Antifungal Activity of Spent Coffee Ground Extracts
Abstract
:1. Introduction
2. Materials and Methods
2.1. Fungal Strains and Growth Conditions
2.2. Coffee Spent Grounds Extracts Preparation
2.3. Analysis of Phenolic Compounds
2.4. Screening of the Antifungal Activity In Vitro
2.4.1. Antimicrobial Susceptibility Testing
2.4.2. Minimum Fungicidal Concentration
2.5. Quantification of Membrane and Cell Wall Components
2.5.1. Inoculum Preparation
2.5.2. Determination of the Ergosterol Contents
2.5.3. Determination the Cell Wall β-(1,3)-Glucan Content
2.5.4. Determination the Cell Wall Chitin Contents
2.6. Characterization of Morphological and Ultrastructural Changes
2.7. Cytotoxicity Activity
2.8. Anti-Inflammatory Activity
2.9. Statistical Analysis
3. Results
3.1. Extract Preparation and Total Phenol Analysis
3.2. Antifungal Activity
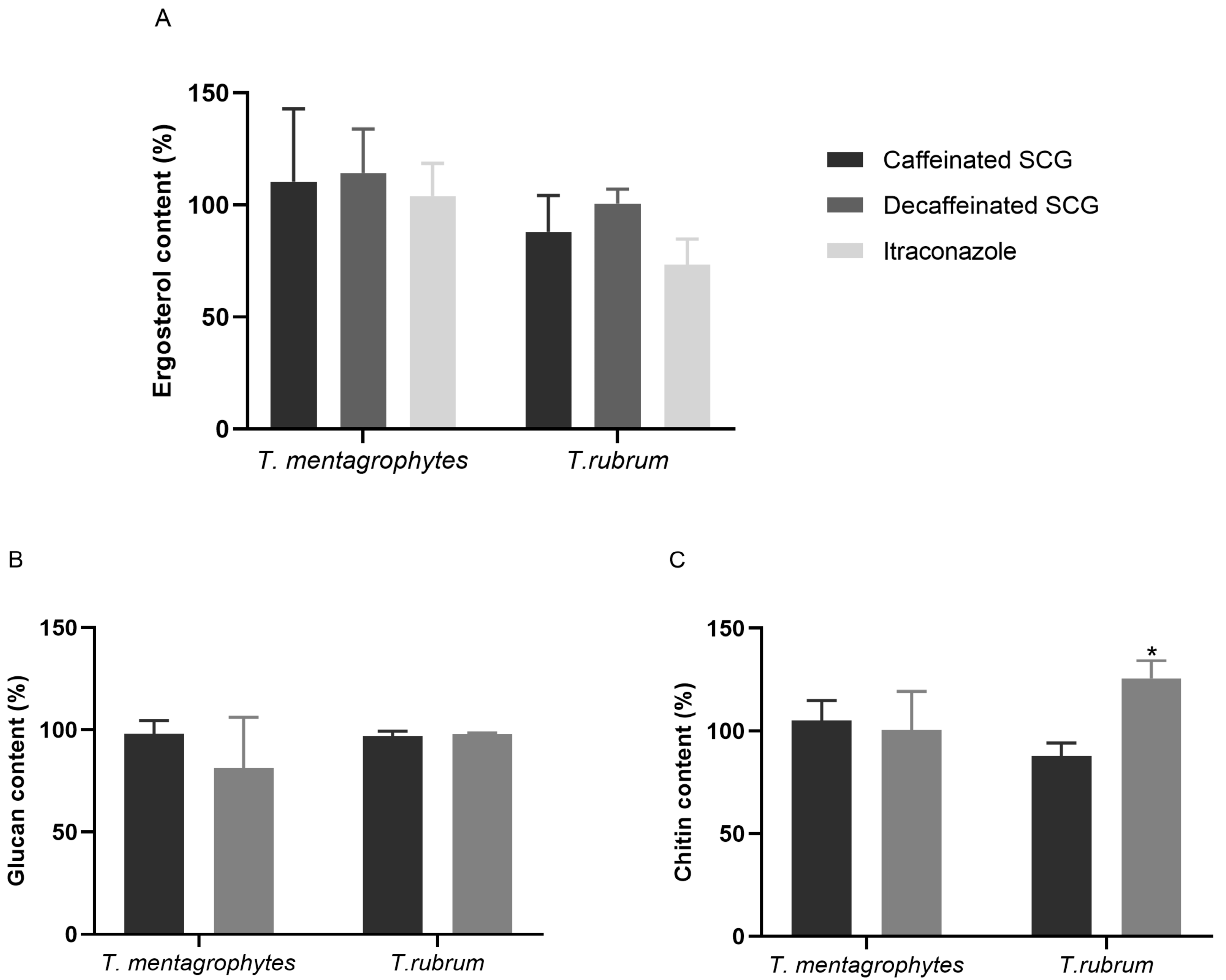
3.3. Cell Membrane and Cell Wall Components Modulation in Response to SCG
3.4. Fungal Ultrastructural Modifications in Response to SCG Evaluated by TEM
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brown, G.D.; Denning, D.W.; Gow, N.A.R.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden killers: Human fungal infections. Sci. Transl. Med. 2012, 4, 165rv13. [Google Scholar] [CrossRef] [Green Version]
- Faway, E.; de Rouvroit, C.L.; Poumay, Y. In vitro models of dermatophyte infection to investigate epidermal barrier alterations. Exp. Dermatol. 2018, 27, 915–922. [Google Scholar] [CrossRef] [Green Version]
- Garber, G. An overview of fungal infections. Drugs 2001, 61 (Suppl. S1), 1–12. [Google Scholar] [CrossRef]
- Ghannoum, M.A.; Isham, N.C. Dermatophytes and dermatophytoses. In Clinical Mycology, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2009; pp. 375–384. [Google Scholar]
- Tainwala, R.; Sharma, Y.K. Pathogenesis of dermatophytoses. Indian J. Dermatol. 2011, 56, 259–261. [Google Scholar] [CrossRef]
- Geddes-McAlister, J.; Shapiro, R.S. New pathogens, new tricks: Emerging, drug-resistant fungal pathogens and future prospects for antifungal therapeutics. Ann. N. Y. Acad. Sci. 2019, 1435, 57–78. [Google Scholar] [CrossRef]
- Alenazy, H.; Alghamdi, A.; Pinto, R.; Daneman, N. Candida colonization as a predictor of invasive candidiasis in non-neutropenic ICU patients with sepsis: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 102, 357–362. [Google Scholar] [CrossRef]
- Kühbacher, A.; Burger-Kentischer, A.; Rupp, S. Interaction of Candida species with the skin. Microorganisms 2017, 5, 32. [Google Scholar] [CrossRef] [Green Version]
- Casadevall, A. Fungal diseases in the 21st century: The near and far horizons. Pathog. Immun. 2018, 3, 183–196. [Google Scholar] [CrossRef]
