheral Artery Disease and Gender
Regarding gender issues and PAD (Paudel et al. 2017; Barshes and Minc 2021; Demsas et al. 2022), the literature analyzed is consistent in supporting a strong correlation between gender and the incidence, course, and severity and PAD (Barshes and Minc 2021; Demsas et al. 2022). First of all, it is emphasized from a biological point of view (Paudel et al. 2017). When considering preoperative medical management, female patients are less likely to receive guideline-recommended high-intensity statins or any statin prescriptions than male patients (Barshes and Minc 2021; Demsas et al. 2022). Furthermore, the role of gender in this VD, more than in the others considered, would seem to have a strong influence on compliance with drug therapy.
Women, in fact, would be less compliant to take statins (Demsas et al. 2022), for fear that it could change their physical appearance, thus preferring alternative therapies such as natural ones or physical activity (Barshes and Minc 2021). In this regard, it is emphasized that women subjected to pharmacological treatment, but convinced that this was dangerous, record greater adverse effects from the therapy (Demsas et al. 2022). Gender also has a strong influence on hospital admissions: women are more reluctant to be hospitalized by election for PAD but show a higher incidence of cases of emergency hospitalization (Paudel et al. 2017; Barshes and Minc 2021; Demsas et al. 2022).
3.9. Chronic Venous Disease and the Social Determinants of Health
Considering CVD and SDHs, eight studies analyzed this relationship.
Considering the various articles included in this review, it is quite evident that CVD is less studied and analyzed than arterial diseases (Evans et al. 1999; Tüchsen et al. 2000; Criqui et al. 2003; Wright et al. 2006; Schul et al. 2014; Ziaja et al. 2015; Davies et al. 2017; Jung et al. 2020). Most of the papers included on CVD relate this disease to an important element of the SES: the type of work and the epidemiology of this disease (Tüchsen et al. 2000; Wright et al. 2006; Jung et al. 2020).
3.9.1. Chronic Venous Disease and SES
Therefore, a certain correlation between the CVD, the type of job covered, and the general working conditions is underlined in the three studies included (Tüchsen et al. 2000; Wright et al. 2006; Jung et al. 2020); it is also possible to provide a list of jobs at the highest risk of developing CVD (Table 5).

Table 5.
Type of work and CVD.
The results showed an important relationship between the type of work performed and hospitalization for CVD (Wright et al. 2006; Jung et al. 2020), and in particular, there is a significant correlation between standing and walking to work and the subsequent development of CVD (Tüchsen et al. 2000; Wright et al. 2006; Jung et al. 2020). Thus, from the analysis of the paper, there are at least three reasons behind the relationship between job position and CVD; (1) based on the type of work activity and its daily duration (Wright et al. 2006); (2) standing and walking during working hours (Tüchsen et al. 2000; Jung et al. 2020); (3) the impact of attitudes or the state of health of the workers (Jung et al. 2020). Regarding the SES, it was also found that socially disadvantaged people are more likely to develop CVD (Ziaja et al. 2015); as for the other diseases analyzed, also for CVD, it is pointed out that patients with CVD residing in the most disadvantaged areas (Ziaja et al. 2015) of the cities are more likely to develop co-morbidities (diabetes, atherosclerosis, smoking, and obesity) (Schul et al. 2014; Ziaja et al. 2015; Davies et al. 2017). Individuals, on the other hand, who are more affluent and/or more educated would be more focused on the perception of venous health, and therefore, have a greater aptitude to turn to specialists for prevention or for timely diagnosis (Ziaja et al. 2015; Davies et al. 2017).
3.9.2. Chronic Venous Disease and Ethnicity
As regards ethnicity, the only study that has dealt with it showed that CVD has a higher incidence among non-Hispanic whites compared to Hispanics, African Americans, or Asians (Criqui et al. 2003).
3.9.3. Chronic Venous Disease and Gender
Ultimately, as regards gender issues, among included studies, (Evans et al. 1999; Tüchsen et al. 2000; Criqui et al. 2003; Wright et al. 2006), women are considered at higher risk than men, regardless of SES or ethnicity; although black women, Latinos, etc., have a higher incidence than white women (Wright et al. 2006). Furthermore, it was found that the risk of developing CVD increases in correlation with the work activities carried out by both men and women, with a specificity, namely, that men subjected to greater physical stress are more affected by CVD, as well as women (Criqui et al. 2003; Wright et al. 2006). An interesting fact on gender issues concerns the fact that women very frequently have standing jobs and therefore a higher incidence of CVD (Wright et al. 2006).
