The Role of the Human Gut Microbiome in Inflammatory Bowel Disease and Radiation Enteropathy
Abstract
:1. Role of the Human Gut Microbiome
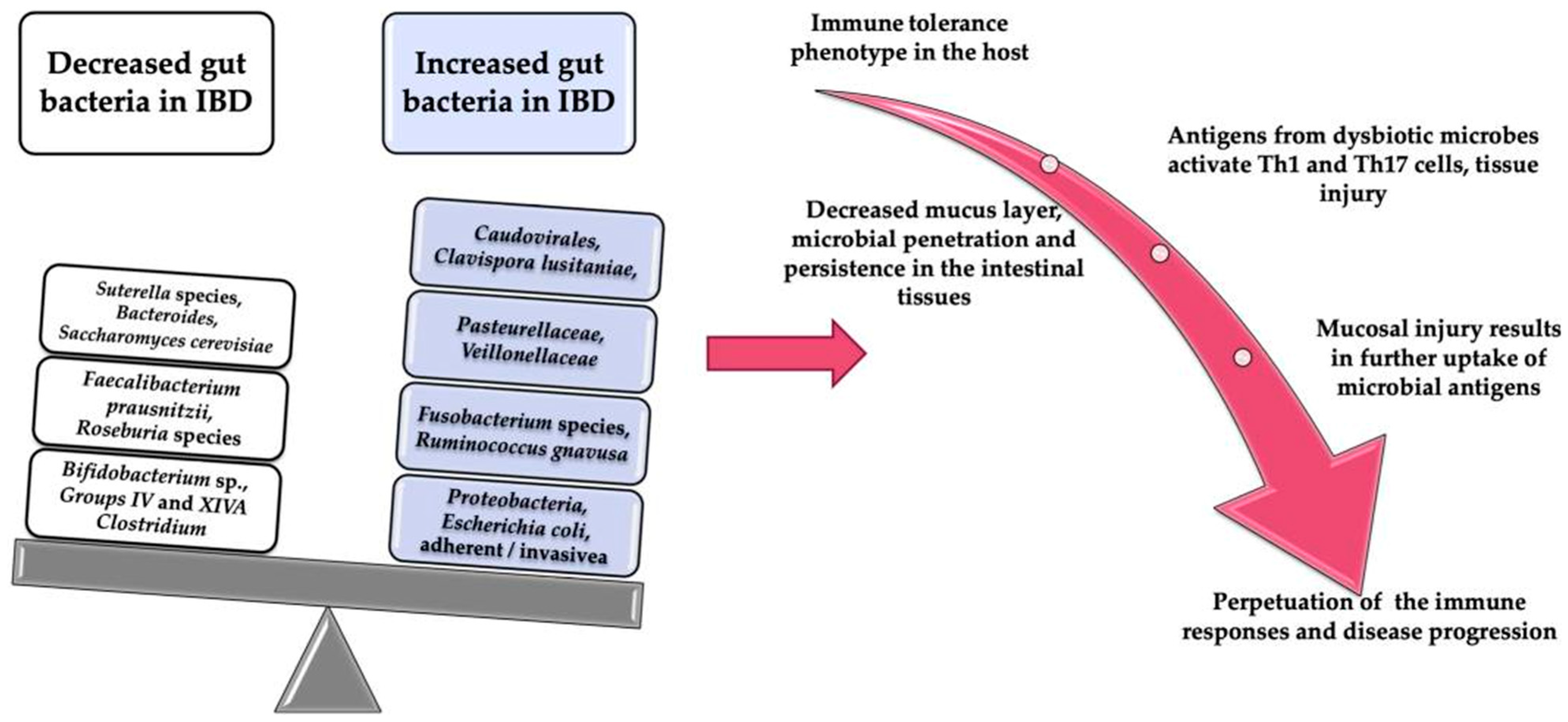
2. The Oxygen Hypothesis
3. IBD and the Gut Microbiome
| Bacterial Species | Nature of Change (Increase/Decrease) | Change in UC or Crohn’s Disease | Likely Effect of the Change | |
|---|---|---|---|---|
| Proteobacteria | Escherichia Salmonella Legionellales | Varies | Both | Pro-inflammatory if increased [25,26], anti-inflammatory if decreased [23,27]. In CD patients, intestinal permeability is increased due to adhesion-invasive E. coli, which leads to inflammation [28,29]. |
| Bacteroidetes | Varies | Both | Pro-inflammatory if increased [25,26], anti-inflammatory if decreased [23,27]. | |
| Firmicutes | Faecalibacterium prausnitzii | Decreased | Both | Pro-inflammatory [30,31] and increased risk of post-operative occurrence in CD [32] due to reduction in short-chain fatty acids, especially butyrate [33]; this has an anti-inflammatory effect, provides energy for colonic epithelial cells, may strengthen epithelial barrier integrity, and plays a role in GI immune responses [34]. Recovery of population associated with maintenance of clinical remission in UC [32] due to production of interleukin (IL)-10 and inhibition of inflammatory cytokines, such as IL-12 and interferon-γ [35]. |
| Roseburia inulinvorans | Decreased | CD | Pro-inflammatory [30,31], higher genetic risk of IBD in healthy individuals with decreased levels [36]. | |
| Ruminococcus torques | Decreased | CD | Pro-inflammatory [30,31] | |
| Blautia faecis | Decreased | CD | Pro-inflammatory [30,31] | |
| Clostridium lavalense | Decreased | CD | Pro-inflammatory [30,31] | |
| Erysipelotrichales Clostridiales | Decreased | CD | Pro-inflammatory due to reduction in butyrate production [28,29,36,37]. | |
| Veillonellaceae | Increased | CD | Pro-inflammatory [36] | |
| Enterobacteriaceae Pasteurellaceae Fusobacteriaceae | Increased | CD | Pro-inflammatory [36] | |
4. Studies Assessing the Microbiome of Twins with IBD
5. The Effects of Radiotherapy on the Gut Microbiome
6. The Human Gut Virome
- Eukaryotic viruses that infect human cells trigger immune responses, which can then lead to disease.
- Phages can affect the host indirectly via modulation of bacterial composition and bacterial fitness.
7. How the Microbiome Acts as the Guardian of the Gut from Radiation: Parallels with IBD
8. Treatment in IBD
9. Probiotics
- Triggering a rise in anti-inflammatory cytokines (IL-10, transforming growth factor beta (TGF β)).
- Release of antimicrobial products and halting of bacterial development.
- Stimulating the immune response.
- Enhancing epithelial barrier function.
- Stopping T-cell generation.
- To be able to withstand the acid secretions of the stomach, gallbladder, and pancreas, thus remaining viable when they reach the small and large intestines.
- To remain functionable during transfer and storing.
- Not to have any adverse effect on normal tissue structures.
- To benefit the host.
- To stick to intestinal epithelial cells.
- To stabilise the intestinal microbiota.
- To secrete antimicrobial products.
10. Prebiotics
11. Synbiotics
12. Faecal Microbial Transplantation
13. Antibiotics
14. Diet
15. Faecal Virome Transplantation
16. Phage Therapy
- An ability to increase their number where their host is present.
- Being highly specific and infecting only a few bacterial strains.
- Remaining in an environment only when their hosts are present.
- Able to modify themselves in relation to evolving bacteria, allowing them to remain capable of infecting and lysing the bacteria.
17. Therapeutic Options for Radiation-Induced Intestinal Injury
18. Probiotics
19. Prebiotics
20. Faecal Microbial Transplantation
21. Antibiotics
22. Conclusions and Future
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Fernandes, A.; Oliveira, A.; Soares, R.; Barata, P. The Effects of Ionizing Radiation on Gut Microbiota, a Systematic Review. Nutrients 2021, 13, 3025. [Google Scholar] [CrossRef] [PubMed]
- Gill Steven, R.; Pop, M.; DeBoy Robert, T.; Eckburg Paul, B.; Turnbaugh Peter, J.; Samuel Buck, S.; Gordon Jeffrey, I.; Relman David, A.; Fraser–Liggett Claire, M.; Nelson Karen, E. Metagenomic analysis of the human distal gut microbiome. Science 2006, 312, 1355–1359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turnbaugh, P.J.; Ley, R.E.; Mahowald, M.A.; Magrini, V.; Mardis, E.R.; Gordon, J.I. An Obesity-Associated Gut Microbiome with Increased Capacity for Energy Harvest. Nature 2006, 444, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, T.; Rahman, F.; Smith, A.M. The Microbiome and Radiation Induced-Bowel Injury: Evidence for Potential Mechanistic Role in Disease Pathogenesis. Nutrients 2018, 10, 1405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alatab, S.; Sepanlou, S.G.; Ikuta, K.; Vahedi, H.; Bisignano, C.; Safiri, S.; Sadeghi, A.; Nixon, M.R.; Abdoli, A.; Abolhassani, H.; et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 17–30. [Google Scholar] [CrossRef] [Green Version]
- DeWitt, T.; Hegazi, R. Nutrition in pelvic radiation disease and inflammatory bowel disease: Similarities and differences. BioMed Res. Int. 2014, 2014, 716579. [Google Scholar] [CrossRef]
- Andreyev, H.J.; Benton, B.E.; Lalji, A.; Norton, C.; Mohammed, K.; Gage, H.; Pennert, K.; Lindsay, J.O. Algorithm-based management of patients with gastrointestinal symptoms in patients after pelvic radiation treatment (ORBIT): A randomised controlled trial. Lancet 2013, 382, 2084–2092. [Google Scholar] [CrossRef]
- Friedman, E.S.; Bittinger, K.; Esipova, T.V.; Hou, L.; Chau, L.; Jiang, J.; Mesaros, C.; Lund, P.J.; Liang, X.; FitzGerald, G.A.; et al. Microbes vs. chemistry in the origin of the anaerobic gut lumen. Proc. Natl. Acad. Sci. USA 2018, 115, 4170–4175. [Google Scholar] [CrossRef] [Green Version]
- Rivera-Chavez, F.; Lopez, C.A.; Zhang, L.F.; Garcia-Pastor, L.; Chavez-Arroyo, A.; Lokken, K.L.; Tsolis, R.M.; Winter, S.E.; Baumler, A.J. Energy Taxis toward Host-Derived Nitrate Supports a Salmonella Pathogenicity Island 1-Independent Mechanism of Invasion. mBio 2016, 7, e00960-16. [Google Scholar] [CrossRef] [Green Version]
- Sundin, O.H.; Mendoza-Ladd, A.; Zeng, M.; Diaz-Arevalo, D.; Morales, E.; Fagan, B.M.; Ordonez, J.; Velez, P.; Antony, N.; McCallum, R.W. The human jejunum has an endogenous microbiota that differs from those in the oral cavity and colon. BMC Microbiol. 2017, 17, 160. [Google Scholar] [CrossRef] [Green Version]
- Byndloss, M.X.; Olsan, E.E.; Rivera-Chavez, F.; Tiffany, C.R.; Cevallos, S.A.; Lokken, K.L.; Torres, T.P.; Byndloss, A.J.; Faber, F.; Gao, Y.; et al. Microbiota-activated PPAR-gamma signaling inhibits dysbiotic Enterobacteriaceae expansion. Science 2017, 357, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Henson, M.A.; Phalak, P. Microbiota dysbiosis in inflammatory bowel diseases: In silico investigation of the oxygen hypothesis. BMC Syst. Biol. 2017, 11, 145. [Google Scholar] [CrossRef] [PubMed]
- Rigottier-Gois, L. Dysbiosis in inflammatory bowel diseases: The oxygen hypothesis. ISME J. 2013, 7, 1256–1261. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Li, Y.R. Oxidative stress and redox signaling mechanisms of inflammatory bowel disease: Updated experimental and clinical evidence. Exp. Biol. Med. 2012, 237, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Sokol, H.; Adolph, T.E. The microbiota: An underestimated actor in radiation-induced lesions? Gut 2018, 67, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Albenberg, L.; Esipova, T.V.; Judge, C.P.; Bittinger, K.; Chen, J.; Laughlin, A.; Grunberg, S.; Baldassano, R.N.; Lewis, J.D.; Li, H.; et al. Correlation between intraluminal oxygen gradient and radial partitioning of intestinal microbiota. Gastroenterology 2014, 147, 1055–1063.e8. [Google Scholar] [CrossRef] [Green Version]
- Hartman, A.L.; Lough, D.M.; Barupal, D.K.; Fiehn, O.; Fishbein, T.; Zasloff, M.; Eisen, J.A. Human gut microbiome adopts an alternative state following small bowel transplantation. Proc. Natl. Acad. Sci. USA 2009, 106, 17187–17192. [Google Scholar] [CrossRef] [Green Version]
- Kelly, C.J.; Zheng, L.; Campbell, E.L.; Saeedi, B.; Scholz, C.C.; Bayless, A.J.; Wilson, K.E.; Glover, L.E.; Kominsky, D.J.; Magnuson, A.; et al. Crosstalk between Microbiota-Derived Short-Chain Fatty Acids and Intestinal Epithelial HIF Augments Tissue Barrier Function. Cell Host Microbe 2015, 17, 662–671. [Google Scholar] [CrossRef] [Green Version]
- Miquel, S.; Leclerc, M.; Martin, R.; Chain, F.; Lenoir, M.; Raguideau, S.; Hudault, S.; Bridonneau, C.; Northen, T.; Bowen, B.; et al. Identification of metabolic signatures linked to anti-inflammatory effects of Faecalibacterium prausnitzii. mBio 2015, 6, e00300-15. [Google Scholar] [CrossRef] [Green Version]
- Veltkamp, C.; Tonkonogy, S.L.; De Jong, Y.P.; Albright, C.; Grenther, W.B.; Balish, E.; Terhorst, C.; Sartor, R.B. Continuous stimulation by normal luminal bacteria is essential for the development and perpetuation of colitis in Tg(epsilon26) mice. Gastroenterology 2001, 120, 900–913. [Google Scholar] [CrossRef]
- Glassner, K.L.; Abraham, B.P.; Quigley, E.M.M. The microbiome and inflammatory bowel disease. J. Allergy Clin. Immunol. 2020, 145, 16–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belkaid, Y.; Hand, T.W. Role of the microbiota in immunity and inflammation. Cell 2014, 157, 121–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamada, N.; Seo, S.U.; Chen, G.Y.; Nunez, G. Role of the gut microbiota in immunity and inflammatory disease. Nat. Rev. Immunol. 2013, 13, 321–335. [Google Scholar] [CrossRef] [PubMed]
- Manichanh, C.; Borruel, N.; Casellas, F.; Guarner, F. The gut microbiota in IBD. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 599–608. [Google Scholar] [CrossRef]
