Biofilm Growth Causes Damage to Silicone Voice Prostheses in Patients after Surgical Treatment of Locally Advanced Laryngeal Cancer
Abstract
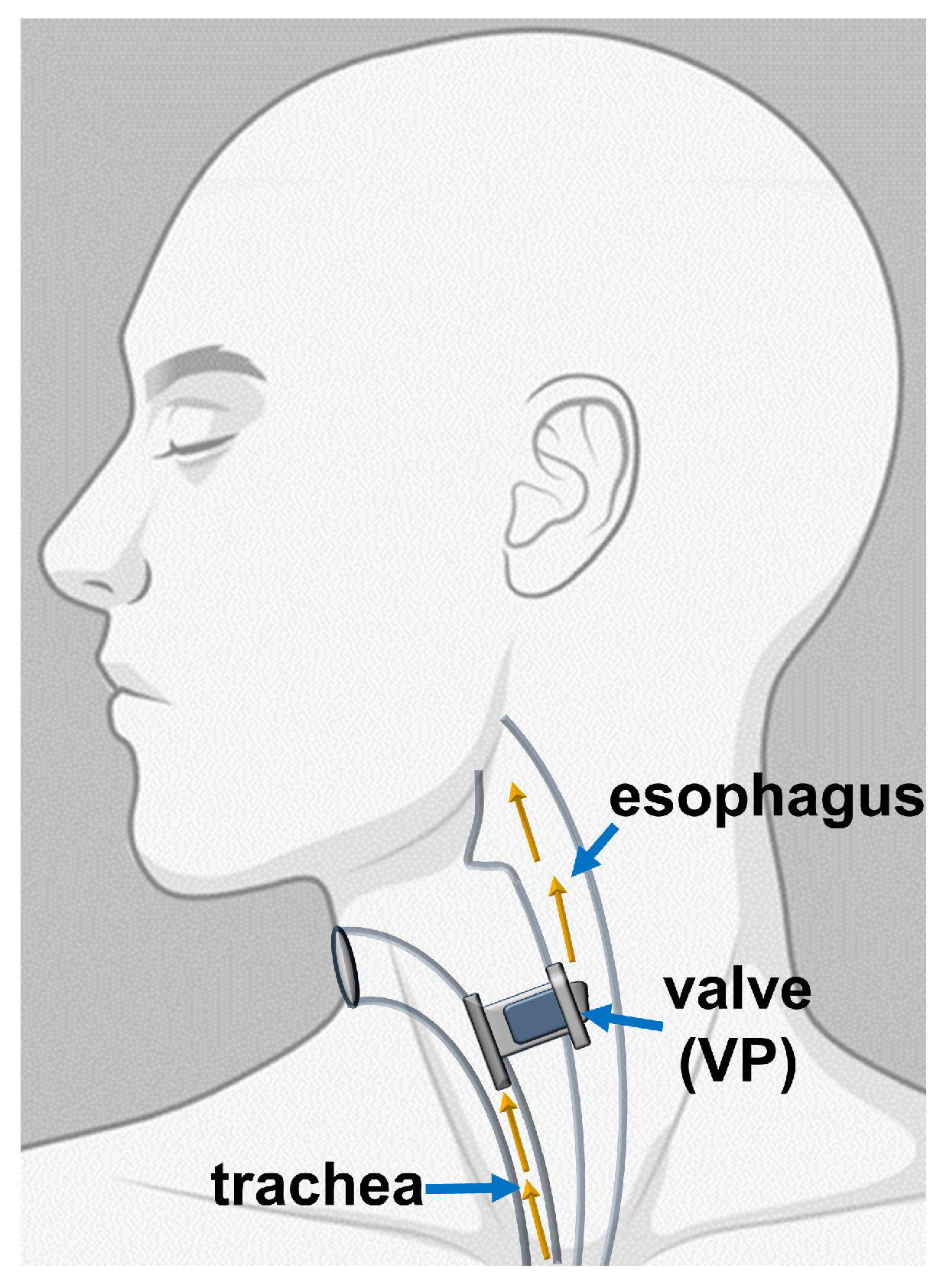
:1. Introduction
2. Results
2.1. Assessment of Microorganism Species Growing in Collected Biofilm Samples
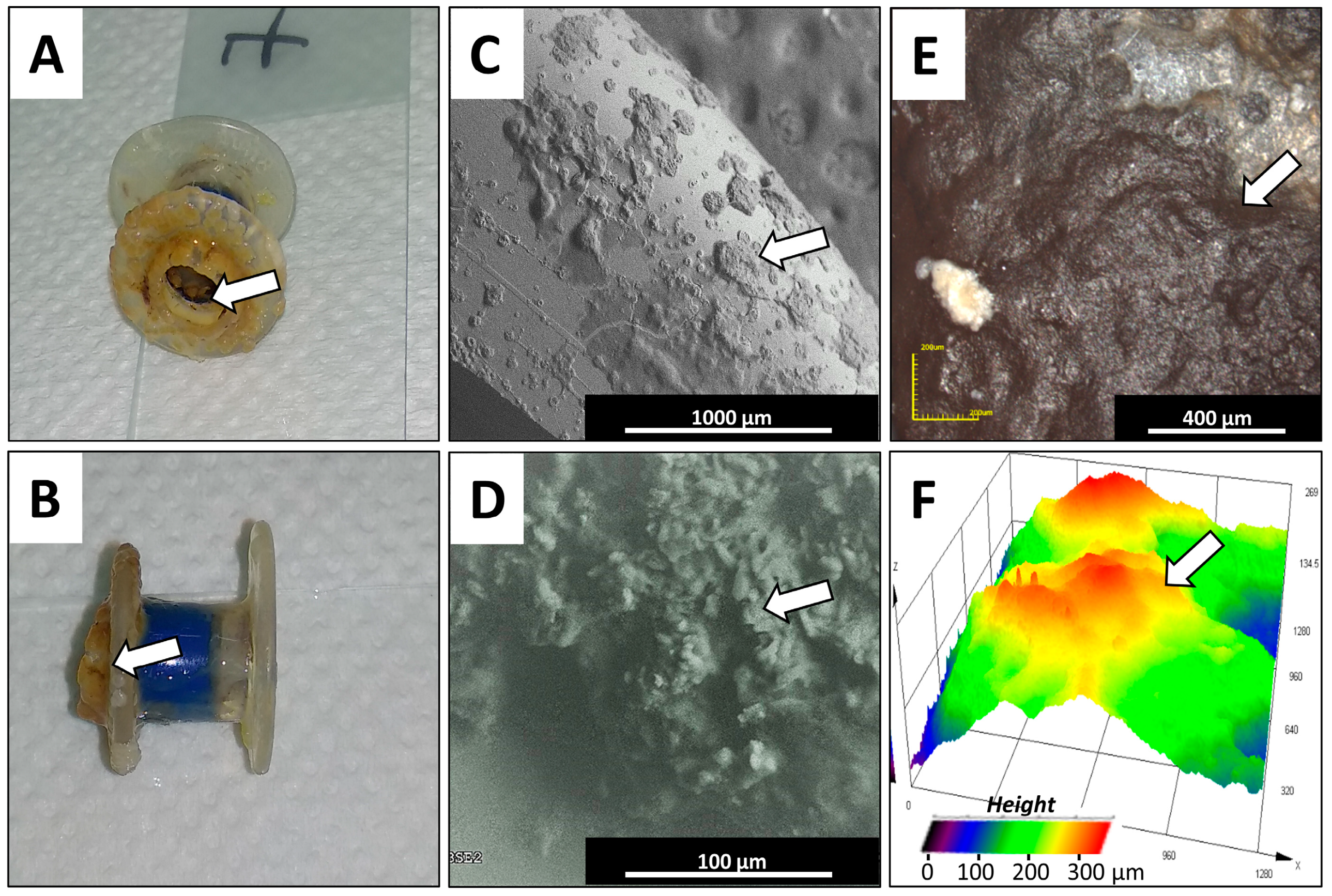
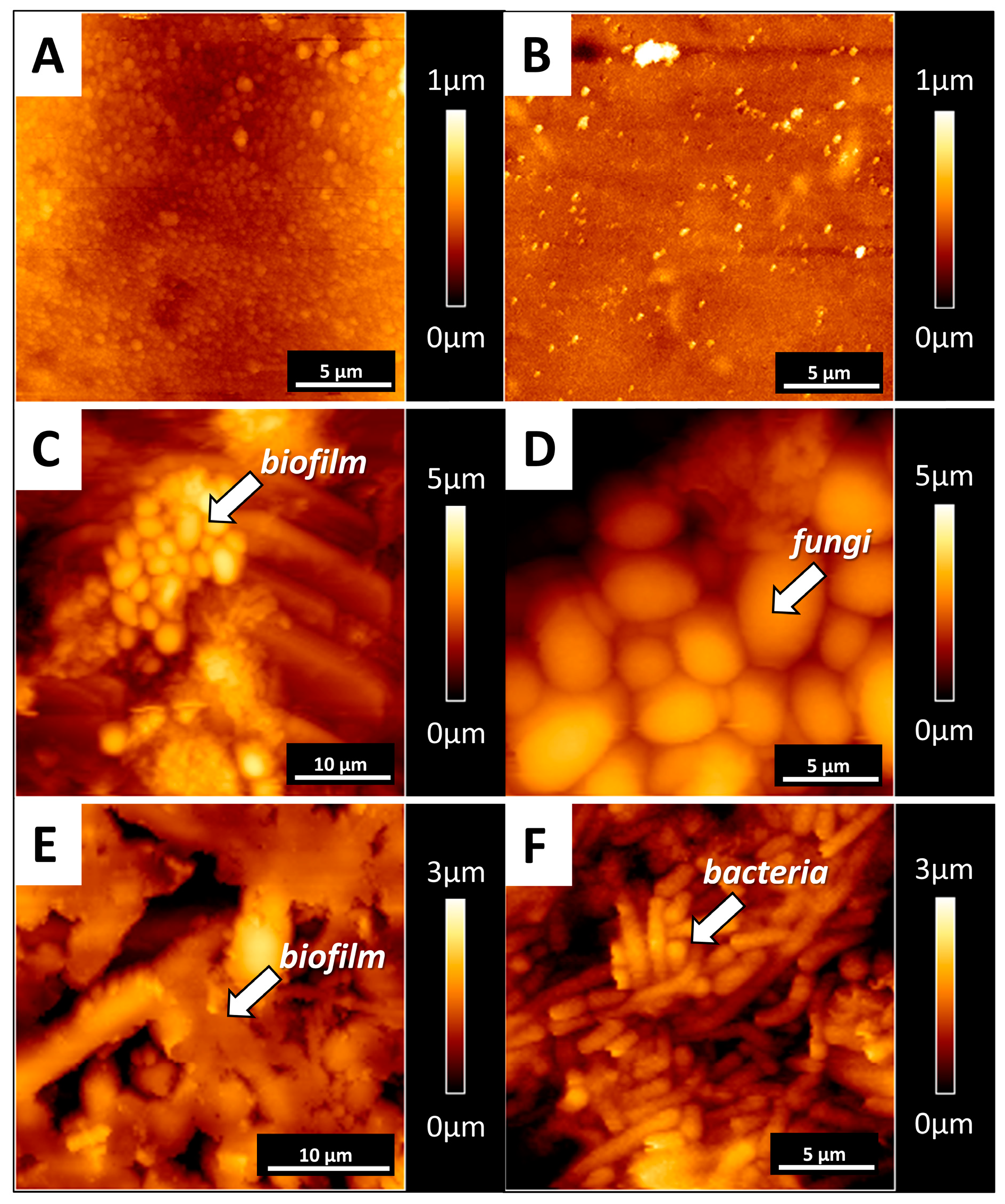
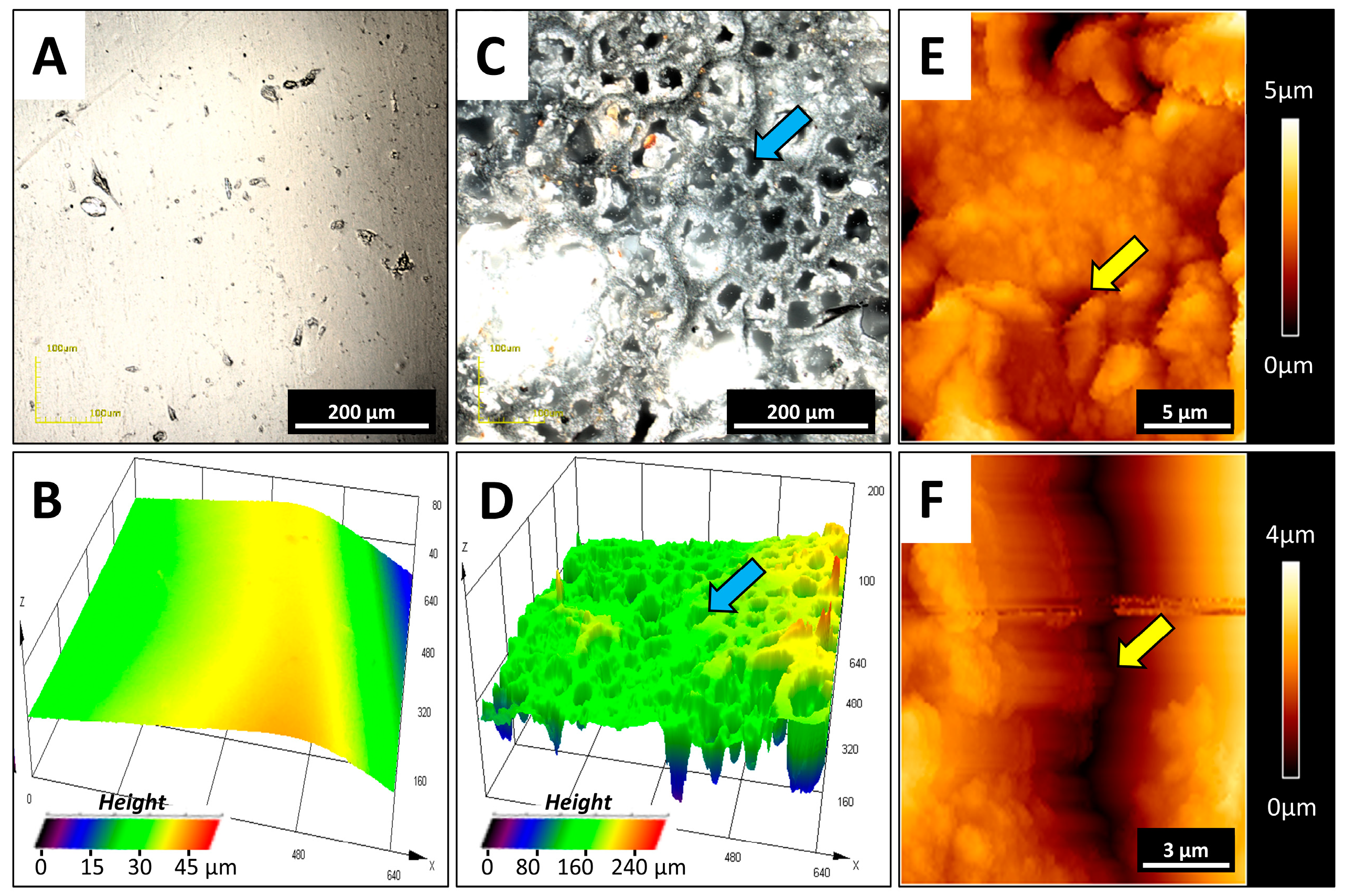
2.2. Microscopic Examination
3. Discussion
3.1. Analysis of the Study Group
3.2. Assessment of Microorganism Species Growing in Collected Biofilm Samples
3.3. Microscopic Examination
4. Materials and Methods
4.1. Voice Prostheses Collection
4.2. Characteristics of the Study Group
4.3. Assessment of Microorganisms Growing in Collected Biofilm Samples
4.4. Microscopic Studies
4.5. Thermal Measurements
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| VP | Voice prostheses |
| TL | Total laryngectomy |
| SEM | Scanning electron microscope |
| AFM | Atomic force microscope |
| TE | Tracheoesophageal |
| ECM | Extracelullar matrix |
| NADPH | Nicotinamide adenine dinucleotide phosphate |
| CLSM | Laser confocal microscope |
| DSC | Differential scanning calorimetry |
| TG | Thermogravimetry |
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2018, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Silva, A.P.; Feliciano, T.; Freitas, S.V.; Esteves, S.; Sousa, C.A.E. Quality of Life in Patients Submitted to Total Laryngectomy. J. Voice 2015, 29, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Souza, F.G.R.; Santos, I.C.; Bergmann, A.; Thuler, L.C.S.; Freitas, A.S.; Freitas, E.Q.; Dias, F.L. Quality of life after total laryngectomy: Impact of different vocal rehabilitation methods in a middle income country. Health Qual. Life Outcomes 2020, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mozolewski, E. Surgical rehabilitation of voice and speech following laryngectomy. Otolaryngol. Polska 1972, 26, 653–661. [Google Scholar]
- Singer, M.I.; Blom, E.D. An Endoscopic Technique for Restoration of Voice after Laryngectomy. Ann. Otol. Rhinol. Laryngol. 1980, 89, 529–533. [Google Scholar] [CrossRef]
- Hilgers, F.; Cornelissen, M.; Balm, A. Aerodynamic characteristics of the Provox low-resistance indwelling voice prosthesis. Eur. Arch. Oto Rhino Laryngol. 1993, 250, 375–378. [Google Scholar] [CrossRef]
