Viral Hepatitis: Host Immune Interaction, Pathogenesis and New Therapeutic Strategies
Abstract
:1. Introduction
2. Overview of Viral Hepatitis and Host–Pathogen Interactions
2.1. Hepatitis A Virus
2.2. Hepatitis B Virus
2.3. Hepatitis D Virus
2.4. Hepatitis C Virus
2.5. Hepatitis E Virus
3. Mechanisms of Viral Entry
3.1. Mechanisms of Viral Entry: Hepatitis B and Hepatitis D Viruses
3.2. Mechanisms of Viral Entry: Hepatitis C Virus
3.3. Mechanisms of Viral Entry: Hepatitis E Virus
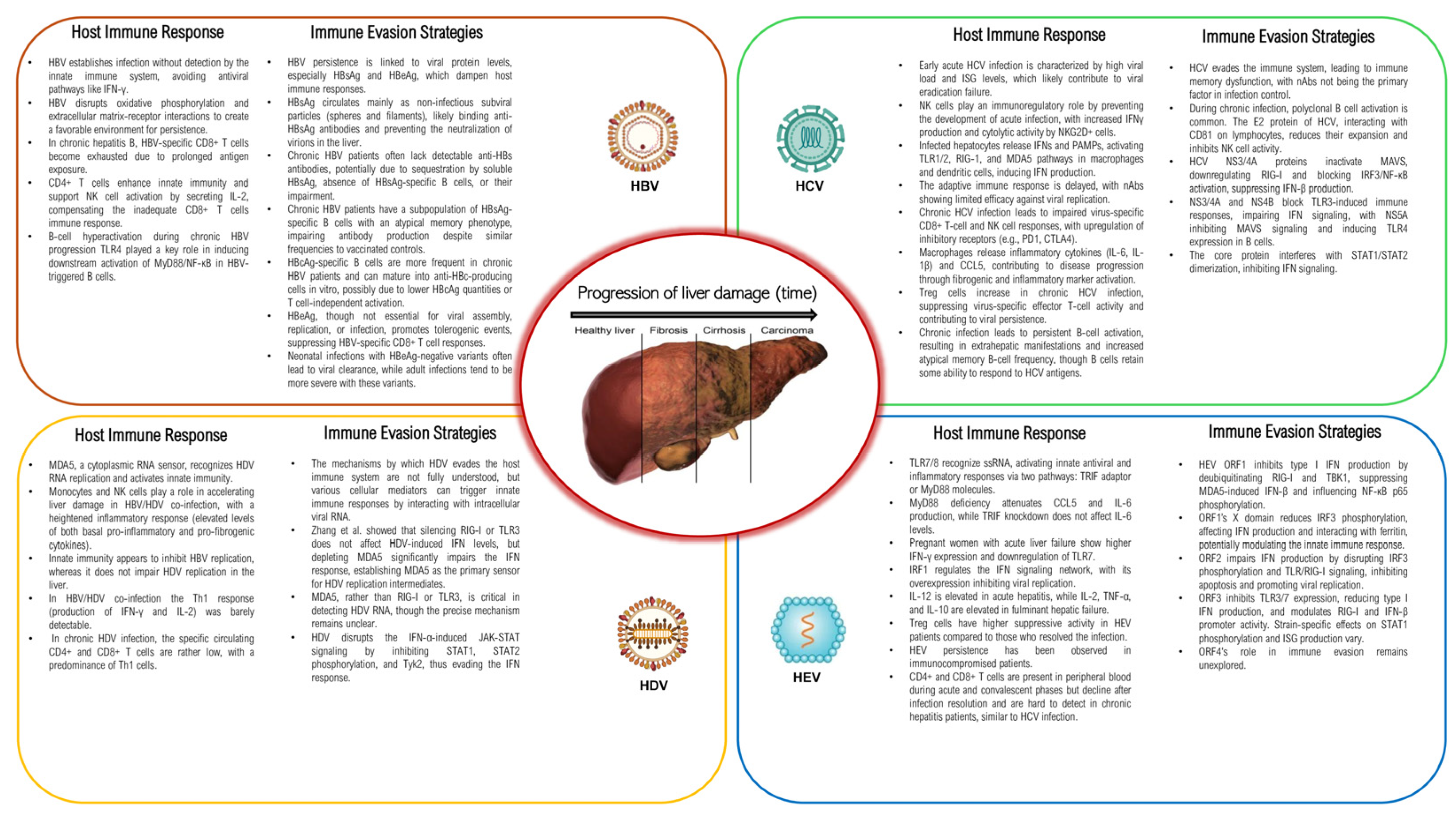
4. Host Immune Response
4.1. Innate and Adaptive Immune Response: Hepatitis B and Hepatitis D Viruses
4.2. Innate and Adaptive Immune Response: Hepatitis C Virus
4.3. Innate and Adaptive Immune Response: Hepatitis E Virus
5. Immune Evasion Strategies
5.1. Immune Evasion Strategies: Hepatitis B Virus
5.2. Immune Evasion Strategies: Hepatitis D Virus
5.3. Immune Evasion Strategies: Hepatitis C Virus
5.4. Immune Evasion Strategies: Hepatitis E Virus
6. Pathogenesis and Liver Damage
7. Current Therapies and Limitations and Emerging Therapeutic Strategies
| Virus | Antiviral Targets | Mechanism of Action | Example of Therapeutics | References |
|---|---|---|---|---|
| HAV | RNA-dependent RNA polymerase | Inhibits viral RNA synthesis | No specific approved antiviral therapy; supportive care | [234] |
| Immune modulation | Enhances host immune response | HAV vaccination (preventive), immune globulin | [235,236] | |
| HBV | Reverse Transcriptase | Inhibits DNA replication | Tenofovir, Entecavir, Lamivudine | [237,238] |
| HBsAg | Inhibits viral entry and immune evasion | Vaccination (preventive), pegylated interferon | [239,240] | |
| HCV | NS3/4A Protease | Inhibits viral polyprotein processing | Simeprevir, Grazoprevir | [241,242] |
| NS5B RNA-dependent RNA polymerase | Blocks viral RNA replication | Sofosbuvir | [243,244] | |
| NS5A Protein | Disrupts viral replication and assembly | Ledipasvir, Velpatasvir | [245,246] | |
| HDV | HDAg | Inhibits viral replication | Pegylated interferon, Bulevirtide (HDV entry inhibitor) | [247,248] |
| HBsAg (in HBV/HDV co-infection) | Prevents HDV assembly and release | HBV vaccination (indirect protection against HDV) | [249] | |
| HEV | RNA-dependent RNA polymerase | Inhibits viral RNA synthesis | Ribavirin (off-label use in severe cases) | [250] |
| Immune Modulation | Enhances host immune response | No specific approved antiviral therapy; supportive care | [251] |
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Global Hepatitis Report 2024: Action for Access in Low- and Middle-Income Countries. Available online: https://www.who.int/publications/i/item/9789240091672 (accessed on 13 July 2024).
- Cox, A.L.; El-Sayed, M.H.; Kao, J.-H.; Lazarus, J.V.; Lemoine, M.; Lok, A.S.; Zoulim, F. Progress towards elimination goals for viral hepatitis. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Global Health Sector Strategies. Available online: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/strategies/global-health-sector-strategies (accessed on 13 July 2024).
- Interim Guidance for Country Validation of Viral Hepatitis Elimination. Available online: https://www.who.int/publications/i/item/9789240028395 (accessed on 14 July 2024).
- Nassal, M. HBV cccDNA: Viral persistence reservoir and key obstacle for a cure of chronic hepatitis B. Gut 2015, 64, 1972–1984. [Google Scholar] [CrossRef] [PubMed]
- Iannacone, M.; Guidotti, L.G. Developing a cure for chronic hepatitis B requires a fresh approach. Nature 2022, 603, S49. [Google Scholar] [CrossRef] [PubMed]
- Dusheiko, G.; Agarwal, K.; Maini, M.K. New Approaches to Chronic Hepatitis B. N. Engl. J. Med. 2023, 388, 55–69. [Google Scholar] [CrossRef]
- Manns, M.P.; Maasoumy, B. Breakthroughs in hepatitis C research: From discovery to cure. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 533–550. [Google Scholar] [CrossRef]
- Page, K.; Melia, M.T.; Veenhuis, R.T.; Winter, M.; Rousseau, K.E.; Massaccesi, G.; Osburn, W.O.; Forman, M.; Thomas, E.; Thornton, K.; et al. Randomized Trial of a Vaccine Regimen to Prevent Chronic HCV Infection. N. Engl. J. Med. 2021, 384, 541–549. [Google Scholar] [CrossRef]
- Hepatitis. Available online: https://www.who.int/multi-media/details/elimination-of-hepatitis-by-2030 (accessed on 13 July 2024).
- Ghulam, F.; Zakaria, N.; Majeed, M.I.; Ismail, F.W. Viral Hepatitis—The Road Traveled and the Journey Remaining. Hepatic Med. Evid. Res. 2022, 14, 13–26. [Google Scholar] [CrossRef]
- Li, S.; Li, J.; Xu, Y.; Xiang, Z.; Wu, J. Editorial: Pathogen-host interaction in the development of viral hepatitis. Front. Cell. Infect. Microbiol. 2023, 13, 1333470. [Google Scholar] [CrossRef]
- Dancygier, H. Viral Infections by Nonhepatotropic Viruses. In Clinical Hepatology; Springer: Berlin/Heidelberg, Germany, 2010; pp. 823–830. [Google Scholar] [CrossRef]
- Wang, R.; Xie, Z. Non-hepatotropic viral hepatitis and its causative pathogens: The ongoing need for monitoring in children with severe acute hepatitis of unknown etiology. Pediatr. Investig. 2022, 6, 151–155. [Google Scholar] [CrossRef]
- Clinical Practice Guidelines Archives. EASL-The Home of Hepatology. 2023. Available online: https://easl.eu/publication-category/clinical-practice-guidelines/ (accessed on 29 July 2024).
- Melnick, J.L. Properties and classification of hepatitis A virus. Vaccine 1992, 10, S24–S26. [Google Scholar] [CrossRef]
- Zell, R.; Delwart, E.; Gorbalenya, A.E.; Hovi, T.; King, A.M.Q.; Knowles, N.J.; Lindberg, A.M.; Pallansch, M.A.; Palmenberg, A.C.; Reuter, G.; et al. ICTV Virus Taxonomy Profile: Picornaviridae. J. Gen. Virol. 2017, 98, 2421–2422. [Google Scholar] [CrossRef] [PubMed]
- Feinstone, S.M.; Kapikian, A.Z.; Purcell, R.H. Hepatitis A: Detection by Immune Electron Microscopy of a Viruslike Antigen Associated with Acute Illness. Science 1973, 182, 1026–1028. [Google Scholar] [CrossRef]
- Hepatitis A. Available online: https://www.who.int/news-room/fact-sheets/detail/hepatitis-a (accessed on 14 July 2024).