- Wang, M.; Dong, Y.; Wu, J.; Li, H.; Zhang, Y.; Fan, S.; Li, D. Baicalein ameliorates ionizing radiation-induced injuries by rebalancing gut microbiota and inhibiting apoptosis. Life Sci. 2020, 261, 118463. [Google Scholar] [CrossRef]
- Zhao, Z.; Cheng, W.; Qu, W.; Shao, G.; Liu, S. Antibiotic Alleviates Radiation-Induced Intestinal Injury by Remodeling Microbiota, Reducing Inflammation, and Inhibiting Fibrosis. ACS Omega 2020, 5, 2967–2977. [Google Scholar] [CrossRef]
- Matsuoka, K.; Kanai, T. The gut microbiota and inflammatory bowel disease. Semin. Immunopathol. 2015, 37, 47–55. [Google Scholar] [CrossRef] [Green Version]
- Cui, B.; Feng, Q.; Wang, H.; Wang, M.; Peng, Z.; Li, P.; Huang, G.; Liu, Z.; Wu, P.; Fan, Z.; et al. Fecal microbiota transplantation through mid-gut for refractory Crohn’s disease: Safety, feasibility, and efficacy trial results. J. Gastroenterol. Hepatol. 2015, 30, 51–58. [Google Scholar] [CrossRef]
- Ahmed, I.; Roy, B.C.; Khan, S.A.; Septer, S.; Umar, S. Microbiome, Metabolome and Inflammatory Bowel Disease. Microorganisms 2016, 4, 20. [Google Scholar] [CrossRef] [Green Version]
- Fujimoto, T.; Imaeda, H.; Takahashi, K.; Kasumi, E.; Bamba, S.; Fujiyama, Y.; Andoh, A. Decreased abundance of Faecalibacterium prausnitzii in the gut microbiota of Crohn’s disease. J. Gastroenterol. Hepatol. 2013, 28, 613–619. [Google Scholar] [CrossRef]
- Takahashi, K.; Nishida, A.; Fujimoto, T.; Fujii, M.; Shioya, M.; Imaeda, H.; Inatomi, O.; Bamba, S.; Sugimoto, M.; Andoh, A. Reduced Abundance of Butyrate-Producing Bacteria Species in the Fecal Microbial Community in Crohn’s Disease. Digestion 2016, 93, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Varela, E.; Manichanh, C.; Gallart, M.; Torrejon, A.; Borruel, N.; Casellas, F.; Guarner, F.; Antolin, M. Colonisation by Faecalibacterium prausnitzii and maintenance of clinical remission in patients with ulcerative colitis. Aliment. Pharmacol. Ther. 2013, 38, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Mentella, M.C.; Scaldaferri, F.; Pizzoferrato, M.; Gasbarrini, A.; Miggiano, G.A.D. Nutrition, IBD and Gut Microbiota: A Review. Nutrients 2020, 12, 944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frank, D.N.; St Amand, A.L.; Feldman, R.A.; Boedeker, E.C.; Harpaz, N.; Pace, N.R. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc. Natl. Acad. Sci. USA 2007, 104, 13780–13785. [Google Scholar] [CrossRef] [Green Version]
- Sokol, H.; Pigneur, B.; Watterlot, L.; Lakhdari, O.; Bermudez-Humaran, L.G.; Gratadoux, J.J.; Blugeon, S.; Bridonneau, C.; Furet, J.P.; Corthier, G.; et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. USA 2008, 105, 16731–16736. [Google Scholar] [CrossRef] [Green Version]
- Imhann, F.; Vich Vila, A.; Bonder, M.J.; Fu, J.; Gevers, D.; Visschedijk, M.C.; Spekhorst, L.M.; Alberts, R.; Franke, L.; van Dullemen, H.M.; et al. Interplay of host genetics and gut microbiota underlying the onset and clinical presentation of inflammatory bowel disease. Gut 2018, 67, 108–119. [Google Scholar] [CrossRef]
- Ding, X.; Bin, P.; Wu, W.; Chang, Y.; Zhu, G. Tryptophan Metabolism, Regulatory T Cells, and Inflammatory Bowel Disease: A Mini Review. Mediat. Inflamm. 2020, 2020, 9706140. [Google Scholar] [CrossRef]
- Pavel, F.M.; Vesa, C.M.; Gheorghe, G.; Diaconu, C.C.; Stoicescu, M.; Munteanu, M.A.; Babes, E.E.; Tit, D.M.; Toma, M.M.; Bungau, S. Highlighting the Relevance of Gut Microbiota Manipulation in Inflammatory Bowel Disease. Diagnostics 2021, 11, 1090. [Google Scholar] [CrossRef]
- Willing, B.P.; Dicksved, J.; Halfvarson, J.; Andersson, A.F.; Lucio, M.; Zheng, Z.; Jarnerot, G.; Tysk, C.; Jansson, J.K.; Engstrand, L. A pyrosequencing study in twins shows that gastrointestinal microbial profiles vary with inflammatory bowel disease phenotypes. Gastroenterology 2010, 139, 1844–1854.e1. [Google Scholar] [CrossRef]
- Erickson, A.R.; Cantarel, B.L.; Lamendella, R.; Darzi, Y.; Mongodin, E.F.; Pan, C.; Shah, M.; Halfvarson, J.; Tysk, C.; Henrissat, B.; et al. Integrated metagenomics/metaproteomics reveals human host-microbiota signatures of Crohn’s disease. PLoS ONE 2012, 7, e49138. [Google Scholar] [CrossRef] [Green Version]
- Dicksved, J.; Halfvarson, J.; Rosenquist, M.; Jarnerot, G.; Tysk, C.; Apajalahti, J.; Engstrand, L.; Jansson, J.K. Molecular analysis of the gut microbiota of identical twins with Crohn’s disease. ISME J. 2008, 2, 716–727. [Google Scholar] [CrossRef] [PubMed]
- Lepage, P.; Hasler, R.; Spehlmann, M.E.; Rehman, A.; Zvirbliene, A.; Begun, A.; Ott, S.; Kupcinskas, L.; Dore, J.; Raedler, A.; et al. Twin study indicates loss of interaction between microbiota and mucosa of patients with ulcerative colitis. Gastroenterology 2011, 141, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Willing, B.; Halfvarson, J.; Dicksved, J.; Rosenquist, M.; Jarnerot, G.; Engstrand, L.; Tysk, C.; Jansson, J.K. Twin studies reveal specific imbalances in the mucosa-associated microbiota of patients with ileal Crohn’s disease. Inflamm. Bowel Dis. 2009, 15, 653–660. [Google Scholar] [CrossRef]
- Brand, E.C.; Klaassen, M.A.Y.; Gacesa, R.; Vich Vila, A.; Ghosh, H.; De Zoete, M.R.; Boomsma, D.I.; Hoentjen, F.; Horjus Talabur Horje, C.S.; Van De Meeberg, P.C.; et al. Healthy Cotwins Share Gut Microbiome Signatures with Their Inflammatory Bowel Disease Twins and Unrelated Patients. Gastroenterology 2021, 160, 1970–1985. [Google Scholar] [CrossRef] [PubMed]
- Allison, R.R.; Patel, R.M.; McLawhorn, R.A. Radiation oncology: Physics advances that minimize morbidity. Future Oncol. 2014, 10, 2329–2344. [Google Scholar] [CrossRef] [PubMed]
- Barton, M.B.; Jacob, S.; Shafiq, J.; Wong, K.; Thompson, S.R.; Hanna, T.P.; Delaney, G.P. Estimating the demand for radiotherapy from the evidence: A review of changes from 2003 to 2012. Radiother. Oncol. 2014, 112, 140–144. [Google Scholar] [CrossRef]
- Stacey, R.; Green, J.T. Radiation-induced small bowel disease: Latest developments and clinical guidance. Ther. Adv. Chronic Dis. 2014, 5, 15–29. [Google Scholar] [CrossRef] [Green Version]
- Lefevre, J.H.; Amiot, A.; Joly, F.; Bretagnol, F.; Panis, Y. Risk of recurrence after surgery for chronic radiation enteritis. Br. J. Surg. 2011, 98, 1792–1797. [Google Scholar] [CrossRef]
- Stokman, M.A.; Spijkervet, F.K.; Boezen, H.M.; Schouten, J.P.; Roodenburg, J.L.; de Vries, E.G. Preventive intervention possibilities in radiotherapy- and chemotherapy-induced oral mucositis: Results of meta-analyses. J. Dent. Res. 2006, 85, 690–700. [Google Scholar] [CrossRef]
- Villa, A.; Sonis, S.T. Mucositis: Pathobiology and management. Curr. Opin. Oncol. 2015, 27, 159–164. [Google Scholar] [CrossRef]
- Reis Ferreira, M.; Andreyev, H.J.N.; Mohammed, K.; Truelove, L.; Gowan, S.M.; Li, J.; Gulliford, S.L.; Marchesi, J.R.; Dearnaley, D.P. Microbiota- and Radiotherapy-Induced Gastrointestinal Side-Effects (MARS) Study: A Large Pilot Study of the Microbiome in Acute and Late-Radiation Enteropathy. Clin. Cancer Res. 2019, 25, 6487–6500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.; Wang, Q.; Wang, X.; Zhu, L.; Chen, J.; Zhang, B.; Chen, Y.; Yuan, Z. Gut microbial dysbiosis is associated with development and progression of radiation enteritis during pelvic radiotherapy. J. Cell Mol. Med. 2019, 23, 3747–3756. [Google Scholar] [CrossRef] [PubMed]
- Gerassy-Vainberg, S.; Blatt, A.; Danin-Poleg, Y.; Gershovich, K.; Sabo, E.; Nevelsky, A.; Daniel, S.; Dahan, A.; Ziv, O.; Dheer, R.; et al. Radiation induces proinflammatory dysbiosis: Transmission of inflammatory susceptibility by host cytokine induction. Gut 2018, 67, 97–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bennett, K.W.; Eley, A. Fusobacteria: New taxonomy and related diseases. J. Med. Microbiol. 1993, 39, 246–254. [Google Scholar] [CrossRef]
- Cuzzolin, L.; Zambreri, D.; Donini, M.; Griso, C.; Benoni, G. Influence of radiotherapy on intestinal microflora in cancer patients. J. Chemother. 1992, 4, 176–179. [Google Scholar] [CrossRef]
- Sheikh Sajjadieh, M.R.; Kuznetsova, L.V.; Bojenko, V.B. Dysbiosis in ukrainian children with irritable bowel syndrome affected by natural radiation. Iran. J. Pediatr. 2012, 22, 364–368. [Google Scholar]
- Garcia-Peris, P.; Velasco, C.; Lozano, M.A.; Moreno, Y.; Paron, L.; de la Cuerda, C.; Breton, I.; Camblor, M.; Garcia-Hernandez, J.; Guarner, F.; et al. Effect of a mixture of inulin and fructo-oligosaccharide on Lactobacillus and Bifidobacterium intestinal microbiota of patients receiving radiotherapy: A randomised, double-blind, placebo-controlled trial. Nutr. Hosp. 2012, 27, 1908–1915. [Google Scholar] [CrossRef]
- Yamanouchi, K.; Tsujiguchi, T.; Sakamoto, Y.; Ito, K. Short-term follow-up of intestinal flora in radiation-exposed mice. J. Radiat. Res. 2019, 60, 328–332. [Google Scholar] [CrossRef] [Green Version]
- Yi, Y.; Shen, L.; Shi, W.; Xia, F.; Zhang, H.; Wang, Y.; Zhang, J.; Wang, Y.; Sun, X.; Zhang, Z.; et al. Gut Microbiome Components Predict Response to Neoadjuvant Chemoradiotherapy in Patients with Locally Advanced Rectal Cancer: A Prospective, Longitudinal Study. Clin. Cancer Res. 2021, 27, 1329–1340. [Google Scholar] [CrossRef]
- Wang, A.; Ling, Z.; Yang, Z.; Kiela, P.R.; Wang, T.; Wang, C.; Cao, L.; Geng, F.; Shen, M.; Ran, X.; et al. Gut microbial dysbiosis may predict diarrhea and fatigue in patients undergoing pelvic cancer radiotherapy: A pilot study. PLoS ONE 2015, 10, e0126312. [Google Scholar] [CrossRef] [Green Version]
- Sahly, N.; Moustafa, A.; Zaghloul, M.; Salem, T.Z. Effect of radiotherapy on the gut microbiome in pediatric cancer patients: A pilot study. PeerJ 2019, 7, e7683. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, N.; Yamashita, T.; Kishino, S.; Watanabe, H.; Sasaki, K.; Sasaki, D.; Tabata, T.; Sugiyama, Y.; Kitamura, N.; Saito, Y.; et al. A possible beneficial effect of Bacteroides on faecal lipopolysaccharide activity and cardiovascular diseases. Sci. Rep. 2020, 10, 13009. [Google Scholar] [CrossRef] [PubMed]