- Rodrigues, M.E.; Gomes, F.; Rodrigues, C.F. Candida spp./Bacteria Mixed Biofilms. J. Fungi 2020, 6, 5. [Google Scholar] [CrossRef] [Green Version]
- Lequeux, T.; Badreldin, A.; Saussez, S.; Thill, M.P.; Oujjan, L.; Chantrain, G. A comparison of survival lifetime of the Provox® and the Provox®2 voice prosthesis. J. Laryngol. Otol. 2003, 117, 875–878. [Google Scholar] [CrossRef]
- Douglas, L.J. Candida biofilms and their role in infection. Trends Microbiol. 2003, 11, 30–36. [Google Scholar] [CrossRef]
- Kojic, E.M.; Darouiche, R.O. Candida Infections of Medical Devices. Clin. Microbiol. Rev. 2004, 17, 255–267. [Google Scholar] [CrossRef] [Green Version]
- Galli, J.; Calo, L.; Meucci, D.; Giuliani, M.; Lucidi, D.; Troiani, G.P.; Torelli, R.; Sanguinetti, M.; Parrilla, C. Biofilm in voice prosthesis: A prospective cohort study and laboratory tests using sonication and SEM analysis. Clin. Otolaryngol. 2018, 43, 1260–1265. [Google Scholar] [CrossRef] [PubMed]
- Ell, S.R. Candida—‘the cancer of silastic’. J. Laryngol. Otol. 1996, 110, 240–242. [Google Scholar] [CrossRef]
- Bertl, K.; Ma, B.Z.; Leonhard, M.; Matejka, M.; Schneider-Stickler, B. Anaerobic and microaerophilic pathogens in the biofilm formation on voice prostheses: A pilot study. Laryngoscope 2012, 122, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Nobbs, A.H.; Vickerman, M.M.; Jenkinson, H.F. Heterologous Expression of Candida albicans Cell Wall-Associated Adhesins in Saccharomyces cerevisiae Reveals Differential Specificities in Adherence and Biofilm Formation and in Binding Oral Streptococcus gordonii. Eukaryot. Cell 2010, 9, 1622–1634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, B.M.; Ovchinnikova, E.S.; Krom, B.P.; Schlecht, L.M.; Zhou, H.; Hoyer, L.L.; Busscher, H.J.; Van Der Mei, H.C.; Jabra-Rizk, M.A.; Shirtliff, M.E. Staphylococcus aureus adherence to Candida albicans hyphae is mediated by the hyphal adhesin Als3p. Microbiology 2012, 158, 2975–2986. [Google Scholar] [CrossRef] [Green Version]
- Van Weissenbruch, R.; Albers, F.W.J.; Bouckaert, S.; Nelis, H.J.; Criel, G.; Remon, J.P.; Sulter, A.M. Deterioration of the Provox™Silicone Tracheoesophageal Voice Prosthesis: Microbial Aspects and Structural Changes. Acta Oto Laryngol. 1997, 117, 452–458. [Google Scholar] [CrossRef]
- Babior, B.; Lambeth, J.; Nauseef, W.M. The Neutrophil NADPH Oxidase. Arch. Biochem. Biophys. 2002, 397, 342–344. [Google Scholar] [CrossRef]