- The Immunological Basis for Immunization Series: Module 18—Hepatitis A. Available online: https://www.who.int/publications/i/item/97892516327 (accessed on 14 July 2024).
- CDC Hepatitis A Basics. Available online: https://www.cdc.gov/hepatitis-a/about/index.html (accessed on 25 July 2024).
- Lemon, S.M.; Ott, J.J.; Van Damme, P.; Shouval, D. Type A viral hepatitis: A summary and update on the molecular virology, epidemiology, pathogenesis and prevention. J. Hepatol. 2017, 68, 167–184. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, S.; Malirat, V.; Scodeller, E.; Mattion, N. First full-length genomic sequence of a hepatitis A virus isolated in Argentina shows recombination between subgenotypes IA and IB. Virus Res. 2011, 155, 316–324. [Google Scholar] [CrossRef]
- Lee, G.-Y.; Kim, W.-K.; Cho, S.; Park, K.; Kim, J.; Lee, S.-H.; Lee, J.; Lee, Y.-S.; Kim, J.H.; Byun, K.S.; et al. Genotyping and Molecular Diagnosis of Hepatitis A Virus in Human Clinical Samples Using Multiplex PCR-Based Next-Generation Sequencing. Microorganisms 2022, 10, 100. [Google Scholar] [CrossRef]
- 2016-2020 Number & Rates of Deaths with Hepatitis A Listed as Cause by Demographics|CDC. Available online: https://www.cdc.gov/hepatitis/statistics/2020surveillance/hepatitis-a/table-1.4.htm (accessed on 14 July 2024).
- Van Damme, P.; Pintó, R.M.; Feng, Z.; Cui, F.; Gentile, A.; Shouval, D. Hepatitis A virus infection. Nat. Rev. Dis. Prim. 2023, 9, 51. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, B.S.; Alter, H.J. A “New” Antigen in Leukemia Sera. JAMA 1965, 191, 541–546. [Google Scholar] [CrossRef]
- Iannacone, M.; Guidotti, L.G. Immunobiology and pathogenesis of hepatitis B virus infection. Nat. Rev. Immunol. 2022, 22, 19–32. [Google Scholar] [CrossRef]
- Tsukuda, S.; Watashi, K. Hepatitis B virus biology and life cycle. Antivir. Res. 2020, 182, 104925. [Google Scholar] [CrossRef]
- Hepatitis B Virus Variants|Nature Reviews Gastroenterology & Hepatology. Available online: https://www.nature.com/articles/nrgastro.2009.107 (accessed on 14 July 2024).
- Kim, B.K.; Revill, P.A.; Ahn, S.H. HBV Genotypes: Relevance to Natural History, Pathogenesis and Treatment of Chronic Hepatitis B. Antivir. Ther. 2011, 16, 1169–1186. [Google Scholar] [CrossRef]
- Liu, C.-J.; Kao, J.-H. Global Perspective on the Natural History of Chronic Hepatitis B: Role of Hepatitis B Virus Genotypes A to J. Semin. Liver Dis. 2013, 33, 097–102. [Google Scholar] [CrossRef]
- Mayerat, C.; Mantegani, A.; Frei, P.C. Does hepatitis B virus (HBV) genotype influence the clinical outcome of HBV infection? J. Viral Hepat. 1999, 6, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, O.E.; Widera, M.; Westhaus, S.; Timmer, L.; Korth, J.; Gerken, G.; Canbay, A.; Todt, D.; Steinmann, E.; Schwarz, T.; et al. Clinical Outcome and Viral Genome Variability of Hepatitis B Virus–Induced Acute Liver Failure. Hepatology 2019, 69, 993–1003. [Google Scholar] [CrossRef]
- Kao, J.-H.; Chen, P.-J.; Lai, M.-Y.; Chen, D.-S. Hepatitis B virus genotypes and spontaneous hepatitis B e antigen seroconversion in Taiwanese hepatitis B carriers. J. Med. Virol. 2004, 72, 363–369. [Google Scholar] [CrossRef]
- Sozzi, V.; Shen, F.; Chen, J.; Colledge, D.; Jackson, K.; Locarnini, S.; Yuan, Z.; Revill, P.A. In vitro studies identify a low replication phenotype for hepatitis B virus genotype H generally associated with occult HBV and less severe liver disease. Virology 2018, 519, 190–196. [Google Scholar] [CrossRef]
- Yuen, M.-F.; Chen, D.-S.; Dusheiko, G.M.; Janssen, H.L.A.; Lau, D.T.Y.; Locarnini, S.A.; Peters, M.G.; Lai, C.-L. Hepatitis B virus infection. Nat. Rev. Dis. Prim. 2018, 4, 18035. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, G.E.M.; Cabibbo, G.; Craxì, A. Hepatitis B Virus-Associated Hepatocellular Carcinoma. Viruses 2022, 14, 986. [Google Scholar] [CrossRef] [PubMed]
- Guidelines for the Prevention, Diagnosis, Care and Treatment for People with Chronic Hepatitis B Infection. Available online: https://www.who.int/publications/i/item/9789240090903 (accessed on 14 July 2024).
- Grossi, G.; Viganò, M.; Loglio, A.; Lampertico, P. Hepatitis B virus long-term impact of antiviral therapy nucleot(s)ide analogues (NUCs). Liver Int. 2017, 37, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Rizzetto, M.; Canese, M.G.; Arico, S.; Crivelli, O.; Trepo, C.; Bonino, F.; Verme, G. Immunofluorescence detection of new antigen-antibody system (delta/anti-delta) associated to hepatitis B virus in liver and in serum of HBsAg carriers. Gut 1977, 18, 997–1003. [Google Scholar] [CrossRef]
- Poison, A.G.; Bass, B.L.; Casey, J.L. RNA editing of hepatitis delta virus antigenome by dsRNA-adenosine deaminase. Nature 1996, 380, 454–456. [Google Scholar] [CrossRef]
- Otto, J.C.; Casey, P.J. The Hepatitis Delta Virus Large Antigen Is Farnesylated Both in Vitro and in Animal Cells. J. Biol. Chem. 1996, 271, 4569–4572. [Google Scholar] [CrossRef]
- Urban, S.; Neumann-Haefelin, C.; Lampertico, P. Hepatitis D virus in 2021: Virology, immunology and new treatment approaches for a difficult-to-treat disease. Gut 2021, 70, 1782–1794. [Google Scholar] [CrossRef] [PubMed]
- Kucirka, L.M.; Farzadegan, H.; Feld, J.J.; Mehta, S.H.; Winters, M.; Glenn, J.S.; Kirk, G.D.; Segev, D.L.; Nelson, K.E.; Marks, M.; et al. Prevalence, Correlates, and Viral Dynamics of Hepatitis Delta among Injection Drug Users. J. Infect. Dis. 2010, 202, 845–852. [Google Scholar] [CrossRef]
- Sellier, P.O.; Maylin, S.; Brichler, S.; Berçot, B.; Lopes, A.; Chopin, D.; Pogliaghi, M.; Munier, A.; Delcey, V.; Simoneau, G.; et al. Hepatitis B Virus-Hepatitis D Virus mother-to-child co-transmission: A retrospective study in a developed country. Liver Int. 2018, 38, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Le Gal, F.; Gault, E.; Ripault, M.-P.; Serpaggi, J.; Trinchet, J.-C.; Gordien, E.; Deny, P. Eighth Major Clade for Hepatitis Delta Virus. Emerg. Infect. Dis. 2006, 12, 1447–1450. [Google Scholar] [CrossRef]
- Wranke, A.; Pinheiro Borzacov, L.M.; Parana, R.; Lobato, C.; Hamid, S.; Ceausu, E.; Dalekos, G.N.; Rizzetto, M.; Turcanu, A.; Niro, G.A.; et al. Clinical and virological heterogeneity of hepatitis delta in different regions world-wide: The Hepatitis Delta International Network (HDIN). Liver Int. 2018, 38, 842–850. [Google Scholar] [CrossRef]
- Spaan, M.; Carey, I.; Bruce, M.; Shang, D.; Horner, M.; Dusheiko, G.; Agarwal, K. Hepatitis delta genotype 5 is associated with favourable disease outcome and better response to treatment compared to genotype 1. J. Hepatol. 2020, 72, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
- Rizzetto, M.; Hamid, S.; Negro, F. The changing context of hepatitis D. J. Hepatol. 2021, 74, 1200–1211. [Google Scholar] [CrossRef]
- Alfaiate, D.; Clément, S.; Gomes, D.; Goossens, N.; Negro, F. Chronic hepatitis D and hepatocellular carcinoma: A systematic review and meta-analysis of observational studies. J. Hepatol. 2020, 73, 533–539. [Google Scholar] [CrossRef]
- Hepcludex | European Medicines Agency (EMA). Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/hepcludex (accessed on 30 July 2024).
- Brunetto, M.R.; Ricco, G.; Negro, F.; Wedemeyer, H.; Yurdaydin, C.; Asselah, T.; Papatheodoridis, G.; Gheorghe, L.; Agarwal, K.; Farci, P.; et al. EASL Clinical Practice Guidelines on hepatitis delta virus. J. Hepatol. 2023, 79, 433–460. [Google Scholar] [CrossRef]
- Feinstone, S.M.; Kapikian, A.Z.; Purcell, R.H.; Alter, H.J.; Holland, P.V. Transfusion-Associated Hepatitis Not Due to Viral Hepatitis Type A or B. N. Engl. J. Med. 1975, 292, 767–770. [Google Scholar] [CrossRef]
- Choo, Q.-L.; Kuo, G.; Weiner, A.J.; Overby, L.R.; Bradley, D.W.; Houghton, M. Isolation of a cDNA cLone Derived from a Blood-Borne Non-A, Non-B Viral Hepatitis Genome. Science 1989, 244, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Houghton, M. Discovery of the hepatitis C virus. Liver Int. 2009, 29 (Suppl. S1), 82–88. [Google Scholar] [CrossRef]
- Thursz, M.; Fontanet, A. HCV transmission in industrialized countries and resource-constrained areas. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Marascio, N.; Mazzitelli, M.; Pavia, G.; Giancotti, A.; Barreca, G.S.; Costa, C.; Pisani, V.; Greco, G.; Serapide, F.; Trecarichi, E.M.; et al. Clinical, Virological Characteristics, and Outcomes of Treatment with Sofosbuvir/Ledipasvir in Two Pediatric Patients Infected by HCV Genotype 4. Cells 2019, 8, 416. [Google Scholar] [CrossRef]
- Moradpour, D.; Penin, F.; Rice, C.M. Replication of hepatitis C virus. Nat. Rev. Microbiol. 2007, 5, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Flaviviridae: Hepacivirus C Classification|ICTV. Available online: https://ictv.global/sg_wiki/flaviviridae/hepacivirus (accessed on 15 July 2024).