- Fisher, M.C.; Gurr, S.J.; Cuomo, C.A.; Blehert, D.S.; Jin, H.; Stukenbrock, E.H.; Stajich, J.E.; Kahmann, R.; Boone, C.; Denning, D.W.; et al. Threats Posed by the Fungal Kingdom to Humans, Wildlife, and Agriculture. mBio 2020, 11, e00449-20. [Google Scholar] [CrossRef]
- Mishra, K.K.; Kaur, C.D.; Sahu, A.K.; Panik, R.; Kashyap, P.; Mishra, S.P.; Dutta, S. Medicinal Plants Having Antifungal Properties. In Medicinal Plants-Use in Prevention and Treatment of Diseases; Hassan, B.A.R., Ed.; IntechOpen: London, UK, 2020. [Google Scholar]
- Sousa, C.; Gabriel, C.; Cerqueira, F.; Manso, M.C.; Vinha, A.F. Coffee industrial waste as a natural source of bioactive compounds with antibacterial and antifungal activities. In The Battle Against Microbial Pathogens: Basic Science, Technological Advances and Educational Programs; Méndez-Vilas, A., Ed.; Formatex Research Center: Badajoz, Spain, 2016; pp. 131–136. [Google Scholar]
- Campos-Vega, R.; Loarca-Piña, G.; Vergara-Castañeda, H.A.; Dave Oomah, B. Spent coffee grounds: A review on current research and future prospects. Trends Food Sci. Technol. 2015, 45, 24–36. [Google Scholar] [CrossRef]
- Nieber, K. The Impact of Coffee on Health Author Pharmacokinetics and Mode of Action Bioactive Components in Coffee. Planta Med. 2017, 83, 1256–1263. [Google Scholar]
- Panusa, A.; Zuorro, A.; Lavecchia, R.; Marrosu, G.; Petrucci, R. Recovery of natural antioxidants from spent coffee grounds. J. Agric. Food Chem. 2013, 61, 4162–4168. [Google Scholar] [CrossRef]
- Kovalcik, A.; Obruca, S.; Marova, I. Valorization of spent coffee grounds: A review. Food Bioprod. Process. 2018, 110, 104–119. [Google Scholar] [CrossRef]
- Colombo, R.; Papetti, A. Decaffeinated coffee and its benefits on health: Focus on systemic disorders. Crit. Rev. Food Sci. Nutr. 2021, 61, 2506–2522. [Google Scholar] [CrossRef]
- Duangjai, A.; Suphrom, N.; Wungrath, J.; Ontawong, A.; Nuengchamnong, N.; Yosboonruang, A. Comparison of antioxidant, antimicrobial activities and chemical profiles of three coffee (Coffea arabica L.) pulp aqueous extracts. Integr. Med. Res. 2016, 5, 324–331. [Google Scholar] [CrossRef] [Green Version]
- Alvarado-Ambriz, S.; Lobato-Calleros, C.; Hernández-Rodríguez, L.; Vernon-Carter, E. Wet processing coffee waste as an alternative to produce extracts with antifungal activity: In vitro and in vivo valorization. Rev. Mex. De Ing. Química 2020, 19 (Suppl. S1), 135–149. [Google Scholar] [CrossRef]
- Sangta, J.; Wongkaew, M.; Tangpao, T.; Withee, P.; Haituk, S.; Arjin, C.; Sringarm, K.; Hongsibsong, S.; Sutan, K.; Pusadee, T.; et al. Recovery of Polyphenolic Fraction from Arabica Coffee Pulp and Its Antifungal Applications. Plants 2021, 10, 1422. [Google Scholar] [CrossRef]