- Goudarzi, M.; Mak, T.D.; Jacobs, J.P.; Moon, B.H.; Strawn, S.J.; Braun, J.; Brenner, D.J.; Fornace, A.J., Jr.; Li, H.H. An Integrated Multi-Omic Approach to Assess Radiation Injury on the Host-Microbiome Axis. Radiat. Res. 2016, 186, 219–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salyers, A.A. Bacteroides of the human lower intestinal tract. Annu. Rev. Microbiol. 1984, 38, 293–313. [Google Scholar] [CrossRef]
- Wexler, H.M. Bacteroides: The good, the bad, and the nitty-gritty. Clin. Microbiol. Rev. 2007, 20, 593–621. [Google Scholar] [CrossRef] [Green Version]
- Iizumi, T.; Battaglia, T.; Ruiz, V.; Perez Perez, G.I. Gut Microbiome and Antibiotics. Arch. Med. Res. 2017, 48, 727–734. [Google Scholar] [CrossRef]
- Villeger, R.; Lopes, A.; Carrier, G.; Veziant, J.; Billard, E.; Barnich, N.; Gagniere, J.; Vazeille, E.; Bonnet, M. Intestinal Microbiota: A Novel Target to Improve Anti-Tumor Treatment? Int. J. Mol. Sci. 2019, 20, 4584. [Google Scholar] [CrossRef] [Green Version]
- Shkoporov, A.N.; Hill, C. Bacteriophages of the Human Gut: The “Known Unknown” of the Microbiome. Cell Host Microbe 2019, 25, 195–209. [Google Scholar] [CrossRef] [Green Version]
- Gregory, A.C.; Zablocki, O.; Zayed, A.A.; Howell, A.; Bolduc, B.; Sullivan, M.B. The Gut Virome Database Reveals Age-Dependent Patterns of Virome Diversity in the Human Gut. Cell Host Microbe 2020, 28, 724–740.e8. [Google Scholar] [CrossRef]
- Liang, G.; Bushman, F.D. The human virome: Assembly, composition and host interactions. Nat. Rev. Microbiol. 2021, 19, 514–527. [Google Scholar] [CrossRef]
- Mukhopadhya, I.; Segal, J.P.; Carding, S.R.; Hart, A.L.; Hold, G.L. The gut virome: The ‘missing link’ between gut bacteria and host immunity? Therap. Adv. Gastroenterol. 2019, 12, 1756284819836620. [Google Scholar] [CrossRef] [PubMed]
- Lopetuso, L.R.; Ianiro, G.; Scaldaferri, F.; Cammarota, G.; Gasbarrini, A. Gut Virome and Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2016, 22, 1708–1712. [Google Scholar] [CrossRef] [PubMed]
- Lepage, P.; Colombet, J.; Marteau, P.; Sime-Ngando, T.; Dore, J.; Leclerc, M. Dysbiosis in inflammatory bowel disease: A role for bacteriophages? Gut 2008, 57, 424–425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, J.; Maksimovic, J.; Farries, G.; Sim, W.H.; Bishop, R.F.; Cameron, D.J.; Catto-Smith, A.G.; Kirkwood, C.D. Bacteriophages in gut samples from pediatric Crohn’s disease patients: Metagenomic analysis using 454 pyrosequencing. Inflamm. Bowel Dis. 2013, 19, 1598–1608. [Google Scholar] [CrossRef]
- Perez-Brocal, V.; Garcia-Lopez, R.; Nos, P.; Beltran, B.; Moret, I.; Moya, A. Metagenomic Analysis of Crohn’s Disease Patients Identifies Changes in the Virome and Microbiome Related to Disease Status and Therapy, and Detects Potential Interactions and Biomarkers. Inflamm. Bowel Dis. 2015, 21, 2515–2532. [Google Scholar] [CrossRef]
- Wang, W.; Jovel, J.; Halloran, B.; Wine, E.; Patterson, J.; Ford, G.; O’Keefe, S.; Meng, B.; Song, D.; Zhang, Y.; et al. Metagenomic analysis of microbiome in colon tissue from subjects with inflammatory bowel diseases reveals interplay of viruses and bacteria. Inflamm. Bowel Dis. 2015, 21, 1419–1427. [Google Scholar] [CrossRef]
- Norman, J.M.; Handley, S.A.; Baldridge, M.T.; Droit, L.; Liu, C.Y.; Keller, B.C.; Kambal, A.; Monaco, C.L.; Zhao, G.; Fleshner, P.; et al. Disease-specific alterations in the enteric virome in inflammatory bowel disease. Cell 2015, 160, 447–460. [Google Scholar] [CrossRef] [Green Version]
- Zuo, T.; Lu, X.J.; Zhang, Y.; Cheung, C.P.; Lam, S.; Zhang, F.; Tang, W.; Ching, J.Y.L.; Zhao, R.; Chan, P.K.S.; et al. Gut mucosal virome alterations in ulcerative colitis. Gut 2019, 68, 1169–1179. [Google Scholar] [CrossRef] [Green Version]
- Clooney, A.G.; Sutton, T.D.S.; Shkoporov, A.N.; Holohan, R.K.; Daly, K.M.; O’Regan, O.; Ryan, F.J.; Draper, L.A.; Plevy, S.E.; Ross, R.P.; et al. Whole-Virome Analysis Sheds Light on Viral Dark Matter in Inflammatory Bowel Disease. Cell Host Microbe 2019, 26, 764–778.e5. [Google Scholar] [CrossRef]
- Fernandes, M.A.; Verstraete, S.G.; Phan, T.G.; Deng, X.; Stekol, E.; LaMere, B.; Lynch, S.V.; Heyman, M.B.; Delwart, E. Enteric Virome and Bacterial Microbiota in Children with Ulcerative Colitis and Crohn Disease. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 30–36. [Google Scholar] [CrossRef]
- Yan, A.; Butcher, J.; Mack, D.; Stintzi, A. Virome Sequencing of the Human Intestinal Mucosal-Luminal Interface. Front. Cell. Infect. Microbiol. 2020, 10, 582187. [Google Scholar] [CrossRef] [PubMed]
- Liang, G.; Conrad, M.A.; Kelsen, J.R.; Kessler, L.R.; Breton, J.; Albenberg, L.G.; Marakos, S.; Galgano, A.; Devas, N.; Erlichman, J.; et al. Dynamics of the Stool Virome in Very Early-Onset Inflammatory Bowel Disease. J. Crohn’s Colitis 2020, 14, 1600–1610. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Li, X.; Liu, S.; Zhang, Y.; Zhang, D. Toll-like Receptors and Inflammatory Bowel Disease. Front. Immunol. 2018, 9, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, K.H.; Staudt, L.M. Toll-like receptor signaling. Cold Spring Harb. Perspect. Biol. 2013, 5, a011247. [Google Scholar] [CrossRef] [Green Version]
- Abreu, M.T. Toll-like receptor signalling in the intestinal epithelium: How bacterial recognition shapes intestinal function. Nat. Rev. Immunol. 2010, 10, 131–144. [Google Scholar] [CrossRef]
- Cario, E. Toll-like receptors in inflammatory bowel diseases: A decade later. Inflamm. Bowel Dis. 2010, 16, 1583–1597. [Google Scholar] [CrossRef]
- Kamdar, K.; Khakpour, S.; Chen, J.; Leone, V.; Brulc, J.; Mangatu, T.; Antonopoulos, D.A.; Chang, E.B.; Kahn, S.A.; Kirschner, B.S.; et al. Genetic and Metabolic Signals during Acute Enteric Bacterial Infection Alter the Microbiota and Drive Progression to Chronic Inflammatory Disease. Cell Host Microbe 2016, 19, 21–31. [Google Scholar] [CrossRef] [Green Version]
- Toiyama, Y.; Araki, T.; Yoshiyama, S.; Hiro, J.; Miki, C.; Kusunoki, M. The expression patterns of Toll-like receptors in the ileal pouch mucosa of postoperative ulcerative colitis patients. Surg. Today 2006, 36, 287–290. [Google Scholar] [CrossRef]
- Berger, M.; Hsieh, C.Y.; Bakele, M.; Marcos, V.; Rieber, N.; Kormann, M.; Mays, L.; Hofer, L.; Neth, O.; Vitkov, L.; et al. Neutrophils express distinct RNA receptors in a non-canonical way. J. Biol. Chem. 2012, 287, 19409–19417. [Google Scholar] [CrossRef] [Green Version]
- Depaolo, R.W.; Tang, F.; Kim, I.; Han, M.; Levin, N.; Ciletti, N.; Lin, A.; Anderson, D.; Schneewind, O.; Jabri, B. Toll-like receptor 6 drives differentiation of tolerogenic dendritic cells and contributes to LcrV-mediated plague pathogenesis. Cell Host Microbe 2008, 4, 350–361. [Google Scholar] [CrossRef] [Green Version]
- Sugiura, Y.; Kamdar, K.; Khakpour, S.; Young, G.; Karpus, W.J.; DePaolo, R.W. TLR1-induced chemokine production is critical for mucosal immunity against Yersinia enterocolitica. Mucosal Immunol. 2013, 6, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Sainathan, S.K.; Bishnupuri, K.S.; Aden, K.; Luo, Q.; Houchen, C.W.; Anant, S.; Dieckgraefe, B.K. Toll-like receptor-7 ligand Imiquimod induces type I interferon and antimicrobial peptides to ameliorate dextran sodium sulfate-induced acute colitis. Inflamm. Bowel Dis. 2012, 18, 955–967. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKernan, D.P.; Finn, D.P. An apPEAling new therapeutic for ulcerative colitis? Gut 2014, 63, 1207–1208. [Google Scholar] [CrossRef] [PubMed]
- Junker, Y.; Zeissig, S.; Kim, S.J.; Barisani, D.; Wieser, H.; Leffler, D.A.; Zevallos, V.; Libermann, T.A.; Dillon, S.; Freitag, T.L.; et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J. Exp. Med. 2012, 209, 2395–2408. [Google Scholar] [CrossRef]
- Zevallos, V.F.; Raker, V.; Tenzer, S.; Jimenez-Calvente, C.; Ashfaq-Khan, M.; Russel, N.; Pickert, G.; Schild, H.; Steinbrink, K.; Schuppan, D. Nutritional Wheat Amylase-Trypsin Inhibitors Promote Intestinal Inflammation via Activation of Myeloid Cells. Gastroenterology 2017, 152, 1100–1113.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, D.L.; Montero, M.; Ropeleski, M.J.; Bergstrom, K.S.; Ma, C.; Ghosh, S.; Merkens, H.; Huang, J.; Mansson, L.E.; Sham, H.P.; et al. Interleukin-11 reduces TLR4-induced colitis in TLR2-deficient mice and restores intestinal STAT3 signaling. Gastroenterology 2010, 139, 1277–1288. [Google Scholar] [CrossRef]
- Chassaing, B.; Ley, R.E.; Gewirtz, A.T. Intestinal epithelial cell toll-like receptor 5 regulates the intestinal microbiota to prevent low-grade inflammation and metabolic syndrome in mice. Gastroenterology 2014, 147, 1363–1377.e7. [Google Scholar] [CrossRef] [Green Version]
- Saruta, M.; Targan, S.R.; Mei, L.; Ippoliti, A.F.; Taylor, K.D.; Rotter, J.I. High-frequency haplotypes in the X chromosome locus TLR8 are associated with both CD and UC in females. Inflamm. Bowel Dis. 2009, 15, 321–327. [Google Scholar] [CrossRef]
- Obermeier, F.; Dunger, N.; Strauch, U.G.; Hofmann, C.; Bleich, A.; Grunwald, N.; Hedrich, H.J.; Aschenbrenner, E.; Schlegelberger, B.; Rogler, G.; et al. CpG motifs of bacterial DNA essentially contribute to the perpetuation of chronic intestinal inflammation. Gastroenterology 2005, 129, 913–927. [Google Scholar] [CrossRef]
- Weber, A.; Wasiliew, P.; Kracht, M. Interleukin-1 (IL-1) pathway. Sci. Signal. 2010, 3, cm1. [Google Scholar] [CrossRef]
- Atreya, R.; Bloom, S.; Scaldaferri, F.; Gerardi, V.; Admyre, C.; Karlsson, A.; Knittel, T.; Kowalski, J.; Lukas, M.; Lofberg, R.; et al. Clinical Effects of a Topically Applied Toll-like Receptor 9 Agonist in Active Moderate-to-Severe Ulcerative Colitis. J. Crohn’s Colitis 2016, 10, 1294–1302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burdelya, L.G.; Krivokrysenko, V.I.; Tallant, T.C.; Strom, E.; Gleiberman, A.S.; Gupta, D.; Kurnasov, O.V.; Fort, F.L.; Osterman, A.L.; Didonato, J.A.; et al. An agonist of toll-like receptor 5 has radioprotective activity in mouse and primate models. Science 2008, 320, 226–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saha, S.; Bhanja, P.; Liu, L.; Alfieri, A.A.; Yu, D.; Kandimalla, E.R.; Agrawal, S.; Guha, C. TLR9 agonist protects mice from radiation-induced gastrointestinal syndrome. PLoS ONE 2012, 7, e29357. [Google Scholar] [CrossRef] [PubMed]