- Pawlotsky, J.M.; Negro, F.; Aghemo, A.; Berenguer, M.; Dalgard, O.; Dusheiko, G.; Marra, F.; Puoti, M.; Wedemeyer, H.; European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C: Final update of the series. J. Hepatol. 2020, 73, 1170–1218. [Google Scholar] [CrossRef] [PubMed]
- Galli, A.; Bukh, J. Mechanisms and Consequences of Genetic Variation in Hepatitis C Virus (HCV). Curr. Top. Microbiol. Immunol. 2023, 439, 237–264. [Google Scholar] [CrossRef]
- Falade-Nwulia, O.; Suarez-Cuervo, C.; Nelson, D.R.; Fried, M.W.; Segal, J.B.; Sulkowski, M.S. Oral Direct-Acting Agent Therapy for Hepatitis C Virus Infection: A Systematic Review. Ann. Intern. Med. 2017, 166, 637–648. [Google Scholar] [CrossRef]
- Zhang, H.; Quadeer, A.A.; McKay, M.R. Direct-acting antiviral resistance of Hepatitis C virus is promoted by epistasis. Nat. Commun. 2023, 14, 7457. [Google Scholar] [CrossRef]
- Marascio, N.; Pavia, G.; Romeo, I.; Talarico, C.; Di Salvo, S.; Reale, M.; Marano, V.; Barreca, G.S.; Fabiani, F.; Perrotti, N.; et al. Real-life 3D therapy failure: Analysis of NS5A 93H RAS plus 108 K polymorphism in complex with ombitasvir by molecular modeling. J. Med. Virol. 2018, 90, 1257–1263. [Google Scholar] [CrossRef]
- Marascio, N.; Pavia, G.; Strazzulla, A.; Dierckx, T.; Cuypers, L.; Vrancken, B.; Barreca, G.S.; Mirante, T.; Malanga, D.; Oliveira, D.M.; et al. Detection of Natural Resistance-Associated Substitutions by Ion Semiconductor Technology in HCV1b Positive, Direct-Acting Antiviral Agents-Naïve Patients. Int. J. Mol. Sci. 2016, 17, 1416. [Google Scholar] [CrossRef] [PubMed]
- Romeo, I.; Marascio, N.; Pavia, G.; Talarico, C.; Costa, G.; Alcaro, S.; Artese, A.; Torti, C.; Liberto, M.C.; Focà, A. Structural Modeling of New Polymorphism Clusters of HCV Polymerase Isolated from Direct-Acting Antiviral Naïve Patients: Focus on Dasabuvir and Setrobuvir Binding Affinity. ChemistrySelect 2018, 3, 6009–6017. [Google Scholar] [CrossRef]
- Tam, A.W.; Smith, M.M.; Guerra, M.E.; Huang, C.-C.; Bradley, D.W.; Fry, K.E.; Reyes, G.R. Hepatitis E virus (HEV): Molecular cloning and sequencing of the full-length viral genome. Virology 1991, 185, 120–131. [Google Scholar] [CrossRef]
- Smith, D.B.; Simmonds, P.; Members of the International Committee on the Taxonomy of Viruses Hepeviridae Study Group; Jameel, S.; Emerson, S.U.; Harrison, T.J.; Meng, X.-J.; Okamoto, H.; Van der Poel, W.H.M.; Purdy, M.A. Consensus proposals for classification of the family Hepeviridae. J. Gen. Virol. 2015, 96, 1191–1192. [Google Scholar] [CrossRef] [PubMed]
- Balayan, M.S.; Andjaparidze, A.G.; Savin Skaya, S.S.; Ketiladze, E.S.; Braginsky, D.M.; Suavinov, A.P.; Poleschuk, V.F. Evidence for a Virus in Non-A, Non-B Hepatitis Transmitted via the Fecal-Oral Route. Intervirology 1983, 20, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Purcell, R.H.; Emerson, S.U. Identification of the 5′ terminal sequence of the SAR-55 and MEX-14 strains of hepatitis E virus and confirmation that the genome is capped. J. Med. Virol. 2001, 65, 293–295. [Google Scholar] [CrossRef]
- Panda, S.K.; Thakral, D.; Rehman, S. Hepatitis E virus. Rev. Med. Virol. 2007, 17, 151–180. [Google Scholar] [CrossRef]
- Nimgaonkar, I.; Ding, Q.; Schwartz, R.E.; Ploss, A. Hepatitis E virus: Advances and challenges. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 96–110. [Google Scholar] [CrossRef]
- Muñoz-Chimeno, M.; Cenalmor, A.; Garcia-Lugo, M.A.; Hernandez, M.; Rodriguez-Lazaro, D.; Avellon, A. Proline-Rich Hypervariable Region of Hepatitis E Virus: Arranging the Disorder. Microorganisms 2020, 8, 1417. [Google Scholar] [CrossRef]
- Li, T.C.; Yamakawa, Y.; Suzuki, K.; Tatsumi, M.; Razak, M.A.; Uchida, T.; Takeda, N.; Miyamura, T. Expression and self-assembly of empty virus-like particles of hepatitis E virus. J. Virol. 1997, 71, 7207–7213. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Takahashi, M.; Hoshino, Y.; Takahashi, H.; Ichiyama, K.; Nagashima, S.; Tanaka, T.; Okamoto, H. ORF3 protein of hepatitis E virus is essential for virion release from infected cells. J. Gen. Virol. 2009, 90, 1880–1891. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.B.; Simmonds, P.; Izopet, J.; Oliveira-Filho, E.F.; Ulrich, R.G.; Johne, R.; Koenig, M.; Jameel, S.; Harrison, T.J.; Meng, X.-J.; et al. Proposed reference sequences for hepatitis E virus subtypes. J. Gen. Virol. 2016, 97, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, S.; Teng, J.L.L.; Chiu, T.-H.; Lau, S.K.P.; Woo, P.C.Y. Hepatitis E Virus Genotypes and Evolution: Emergence of Camel Hepatitis E Variants. Int. J. Mol. Sci. 2017, 18, 869. [Google Scholar] [CrossRef]
- Pavia, G.; Gioffrè, A.; Pirolo, M.; Visaggio, D.; Clausi, M.T.; Gherardi, M.; Samele, P.; Ciambrone, L.; Di Natale, R.; Spatari, G.; et al. Seroprevalence and phylogenetic characterization of hepatitis E virus in pig farms in Southern Italy. Prev. Veter. Med. 2021, 194, 105448. [Google Scholar] [CrossRef]
- Lhomme, S.; Marion, O.; Abravanel, F.; Izopet, J.; Kamar, N. Clinical Manifestations, Pathogenesis and Treatment of Hepatitis E Virus Infections. J. Clin. Med. 2020, 9, 331. [Google Scholar] [CrossRef]
- Kamar, N.; Selves, J.; Mansuy, J.-M.; Ouezzani, L.; Péron, J.-M.; Guitard, J.; Cointault, O.; Esposito, L.; Abravanel, F.; Danjoux, M.; et al. Hepatitis E Virus and Chronic Hepatitis in Organ-Transplant Recipients. N. Engl. J. Med. 2008, 358, 811–817. [Google Scholar] [CrossRef]
- Kanda, T.; Arima, S.; Sasaki-Tanaka, R.; Totsuka, M.; Honda, M.; Masuzaki, R.; Matsumoto, N.; Ogawa, M.; Takahashi, M.; Okamoto, H.; et al. Severe hepatitis E virus genotype 3b in a patient with alcohol-associated liver disease: A case report. Med. Int. 2024, 4, 22. [Google Scholar] [CrossRef]
- Ma, Z.; de Man, R.A.; Kamar, N.; Pan, Q. Chronic hepatitis E: Advancing research and patient care. J. Hepatol. 2022, 77, 1109–1123. [Google Scholar] [CrossRef]
- Chen, C.; Wang, M.-L.; Li, W.-X.; Qi, X.; Li, Q.; Chen, L. Hepatitis E virus infection increases the risk of obstetric complications and perinatal adverse outcomes in pregnant women with chronic hepatitis B virus infection. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 1904–1912. [Google Scholar] [CrossRef]
- Dalton, H.R.; Kamar, N.; Baylis, S.A.; Moradpour, D.; Wedemeyer, H.; Negro, F.; Dalton, H.R.; Kamar, N.; Baylis, S.A.; Moradpour, D.; et al. EASL Clinical Practice Guidelines on hepatitis E virus infection. J. Hepatol. 2018, 68, 1256–1271. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Zhang, J.; Luo, D.; Cheng, L.; Wang, Y. Chinese Consortium for the Study of Hepatitis E (CCSHE) Deregulation of immune response contributing to fulminant hepatitis in HEV infected pregnant women. J. Med. Virol. 2024, 96, e29639. [Google Scholar] [CrossRef]
- Shrestha, M.P.; Scott, R.M.; Joshi, D.M.; Mammen, M.P.J.; Thapa, G.B.; Thapa, N.; Myint, K.S.A.; Fourneau, M.; Kuschner, R.A.; Shrestha, S.K.; et al. Safety and Efficacy of a Recombinant Hepatitis E Vaccine. N. Engl. J. Med. 2007, 356, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.-C.; Zhang, J.; Zhang, X.-F.; Zhou, C.; Wang, Z.-Z.; Huang, S.-J.; Wang, H.; Yang, C.-L.; Jiang, H.-M.; Cai, J.-P.; et al. Efficacy and safety of a recombinant hepatitis E vaccine in healthy adults: A large-scale, randomised, double-blind placebo-controlled, phase 3 trial. Lancet 2010, 376, 895–902. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, X.-F.; Huang, S.-J.; Wu, T.; Hu, Y.-M.; Wang, Z.-Z.; Wang, H.; Jiang, H.-M.; Wang, Y.-J.; Yan, Q.; et al. Long-Term Efficacy of a Hepatitis E Vaccine. N. Engl. J. Med. 2015, 372, 914–922. [Google Scholar] [CrossRef] [PubMed]
- Abravanel, F.; Lhomme, S. Hecolin vaccine: Long-term efficacy against HEV for a three-dose regimen. Lancet 2024, 403, 782–783. [Google Scholar] [CrossRef]
- Huang, S.; Zhang, X.; Su, Y.; Zhuang, C.; Tang, Z.; Huang, X.; Chen, Q.; Zhu, K.; Hu, X.; Ying, D.; et al. Long-term efficacy of a recombinant hepatitis E vaccine in adults: 10-year results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2024, 403, 813–823. [Google Scholar] [CrossRef]
- Ueda, K.; Tsurimoto, T.; Matsubara, K. Three envelope proteins of hepatitis B virus: Large S, middle S, and major S proteins needed for the formation of Dane particles. J. Virol. 1991, 65, 3521–3529. [Google Scholar] [CrossRef]