- Rodrigues, F.; Palmeira-de-Oliveira, A.; das Neves, J.; Sarmento, B.; Amaral, M.H.; Oliveira, M.B. Coffee silverskin: A possible valuable cosmetic ingredient. Pharm. Biol. 2015, 53, 386–394. [Google Scholar] [CrossRef]
- Mathur, I.; Shruthi, S.; Gandrakota, K.; Nisha, K.K. Comparative Evaluation of Antifungal Activity of Green Coffee and Green Tea Extract against Candida albicans: An In Vitro Study. World J. Dent. 2021, 12, 265–270. [Google Scholar] [CrossRef]
- Antoine, G.; Vaissayre, V.; Meile, J.-C.; Payet, J.; Conéjéro, G.; Costet, L.; Fock-Bastide, I.; Joët, T.; Dussert, S. Diterpenes of Coffea seeds show antifungal and anti-insect activities and are transferred from the endosperm to the seedling after germination. Plant Physiol. Biochem. 2023, 194, 627–637. [Google Scholar] [CrossRef]
- Mahajan, R.; Kapoor, N. Phytochemical analysis and antimicrobial activity of roasted beans of coffea robusta. Int. J. Pharm. Biol. Sci. 2018, 8, 89–95. [Google Scholar]
- Martínez-Tomé, M.; Jiménez-Monreal, A.M.; García-Jiménez Almela, L.L.; García-Diz, L.; Mariscal-Arcas, M.; Murcia, M.A. Assessment of antimicrobial activity of coffee brewed in three different ways from different origins. Eur. Food Res. Technol. 2011, 233, 497. [Google Scholar] [CrossRef]
- Mehta, V.; Rajesh, G.; Rao, A.; Shenoy, R.; Pai, M. Antimicrobial Efficacy of Punica granatum mesocarp, Nelumbo nucifera Leaf, Psidium guajava Leaf and Coffea Canephora Extract on Common Oral Pathogens: An In-vitro Study. J. Clin. Diagn. Res. 2014, 8, 65–68. [Google Scholar]
- Mussatto, S.I.; Ballesteros, L.F.; Martins, S.; Teixeira, J.A. Extraction of antioxidant phenolic compounds from spent coffee grounds. Sep. Purif. Technol. 2011, 83, 173–179. [Google Scholar] [CrossRef] [Green Version]
- Farah, A.; Donangelo, C.M. Phenolic compounds in coffee. Braz. J. Plant Physiol. 2006, 18, 23–36. [Google Scholar] [CrossRef]
- Murthy, P.S.; Naidu, M.M. Recovery of Phenolic Antioxidants and Functional Compounds from Coffee Industry By-Products. Food Bioprocess Technol. 2012, 5, 897–903. [Google Scholar] [CrossRef]
- Ramalakshmi, K.; Rao, L.J.M.; Takano-Ishikawa, Y.; Goto, M. Bioactivities of low-grade green coffee and spent coffee in different in vitro model systems. Food Chem. 2009, 115, 79–85. [Google Scholar] [CrossRef]
- Fernandes, C.; Anjos, J.; Walker, L.A.; Silva, B.M.A.; Cortes, L.; Mota, M.; Munro, C.A.; Gow, N.A.R.; Gonçalves, T. Modulation of Alternaria infectoria cell wall chitin and glucan synthesis by cell wall synthase inhibitors. Antimicrob. Agents Chemother. 2014, 58, 2894–2904. [Google Scholar] [CrossRef] [Green Version]
