Evaluation of a Tetracycline-Resistant E. coli Enumeration Method for Correctly Classifying E. coli in Environmental Waters in Kentucky, USA
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area and Sample Collection
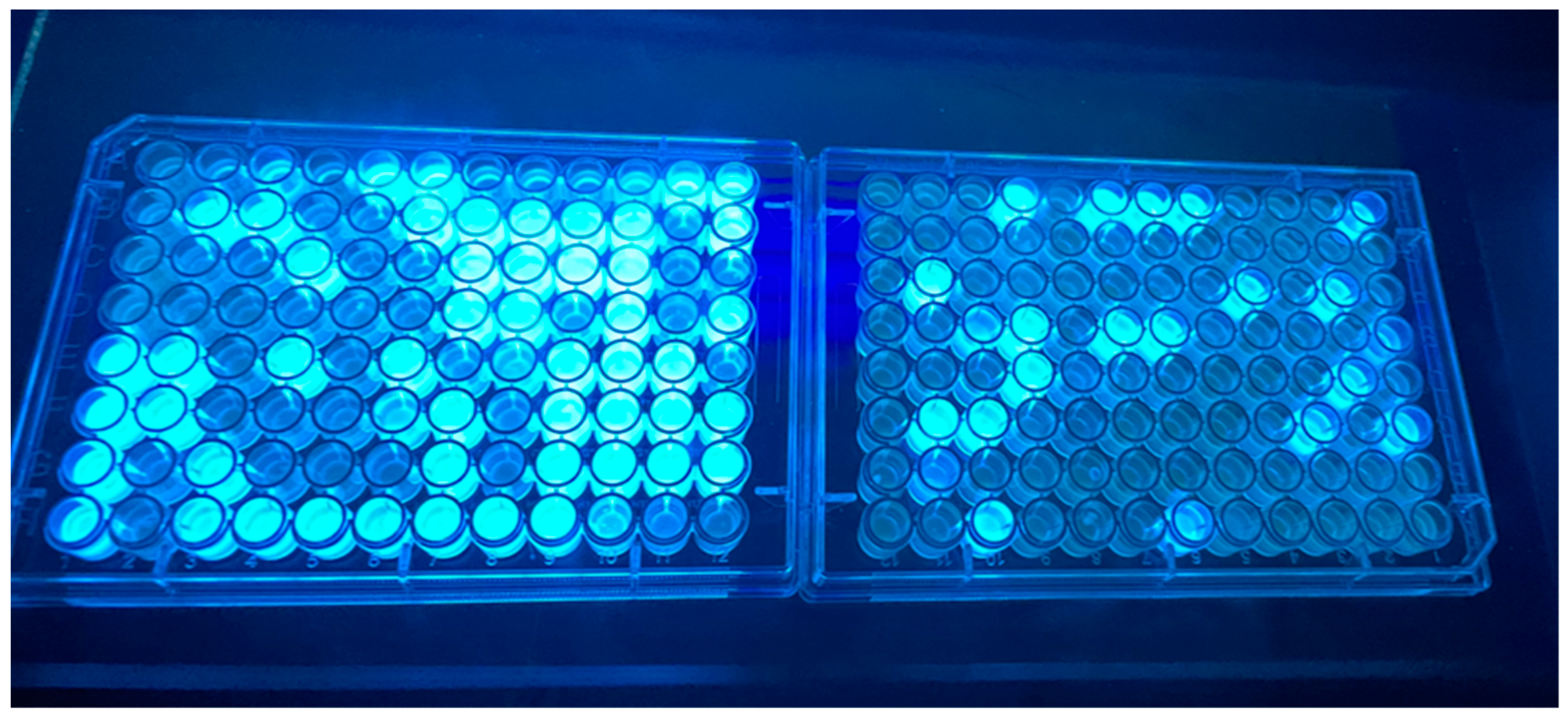
2.2. Obtaining Presumed E. coli and Tetracycline-Resistant E. coli Isolates
2.3. Species Identification
2.4. Assessment of Tetracycline Susceptibility/Resistance
2.5. Statistical Analysis
3. Results and Discussion
3.1. Species Identification of Isolates
3.2. Tetracycline Impact on E. coli Selection and Species Identification
3.3. Microbial Load and Likelihood of Selecting Non-Target Species as Isolates
3.4. Evaluation of Tetracycline Treatment for Screening Tetracycline-Resistant E. coli
3.5. E. coli Densities and Likelihood of Obtaining Tetracycline-Resistant Isolates
3.6. Challenges for Interpreting and Generalizing Species Identification Results
3.7. Value of Applying Tetracycline-Treated Culture-Based E. coli Detection Methods
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- CDC. Antibiotic Resistance Threats in the United States; U.S. Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019. Available online: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf (accessed on 11 July 2023).