- Mendenhall, M.A.; Hong, X.; Hu, J. Hepatitis B Virus Capsid: The Core in Productive Entry and Covalently Closed Circular DNA Formation. Viruses 2023, 15, 642. [Google Scholar] [CrossRef]
- Iwamoto, M.; Saso, W.; Sugiyama, R.; Ishii, K.; Ohki, M.; Nagamori, S.; Suzuki, R.; Aizaki, H.; Ryo, A.; Yun, J.-H.; et al. Epidermal growth factor receptor is a host-entry cofactor triggering hepatitis B virus internalization. Proc. Natl. Acad. Sci. USA 2019, 116, 8487–8492. [Google Scholar] [CrossRef] [PubMed]
- Hayes, C.N.; Zhang, Y.; Makokha, G.N.; Hasan, M.Z.; Omokoko, M.D.; Chayama, K. Early events in hepatitis B virus infection: From the cell surface to the nucleus. J. Gastroenterol. Hepatol. 2016, 31, 302–309. [Google Scholar] [CrossRef]
- Stephenson-Tsoris, S.; Liang, T.J. Hepatitis Delta Virus–Host Protein Interactions: From Entry to Egress. Viruses 2023, 15, 1530. [Google Scholar] [CrossRef] [PubMed]
- Gerold, G.; Moeller, R.; Pietschmann, T. Hepatitis C Virus Entry: Protein Interactions and Fusion Determinants Governing Productive Hepatocyte Invasion. Cold Spring Harb. Perspect. Med. 2020, 10, a036830. [Google Scholar] [CrossRef] [PubMed]
- Tscherne, D.M.; Jones, C.T.; Evans, M.J.; Lindenbach, B.D.; McKeating, J.A.; Rice, C.M. Time- and Temperature-Dependent Activation of Hepatitis C Virus for Low-pH-Triggered Entry. J. Virol. 2006, 80, 1734–1741. [Google Scholar] [CrossRef] [PubMed]
- Tzarum, N.; Wilson, I.A.; Law, M. The Neutralizing Face of Hepatitis C Virus E2 Envelope Glycoprotein. Front. Immunol. 2018, 9, 1315. [Google Scholar] [CrossRef]
- Rothwangl, K.B.; Manicassamy, B.; Uprichard, S.L.; Rong, L. Dissecting the role of putative CD81 binding regions of E2 in mediating HCV entry: Putative CD81 binding region 1 is not involved in CD81 binding. Virol. J. 2008, 5, 46. [Google Scholar] [CrossRef]
- Drummer, H.E.; Wilson, K.A.; Poumbourios, P. Identification of the Hepatitis C Virus E2 Glycoprotein Binding Site on the Large Extracellular Loop of CD81. J. Virol. 2002, 76, 11143–11147. [Google Scholar] [CrossRef]
- Drummer, H.E.; Boo, I.; Maerz, A.L.; Poumbourios, P. A Conserved Gly436-Trp-Leu-Ala-Gly-Leu-Phe-Tyr Motif in Hepatitis C Virus Glycoprotein E2 Is a Determinant of CD81 Binding and Viral Entry. J. Virol. 2006, 80, 7844–7853. [Google Scholar] [CrossRef]
- Owsianka, A.M.; Timms, J.M.; Tarr, A.W.; Brown, R.J.P.; Hickling, T.P.; Szwejk, A.; Bienkowska-Szewczyk, K.; Thomson, B.J.; Patel, A.H.; Ball, J.K. Identification of Conserved Residues in the E2 Envelope Glycoprotein of the Hepatitis C Virus That Are Critical for CD81 Binding. J. Virol. 2006, 80, 8695–8704. [Google Scholar] [CrossRef]
- Zhao, Z.; Zhong, L.; Elrod, E.; Struble, E.; Ma, L.; Yan, H.; Harman, C.; Deng, L.; Virata-Theimer, M.L.; Liu, P.; et al. A Neutralization Epitope in the Hepatitis C Virus E2 Glycoprotein Interacts with Host Entry Factor CD81. PLoS ONE 2014, 9, e84346. [Google Scholar] [CrossRef]
- Higginbottom, A.; Quinn, E.R.; Kuo, C.-C.; Flint, M.; Wilson, L.H.; Bianchi, E.; Nicosia, A.; Monk, P.N.; McKeating, J.A.; Levy, S. Identification of Amino Acid Residues in CD81 Critical for Interaction with Hepatitis C Virus Envelope Glycoprotein E2. J. Virol. 2000, 74, 3642–3649. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Hossain, R.A.; Yost, S.A.; Bu, W.; Wang, Y.; Dearborn, A.D.; Grakoui, A.; Cohen, J.I.; Marcotrigiano, J. Structural insights into hepatitis C virus receptor binding and entry. Nature 2021, 598, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Rivera-Serrano, E.E.; Yin, X.; Walker, C.M.; Feng, Z.; Lemon, S.M. Cell entry and release of quasi-enveloped human hepatitis viruses. Nat. Rev. Microbiol. 2023, 21, 573–589. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.D.; Hensley, L.; McKnight, K.L.; Hu, F.Y.; Madden, V.; Ping, L.F.; Jeong, S.-H.; Walker, C.; Lanford, R.E.; Lemon, S.M. A pathogenic picornavirus acquires an envelope by hijacking cellular membranes. Nature 2013, 496, 367–371. [Google Scholar] [CrossRef]
- Nagashima, S.; Jirintai, S.; Takahashi, M.; Kobayashi, T.; Tanggis; Nishizawa, T.; Kouki, T.; Yashiro, T.; Okamoto, H. Hepatitis E virus egress depends on the exosomal pathway, with secretory exosomes derived from multivesicular bodies. J. Gen. Virol. 2014, 95, 2166–2175. [Google Scholar] [CrossRef]
- Hessvik, N.P.; Llorente, A. Current knowledge on exosome biogenesis and release. Cell. Mol. Life Sci. 2018, 75, 193–208. [Google Scholar] [CrossRef]
- Takahashi, M.; Kobayashi, T.; Tanggis; Jirintai, S.; Mulyanto; Nagashima, S.; Nishizawa, T.; Kunita, S.; Okamoto, H. Production of monoclonal antibodies against the ORF3 protein of rat hepatitis E virus (HEV) and demonstration of the incorporation of the ORF3 protein into enveloped rat HEV particles. Arch. Virol. 2016, 161, 3391–3404. [Google Scholar] [CrossRef]
- Nagashima, S.; Takahashi, M.; Jirintai, S.; Tanaka, T.; Nishizawa, T.; Yasuda, J.; Okamoto, H. Tumour susceptibility gene 101 and the vacuolar protein sorting pathway are required for the release of hepatitis E virions. J. Gen. Virol. 2011, 92, 2838–2848. [Google Scholar] [CrossRef]
- Gouttenoire, J.; Pollán, A.; Abrami, L.; Oechslin, N.; Mauron, J.; Matter, M.; Oppliger, J.; Szkolnicka, D.; Dao Thi, V.L.; van der Goot, F.G.; et al. Palmitoylation mediates membrane association of hepatitis E virus ORF3 protein and is required for infectious particle secretion. PLOS Pathog. 2018, 14, e1007471. [Google Scholar] [CrossRef]
- Capelli, N.; Marion, O.; Dubois, M.; Allart, S.; Bertrand-Michel, J.; Lhomme, S.; Abravanel, F.; Izopet, J.; Chapuy-Regaud, S. Vectorial Release of Hepatitis E Virus in Polarized Human Hepatocytes. J. Virol. 2019, 93, e01207-18. [Google Scholar] [CrossRef] [PubMed]
- Sari, G.; Zhu, J.; Ambardekar, C.; Yin, X.; Boonstra, A.; Feng, Z.; Vanwolleghem, T. The Viral ORF3 Protein Is Required for Hepatitis E Virus Apical Release and Efficient Growth in Polarized Hepatocytes and Humanized Mice. J. Virol. 2021, 95, e0058521. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.C. Viral membrane fusion. Nat. Struct. Mol. Biol. 2008, 15, 690–698. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Ambardekar, C.; Lu, Y.; Feng, Z. Distinct Entry Mechanisms for Nonenveloped and Quasi-Enveloped Hepatitis E Viruses. J. Virol. 2016, 90, 4232–4242. [Google Scholar] [CrossRef]
- Kolter, T.; Sandhoff, K. Lysosomal degradation of membrane lipids. FEBS Lett. 2010, 584, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Serrano, E.E.; González-López, O.; Das, A.; Lemon, S.M. Cellular entry and uncoating of naked and quasi-enveloped human hepatoviruses. eLife 2019, 8, e43983. [Google Scholar] [CrossRef] [PubMed]
- Surjit, M.; Jameel, S.; Lal, S.K. Cytoplasmic Localization of the ORF2 Protein of Hepatitis E Virus Is Dependent on Its Ability To Undergo Retrotranslocation from the Endoplasmic Reticulum. J. Virol. 2007, 81, 3339–3345. [Google Scholar] [CrossRef]
- Kumar, C.S.; Dey, D.; Ghosh, S.; Banerjee, M. Breach: Host Membrane Penetration and Entry by Nonenveloped Viruses. Trends Microbiol. 2018, 26, 525–537. [Google Scholar] [CrossRef]
- He, S.; Miao, J.; Zheng, Z.; Wu, T.; Xie, M.; Tang, M.; Zhang, J.; Ng, M.-H.; Xia, N. Putative receptor-binding sites of hepatitis E virus. J. Gen. Virol. 2008, 89, 245–249. [Google Scholar] [CrossRef]
- Guu, T.S.Y.; Liu, Z.; Ye, Q.; Mata, D.A.; Li, K.; Yin, C.; Zhang, J.; Tao, Y.J. Structure of the hepatitis E virus-like particle suggests mechanisms for virus assembly and receptor binding. Proc. Natl. Acad. Sci. USA 2009, 106, 12992–12997. [Google Scholar] [CrossRef]
- Sayed, I.M.; Foquet, L.; Verhoye, L.; Abravanel, F.; Farhoudi, A.; Leroux-Roels, G.; Izopet, J.; Meuleman, P. Transmission of hepatitis E virus infection to human-liver chimeric FRG mice using patient plasma. Antivir. Res. 2017, 141, 150–154. [Google Scholar] [CrossRef]
- Li, Y.; Qu, C.; Yu, P.; Ou, X.; Pan, Q.; Wang, W. The Interplay between Host Innate Immunity and Hepatitis E Virus. Viruses 2019, 11, 541. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Akira, S. The roles of TLRs, RLRs and NLRs in pathogen recognition. Int. Immunol. 2009, 21, 317–337. [Google Scholar] [CrossRef] [PubMed]