- Bessada, S.M.F.; Barreira, J.C.M.; Barros, L.; Ferreira, I.C.F.R.; Oliveira, M.B.P.P. Phenolic profile and antioxidant activity of Coleostephus myconis (L.) Rchb.f.: An underexploited and highly disseminated species. Ind. Crops Prod. 2016, 89, 45–51. [Google Scholar] [CrossRef] [Green Version]
- Espinel-Ingroff, A.; Chaturvedi, V.; Fothergill, A.; Rinaldi, M. Optimal testing conditions for determining MICs and minimum fungicidal concentrations of new and established antifungal agents for uncommon molds: NCCLS collaborative study. J. Clin. Microbiol. 2002, 40, 3776–3781. [Google Scholar] [CrossRef] [Green Version]
- Breivik, O.N.; Owades, J.L. Yeast analysis, spectrophotometric semimicrodetermination of ergosterol in yeast. J. Agric. Food Chem. 1957, 5, 360–363. [Google Scholar] [CrossRef]
- Fernandes, C.; Mota, M.; Barros, L.; Dias, M.I.; Ferreira, I.C.F.R.; Piedade, A.P.; Casadevall, A.; Gonçalves, T. Pyomelanin Synthesis in Alternaria alternata Inhibits DHN-Melanin Synthesis and Decreases Cell Wall Chitin Content and Thickness. Front Microbiol. 2021, 12, 691433. [Google Scholar] [CrossRef]
- Zuorro, A.; Lavecchia, R. Spent coffee grounds as a valuable source of phenolic compounds and bioenergy. J. Clean. Prod. 2012, 34, 49–56. [Google Scholar] [CrossRef]
- Sung, W.S.; Lee, D.G. Antifungal action of chlorogenic acid against pathogenic fungi, mediated by membrane disruption. Pure Appl. Chem. 2010, 82, 219–226. [Google Scholar] [CrossRef]
- Martínez, G.; Regente, M.; Jacobi, S.; Del Rio, M.; Pinedo, M.; de la Canal, L. Chlorogenic acid is a fungicide active against phytopathogenic fungi. Pestic. Biochem. Physiol. 2017, 140, 30–35. [Google Scholar] [CrossRef]
- Ma, J.-N.; Ma, C.-M. Antifungal inhibitory activities of caffeic and quinic acid derivatives. In Coffee in Health and Disease Prevention; Preedy, V.R., Ed.; Elsevier Inc.: Amsterdam, The Netherlands; Academic Press: London, UK, 2015; pp. 635–641. [Google Scholar]
- Kalinowska, M.; Bajko, E.; Matejczyk, M.; Kaczyński, P.; Łozowicka, B.; Lewandowski, W. The Study of Anti-/Pro-Oxidant, Lipophilic, Microbial and Spectroscopic Properties of New Alkali Metal Salts of 5-O-Caffeoylquinic Acid. Int. J. Mol. Sci. 2018, 19, 463. [Google Scholar] [CrossRef] [Green Version]
- Suárez-Quiroz, M.L.; Alonso Campos, A.; Valerio Alfaro, G.; González-Ríos, O.; Villeneuve, P.; Figueroa-Espinoza, M.C. Anti-Aspergillus activity of green coffee 5-O-caffeoyl quinic acid and its alkyl esters. Microb. Pathog. 2013, 61–62, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Almeida, A.A.P.; Farah, A.; Silva, D.A.; Nunan, E.A.; Glória, M.B.A. Antibacterial activity of coffee extracts and selected coffee chemical compounds against enterobacteria. J. Agric. Food Chem. 2006, 54, 8738–8743. [Google Scholar] [CrossRef]