- Beranová, M.; Wasserbauer, R.; Vancurová, D.; Stifter, M.; Očenášková, J.; Mára, M. Effect of cytochrome P-450 inhibition and stimulation on intensity of polyethylene degradation in microsomal fraction of mouse and rat livers. Biomaterials 1990, 11, 521–524. [Google Scholar] [CrossRef]
- Lagree, K.; Mon, H.H.; Mitchell, A.P.; Ducker, W.A. Impact of surface topography on biofilm formation by Candida albicans. PLoS ONE 2018, 13, e0197925. [Google Scholar] [CrossRef] [Green Version]
- Finkel, J.S.; Xu, W.; Huang, D.; Hill, E.M.; Desai, J.V.; Woolford, C.; Nett, J.E.; Taff, H.; Norice, C.T.; Andes, D.R.; et al. Portrait of Candida albicans Adherence Regulators. PLOS Pathog. 2012, 8, e1002525. [Google Scholar] [CrossRef] [Green Version]
- Fusconi, M.; Taddei, A.R.; Gallo, A.; Conte, M.; De Virgilio, A.; Greco, A.; Vasco, V.R.L.; Macri, G.F.; Roma, R.; Volpini, F.; et al. Degradation of Silicone Rubber Causes Provox 2 Voice Prosthesis Malfunctioning. J. Voice 2014, 28, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Costerton, J.W.; Philip, S.P.; Greenberg, E.P. Bacterial biofilms: A common cause of persistent infections. Science 1999, 284, 1318–1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carolus, H.; Van Dyck, K.; Van Dijck, P. Candida albicans and Staphylococcus Species: A Threatening Twosome. Front. Microbiol. 2019, 10, 2162. [Google Scholar] [CrossRef] [PubMed]
- Van Den Hoogen, F.J.; Oudes, M.J.; Hombergen, G.; Nijdam, H.F.; Manni, J.J. The Groningen, Nijdam and Provox Voice Prostheses: A Prospective Clinical Comparison Based on 845 Replacements. Acta Oto Laryngol. 1996, 116, 119–124. [Google Scholar] [CrossRef]
- Laccourreye, O.; Ménard, M.; Crevier-Buchman, L.; Couloigner, V.; Brasnu, D. In Situ Lifetime, Causes for Replacement, and Complications of the ProvoxTM Voice Prosthesis. Laryngoscope 2009, 107, 527–530. [Google Scholar] [CrossRef]
- Lewin, J.; Baumgart, L.M.; Barrow, M.P.; Hutcheson, K.A. Device Life of the Tracheoesophageal Voice Prosthesis Revisited. JAMA Otolaryngol. Neck Surg. 2017, 143, 65–71. [Google Scholar] [CrossRef]
- Kress, P.; Schäfer, P.; Schwerdtfeger, F.P.; Rößler, S. Are modern voice prostheses better? A lifetime comparison of 749 voice prostheses. Eur. Arch. Oto Rhino Laryngol. 2013, 271, 133–140. [Google Scholar] [CrossRef] [Green Version]
