Clostridioides difficile in Pigs and Dairy Cattle in Northern Italy: Prevalence, Characterization and Comparison between Animal and Human Strains
Abstract
1. Introduction
2. Materials and Methods
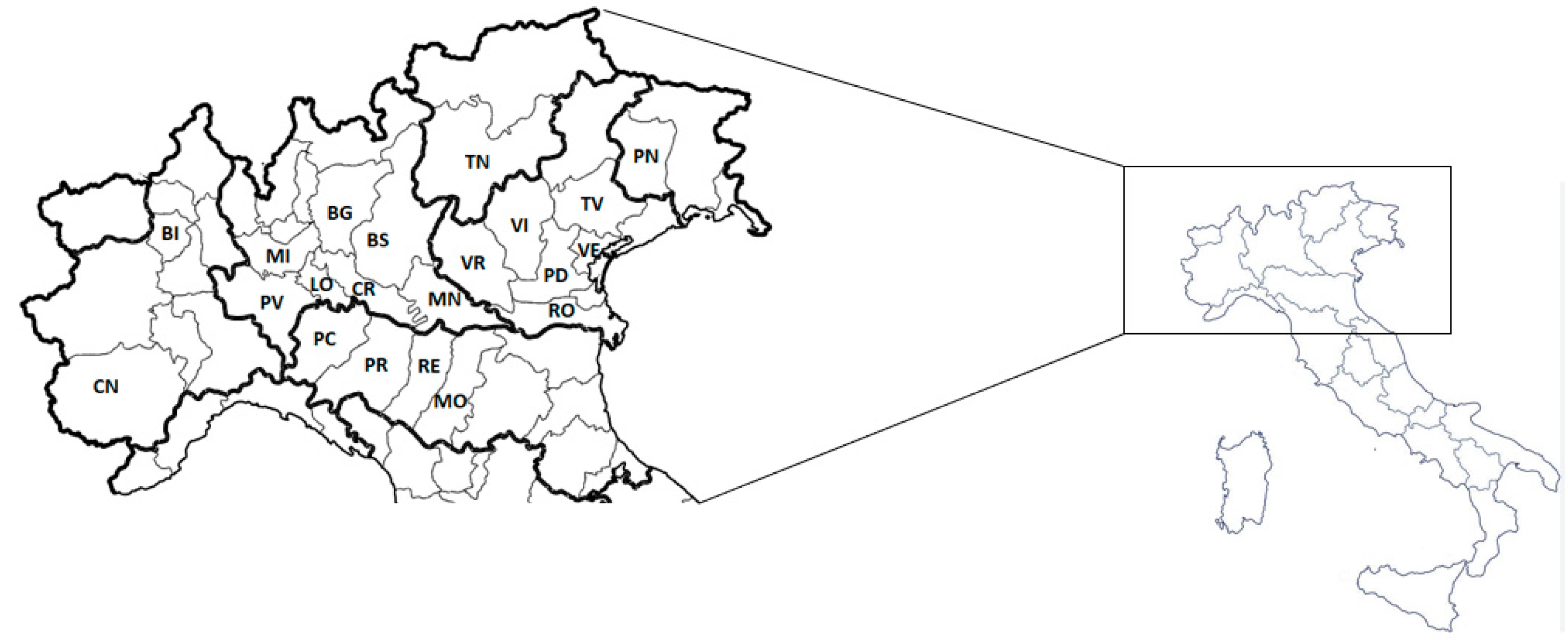
2.1. Collection of Animal Samples
2.1.1. Collection of Porcine Samples
2.1.2. Collection of Bovine Samples
2.2. Collection of Human Strains
2.3. C. difficile Sampling and Storage
2.4. C. difficile Isolation
2.5. DNA Extraction and C. difficile Identification
2.6. C. difficile Molecular Toxin Profile and Typing
2.7. Molecular Analysis of Resistance Mechanisms
2.8. Antimicrobial Susceptibility Testing
2.9. Statistical Analysis
3. Results
3.1. Sampling and C. difficile Isolation from Animals and Humans
3.2. C. difficile Molecular Toxin Profile and Typing
3.3. Antibiotic Susceptibility
3.4. Antibiotic Resistance Mechanisms
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Loo, V.G.; Bourgault, A.-M.; Poirier, L.; Lamothe, F.; Michaud, S.; Turgeon, N.; Toye, B.; Beaudoin, A.; Frost, E.H.; Gilca, R.; et al. Host and pathogen factors for Clostridium difficile infection and colonization. N. Engl. J. Med. 2011, 365, 1693–1703. [Google Scholar] [CrossRef] [PubMed]
- Asensio, Á.; Vallejo-Plaza, A.; Parra, L.M.; Ortí-Lucas, R. Epidemiology of Clostridioides difficile infection in hospitalized patients in Spain: An eight-year review (2012–2019). Enfermedades Infecc. y Microbiol. Clin. 2022, 40, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Feuerstadt, P.; Theriault, N.; Tillotson, G. The burden of CDI in the United States: A multifactorial challenge. BMC Infect. Dis. 2023, 23, 132. [Google Scholar] [CrossRef]
- Finn, E.; Andersson, F.L.; Madin-Warburton, M. Burden of Clostridioides difficile infection (CDI)—A systematic review of the epidemiology of primary and recurrent CDI. BMC Infect. Dis. 2021, 21, 456. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Tunis, M.; Frenette, C.; Katz, K.; Amaratunga, K.; Rose, S.R.; House, A.; Quach, C. Epidemiology of Clostridioides difficile infection in Canada: A six-year review to support vaccine decision-making. Can. Commun. Dis. Rep. 2019, 45, 191–211. [Google Scholar] [CrossRef] [PubMed]
- Fatima, R.; Aziz, M. The Hypervirulent Strain of Clostridium difficile: NAP1/B1/027—A Brief Overview. Cureus 2019, 11. [Google Scholar] [CrossRef]
- Kuijper, E.J.; Coignard, B.; Tüll, P. Emergence of Clostridium difficile-associated disease in North America and Europe. Clin. Microbiol. Infect. 2006, 12, 2–18. [Google Scholar] [CrossRef]
- Loo, V.G.; Poirier, L.; Miller, M.A.; Oughton, M.; Libman, M.D.; Michaud, S.; Bourgault, A.M.; Nguyen, T.; Frenette, C.; Kelly, M.; et al. A Predominantly Clonal Multi-Institutional Outbreak of Clostridium difficile—Associated Diarrhea with High Morbidity and Mortality. N. Engl. J. Med. 2005, 353, 2442–2449. [Google Scholar] [CrossRef]
- Candel-Pérez, C.; Ros-Berruezo, G.; Martínez-Graciá, C. A review of Clostridioides [Clostridium] difficile occurrence through the food chain. Food Microbiol. 2019, 77, 118–129. [Google Scholar] [CrossRef]
- Goorhuis, A.; Bakker, D.; Corver, J.; Debast, S.B.; Harmanus, C.; Notermans, D.W.; Bergwerff, A.A.; Dekker, F.W.; Kuijper, E.J. Emergence of Clostridium difficile infection due to a new hypervirulent strain, polymerase chain reaction ribotype 078. Clin. Infect. Dis. 2008, 47, 1162–1170. [Google Scholar] [CrossRef]
- Kachrimanidou, M.; Tzika, E.; Filioussis, G. Clostridioides (Clostridium) difficile in food-producing animals, horses and household pets: A comprehensive review. Microorganisms 2019, 7, 667. [Google Scholar] [CrossRef] [PubMed]
- De Roo, A.C.; Regenbogen, S.E. Clostridium difficile Infection: An Epidemiology Update. Clin. Colon. Rectal. Surg. 2020, 33, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Ofori, E.; Ramai, D.; Dhawan, M.; Mustafa, F.; Gasperino, J.; Reddy, M. Community-acquired Clostridium difficile: Epidemiology, ribotype, risk factors, hospital and intensive care unit outcomes, and current and emerging therapies. J. Hosp. Infect. 2018, 99, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.P.; Veenendaal, D.; Verhoef, L.; Bloembergen, P.; van Dissel, J.T.; Kuijper, E.J. Clinical and microbiological characteristics of community-onset Clostridium difficile infection in The Netherlands. Clin. Microbiol. Infect. 2009, 15, 1087–1092. [Google Scholar] [CrossRef]
- Knight, D.R.; Riley, T.V. Genomic delineation of zoonotic origins of Clostridium difficile. Front. Public Health 2019, 7, 164. [Google Scholar] [CrossRef]
- Rodriguez Diaz, C.; Seyboldt, C.; Rupnik, M. Non-human C. difficile reservoirs and sources: Animals, food, environment. Adv. Exp. Med. Biol. 2018, 8, 227–243. [Google Scholar]