- Patel, J.; Harant, A.; Fernandes, G.; Mwamelo, A.J.; Hein, W.; Dekker, D.; Sridhar, D. Measuring the global response to antimicrobial resistance, 2020–2021: A systematic governance analysis of 114 countries. Lancet Infect. Dis. 2023, 23, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Ashbolt, N.J.; Pruden, A.; Miller, J.H.; Riquelme, M.V.; Maile-Moskowitz, A. Antimicrobial resistance: Fecal sanitation strategies for combatting a global public health threat. In Global Water Pathogens Project; Part 3 Bacteria; Pruden, A., Ashbolt, N., Miller, J., Eds.; UNESCO and Michigan State University: East Lansing, MI, USA, 2018; Available online: https://www.waterpathogens.org/book/antimicrobal-resistance-fecal-sanitation-strategies-combatting-global-public-health-threat (accessed on 12 July 2023).
- Fuhrmeister, E.R.; Harvey, A.P.; Nadimpalli, M.L.; Gallandat, K.; Ambelu, A.; Arnold, B.F.; Brown, J.; Cumming, O.; Earl, A.M.; Kang, G.; et al. Evaluating the relationship between community water and sanitation access and the global burden of antibiotic resistance: An ecological study. Lancet Microbe 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Walsh, T.R.; Weeks, J.; Livermore, D.M.; Toleman, M.A. Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: An environmental point prevalence study. Lancet Infect. Dis. 2011, 11, 355–362. [Google Scholar] [CrossRef]
- Hendriksen, R.S.; Munk, P.; Njage, P.; Van Bunnik, B.; McNally, L.; Lukjancenko, O.; Röder, T.; Nieuwenhuijse, D.; Pedersen, S.K.; Kjeldgaard, J.; et al. Global monitoring of antimicrobial resistance based on metagenomics analyses of urban sewage. Nat. Comm. 2019, 10, 1124. [Google Scholar] [CrossRef]
- FDA; CDC; USDA. The National Antimicrobial Resistance Monitoring System: Strategic Plan 2021–2025; U.S. Department of Health and Human Services, FDA: Silver Spring, MD, USA, 2021. Available online: https://www.fda.gov/media/79976/download (accessed on 13 July 2023).
- White, A.; Hughes, J.M. Critical importance of a one health approach to antimicrobial resistance. EcoHealth 2019, 16, 404–409. [Google Scholar] [CrossRef]
- Singh, K.S.; Anand, S.; Dholpuria, S.; Sharma, J.K.; Blankenfeldt, W.; Shouche, Y. Antimicrobial resistance dynamics and the one-health strategy: A review. Environ. Chem. Lett. 2021, 19, 2995–3007. [Google Scholar] [CrossRef]
- Booton, R.D.; Meeyai, A.; Alhusein, N.; Buller, H.; Feil, E.; Lambert, H.; Mongkolsuk, S.; Pitchforth, E.; Reyher, K.K.; Sakcamduang, W.; et al. One Health drivers of antibacterial resistance: Quantifying the relative impacts of human, animal and environmental use and transmission. One Health 2021, 12, 100220. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Recommendations on Scientific, Analytical and Epidemiological Developments Relevant to the Parameters for Bathing Water Quality in the Bathing Water Directive (2006/7/EC)—Final Report; World Health Organization: Geneva, Switzerland, 2018. Available online: https://cdn.who.int/media/docs/default-source/wash-documents/who-recommendations-on-ec-bwd-august-2018.pdf?sfvrsn=5c9ce1e0_6 (accessed on 13 July 2023).
- U.S. EPA. Recreational Water Quality Criteria; U.S. Environmental Protection Agency Office of Water: Washington, DC, USA, 2012. Available online: https://www.epa.gov/sites/default/files/2015-10/documents/rwqc2012.pdf (accessed on 13 July 2023).
- WHO. Guidelines for Drinking-Water Quality—Fourth Edition Incorporating the First and Second Addenda; World Health Organizaton: Geneva, Switzerland, 2022. Available online: https://www.who.int/publications/i/item/9789240045064 (accessed on 13 July 2023).