- Riehl, T.; Cohn, S.; Tessner, T.; Schloemann, S.; Stenson, W.F. Lipopolysaccharide is radioprotective in the mouse intestine through a prostaglandin-mediated mechanism. Gastroenterology 2000, 118, 1106–1116. [Google Scholar] [CrossRef]
- Riehl, T.E.; Newberry, R.D.; Lorenz, R.G.; Stenson, W.F. TNFR1 mediates the radioprotective effects of lipopolysaccharide in the mouse intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 2004, 286, G166–G173. [Google Scholar] [CrossRef]
- van Vliet, M.J.; Harmsen, H.J.; de Bont, E.S.; Tissing, W.J. The role of intestinal microbiota in the development and severity of chemotherapy-induced mucositis. PLoS Pathog. 2010, 6, e1000879. [Google Scholar] [CrossRef] [Green Version]
- Egan, L.J.; Eckmann, L.; Greten, F.R.; Chae, S.; Li, Z.W.; Myhre, G.M.; Robine, S.; Karin, M.; Kagnoff, M.F. IkappaB-kinasebeta-dependent NF-kappaB activation provides radioprotection to the intestinal epithelium. Proc. Natl. Acad. Sci. USA 2004, 101, 2452–2457. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Liu, C.; Yue, J. Radiotherapy and the gut microbiome: Facts and fiction. Radiat. Oncol. 2021, 16, 9. [Google Scholar] [CrossRef]
- Banerjee, S.; Fu, Q.; Shah, S.K.; Ponnappan, U.; Melnyk, S.B.; Hauer-Jensen, M.; Pawar, S.A. Role of TLR4 in the Pathogenesis of Radiation-Induced Ibtestinal Injury in C/EBP Delta-Knockout Mice. Shock 2017, 47, 84. [Google Scholar]
- McLaughlin, M.M.; Dacquisto, M.P.; Jacobus, D.P.; Horowitz, R.E. Effects of the Germfree State on Responses of Mice to Whole-Body Irradiation. Radiat. Res. 1964, 23, 333–349. [Google Scholar] [CrossRef]
- Crawford, P.A.; Gordon, J.I. Microbial regulation of intestinal radiosensitivity. Proc. Natl. Acad. Sci. USA 2005, 102, 13254–13259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regueiro, M.; Velayos, F.; Greer, J.B.; Bougatsos, C.; Chou, R.; Sultan, S.; Singh, S. American Gastroenterological Association Institute Technical Review on the Management of Crohn’s Disease after Surgical Resection. Gastroenterology 2017, 152, 277–295.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santavirta, J.; Mattila, J.; Kokki, M.; Matikainen, M. Mucosal morphology and faecal bacteriology after ileoanal anastomosis. Int. J. Colorectal Dis. 1991, 6, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Nerstedt, A.; Nilsson, E.C.; Ohlson, K.; Hakansson, J.; Thomas Svensson, L.; Lowenadler, B.; Svensson, U.K.; Mahlapuu, M. Administration of Lactobacillus evokes coordinated changes in the intestinal expression profile of genes regulating energy homeostasis and immune phenotype in mice. Br. J. Nutr. 2007, 97, 1117–1127. [Google Scholar] [CrossRef] [Green Version]
- Tomasik, P.J.; Tomasik, P. Probiotics and Prebiotics. Cereal Chem. 2003, 80, 113–117. [Google Scholar] [CrossRef]
- Delzenne, N.M. Oligosaccharides: State of the art. Proc. Nutr. Soc. 2003, 62, 177–182. [Google Scholar] [CrossRef]
- Sartor, R.B. Therapeutic manipulation of the enteric microflora in inflammatory bowel diseases: Antibiotics, probiotics, and prebiotics. Gastroenterology 2004, 126, 1620–1633. [Google Scholar] [CrossRef] [Green Version]
- Guslandi, M.; Mezzi, G.; Sorghi, M.; Testoni, P.A. Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Dig. Dis. Sci. 2000, 45, 1462–1464. [Google Scholar] [CrossRef]
- Generoso, S.V.; Viana, M.L.; Santos, R.G.; Arantes, R.M.; Martins, F.S.; Nicoli, J.R.; Machado, J.A.; Correia, M.I.; Cardoso, V.N. Protection against increased intestinal permeability and bacterial translocation induced by intestinal obstruction in mice treated with viable and heat-killed Saccharomyces boulardii. Eur. J. Nutr. 2011, 50, 261–269. [Google Scholar] [CrossRef]
- Steed, H.; Macfarlane, G.T.; Blackett, K.L.; Bahrami, B.; Reynolds, N.; Walsh, S.V.; Cummings, J.H.; Macfarlane, S. Clinical trial: The microbiological and immunological effects of synbiotic consumption—A randomized double-blind placebo-controlled study in active Crohn’s disease. Aliment. Pharmacol. Ther. 2010, 32, 872–883. [Google Scholar] [CrossRef]
- Fedorak, R.N.; Feagan, B.G.; Hotte, N.; Leddin, D.; Dieleman, L.A.; Petrunia, D.M.; Enns, R.; Bitton, A.; Chiba, N.; Pare, P.; et al. The probiotic VSL#3 has anti-inflammatory effects and could reduce endoscopic recurrence after surgery for Crohn’s disease. Clin. Gastroenterol. Hepatol. 2015, 13, 928–935.e2. [Google Scholar] [CrossRef] [PubMed]
- Mallon, P.; McKay, D.; Kirk, S.; Gardiner, K. Probiotics for induction of remission in ulcerative colitis. Cochrane Database Syst. Rev. 2007, 3, CD005573. [Google Scholar] [CrossRef]
- Sood, A.; Midha, V.; Makharia, G.K.; Ahuja, V.; Singal, D.; Goswami, P.; Tandon, R.K. The probiotic preparation, VSL#3 induces remission in patients with mild-to-moderately active ulcerative colitis. Clin. Gastroenterol. Hepatol. 2009, 7, 1202–1209.e1. [Google Scholar] [CrossRef] [PubMed]
- Miele, E.; Pascarella, F.; Giannetti, E.; Quaglietta, L.; Baldassano, R.N.; Staiano, A. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am. J. Gastroenterol. 2009, 104, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Huynh, H.Q.; deBruyn, J.; Guan, L.; Diaz, H.; Li, M.; Girgis, S.; Turner, J.; Fedorak, R.; Madsen, K. Probiotic preparation VSL#3 induces remission in children with mild to moderate acute ulcerative colitis: A pilot study. Inflamm. Bowel Dis. 2009, 15, 760–768. [Google Scholar] [CrossRef]
- Kato, K.; Mizuno, S.; Umesaki, Y.; Ishii, Y.; Sugitani, M.; Imaoka, A.; Otsuka, M.; Hasunuma, O.; Kurihara, R.; Iwasaki, A.; et al. Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment. Pharmacol. Ther. 2004, 20, 1133–1141. [Google Scholar] [CrossRef]
- Shanahan, F.; Collins, S.M. Pharmabiotic manipulation of the microbiota in gastrointestinal disorders, from rationale to reality. Gastroenterol. Clin. N. Am. 2010, 39, 721–726. [Google Scholar] [CrossRef]
- Kruis, W.; Schutz, E.; Fric, P.; Fixa, B.; Judmaier, G.; Stolte, M. Double-blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Aliment. Pharmacol. Ther. 1997, 11, 853–858. [Google Scholar] [CrossRef]
- Rembacken, B.J.; Snelling, A.M.; Hawkey, P.M.; Chalmers, D.M.; Axon, A.T. Non-pathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: A randomised trial. Lancet 1999, 354, 635–639. [Google Scholar] [CrossRef]
- Kruis, W.; Fric, P.; Pokrotnieks, J.; Lukas, M.; Fixa, B.; Kascak, M.; Kamm, M.A.; Weismueller, J.; Beglinger, C.; Stolte, M.; et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 2004, 53, 1617–1623. [Google Scholar] [CrossRef]
- Guslandi, M. Saccharomyces boulardii plus rifaximin in mesalamine-intolerant ulcerative colitis. J. Clin. Gastroenterol. 2010, 44, 385. [Google Scholar] [CrossRef] [PubMed]
- Colombel, J.F.; D’Haens, G.; Lee, W.J.; Petersson, J.; Panaccione, R. Outcomes and Strategies to Support a Treat-to-target Approach in Inflammatory Bowel Disease: A Systematic Review. J. Crohn’s Colitis 2020, 14, 254–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, G.R.; Roberfroid, M.B. Dietary modulation of the human colonic microbiota: Introducing the concept of prebiotics. J. Nutr. 1995, 125, 1401–1412. [Google Scholar] [CrossRef] [PubMed]
- Gibson, G.R.; Hutkins, R.; Sanders, M.E.; Prescott, S.L.; Reimer, R.A.; Salminen, S.J.; Scott, K.; Stanton, C.; Swanson, K.S.; Cani, P.D.; et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 491–502. [Google Scholar] [CrossRef] [Green Version]
- Aggeletopoulou, I.; Konstantakis, C.; Assimakopoulos, S.F.; Triantos, C. The role of the gut microbiota in the treatment of inflammatory bowel diseases. Microb. Pathog. 2019, 137, 103774. [Google Scholar] [CrossRef]
- Laurell, A.; Sjoberg, K. Prebiotics and synbiotics in ulcerative colitis. Scand. J. Gastroenterol. 2017, 52, 477–485. [Google Scholar] [CrossRef]
- Valcheva, R.; Koleva, P.; Martinez, I.; Walter, J.; Ganzle, M.G.; Dieleman, L.A. Inulin-type fructans improve active ulcerative colitis associated with microbiota changes and increased short-chain fatty acids levels. Gut Microbes 2019, 10, 334–357. [Google Scholar] [CrossRef]
- Cai, Y.; Liu, W.; Lin, Y.; Zhang, S.; Zou, B.; Xiao, D.; Lin, L.; Zhong, Y.; Zheng, H.; Liao, Q.; et al. Compound polysaccharides ameliorate experimental colitis by modulating gut microbiota composition and function. J. Gastroenterol. Hepatol. 2019, 34, 1554–1562. [Google Scholar] [CrossRef]
- Ferenczi, S.; Szegi, K.; Winkler, Z.; Barna, T.; Kovacs, K.J. Oligomannan Prebiotic Attenuates Immunological, Clinical and Behavioral Symptoms in Mouse Model of Inflammatory Bowel Disease. Sci. Rep. 2016, 6, 34132. [Google Scholar] [CrossRef]
- Hedin, C.R.; Mullard, M.; Sharratt, E.; Jansen, C.; Sanderson, J.D.; Shirlaw, P.; Howe, L.C.; Djemal, S.; Stagg, A.J.; Lindsay, J.O.; et al. Probiotic and prebiotic use in patients with inflammatory bowel disease: A case-control study. Inflamm. Bowel Dis. 2010, 16, 2099–2108. [Google Scholar] [CrossRef]
- Koleva, P.T.; Valcheva, R.S.; Sun, X.; Ganzle, M.G.; Dieleman, L.A. Inulin and fructo-oligosaccharides have divergent effects on colitis and commensal microbiota in HLA-B27 transgenic rats. Br. J. Nutr. 2012, 108, 1633–1643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rufino, M.N.; Aleixo, G.F.P.; Trombine-Batista, I.E.; Giuffrida, R.; Keller, R.; Bremer-Neto, H. Systematic review and meta-analysis of preclinical trials demonstrate robust beneficial effects of prebiotics in induced inflammatory bowel disease. J. Nutr. Biochem. 2018, 62, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, F.; Quigley, E.M. Manipulation of the microbiota for treatment of IBS and IBD-challenges and controversies. Gastroenterology 2014, 146, 1554–1563. [Google Scholar] [CrossRef] [PubMed]