- Schneider, W.M.; Chevillotte, M.D.; Rice, C.M. Interferon-Stimulated Genes: A Complex Web of Host Defenses. Annu. Rev. Immunol. 2014, 32, 513–545. [Google Scholar] [CrossRef] [PubMed]
- Horner, S.M.; Gale, M. Regulation of hepatic innate immunity by hepatitis C virus. Nat. Med. 2013, 19, 879–888. [Google Scholar] [CrossRef]
- Xu, C.; Chen, J.; Chen, X. Host Innate Immunity Against Hepatitis Viruses and Viral Immune Evasion. Front. Microbiol. 2021, 12, 740464. [Google Scholar] [CrossRef] [PubMed]
- Zaki, M.Y.W.; Fathi, A.M.; Samir, S.; Eldafashi, N.; William, K.Y.; Nazmy, M.H.; Fathy, M.; Gill, U.S.; Shetty, S. Innate and Adaptive Immunopathogeneses in Viral Hepatitis; Crucial Determinants of Hepatocellular Carcinoma. Cancers 2022, 14, 1255. [Google Scholar] [CrossRef]
- Chiale, C.; Marchese, A.M.; Robek, M.D. Innate immunity and HBV persistence. Curr. Opin. Virol. 2021, 49, 13–20. [Google Scholar] [CrossRef]
- Winer, B.Y.; Gaska, J.M.; Lipkowitz, G.; Bram, Y.; Parekh, A.; Parsons, L.; Leach, R.; Jindal, R.; Cho, C.H.; Shrirao, A.; et al. Analysis of Host Responses to Hepatitis B and Delta Viral Infections in a Micro-scalable Hepatic Co-culture System. Hepatology 2020, 71, 14–30. [Google Scholar] [CrossRef]
- Choi, H.S.; Tonthat, A.; Janssen, H.L.; Terrault, N.A. Aiming for Functional Cure with Established and Novel Therapies for Chronic Hepatitis B. Hepatol. Commun. 2022, 6, 935–949. [Google Scholar] [CrossRef]
- Fung, S.; Choi, H.S.J.; Gehring, A.; Janssen, H.L.A. Getting to HBV cure: The promising paths forward. Hepatology 2022, 76, 233–250. [Google Scholar] [CrossRef]
- Rivino, L.; Le Bert, N.; Gill, U.S.; Kunasegaran, K.; Cheng, Y.; Tan, D.Z.; Becht, E.; Hansi, N.K.; Foster, G.R.; Su, T.-H.; et al. Hepatitis B virus–specific T cells associate with viral control upon nucleos(t)ide-analogue therapy discontinuation. J. Clin. Investig. 2018, 128, 668–681. [Google Scholar] [CrossRef]
- Aliabadi, E.; Urbanek-Quaing, M.; Maasoumy, B.; Bremer, B.; Grasshoff, M.; Li, Y.; Niehaus, C.E.; Wedemeyer, H.; Kraft, A.R.M.; Cornberg, M. Impact of HBsAg and HBcrAg levels on phenotype and function of HBV-specific T cells in patients with chronic hepatitis B virus infection. Gut 2022, 71, 2300–2312. [Google Scholar] [CrossRef]
- Le Bert, N.; Gill, U.S.; Hong, M.; Kunasegaran, K.; Tan, D.Z.M.; Ahmad, R.; Cheng, Y.; Dutertre, C.-A.; Heinecke, A.; Rivino, L.; et al. Effects of Hepatitis B Surface Antigen on Virus-Specific and Global T Cells in Patients with Chronic Hepatitis B Virus infection. Gastroenterology 2020, 159, 652–664. [Google Scholar] [CrossRef]
- Zimmer, C.L.; Rinker, F.; Höner Zu Siederdissen, C.; Manns, M.P.; Wedemeyer, H.; Cornberg, M.; Björkström, N.K. Increased NK Cell Function After Cessation of Long-Term Nucleos(t)ide Analogue Treatment in Chronic Hepatitis B Is Associated with Liver Damage and HBsAg Loss. J. Infect. Dis. 2018, 217, 1656–1666. [Google Scholar] [CrossRef] [PubMed]
- Narmada, B.C.; Khakpoor, A.; Shirgaonkar, N.; Narayanan, S.; Aw, P.P.K.; Singh, M.; Ong, K.H.; Owino, C.O.; Ng, J.W.T.; Yew, H.C.; et al. Single-cell landscape of functionally cured chronic hepatitis B patients reveals activation of innate and altered CD4-CTL-driven adaptive immunity. J. Hepatol. 2024, 81, 42–61. [Google Scholar] [CrossRef] [PubMed]
- Engle, R.E.; De Battista, D.; Danoff, E.J.; Nguyen, H.; Chen, Z.; Lusso, P.; Purcell, R.H.; Farci, P. Distinct Cytokine Profiles Correlate with Disease Severity and Outcome in Longitudinal Studies of Acute Hepatitis B Virus and Hepatitis D Virus Infection in Chimpanzees. mBio 2020, 11, e02580-20. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yin, S.; Chen, Y.; Zhang, Q.; Huang, R.; Jia, B.; Jie, W.; Yao, K.; Wang, J.; Tong, X.; et al. Hepatitis B virus-induced hyperactivation of B cells in chronic hepatitis B patients via TLR4. J. Cell. Mol. Med. 2020, 24, 6096–6106. [Google Scholar] [CrossRef]
- Joshi, S.S.; Sadler, M.; Patel, N.H.; Osiowy, C.; Fonseca, K.; Coffin, C.S. Systemic cytokine and viral antigen-specific responses in hepatitis D virus RNA positive versus HDV RNA negative patients. Front. Med. 2023, 10, 1125139. [Google Scholar] [CrossRef]
- Giersch, K.; Allweiss, L.; Volz, T.; Helbig, M.; Bierwolf, J.; Lohse, A.W.; Pollok, J.M.; Petersen, J.; Dandri, M.; Lütgehetmann, M. Hepatitis Delta co-infection in humanized mice leads to pronounced induction of innate immune responses in comparison to HBV mono-infection. J. Hepatol. 2015, 63, 346–353. [Google Scholar] [CrossRef]
- Schirdewahn, T.; Grabowski, J.; Owusu Sekyere, S.; Bremer, B.; Wranke, A.; Lunemann, S.; Schlaphoff, V.; Kirschner, J.; Hardtke, S.; Manns, M.P.; et al. The Third Signal Cytokine Interleukin 12 Rather Than Immune Checkpoint Inhibitors Contributes to the Functional Restoration of Hepatitis D Virus–Specific T Cells. J. Infect. Dis. 2017, 215, 139–149. [Google Scholar] [CrossRef]
- Hyodo, N.; Nakamura, I.; Imawari, M. Hepatitis B core antigen stimulates interleukin-10 secretion by both T cells and monocytes from peripheral blood of patients with chronic hepatitis B virus infection. Clin. Exp. Immunol. 2004, 135, 462–466. [Google Scholar] [CrossRef] [PubMed]
- Townsend, E.C.; Zhang, G.Y.; Ali, R.; Firke, M.; Moon, M.S.; Han, M.A.T.; Fram, B.; Glenn, J.S.; Kleiner, D.E.; Koh, C.; et al. The balance of type 1 and type 2 immune responses in the contexts of hepatitis B infection and hepatitis D infection. J. Gastroenterol. Hepatol. 2019, 34, 764–775. [Google Scholar] [CrossRef] [PubMed]
- Suslov, A.; Boldanova, T.; Wang, X.; Wieland, S.; Heim, M.H. Hepatitis B Virus Does Not Interfere with Innate Immune Responses in the Human Liver. Gastroenterology 2018, 154, 1778–1790. [Google Scholar] [CrossRef]
- Jung, S.; Altstetter, S.M.; Protzer, U. Innate immune recognition and modulation in hepatitis D virus infection. World J. Gastroenterol. 2020, 26, 2781–2791. [Google Scholar] [CrossRef] [PubMed]
- Oberhardt, V.; Hofmann, M.; Thimme, R.; Neumann-Haefelin, C. Adaptive Immune Responses, Immune Escape and Immune-Mediated Pathogenesis during HDV Infection. Viruses 2022, 14, 198. [Google Scholar] [CrossRef]
- Chida, T.; Ishida, Y.; Morioka, S.; Sugahara, G.; Han, C.; Lam, B.; Yamasaki, C.; Sugahara, R.; Li, M.; Tanaka, Y.; et al. Persistent hepatic IFN system activation in HBV-HDV infection determines viral replication dynamics and therapeutic response. JCI insight 2023, 8, e162404. [Google Scholar] [CrossRef]
- Kefalakes, H.; Koh, C.; Sidney, J.; Amanakis, G.; Sette, A.; Heller, T.; Rehermann, B. Hepatitis D Virus-Specific CD8+ T Cells Have a Memory-Like Phenotype Associated with Viral Immune Escape in Patients with Chronic Hepatitis D Virus Infection. Gastroenterology 2019, 156, 1805–1819.e9. [Google Scholar] [CrossRef] [PubMed]
- Karimzadeh, H.; Kiraithe, M.M.; Oberhardt, V.; Alizei, E.S.; Bockmann, J.; Schulze Zur Wiesch, J.; Budeus, B.; Hoffmann, D.; Wedemeyer, H.; Cornberg, M.; et al. Mutations in Hepatitis D Virus Allow It to Escape Detection by CD8+ T Cells and Evolve at the Population Level. Gastroenterology 2019, 156, 1820–1833. [Google Scholar] [CrossRef]
- Takahashi, K.; Asabe, S.; Wieland, S.; Garaigorta, U.; Gastaminza, P.; Isogawa, M.; Chisari, F.V. Plasmacytoid dendritic cells sense hepatitis C virus–infected cells, produce interferon, and inhibit infection. Proc. Natl. Acad. Sci. USA 2010, 107, 7431–7436. [Google Scholar] [CrossRef]
- Thimme, R.; Oldach, D.; Chang, K.-M.; Steiger, C.; Ray, S.C.; Chisari, F.V. Determinants of Viral Clearance and Persistence during Acute Hepatitis C Virus Infection. J. Exp. Med. 2001, 194, 1395–1406. [Google Scholar] [CrossRef]
- Pestka, J.M.; Zeisel, M.B.; Bläser, E.; Schürmann, P.; Bartosch, B.; Cosset, F.-L.; Patel, A.H.; Meisel, H.; Baumert, J.; Viazov, S.; et al. Rapid induction of virus-neutralizing antibodies and viral clearance in a single-source outbreak of hepatitis C. Proc. Natl. Acad. Sci. USA 2007, 104, 6025–6030. [Google Scholar] [CrossRef] [PubMed]
- Shin, E.-C.; Sung, P.S.; Park, S.-H. Immune responses and immunopathology in acute and chronic viral hepatitis. Nat. Rev. Immunol. 2016, 16, 509–523. [Google Scholar] [CrossRef]
- Kemming, J.; Thimme, R.; Neumann-Haefelin, C. Adaptive Immune Response against Hepatitis C Virus. Int. J. Mol. Sci. 2020, 21, 5644. [Google Scholar] [CrossRef] [PubMed]
