Therapeutic Penetrating Keratoplasty in a Case of Corneal Perforation Caused by Colletotrichum gloeosporioides Infection
Abstract
:1. Introduction
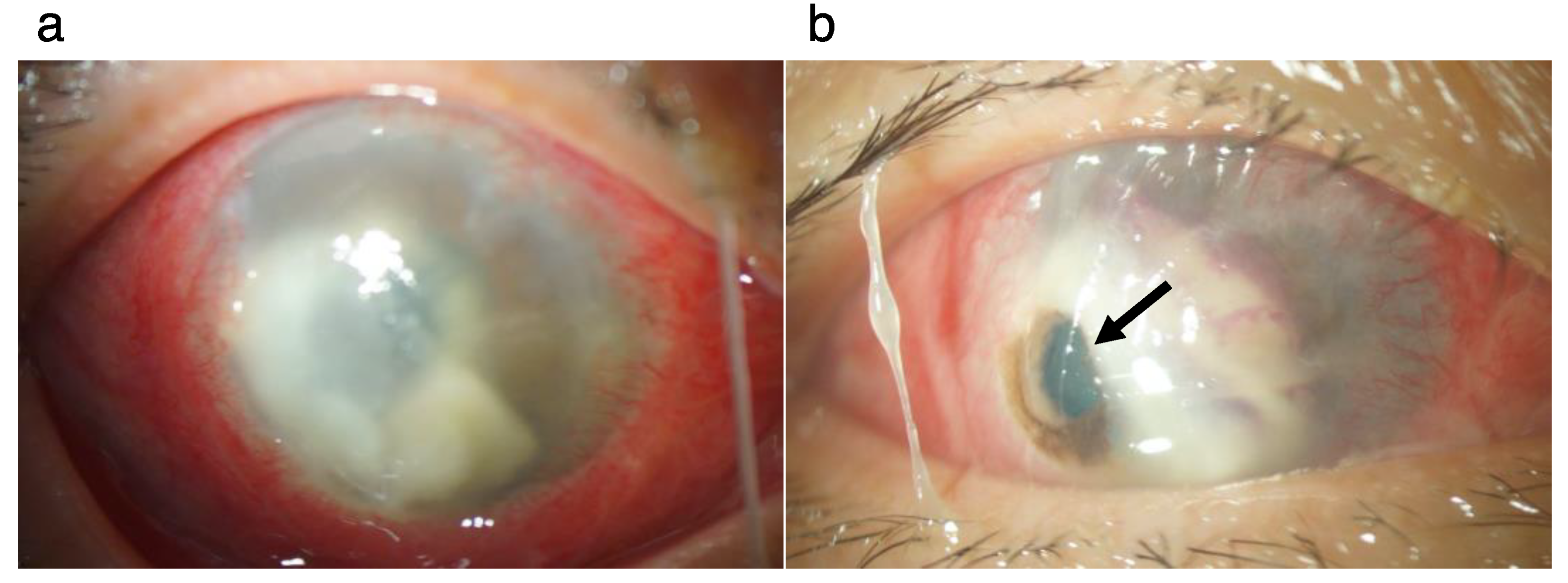
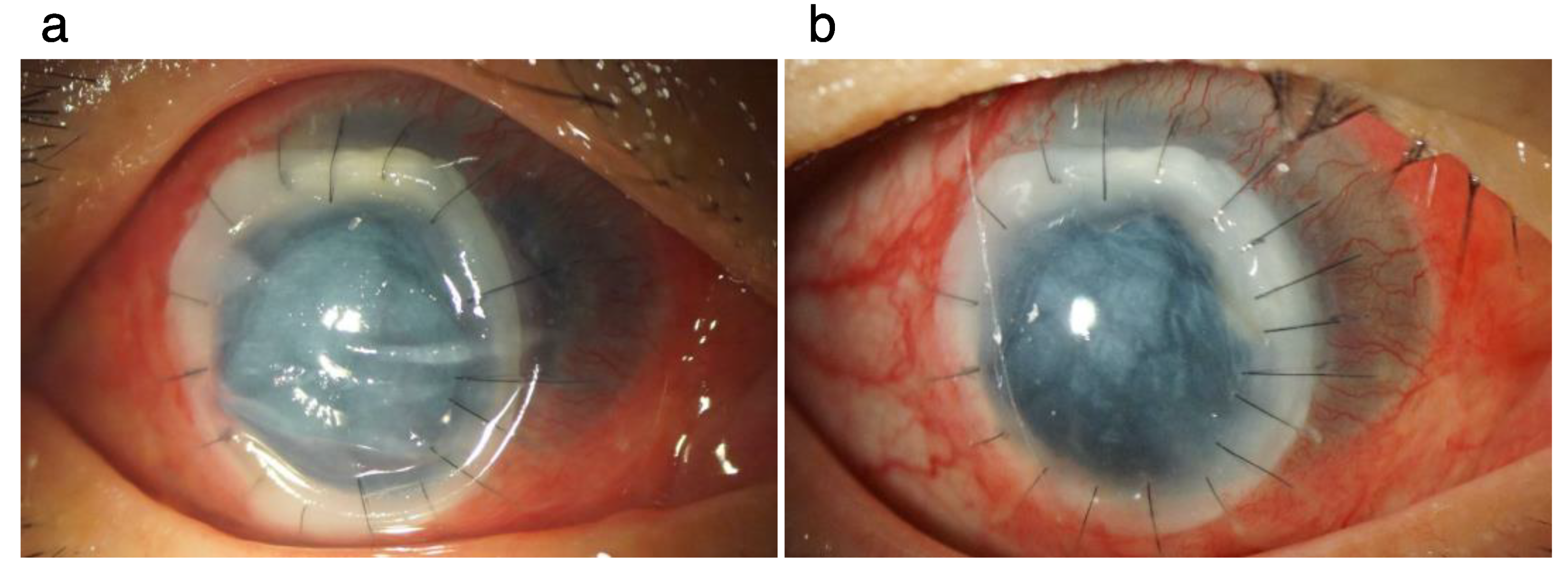
2. Clinical Course
2.1. Patinet
2.2. Surgical Procedure and Postoperative Course
2.3. Histopathology of the Affected Corneal Tissue
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- O’Quinn, R.P.; Hoffmann, J.L.; Boyd, A.S. Colletotrichum species as emerging opportunistic fungal pathogens: A report of 3 cases of phaeohyphomycosis and review. J. Am. Acad. Dermatol. 2001, 45, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Cano, J.; Guarro, J.; Gene, J. Molecular and morphological identification of Colletotrichum species of clinical interest. J. Clin. Microbiol. 2004, 42, 2450–2454. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, A.; Araki-Sasaki, K.; Mitani, A.; Miyamoto, H.; Sunada, A.; Ueda, A.; Asari, S.; Zheng, X.; Yamamoto, Y.; Hara, Y.; et al. Clinical characteristics of keratitis due to Colletotrichum gloeosporioides. J. Ocul. Pharmacol. Ther. 2011, 27, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Shivaprakash, M.R.; Appannanavar, S.B.; Dhaliwal, M.; Gupta, A.; Gupta, S.; Gupta, A.; Chakrabarti, A. Colletotrichum truncatum: An unusual pathogen causing mycotic keratitis and endophthalmitis. J. Clin. Microbiol. 2011, 49, 2894–2898. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Moriwaki, J.; Uzuhashi, S.; Degawa, Y.; Ono, T.; Nishimura, K. Molecular phylogenetic analyses and morphological re-examination of strains belonging to three rare Colletotrichum species in Japan. Microbiol. Cult. Coll. 2012, 28, 121–134. [Google Scholar]
- Kaliamurthy, J.; Kalavathy, C.M.; Ramalingam, M.D.; Prasanth, D.A.; Jesudasan, C.A.; Thomas, P.A. Keratitis due to a coelomycetous fungus: Case reports and review of the literature. Cornea 2004, 23, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Lamarca, J.; Vilaplana, F.; Nadal, J.; García-Barberán, I.; Barraquer, R.I. Treatment resistant fungal keratitis caused by Colletotrichum gloeosporioides. Arch. Soc. Esp. Oftalmol. 