4. Discussion
The aim of the present review was to study the SDHs in VDs, specifically in AAA, CS, PAD, and CVD. Results strongly suggest that SDHs, especially SES, ethnicity, and gender, are sources of health inequality in the specific VDs of this study, according to the current literature. These three SDHs appear to be active in the four VDs analyzed. First of all, in the various VDs, a central role is played by the SES, and this can be explained by the close relationship between the individual health needs and the related social structure (Link and Phelan 1995). Moreover, SES, according to the sociological vision, is a fundamental cause (Cardano et al. 2020) of diseases, including vascular ones. It should be remembered that, by the fundamental causes of illness, in a sociological meaning, everything that arises as a factor of access to resources (such as money, knowledge, power, prestige, social capital, etc.) can be used for preventing or reducing the consequences of a disease once it has manifested (Link and Phelan 1995). Therefore, the SES in the VDs has the following effect: as long as the distribution of resources is unequal, and to the advantage of the most advantaged social groups, which enjoy greater resources, the inequity of health will continue to persist (Solar and Irwin 2010). Health differences due to socioeconomic factors appear when these differences are unevenly distributed among the different social classes. Thus, SES influences people’s attitudes, relations, etc., and SDHs are able to determine health issues (CSDH 2008). VDs may have real “feedback” on the social status related to vascular patients (Solar and Irwin 2010). An interesting element of our analysis concerns employment and VDs, and in particular, in the case of CVD. Importantly, occupation is one of the indicators that compose SES (Costa et al. 2022). Kunst and Mackenbach (2000) pointed out that the study of employment is important, as it defines not only the position in the social hierarchy and determines the place of people in the social hierarchy, but also the degree of risk to which one is exposed during the performance of work activities. This paper shows that the highest CVD rate is related to heavy jobs (health professionals, baker and biscuit makers, automobile assembler, and elementary workers), cleaning in food/lodging/tourism/entertainment, sports managers, environment/housekeeping/protection services, financial and insurance clerks, accounting and bookkeeping clerk and social assistance, and consultancy professional occupations (Wright et al. 2006; Jung et al. 2020). Thus, as for other types of diseases, also for VDs, the occupation is strictly connected to income and, consequently, this affects direct access to resources. Moreover, the relationship with health can be one of an effective interaction between economic resources, and therefore diseases, such as CVD, are found mostly in low job positions, often held by immigrants (CSDH 2008; Solar and Irwin 2010).
Considering ethnicity, in all VDs analyzed, a real differences and iniquities have been found. Ethnic differences, however, are the source not only of division, but mainly of social discrimination (Krieger 2001). The included papers, despite having been written in highly civilized countries, nevertheless underline the presence of ethnic discrimination, which leads to social exclusions, which act by affecting their own health status. As claimed in the literature, also in the VDs, oppressed ethnic groups register worse outcomes in terms of health status with respect to more privileged people (CSDH 2008).
Therefore, ethnic minorities in VDs continue to experience inequalities and a greater incidence of these diseases; moreover, they also continue to receive inferior quality of care with respect to nonminority groups due to the lack or lack of access to health insurance (Nelson 2002). Furthermore, the perceived stigma of ethnic minority groups leads to a significant devaluation and/or negative perception, not only of the quality of health care in VDs, but also as a major stressor and risk factor for vascular diseases (Moreira 2021). It should be emphasized that ethnicity, SES, and gender had a further negative correlation with the health status of patients with VDs and not only the various forms of stress. Moreover, the perception and experience of ethnic and economic marginalization impact the state of health, leading to its deterioration. In fact, in the included papers, it is possible to note how the individuals studied have experienced three main forms of stress: the dramaturgical one (Freund 1990), that is, the stress caused by the limited possibility of being able to control their own life; the effort–reward imbalance (Siegrist 1996) that is the condition for which there are not sufficient gratifications and acknowledgments on the working level; finally, chronic stress (Brunner et al. 1999), i.e., being placed in environments that threaten well-being, and adaptive responses to both escape and struggle are not punishable, and the negative consequences on health are considerable.