- Marascio, N.; Rotundo, S.; Quirino, A.; Matera, G.; Liberto, M.C.; Costa, C.; Russo, A.; Trecarichi, E.M.; Torti, C. Similarities, differences, and possible interactions between hepatitis E and hepatitis C viruses: Relevance for research and clinical practice. World J. Gastroenterol. 2022, 28, 1226–1238. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, W.; Zou, Z.; Hu, Z.; Fan, Q.; Xiong, J. Hepatitis C Virus Entry into Macrophages/Monocytes Mainly Depends on the Phagocytosis of Macrophages. Dig. Dis. Sci. 2019, 64, 1226–1237. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, R.; Devhare, P.B.; Steele, R.; Ray, R.; Ray, R.B. Hepatitis C virus–induced CCL5 secretion from macrophages activates hepatic stellate cells. Hepatology 2017, 66, 746–757. [Google Scholar] [CrossRef] [PubMed]
- Semmo, N.; Day, C.L.; Ward, S.M.; Lucas, M.; Harcourt, G.; Loughry, A.; Klenerman, P. Preferential loss of IL-2-secreting CD4+ T helper cells in chronic HCV infection. Hepatology 2005, 41, 1019–1028. [Google Scholar] [CrossRef]
- Rushbrook, S.M.; Ward, S.M.; Unitt, E.; Vowler, S.L.; Lucas, M.; Klenerman, P.; Alexander, G.J.M. Regulatory T Cells Suppress In Vitro Proliferation of Virus-Specific CD8+T Cells during Persistent Hepatitis C Virus Infection. J. Virol. 2005, 79, 7852–7859. [Google Scholar] [CrossRef]
- Mondelli, M.U.; Ottolini, S.; Oliviero, B.; Mantovani, S.; Cerino, A.; Mele, D.; Varchetta, S. Hepatitis C Virus and the Host: A Mutual Endurance Leaving Indelible Scars in the Host’s Immunity. Int. J. Mol. Sci. 2023, 25, 268. [Google Scholar] [CrossRef]
- Li, Z.; Chen, L.; Liu, Q. Activation of CXCL-8 Transcription by Hepatitis E Virus ORF-1 via AP-1. Mediat. Inflamm. 2015, 2015, 495370. [Google Scholar] [CrossRef]
- Munir, M.; Zohari, S.; Belák, S.; Berg, M. Double-Stranded RNA-Induced Activation of Activating Protein-1 Promoter Is Differentially Regulated by the Non-structural Protein 1 of Avian Influenza A Viruses. Viral Immunol. 2012, 25, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Myoung, J. Host Innate Immunity against Hepatitis E Virus and Viral Evasion Mechanisms. J. Microbiol. Biotechnol. 2017, 27, 1727–1735. [Google Scholar] [CrossRef] [PubMed]
- Saravanabalaji, S.; Tripathy, A.S.; Dhoot, R.R.; Chadha, M.S.; Kakrani, A.L.; Arankalle, V.A. Viral Load, Antibody Titers and Recombinant Open Reading Frame 2 Protein-Induced Th1/Th2 Cytokines and Cellular Immune Responses in Self-Limiting and Fulminant Hepatitis E. Intervirology 2009, 52, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.M. Adaptive Immune Responses in Hepatitis A Virus and Hepatitis E Virus Infections. Cold Spring Harb. Perspect. Med. 2019, 9, a033472. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.; Halliday, J.S.; Swadling, L.; Madden, R.G.; Bendall, R.; Hunter, J.G.; Maggs, J.; Simmonds, P.; Smith, D.B.; Vine, L.; et al. Characterization of the Specificity, Functionality, and Durability of Host T-Cell Responses Against the Full-Length Hepatitis E Virus. Hepatology 2016, 64, 1934–1950. [Google Scholar] [CrossRef]
- Strumillo, S.T.; Kartavykh, D.; de Carvalho, F.F.; Cruz, N.C.; de Souza Teodoro, A.C.; Sobhie Diaz, R.; Curcio, M.F. Host–virus interaction and viral evasion. Cell Biol. Int. 2021, 45, 1124–1147. [Google Scholar] [CrossRef]
- Jo, E.-K. Interplay between host and pathogen: Immune defense and beyond. Exp. Mol. Med. 2019, 51, 1–3. [Google Scholar] [CrossRef]
- Soleiman-Meigooni, S.; Yarahmadi, A.; Kheirkhah, A.-H.; Afkhami, H. Recent advances in different interactions between toll-like receptors and hepatitis B infection: A review. Front. Immunol. 2024, 15, 1363996. [Google Scholar] [CrossRef]
- Kim, C.Y.; Tilles, J.G. Purification and Biophysical Characterization of Hepatitis B Antigen. J. Clin. Investig. 1973, 52, 1176–1186. [Google Scholar] [CrossRef]
- Maini, M.K.; Burton, A.R. Restoring, releasing or replacing adaptive immunity in chronic hepatitis B. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 662–675. [Google Scholar] [CrossRef]
- Burton, A.R.; Pallett, L.J.; McCoy, L.E.; Suveizdyte, K.; Amin, O.E.; Swadling, L.; Alberts, E.; Davidson, B.R.; Kennedy, P.T.; Gill, U.S.; et al. Circulating and intrahepatic antiviral B cells are defective in hepatitis B. J. Clin. Investig. 2018, 128, 4588–4603. [Google Scholar] [CrossRef] [PubMed]
- Salimzadeh, L.; Le Bert, N.; Dutertre, C.-A.; Gill, U.S.; Newell, E.W.; Frey, C.; Hung, M.; Novikov, N.; Fletcher, S.; Kennedy, P.T.; et al. PD-1 blockade partially recovers dysfunctional virus–specific B cells in chronic hepatitis B infection. J. Clin. Investig. 2018, 128, 4573–4587. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.; Chen, Y.; Liu, Y.; Wang, S.; Li, Y.; Wang, G.; Xia, J.; Zhao, X.-A.; Huang, R.; Lu, S.; et al. Use of ELISpot assay to study HBs-specific B cell responses in vaccinated and HBV infected humans. Emerg. Microbes Infect. 2018, 7, 16. [Google Scholar] [CrossRef]
- Xu, X.; Shang, Q.; Chen, X.; Nie, W.; Zou, Z.; Huang, A.; Meng, M.; Jin, L.; Xu, R.; Zhang, J.-Y.; et al. Reversal of B-cell hyperactivation and functional impairment is associated with HBsAg seroconversion in chronic hepatitis B patients. Cell. Mol. Immunol. 2015, 12, 309–316. [Google Scholar] [CrossRef]
- Le Bert, N.; Salimzadeh, L.; Gill, U.S.; Dutertre, C.-A.; Facchetti, F.; Tan, A.; Hung, M.; Novikov, N.; Lampertico, P.; Fletcher, S.P.; et al. Comparative characterization of B cells specific for HBV nucleocapsid and envelope proteins in patients with chronic hepatitis B. J. Hepatol. 2020, 72, 34–44. [Google Scholar] [CrossRef]
- Vanwolleghem, T.; Groothuismink, Z.M.; Kreefft, K.; Hung, M.; Novikov, N.; Boonstra, A. Hepatitis B core-specific memory B cell responses associate with clinical parameters in patients with chronic HBV. J. Hepatol. 2020, 73, 52–61. [Google Scholar] [CrossRef]
- Milich, D.R.; McLachlan, A. The Nucleocapsid of Hepatitis B Virus Is Both a T-Cell-Independent and a T-Cell-Dependent Antigen. Science 1986, 234, 1398–1401. [Google Scholar] [CrossRef]
- Fumagalli, V.; Di Lucia, P.; Venzin, V.; Bono, E.B.; Jordan, R.; Frey, C.R.; Delaney, W.; Chisari, F.V.; Guidotti, L.G.; Iannacone, M. Serum HBsAg clearance has minimal impact on CD8+ T cell responses in mouse models of HBV infection. J. Exp. Med. 2020, 217, e20200298. [Google Scholar] [CrossRef] [PubMed]
- Padarath, K.; Deroubaix, A.; Kramvis, A. The Complex Role of HBeAg and Its Precursors in the Pathway to Hepatocellular Carcinoma. Viruses 2023, 15, 857. [Google Scholar] [CrossRef]
- Chen, M.T.; Billaud, J.-N.; Sällberg, M.; Guidotti, L.G.; Chisari, F.V.; Jones, J.; Hughes, J.; Milich, D.R. A function of the hepatitis B virus precore protein is to regulate the immune response to the core antigen. Proc. Natl. Acad. Sci. USA 2004, 101, 14913–14918. [Google Scholar] [CrossRef]
- Chen, M.; Sällberg, M.; Hughes, J.; Jones, J.; Guidotti, L.G.; Chisari, F.V.; Billaud, J.-N.; Milich, D.R. Immune Tolerance Split between Hepatitis B Virus Precore and Core Proteins. J. Virol. 2005, 79, 3016–3027. [Google Scholar] [CrossRef]
- Tian, Y.; Kuo, C.-F.; Akbari, O.; Ou, J.-H.J. Maternal-Derived Hepatitis B Virus e Antigen Alters Macrophage Function in Offspring to Drive Viral Persistence after Vertical Transmission. Immunity 2016, 44, 1204–1214. [Google Scholar] [CrossRef]
- Brunetto, M.R.; Giarin, M.M.; Oliveri, F.; Chiaberge, E.; Baldi, M.; Alfarano, A.; Serra, A.; Saracco, G.; Verme, G.; Will, H. Wild-type and e antigen-minus hepatitis B viruses and course of chronic hepatitis. Proc. Natl. Acad. Sci. USA 1991, 88, 4186–4190. [Google Scholar] [CrossRef]
- Woo, Y.; Ma, M.; Okawa, M.; Saito, T. Hepatocyte Intrinsic Innate Antiviral Immunity against Hepatitis Delta Virus Infection: The Voices of Bona Fide Human Hepatocytes. Viruses 2024, 16, 740. [Google Scholar] [CrossRef]