- Monente, C.; Bravo, J.; Vitas, A.I.; Arbillaga, L.; De Peña, M.P.; Cid, C. Coffee and spent coffee extracts protect against cell mutagens and inhibit growth of food-borne pathogen microorganisms. J. Funct. Foods 2015, 12, 365–374. [Google Scholar] [CrossRef]
- Díaz-Hernández, G.C.; Alvarez-Fitz, P.; Maldonado-Astudillo, Y.I.; Jiménez-Hernández, J.; Parra-Rojas, I.; Flores-Alfaro, E.; Salazar, R.; Ramírez, M. Antibacterial, Antiradical and Antiproliferative Potential of Green, Roasted, and Spent Coffee Extracts. Appl. Sci. 2022, 12, 1938. [Google Scholar] [CrossRef]
- Badr, A.N.; El-Attar, M.M.; Ali, H.S.; Elkhadragy, M.F.; Yehia, H.M.; Farouk, A. Spent Coffee Grounds Valorization as Bioactive Phenolic Source Acquired Antifungal, Anti-Mycotoxigenic, and Anti-Cytotoxic Activities. Toxins 2022, 14, 109. [Google Scholar] [CrossRef] [PubMed]
- Rawangkan, A.; Siriphap, A.; Yosboonruang, A.; Kiddee, A.; Pook-In, G.; Saokaew, S.; Sutheinkul, O.; Duangjai, A. Potential Antimicrobial Properties of Coffee Beans and Coffee By-Products Against Drug-Resistant Vibrio cholerae. Front. Nutr. 2022, 9, 865684. [Google Scholar] [CrossRef] [PubMed]
- Bouhlal, F.; Aqil, Y.; Chamkhi, I.; Belmaghraoui, W.; Labjar, N.; El Hajjaji, S.; Benabdellah, G.A.; Aurag, J.; Lotfi, E.M.; Mahi, M.E. GC-MS Analysis, Phenolic Compounds Quantification, Antioxidant, and Antibacterial Activities of the Hydro-alcoholic Extract of Spent Coffee Grounds. J. Biol. Act. Prod. Nat. 2020, 10, 325–337. [Google Scholar] [CrossRef]
- Latgé, J.P. Tasting the fungal cell wall. Cell. Microbiol. 2010, 12, 863–872. [Google Scholar] [CrossRef] [PubMed]
- Money, N.P. Fungal Cell Biology and Development. In The Fungi, 3rd ed.; Elsevier Ltd.: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Jordá, T.; Puig, S. Regulation of Ergosterol Biosynthesis in Saccharomyces cerevisiae. Genes 2020, 11, 795. [Google Scholar] [CrossRef]
- Bowman, S.M.; Free, S.J. The structure and synthesis of the fungal cell wall. BioEssays 2006, 28, 799–808. [Google Scholar] [CrossRef]
- Gow, N.A.R.; Latgé, J.P.; Munro, C.A. The fungal cell wall: Structure, biosynthesis, and function. Microbiol. Spectr. 2017, 5, 267–292. [Google Scholar] [CrossRef] [Green Version]
- Kuranda, K.; Leberre, V.; Sokol, S.; Palamarczyk, G.; François, J. Investigating the caffeine effects in the yeast Saccharomyces cerevisiae brings new insights into the connection between TOR, PKC and Ras/cAMP signalling pathways. Mol. Microbiol. 2006, 61, 1147–1166. [Google Scholar] [CrossRef]
- Perfect, J.R. The antifungal pipeline: A reality check. Nat. Rev. Drug Discov. 2017, 16, 603–616. [Google Scholar] [CrossRef] [Green Version]