- Liguori, K.; Keenum, I.; Davis, B.C.; Calarco, J.; Milligan, E.; Harwood, V.J.; Pruden, A. Antimicrobial resistance monitoring of water environments: A framework for standardized methods and quality control. Environ. Sci. Technol. 2022, 56, 9149–9160. [Google Scholar] [CrossRef]
- Paruch, L. Molecular Diagnostic Tools Applied for Assessing Microbial Water Quality. Int. J. Environ. Res. Public Health 2022, 19, 5128. [Google Scholar] [CrossRef]
- Bain, R.; Bartram, J.; Elliott, M.; Matthews, R.; McMahan, L.; Tung, R.; Chuang, P.; Gundry, S. A summary catalogue of microbial drinking water tests for low and medium resource settings. Int. J. Environ. Res. Public Health 2012, 9, 1609–1625. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Bir, A.; Bain, R.E. Novel methods for global water safety monitoring: Comparative analysis of low-cost, field-ready E. coli assays. Npj Clean Water 2020, 3, 9. [Google Scholar] [CrossRef]
- Dinh, Q.T.; Alliot, F.; Moreau-Guigon, E.; Eurin, J.; Chevreuil, M.; Labadie, P. Measurement of trace levels of antibiotics in river water using on-line enrichment and triple-quadrupole LC–MS/MS. Talanta 2011, 85, 1238–1245. [Google Scholar] [CrossRef]
- Brouwers, R.; Vass, H.; Dawson, A.; Squires, T.; Tavaddod, S.; Allen, R.J. Stability of β-lactam antibiotics in bacterial growth media. PLoS ONE 2020, 15, e0236198. [Google Scholar] [CrossRef]
- Amangelsin, Y.; Semenova, Y.; Dadar, M.; Aljofan, M.; Bjørklund, G. The Impact of Tetracycline Pollution on the Aquatic Environment and Removal Strategies. Antibiotics 2023, 12, 440. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Madec, J.Y.; Lupo, A.; Schink, A.K.; Kieffer, N.; Nordmann, P.; Schwarz, S. Antimicrobial resistance in Escherichia coli. Microbiol. Spectr. 2018, 6, 4. [Google Scholar] [CrossRef]
- Eastern Scientific. ColiGlow; Eastern Scientific: Richmond, KY, USA, 2023; Available online: http://www.coliglow.com (accessed on 14 July 2023).
- Mukherjee, M.; Gentry, T.; Mjelde, H.; Brooks, J.P.; Harmel, D.; Gregory, L.; Wagner, K. Escherichia coli antimicrobial resistance variability in water runoff and soil from a remnant native prairie, an improved pasture, and a cultivated agricultural watershed. Water 2020, 12, 1251. [Google Scholar] [CrossRef]
- Mukherjee, M.; Marie, L.; Liles, C.; Mustafa, N.; Bullerjahn, G.; Gentry, T.J.; Brooks, J.P. Elevated incidences of antimicrobial resistance and multidrug resistance in the Maumee River (Ohio, USA), a major tributary of Lake Erie. Microorganisms 2021, 9, 911. [Google Scholar] [CrossRef]
- U.S. EPA. Method 1603: Escherichia coli (E. coli) in Water by Membrane Filtration Using Modified membrane-Thermotolerant Escherichia coli Agar (Modified mTEC); U.S. Environmental Protection Agency, Office of Water: Washington, DC, USA, 2014. Available online: https://www.epa.gov/sites/default/files/2015-08/documents/method_1603_2009.pdf (accessed on 15 July 2023).
- Genter, F.; Marks, S.J.; Clair-Caliot, G.; Mugume, D.S.; Johnston, R.B.; Bain, R.E.; Julian, T.R. Evaluation of the Novel Substrate RUG™ for the Detection of Escherichia coli in Water from Temperate (Zurich, Switzerland) and Tropical (Bushenyi, Uganda) Field Sites. Environ. Sci. Water Res. Technol. 2019, 5, 1082–1091. [Google Scholar] [CrossRef]
- Altheide, S.T. Biochemical and culture-based approaches to identification in the diagnostic microbiology laboratory. Clin. Lab. Sci. 2019, 32, 166–175. [Google Scholar] [CrossRef]
- Topić Popović, N.; Kepec, S.; Kazazić, S.P.; Strunjak-Perović, I.; Bojanić, K.; Čož-Rakovac, R. Identification of environmental aquatic bacteria by mass spectrometry supported by biochemical differentiation. PLoS ONE 2022, 17, e0269423. [Google Scholar] [CrossRef]
- FDA; CDC; USDA. 2021 National Antimicrobial Resistance Monitoring System Interpretive Criteria for Susceptibility Testing; U.S. Department of Health and Human Services, FDA: Silver Spring, MD, USA, 2021. Available online: https://www.fda.gov/media/108180/download (accessed on 14 July 2023).
