CD4 T Cell-Mediated Immune Control of Cytomegalovirus Infection in Murine Salivary Glands
Abstract
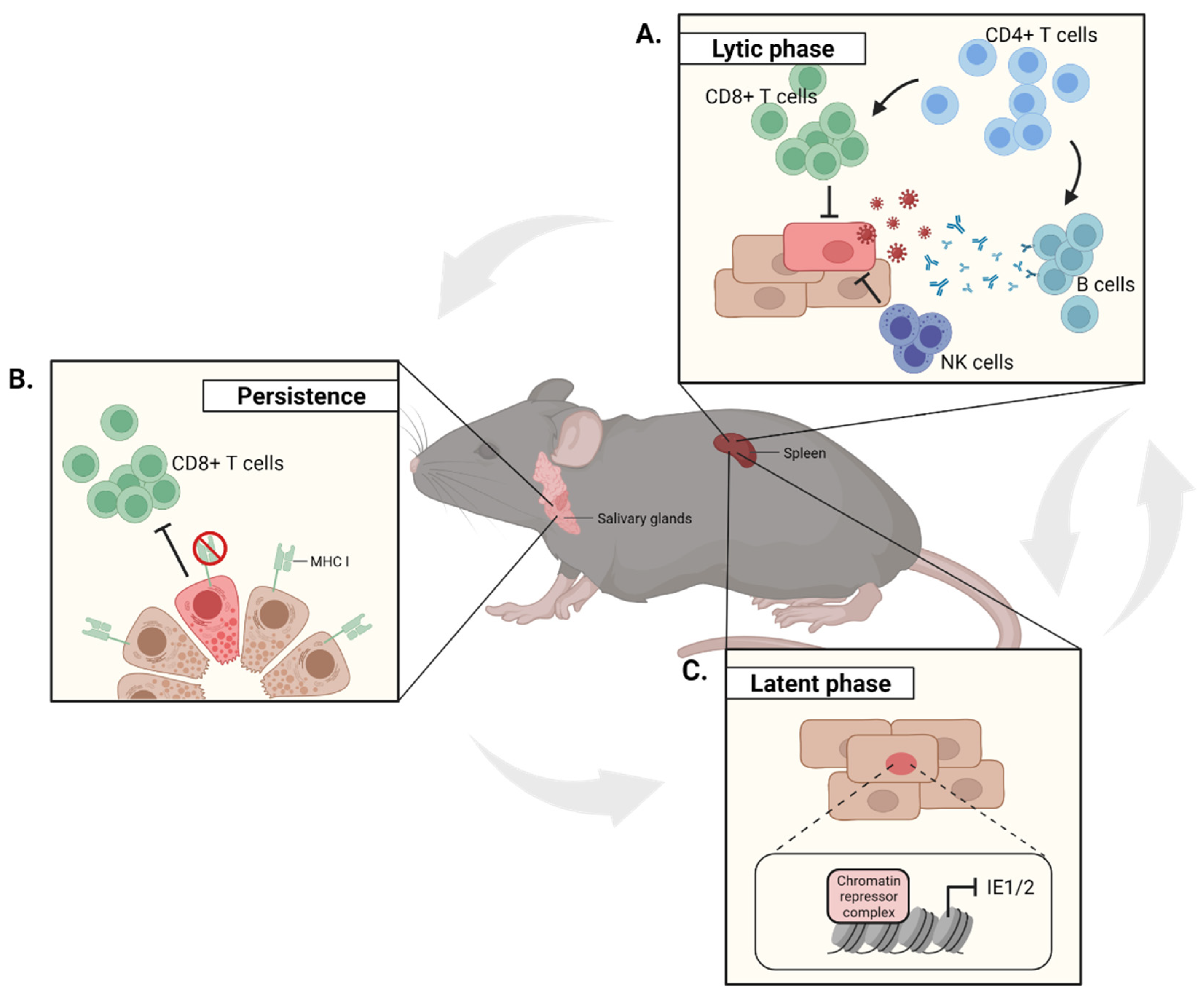
1. Introduction
2. Chemokine-Driven CD4 T Cell Dynamics in the SGs
3. Phenotype of the MCMV-Specific CD4 T Cell Response in the SGs
4. Mode of Action and Regulation of MCMV-Specific CD4 T Cells during Acute Infection
5. Late CD4 T Cell Responses during MCMV Infection
6. Conclusions and Outlook
Funding
Acknowledgments
Conflicts of Interest
References
- Zuhair, M.; Smit, G.S.A.; Wallis, G.; Jabbar, F.; Smith, C.; Devleesschauwer, B.; Griffiths, P. Estimation of the worldwide seroprevalence of cytomegalovirus: A systematic review and meta-analysis. Rev. Med. Virol. 2019, 29, e2034. [Google Scholar] [CrossRef] [PubMed]
- Pembrey, L.; Raynor, P.; Griffiths, P.; Chaytor, S.; Wright, J.; Hall, A.J. Seroprevalence of Cytomegalovirus, Epstein Barr Virus and Varicella Zoster Virus among Pregnant Women in Bradford: A Cohort Study. PLoS ONE 2013, 8, e81881. [Google Scholar] [CrossRef]
- Pamphilon, D.H.; Rider, J.R.; Barbara, J.A.J.; Williamson, L.M. Prevention of transfusion-transmitted cytomegalovirus infection. Transfus. Med. 1999, 9, 115–123. [Google Scholar] [CrossRef]
- Razonable, R.R.; Humar, A. Cytomegalovirus in solid organ transplantation. Am. J. Transplant. 2013, 3, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Lora, A.M.; Khine, J.; Khosrodad, N.; Yeldandi, V. Unusual Manifestations of Acute Cytomegalovirus Infection in Solid Organ Transplant Hosts: A Report of Two Cases. Case Rep. Transplant. 2017, 2017, 1–4. [Google Scholar] [CrossRef]
- Lee, K.H.; Kwon, D.E.; Do Han, K.; La, Y.; Han, S.H. Association between cytomegalovirus end-organ diseases and moderate-to-severe dementia: A population-based cohort study. BMC Neurol. 2020, 20, 216. [Google Scholar] [CrossRef] [PubMed]
- Manicklal, S.; Emery, V.C.; Lazzarotto, T.; Boppana, S.B.; Gupta, R.K. The “Silent” global burden of congenital cytomegalovirus. Clin. Microbiol. Rev. 2013, 26, 86–102. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Peng, G.; Bai, J.; He, B.; Huang, K.; Hu, X.; Liu, D. Cytomegalovirus Infection and Relative Risk of Cardiovascular Disease (Ischemic Heart Disease, Stroke, and Cardiovascular Death): A Meta-Analysis of Prospective Studies up to 2016. J. Am. Hear. Assoc. Cardiovasc. Cerebrovasc. Dis. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Mekker, A.; Tchang, V.S.; Haeberli, L.; Oxenius, A.; Trkola, A.; Karrer, U. Immune Senescence: Relative Contributions of Age and Cytomegalovirus Infection. PLoS Pathog. 2012, 8, e1002850. [Google Scholar] [CrossRef] [PubMed]