The last SDH analyzed was gender. Gender, as is well known, is culturally and socially defined, unlike sex, which is biologically determined. The fact that gender is culturally defined means that it is a source of different forms of discrimination and differentiation. In fact, discrimination related to gender issues can have negative effects on the health of women and sometimes on brutal events such as infanticide, genital mutilation, and several forms of violence. Moreover, gender binary divisions may also affect women’s health status through several biological and sociological determinants (CSDH 2008).
The interplay between sex-based biology and VDs is complex and not completely understood. For example, females, on average, present with PAD 10 to 20 years later than males, but PAD in postmenopausal females may even exceed that in males. Estrogen-mediated effects may play a protective role for premenopausal females in the development of PAD during fertility (Kim et al. 2022). AAA disease is also associated with a clear sex disparity, with a major prevalence in males but with worse short- and long-term mortality in females (Bulder et al. 2022). For CS, about 55,000 females are affected compared with males per year, and approximately 60% of all stroke deaths occur in females (Qaja et al. 2022). Therefore, there is evidence of a marked tendency of more severe complications for atherosclerotic disease (PAD, AAA, CS) in females. Conversely, the role of estrogens in females determines a major prevalence of CVD with respect to males. In fact, CVD prevalence can reach 77% in females and 57% in males (Serra et al. 2016; Costa et al. 2023).
From what has been observed, it is therefore necessary to implement CCIM personnel because “The key principles of CCIM include valuing diversity, developing the capacity for critical self-assessment about one’s own beliefs, being conscious of the inherent power dynamics that exist when different cultures interact, institutionalizing the idea that cultural knowledge is a continuum, and developing policies and methods of service delivery that reflect the high esteem with which culture and diversity is regarded” (Moreira 2021, p. 77). Furthermore, the results obtained are consistent with other studies that have dealt with SDHs in relation to other diseases such as cardiovascular diseases (Dewan et al. 2019).