- CLSI Document M100-S20; Performance Standards for Antimicrobial Susceptibility Testing: 20th Informational Supplement. Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2010.
- Cayci, Y.T.; Ulker, K.H.; Birinci, A. Evaluation of three different methods for susceptibility testing of gentamicin in carbapenem resistant Enterobacterales. Le Infez. Med. 2021, 29, 568–573. [Google Scholar]
- García-Meniño, I.; Lumbreras, P.; Valledor, P.; Díaz-Jiménez, D.; Lestón, L.; Fernández, J.; Mora, A. Comprehensive statistical evaluation of Etest®, UMIC®, MicroScan and disc diffusion versus standard broth microdilution: Workflow for an accurate detection of Colistin-Resistant and Mcr-Positive E. coli. Antibiotics 2020, 9, 861. [Google Scholar] [CrossRef]
- Lee, M.; Chung, H.S. Different antimicrobial susceptibility testing methods to detect ertapenem resistance in Enterobacteriaceae: VITEK2, MicroScan, Etest, disk diffusion, and broth microdilution. J. Microbiol. Meth. 2015, 112, 87–91. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software, Release 14.; StataCorp LP.: College Station, TX, USA, 2015. [Google Scholar]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Chao, W.L. Evaluation of Colilert-18 for the detection of coliforms and Escherichia coli in tropical fresh water. Lett. Appl. Microbiol. 2006, 42, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Jefferson, R.A.; Burgess, S.M.; Hirsh, D. Beta-Glucuronidase from Escherichia coli as a Gene-Fusion Marker. Proc. Natl. Acad. Sci. USA 1986, 83, 8447–8451. [Google Scholar] [CrossRef]
- Frampton, E.W.; Restaino, L.; Blaszko, N. Evaluation of the β-Glucuronidase Substrate 5-Bromo-4-Chloro-3-Indolyl-β-D-Glucuronide (X-GLUC) in a 24-Hour Direct Plating Method for Escherichia coli. J. Food Prot. 1988, 51, 402–404. [Google Scholar] [CrossRef]
- Martins, M.T.; Rivera, I.G.; Clark, D.L.; Stewart, M.H.; Wolfe, R.L.; Olson, B.H. Distribution of uidA Gene Sequences in Escherichia coli Isolates in Water Sources and Comparison with the Expression of Beta-Glucuronidase Activity in 4-Methylumbelliferyl-beta-D-Glucuronide Media. Appl. Environ. Microbiol. 1993, 59, 2271–2276. [Google Scholar] [CrossRef]
- Rice, E.W.; Allen, M.J.; Edberg, S.C. Efficacy of Beta-Glucuronidase Assay for Identification of Escherichia coli by the Defined-Substrate Technology. Appl. Environ. Microbiol. 1990, 56, 1203–1205. [Google Scholar] [CrossRef] [PubMed]
- Frampton, E.W.; Restaino, L. Methods for Escherichia coli Identification in Food, Water and Clinical Samples Based on Beta-Glucuronidase Detection. J. Appl. Bacteriol. 1993, 74, 223–233. [Google Scholar] [CrossRef]
- Tryland, I.; Fiksdal, L. Enzyme Characteristics of β-D-Galactosidase-and β-D-Glucuronidase-Positive Bacteria and Their Interference in Rapid Methods for Detection of Waterborne Coliforms and Escherichia coli. Appl. Environ. Microbiol. 1998, 64, 1018–1023. [Google Scholar] [CrossRef]
- Bain, R.E.; Woodall, C.; Elliott, J.; Arnold, B.F.; Tung, R.; Morley, R.; du Preez, M.; Bartram, J.K.; Davis, A.P.; Gundry, S.W.; et al. Evaluation of an Inexpensive Growth Medium for Direct Detection of Escherichia coli in Temperate and Sub-Tropical Waters. PLoS ONE 2015, 10, e0140997. [Google Scholar] [CrossRef] [PubMed]