- Zhang, Z.; Filzmayer, C.; Ni, Y.; Sültmann, H.; Mutz, P.; Hiet, M.-S.; Vondran, F.W.R.; Bartenschlager, R.; Urban, S. Hepatitis D virus replication is sensed by MDA5 and induces IFN-β/λ responses in hepatocytes. J. Hepatol. 2018, 69, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Pugnale, P.; Pazienza, V.; Guilloux, K.; Negro, F. Hepatitis delta virus inhibits alpha interferon signaling. Hepatology 2009, 49, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Oliviero, B.; Cerino, A.; Varchetta, S.; Paudice, E.; Pai, S.; Ludovisi, S.; Zaramella, M.; Michelone, G.; Pugnale, P.; Negro, F.; et al. Enhanced B-cell differentiation and reduced proliferative capacity in chronic hepatitis C and chronic hepatitis B virus infections. J. Hepatol. 2011, 55, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Cao, X.; Ding, Q.; Zhao, Y.; He, Z.; Zhong, J. Hepatitis C virus NS4B induces the degradation of TRIF to inhibit TLR3-mediated interferon signaling pathway. PLoS Pathog. 2018, 14, e1007075. [Google Scholar] [CrossRef]
- Refolo, G.; Ciccosanti, F.; Di Rienzo, M.; Basulto Perdomo, A.; Romani, M.; Alonzi, T.; Tripodi, M.; Ippolito, G.; Piacentini, M.; Fimia, G.M. Negative Regulation of Mitochondrial Antiviral Signaling Protein–Mediated Antiviral Signaling by the Mitochondrial Protein LRPPRC During Hepatitis C Virus Infection. Hepatology 2019, 69, 34–50. [Google Scholar] [CrossRef]
- Machida, K.; Cheng, K.T.H.; Sung, V.M.-H.; Levine, A.M.; Foung, S.; Lai, M.M.C. Hepatitis C Virus Induces Toll-Like Receptor 4 Expression, Leading to Enhanced Production of Beta Interferon and Interleukin-6. J. Virol. 2006, 80, 866–874. [Google Scholar] [CrossRef]
- Nan, Y.; Yu, Y.; Ma, Z.; Khattar, S.K.; Fredericksen, B.; Zhang, Y.-J. Hepatitis E Virus Inhibits Type I Interferon Induction by ORF1 Products. J. Virol. 2014, 88, 11924–11932. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Myoung, J. Hepatitis E Virus Papain-Like Cysteine Protease Inhibits Type I Interferon Induction by Down-Regulating Melanoma Differentiation-Associated Gene 5. J. Microbiol. Biotechnol. 2018, 28, 1908–1915. [Google Scholar] [CrossRef] [PubMed]
- Myoung, J.; Min, K. Dose-Dependent Inhibition of Melanoma Differentiation-Associated Gene 5-Mediated Activation of Type I Interferon Responses by Methyltransferase of Hepatitis E Virus. J. Microbiol. Biotechnol. 2019, 29, 1137–1143. [Google Scholar] [CrossRef]
- Myoung, J.; Lee, J.Y.; Min, K.S. Methyltransferase of a cell culture-adapted hepatitis E inhibits the MDA5 receptor signaling pathway. J. Microbiol. 2019, 57, 1126–1131. [Google Scholar] [CrossRef] [PubMed]
- Ojha, N.K.; Lole, K.S. Hepatitis E virus ORF1 encoded macro domain protein interacts with light chain subunit of human ferritin and inhibits its secretion. Mol. Cell. Biochem. 2016, 417, 75–85. [Google Scholar] [CrossRef]
- Lin, S.; Yang, Y.; Nan, Y.; Ma, Z.; Yang, L.; Zhang, Y.-J. The Capsid Protein of Hepatitis E Virus Inhibits Interferon Induction via Its N-Terminal Arginine-Rich Motif. Viruses 2019, 11, 1050. [Google Scholar] [CrossRef]
- Hingane, S.; Joshi, N.; Surjit, M.; Ranjith-Kumar, C.T. Hepatitis E Virus ORF2 Inhibits RIG-I Mediated Interferon Response. Front. Microbiol. 2020, 11, 656. [Google Scholar] [CrossRef]
- John, L.; Thomas, S.; Herchenröder, O.; Pützer, B.M.; Schaefer, S. Hepatitis E Virus ORF2 Protein Activates the Pro-Apoptotic Gene CHOP and Anti-Apoptotic Heat Shock Proteins. PLoS ONE 2011, 6, e25378. [Google Scholar] [CrossRef] [PubMed]
- Lei, Q.; Li, L.; Zhang, S.; Li, T.; Zhang, X.; Ding, X.; Qin, B. HEV ORF3 downregulates TLR7 to inhibit the generation of type I interferon via impairment of multiple signaling pathways. Sci. Rep. 2018, 8, 8585. [Google Scholar] [CrossRef]
- Nan, Y.; Ma, Z.; Wang, R.; Yu, Y.; Kannan, H.; Fredericksen, B.; Zhang, Y.-J. Enhancement of Interferon Induction by ORF3 Product of Hepatitis E Virus. J. Virol. 2014, 88, 8696–8705. [Google Scholar] [CrossRef]
- Dong, C.; Zafrullah, M.; Mixson-Hayden, T.; Dai, X.; Liang, J.; Meng, J.; Kamili, S. Suppression of interferon-α signaling by hepatitis E virus. Hepatology 2012, 55, 1324–1332. [Google Scholar] [CrossRef]
- Wang, M.; Huang, Y.; He, M.; Peng, W.-J.; Tian, D.-Y. Effects of hepatitis E virus infection on interferon production via ISG15. World J. Gastroenterol. 2018, 24, 2173–2180. [Google Scholar] [CrossRef]
- Corazza, N.; Badmann, A.; Lauer, C. Immune cell-mediated liver injury. Semin. Immunopathol. 2009, 31, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Oh, I.S.; Park, S.-H. Immune-mediated Liver Injury in Hepatitis B Virus Infection. Immune Netw. 2015, 15, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Irshad, M.; Gupta, P.; Irshad, K. Immunopathogenesis of Liver Injury During Hepatitis C Virus Infection. Viral Immunol. 2019, 32, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Kisseleva, T.; Brenner, D.A. Hepatic stellate cells and the reversal of fibrosis. J. Gastroenterol. Hepatol. 2006, 21 (Suppl. S3), S84–S87. [Google Scholar] [CrossRef] [PubMed]
- Protzer, U.; Maini, M.K.; Knolle, P.A. Living in the liver: Hepatic infections. Nat. Rev. Immunol. 2012, 12, 201–213. [Google Scholar] [CrossRef]
- Kuipery, A.; Gehring, A.J.; Isogawa, M. Mechanisms of HBV immune evasion. Antivir. Res. 2020, 179, 104816. [Google Scholar] [CrossRef]
- Zhao, H.-J.; Hu, Y.-F.; Han, Q.-J.; Zhang, J. Innate and adaptive immune escape mechanisms of hepatitis B virus. World J. Gastroenterol. 2022, 28, 881–896. [Google Scholar] [CrossRef]
- Geller, R.; Estada, Ú.; Peris, J.B.; Andreu, I.; Bou, J.-V.; Garijo, R.; Cuevas, J.M.; Sabariegos, R.; Mas, A.; Sanjuán, R. Highly heterogeneous mutation rates in the hepatitis C virus genome. Nat. Microbiol. 2016, 1, 16045. [Google Scholar] [CrossRef]
- Pan, C.; Gish, R.; Jacobson, I.M.; Hu, K.-Q.; Wedemeyer, H.; Martin, P. Diagnosis and Management of Hepatitis Delta Virus Infection. Dig. Dis. Sci. 2023, 68, 3237–3248. [Google Scholar] [CrossRef]
- Thakur, V.; Ratho, R.K.; Kumar, S.; Saxena, S.K.; Bora, I.; Thakur, P. Viral Hepatitis E and Chronicity: A Growing Public Health Concern. Front. Microbiol. 2020, 11, 577339. [Google Scholar] [CrossRef]
- Tu, T.; Bühler, S.; Bartenschlager, R. Chronic viral hepatitis and its association with liver cancer. Biol. Chem. 2017, 398, 817–837. [Google Scholar] [CrossRef]
- Zuñiga-Aguilar, E.; Ramírez-Fernández, O. Fibrosis and hepatic regeneration mechanism. Transl. Gastroenterol. Hepatol. 2022, 7, 9. [Google Scholar] [CrossRef]
- Li, H. Angiogenesis in the progression from liver fibrosis to cirrhosis and hepatocelluar carcinoma. Expert Rev. Gastroenterol. Hepatol. 2020, 15, 217–233. [Google Scholar] [CrossRef]
- Anzola, M. Hepatocellular carcinoma: Role of hepatitis B and hepatitis C viruses proteins in hepatocarcinogenesis. J. Viral Hepat. 2004, 11, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Wasley, A.; Fiore, A.; Bell, B.P. Hepatitis A in the Era of Vaccination. Epidemiol. Rev. 2006, 28, 101–111. [Google Scholar] [CrossRef]
- Gabrielli, F.; Alberti, F.; Russo, C.; Cursaro, C.; Seferi, H.; Margotti, M.; Andreone, P. Treatment Options for Hepatitis A and E: A Non-Systematic Review. Viruses 2023, 15, 1080. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, N.; Mousa, O.Y. Hepatitis B. In StatPearls; Updated 2023 Jul 9; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK555945/ (accessed on 1 August 2024).
- Schillie, S. Prevention of hepatitis B virus infection in the United States: Recommendations of the Advisory Committee on Im-munization Practices. MMWR Recomm. Rep. 2017, 67, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Nayagam, S.; Thursz, M.; Sicuri, E.; Conteh, L.; Wiktor, S.; Low-Beer, D.; Hallett, T.B. Requirements for global elimination of hepatitis B: A modelling study. Lancet Infect. Dis. 2016, 16, 1399–1408. [Google Scholar] [CrossRef]
- Chiang, C.-J.; Yang, Y.-W.; You, S.-L.; Lai, M.-S.; Chen, C.-J. Thirty-Year Outcomes of the National Hepatitis B Immunization Program in Taiwan. JAMA 2013, 310, 974–976. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Gong, Y.; Brok, J.; Boxall, E.H.; Gluud, C. Hepatitis B immunisation for newborn infants of hepatitis B surface antigen-positive mothers. Cochrane Database Syst. Rev. 2006, 2, CD004790. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman, J.N. Protective efficacy, immunotherapeutic potential, and safety of hepatitis B vaccines. J. Med. Virol. 2005, 78, 169–177. [Google Scholar] [CrossRef]
- World Health Organization. Hepatitis B Vaccines: WHO Position Paper, July 2017–Recommendations. Vaccine 2017, 36, 2170–2171. Available online: https://www.who.int/publications/i/item/WER9227 (accessed on 22 August 2024).