- Nikolich-Žugich, J.; Čicin-Šain, L.; Collins-McMillen, D.; Jackson, S.; Oxenius, A.; Sinclair, J.; Snyder, C.; Wills, M.; Lemmermann, N. Advances in cytomegalovirus (CMV) biology and its relationship to health, diseases, and aging. GeroScience 2020, 42, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Brune, W.; Hengel, H.; Koszinowski, U.H. A Mouse Model for Cytomegalovirus Infection. Curr. Protoc. Immunol. 2001, 43. [Google Scholar] [CrossRef]
- Rawlinson, W.D.; Farrell, H.E.; Barrell, B.G. Analysis of the complete DNA sequence of murine cytomegalovirus. J. Virol. 1996, 70, 8833–8849. [Google Scholar] [CrossRef] [PubMed]
- Stahl, F.R.; Heller, K.; Halle, S.; Keyser, K.A.; Busche, A.; Marquardt, A.; Wagner, K.; Boelter, J.; Bischoff, Y.; Kremmer, E.; et al. Nodular Inflammatory Foci Are Sites of T Cell Priming and Control of Murine Cytomegalovirus Infection in the Neonatal Lung. PLoS Pathog. 2013, 9, e1003828. [Google Scholar] [CrossRef]
- Stahl, F.R.; Keyser, K.A.; Heller, K.; Bischoff, Y.; Halle, S.; Wagner, K.; Messerle, M.; Förster, R. Mck2-dependent infection of alveolar macrophages promotes replication of MCMV in nodular inflammatory foci of the neonatal lung. Mucosal Immunol. 2015, 8, 57–67. [Google Scholar] [CrossRef]
- Campbell, A.E.; Cavanaugh, V.J.; Slater, J.S. The salivary glands as a privileged site of cytomegalovirus immune evasion and persistence. Med. Microbiol. Immunol. 2008, 197, 205–213. [Google Scholar] [CrossRef]
- Almanan, M.; Raynor, J.; Sholl, A.; Wang, M.; Chougnet, C.; Cardin, R.D.; Hildeman, D.A. Tissue-specific control of latent CMV reactivation by regulatory T cells. PLoS Pathog. 2017, 13, e1006507. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.F.; Wang, X.; Yan, S.; Zhang, Z.; Abecassis, M.; Hummel, M. Epigenetic Control of Cytomegalovirus Latency and Reactivation. Viruses 2013, 5, 1325. [Google Scholar] [CrossRef]
- Wills, M.R.; Poole, E.; Lau, B.; Krishna, B.; Sinclair, J.H. The immunology of human cytomegalovirus latency: Could latent infection be cleared by novel immunotherapeutic strategies? Cell. Mol. Immunol. 2014, 12, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Forte, E.; Zhang, Z.; Thorp, E.B.; Hummel, M. Cytomegalovirus Latency and Reactivation: An Intricate Interplay With the Host Immune Response. Front. Cell. Infect. Microbiol. 2020, 10, 130. [Google Scholar] [CrossRef]
- Jonjić, S.; Pavić, I.; Lucin, P.; Rukavina, D.; Koszinowski, U.H. Efficacious control of cytomegalovirus infection after long-term depletion of CD8+ T lymphocytes. J. Virol. 1990, 64. [Google Scholar] [CrossRef]
- Jonjic, S.; Mutter, W.; Weiland, F.; Reddehase, M.; Koszinowski, U.H. Site-restricted persistent cytomegalovirus infection after selective long-term depletion of CD4+ T lymphocytes. J. Exp. Med. 1989, 169, 1199–1212. [Google Scholar] [CrossRef]