- Pitkänen, T.; Paakkari, P.; Miettinen, I.T.; Heinonen-Tanski, H.; Paulin, L.; Hänninen, M.L. Comparison of Media for Enumeration of Coliform Bacteria and Escherichia coli in Non-Disinfected Water. J. Microbiol. Methods 2007, 68, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Kämpfer, P.; Nienhüser, A.; Packroff, G.; Wernicke, F.; Mehling, A.; Nixdorf, K.; Fiedler, S.; Kolauch, C.; Esser, M. Molecular Identification of Coliform Bacteria Isolated from Drinking Water Reservoirs with Traditional Methods and the Colilert-18 System. Int. J. Hyg. Environ. Health 2008, 211, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Olstadt, J.; Schauer, J.J.; Standridge, J.; Kluender, S. A Comparison of Ten USEPA Approved Total Coliform/E. coli Tests. J. Water Health 2007, 5, 267–282. [Google Scholar] [CrossRef]
- Power, D.A.; Johnson, J.A. Difco™ & BBL™ Manual. Manual of Microbiological Culture Media, 3rd ed.; Becton, Dickinson and Company: Sparks, MD, USA, 2009; Volume 359, p. 60. [Google Scholar]
- Bonnet, M.; Lagier, J.C.; Raoult, D.; Khelaifia, S. Bacterial Culture through Selective and Non-Selective Conditions: The Evolution of Culture Media in Clinical Microbiology. New Microbes New Infect. 2020, 34, 100622. [Google Scholar] [CrossRef]
- Martínez, J.L. Effect of Antibiotics on Bacterial Populations: A Multi-Hierarchical Selection Process. F1000Research 2017, 6, 51. [Google Scholar] [CrossRef]
- Pisciotta, J.M.; Rath, D.F.; Stanek, P.A.; Flanery, D.M.; Harwood, V.J. Marine Bacteria Cause False-Positive Results in the Colilert-18 Rapid Identification Test for Escherichia coli in Florida Waters. Appl. Environ. Microbiol. 2002, 68, 539–544. [Google Scholar] [CrossRef]
- Sercu, B.; Van De Werfhorst, L.C.; Murray, J.L.; Holden, P.A. Cultivation-Independent Analysis of Bacteria in IDEXX Quanti-Tray/2000 Fecal Indicator Assays. Appl. Environ. Microbiol. 2011, 77, 627–633. [Google Scholar] [CrossRef]
- Tiwari, A.; Niemelä, S.I.; Vepsäläinen, A.; Rapala, J.; Kalso, S.; Pitkänen, T. Comparison of Colilert-18 with Miniaturized Most Probable Number Method for Monitoring of Escherichia coli in Bathing Water. J. Water Health 2016, 14, 121–131. [Google Scholar] [CrossRef]
- Chao, K.K.; Chao, C.C.; Chao, W.L. Evaluation of Colilert-18 for Detection of Coliforms and Eschericha coli in Subtropical Freshwater. Appl. Environ. Microbiol. 2004, 70, 1242–1244. [Google Scholar] [CrossRef] [PubMed]
- Chou, G. Effects of Land Use in the Ohio River Basin on the Distribution of Coliform and Antibiotic Resistant Bacteria in the Ohio River. Master’s Thesis, Marshall University, Huntington, WV, USA, 2011. Available online: https://mds.marshall.edu/etd/218 (accessed on 27 August 2023).
- Galvin, S.; Boyle, F.; Hickey, P.; Vellinga, A.; Morris, D.; Cormican, M. Enumeration and Characterization of Antimicrobial-Resistant Escherichia coli Bacteria in Effluent from Municipal, Hospital, and Secondary Treatment Facility Sources. Appl. Environ. Microbiol. 2010, 76, 4772–4779. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, T.; Savin, M.C. Populations of Antibiotic-Resistant Coliform Bacteria Change Rapidly in a Wastewater Effluent Dominated Stream. Sci. Total Environ. 2010, 408, 6192–6201. [Google Scholar] [CrossRef] [PubMed]
- Stocker, M.; Smith, J.; Pachepsky, Y. Spatial Variation of Tetracycline-Resistant E. coli and Relationships with Water Quality Variables in Irrigation Water: A Pilot Study. Appl. Microbiol. 2023, 3, 504–518. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; CLSI Supplement M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020. [Google Scholar]
- Sawant, A.A.; Hegde, N.V.; Straley, B.A.; Donaldson, S.C.; Love, B.C.; Knabel, S.J.; Jayarao, B.M. Antimicrobial-Resistant Enteric Bacteria from Dairy Cattle. Appl. Environ. Microbiol. 2007, 73, 156–163. [Google Scholar] [CrossRef]
- NCCLS Document M31-A2; Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals, 2nd ed. National Committee for Clinical Laboratory Standards: Wayne, PA, USA, 2002.