- Bolton, D.; Marcos, P. The Environment, Farm Animals and Foods as Sources of Clostridioides difficile Infection in Humans. Foods 2023, 12, 1094. [Google Scholar] [CrossRef]
- Durovic, A.; Widmer, A.F.; Tschudin-Sutter, S. New insights into transmission of Clostridium difficile infection—Narrative review. Clin. Microbiol. Infect. 2018, 24, 483–492. [Google Scholar] [CrossRef]
- Alves, F.; Castro, R.; Pinto, M.; Nunes, A.; Pomba, C.; Oliveira, M.; Silveira, L.; Gomes, J.P.; Oleastro, M. Molecular epidemiology of Clostridioides difficile in companion animals: Genetic overlap with human strains and public health concerns. Front. Public Health 2022, 10, 1070258. [Google Scholar] [CrossRef]
- Hensgens, M.P.M.; Keessen, E.C.; Squire, M.M.; Riley, T.V.; Koene, M.G.J.; de Boer, E.; Lipman, L.J.A.; Kuijper, E.J. Clostridium difficile infection in the community: A zoonotic disease? Clin. Microbiol. Infect. 2012, 18, 635–645. [Google Scholar] [CrossRef]
- Knetsch, C.W.; Connor, T.R.; Mutreja, A.; van Dorp, S.M.; Sanders, I.M.; Browne, H.P.; Harris, D.; Lipman, L.; Keessen, E.C.; Corver, J.; et al. Whole genome sequencing reveals potential spread of Clostridium difficile between humans and farm animals in the Netherlands, 2002 to 2011. Eurosurveillance 2014, 19, 20954. [Google Scholar] [CrossRef] [PubMed]
- Knight, D.R.; Kullin, B.; Androga, G.O.; Barbut, F.; Eckert, C.; Johnson, S.; Spigaglia, P.; Tateda, K.; Tsai, P.; Riley, T.V. Evolutionary and genomic insights into Clostridioides difficile sequence type 11: A diverse zoonotic and antimicrobial-resistant lineage of global one health importance. mBio 2019, 10, e00446-19. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, C.; Taminiau, B.; Van Broeck, J.; Delmee, M.; Daube, G. Clostridium difficile in food and animals: A comprehensive review. Adv. Exp. Med. Biol. 2016, 932, 65–92. [Google Scholar] [PubMed]
- Tsai, C.S.; Hung, Y.P.; Lee, J.C.; Syue, L.; Hsueh, P.; Ko, W. Clostridioides difficile infection: An emerging zoonosis? Expert Rev. Anti-Infect. Ther. 2021, 19, 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Miyajima, F.; Roberts, P.; Ellison, L.; Pickard, D.J.; Martin, M.J.; Connor, T.R.; Harris, S.R.; Fairley, D.; Bamford, K.B.; et al. Emergence and global spread of epidemic healthcare-associated Clostridium difficile. Nat. Genet. 2013, 45, 109–113. [Google Scholar] [CrossRef]
- Knetsch, C.W.; Kumar, N.; Forster, S.C.; Connor, T.R.; Browne, H.P.; Harmanus, C.; Sanders, I.M.; Harris, S.R.; Turner, L.; Morris, T.; et al. Zoonotic transfer of Clostridium difficile harboring antimicrobial resistance between farm animals and humans. J. Clin. Microbiol. 2018, 56, e01384-17. [Google Scholar] [CrossRef]
- Mitchell, M.; Nguyen, S.V.; MacOri, G.; Bolton, D.; McMullan, G.; Drudy, D.; Fanning, S. Clostridioides difficile as a Potential Pathogen of Importance to One Health: A Review. Foodborne Pathog. Dis. 2022, 19, 806–816. [Google Scholar] [CrossRef]
- Moloney, G.; Eyre, D.W.; Mac Aogáin, M.; McElroy, M.C.; Vaughan, A.; Peto, T.E.A.; Crook, D.W.; Rogers, T.R. Human and porcine transmission of Clostridioides difficile Ribotype 078, Europe. Emerg. Infect. Dis. 2021, 27, 2294–2300. [Google Scholar] [CrossRef]
- Beres, C.; Colobatiu, L.; Tabaran, A.; Mihaiu, R.; Iuhas, C.; Mihaiu, M. Clostridioides difficile in Food-Producing Animals in Romania: First Study on the Prevalence and Antimicrobial Resistance. Antibiotics 2022, 11, 1194. [Google Scholar] [CrossRef]
- Moono, P.; Foster, N.F.; Hampson, D.J.; Knight, D.R.; Bloomfield, L.E.; Riley, T.V. Clostridium difficile Infection in Production Animals and Avian Species: A Review. Foodborne Pathog. Dis. 2016, 13, 647–655. [Google Scholar] [CrossRef]
- Uzal, F.A.; Navarro, M.A.; Asin, J.; Boix, O.; Ballarà-Rodriguez, I.; Gibert, X. Clostridial diarrheas in piglets: A review. Vet. Microbiol. 2023, 280, 109691. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Palacios, A.; Reid-Smith, R.J.; Staempfli, H.R.; Weese, J.S. Clostridium difficile survives minimal temperature recommended for cooking ground meats. Anaerobe 2010, 16, 540–542. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, C.; Avesani, V.; Van Broeck, J.; Taminiau, B.; Delmée, M.; Daube, G. Presence of Clostridium difficile in pigs and cattle intestinal contents and carcass contamination at the slaughterhouse in Belgium. Int. J. Food Microbiol. 2013, 166, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Rupnik, M.; Songer, J.G. Clostridium difficile: Its potential as a source of foodborne disease. Adv. Food Nutr. Res. 2010, 60, 53–66. [Google Scholar] [PubMed]
- Songer, J.G.; Trinh, H.T.; Killgore, G.E.; Thompson, A.D.; McDonald, L.C.; Limbago, B.M. Clostridium difficile in retail meat products, USA, 2007. Emerg. Infect. Dis. 2009, 15, 819–821. [Google Scholar] [CrossRef]