- Cavanaugh, V.J.; Deng, Y.; Birkenbach, M.P.; Slater, J.S.; Campbell, A.E. Vigorous Innate and Virus-Specific Cytotoxic T-Lymphocyte Responses to Murine Cytomegalovirus in the Submaxillary Salivary Gland. J. Virol. 2003, 77, 1703–1717. [Google Scholar] [CrossRef] [PubMed]
- Arens, R.; Wang, P.; Sidney, J.; Loewendorf, A.; Sette, A.; Schoenberger, S.P.; Peters, B.; Benedict, C.A. Cutting Edge: Murine Cytomegalovirus Induces a Polyfunctional CD4 T Cell Response. J. Immunol. 2008, 180, 6472–6476. [Google Scholar] [CrossRef]
- Oderbolz, J.; Zangger, N.; Zimmermann, L.; Sandu, I.; Starruß, J.; Graw, F.; Oxenius, A. Locally confined IFNγ production by CD4+ T cells provides niches for murine cytomegalovirus replication in the salivary glands. bioRxiv 2021. [Google Scholar] [CrossRef]
- Humphreys, I.R.; De Trez, C.; Kinkade, A.; Benedict, C.A.; Croft, M.; Ware, C.F. Cytomegalovirus exploits IL-10-mediated immune regulation in the salivary glands. J. Exp. Med. 2007, 204, 1217–1225. [Google Scholar] [CrossRef]
- Jeitziner, S.M.; Walton, S.M.; Torti, N.; Oxenius, A. Adoptive transfer of cytomegalovirus-specific effector CD4+ T cells provides antiviral protection from murine CMV infection. Eur. J. Immunol. 2013, 43, 2886–2895. [Google Scholar] [CrossRef]
- Verma, S.; Weiskopf, D.; Gupta, A.; McDonald, B.; Peters, B.; Sette, A.; Benedict, C.A. Cytomegalovirus-Specific CD4 T Cells Are Cytolytic and Mediate Vaccine Protection. J. Virol. 2016, 90, 650. [Google Scholar] [CrossRef]
- McDermott, D.S.; Varga, S.M. Quantifying antigen-specific CD4 T cells during a viral infection: CD4 T cell responses are larger than we think. J. Immunol. 2011, 187, 5568–5576. [Google Scholar] [CrossRef] [PubMed]
- Thom, J.T.; Weber, T.C.; Walton, S.M.; Torti, N.; Oxenius, A. The Salivary Gland Acts as a Sink for Tissue-Resident Memory CD8+ T Cells, Facilitating Protection from Local Cytomegalovirus Infection. Cell Rep. 2015, 13, 1125–1136. [Google Scholar] [CrossRef] [PubMed]
- Loetscher, P.; Uguccioni, M.; Bordoli, L.; Baggiolini, M.; Moser, B.; Chizzolini, C.; Dayer, J.-M. CCR5 is characteristic of Th1 lymphocytes. Nature 1998, 391, 344–345. [Google Scholar] [CrossRef] [PubMed]
- Sallusto, F.; Lenig, D.; Mackay, C.; Lanzavecchia, A. Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. J. Exp. Med. 1998, 187, 875–883. [Google Scholar] [CrossRef]
- Weng, Y.; Siciliano, S.J.; Waldburger, K.E.; Sirotina-Meisher, A.; Staruch, M.J.; Daugherty, B.L.; Gould, S.L.; Springer, M.S.; DeMartino, J.A. Binding and functional properties of recombinant and endogenous CXCR3 chemokine receptors. J. Biol. Chem. 1998, 273, 18288–18291. [Google Scholar] [CrossRef]