- Scorzoni, L.; de Paula e Silva, A.C.A.; Marcos, C.M.; Assato, P.A.; de Melo, W.C.M.A.; de Oliveira, H.C.; Costa-Orlandi, C.B.; Mendes-Giannini, M.J.S.; Fusco-Almeida, A.M. Antifungal therapy: New advances in the understanding and treatment of mycosis. Front. Microbiol. 2017, 8, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Fernandes, C.; Gow, N.A.R.; Gonçalves, T. The importance of subclasses of chitin synthase enzymes with myosin-like domains for the fitness of fungi. Fungal Biol. Rev. 2016, 30, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Arias, P.; Díez-Muñiz, S.; García, R.; Nombela, C.; Rodríguez-Peña, J.M.; Arroyo, J. Genome-wide survey of yeast mutations leading to activation of the yeast cell integrity MAPK pathway: Novel insights into diverse MAPK outcomes. BMC Genom. 2011, 12, 390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shingu-Vazquez, M.; Traven, A. Mitochondria and fungal pathogenesis: Drug tolerance, virulence, and potential for antifungal therapy. Eukaryot. Cell 2011, 10, 1376–1383. [Google Scholar] [CrossRef] [PubMed]
- Angeloni, S.; Freschi, M.; Marrazzo, P.; Hrelia, S.; Beghelli, D.; Juan-García, A.; Juan, C.; Caprioli, G.; Sagratini, G.; Angeloni, C. Antioxidant and Anti-Inflammatory Profiles of Spent Coffee Ground Extracts for the Treatment of Neurodegeneration. Oxidative Med. Cell. Longev. 2021, 2021, 6620913. [Google Scholar] [CrossRef]




| Peak | Rt (min) | λmax (nm) | [M-H]− (m/z) | MS2 (m/z) | Tentative Identification | Quantification (mg/g Extract) | t-Students Test p-Value | |
|---|---|---|---|---|---|---|---|---|
| SCG Caffeinated | SCG Decaffeinated | |||||||
| 1 | 4.64 | 316 | 353 | 191(100), 179(78), 173(11), 135(14). | 3-O-Caffeoylquinic acid | 12.1 ± 0.1 | 8 ± 1 | <0.001 |
| 2 | 5.23 | 319 | 353 | 191(49), 179(72), 173(100), 135(11). | 4-O-Caffeoylquinic acid | 5.26 ± 0.03 | 12.1 ± 0.3 | <0.001 |
| 3 | 5.77 | 323 | 353 | 191(100), 179(49), 173(52), 135(12). | cis 5-O-Caffeoylquinic acid | 16.6 ± 0.5 | 24 ± 1 | <0.001 |
| 4 | 6.44 | 323 | 353 | 191(100), 179(28), 173(35), 135(5). | trans 5-O-Caffeoylquinic acid | 24 ± 1 | 14 ± 1 | <0.001 |
| 5 | 9.66 | 325 | 367 | 193(23), 191(5), 173(100), 161(10), 149(4). | 4-O-Feruloylquinic acid | 21.17 ± 0.02 | 2.49 ± 0.04 | <0.001 |
| 6 | 12.01 | 326 | 335 | 179/13), 161(100), 134(41). | Caffeoylshikimic acid | 17.2 ± 0.1 | 20.3 ± 0.5 | <0.001 |
| 7 | 17.87 | 324 | 515 | MS2: 353(100), 335(12), 317(5), 299(12), 203(10), 179(14), 173(13). MS3:191(52), 179(70), 173(100). | 1,4-O-diCaffeoylquinic acid | 11.3 ± 0.5 | 10.2 ± 0.3 | <0.001 |
| 8 | 19.1 | 324 | 515 | MS2: 353(100). MS3: 335(12), 191(100), 179(81), 173(142). | 1,3-O-diCaffeoylquinic acid | 7.02 ± 0.11 | 4.7 ± 0.2 | <0.001 |
| 9 | 21.64 | 324 | 515 | MS2: 353(100), 335(9), 317(5), 299(21), 203(9), 173(5). MS3:191(32), 179(51), 173(100). | 3,4-O-diCaffeoylquinic acid | 8.3 ± 0.2 | 6.8 ± 0.5 | <0.001 |