2016, 91, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Mitani, A.; Shiraishi, A.; Uno, T.; Miyamoto, H.; Hara, Y.; Yamaguchi, M.; Ohashi, Y. In vivo and in vitro investigations of fungal keratitis caused by Colletotrichum gloeosporioides. J. Ocul. Pharmacol. Ther. 2009, 25, 563–565. [Google Scholar] [CrossRef] [PubMed]
- Pote, S.T.; Chakraborty, A.; Lahiri, K.K.; Patole, M.S.; Deshmukh, R.A.; Shah, S.R. Keratitis by a rare pathogen Colletotrichum gloeosporioides: A case report. J. Mycol. Med. 2017, 27, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Matsumoto, T.; Ishibashi, Y. Fungal keratitis caused by Colletotrichum gloeosporioides. Cornea 2001, 20, 902–903. [Google Scholar] [CrossRef] [PubMed]
- Ritterband, D.C.; Shah, M.; Seedor, J.A. Colletotrichum graminicola: A new corneal pathogen. Cornea 1997, 16, 362–364. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, V.; Dursun, D.; Miller, D.; Alfonso, E.C. Colletotrichum keratitis. Am. J. Ophthalmol. 2002, 134, 435–438. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imai, K.; Sumioka, T.; Iwanishi, H.; Takada, Y.; Murata, S.; Iwamoto, R.; Okada, Y.; Saika, S. Therapeutic Penetrating Keratoplasty in a Case of Corneal Perforation Caused by Colletotrichum gloeosporioides Infection. Pathogens 2022, 11, 526. https://doi.org/10.3390/pathogens11050526
Imai K, Sumioka T, Iwanishi H, Takada Y, Murata S, Iwamoto R, Okada Y, Saika S. Therapeutic Penetrating Keratoplasty in a Case of Corneal Perforation Caused by Colletotrichum gloeosporioides Infection. Pathogens. 2022; 11(5):526. https://doi.org/10.3390/pathogens11050526
Chicago/Turabian StyleImai, Kazuki, Takayoshi Sumioka, Hiroki Iwanishi, Yukihisa Takada, Shin’ichi Murata, Ryuta Iwamoto, Yuka Okada, and Shizuya Saika. 2022. "Therapeutic Penetrating Keratoplasty in a Case of Corneal Perforation Caused by Colletotrichum gloeosporioides Infection" Pathogens 11, no. 5: 526. https://doi.org/10.3390/pathogens11050526