- Pawar, P.; Kelkar, R.; Biswas, S.; Datta, S.; Nair, D.; Chaukar, D.; D′cruz, A.; Chaturvedi, P.; Syed, S. Microbial colonization of Provox voice prosthesis in the Indian scenario. Indian J. Cancer 2014, 51, 184. [Google Scholar] [CrossRef]
- Ameye, D.; Honraet, K.; Loose, D.; Vermeersch, H.; Nelis, H.; Remon, J.P. Effect of a buccal bioadhesive nystatin tablet on the lifetime of a Provox™ silicone tracheoesophageal voice prosthesis. Acta Oto Laryngol. 2005, 125, 304–306. [Google Scholar] [CrossRef]
- Messing, B.P.; Kim, M.; Hirata, R.; Thompson, C.B.; Gebhart, S.; Sugar, E.A.; Saunders, J.M.; Sciubba, J.; Califano, J. Evaluation of prophylaxis treatment of Candida in alaryngeal patients with tracheoesophageal voice prostheses. Laryngoscope 2014, 125, 1118–1123. [Google Scholar] [CrossRef]
- Obid, R.; Redlich, M.; Tomeh, C. The Treatment of Laryngeal Cancer. Oral Maxillofac. Surg. Clin. 2019, 31, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Op de Coul, B.M.; Hilgers, F.J.; Balm, A.J.; Tan, I.B.; Van den Hoogen, F.J.; Van Tinteren, H. A decade of postlaryngectomy vocal rehabilitation in 318 patients: A single Institution’s experience with consistent application of provox indwelling voice prostheses. Arch Otolaryngol. Head Neck Surg. 2000, 126, 1320–1328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talpaert, M.J.; Balfour, A.; Stevens, S.; Baker, M.; Muhlschlegel, F.A.; Gourlay, C.W. Candida biofilm formation on voice prostheses. J. Med. Microbiol. 2015, 64, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Timmermans, A.J.; Harmsen, H.J.; Bus-Spoor, C.; Buijssen, K.J.; Van As-Brooks, C.; De Goffau, M.C.; Tonk, R.H.; Van den Brekel, M.W.; Hilgers, F.J.; Van der Laan, B.F. Biofilm formation on the Provox ActiValve: Composition and ingrowth analyzed by Illumina paired-end RNA sequencing, fluorescence in situ hybridization, and confocal laser scanning microscopy. Head Neck 2015, 38, E432–E440. [Google Scholar] [CrossRef]
- Leonhard, M.; Zatorska, B.; Tan, Y.; Moser, D.; Schneider-Stickler, B. In vitro biofilm growth on modern voice prostheses. Head Neck 2017, 40, 763–769. [Google Scholar] [CrossRef]
- Leonhard, M.; Moser, D.; Reumueller, A.; Mancusi, G.; Bigenzahn, W.; Schneider-Stickler, B. Comparison of biofilm formation on new Phonax and Provox 2 voice prostheses-A pilot study. Head Neck 2009, 32, 886–895. [Google Scholar] [CrossRef]