| 10 | 23.27 | 325 | 529 | MS2: 367(100), 335(20), 193(14). MS3: 173(100). | 4-Feruloyl-5-caffeoylquinic acid | 1.87 ± 0.03 | 1.5 ± 0.1 | <0.001 |
| 11 | 27.29 | 325 | 529 | MS2: 367(100), 193(14). MS3: 191(100). | 3-Feruloyl-5-caffeoylquinic acid | 2.1 ± 0.2 | 2.7 ± 0.1 | <0.001 |
| Total Phenolic Compounds | 127.39 ± 1.03 | 107 ± 1 | <0.001 | |||||
| Species | Caffeinated Coffee Extract | Decaffeinated Coffee Extract | Itraconazole | ||
|---|---|---|---|---|---|
| GC | SCG | GC | SCG | ||
| A. alternata | >1770.00 | >1100.00 | >1415.00 | >2400.00 | 0.50 |
| A. fumigatus | >1770.00 | >1100.00 | >1415.00 | >2400.00 | 2.00 |
| A. infectoria | >1770.00 | >1100.00 | >1415.00 | >2400.00 | 0.50 |
| A. niger | >1770.00 | >1100.00 | >1415.00 | >2400.00 | >16.00 |
| C. albicans | >1770.00 | >1100.00 | >1415.00 | >2400.00 | 0.06 |
| C. glabrata | >1770.00 | >1100.00 | >1415.00 | >2400.00 | 0.01 |
| C. krusei | 55.31 | 137.50 | 44.22 | 150.00 | 0.25 |
| C. parapsilosis | 110.63 | 275.00 | 44.22 | 150.00 | 0.03 |
| F. oxysporum | >1770.00 | >1100.00 | >1415.00 | >2400.00 | >16.00 |
| T. mentagrophytes | 27.66 | 137.50 | 22.11 | 300.00 | 0.03 |
| T. rubrum | 27.66 | 137.50 | 22.11 | 150.00 | 0.03 |
| Species | MFC (μg/mL) | |
|---|---|---|
| Caffeinated SCG Extract | Decaffeinated SCG Extract | |
| T. mentagrophytes | 137.50 | 300 |
| T. rubrum | 137.50 | 150 |
| Caffeinated SCG Extract | Decaffeinated SCG Extract | Positive Control | |
|---|---|---|---|
| Cytotoxic activity (GI50 and µg/mL) | Ellipticine | ||
| AGS | 55 ± 4 | 52 ± 2 | 1.20 ± 0.03 |
| CaCo2 | 214 ± 9 | 179 ± 10 | 1.20 ± 0.02 |
| MCF-7 | 207 ± 16 | 75.7 ± 0.3 | 1.00 ± 0.02 |
| NCI-H460 | 217 ± 18 | 228 ± 10 | 1.21 ± 0.02 |
| Cytotoxic activity (GI50 and µg/mL) | |||
| PLP2 | >400 | 240 ± 25 | 1.4 ± 0.1 |
| Anti-inflammatory activity (IC50 and µg/mL) | Dexametasone | ||
| RAW 264.7 | >400 | >400 | 6.3 ± 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calheiros, D.; Dias, M.I.; Calhelha, R.C.; Barros, L.; Ferreira, I.C.F.R.; Fernandes, C.; Gonçalves, T. Antifungal Activity of Spent Coffee Ground Extracts. Microorganisms 2023, 11, 242. https://doi.org/10.3390/microorganisms11020242
Calheiros D, Dias MI, Calhelha RC, Barros L, Ferreira ICFR, Fernandes C, Gonçalves T. Antifungal Activity of Spent Coffee Ground Extracts. Microorganisms. 2023; 11(2):242. https://doi.org/10.3390/microorganisms11020242
Chicago/Turabian StyleCalheiros, Daniela, Maria Inês Dias, Ricardo C. Calhelha, Lillian Barros, Isabel C. F. R. Ferreira, Chantal Fernandes, and Teresa Gonçalves. 2023. "Antifungal Activity of Spent Coffee Ground Extracts" Microorganisms 11, no. 2: 242. https://doi.org/10.3390/microorganisms11020242