A final and brief consideration concerns the different ways of studying VDs affecting the arterial system compared to the venous system with a very interesting sociological significance. Of the 22 articles included, 14 dealt with diseases affecting arteries, while only 8 dealt with diseases affecting the venous system. It is also an example of how illness is a cultural construct; in fact, social representations of aortic diseases, and therefore the conception of the same, primarily by health personnel, and more generally by the community, are considered much more dangerous and relevant than venous ones.
From a cultural point of view, in VDs, it should be considered that some subspecialties of VS such as venous surgery, used for CVD treatment, remain “Cinderella” subspecialties, and one could expect a lower standard of care with respect to other more appealing fields such as arterial surgery (used for PAD, CS, and AAA treatment) (Ballard and Bergan 2000), and this could affect the consciousness of being really ill and consequently the lack of seeking care among CVD patients.
5. Conclusions
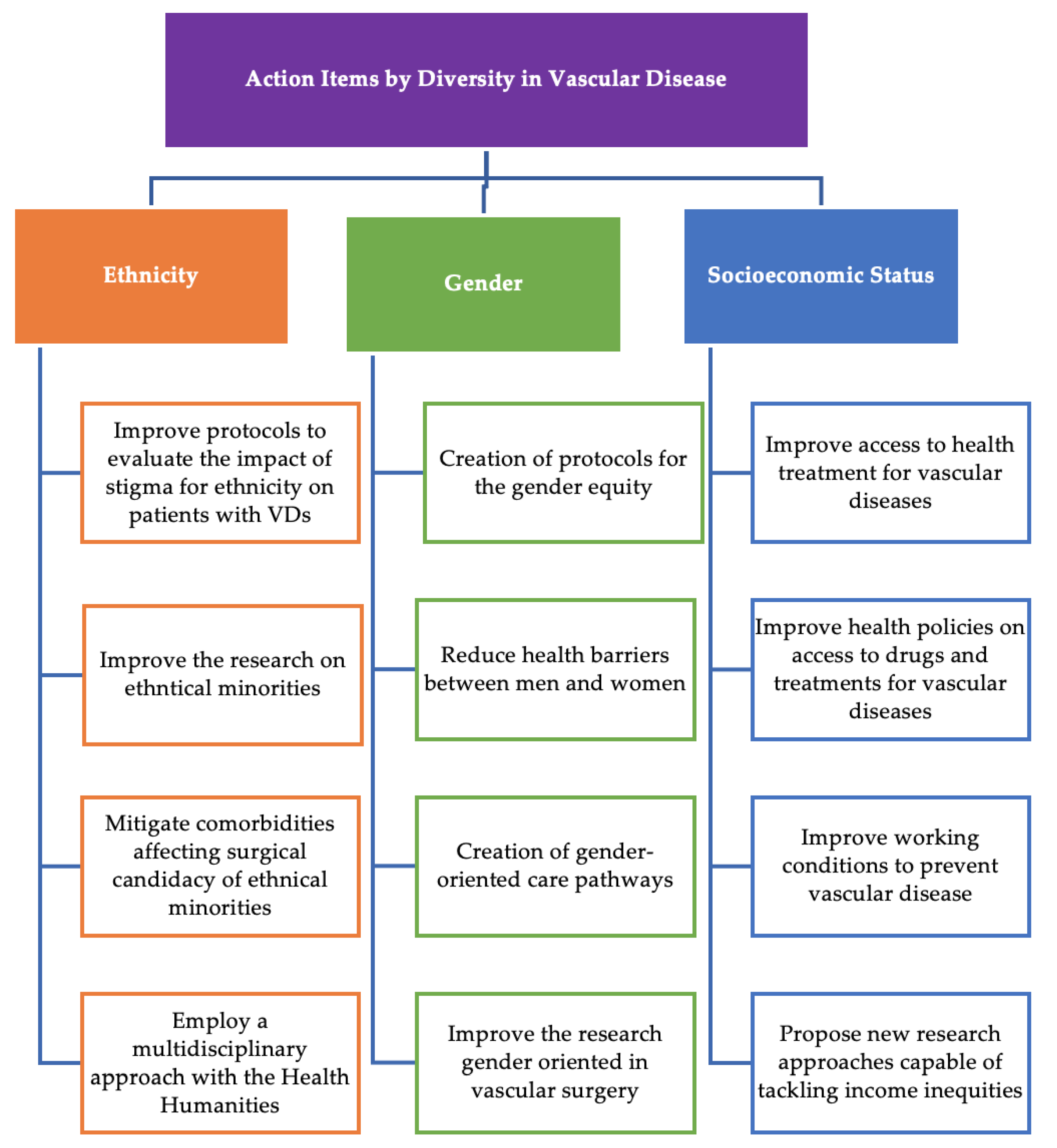
For the purposes of this systematic review, the attention was focused on the main forms of inequality on which health systems should act to improve health outcomes by applying the principles of cultural and inclusive competence in health (Figure 4).
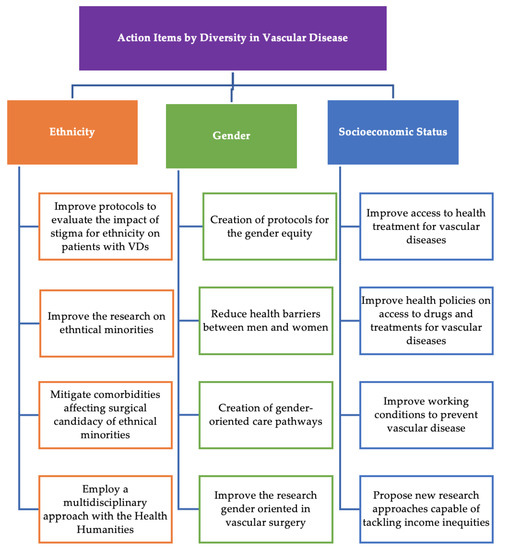
Figure 4.
Action Items on SDHs in VDs.
Thus, to manage the role of SDHs, it is important (1) to improve health care with the awareness of the SDHs of SES of gender and ethnicity and how these variables can impact VD, their management and progression; (2) to provide for a concrete multidisciplinary collaboration able of merging health knowledge with sociological knowledge, thus proposing a form of “Sociology with medicine” (Levine 1987) able of reading and analyzing the social and cultural component of VDs and (3) to provide concrete solutions in the management of SDHs in health with specific training courses aimed at transmitting the concept and concreteness of cultural competence in the management of SDHs.