- Free, R.H.; Elving, G.J.; Van Weissenbruch, R.; Busscher, H.J.; Van Der Mei, H.C.; Albers, F.W.J. Biofilm formation on voice prostheses: In vitro influence of probiotics. Ann. Otol. Rhinol. Laryngol. 2001, 110, 946–951. [Google Scholar] [CrossRef]
- Leonhard, M.; Reumueller, A.; Moser, D.; Bigenzahn, W.; Schneider-Stickler, B. Examination of biofilm related material deterioration on 20 PROVOX2 voice prostheses by scanning electron microscopy. Laryngo Rhino Otol. 2009, 88, 392–397. [Google Scholar] [CrossRef]
- Ariani, N.; Vissink, A.; Van Oort, R.P.; Kusdhany, L.; Djais, A.; Rahardjo, T.B.W.; Van Der Mei, H.C.; Krom, B.P. Microbial biofilms on facial prostheses. Biofouling 2012, 28, 583–591. [Google Scholar] [CrossRef]
- Flemming, H.-C. Relevance of biofilms for the biodeterioration of surfaces of polymeric materials. Polym. Degrad. Stab. 1998, 59, 309–315. [Google Scholar] [CrossRef]
- Bucki, R.; Niemirowicz-Laskowska, K.; Deptuła, P.; Wilczewska, A.Z.; Misiak, P.; Durnaś, B.; Fiedoruk, K.; Piktel, E.; Mystkowska, J.; Janmey, P.A. Susceptibility of microbial cells to the modified PIP2-binding sequence of gelsolin anchored on the surface of magnetic nanoparticles. J. Nanobiotechnol. 2019, 17, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durnaś, B.; Wnorowska, U.; Pogoda, K.; Deptuła, P.; Wątek, M.; Piktel, E.; Gluszek, S.; Gu, X.; Savage, P.B.; Niemirowicz, K.; et al. Candidacidal Activity of Selected Ceragenins and Human Cathelicidin LL-37 in Experimental Settings Mimicking Infection Sites. PLoS ONE 2016, 11, e0157242. [Google Scholar] [CrossRef] [PubMed]
- Durnaś, B.; Piktel, E.; Wątek, M.; Wollny, T.; Góźdź, S.; Smok-Kalwat, J.; Niemirowicz-Laskowska, K.; Savage, P.B.; Bucki, R. Anaerobic bacteria growth in the presence of cathelicidin LL-37 and selected ceragenins delivered as magnetic nanoparticles cargo. BMC Microbiol. 2017, 17, 167. [Google Scholar] [CrossRef] [PubMed]
- Niemirowicz, K.; Durnaś, B.; Tokajuk, G.; Piktel, E.; Michalak, G.; Gu, X.; Kułakowska, A.; Savage, P.B.; Bucki, R. Formulation and candidacidal activity of magnetic nanoparticles coated with cathelicidin LL-37 and ceragenin CSA-13. Sci. Rep. 2017, 7, 4610. [Google Scholar] [CrossRef] [PubMed]