- Cox, M.A.; Jenh, C.-H.; Gonsiorek, W.; Fine, J.; Narula, S.K.; Zavodny, P.J.; Hipkin, R.W. Human interferon-inducible 10-kDa protein and human interferon-inducible T cell alpha chemoattractant are allotopic ligands for human CXCR3: Differential binding to receptor states. Mol. Pharmacol. 2001, 59, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Groom, J.R.; Luster, A.D. CXCR3 ligands: Redundant, collaborative and antagonistic functions. Immunol. Cell Biol. 2011, 89, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; LaRosa, G.; Kassam, N.; Gordon, C.J.; Heath, H.; Ruffing, N.; Chen, H.; Humblias, J.; Samson, M.; Parmentier, M.; et al. Interaction of Chemokine Receptor CCR5 with its Ligands: Multiple Domains for HIV-1 gp120 Binding and a Single Domain for Chemokine Binding. J. Exp. Med. 1997, 186, 1373. [Google Scholar] [CrossRef]
- Clement, M.; Marsden, M.; Stacey, M.A.; Abdul-Karim, J.; Gimeno Brias, S.; Costa Bento, D.; Scurr, M.J.; Ghazal, P.; Weaver, C.T.; Carlesso, G.; et al. Cytomegalovirus-Specific IL-10-Producing CD4+ T Cells Are Governed by Type-I IFN-Induced IL-27 and Promote Virus Persistence. PLoS Pathog. 2016, 12, e1006050. [Google Scholar] [CrossRef]
- Caldeira-Dantas, S.; Furmanak, T.; Smith, C.; Quinn, M.; Teos, L.Y.; Ertel, A.; Kurup, D.; Tandon, M.; Alevizos, I.; Snyder, C.M. The Chemokine Receptor CXCR3 Promotes CD8+ T Cell Accumulation in Uninfected Salivary Glands but Is Not Necessary after Murine Cytomegalovirus Infection. J. Immunol. 2018, 200, 1133–1145. [Google Scholar] [CrossRef] [PubMed]
- Hokeness, K.L.; Deweerd, E.S.; Munks, M.W.; Lewis, C.A.; Gladue, R.P.; Salazar-Mather, T.P. CXCR3-Dependent Recruitment of Antigen-Specific T Lymphocytes to the Liver during Murine Cytomegalovirus Infection. J. Virol. 2007, 81. [Google Scholar] [CrossRef]
- Stolp, B.; Thelen, F.; Ficht, X.; Altenburger, L.M.; Ruef, N.; Krishna Inavalli, V.V.G.; Germann, P.; Page, N.; Moalli, F.; Raimondi, A.; et al. Salivary gland macrophages and tissue-resident CD8+ T cells cooperate for homeostatic organ surveillance. Sci. Immunol. 2020, 5. [Google Scholar] [CrossRef]
- Verstappen, G.M.; Pringle, S.; Bootsma, H.; Kroese, F.G.M. Epithelial–immune cell interplay in primary Sjögren syndrome salivary gland pathogenesis. Nat. Rev. Rheumatol. 2021, 17, 333–348. [Google Scholar] [CrossRef]
- Sfriso, P.; Oliviero, F.; Calabrese, F.; Miorin, M.; Facco, M.; Contri, A.; Cabrelle, A.; Baesso, I.; Cozzi, F.; Andretta, M.; et al. Epithelial CXCR3-B Regulates Chemokines Bioavailability in Normal, but Not in Sjögren’s Syndrome, Salivary Glands. J. Immunol. 2006, 176, 2581–2589. [Google Scholar] [CrossRef]
- Davis, A.S.W.; Roozen, H.N.; Dufort, M.J.; DeBerg, H.A.; Delaney, M.A.; Mair, F.; Erickson, J.R.; Slichter, C.K.; Berkson, J.D.; Klock, A.M.; et al. The human tissue-resident CCR5 + T cell compartment maintains protective and functional properties during inflammation. Sci. Transl. Med. 2019, 11. [Google Scholar] [CrossRef]