Author Contributions
Conceptualization, D.C. and R.S.; methodology, D.C.; validation, D.C., N.I., E.B., S.C., L.C., G.T. and R.S.; formal analysis, D.C., and R.S.; investigation, D.C., N.I., E.B., S.C., L.C., G.T. and R.S.; data curation, D.C., and R.S.; writing—original draft preparation, D.C., N.I., E.B., S.C., L.C., G.T. and R.S.; writing—review and editing, D.C. and R.S; visualization, D.C., N.I., E.B., S.C., L.C., G.T. and R.S.; software, D.C.; supervision, R.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ballard, Jeffrey L., and John Bergan. 2000. Chronic Venous Insufficiency: Diagnosis and Treatment. Berlin/Heidelberg: Springer Science & Business Media. [Google Scholar]
- Barnes, Robert W. 1995. Vascular holism: The epidemiology of vascular disease. Annals of Vascular Surgery 9: 576–82. [Google Scholar] [CrossRef]
- Barshes, Neal, and Samantha Minc. 2021. Healthcare disparities in vascular surgery: A critical review. Journal of Vascular Surgery 74: 6S–14S. [Google Scholar] [CrossRef] [PubMed]
- Berkman, Lisa, Ichirō Kawachi, and Maria Glymour, eds. 2014. Social Epidemiology. New York: Oxford University Press. [Google Scholar]
- Blais, Claudia, Louis Rochette, Suzie Ouellet, and Thao Huynh. 2020. Complex Evolution of Epidemiology of Vascular Diseases, Including Increased Disease Burden: From 2000 to 2015. Canadian Journal of Cardiology 36: 740–46. [Google Scholar] [CrossRef]
- Brathwaite, Shayna, Lauren West-Livingston, D’Andre Williams, Channa Blakely, Jayne Rice, and Olamide Alabi. 2021. Moving forward: Recommendations to overcome existing structural racism. Journal of Vascular Surgery 74: 47S–55S. [Google Scholar] [CrossRef] [PubMed]
- Braveman, Paula. 2023. Social Determinants of Health and Health Disparities. New York: Oxford University Press. [Google Scholar]
- Brunner, Eric, Michael Shipley, David Blane, George Davey Smith, and Michael G. Marmot. 1999. When does cardiovascular risk start? Past and present socioeconomic circumstances and risk factors in adulthood. Journal of Epidemiology & Community Health 53: 757–64. [Google Scholar]
- Bulder, Ruth, Victoria Tedjawirja, Jaap Hamming, Mark Koelemay, Ron Balm, Jan Lindeman, and A Study Group Collaborators. 2022. Hypothesis of the High Mortality of Female Patients Following Elective Open Abdominal Aortic Aneurysm Repair. European Journal of Vascular and Endovascular Surgery 63: 773–74. [Google Scholar] [CrossRef] [PubMed]
- Camelo, Lidyane, Amanda Viana Machado, Dóra Chor, Rosane Harter Griep, José Geraldo Mill, Luisa Campos Caldeira Brant, and Sandhi Maria Barreto. 2022. Racial discrimination is associated with greater arterial stiffness and carotid intima-media thickness: The ELSA-Brasil study. Annals of Epidemiology 72: 40–47. [Google Scholar]
- Cardano, Mario, Giudo Giarelli, and Giovanna Vicarelli. 2020. Sociologia della Salute e della Medicina. Bologna: il Mulino, pp. 1–442. [Google Scholar]
- Cassel, John. 1976. The contribution of the Social environment to host resistance. American Journal of Epidemiology 104: 107–23. [Google Scholar] [CrossRef] [PubMed]
- Costa, Davide. 2023. Diversity and Health: Two Sides of the Same Coin. Italian Sociological Review 13: 69–90. [Google Scholar]
- Costa, Davide, Michele Andreucci, Nicola Ielapi, Giuseppe Filiberto, Serraino Pasquale, Mastroroberto Umberto, Marcello Bracale, and Raffaele Serra. 2023. Molecular Determinants of Chronic Venous Disease: A Comprehensive Review. International Journal of Molecular Sciences 24: 1928. [Google Scholar] [CrossRef]
- Costa, Davide, Nicola Ielapi, Francesco Caprino, Nicola Giannotta, Antonio Sisinni, Andrea Abramo, Lwanga Ssempijja, Michele Andreucci, Umberto Marcello Bracale, and Raffaele Serra. 2022. Social Aspects of Diabetic Foot: A Scoping Review. Social Sciences 11: 149. [Google Scholar]
- Criqui, Michael, H. Maritess, Jamosmos Arnost, Fronek Julie, O Denenberg, Robert D. Langer, John Bergan, and Beatrice A. Golomb. 2003. Chronic venous disease in an ethnically diverse population: The San Diego Population Study. American Journal of Epidemiology 158: 448–56. [Google Scholar] [CrossRef]
- Cross, Terry. 1989. Towards a Culturally Competent System of Care: A Monograph on Effective Services for Minority Children Who Are Severely Emotionally Disturbed. Washington, DC: ERIC—Education Resources Information Center. [Google Scholar]
- CSDH (Commision on Social Determinats of Health). 2008. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health—Final Report of the Commission on Social Determinants of Health. Genève: World Health Organization. Available online: https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1 (accessed on 10 January 2023).