- Tan, D.T.; Mulvey, M.R.; Zhanel, G.G.; Bay, D.C.; Reid-Smith, R.J.; Janecko, N.; Golding, G.R. A Clostridioides difficile surveillance study of Canadian retail meat samples from 2016–2018. Anaerobe 2022, 74, 102551. [Google Scholar] [CrossRef]
- Tkalec, V.; Jamnikar-Ciglenecki, U.; Rupnik, M.; Vadnjal, S.; Zelenik, K.; Biasizzo, M. Clostridioides difficile in national food surveillance, Slovenia, 2015 to 2017. Eurosurveillance 2020, 25, 1900479. [Google Scholar] [CrossRef] [PubMed]
- Usui, M.; Maruko, A.; Harada, M.; Kawabata, F.; Sudo, T.; Noto, S.; Sato, T.; Shinagawa, M.; Takahashi, S.; Tamura, Y. Prevalence and characterization of Clostridioides difficile isolates from retail food products (vegetables and meats) in Japan. Anaerobe 2020, 61, 102132. [Google Scholar] [CrossRef]
- Imwattana, K.; Rodríguez, C.; Riley, T.V.; Knight, D.R. A species-wide genetic atlas of antimicrobial resistance in Clostridioides difficile. Microb. Genom. 2021, 7, 000696. [Google Scholar] [CrossRef]
- Dingle, K.E.; Didelot, X.; Quan, T.P.; Eyre, D.W.; Stoesser, N.; Marwick, C.A.; Coia, J.; Brown, D.; Buchanan, S.; Ijaz, U.Z.; et al. A role for tetracycline selection in recent evolution of agriculture-associated Clostridioides difficile pcr ribotype 078. mBio 2019, 10, e02790-18. [Google Scholar] [CrossRef]
- Imwattana, K.; Putsathit, P.; Collins, D.A.; Leepattarakit, T.; Kiratisin, P.; Riley, T.V.; Knight, D.R. Global evolutionary dynamics and resistome analysis of Clostridioides difficile ribotype 017. Microb. Genom. 2022, 8, 000792. [Google Scholar] [CrossRef] [PubMed]
- Debast, S.B.; Van Leengoed, L.A.M.G.; Goorhuis, A.; Harmanus, C.; Kuijper, E.J.; Bergwerff, A.A. Clostridium difficile PCR ribotype 078 toxinotype V found in diarrhoeal pigs identical to isolates from affected humans. Environ. Microbiol. 2009, 11, 505–511. [Google Scholar] [CrossRef]
- Spigaglia, P.; Mastrantonio, P.; Barbanti, F. Antibiotic resistances of Clostridium difficile. Adv. Exp. Med. Biology. 2018, 1050, 137–159. [Google Scholar] [CrossRef]
- O’Grady, K.; Knight, D.R.; Riley, T.V. Antimicrobial resistance in Clostridioides difficile. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 2459–2478. [Google Scholar] [CrossRef] [PubMed]
- 17604 ISO/FDIS; Microbiology of the Food Chain—Carcass Sampling for Microbiological Analysis, 2nd ed. ISO—International Organization for Standardization: Geneva, Switzerland, 2015.
- Lemee, L.; Dhalluin, A.; Testelin, S.; Mattrat, M.; Maillard, K.; Lemeland, J.; Pons, J. Multiplex PCR targeting tpi (triose phosphate isomerase), tcdA (toxin A), and tcdB (toxin B) genes for toxigenic culture of Clostridium difficile. J. Clin. Microbiol. 2004, 42, 5710–5714. [Google Scholar] [CrossRef]
- ECDC—European Centre for Disease Prevention and Control. Laboratory Procedures for Diagnosis and Typing of Human Clostridium difficile Infection; ECDC Technical Report; ECDC—European Centre for Disease Prevention and Control: Stockholm, Sweden, 2018.
- Indra, A.; Huhulescu, S.; Schneeweis, M.; Hasenberger, P.; Kernbichler, S.; Fiedler, A.; Wewalka, G.; Allerberger, F.; Kuijper, E.J. Characterization of Clostridium difficile isolates using capillary gel electrophoresis-based PCR ribotyping. J. Med. Microbiol. 2008, 57 Pt 11, 1377. [Google Scholar] [CrossRef]
- Spigaglia, P.; Mastrantonio, P. Comparative analysis of Clostridium difficile clinical isolates belonging to different genetic lineages and time periods. J. Med. Microbiol. 2004, 53, 1129–1136. [Google Scholar] [CrossRef]
- Patterson, A.J.; Colangeli, R.; Spigaglia, P.; Scott, K.P. Distribution of specific tetracycline and erythromycin resistance genes in environmental samples assessed by macroarray detection. Environ. Microbiol. 2007, 9, 703–715. [Google Scholar] [CrossRef]
- Spigaglia, P.; Barbanti, F.; Mastrantonio, P. New variants of the tet(M) gene in Clostridium difficile clinical isolates harbouring Tn916-like elements. J. Antimicrob. Chemother. 2006, 57, 1205–1209. [Google Scholar] [CrossRef]
- Spigaglia, P.; Barbanti, F.; Mastrantonio, P.; Brazier, J.S.; Barbut, F.; Delmee, M.; Kuijper, E.; R Poxton, I.; on Behalf of the European Study Group. On Esgcd Fluoroquinolone resistance in Clostridium difficile isolates from a prospective study of C. difficile infections in Europe. J. Med. Microbiol. 2008, 57, 784–789. [Google Scholar] [CrossRef]
- CLSI—Clinical and Laboratory Standards Institute. Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria, 7th ed.; Approved Standard M11-A7; CLSI—Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2007. [Google Scholar]
- EUCAST—European Committee on Antimicrobial Susceptibility Testing. Clinical Breakpoint Tables, Version 9.0. 2015. Available online: www.eucast.org/clinical_breakpoints (accessed on 1 March 2023).