- Poole, E.; Atkins, E.; Nakayama, T.; Yoshie, O.; Groves, I.; Alcami, A.; Sinclair, J. NF-kappaB-mediated activation of the chemokine CCL22 by the product of the human cytomegalovirus gene UL144 escapes regulation by viral IE86. J. Virol. 2008, 82, 4250–4256. [Google Scholar] [CrossRef]
- Ushio, A.; Arakaki, R.; Otsuka, K.; Yamada, A.; Tsunematsu, T.; Kudo, Y.; Aota, K.; Azuma, M.; Ishimaru, N. CCL22-Producing Resident Macrophages Enhance T Cell Response in Sjögren’s Syndrome. Front. Immunol. 2018, 9, 2594. [Google Scholar] [CrossRef]
- Walton, S.M.; Mandaric, S.; Torti, N.; Zimmermann, A.; Hengel, H.; Oxenius, A. Absence of cross-presenting cells in the salivary gland and viral immune evasion confine cytomegalovirus immune control to effector CD4 T cells. PLoS Pathog. 2011, 7, e1002214. [Google Scholar] [CrossRef] [PubMed]
- Gamadia, L.E.; Remmerswaal, E.B.M.; Weel, J.F.; Bemelman, F.; Van Lier, R.A.W.; Ten Berge, I.J.M. Primary immune responses to human CMV: A critical role for IFN-γ-producing CD4+ T cells in protection against CMV disease. Blood 2003, 101. [Google Scholar] [CrossRef]
- Walton, S.M.; Wyrsch, P.; Munks, M.W.; Zimmermann, A.; Hengel, H.; Hill, A.B.; Oxenius, A. The Dynamics of Mouse Cytomegalovirus-Specific CD4 T Cell Responses during Acute and Latent Infection. J. Immunol. 2008, 181, 1128–1134. [Google Scholar] [CrossRef]
- Lucin, P.; Pavić, I.; Polić, B.; Jonjić, S.; Koszinowski, U.H. Gamma interferon-dependent clearance of cytomegalovirus infection in salivary glands. J. Virol. 1992, 66. [Google Scholar] [CrossRef]
- Smith, S.G.; Smits, K.; Joosten, S.A.; Van Meijgaarden, K.E.; Satti, I.; Fletcher, H.A.; Caccamo, N.; Dieli, F.; Mascart, F.; McShane, H.; et al. Intracellular cytokine staining and flow cytometry: Considerations for application in clinical trials of novel tuberculosis vaccines. PLoS ONE 2015, 10, e0138042. [Google Scholar] [CrossRef] [PubMed]
- Wehrens, E.J.; Wong, K.A.; Gupta, A.; Khan, A.; Benedict, C.A.; Zuniga, E.I. IL-27 regulates the number, function and cytotoxic program of antiviral CD4 T cells and promotes cytomegalovirus persistence. PLoS ONE 2018, 13, e0201249. [Google Scholar] [CrossRef]
- Gong, Y.-Z.; Nititham, J.; Taylor, K.; Miceli-Richard, C.; Sordet, C.; Wachsmann, D.; Bahram, S.; Georgel, P.; Criswell, L.A.; Sibilia, J.; et al. Differentiation of follicular helper T cells by salivary gland epithelial cells in primary Sjögren’s syndrome. J. Autoimmun. 2014, 51, 57–66. [Google Scholar] [CrossRef]
- Chen, L.; Flies, D.B. Molecular mechanisms of T cell co-stimulation and co-inhibition. Nat. Rev. Immunol. 2013, 13, 227–242. [Google Scholar] [CrossRef] [PubMed]