- Niemirowicz-Laskowska, K.; Głuszek, K.; Piktel, E.; Pajuste, K.; Durnaś, B.; Król, G.; Wilczewska, A.Z.; Janmey, A.P.; Plotniece, A.; Bucki, R. Bactericidal and immunomodulatory properties of magnetic nanoparticles functionalized by 1,4-dihydropyridines. Int. J. Nanomed. 2018, 13, 3411–3424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niemirowicz-Laskowska, K.; Mystkowska, J.; Łysik, D.; Chmielewska, S.; Tokajuk, G.; Misztalewska-Turkowicz, I.; Wilczewska, A.Z.; Bucki, R. Antimicrobial and Physicochemical Properties of Artificial Saliva Formulations Supplemented with Core-Shell Magnetic Nanoparticles. Int. J. Mol. Sci. 2020, 21, 1979. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hutcheson, K.A.; Lewin, J.; Sturgis, E.M.; Risser, J. Outcomes and adverse events of enlarged tracheoesophageal puncture after total laryngectomy. Laryngoscope 2011, 121, 1455–1461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lekka, M.; Gil, D.; Pogoda, K.; Dulińska-Litewka, J.; Jach, R.; Gostek, J.; Klymenko, O.; Prauzner-Bechcicki, S.; Stachura, Z.; Wiltowska-Zuber, J.; et al. Cancer cell detection in tissue sections using AFM. Arch. Biochem. Biophys. 2012, 518, 151–156. [Google Scholar] [CrossRef]
- Pogoda, K.; Chin, L.; Georges, P.C.; Byfield, F.J.; Bucki, R.; Kim, R.; Weaver, M.; Wells, R.G.; Marcinkiewicz, C.; Janmey, P.A. Compression stiffening of brain and its effect on mechanosensing by glioma cells. New J. Phys. 2014, 16, 075002. [Google Scholar] [CrossRef]
- Łysik, D.; Mystkowska, J.; Markiewicz, G.; Deptuła, P.; Bucki, R. The Influence of Mucin-Based Artificial Saliva on Properties of Polycaprolactone and Polylactide. Polymers 2019, 11, 1880. [Google Scholar] [CrossRef] [Green Version]


| Species/Group of the Prostheses | Group 1 (n = 7) n (%) | Group 2 (n = 24) n (%) | Group 3 (n = 32) n (%) | Group 4 (n = 49) n (%) | Group 5 (n = 17) n (%) | Total (n = 129) n (%) | p = Value |
|---|---|---|---|---|---|---|---|
| Candida krusei | 3 (2.3) | 13 (10.1) | 16 (12.4) | 28 (21.7) | 12 (9.3) | 72 (55.8) | p = 0.648 * |
| Candida albicans | 3 (2.3) | 11 (8.5) | 16 (12.4) | 24 (18.6) | 6 (4.7) | 60 (46.5) | p = 0.882 * |
| Candida glabrata | 4 (3.1) | 9 (7.0) | 11 (8.5) | 20 (15.5) | 11 (8.5) | 55 (42.6) | p = 0.268 * |
| Candida tropicalis | 2 (1.55) | 4 (3.1) | 7 (5.4) | 9 (7.0) | 2 (1.55) | 24 (18.6) | p = 0.865 * |
| Saccharomyces cerevisiae | 0 (0.0) | 1 (0.8) | 1 (0.8) | 5 (3.9) | 1 (0.8) | 8 (6.2) | p = 0.581 * |
| Species/Group of the Prosthesis | Group 1 (n = 7) n | Group 2 (n = 24) n | Group 3 (n = 32) n | Group 4 (n = 49) n | Group 5 (n = 17) n | Total (n = 129) n |