- Freeman, J.; Vernon, J.; Pilling, S.; Morris, K.; Nicholson, S.; Shearman, S.; Longshaw, C.; Wilcox, M.H. The ClosER study: Results from a three-year pan-European longitudinal surveillance of antibiotic resistance among prevalent Clostridium difficile ribotypes, 2011–2014. Clin. Microbiol. Infect. 2018, 24, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Arruda, P.H.E.; Madson, D.M.; Ramirez, A.; Rowe, E.; Lizer, J.T.; Songer, J.G. Effect of age, dose and antibiotic therapy on the development of Clostridium difficile infection in neonatal piglets. Anaerobe 2013, 22, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Chan, G.; Farzan, A.; DeLay, J.; McEwen, B.; Prescott, J.F.; Friendship, R.M. A retrospective study on the etiological diagnoses of diarrhea in neonatal piglets in Ontario, Canada, between 2001 and 2010. Can. J. Vet. Res. 2013, 77, 254–260. [Google Scholar]
- Yaeger, M.J.; Kinyon, J.M.; Songer, J.G. A prospective, case control study evaluating the association between Clostridium difficile toxins in the colon of neonatal swine and gross and microscopic lesions. J. Vet. Diagnostic. Investig. 2007, 19, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Songer, J.G.; Uzal, F.A. Clostridial enteric infections in pigs. J. Vet. Diagnostic. Investig. 2005, 17, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Keessen, E.C.; Hopman, N.E.M.; Van Leengoed, L.A.M.G.; van Asten, A.J.A.M.; Hermanus, C.; Kuijper, E.J.; Lipman, L.J.A. Evaluation of four different diagnostic tests to detect Clostridium difficile in piglets. J. Clin. Microbiol. 2011, 49, 1816–1821. [Google Scholar] [CrossRef]
- Squire, M.M.; Carter, G.P.; Mackin, K.E.; Chakravorty, A.; Noren, T.; Elliott, B.; Lyras, D.; Riley, T.V. Novel molecular type of Clostridium difficile in neonatal pigs, Western Australia. Emerg. Infect. Dis. 2013, 19, 790–792. [Google Scholar] [CrossRef]
- Vidal, A.; Martín-Valls, G.E.; Tello, M.; Mateu, E.; Martín, M.; Darwich, L. Prevalence of enteric pathogens in diarrheic and non-diarrheic samples from pig farms with neonatal diarrhea in the North East of Spain. Vet. Microbiol. 2019, 237, 108419. [Google Scholar] [CrossRef]
- Avbersek, J.; Janezic, S.; Pate, M.; Rupnik, M.; Zidaric, V.; Logar, K.; Vengust, M.; Zemljic, M.; Pirs, T.; Ocepek, M. Diversity of Clostridium difficile in pigs and other animals in Slovenia. Anaerobe 2009, 15, 252–255. [Google Scholar] [CrossRef]
- Krutova, M.; Zouharova, M.; Matejkova, J.; Tkadlec, J.; Krejčí, J.; Faldyna, M.; Nyc, O.; Bernardy, J. The emergence of Clostridium difficile PCR ribotype 078 in piglets in the Czech Republic clusters with Clostridium difficile PCR ribotype 078 isolates from Germany, Japan and Taiwan. Int. J. Med. Microbiol. 2018, 308, 770–775. [Google Scholar] [CrossRef]
- Norén, T.; Johansson, K.; Unemo, M. Clostridium difficile PCR ribotype 046 is common among neonatal pigs and humans in Sweden. Clin. Microbiol. Infect. 2014, 20, O2–O6. [Google Scholar] [CrossRef] [PubMed]
- Schneeberg, A.; Neubauer, H.; Schmoock, G.; Baier, S.; Harlizius, J.; Nienhoff, H.; Brase, K.; Zimmermann, S.; Seyboldt, C. Clostridium difficile genotypes in piglet populations in Germany. J. Clin. Microbiol. 2013, 51, 3796–3803. [Google Scholar] [CrossRef] [PubMed]
- Knight, D.R.; Squire, M.M.; Riley, T.V. Nationwide surveillance study of Clostridium difficile in Australian neonatal pigs shows high prevalence and heterogeneity of PCR ribotypes. Appl. Environ. Microbiol. 2015, 81, 119–123. [Google Scholar] [CrossRef] [PubMed]
- O’Shaughnessy, R.A.; Habing, G.G.; Gebreyes, W.A.; Bowman, A.S.; Weese, J.S.; Rousseau, J.; Stull, J.W. Clostridioides difficile on Ohio swine farms (2015): A comparison of swine and human environments and assessment of on-farm risk factors. Zoonoses Public Health 2019, 66, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Abay, S.; Ahmed, E.F.; Aydin, F.; Müştak, H.K. Presence of Clostridioides difficile in cattle feces, carcasses, and slaughterhouses: Molecular characterization and antibacterial susceptibility of the recovered isolates. Anaerobe 2022, 75, 102575. [Google Scholar] [CrossRef]
- Bandelj, P.; Blagus, R.; Briski, F.; Frlic, O.; Vergles Rataj, A.; Rupnik, M.; Ocepek, M.; Vengust, M. Identification of risk factors influencing Clostridium difficile prevalence in middle-size dairy farms. Vet. Res. 2016, 237, 108419. [Google Scholar] [CrossRef]
- Doosti, A.; Mokhtari-Farsani, A. Study of the frequency of Clostridium difficile tcdA, tcdB, cdtA and cdtB genes in feces of Calves in south west of Iran. Ann. Clin. Microbiol. Antimicrob. 2014, 13, 21. [Google Scholar] [CrossRef]