- Jost, N.H.; Abel, S.; Hutzler, M.; Sparwasser, T.; Zimmermann, A.; Roers, A.; Müller, W.; Klopfleisch, R.; Hengel, H.; Westendorf, A.M.; et al. Regulatory T cells and T-cell-derived IL-10 interfere with effective anti-cytomegalovirus immune response. Immunol. Cell Biol. 2014. [Google Scholar] [CrossRef] [PubMed]
- Chen, X. BALB/c mice have more CD4+CD25+ T regulatory cells and show greater susceptibility to suppression of their CD4+CD25- responder T cells than C57BL/6 mice. J. Leukoc. Biol. 2005, 78, 114–121. [Google Scholar] [CrossRef]
- Pavić, I.; Polić, B.; Crnković, I.; Lučin, P.; Jonjić, S.; Koszinowski, U.H. Participation of endogenous tumour necrosis factor α in host resistance to cytomegalovirus infection. J. Gen. Virol. 1993, 74, 2215–2223. [Google Scholar] [CrossRef][Green Version]
- Moran, A.E.; Holzapfel, K.L.; Xing, Y.; Cunningham, N.R.; Maltzman, J.S.; Punt, J.; Hogquist, K.A. T cell receptor signal strength in Treg and iNKT cell development demonstrated by a novel fluorescent reporter mouse. J. Exp. Med. 2011, 208, 1279. [Google Scholar] [CrossRef] [PubMed]
- Müller, A.J.; Filipe-Santos, O.; Eberl, G.; Aebischer, T.; Späth, G.F.; Bousso, P. CD4+ T cells rely on a cytokine gradient to control intracellular pathogens beyond sites of antigen presentation. Immunity 2012, 37, 147–157. [Google Scholar] [CrossRef]
- Schuster, I.S.; Wikstrom, M.E.; Brizard, G.; Coudert, J.D.; Estcourt, M.J.; Manzur, M.; O’Reilly, L.A.; Smyth, M.J.; Trapani, J.A.; Hill, G.R.; et al. TRAIL+ NK Cells Control CD4+ T Cell Responses during Chronic Viral Infection to Limit Autoimmunity. Immunity 2014, 41, 646–656. [Google Scholar] [CrossRef]
- Picarda, G.; Ghosh, R.; McDonald, B.; Verma, S.; Thiault, N.; El Morabiti, R.; Griffith, T.S.; Benedict, C.A. Cytomegalovirus Evades TRAIL-Mediated Innate Lymphoid Cell 1 Defenses. J. Virol. 2019, 93. [Google Scholar] [CrossRef]
- Teijaro, J.R.; Turner, D.; Pham, Q.; Wherry, E.J.; Lefrançois, L.; Farber, D.L. Cutting Edge: Tissue-Retentive Lung Memory CD4 T Cells Mediate Optimal Protection to Respiratory Virus Infection. J. Immunol. 2011, 187, 5510–5514. [Google Scholar] [CrossRef]
- Hiroi, T.; Fujihashi, K.; McGhee, J.R.; Kiyono, H. Characterization of cytokine-producing cells in mucosal effector sites: CD3+ T cells of Th1 and Th2 type in salivary gland-associated tissues. Eur. J. Immunol. 1994, 24, 2653–2658. [Google Scholar] [CrossRef]
- Jonjić, S.; Pavić, I.; Polic, B.; Crnković, I.; Lucin, P.; Koszinowski, U.H. Antibodies are not essential for the resolution of primary cytomegalovirus infection but limit dissemination of recurrent virus. J. Exp. Med. 1994, 179, 1713–1717. [Google Scholar] [CrossRef]