- Damaskos, D.; Kolios, G. Probiotics and prebiotics in inflammatory bowel disease: Microflora ‘on the scope’. Br. J. Clin. Pharmacol. 2008, 65, 453–467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olveira, G.; Gonzalez-Molero, I. An update on probiotics, prebiotics and symbiotics in clinical nutrition. Endocrinol. Nutr. 2016, 63, 482–494. [Google Scholar] [CrossRef]
- Pandey, K.R.; Naik, S.R.; Vakil, B.V. Probiotics, prebiotics and synbiotics—A review. J. Food Sci. Technol. 2015, 52, 7577–7587. [Google Scholar] [CrossRef]
- Furrie, E.; Macfarlane, S.; Kennedy, A.; Cummings, J.H.; Walsh, S.V.; O’Neil D, A.; Macfarlane, G.T. Synbiotic therapy (Bifidobacterium longum/Synergy 1) initiates resolution of inflammation in patients with active ulcerative colitis: A randomised controlled pilot trial. Gut 2005, 54, 242–249. [Google Scholar] [CrossRef]
- Hansen, R.; Mahdi, G.; McIntyre, K.; Macfarlane, G.T.; Macfarlane, S.; Wilson, D.C. Synbiotics for inflammatory bowel disease: Useful in adults but problematic in paediatrics. Arch. Dis. Child. 2011, 96, A18–A19. [Google Scholar] [CrossRef] [Green Version]
- Chermesh, I.; Tamir, A.; Reshef, R.; Chowers, Y.; Suissa, A.; Katz, D.; Gelber, M.; Halpern, Z.; Bengmark, S.; Eliakim, R. Failure of Synbiotic 2000 to prevent postoperative recurrence of Crohn’s disease. Dig. Dis. Sci. 2007, 52, 385–389. [Google Scholar] [CrossRef]
- Akutko, K.; Stawarski, A. Probiotics, Prebiotics and Synbiotics in Inflammatory Bowel Diseases. J. Clin. Med. 2021, 10, 2466. [Google Scholar] [CrossRef]
- Borody, T.J.; Clancy, A. Fecal microbiota transplantation for ulcerative colitis-where to from here? Transl. Gastroenterol. Hepatol. 2019, 4, 48. [Google Scholar] [CrossRef]
- Moayyedi, P.; Surette, M.G.; Kim, P.T.; Libertucci, J.; Wolfe, M.; Onischi, C.; Armstrong, D.; Marshall, J.K.; Kassam, Z.; Reinisch, W.; et al. Fecal Microbiota Transplantation Induces Remission in Patients with Active Ulcerative Colitis in a Randomized Controlled Trial. Gastroenterology 2015, 149, 102–109.e6. [Google Scholar] [CrossRef] [Green Version]
- Paramsothy, S.; Kamm, M.A.; Kaakoush, N.O.; Walsh, A.J.; van den Bogaerde, J.; Samuel, D.; Leong, R.W.L.; Connor, S.; Ng, W.; Paramsothy, R.; et al. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: A randomised placebo-controlled trial. Lancet 2017, 389, 1218–1228. [Google Scholar] [CrossRef]
- Sood, A.; Singh, A.; Midha, V.; Mahajan, R.; Kao, D.; Rubin, D.T.; Bernstein, C.N. Fecal Microbiota Transplantation for Ulcerative Colitis: An Evolving Therapy. Crohn’s Colitis 360 2020, 2, otaa067. [Google Scholar] [CrossRef]
- Lai, C.Y.; Sung, J.; Cheng, F.; Tang, W.; Wong, S.H.; Chan, P.K.S.; Kamm, M.A.; Sung, J.J.Y.; Kaplan, G.; Chan, F.K.L.; et al. Systematic review with meta-analysis: Review of donor features, procedures and outcomes in 168 clinical studies of faecal microbiota transplantation. Aliment. Pharmacol. Ther. 2019, 49, 354–363. [Google Scholar] [CrossRef]
- Fang, H.; Fu, L.; Wang, J. Protocol for Fecal Microbiota Transplantation in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Biomed Res. Int. 2018, 2018, 8941340. [Google Scholar] [CrossRef] [Green Version]
- Qazi, T.; Amaratunga, T.; Barnes, E.L.; Fischer, M.; Kassam, Z.; Allegretti, J.R. The risk of inflammatory bowel disease flares after fecal microbiota transplantation: Systematic review and meta-analysis. Gut Microbes 2017, 8, 574–588. [Google Scholar] [CrossRef] [Green Version]
- Scott, K.P.; Antoine, J.M.; Midtvedt, T.; van Hemert, S. Manipulating the gut microbiota to maintain health and treat disease. Microb. Ecol. Health Dis. 2015, 26, 25877. [Google Scholar] [CrossRef]
- Nitzan, O.; Elias, M.; Peretz, A.; Saliba, W. Role of antibiotics for treatment of inflammatory bowel disease. World J. Gastroenterol. 2016, 22, 1078–1087. [Google Scholar] [CrossRef]
- Khan, K.J.; Ullman, T.A.; Ford, A.C.; Abreu, M.T.; Abadir, A.; Marshall, J.K.; Talley, N.J.; Moayyedi, P. Antibiotic therapy in inflammatory bowel disease: A systematic review and meta-analysis. Am. J. Gastroenterol. 2011, 106, 661–673. [Google Scholar] [CrossRef]
- Wang, S.L.; Wang, Z.R.; Yang, C.Q. Meta-analysis of broad-spectrum antibiotic therapy in patients with active inflammatory bowel disease. Exp. Ther. Med. 2012, 4, 1051–1056. [Google Scholar] [CrossRef] [Green Version]
- Su, J.W.; Ma, J.J.; Zhang, H.J. Use of antibiotics in patients with Crohn’s disease: A systematic review and meta-analysis. J. Dig. Dis. 2015, 16, 58–66. [Google Scholar] [CrossRef]
- Arnold, G.L.; Beaves, M.R.; Pryjdun, V.O.; Mook, W.J. Preliminary study of ciprofloxacin in active Crohn’s disease. Inflamm. Bowel Dis. 2002, 8, 10–15. [Google Scholar] [CrossRef]
- Steinhart, A.H.; Feagan, B.G.; Wong, C.J.; Vandervoort, M.; Mikolainis, S.; Croitoru, K.; Seidman, E.; Leddin, D.J.; Bitton, A.; Drouin, E.; et al. Combined budesonide and antibiotic therapy for active Crohn’s disease: A randomized controlled trial. Gastroenterology 2002, 123, 33–40. [Google Scholar] [CrossRef]
- Sutherland, L.; Singleton, J.; Sessions, J.; Hanauer, S.; Krawitt, E.; Rankin, G.; Summers, R.; Mekhjian, H.; Greenberger, N.; Kelly, M.; et al. Double blind, placebo controlled trial of metronidazole in Crohn’s disease. Gut 1991, 32, 1071–1075. [Google Scholar] [CrossRef] [Green Version]
- Prantera, C.; Zannoni, F.; Scribano, M.L.; Berto, E.; Andreoli, A.; Kohn, A.; Luzi, C. An antibiotic regimen for the treatment of active Crohn’s disease: A randomized, controlled clinical trial of metronidazole plus ciprofloxacin. Am. J. Gastroenterol. 1996, 91, 328–332. [Google Scholar]
- Jigaranu, A.O.; Nedelciuc, O.; Blaj, A.; Badea, M.; Mihai, C.; Diculescu, M.; Cijevschi-Prelipcean, C. Is rifaximin effective in maintaining remission in Crohn’s disease? Dig. Dis. 2014, 32, 378–383. [Google Scholar] [CrossRef]
- Chapman, R.W.; Selby, W.S.; Jewell, D.P. Controlled trial of intravenous metronidazole as an adjunct to corticosteroids in severe ulcerative colitis. Gut 1986, 27, 1210–1212. [Google Scholar] [CrossRef] [Green Version]
- Gilat, T.; Suissa, A.; Leichtman, G.; Delpre, G.; Pavlotzky, M.; Grossman, A.; Fireman, Z. A comparative study of metronidazole and sulfasalazine in active, not severe, ulcerative colitis. An Israeli multicenter trial. J. Clin. Gastroenterol. 1987, 9, 415–417. [Google Scholar] [CrossRef]
- Mantzaris, G.J.; Archavlis, E.; Christoforidis, P.; Kourtessas, D.; Amberiadis, P.; Florakis, N.; Petraki, K.; Spiliadi, C.; Triantafyllou, G. A prospective randomized controlled trial of oral ciprofloxacin in acute ulcerative colitis. Am. J. Gastroenterol. 1997, 92, 454–456. [Google Scholar]
- Husserl, E. Logical Investigations, Volumes One and Two; Findlay, J.N., Ed.; With translation corrections and with a new Introduction by Dermot Moran; With a new Preface by Michael Dummett; A new and revised edition of the original English translation by J. N. Findlay; Routledge & Kegan Paul: London, UK, 1970. [Google Scholar]
- Burke, D.A.; Axon, A.T.; Clayden, S.A.; Dixon, M.F.; Johnston, D.; Lacey, R.W. The efficacy of tobramycin in the treatment of ulcerative colitis. Aliment. Pharmacol. Ther. 1990, 4, 123–129. [Google Scholar] [CrossRef]
- Mantzaris, G.J.; Hatzis, A.; Kontogiannis, P.; Triadaphyllou, G. Intravenous tobramycin and metronidazole as an adjunct to corticosteroids in acute, severe ulcerative colitis. Am. J. Gastroenterol. 1994, 89, 43–46. [Google Scholar] [PubMed]
- Turunen, U.M.; Farkkila, M.A.; Hakala, K.; Seppala, K.; Sivonen, A.; Ogren, M.; Vuoristo, M.; Valtonen, V.V.; Miettinen, T.A. Long-term treatment of ulcerative colitis with ciprofloxacin: A prospective, double-blind, placebo-controlled study. Gastroenterology 1998, 115, 1072–1078. [Google Scholar] [CrossRef]
- Petersen, A.M.; Mirsepasi, H.; Halkjaer, S.I.; Mortensen, E.M.; Nordgaard-Lassen, I.; Krogfelt, K.A. Ciprofloxacin and probiotic Escherichia coli Nissle add-on treatment in active ulcerative colitis: A double-blind randomized placebo controlled clinical trial. J. Crohn’s Colitis 2014, 8, 1498–1505. [Google Scholar] [CrossRef]
- Gionchetti, P.; Rizzello, F.; Ferrieri, A.; Venturi, A.; Brignola, C.; Ferretti, M.; Peruzzo, S.; Miglioli, M.; Campieri, M. Rifaximin in patients with moderate or severe ulcerative colitis refractory to steroid-treatment: A double-blind, placebo-controlled trial. Dig. Dis. Sci. 1999, 44, 1220–1221. [Google Scholar] [CrossRef]
- Limketkai, B.N.; Wolf, A.; Parian, A.M. Nutritional Interventions in the Patient with Inflammatory Bowel Disease. Gastroenterol Clin. N. Am. 2018, 47, 155–177. [Google Scholar] [CrossRef]
- Knight-Sepulveda, K.; Kais, S.; Santaolalla, R.; Abreu, M.T. Diet and Inflammatory Bowel Disease. Gastroenterol. Hepatol. 2015, 11, 511–520. [Google Scholar]
- Weber, A.T.; Shah, N.D.; Sauk, J.; Limketkai, B.N. Popular Diet Trends for Inflammatory Bowel Diseases: Claims and Evidence. Curr. Treat. Options Gastroenterol. 2019, 17, 564–576. [Google Scholar] [CrossRef]
- Kakodkar, S.; Farooqui, A.J.; Mikolaitis, S.L.; Mutlu, E.A. The Specific Carbohydrate Diet for Inflammatory Bowel Disease: A Case Series. J. Acad. Nutr. Diet. 2015, 115, 1226–1232. [Google Scholar] [CrossRef] [Green Version]
- Suskind, D.L.; Wahbeh, G.; Cohen, S.A.; Damman, C.J.; Klein, J.; Braly, K.; Shaffer, M.; Lee, D. Patients Perceive Clinical Benefit with the Specific Carbohydrate Diet for Inflammatory Bowel Disease. Dig. Dis. Sci. 2016, 61, 3255–3260. [Google Scholar] [CrossRef]
- Kamal, A.; Pimentel, M. Influence of Dietary Restriction on Irritable Bowel Syndrome. Am. J. Gastroenterol. 2019, 114, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, N.; Ankersen, D.V.; Felding, M.; Wachmann, H.; Vegh, Z.; Molzen, L.; Burisch, J.; Andersen, J.R.; Munkholm, P. Low-FODMAP diet reduces irritable bowel symptoms in patients with inflammatory bowel disease. World J. Gastroenterol. 2017, 23, 3356–3366. [Google Scholar] [CrossRef] [PubMed]