- Mcnamara, S.E.; Abdujamilova, N.; Somsel, P.; Gordoncillo, M.J.; DeDecker, J.M.; Bartlett, P.C. Carriage of Clostridium difficile and Other Enteric Pathogens Among a 4-H Avocational Cohort. Zoonoses Public Health 2011, 58, 192–199. [Google Scholar] [CrossRef]
- Rodriguez, C.; Hakimi, D.E.; Vanleyssem, R.; Taminiau, B.; Van Broeck, J.; Delmée, M.; Korsak, N.; Daube, G. Clostridium difficile in beef cattle farms, farmers and their environment: Assessing the spread of the bacterium. Vet. Microbiol. 2017, 210, 183–187. [Google Scholar] [CrossRef]
- Rodriguez-Palacios, A.; Stämpfli, H.R.; Duffield, T.; Peregrine, A.S.; Trotz-Williams, L.A.; Arroyo, L.G.; Brazier, J.S.; Weese, J.S. Clostridium difficile PCR ribotypes in calves, Canada. Emerg. Infect. Dis. 2006, 12, 1730–1736. [Google Scholar] [CrossRef]
- Squire, M.M.; Riley, T.V. Clostridium difficile Infection in Humans and Piglets: A ‘One Health’ Opportunity. Curr. Top Microbiol. Immunol. 2013, 365, 299–314. [Google Scholar] [CrossRef] [PubMed]
- Knight, D.R.; Riley, T.V. Prevalence of gastrointestinal Clostridium difficile carriage in australian sheep and lambs. Appl. Environ. Microbiol. 2013, 79, 5689–5692. [Google Scholar] [CrossRef] [PubMed]
- Cho, A.; Byun, J.W.; Kim, J.W.; Oh, S.; Lee, M.; Kim, H. Low prevalence of Clostridium difficile in slaughter pigs in Korea. J. Food Prot. 2015, 78, 1034–1036. [Google Scholar] [CrossRef]
- Licciardi, C.; Primavilla, S.; Roila, R.; Lupattelli, A.; Farneti, S.; Blasi, G.; Petruzzelli, A.; Drigo, I.; Di Raimo Marrocchi, E. Prevalence, molecular characterization and antimicrobial susceptibility of Clostridioides difficile isolated from pig carcasses and pork products in central italy. Int. J. Environ. Res. Public Health 2021, 18, 11368. [Google Scholar] [CrossRef]
- Magistrali, C.F.; Maresca, C.; Cucco, L.; Bano, L.; Drigo, I.; Filippini, G.; Dettori, A.; Broccatelli, S.; Pezzotti, G. Prevalence and risk factors associated with Clostridium difficile shedding in veal calves in Italy. Anaerobe 2015, 33, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Knight, D.R.; Putsathit, P.; Elliott, B.; Riley, T.V. Contamination of Australian newborn calf carcasses at slaughter with Clostridium difficile. Clin. Microbiol. Infect. 2016, 22, 266.e1–266.e7. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Palacios, A.; Koohmaraie, M.; Lejeune, J.T. Prevalence, enumeration, and antimicrobial agent resistance of Clostridium difficile in cattle at harvest in the United States. J. Food Prot. 2011, 74, 1618–1624. [Google Scholar] [CrossRef]
- Houser, B.A.; Soehnlen, M.K.; Wolfgang, D.R. Prevalence of Clostridium difficile toxin genes in the feces of veal calves and incidence of ground veal contamination. Foodborne Pathog. Dis. 2012, 9, 32–36. [Google Scholar] [CrossRef]
- Freeman, J.; Vernon, J.; Pilling, S.; Morris, K.; Nicolson, S.; Shearman, S.; Clark, E.; Palacios-Fabrega, J.A.; Wilcox, M. Five-year Pan-European, longitudinal surveillance of Clostridium difficile ribotype prevalence and antimicrobial resistance: The extended ClosER study. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 169–177. [Google Scholar] [CrossRef]
- Barbanti, F.; Spigaglia, P. Microbiological characteristics of human and animal isolates of Clostridioides difficile in Italy: Results of the Istituto Superiore di Sanità in the years 2006–2016. Anaerobe 2020, 61, 102136. [Google Scholar] [CrossRef]
- Bandelj, P.; Harmanus, C.; Blagus, R.; Cotman, M.; Kuijper, E.J.; Ocepek, M.; Vengust, M. Quantification of Clostridioides (Clostridium) difficile in feces of calves of different age and determination of predominant Clostridioides difficile ribotype 033 relatedness and transmission between family dairy farms using multilocus variable-number ta. BMC Vet. Res. 2018, 14, 298. [Google Scholar] [CrossRef] [PubMed]
- Blasi, F.; Lovito, C.; Albini, E.; Bano, L.; Dalmonte, G.; Drigo, I.; Maresca, C.; Massacci, F.R.; Orsini, S.; Primavilla, S.; et al. Clostridioides difficile in calves in central italy: Prevalence, molecular typing, antimicrobial susceptibility and association with antibiotic administration. Animals 2021, 11, 515. [Google Scholar] [CrossRef] [PubMed]
- Masarikova, M.; Simkova, I.; Plesko, M.; Eretova, V.; Krutova, M.; Cizek, A. The colonisation of calves in czech large-scale dairy farms by clonally-related Clostridioides difficile of the sequence type 11 represented by ribotypes 033 and 126. Microorganisms 2020, 8, 901. [Google Scholar] [CrossRef] [PubMed]
- Romano, V.; Albanese, F.; Dumontet, S.; Krovacek, K.; Petrini, O.; Pasquale, V. Prevalence and genotypic characterization of Clostridium difficile from ruminants in Switzerland. Zoonoses Public Health 2012, 59, 545–548. [Google Scholar] [CrossRef] [PubMed]