- Davies, Huw O. B., Matthew Popplewell, Gareth Bate, Lisa Kelly, Andreas Koutsoumpelis, and Andrew W. Bradbury. 2017. Impact of UK NICE Clinical Guidelines 168 and social deprivation on access to interventional treatment for symptomatic varicose vein and specialist referral for leg ulceration. Phlebology 32: 548–52. [Google Scholar] [CrossRef] [PubMed]
- Demsas, Falen, Malachi M. Joiner, Kate Telma, Alyssa M. Flores, Semhar Teklu, and Elsie Gyang Ross. 2022. Disparities in peripheral artery disease care: A review and call for action. Seminars in Vascular Surgery 35: 141–54. [Google Scholar] [CrossRef] [PubMed]
- Dewan, Pooja, Rasmus Rørth, Pardeep S. Jhund, Joao Pedro Ferreira, Faiez Zannad, Li Shen, Lars Køber, William T. Abraham, Akshay S. Desai, Kenneth Dickstein, and et al. 2019. Income Inequality and Outcomes in Heart Failure: A Global Between-Country Analysis. JACC Heart Failure 7: 336–46. [Google Scholar] [CrossRef]
- de Weerd, Marjolein, Jaboba Greving, Anne De Jong, Erik Buskens, and Michiel Bots. 2009. Prevalence of asymptomatic carotid artery stenosis according to age and sex: Systematic review and metaregression analysis. Stroke 40: 1105–13. [Google Scholar] [CrossRef] [PubMed]
- Evans, C. J., F. G. R. Fowkes, C. V. Ruckley, and A. J. Lee. 1999. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. Journal of Epidemiology and Community Health 53: 149–53. [Google Scholar] [CrossRef] [PubMed]
- Federman, D. G., J. T. Trent, C. W. Froelich, J. Demirovic, and R. S. Kirsner. 1998. Epidemiology of peripheral vascular disease: A predictor of systemic vascular disease. Ostomy Wound Manage 44: 58–62. [Google Scholar]
- Freund, Peter. 1990. The expressive body: A common ground for the sociology of emotions and health and illness. Sociology of Health & Illness 12: 452–77. [Google Scholar]
- Haider, Adil, David Efron, Elliott Haut, Stephen DiRusso, Thomas Sullivan, and Edward Cornwell, III. 2007. Black children experience worse clinical and functional outcomes after traumatic brain injury: An analysis of the National Pediatric Trauma Registry. Journal of Trauma and Acute Care Surgery 62: 1259–63. [Google Scholar] [CrossRef]
- Hsu, Harold, Lu Tony, Hansraj Natasha, Russeau Andrew, Kougias Panagiotis, and Barshes Neal R. 2022. Gender, racial and ethnic disparities in index hospitalization operations for symptomatic carotid stenosis in Texas hospitals. Annals of Vascular Surgery 80: 152–57. [Google Scholar] [CrossRef]
- Jacomelli, Jo, Lisa Summers, Anne Stevenson, Timothy Lees, and Jonathan Earnshaw. 2017. Editor’s Choice—Inequalities in Abdominal Aortic Aneurysm Screening in England: Effects of Social Deprivation and Ethnicity. European Journal of Vascular and Endovascular Surgery: The Official Journal of the European Society for Vascular Surgery 53: 837–43. [Google Scholar] [CrossRef] [PubMed]
- Jung, Saemi, Youngki Kim, Dongmug Kang, Se Yeong, Kim Inah, Kim Eun, and Mi Kim. 2020. Distribution of working position among workers with varicose veins based on the National Health Insurance and National Employment Insurance data. Annals of Occupational and Environmental Medicine 32: e21. [Google Scholar] [CrossRef] [PubMed]
- Kim, Sooyeon, Anna Pendleton, and Katharine McGinigle. 2022. Women’s vascular health: Peripheral artery disease in female patients. Seminars in Vascular Surgery 35: 155–61. [Google Scholar] [CrossRef]
- Krieger, Nancy. 2001. Theories for social epidemiology in the 21st century: An ecosocial perspective. International Journal of Epidemiology 30: 668–77. [Google Scholar] [CrossRef] [PubMed]