- Bodini, G.; Zanella, C.; Crespi, M.; Lo Pumo, S.; Demarzo, M.G.; Savarino, E.; Savarino, V.; Giannini, E.G. A randomized, 6-wk trial of a low FODMAP diet in patients with inflammatory bowel disease. Nutrition 2019, 67–68, 110542. [Google Scholar] [CrossRef]
- Herfarth, H.H.; Martin, C.F.; Sandler, R.S.; Kappelman, M.D.; Long, M.D. Prevalence of a gluten-free diet and improvement of clinical symptoms in patients with inflammatory bowel diseases. Inflamm. Bowel Dis. 2014, 20, 1194–1197. [Google Scholar] [CrossRef] [PubMed]
- Schreiner, P.; Yilmaz, B.; Rossel, J.B.; Franc, Y.; Misselwitz, B.; Scharl, M.; Zeitz, J.; Frei, P.; Greuter, T.; Vavricka, S.R.; et al. Vegetarian or gluten-free diets in patients with inflammatory bowel disease are associated with lower psychological well-being and a different gut microbiota, but no beneficial effects on the course of the disease. United Eur. Gastroenterol. J. 2019, 7, 767–781. [Google Scholar] [CrossRef] [Green Version]
- Olendzki, B.C.; Silverstein, T.D.; Persuitte, G.M.; Ma, Y.; Baldwin, K.R.; Cave, D. An anti-inflammatory diet as treatment for inflammatory bowel disease: A case series report. Nutr. J. 2014, 13, 5. [Google Scholar] [CrossRef] [Green Version]
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.I.; Di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2016, 65, 1812–1821. [Google Scholar] [CrossRef]
- Marlow, G.; Ellett, S.; Ferguson, I.R.; Zhu, S.; Karunasinghe, N.; Jesuthasan, A.C.; Han, D.Y.; Fraser, A.G.; Ferguson, L.R. Transcriptomics to study the effect of a Mediterranean-inspired diet on inflammation in Crohn’s disease patients. Hum. Genomics 2013, 7, 24. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, T.S.; Koefoed, A.K.; Jakobsen, R.R.; Deng, L.; Castro-Mejia, J.L.; Brunse, A.; Neve, H.; Vogensen, F.K.; Nielsen, D.S. Bacteriophage-mediated manipulation of the gut microbiome—Promises and presents limitations. FEMS Microbiol. Rev. 2020, 44, 507–521. [Google Scholar] [CrossRef]
- Ott, S.J.; Waetzig, G.H.; Rehman, A.; Moltzau-Anderson, J.; Bharti, R.; Grasis, J.A.; Cassidy, L.; Tholey, A.; Fickenscher, H.; Seegert, D.; et al. Efficacy of Sterile Fecal Filtrate Transfer for Treating Patients with Clostridium difficile Infection. Gastroenterology 2017, 152, 799–811.e7. [Google Scholar] [CrossRef] [Green Version]
- Kao, D.H.; Roach, B.; Walter, J.; Lobenberg, R.; Wong, K. A51 Effect of lyophilized sterile fecal filtrate vs lyophilized donor stool on recurrent clostridium difficile infection (RCDI): Preliminary results from a randomized, double-blind pilot study. J. Can. Assoc. Gastroenterol. 2019, 2, 101–102. [Google Scholar] [CrossRef]
- Draper, L.A.; Ryan, F.J.; Dalmasso, M.; Casey, P.G.; McCann, A.; Velayudhan, V.; Ross, R.P.; Hill, C. Autochthonous faecal viral transfer (FVT) impacts the murine microbiome after antibiotic perturbation. BMC Biol. 2020, 18, 173. [Google Scholar] [CrossRef] [PubMed]
- Brunse, A.; Deng, L.; Pan, X.; Hui, Y.; Castro-Mejia, J.L.; Kot, W.; Nguyen, D.N.; Secher, J.B.; Nielsen, D.S.; Thymann, T. Fecal filtrate transplantation protects against necrotizing enterocolitis. ISME J. 2022, 16, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Sugimura, N.; Burgermeister, E.; Ebert, M.P.; Zuo, T.; Lan, P. The gut virome: A new microbiome component in health and disease. EBioMedicine 2022, 81, 104113. [Google Scholar] [CrossRef] [PubMed]
- Gordillo Altamirano, F.L.; Barr, J.J. Phage Therapy in the Postantibiotic Era. Clin. Microbiol. Rev. 2019, 32, e00066-18. [Google Scholar] [CrossRef] [Green Version]
- Rehman, S.; Ali, Z.; Khan, M.; Bostan, N.; Naseem, S. The dawn of phage therapy. Rev. Med. Virol. 2019, 29, e2041. [Google Scholar] [CrossRef]
- Lamps, L.W.; Madhusudhan, K.T.; Havens, J.M.; Greenson, J.K.; Bronner, M.P.; Chiles, M.C.; Dean, P.J.; Scott, M.A. Pathogenic Yersinia DNA is detected in bowel and mesenteric lymph nodes from patients with Crohn’s disease. Am. J. Surg. Pathol. 2003, 27, 220–227. [Google Scholar] [CrossRef]
- Sartor, R.B.; Wu, G.D. Roles for Intestinal Bacteria, Viruses, and Fungi in Pathogenesis of Inflammatory Bowel Diseases and Therapeutic Approaches. Gastroenterology 2017, 152, 327–339.e4. [Google Scholar] [CrossRef] [Green Version]
- Palmela, C.; Chevarin, C.; Xu, Z.; Torres, J.; Sevrin, G.; Hirten, R.; Barnich, N.; Ng, S.C.; Colombel, J.F. Adherent-invasive Escherichia coli in inflammatory bowel disease. Gut 2018, 67, 574–587. [Google Scholar] [CrossRef]
- Chervy, M.; Barnich, N.; Denizot, J. Adherent-Invasive E. coli: Update on the Lifestyle of a Troublemaker in Crohn’s Disease. Int. J. Mol. Sci. 2020, 21, 3734. [Google Scholar] [CrossRef]
- Galtier, M.; De Sordi, L.; Sivignon, A.; de Vallee, A.; Maura, D.; Neut, C.; Rahmouni, O.; Wannerberger, K.; Darfeuille-Michaud, A.; Desreumaux, P.; et al. Bacteriophages Targeting Adherent Invasive Escherichia coli Strains as a Promising New Treatment for Crohn’s Disease. J. Crohn’s Colitis 2017, 11, 840–847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vahedi, A.; Soltan Dallal, M.M.; Douraghi, M.; Nikkhahi, F.; Rajabi, Z.; Yousefi, M.; Mousavi, M. Isolation and identification of specific bacteriophage against enteropathogenic Escherichia coli (EPEC) and in vitro and in vivo characterization of bacteriophage. FEMS Microbiol. Lett. 2018, 365, fny136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, L.; Wang, S.; Guo, Z.; Liu, H.; Sun, D.; Yan, G.; Hu, D.; Du, C.; Feng, X.; Han, W.; et al. A guard-killer phage cocktail effectively lyses the host and inhibits the development of phage-resistant strains of Escherichia coli. Appl. Microbiol. Biotechnol. 2018, 102, 971–983. [Google Scholar] [CrossRef] [PubMed]
- Febvre, H.P.; Rao, S.; Gindin, M.; Goodwin, N.D.M.; Finer, E.; Vivanco, J.S.; Lu, S.; Manter, D.K.; Wallace, T.C.; Weir, T.L. PHAGE Study: Effects of Supplemental Bacteriophage Intake on Inflammation and Gut Microbiota in Healthy Adults. Nutrients 2019, 11, 666. [Google Scholar] [CrossRef] [Green Version]
- Francois, A.; Milliat, F.; Guipaud, O.; Benderitter, M. Inflammation and immunity in radiation damage to the gut mucosa. BioMed Res. Int. 2013, 2013, 123241. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Zhang, Y.; Wei, K.; He, J.; Ding, N.; Hua, J.; Zhou, T.; Niu, F.; Zhou, G.; Shi, T.; et al. Review: Effect of Gut Microbiota and Its Metabolite SCFAs on Radiation-Induced Intestinal Injury. Front. Cell. Infect. Microbiol. 2021, 11, 577236. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, H.J.; Kim, J.S.; Moon, C.; Kim, J.C.; Park, H.R.; Jung, U.; Jang, J.S.; Jo, S.K. Protective effect of an herbal preparation (HemoHIM) on radiation-induced intestinal injury in mice. J. Med. Food 2009, 12, 1353–1358. [Google Scholar] [CrossRef]
- Ciorba, M.A.; Hallemeier, C.L.; Stenson, W.F.; Parikh, P.J. Probiotics to prevent gastrointestinal toxicity from cancer therapy: An interpretive review and call to action. Curr. Opin. Support Palliat. Care 2015, 9, 157–162. [Google Scholar] [CrossRef] [Green Version]
- Salminen, E.; Elomaa, I.; Minkkinen, J.; Vapaatalo, H.; Salminen, S. Preservation of intestinal integrity during radiotherapy using live Lactobacillus acidophilus cultures. Clin. Radiol. 1988, 39, 435–437. [Google Scholar] [CrossRef]
- Segers, C.; Verslegers, M.; Baatout, S.; Leys, N.; Lebeer, S.; Mastroleo, F. Food Supplements to Mitigate Detrimental Effects of Pelvic Radiotherapy. Microorganisms 2019, 7, 97. [Google Scholar] [CrossRef] [Green Version]
- Ki, Y.; Kim, W.; Cho, H.; Ahn, K.; Choi, Y.; Kim, D. The effect of probiotics for preventing radiation-induced morphological changes in intestinal mucosa of rats. J. Korean Med. Sci. 2014, 29, 1372–1378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badgeley, A.; Anwar, H.; Modi, K.; Murphy, P.; Lakshmikuttyamma, A. Effect of probiotics and gut microbiota on anti-cancer drugs: Mechanistic perspectives. Biochim. Biophys. Acta Rev. Cancer 2021, 1875, 188494. [Google Scholar] [CrossRef] [PubMed]
- Demers, M.; Dagnault, A.; Desjardins, J. A randomized double-blind controlled trial: Impact of probiotics on diarrhea in patients treated with pelvic radiation. Clin. Nutr. 2014, 33, 761–767. [Google Scholar] [CrossRef]
- Garcia-Peris, P.; Velasco, C.; Hernandez, M.; Lozano, M.A.; Paron, L.; de la Cuerda, C.; Breton, I.; Camblor, M.; Guarner, F. Effect of inulin and fructo-oligosaccharide on the prevention of acute radiation enteritis in patients with gynecological cancer and impact on quality-of-life: A randomized, double-blind, placebo-controlled trial. Eur. J. Clin. Nutr. 2016, 70, 170–174. [Google Scholar] [CrossRef]
- Ding, X.; Li, Q.; Li, P.; Chen, X.; Xiang, L.; Bi, L.; Zhu, J.; Huang, X.; Cui, B.; Zhang, F. Fecal microbiota transplantation: A promising treatment for radiation enteritis? Radiother. Oncol. 2020, 143, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Cui, M.; Xiao, H.; Li, Y.; Zhou, L.; Zhao, S.; Luo, D.; Zheng, Q.; Dong, J.; Zhao, Y.; Zhang, X.; et al. Faecal microbiota transplantation protects against radiation-induced toxicity. EMBO Mol. Med. 2017, 9, 448–461. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wiesnoski, D.H.; Helmink, B.A.; Gopalakrishnan, V.; Choi, K.; DuPont, H.L.; Jiang, Z.D.; Abu-Sbeih, H.; Sanchez, C.A.; Chang, C.C.; et al. Fecal microbiota transplantation for refractory immune checkpoint inhibitor-associated colitis. Nat. Med. 2018, 24, 1804–1808. [Google Scholar] [CrossRef]
- Ren, R.R.; Sun, G.; Yang, Y.S.; Peng, L.H.; Wang, S.F.; Shi, X.H.; Zhao, J.Q.; Ban, Y.L.; Pan, F.; Wang, X.H.; et al. Chinese physicians’ perceptions of fecal microbiota transplantation. World J. Gastroenterol. 2016, 22, 4757–4765. [Google Scholar] [CrossRef]
- Jian, Y.; Zhang, D.; Liu, M.; Wang, Y.; Xu, Z.X. The Impact of Gut Microbiota on Radiation-Induced Enteritis. Front. Cell. Infect. Microbiol. 2021, 11, 586392. [Google Scholar] [CrossRef]
| Phylum | Genus | Nature of Change |
|---|---|---|
| Proteobacteria | Aeromonadaceae | Increased in ICD [39] |
| Enterobacteriaceae | Increased in ICD [39] | |