- Rupnik, M.; Janezic, S. An update on Clostridium difficile toxinotyping. J. Clin. Microbiol. 2016, 54, 13–18. [Google Scholar] [CrossRef]
- Eckert, C.; Emirian, A.; Le Monnier, A.; Cathala, L.; De Montclos, H.; Goret, J.; Berger, P.; Petit, A.; De Chevigny, A.; Jean-Pierre, H.; et al. Prevalence and pathogenicity of binary toxin-positive Clostridium difficile strains that do not produce toxins A and B. New Microbes New Infect. 2015, 3, 12–17. [Google Scholar] [CrossRef]
- Grandesso, S.; Arena, F.; Eseme, F.E.; Panese, S.; Henrici De Angelis, L.; Spigaglia, P.; Barbanti, F.; Rossolini, G.M. Clostridium difficile ribotype 033 colitis in a patient following broad-spectrum antibiotic treatment for KPC-producing Klebsiella pneumoniae infection, Italy. New Microbiol. 2016, 39, 235–236. [Google Scholar]
- Rupnik, M. Heterogeneity of large clostridial toxins: Importance of Clostridium difficile toxinotypes. FEMS Microbiol. Rev. 2008, 32, 541–555. [Google Scholar] [CrossRef]
- Rupnik, M.; Brazier, J.S.; Duerden, B.I.; Grabnar, M.; Stubbs, S.L.J. Comparison of toxinotyping and PCR ribotyping of Clostridium difficile strains and description of novel toxinotypes. Microbiology 2001, 147, 439–447. [Google Scholar] [CrossRef]
- Stojković, V.; Ulate, M.F.; Hidalgo-Villeda, F.; Aguilar, E.; Monge-Cascante, C.; Pizarro-Guajardo, M.; Tsai, K.; Tzoc, E.; Camorlinga, M.; Paredes-Sabja, D.; et al. Cfr(B), cfr(C), and a New cfr-Like Gene, cfr(E), in Clostridium difficile Strains Recovered across Latin America. Antimicrob. Agents Chemother. 2019, 64, e01074-19. [Google Scholar] [CrossRef]
- Lebel, S.; Bouttier, S.; Lambert, T. The cme gene of Clostridium difficile confers multidrug resistance in Enterococcus faecalis. FEMS Microbiol. Lett. 2004, 238, 93–100. [Google Scholar] [PubMed]
- Pirš, T.; Avberšek, J.; Zdovc, I.; Krt, B.; Andlovic, A.; Lejko-Zupanc, T.; Rupnik, M.; Ocepek, M. Antimicrobial susceptibility of animal and human isolates of Clostridium difficile by broth microdilution. J. Med. Microbiol. 2013, 62, 1478–1485. [Google Scholar] [CrossRef] [PubMed]
- Rivas, L.; Dupont, P.Y.; Gilpin, B.J.; Cornelius, A.J. Isolation and characterization of Clostridium difficile from a small survey of wastewater, food and animals in New Zealand. Lett. Appl. Microbiol. 2020, 70, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.Z.; Li, W.G.; Liu, Y.Q.; Gu, W.; Zhang, Q.; Li, H.; Liu, Z.; Zhang, X.; Wu, Y.; Lu, J. The molecular characters and antibiotic resistance of Clostridioides difficile from economic animals in China. BMC Microbiol. 2020, 20, 70. [Google Scholar] [CrossRef]
- Spigaglia, P. Recent advances in the understanding of antibiotic resistance in Clostridium difficile infection. Ther. Adv. Infect. Dis. 2016, 3, 23–42. [Google Scholar] [CrossRef] [PubMed]
- AIFA—Agenzia Italiana del Farmaco, Italian Medicines Agency. National Report on Antibiotics Use in Italy—Year 2019; The Medicines Utilisation Monitoring Centre: Rome, Italy, 2020.
- EMA, European Medicines Agency. Sales of veterinary antimicrobial agents in 31 European countries in 2019 and 2020. In European Surveillance of Veterinary Antimicrobial Consumption (ESVAC); EMA: Amsterdam, The Netherlands, 2021; p. 58183. [Google Scholar]
- Owens, R.C.; Donskey, C.J.; Gaynes, R.P.; Loo, V.G.; Muto, C.A. Antimicrobial-associated risk factors for Clostridium difficile infection. Clin. Infect. Dis. 2008, 46 (Suppl. S1), S19–S31. [Google Scholar] [CrossRef]
- Gustafsson, A.; Båverud, V.; Gunnarsson, A.; Pringle, J.; Franklin, A. Study of faecal shedding of Clostridium difficile in horses treated with penicillin. Equine Vet. J. 2004, 36, 180–182. [Google Scholar] [CrossRef]

| Investigation | Animal Species (Type of Sample) | Age Class (Clinical Data) | N. Samples Tested | N. Positive (%) | Ribotypes (N. of Strains) |
|---|---|---|---|---|---|
| Passive surveillance on neonatal animals | Swine (feces/intestinal content) | suckling piglet in the first 2 weeks of life (live animals with diarrhea or animals that had died with enterocolitis) | 493 | 143 (29.0%) | 078 (130), 620 (4), 066/2 (3), 068 (2), 126 (2), 085 (1), 569 (1) |
| Bovine (feces/intestinal content) | calves in the first 3 weeks of life (live animals with diarrhea or animals that had died with enterocolitis) | 140 | 2 (1.4%) | 033 (1), 078 (1) | |
| Cross-sectional study at farms | Swine (feces) | suckling piglets in the first 2 weeks of life (with diarrhea) | 179 | 39 (21.8%) | 078 (32), 126 (3), 569 (2), 620 (2) |
| suckling piglets in the first 2 weeks of life (without diarrhea) | 271 | 51 (18.8%) | 078 (41), 620 (5), 126 (3), 068 (1), 569 (1) | ||
| weaned piglets | 45 | 2 (4.4%) | 078 (2) | ||
| grower pigs | 45 | 0 (0.0%) | |||