|---|---|---|---|---|---|---|
| Candida dubliniensis | 0 | 0 | 1 | 0 | 0 | 1 |
| Candida kefyr | 0 | 1 | 1 | 2 | 0 | 4 |
| Candida lusitaniae | 1 | 0 | 0 | 0 | 0 | 1 |
| Cryptococcus neoformans | 0 | 0 | 1 | 0 | 0 | 1 |
| Candida norvegensis | 0 | 0 | 1 | 2 | 0 | 1 |
| Candida parapsilosis | 0 | 1 | 0 | 1 | 0 | 2 |
| Rhodotorula glutinis | 0 | 0 | 2 | 1 | 1 | 4 |
| Cryptococcus laurenti | 0 | 0 | 0 | 1 | 0 | 1 |
| No species identified | 0 | 1 | 0 | 3 | 0 | 4 |
| Cat. | Species | Group 1 (n = 7) n | Group 2 (n = 24) n | Group 3 (n = 32) n | Group 4 (n = 49) n | Group 5 (n = 17) n | Total (n = 129) n |
|---|---|---|---|---|---|---|---|
| I * | Citrobacter freundi | 0 | 1 | 1 | 0 | 0 | 2 |
| Enterobacter cloacae | 0 | 0 | 1 | 0 | 0 | 1 | |
| Escherichia coli | 0 | 1 | 3 | 2 | 3 | 9 | |
| Klebsiella oxytoca | 0 | 1 | 0 | 4 | 1 | 6 | |
| Klebsiella pneumoniae | 1 | 1 | 2 | 1 | 1 | 6 | |
| Morganella morganii | 0 | 0 | 0 | 1 | 0 | 1 | |
| Proteus hauseri | 0 | 0 | 0 | 0 | 1 | 1 | |
| Proteus mirabilis | 0 | 0 | 2 | 3 | 2 | 7 | |
| Raoultella planticola | 0 | 1 | 1 | 2 | 0 | 4 | |
| Serratia marcescens | 0 | 2 | 3 | 1 | 0 | 6 | |
| II * | Streptococcus agalactiae | 1 | 1 | 3 | 1 | 0 | 6 |
| Streptococcus group C | 0 | 0 | 1 | 0 | 0 | 1 | |
| III * | Streptococcus spp. | 2 | 4 | 6 | 5 | 0 | 17 |
| Streptococcus viridans | 0 | 1 | 0 | 5 | 0 | 6 | |
| Enterococcus spp. | 0 | 0 | 0 | 0 | 1 | 1 | |
| Staphylococcus coag. (−) | 0 | 2 | 1 | 3 | 0 | 6 | |
| No Cat. * | Pseudomonas aeruginosa | 1 | 2 | 3 | 1 | 1 | 8 |
| Staphylococcus aureus | 3 | 11 | 16 | 23 | 4 | 57 |
| Species/Group of the Prosthesis | Group 1 (n = 7) n | Group 2 (n = 24) n | Group 3 (n = 32) n | Group 4 (n = 49) n | Group 5 (n = 17) n | Total (n = 129) n | p = Value |
|---|---|---|---|---|---|---|---|
| Staphylococcus aureus | |||||||
| 3 (2.3) | 11 (8.5) | 16 (12.4) | 23 (17.8) | 4 (3.1) | 57 (44.2) | p = 0.439 * | |
| Physiological oropharyngeal microbiota | |||||||
| 2 (1.55) | 13 (10.1) | 10 (7.75) | 14 (10.85) | 3 (2.3) | 42 (32.6) | p = 0.131 * | |
| Enterobacteria | |||||||
| 1 (0.78) | 6 (4.65) | 12 (9.3) | 14 (10.85) | 6 (4.65) | 39 (30.2) | p = 0.675 * | |
| Physiological oropharyngeal microbiota only | |||||||
| 1 (0.78) | 11 (8.5) | 6 (4.65) | 11 (8.5) | 2 (1.55) | 31 (24.0) | p = 0.090 * | |
| ß-hemolytic streptococci | |||||||