| Escherichia | Increased in UC [42] and ICD [43], decreased in CCD [43] | |
| Bacteroidetes | Prevotellaceae | Decreased in ICD and CCD [39] |
| Bacteroidales | ||
| Bacteroides uniformis | Decreased in CD [41] | |
| Bacteroides ovatus | Increased in CD [41] | |
| Bacteroides vulgatus | Increased in CD [41] | |
| Firmicutes | Ruminococcaceae | Decreased in ICD [39] |
| Increased in CCD [39] | ||
| Peptococcaceae | Decreased in ICD [39] | |
| Un_Clostridiales | Decreased in ICD [39] | |
| Lactobacillaceae | Increased in ICD [39] | |
| Faecalibacterium Roseburia | Increased in ICD [40] | |
| Coprococcus | Increased in ICD [40] | |
| Dialaster | Increased in ICD [40] | |
| Faecalibacterium prausnitzii | Decreased in ICD [43] | |
| Fusobacteria | Fusobacteriaceae | Increased in ICD [39] |
| Decreased in CCD [39] | ||
| Tenericutes | Anaeroplasmataceae | Decreased in ICD [39] |
| Increased in CCD [39] | ||
| Actinobacteria | Rhodococcus | Increased in UC |
| Study | Observed Change in Microbiota and Potential Causative Mechanisms in Inflammatory Response of the Gut |
|---|---|
| Reis-Ferreira et al., 2019 [51]. | There is a link between radiation enteropathy (RE) and higher Clostridium IV, Roseburia, and Phascolarctobacterium counts. In addition, there was a reduction in intestinal mucosal cytokines associated with intestinal flora regulation and intestinal wall maintenance. |
| Wang et al., 2019 [52]. | Richer number of Proteobacteria, Gammaproteobacteria, Virgibacillus, and Alcanivorax, but less Bacteroides, in patients with mild enteritis. RE-derived flora capable of initiating epithelial inflammation and barrier dysfunction, and enhancing the expression of TNF-α and IL-1β. |
| Gerassy-Vainberg et al., 2018 [53]. | Rectal radiation induces dysbiosis, which is in part mediated by IL-1β; this results in an increased susceptibility to radiation and inflammation. |
| Fernandes et al., 2021 [1]. Bennett and Eley, 1993 [54]. | Increased abundance of Proteobacteria with decreased abundance of Faecalibacterium following exposure to ionising radiation [1]. In addition, there was also an increased relative abundance of bacteria belonging to the Fusobacteria phylum, which are known to be associated with an extensive spectrum of infections [54]. |
| Cuzzolin et al., 1992 [55]; Sajjadieh et al., 2012 [56]; Garcia-Peris et al., 2012 [57]; Yamanouchi et al., 2019 [58]; Yi et al., 2021 [59]. | Bifidobacterium and Lactobacillus genera display probiotic effects, and have been used in the management of GI conditions [56,57,58]. Two studies reported decreases in abundances of the genera Bifidobacterium and Lactobacillus, whilst another reported a decrease in Lactobacilli (aerobic and anaerobic) in subjects exposed to radiation [55,56,57]. Conversely, Yi Y et al. [59] reported an increase in Lactobacillus. |
| Wang et al., 2015 [60]; Sahly et al., 2019 [61]; Wang et al., 2019 [52]; Yi et al., 2021 [59]. | Bacteroides is one of the most abundant genera in the human gut, and its members are vital in maintaining the stability of a healthy gut ecosystem [62]. They play an important role in the hydrolysis and fermentation of exogenous fibre and endogenous mucins, both in the deconjugation of bile acids and in the production of acetic and lactic acids [63,64]. Additionally, they play a part in stimulating the immune system, by augmenting the production of IL-2 by macrophages and B cells [56,65]. They have been found to be beneficial to the gut when present in other locations, but can cause significant infections [65]. The analysed studies reported mixed results: increases in relative abundance in two studies [60,61]; decreases in two other studies [52,59]. These studies were limited due to small sample sizes, not having a healthy control group, and for including patients on medications known to disrupt the gut microbiota [66,67], thus, making it more difficult to fully isolate the unique effect of radiation. |
| Study | Findings |
|---|---|
| Lepage et al., 2008 [73] | Biopsies of colonic mucosa of CD patients found that CD patients possessed significantly more virus-like particles (VLPs) than healthy individuals. |
| Wagner et al., 2013 [74] | Higher abundance of phages in paediatric CD patients compared to controls. Bacteroides phage B10-8 and phage B124-14 represented the largest proportion of sequences. Finally, the Mycobacterium phage composition in ileum tissue samples of CD patients was different compared to controls. |
| Perez-Brocal et al., 2015 [75] | Phages were three times more abundant in faeces than in colonic biopsies, and the disease status of individuals was more accurately reflected by the bacterial rather than the viral communities. Moreover, a number of viral biomarkers that are associated only with CD disease were identified. Finally, they found that there was a rise, in CD patients, in phages infecting bacterial orders Alteromonadales and Clostridiales, including bacterial species Clostridium acetobutylicum and the Retroviridae family. |
| Wang et al., 2015 [76] | Increased viral sequences in CD and difference in the abundance and diversity within the virome between CD and the control group. |
| Norman et al., 2015 [77] | Higher viral richness and Caudovirales growth in CD and UC patients, reduced bacterial richness and diversity in CD and UC, and a negative association between Caudovirales and prevalent bacterial taxa in CD. |
| Zuo et al., 2019 [78] | Larger number of Caudovirales phages, but reduced diversity, richness, and uniformity of mucosa Caudovirales in UC patients compared with healthy controls. In addition, there was a higher abundance of Escherichia and Enterobacteria phages in the mucosa of UC patients than in heathy controls. |
| Clooney et al., 2019 [79] | Showed that a healthy core of virulent phages is substituted by temperate phages in CD patients. |
| Fernandes et al., 2019 [80] | Paediatric IBD subjects had a greater relative abundance of Caudovirales to Microviridae phages compared to controls. The Caudovirales phages were also more abundant in CD than UC, but not controls. The richness of viral strains in Microviridae, but not Caudovirales, was increased in controls compared to CD but not UC. |
| Yan et al., 2020 [81] | Paediatric CD patients in a virome sequencing study showed higher diversity between patients, and low variation within patients, of wash samples taken from the proximal and distal colon. |
| Liang et al., 2020 [82] | No significant difference in the total number of VLPs between very early onset IBD, defined as the occurring before the age of 6 years, and healthy controls. However, the very early onset IBD subjects exhibited a higher ratio of Caudovirales vs. Microviridae compared to healthy controls. |
| TLRs | Role in IBD |
|---|---|
| TLR1/2 | Stops chronic inflammation [87,88] |
| TLR2/6 | Stimulates colitis [89,90] |
| Dampens down the immune response [91] | |
| TLR3 | Assists in protective immunity under an inflammatory environment [92] |
| TLR4 | Leads to a breakdown of intestinal tissue and ulceration [93,94,95] |
| Has a defensive role [96] | |
| TLR5 | Inhibits diseases that can occur due to intestinal inflammation [97] |
| TLR7 | Provides ability to fight of infection under inflammatory conditions [92] |
| TLR8 | Stimulates inflammation of mucosa [98] |
| TLR9 | Has a defensive role [99,100,101] |
| Probiotic | Effect | |
|---|---|---|
| Crohn’s Disease | Saccharomyces boulardii | Reduced recurrence rates when combined with 5-ASA treatment [118]. |
| Reduces intestinal permeability and secondary bacterial translocation, as well as demonstrating an immunomodulatory effect by causing a rise in plasma levels of IL-10 and intestinal IgA secretion [119]. | ||
| Synergy 1 (containing Bifidobacterium longum, oligofructose, and inulin) | TNF-α, a pro-inflammatory biomarker in the intestinal mucosa, was reduced, as was disease activity, after 6 months of treatment. This was also found using histological indices [120]. | |
| VSL#3 (containing Bifidobacterium infantis, Bifidobacterium breve, Bifidobacterium longum, Streptococcus thermophilus, Lactobacillus paracasei, Lactobacillus acidophilus, Lactobacillus recarurus) | Patients given VSL#3 immediately after surgery had reduced levels of Il-8 and IL-1b, which are pro-inflammatory cytokines, and also had lower rates of disease recurrence compared to those given treatment 90 days post-surgery [121]. | |
| Ulcerative Colitis | Combination of Saccharomices boulardii and VSL#3 with conventional therapy | No significant improvement in the remission rates of the disease, but found to be beneficial in decreasing disease activity [122]. |
| Combining VSL#3 with standard therapy | Endoscopic healing of colonic mucosa and a decrease in ulcerative colitis disease activity index (UCDAI) score by more than 50% after 12 weeks of treatment [123]. | |
| VSL#3 | The use of VSL#3 amongst children with UC in the induction and maintenance of remission is effective when either used alongside steroids and 5-ASA treatment [124], or when used alone [125]. | |
| Bifidobacteria-fermented milk (a combination of Bifidobacterium strains and Lactobacillus acidophilus) | Improved endoscopic and histological scores in patients with UC [126]. | |
| Escherichia coli Nissle 1917 Bifidobacterium breve strain Yakult Bifidobacterium breve Saccharomyces boulardii | Showed to have a comparable effect with 5-ASA in maintaining remission when used in patients with mild to moderate UC [127,128,129,130]. | |
| Saccharomyces boulardii | Clinical remission of UC was maintained with 400 mg rifaximin and 500 mg Saccharomyces boulardii after 3 months of use. This treatment regimen may be helpful in preventing early relapses in UC [131], which is an important therapeutic target in the management of patients with IBD [132]. |
| Antibiotic | Study | Findings |
|---|---|---|