| finisher pigs | 90 | 1 (1.1%) | 001 (1) | ||
| breeding sows | 90 | 12 (13.3%) | 078 (12) | ||
| Bovine (feces) | calves in the first 3 weeks of life (with diarrhea) | 51 | 3 (5.9%) | 033 (2), 078 (1) | |
| calves in the first 3 weeks of life (without diarrhea) | 99 | 7 (7.1%) | 126 (3), 033 (2), 078 (1), 045/2 (1) | ||
| 2–3-month-old heifers | 30 | 0 (0.0%) | |||
| 4–5-month-old heifers | 30 | 1 (3.3%) | 078 (1) | ||
| 6–12-month-old heifers | 30 | 1 (3.3%) | 033 (1) | ||
| 13–18-month-old heifers | 30 | 0 (0.0%) | |||
| 19–24-month-old heifers | 30 | 1 (3.3%) | 033 (1) | ||
| primiparous cows | 30 | 0 (0.0%) | |||
| pluriparous cows | 30 | 0 (0.0%) | |||
| Cross-sectional study at slaughterhouses | Swine (intestinal content) | Italian heavy pig (160–180 Kg b.w.) | 113 | 2 (1.8%) | 078 (1), 005 (1) |
| Swine (carcass swab) | Italian heavy pig (160–180 Kg b.w.) | 113 | 0 (0.0%) | ||
| Bovine (intestinal content) | dairy cows | 100 | 0 (0.0%) | ||
| Bovine (carcass swab) | dairy cows | 100 | 2 (2.0%) | 126 (1) PR23597 (1) | |
| Tot. | 2139 | 267 (12.5%) |
| Onset CDI § (N. of Strains) | Age of Patients | Gender of Patients * (N. of Strains) | PCR-Ribotype | N. of Strains |
|---|---|---|---|---|
| HA-CDI (61) | 62 | M (1) | 001 | 1 |
| 78 | F (1) | 002 | 1 | |
| 76–89 | M (2), F (2) | 005 | 4 | |
| 87 | F (1) | 012 | 1 | |
| 35–99 | M (4), F (1) | 014 | 5 | |
| 65–92 | M (6), F (19) | 018 | 25 | |
| 59–97 | M (3), F (5) | 078 | 8 | |
| 76–89 | M (2) | 085 | 2 | |
| 35–82 | M (1), F (1) | 126 | 2 | |
| 54 | M (1) | 220 | 1 | |
| 84 | F (1) | 241 | 1 | |
| 68 | M (1) | 427 | 1 | |
| 79 | F (1) | 446 | 1 | |
| 81 | F (1) | 449 | 1 | |
| 53–79 | F (2) | 607 | 2 | |
| 92 | M (1) | 620 | 1 | |
| 60 | F (1) | 743 | 1 | |
| 81 | F (1) | AI-82/1 | 1 | |
| 80–81 | M (2) | PR18626 | 2 | |
| CA-CDI (25) | 65–81 | F (3) | 002 | 3 |
| 74 | F (1) | 003 | 1 | |
| 78 | M (1) | 005 | 1 | |
| 96 | F (1) | 014 | 1 | |
| 51–91 | M (2), F (5) | 018 | 7 | |
| 84–86 | F (2) | 020 | 2 | |
| 81 | F (2) | 054 | 2 | |
| 1 | F (1) | 087 | 1 | |
| 1 | M (1) | 106 | 1 | |
| 54 | M (1) | 220 | 1 | |
| 42–85 | F (2) | 425 | 2 | |
| 79–86 | M (2) | 569 | 2 | |
| 95 | F (1) | 607 | 1 | |
| LTCFs (11) | 93–95 | F (2) | 014 | 2 |
| 77–95 | M (1), F (5) | 018 | 6 | |
| 97 | F (1) | 023 | 1 | |
| 92 | M (1) | 033/1 | 1 | |
| 87 | F (1) | 126 | 1 |
| Origin | N. of Strains (Species) | Toxin Genes Profile * | PCR-Ribotypes (N. of Strains) |
|---|---|---|---|
| Animal | 252 (243 porcine 9 bovine) | tcdA+/tcdB+/cdtA+/cdtB+ | 045 (1), 066/2 (3), 078 (225), 126 (12), 620 (11) |
| 7 (bovine) | tcdA+/tcdB−/cdtA+/cdtB+ | 033 (7) | |
| 6 (porcine) | tcdA+/tcdB+/cdtA−/cdtB− | 001 (1), 005 (1), 569 (4) | |
| 2 (1 porcine 1 bovine) | tcdA−/tcdB−/cdtA−/cdtB− | 085 (1), PR23597 (1) | |
| Human | 16 | tcdA+/tcdB+/cdtA+/cdtB+ | 023 (1), 033/1 (1), 078 (8), 126 (3), 427 (1), 620 (1), 743 (1) |
| 79 | tcdA+/tcdB+/cdtA−/cdtB− | 001 (1), 002 (4), 003 (1), 005 (5), 012 (1), 014 (8), 018 (38), 020 (2), 054 (2), 087 (1), 106 (1), 220 (2), 241 (1), 425 (2), 446 (1), 449 (1), 569 (2), 607 (3), AI-82/1 (1), PR18626 (2) | |
| 2 | tcdA−/tcdB−/cdtA−/cdtB− | 085 (2) |
| C. difficile RT | Animal Species (N. of Strains and Status) | Human CDI Onset * (N. of Strains) |
|---|---|---|
| 001 | Swine (1 asymptomatic) | HA-CDI (1) |
| 005 | Swine (1 asymptomatic) | CA-CDI (1) HA-CDI (4) |
| 033 | Cattle (3 symptomatic, 4 asymptomatic) | - |
| 045 | Cattle (1 asymptomatic) | - |
| 066/2 | Swine (3 symptomatic) | - |
| 078 | Swine (165 symptomatic, 56 asymptomatic) | HA-CDI (8) |
| Cattle (2 symptomatic, 2 asymptomatic) | ||
| 085 | Swine (1 symptomatic) | HA-CDI (2) |
| 126 | Swine (8 symptomatic) | HA-CDI (2) LTCF (1) |
| Cattle (4 asymptomatic) | ||
| 569 | Swine (3 symptomatic, 1 asymptomatic) | CA-CDI (2) |
| 620 | Swine (6 symptomatic, 5 asymptomatic) | HA-CDI (1) |
| PR23597 | Cattle (1 Asymptomatic) | - |
| Erythromycin (Breakpoint: 8 mg/L) | |||||
|---|---|---|---|---|---|
| Origin | MIC Range (µg/mL) | MIC 90 (µg/mL) | MIC 50 (µg/mL) | N. of Resistant Strains (%) | Ribotypes (N. of Strains) |
| Human | ≤0.016–≥256 | ≥256 | ≥256 | 59 (62%) | 012 (1) 014 (1) 018 (38) 078 (7) 085 (2) 126 (3) 220 (2) 569 (2) 607 (2) 620 (1) |
| Porcine | 0.25–≥256 | ≥256 | ≥256 | 130 (93%) | 078 (113) 085 (1) 126 (4) 569 (4) 620 (8) |
| Bovine | 0.125–≥256 | ≥256 | 0.25 | 7 (47%) | 078 (4) 126 (3) |
| Moxifloxacin (Breakpoint: 8 mg/L) | |||||
| Origin | MIC range (µg/mL) | MIC 90 (µg/mL) | MIC 50 (µg/mL) | N. of resistant strains (%) | Ribotypes (n. of strains) |
| Human | 0.38–≥32 | ≥32 | 4 | 46 (48%) | 012 (1) 014 (1) 018 (37) 078 (3) 126 (2) 607 (2) |