- Serwecińska, L. Antimicrobials and Antibiotic-Resistant Bacteria: A Risk to the Environment and to Public Health. Water 2020, 12, 3313. [Google Scholar] [CrossRef]
- Gullberg, E.; Cao, S.; Berg, O.G.; Ilbäck, C.; Sandegren, L.; Hughes, D.; Andersson, D.I. Selection of Resistant Bacteria at Very Low Antibiotic Concentrations. PLoS Pathog. 2011, 7, e1002158. [Google Scholar] [CrossRef]
- Lundström, S.V.; Östman, M.; Bengtsson-Palme, J.; Rutgersson, C.; Thoudal, M.; Sircar, T.; Blanck, H.; Eriksson, K.M.; Tysklind, M.; Flach, C.F.; et al. Minimal Selective Concentrations of Tetracycline in Complex Aquatic Bacterial Biofilms. Sci. Total Environ. 2016, 553, 587–595. [Google Scholar] [CrossRef]
- Duff, J.A.; Aslan, A.; Cohen, R.A. Land Use and Environmental Variables Influence Tetracycline-Resistant Bacteria Occurrence in Southeastern Coastal Plain Streams. J. Environ. Qual. 2019, 48, 1809–1816. [Google Scholar] [CrossRef]
- Di Cesare, A.; Eckert, E.M.; Rogora, M.; Corno, G. Rainfall Increases the Abundance of Antibiotic Resistance Genes within a Riverine Microbial Community. Environ. Pollut. 2017, 226, 473–478. [Google Scholar] [CrossRef]
- Williams, N.L.; Siboni, N.; McLellan, S.L.; Potts, J.; Scanes, P.; Johnson, C.; James, M.; McCann, V.; Seymour, J.R. Rainfall Leads to Elevated Levels of Antibiotic Resistance Genes within Seawater at an Australian Beach. Environ. Pollut. 2022, 307, 119456. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Agidi, S.; Marion, J.W.; Lee, J. Arcobacter in Lake Erie Beach Waters: An Emerging Gastrointestinal Pathogen Linked with Human-Associated Fecal Contamination. Appl. Environ. Microbiol. 2012, 78, 5511–5519. [Google Scholar] [CrossRef] [PubMed]
- Carney, R.L.; Labbate, M.; Siboni, N.; Tagg, K.A.; Mitrovic, S.M.; Seymour, J.R. Urban Beaches Are Environmental Hotspots for Antibiotic Resistance following Rainfall. Water Res. 2019, 167, 115081. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, C.M.; Tenover, F.C.; Miller, J.M. Parallel Comparison of Accuracy of API 20E, Vitek GNI, MicroScan Walk/Away Rapid ID, and Becton Dickinson Cobas Micro ID-E/NF for Identification of Members of the Family Enterobacteriaceae and Common Gram-Negative, Non-Glucose-Fermenting Bacilli. J. Clin. Microbiol. 1993, 31, 3165–3169. [Google Scholar] [CrossRef] [PubMed]
- Molina, F.; López-Acedo, E.; Tabla, R.; Roa, I.; Gómez, A.; Rebollo, J.E. Improved Detection of Escherichia coli and Coliform Bacteria by Multiplex PCR. BMC Biotechnol. 2015, 15, 48. [Google Scholar] [CrossRef]
- Osińska, A.; Korzeniewska, E.; Korzeniowska-Kowal, A.; Wzorek, A.; Harnisz, M.; Jachimowicz, P.; Buta-Hubeny, M.; Zieliński, W. The Challenges in the Identification of Escherichia coli from Environmental Samples and Their Genetic Characterization. Environ. Sci. Pollut. Res. 2023, 30, 11572–11583. [Google Scholar] [CrossRef]
- McLain, J.E.; Cytryn, E.; Durso, L.M.; Young, S. Culture-based methods for detection of antibiotic resistance in agroecosystems: Advantages, challenges, and gaps in knowledge. J. Environ. Qual. 2016, 45, 432–440. [Google Scholar] [CrossRef]