- Kunst, Anton, and Jonathan Mackenbach. 2000. Measuring Socioeconomic Inequalities in Health. Copenhagen: WHO Regional Office Europe. [Google Scholar]
- Levine, Sol. 1987. The changing terrains in medical sociology: Emergent concern with quality of life. Journal of Health and Social Behavior 28: 1–6. [Google Scholar] [CrossRef] [PubMed]
- Li, Shimena R., Katherine M. Reitz, Jason Kennedy, Lucine Gabriel, Amanda R. Phillips, Paula K. Shireman, Mohammad H. Eslami, and Edith Tzeng. 2022. Epidemiology of age-, sex-, and race-specific hospitalizations for abdominal aortic aneurysms highlights gaps in current screening recommendations. Journal of Vascular Surgery 76: 1216–26. [Google Scholar] [PubMed]
- Link, Bruce George, and Jo Phelan. 1995. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 80–94. [Google Scholar] [CrossRef]
- Mackenbach, Johan. 2012. The persistence of health inequalities in modern welfare states: The explanation of a paradox. Social Science & Medicine 75: 761–69. [Google Scholar]
- Marcaccio, Cristina, and Marc Schermerhorn. 2021. Epidemiology of abdominal aortic aneurysms. Seminars in Vascular Surgery 34: 29–37. [Google Scholar] [CrossRef] [PubMed]
- Marmot, Michael. 2014. Review of Social Determinants and the Health Divide in the WHO European Region. Copenhagen: World Health Organization. Regional Office for Europe. [Google Scholar]
- Marmot, Michael. 2015. The health gap: The challenge of an unequal world. The Lancet 386: 2442–44. [Google Scholar] [CrossRef]
- Moreira, Carla. 2021. Developing cultural competency and maximizing its effect in vascular surgery. Journal of Vascular Surgery 74: 76S–85S. [Google Scholar] [CrossRef] [PubMed]
- Morin, Edgar. 2007. Restricted Complexity, General Complexity. Science and Us: Philosophy and Complexity. Singapore: World Scientific, pp. 1–25. [Google Scholar]
- Morrissey, Nicholas J., Jeannine Giacovelli, Natalia Egorova, Annetine Gelijns, Alan Moskowitz, James McKinsey, Kenneth Craig Kent, and Giampaolo Greco. 2007. Disparities in the treatment and outcomes of vascular disease in Hispanic patients. Journal of Vascular Surgery 46: 971–78. [Google Scholar] [CrossRef] [PubMed]
- Nelson, Alan. 2002. Unequal treatment: Confronting racial and ethnic disparities in health care. Journal of the National Medical Association 94: 666. [Google Scholar] [PubMed]
- Ohrlander, Tomasa Merlo Juanb, Henrik Ohlsson, Björna Sonesson, and Stefan Acosta. 2012. Socioeconomic position, comorbidity, and mortality in aortic aneurysms: A 13-year prospective cohort study. Annals of Vascular Surgery 26: 312–21. [Google Scholar] [CrossRef] [PubMed]
- Osborne, Nicholas H., Amit K. Mathur, Gilbert R. Upchurch, and Justin B. Dimick. 2010. Understanding the racial disparity in the receipt of endovascular abdominal aortic aneurysm repair. Archives of Urgery 145: 1105–8. [Google Scholar] [CrossRef] [PubMed]
- Osborne, Nicholas H., Gilbert R. Upchurch, Amit K. Mathur, and Justin B. Dimick. 2009. Explaining racial disparities in mortality after abdominal aortic aneurysm repair. Journal of Vascular Surgery 50: 709–13. [Google Scholar] [CrossRef] [PubMed]
- Ottersen, Ole Petter, Jashodhara Dasgupta, Chantal Blouin, Paulo Buss, Virasakdi Chongsuvivatwong, Julio Frenk, Sakiko Fukuda-Parr, Bience P. Gawanas, Rita Giacaman, John Gyapong, and et al. 2014. The political origins of health inequity: Prospects for change. The Lancet 383: 630–67. [Google Scholar] [CrossRef]
- Page, Matthew J., Joanne E. McKenzie, Patrick M. Bossuyt, Isabelle Boutron, Tammy C. Hoffmann, Cynthia D. Mulrow, Larissa Shamseer, Jennifer M. Tetzlaff, Elie A. Akl, Sue E. Brennan, and et al. 2021. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372: n71. [Google Scholar] [CrossRef]