| Porcine | 0.25–≥32 | ≥32 | 8 | 71 (52%) | 066/2 (3) 078 (57) 085 (1) 126 (3) 620 (7) |
| Bovine | 0.25–≥32 | ≥32 | 0.5 | 2 (13%) | 045 (1) 078 (1) |
| Tetracycline (Breakpoint: 16 mg/L) | |||||
| Origin | MIC range (µg/mL) | MIC 90 (µg/mL) | MIC 50 (µg/mL) | N. of resistant strains (%) | Ribotypes (n. of strains) |
| Human | ≤0.016–16 | 3 | 0.047 | 1 (1%) | 220 (1) |
| Porcine | 0.023–12 | 6 | 3 | 0 | - |
| Bovine | 0.032–8 | 4 | 0.064 | 0 | - |
| Metronidazole (Breakpoint: 2 mg/L) | |||||
| Origin | MIC range (µg/mL) | MIC 90 (µg/mL) | MIC 50 (µg/mL) | N. of resistant strains (%) | Ribotypes (n. of strains) |
| Human | ≤0.016–0.32 | 0.094 | 0.047 | 0 | - |
| Porcine | ≤0.016–0.125 | 0.094 | 0.047 | 0 | - |
| Bovine | ≤0.016–0.19 | 0.125 | 0.064 | 0 | - |
| Amoxycillin (Breakpoint: 16 mg/L) | |||||
| Origin | MIC range (µg/mL) | MIC 90 (µg/mL) | MIC 50 (µg/mL) | N. of resistant strains (%) | Ribotypes (n. of strains) |
| Human | 0.064–4 | 1 | 0.038 | 0 | - |
| Porcine | 0.094–0.047 | 0.38 | 0.25 | 0 | - |
| Bovine | 0.125–0.5 | 0.5 | 0.125 | 0 | - |
| Vancomycin (Breakpoint: 2 mg/L) | |||||
| Origin | MIC range (µg/mL) | MIC 90 (µg/mL) | MIC 50 (µg/mL) | N. of resistant strains (%) | Ribotypes (n. of strains) |
| Human | 0.75–2 | 2 | 1.5 | 0 | - |
| Porcine | 0.5–1.5 | 1.5 | 1.5 | 0 | - |
| Bovine | 0.75–1.5 | 1.5 | 1.5 | 0 | - |
| Origin | Antibiotic Resistance Molecular Profile a | PCR-Ribotypes (N. of Strains) c |
|---|---|---|
| Porcine | Thr82-Ile (25) | 066/2 (2), 078 (23), 126 (1) |
| Thr82-Ile + ermB (6) | 078 (5) | |
| Thr82-Ile + ermB + tetM + tetO (5) | 078 (4), 126 (1) | |
| Thr82-Ile + ermB + tetM + tetW (2) | 078 (2) | |
| Thr82-Ile + ermB + tetM + tetO + tetW (2) | 078 (2) | |
| Thr82-Ile + tetM (9) | 066/2 (1), 078 (7), 620 (1) | |
| Thr82-Ile + tetM + tetO (18) | 078 (13), 620 (5) | |
| Thr82-Ile + tetM + tetO + tetW (3) | 126 (2), 620 (1) | |
| Thr82-Ile + ermQ (1) | 078 (1) | |
| Thr82-Val + tetM (1) | 085 (1) | |
| ermB (9) | 078 (9) | |
| ermB + tetM + tetO (2) | 078 (2) | |
| ermB + tetM + tetO + tetW (2) | 078 (2) | |
| tetM (1) | 078 (1) | |
| tetM + tetO (11) | 078 (10), 620 (1) | |
| tetO (1) | 569 (1) | |
| No resistance genes (37) b | 078 (34), 569 (3) | |
| Bovine | Thr82-Ile (2) | 045 (1), 078 (1) |
| ermB (1) | 126 (1) | |
| ermB + tetM + tetO (1) | 126 (1) | |
| ermB + tetM + tetO + tetW (1) | 126 (1) | |
| tetM + tetO + tetW (1) | 078 (1) | |
| No resistance genes (2) b | 078 (2) |
| Onset (N. of Strains) | Mechanisms of Resistance (N. of Strains) * | PCR-Ribotypes (N. of Strains) |
|---|---|---|
| HA-CDI (43) | Thr82Ile (24) | 002 (1), 014 (1), 018 (19), 078 (2), 607 (1) |
| Thr82Ile + ermB (5) | 018 (4), 126 (1) | |
| Thr82Ile + ermB + tetM (1) | 078 (1) | |
| Thr82-Ile + ermQ (2) | 018 (2) | |
| ermB (4) | 012 (1), 078 (1), 085 (2) | |
| ermB + tetM (2) | 078 (1), 220 (1) | |
| tetM + tetO (3) | 078 (2), 126 (1) | |
| No substitutions nor resistance genes (2) § | 078 (1), 620 (1) | |
| CA-CDI (11) | Thr82Ile (8) | 018 (7), 607 (1) |
| ermB + tetM (1) | 220 (1) | |
| ermQ (1) | 569 (1) | |
| No substitutions nor resistance genes (1) § | 569 (1) | |
| LTCF (7) | Thr82Ile (6) | 018 (5), 126 (1) |
| Thr82-Ile + ermC + tetM + tetW (1) | 018 (1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spigaglia, P.; Barbanti, F.; Faccini, S.; Vescovi, M.; Criscuolo, E.M.; Ceruti, R.; Gaspano, C.; Rosignoli, C. Clostridioides difficile in Pigs and Dairy Cattle in Northern Italy: Prevalence, Characterization and Comparison between Animal and Human Strains. Microorganisms 2023, 11, 1738. https://doi.org/10.3390/microorganisms11071738
Spigaglia P, Barbanti F, Faccini S, Vescovi M, Criscuolo EM, Ceruti R, Gaspano C, Rosignoli C. Clostridioides difficile in Pigs and Dairy Cattle in Northern Italy: Prevalence, Characterization and Comparison between Animal and Human Strains. Microorganisms. 2023; 11(7):1738. https://doi.org/10.3390/microorganisms11071738
Chicago/Turabian StyleSpigaglia, Patrizia, Fabrizio Barbanti, Silvia Faccini, Mariella Vescovi, Enrico Maria Criscuolo, Rossella Ceruti, Clara Gaspano, and Carlo Rosignoli. 2023. "Clostridioides difficile in Pigs and Dairy Cattle in Northern Italy: Prevalence, Characterization and Comparison between Animal and Human Strains" Microorganisms 11, no. 7: 1738. https://doi.org/10.3390/microorganisms11071738
APA StyleSpigaglia, P., Barbanti, F., Faccini, S., Vescovi, M., Criscuolo, E. M., Ceruti, R., Gaspano, C., & Rosignoli, C. (2023). Clostridioides difficile in Pigs and Dairy Cattle in Northern Italy: Prevalence, Characterization and Comparison between Animal and Human Strains. Microorganisms, 11(7), 1738. https://doi.org/10.3390/microorganisms11071738