| Various combinations (including ciprofloxacin, metronidazole, rifaximin, clarithromycin) | Khan et al., 2011 [160] | Antibiotics were better at inducing remission of active CD compared to placebo. |
| Wang et al., 2012 [161] | 56.1% (214/429) of patients treated with antibiotics showed a response compared to 37.9% (153/403) of patients given the placebo. | |
| Su et al., 2015 [162] | The combined relative risk (RR) for clinical remission or response in patients with CD was 1.33. | |
| Ciprofloxacin | Arnold et al., 2002 [163] | There were significantly lower disease activity scores in 47 patients with moderately active resistant disease who had been treated with a twice daily regime of ciprofloxacin 500 mg compared to those who received placebo only. |
| Steinhart et al., 2002 [164] | Ciprofloxacin treatment was found to be more beneficial for those who had active disease and colonic involvement. | |
| Su et al., 2015. [162] | There was a similar clinical response rate between the ciprofloxacin and placebo group. | |
| Metronidazole | Sutherland et al., 1991 [165] | There was minimal benefit of Metronidazole use in active CD, with a decrease in disease activity index but no difference in the rate of remission. |
| Combination of Ciprofloxacin and Metronidazole | Prantera et al., 1996 [166] | Although not statistically significant, the steroid group contained a higher number of patients in clinical remission. |
| Steinhart et al., 2002 [164] | No difference in remission rates. | |
| Rifaximin | Prantera et al., 1996 [166] | 402 patients with CD received 12 weeks of treatment with extended release rifaximin; 62% of those given Rifaximin 800 mg were in remission compared with 43% who received the placebo. |
| Khan et al., 2011 [160] | Able to induce remission, and led to a decreased risk of persisting active disease compared to the placebo. | |
| Jigaranu et al., 2014 [167] | All patients receiving Rifaximin 800 mg twice daily for 12 weeks achieved remission compared to 84% in the placebo group. |
| Metronidazole | Chapman et al., 1986 [168] | In this RCT, 39 patients were given either metronidazole with steroids or placebo with steroids for 5 days. There was no significant difference between either treatment group. |
| Gilat et al., 1987 [169] | From a prospective RCT, it was found that 1.35 g/day of oral metronidazole was ineffective in managing an attack flare of non-severe UC compared to 4.5 g/day of sulfasalazine. | |
| Mantzaris et al., 1997 [170]; Mantzaris et al., 2001 [171] | Two RCTs found no significant difference in clinical improvement when assessing intravenous or oral treatment with metronidazole alongside steroids for 2 weeks in patients with mild to severe UC. | |
| Metronidazole/Tobramycin | Burke et al., 1990 [172] | In 84 patients with an acute flare of UC that were randomised to receive either oral tobramycin or placebo alongside steroid therapy for 1 week, 74% of those given tobramycin achieved complete symptomatic remission, compared with 43% in the placebo group. There were also better histological scores at the study endpoint in the tobramycin group. |
| Mantzaris et al., 1994 [173] | In 39 patients with severe UC received either metronidazole and tobramycin or placebo in addition to total parenteral nutrition (TPN), IV hydrocortisone, and hydrocortisone enemas. In total, 66% of patients given antibiotics, and 65% of those that took the placebo, showed considerable improvement. | |
| Ciprofloxacin | Turunen et al., 1998 [174] | This study revealed that 6 months of ciprofloxacin treatment compared to placebo, in addition to steroids, in 83 patients known to be poor responders to conventional therapy, resulted in a lower rate of treatment failure; 21% vs. 44%, respectively. |
| Peterson et al., 2014 [175] | In contrast with the above, a double-blind randomised placebo-controlled trial of ciprofloxacin and probiotic Escherichia coli Nissle add-on treatment in 100 patients with active UC found that 78% reached remission in the ciprofloxacin/placebo vs. 89% in the placebo/placebo group. | |
| Rifaximin | Gionchetti et al., 1999 [176] | In the treatment of active UC, rifaximin was found to be better than the placebo. |
| Diet | Findings |
|---|---|
| Specific Carbohydrate Diet | Consuming complex carbohydrates results in a pro-inflammatory microbiome due to fermentation and overgrowth of bacteria when they arrive in the colon [177,178]. Therefore, complex carbohydrates are avoided. Instead, foods that can be eaten include unprocessed meats, most fruits and vegetables, all fats and oils, aged cheeses, and lactose-free yogurt [179]. Following this diet was found to lead to clinical remission in 66% of patients after 10 months, and many were able to stop corticosteroid use [180]. Another survey also demonstrated beneficial results, with 42 % showing remission at both 6 and 12 months [181]. |
| Low FODMAP diet | The low FODMAP diet restricts carbohydrates that are poorly absorbed and highly fermentable [33]. Positive results have been shown when utilising this diet in the management of symptoms relating to irritable bowel syndrome (IBS) [182,183,184]. Yet, there is a lack of knowledge on how underlying inflammation may be affected by this diet [179]. |
| Gluten-free diet | Two large studies have examined its effects. One assessed patients who had a co-diagnosis of coeliac disease, and found that approximately 66% had an improvement in bowel symptoms, and 38% had less severe and frequent IBD flares when on a gluten-free diet [185]. The other study, involving 1254 patients mostly without coeliac disease, found no significant differences between patients following a gluten-free diet and those who were not [186]. |
| Anti-inflammatory Diet | The anti-inflammatory diet (AID) is based on the daily consumption of fruits and vegetables that provide anti-inflammatory compounds such as vitamins B3, B6, E, C, beta-carotene, as well as zinc and magnesium [33]. Olendzki et al., who developed the IBD-AID diet, found that it improved symptoms of patients who were responsive to pharmacological treatment [187]. |
| Mediterranean Diet | The Mediterranean diet involves consuming phytonutrients, replacing saturated and trans-fatty acids with unsaturated fats (such as olive oil), omega-3 polyunsaturated fats, vegetables, high-fibre whole grains, nuts, and a low intake of red meats [33]. In 153 healthy Italian subjects, compliance with a Mediterranean diet resulted in a positive effect on the gut microbiota and associated metabolome [188]. Furthermore, when eight adult patients suffering from CD followed the Mediterranean diet for 6 weeks, their transcriptome analysis showed a change in expression of more than 3000 genes. They also showed that the intestinal microbiota began to normalise [189]. |
| Study | Condition | Findings |
|---|---|---|
| Ott et al., 2017 [191] | Recurrent Clostridioides difficile infection (rCDI) | Restored normal stool habits of patients and alleviated symptoms of CDI for at least 6 months. |
| Kao et al., 2019 [192] | Recurrent Clostridioides difficile infection (rCDI) | Primary outcome of no recurrence of CDI at the end of 8 weeks post treatment was achieved in 75% (three out of four) patients. |
| Draper et al., 2020 [193] | Antibiotic-induced dysbiosis | The gut bacteriome was reshaped towards that of pre-antibiotic-treated mice. |
| Brunse et al., 2022 [194] | Necrotising Enterocolitis | Oro-gastric FVT completely prevented NEC, increased viral diversity, and reduced Proteobacteria relative abundance. |
| Study | Findings |
|---|---|
| Galtier at al., 2017 [202] | Oral treatment with a phage cocktail in colitis mouse model was effective at decreasing colonisation and symptoms over a 2-week period. |
| Vahedi et al., 2018 [203] | Single dose of phage cocktail was effective at controlling infection. |
| Yu et al., 2018 [204] | Treatment with phage cocktail was able to control infection, but also led to fewer phage-resistant bacteria. |
| Febvre et al., 2019 [205] | Taking a commercial cocktail of E. coli-targeting phages for 28 days selectively decreased the faecal E. coli levels without the gut microbiota community being affected. |
| Probiotic | Effect |
|---|---|
| Lactobacillus | Clinical studies and preclinical models have shown its potential to reduce GI toxicity after RT [209]. |
| In gynaecological cancer patients who had received pelvic RT, twice daily ingestion >2 × 109 live Lactobacillus, resulted in a reduction in diarrhoea symptoms post treatment [210]. | |
| Lactobacillus and Bifidobacterium | Have been found to decrease cancerous tumour size through their influence on immune regulation [207,211]. |
| L. acidophilus | Shown to be beneficial against radiation-induced intestinal mucosal injury in rats [212]. |
| Bifidobacterium | Reduce chemotherapy-induced mucositis and radiation-induced diarrhoea [213]. |
| Lactobacillus acidophilus LAC-361 and Bifidobacterium longum BB-536 | May decrease radiation-induced diarrhoea after the completion of treatment in patients with pelvic cancers [214]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, D.; Andreyev, J. The Role of the Human Gut Microbiome in Inflammatory Bowel Disease and Radiation Enteropathy. Microorganisms 2022, 10, 1613. https://doi.org/10.3390/microorganisms10081613
Fernandes D, Andreyev J. The Role of the Human Gut Microbiome in Inflammatory Bowel Disease and Radiation Enteropathy. Microorganisms. 2022; 10(8):1613. https://doi.org/10.3390/microorganisms10081613
Chicago/Turabian StyleFernandes, Darren, and Jervoise Andreyev. 2022. "The Role of the Human Gut Microbiome in Inflammatory Bowel Disease and Radiation Enteropathy" Microorganisms 10, no. 8: 1613. https://doi.org/10.3390/microorganisms10081613
APA StyleFernandes, D., & Andreyev, J. (2022). The Role of the Human Gut Microbiome in Inflammatory Bowel Disease and Radiation Enteropathy. Microorganisms, 10(8), 1613. https://doi.org/10.3390/microorganisms10081613