- Paudel, Sudarshan, Anwar Zaitoun, Saif Al-Najafi, Thaer Musa, R. N. Dawn Light, Rajendra H. Mehta, and Howard S. Rosman. 2017. The association of gender with quality of health in peripheral arterial disease following peripheral vascular intervention. Vascular Disease Management 14: E218–E224. [Google Scholar]
- Qaja, Erion, Prasanna Tadi, and Theetha Pramod Kariyanna. 2022. Carotid Artery Stenosis. In StatPearls [Internet]. Treasure Island: StatPearls Publishing. [Google Scholar]
- Ramkumar, Niveditta, Bjoern Suckow, Shipra Arya, Art Sedrakyan, Todd Mackenzie, Philip Goodney, and Jeremiah Brown. 2020. Association of Sex with Repair Type and Long-Term Mortality in Adults with Abdominal Aortic Aneurysm. JAMA Network Open 3: e1921240. [Google Scholar] [CrossRef]
- Raphael, Dennis. 2006. Social determinants of health: Present status, unanswered questions, and future directions. International Journal of Health Services 36: 651–77. [Google Scholar] [CrossRef]
- Samson, David, and Karen Schoelles. 2012. Medical tests guidance (2) developing the topic and structuring systematic reviews of med-512 ical tests: Utility of PICOTS, analytic frameworks, decision trees, and other frameworks. Journal of General Internal Medcine 27: 11–19. [Google Scholar] [CrossRef]
- Sandiford, Peter, Damien Mosquera, and Dale Bramley. 2012. Ethnic inequalities in incidence, survival and mortality from abdominal aortic aneurysm in New Zealand. Journal of Epidemiol Community Health 66: 12. [Google Scholar] [CrossRef]
- Schul, Marlin W., Ted King, and Lowell Kabnick. 2014. Inequalities of health insurance guidelines for the treatment of symptomatic varicose veins. Phlebology 29: 236–46. [Google Scholar] [CrossRef]
- Serra, Raffaele, Raffaele Grande, Lucia Butrico, Franceso Fugetto, and Stefano de Franciscis. 2016. Epidemiology, diagnosis and treatment of chronic venous disease: A systematic review. Chirurgia 29: 34–45. [Google Scholar]
- Siegrist, Johannes. 1996. Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology 1: 27. [Google Scholar] [CrossRef] [PubMed]
- Solar, Orielle, and Alec Irwin. 2010. A conceptual Framework for Action on the Social Determinants of Health. Geneva: WHO Document Production Services. [Google Scholar]
- Tüchsen, Finn, Neal Krause, Hermann Burr, and Tage Kristensen. 2000. Standing at work and varicose veins. Scandinavian Journal of Work, Environment & Health 26: 414–20. [Google Scholar]
- Wilkinson, Richard, and Kate Pickett. 2006. Income inequality and population health: A review and explanation of the evidence. Social Science & Medicine 62: 1768–84. [Google Scholar]
- Wright, A. P., D. C. Berridge, and D. J. A. Scott. 2006. Return to work following varicose vein surgery: Influence of type of operation, employment and social status. European Journal of Vascular and Endovascular Surgery: The Official Journal of the European Society for Vascular Surgery 31: 553–57. [Google Scholar] [CrossRef]
- Ziaja, Damian, Mariola Sznapka, Joanna Grzela, Jacek Kostecki, Grzegorz Biolik, Krzysztof Pawlicki, Krzysztof Ziaja, Jerzy Chudek, Marek Maruszynski, Aleksander Molski, and et al. 2015. Regional variations of symptoms of the chronic venous disease among primary health care patients in Poland. Acta Angiologica 21: 31–39. [Google Scholar] [CrossRef]
- Zommorodi, Sayid, Karin Leander, Joy Roy, Johnny Steuer, and Rebecka Hultgren. 2018. Understanding abdominal aortic aneurysm epidemiology: Socioeconomic position affects outcome. Journal Epidemiol Community Health 72: 904–10. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).