| 1 (0.78) | 1 (0.78) | 4 (3.1) | 1 (0.78) | 0 (0.0) | 7 (5.4) | p = 0.166 * | |
| Pseudomonas aeruginosa | |||||||
| 1 (0.78) | 2 (1.55) | 3 (2.3) | 1 (0.78) | 1 (0.78) | 8 (6.2) | p = 0.527 * | |
| Type of Biofilm | Occurrence of the Certain Type of Biofilm in Each Group (%) | |||||
|---|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | Total | |
| mixed (bacteria/fungi) | 71.4 | 87.5 | 93.8 | 79.6 | 70.6 | 83.0 |
| fungi | 28.6 | 8.3 | 6.3 | 16.3 | 29.4 | 14.7 |
| bacteria | 0.0 | 4.2 | 0.0 | 4.1 | 0.0 | 2.3 |
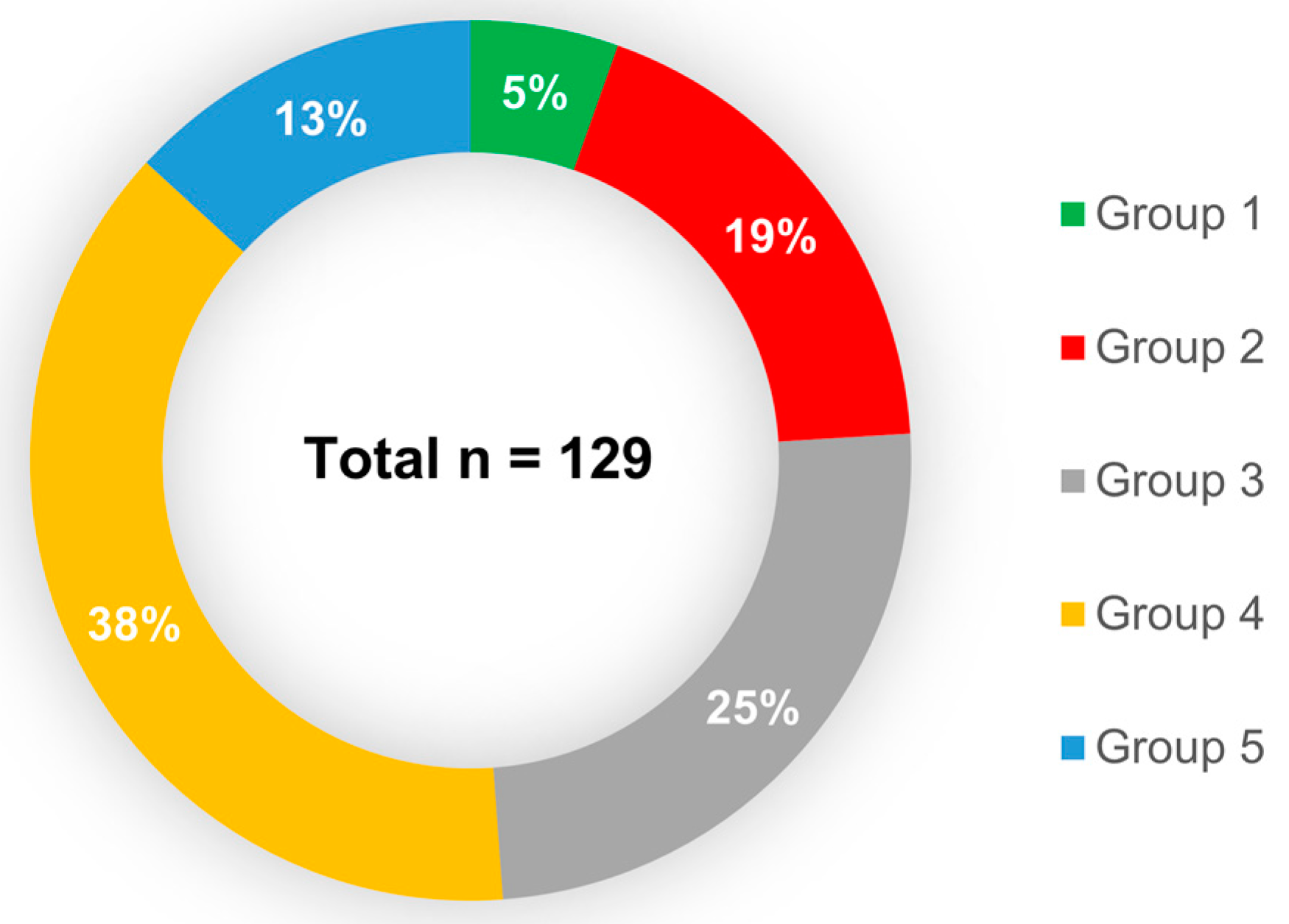
| The Time of Exploitation | Number of Prostheses Tested n (%) | Number of Males n (%) | Number of Females n (%) |
|---|---|---|---|
| Total | 129 (100) | 116 (90) | 13 (10) |
| <one month (Group 1) | 7 (5) | 6 (4.7) | 1 (0.8) |
| 1–3 months (Group 2) | 24 (19) | 21 (16.3) | 3 (2.3) |
| 4–6 months (Group 3) | 31 (25) | 28 (21.8) | 4 (3.1) |
| 7–12 months (Group 4) | 49 (38) | 47 (36.4) | 2 (1.6) |
| >12 months (Group 5) | 17 (13) | 14 (10.9) | 3 (2.3) |
| Type of Voice Prosthesis | Number of Prostheses Tested n (%) |
|---|---|
| Total | 129 (100) |
| Provox Vega | 119 (92) |
| 4 mm | 1 |
| 6 mm | 30 |
| 8 mm | 66 |
| 10 mm | 17 |
| 12.5 mm | 5 |
| Provox 2 | 4 (3) |
| Provox XS | 6 (5) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spałek, J.; Deptuła, P.; Cieśluk, M.; Strzelecka, A.; Łysik, D.; Mystkowska, J.; Daniluk, T.; Król, G.; Góźdź, S.; Bucki, R.; et al. Biofilm Growth Causes Damage to Silicone Voice Prostheses in Patients after Surgical Treatment of Locally Advanced Laryngeal Cancer. Pathogens 2020, 9, 793. https://doi.org/10.3390/pathogens9100793
Spałek J, Deptuła P, Cieśluk M, Strzelecka A, Łysik D, Mystkowska J, Daniluk T, Król G, Góźdź S, Bucki R, et al. Biofilm Growth Causes Damage to Silicone Voice Prostheses in Patients after Surgical Treatment of Locally Advanced Laryngeal Cancer. Pathogens. 2020; 9(10):793. https://doi.org/10.3390/pathogens9100793
Chicago/Turabian StyleSpałek, Jakub, Piotr Deptuła, Mateusz Cieśluk, Agnieszka Strzelecka, Dawid Łysik, Joanna Mystkowska, Tamara Daniluk, Grzegorz Król, Stanisław Góźdź, Robert Bucki, and et al. 2020. "Biofilm Growth Causes Damage to Silicone Voice Prostheses in Patients after Surgical Treatment of Locally Advanced Laryngeal Cancer" Pathogens 9, no. 10: 793. https://doi.org/10.3390/pathogens9100793