- Grewal, J.S.; Pilgrim, M.J.; Grewal, S.; Kasman, L.; Werner, P.; Bruorton, M.E.; London, S.D.; London, L. Salivary glands act as mucosal inductive sites via the formation of ectopic germinal centers after site-restricted MCMV infection. FASEB J. 2011, 25, 1680–1696. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, V.R.; Romão, V.C.; Agua-Doce, A.; Santos, M.J.; López-Presa, D.; Ferreira, A.C.; Fonseca, J.E.; Graca, L. The Ratio of Blood T Follicular Regulatory Cells to T Follicular Helper Cells Marks Ectopic Lymphoid Structure Formation While Activated Follicular Helper T Cells Indicate Disease Activity in Primary Sjögren’s Syndrome. Arthritis Rheumatol. 2018, 70, 774–784. [Google Scholar] [CrossRef] [PubMed]
- Pontarini, E.; Murray-Brown, W.J.; Croia, C.; Lucchesi, D.; Conway, J.; Rivellese, F.; Fossati-Jimack, L.; Astorri, E.; Prediletto, E.; Corsiero, E.; et al. Unique expansion of IL-21+ Tfh and Tph cells under control of ICOS identifies Sjögren’s syndrome with ectopic germinal centres and MALT lymphoma. Ann. Rheum. Dis. 2020, 79, 1588–1599. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.; Maerz, M.D.; Buckner, J.H. IL-6: A cytokine at the crossroads of autoimmunity. Curr. Opin. Immunol. 2018, 55, 9–14. [Google Scholar] [CrossRef] [PubMed]


| MCMV-Specific Populations | Sequence | Protein Family/Function | HCMV Homologue | Reported Cytokine Profile | Features | Ref. |
|---|---|---|---|---|---|---|
| m09133–147 | GYLYIYPSAGNSFDL | Glycoprotein family | − | IFNγ, IL-10 | Expand at later time point | [36] |
| M25409–423 | NHLYETPISATAMVI | Tegument protein | UL25 | IFNγ, IL-10 | - | [36] |
| M25411–425 | LYETPISATAMVIDI | Tegument protein | UL25 | IFNγ, TNFα | Immunodominant epitope | [24,29] |
| M78417–431 | SQQKMTSLPMSVFYS | UL78 family/transmembrane receptor homologue | UL78 | − | Show cytolytic phenotype in spleen but not in SG | [27] |
| m139560–574 | TRPYRYPRVCDASLS | US22 family homologue | − | IFNγ, IL-10 | − | [36] |
| m14224–38 | RSRYLTAAAVTAVLQ | US22 family homologue | − | IFNγ, IL-10 | − | [36] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zangger, N.; Oderbolz, J.; Oxenius, A. CD4 T Cell-Mediated Immune Control of Cytomegalovirus Infection in Murine Salivary Glands. Pathogens 2021, 10, 1531. https://doi.org/10.3390/pathogens10121531
Zangger N, Oderbolz J, Oxenius A. CD4 T Cell-Mediated Immune Control of Cytomegalovirus Infection in Murine Salivary Glands. Pathogens. 2021; 10(12):1531. https://doi.org/10.3390/pathogens10121531
Chicago/Turabian StyleZangger, Nathan, Josua Oderbolz, and Annette Oxenius. 2021. "CD4 T Cell-Mediated Immune Control of Cytomegalovirus Infection in Murine Salivary Glands" Pathogens 10, no. 12: 1531. https://doi.org/10.3390/pathogens10121531
APA StyleZangger, N., Oderbolz, J., & Oxenius, A. (2021). CD4 T Cell-Mediated Immune Control of Cytomegalovirus Infection in Murine Salivary Glands. Pathogens, 10(12), 1531. https://doi.org/10.3390/pathogens10121531