- Hang, T.-V.P.; Wedd, J.P. The optimal timing and management of hepatitis B and C in patients with hepatocellular carcinoma. Chin. Clin. Oncol. 2021, 10, 4. [Google Scholar] [CrossRef] [PubMed]
- Schlaak, J.F. Current Therapy of Chronic Viral Hepatitis B, C and D. J. Pers. Med. 2023, 13, 964. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, H.; Mehmood, B.F.; Sohal, A.; Roytman, M. Hepatitis E infection: A review. World J. Virol. 2023, 12, 262–271. [Google Scholar] [CrossRef]
- Stone, D.; Long, K.R.; Loprieno, M.A.; Feelixge, H.S.D.S.; Kenkel, E.J.; Liley, R.M.; Rapp, S.; Roychoudhury, P.; Nguyen, T.; Stensland, L.; et al. CRISPR-Cas9 gene editing of hepatitis B virus in chronically infected humanized mice. Mol. Ther. Methods Clin. Dev. 2020, 20, 258–275. [Google Scholar] [CrossRef]
- Martin, A.; Lemon, S.M. Hepatitis A Virus: From Discovery to Vaccines. Hepatology 2006, 43, S164–S172. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, J.T.; Lemon, S.M. Neutralization escape mutants define a dominant immunogenic neutralization site on hepatitis A virus. J. Virol. 1987, 61, 491–498. [Google Scholar] [CrossRef]
- Innis, B.L.; Snitbhan, R.; Kunasol, P.; Laorakpongse, T.; Poopatanakool, W.; Kozik, C.A.; Suntayakorn, S.; Suknuntapong, T.; Safary, A.; Tang, D.B.; et al. Protection Against Hepatitis A by an Inactivated Vaccine. JAMA 1994, 271, 1328–1334. [Google Scholar] [CrossRef] [PubMed]
- Zoulim, F.; Locarnini, S. Hepatitis B Virus Resistance to Nucleos(t)ide Analogues. Gastroenterology 2009, 137, 1593–1608.e2. [Google Scholar] [CrossRef]
- Tenney, D.J.; Rose, R.E.; Baldick, C.J.; Pokornowski, K.A.; Eggers, B.J.; Fang, J.; Wichroski, M.J.; Xu, D.; Yang, J.; Wilber, R.B.; et al. Long-term monitoring shows hepatitis B virus resistance to entecavir in nucleoside-naïve patients is rare through 5 years of therapy. Hepatology 2009, 49, 1503–1514. [Google Scholar] [CrossRef]
- Dienstag, J.L. Hepatitis B virus infection. N. Engl. J. Med. 2008, 359, 1486–1500. [Google Scholar] [CrossRef]
- Tseng, T.-C.; Kao, J.-H. Elimination of Hepatitis B: Is It a Mission Possible? BMC Med. 2017, 15, 53. [Google Scholar] [CrossRef]
- Manns, M.P.; McHutchison, J.G.; Gordon, S.C.; Rustgi, V.K.; Shiffman, M.; Reindollar, R.; Goodman, Z.D.; Koury, K.; Ling, M.-H.; Albrecht, J.K. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: A randomised trial. Lancet 2001, 358, 958–965. [Google Scholar] [CrossRef]
- Sarrazin, C.; Zeuzem, S. Resistance to Direct Antiviral Agents in Patients with Hepatitis C Virus Infection. Gastroenterology 2010, 138, 447–462. [Google Scholar] [CrossRef] [PubMed]
- Sofia, M.J.; Bao, D.; Chang, W.; Du, J.; Nagarathnam, D.; Rachakonda, S.; Reddy, P.G.; Ross, B.S.; Wang, P.; Zhang, H.R.; et al. Discovery of a β-d-2′-deoxy-2′-α-fluoro-2′-β-C-methyluridine nucleotide prodrug (PSI-7977) for the treatment of hepatitis C virus. J. Med. Chemistry. 2010, 53, 7202–7218. [Google Scholar] [CrossRef]
- Lawitz, E.; Mangia, A.; Wyles, D.; Rodriguez-Torres, M.; Hassanein, T.; Gordon, S.C.; Schultz, M.; Davis, M.N.; Kayali, Z.; Reddy, K.R.; et al. Sofosbuvir for Previously Untreated Chronic Hepatitis C Infection. N. Engl. J. Med. 2013, 368, 1878–1887. [Google Scholar] [CrossRef]
- Gao, M.; Nettles, R.E.; Belema, M.; Snyder, L.B.; Nguyen, V.N.; Fridell, R.A.; Serrano-Wu, M.H.; Langley, D.R.; Sun, J.H.; O’Boyle, I.I.D.R.; et al. Chemical genetics strategy identifies an HCV NS5A inhibitor with a potent clinical effect. Nature 2010, 465, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Asselah, T. Daclatasvir plus sofosbuvir for HCV infection: An oral combination therapy with high antiviral efficacy. J. Hepatol. 2014, 61, 435–438. [Google Scholar] [CrossRef] [PubMed]
- Abbas, Z.; Abbas, M. Management of hepatitis delta: Need for novel therapeutic options. World J. Gastroenterol. 2015, 21, 9461. [Google Scholar] [CrossRef]
- Wedemeyer, H.; Yurdaydìn, C.; Dalekos, G.N.; Erhardt, A.; Çakaloğlu, Y.; Değertekin, H.; Gürel, S.; Zeuzem, S.; Zachou, K.; Bozkaya, H.; et al. Peginterferon plus Adefovir versus Either Drug Alone for Hepatitis Delta. N. Engl. J. Med. 2011, 364, 322–331. [Google Scholar] [CrossRef] [PubMed]
- Hughes, S.A.; Wedemeyer, H.; Harrison, P.M. Hepatitis delta virus. Lancet 2011, 378, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Pischke, S.; Stiefel, P.; Franz, B.; Bremer, B.; Suneetha, P.V.; Heim, A.; Ganzenmueller, T.; Schlue, J.; Horn-Wichmann, R.; Raupach, R.; et al. Chronic hepatitis E in heart transplant recipients. Am. J. Transplant. 2012, 12, 3128–3133. [Google Scholar] [CrossRef]
- Kamar, N.; Izopet, J.; Dalton, H.R. Chronic Hepatitis E Virus Infection and Treatment. J. Clin. Exp. Hepatol. 2013, 3, 134–140. [Google Scholar] [CrossRef]
| Major Points | Content of Discussion |
|---|---|
| Overview of Viral Hepatitis and Host–Pathogen interactions | Viral hepatitis primarily affects the hepatic cells. The host–pathogen interaction is pivotal in determining disease progression and outcomes across the spectrum of hepatitis viruses. |
| Mechanisms of Viral Entry | The entry of hepatotropic viruses into liver cells relies on specific molecular mechanisms unique to each virus. The viral entry started the progression of liver disease in acute or chronic hepatitis. |
| Innate and Adaptive Immune Response | The innate immune system quickly detects viruses through receptors like TLRs and induces interferons to activate antiviral genes. Adaptive immunity, primarily through T and B cells, helps resolve acute infection or contributes to viral persistence. |
| Immune Evasion Strategies | Hepatotropic viruses could manipulate host immune responses by degrading key signaling molecules, determining infection resolution or chronicity. |
| Pathogenesis and Liver Damage | The pathogenesis of viral hepatitis results from complex interactions between the virus and the host immune system, causing different degrees of liver damage. |
| Current and Emerging Therapeutic Strategies | Even if current therapies can manage viral hepatitis and its complications, emerging treatments hold promise for more effective and targeted solutions. |
| Type of Virus Characteristics | HAV | HBV | HCV | HDV | HEV |
|---|---|---|---|---|---|
| Family | Picornaviridae | Hepadnaviridae | Flaviviridae | Deltaviridae | Hepeviridae |
| Genus | Hepatovirus | Orthohepadnavirus | Hepacivirus | Deltavirus | Orthohepevirus |
| Genome Characteristics | Quasi-enveloped, ssRNA, ~7.5 kb | Enveloped, partial dsDNA, ~3.2 kb | Enveloped, ssRNA, ~9.6 kb | Enveloped, ssRNA, ~1.7 kb (requires HBV for replication) | Quasi-enveloped, ssRNA, ~7.2 kb |
| First Discovery (year) | 1973 | 1965 | 1989 | 1977 | 1983 |
| Prevalence | 1.4–1.5 million annually | 350 million chronically infected | 58 million chronically infected | 10–20 million co-infected with HBV | 20 million cases annually |
| Incidence | 1.4 million new cases annually | 10 million new cases annually | 1.5 million new cases annually | 500,000 new cases annually | 3.3 million symptomatic cases annually |
| Transmission Route | Fecal-oral | Blood, sexual contact, perinatal | Blood, intravenous drug use, sexual contact | Blood, sexual contact, perinatal (requires HBV co-infection) | Fecal-oral, zoonotic (genotypes 3, 4), from mother to child |
| Type of hepatitis | Acute | Acute, chronic | Acute, chronic | Acute, chronic (with HBV) | Acute, chronic |
| Clinical symptoms | Jaundice, nausea, abdominal pain, fatigue, loss of appetite | Jaundice, fatigue, liver cirrhosis, HCC | Fatigue, jaundice, liver cirrhosis, HCC | Exacerbation of HBV symptoms, rapid progression to cirrhosis, HCC | Jaundice, fatigue, abdominal pain, more severe in pregnant women |
| Diagnosis | Serology (IgM anti-HAV), PCR | Serology (HBsAg, anti-HBc, HBeAg), PCR | Serology (anti-HCV), PCR | Serology (anti-HDV), PCR | Serology (IgM anti-HEV), PCR |
| Treatment | Supportive care | Nucleos(t)ide analogues, interferon | Direct-acting antivirals | Pegylated interferon-alpha, entry inhibitor Bulevirtide (authorized in Europe in July 2020) | ribavirin or pegylated interferon-α |
| Prevention | Vaccination, improved sanitation | Vaccination, safe sex practices, blood screening | Blood screening, safe injection practices | HBV vaccination, safe sex practices | Improved sanitation, vaccine available in China |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quirino, A.; Marascio, N.; Branda, F.; Ciccozzi, A.; Romano, C.; Locci, C.; Azzena, I.; Pascale, N.; Pavia, G.; Matera, G.; et al. Viral Hepatitis: Host Immune Interaction, Pathogenesis and New Therapeutic Strategies. Pathogens 2024, 13, 766. https://doi.org/10.3390/pathogens13090766
Quirino A, Marascio N, Branda F, Ciccozzi A, Romano C, Locci C, Azzena I, Pascale N, Pavia G, Matera G, et al. Viral Hepatitis: Host Immune Interaction, Pathogenesis and New Therapeutic Strategies. Pathogens. 2024; 13(9):766. https://doi.org/10.3390/pathogens13090766
Chicago/Turabian StyleQuirino, Angela, Nadia Marascio, Francesco Branda, Alessandra Ciccozzi, Chiara Romano, Chiara Locci, Ilenia Azzena, Noemi Pascale, Grazia Pavia, Giovanni Matera, and et al. 2024. "Viral Hepatitis: Host Immune Interaction, Pathogenesis and New Therapeutic Strategies" Pathogens 13, no. 9: 766. https://doi.org/10.3390/pathogens13090766