- Wuijts, S.; van den Berg, H.H.; Miller, J.; Abebe, L.; Sobsey, M.; Andremont, A.; Medlicott, K.O.; van Passel, M.W.; de Roda Husman, A.M. Towards a research agenda for water, sanitation and antimicrobial resistance. J. Water Health 2017, 15, 175–184. [Google Scholar] [CrossRef]
| Isolates from ColiGlow Wells without Tetracycline | Isolates from ColiGlow Wells with Tetracycline | |||
|---|---|---|---|---|
| Species (no.) | Susceptible | Resistant | Susceptible | Resistant |
| Escherichia coli (50) | 15 | 7 | 3 | 25 |
| Enterobacter cloacae (6) | 2 | 4 | 0 | 0 |
| Kluyvera ascorbate (1) | 0 | 1 | 0 | 0 |
| Kluyvera intermedia (1) | 1 | 0 | 0 | 0 |
| Klebsiella pneumoniae (1) | 0 | 1 | 0 | 0 |
| Serratia odorifera (1) | 0 | 1 | 0 | 0 |
| Citrobacter braakii (1) | 1 | 0 | 0 | 0 |
| Total (61) | 19 | 14 | 3 | 25 |
| Species Identification Reported by ID Method | Frequency (%) | |
|---|---|---|
| E. coli Density within Method Range | E. coli Density over Method Range | |
| E. coli | 38 (90.5%) | 12 (63.2%) |
| Not E. coli | 4 (9.5%) | 7 (37.8%) |
| Overall | 42 (100%) | 19 (100%) |
| Tetracycline Susceptibility | Frequency (%) | |
|---|---|---|
| E. coli Density within Method Range | E. coli Density over Method Range | |
| Tetracycline-Resistant | 23 (54.8%) | 16 (84.2%) |
| Tetracycline-Susceptible | 19 (45.2%) | 3 (15.8%) |
| Overall: All Isolates | 42 (100.0%) | 19 (100.0%) |
| Tetracycline-Resistant E. coli | 18 (52.6%) | 12 (100.0%) |
| Tetracycline-Susceptible E. coli | 20 (47.4%) | 0 (0%) |
| Overall: E. coli Isolates | 38 (100.0%) | 12 (100.0%) |
| Species Identification Reported | Frequency (%) | |
|---|---|---|
| API20E Identification Method | MicroScan Urine Panel-85 Identification Method | |
| E. coli | 30 (96.8%) | 20 (66.7%) |
| Not E. coli | 1 (3.2%) | 10 (33.3%) |
| Overall | 31 (100%) | 30 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boggs, C.; Shiferawe, K.; Karsten, E.; Hamlet, J.; Altheide, S.T.; Marion, J.W. Evaluation of a Tetracycline-Resistant E. coli Enumeration Method for Correctly Classifying E. coli in Environmental Waters in Kentucky, USA. Pathogens 2023, 12, 1090. https://doi.org/10.3390/pathogens12091090
Boggs C, Shiferawe K, Karsten E, Hamlet J, Altheide ST, Marion JW. Evaluation of a Tetracycline-Resistant E. coli Enumeration Method for Correctly Classifying E. coli in Environmental Waters in Kentucky, USA. Pathogens. 2023; 12(9):1090. https://doi.org/10.3390/pathogens12091090
Chicago/Turabian StyleBoggs, Callie, Kidus Shiferawe, Eckhardt Karsten, Jayden Hamlet, S. Travis Altheide, and Jason W. Marion. 2023. "Evaluation of a Tetracycline-Resistant E. coli Enumeration Method for Correctly Classifying E. coli in Environmental Waters in Kentucky, USA" Pathogens 12, no. 9: 1090. https://doi.org/10.3390/pathogens12091090
APA StyleBoggs, C., Shiferawe, K., Karsten, E., Hamlet, J., Altheide, S. T., & Marion, J. W. (2023). Evaluation of a Tetracycline-Resistant E. coli Enumeration Method for Correctly Classifying E. coli in Environmental Waters in Kentucky, USA. Pathogens, 12(9), 1090. https://doi.org/10.3390/pathogens12091090






