Detection of Salmonella Reservoirs in Birds of Prey Hosted in an Italian Wildlife Centre: Molecular and Antimicrobial Resistance Characterisation
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. Microbiological Identification
2.3. Antimicrobial Susceptibility Testing (AST)
2.4. Whole-Genome Sequencing and In Silico Analysis
3. Results
3.1. Microbiological Identification
3.2. AST
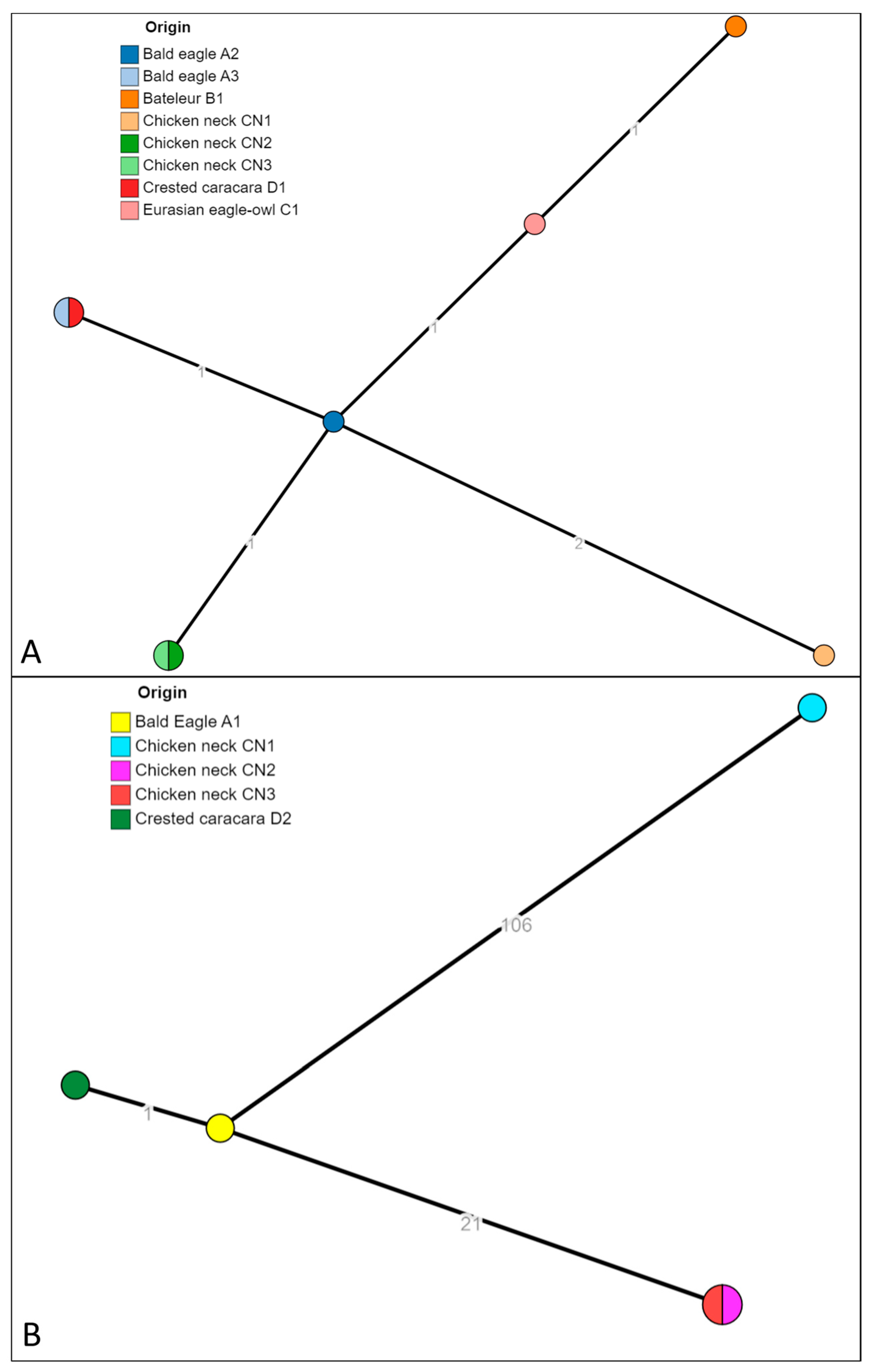
3.3. Whole-Genome Sequencing and In Silico Analysis
3.4. pESI-like Megaplasmid Presence in S. Infantis Isolates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Milanov, D.; Fabijan, D.; Prunić, B.; Velhner, M.; Petrović, T. Enteric bacteria in fecal samples of Eurasian griffon vultures. Arch. Vet. Med. 2014, 6, 45–53. [Google Scholar] [CrossRef]
- Konicek, C.; Vodrážka, P.; Barták, P.; Knotek, Z.; Hess, C.; Račka, K.; Hess, M.; Troxler, S. Detection of zoonotic pathogens in wild birds in the cross-border region Austria—Czech Republic. J. Wildl. Dis. 2016, 52, 850. [Google Scholar] [CrossRef] [PubMed]
- Martín-Maldonado, B.; Montoro-Dasi, L.; Pérez-Gracia, M.T.; Jordá, J.; Vega, S.; Marco-Jiménez, F.; Marin, C. Wild Bonelli’s eagles (Aquila fasciata) as carrier of antimicrobial resistant Salmonella and Campylobacter in Eastern Spain. Comp. Immunol. Microbiol. Infect. Dis. 2019, 67, 101372. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Tarifa, E.; Torralbo, A.; Borge, C.; Cerdà-Cuéllar, M.; Ayats, T.; Carbonero, A.; García-Bocanegra, I. Genetic diversity and antimicrobial resistance of Campylobacter and Salmonella strains isolated from decoys and raptors. Comp. Immunol. Microbiol. Infect. Dis. 2016, 48, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Khafagy, A.; Kamel, A.; Moursy, M.; Aidaroos, N.; Ahmed, D. Phenotypic and Genotypic Characterization of Gram negative bacteria Isolated from Birds of Prey (Raptors). Suez Canal Vet. Med. J. SCVMJ 2018, 23, 31–44. [Google Scholar] [CrossRef]
- Tizard, I. Salmonellosis in wild birds. Semin. Avian Exot. Pet Med. 2004, 13, 50–66. [Google Scholar] [CrossRef]
- De Luca, C.; Niero, G.; Cattarossi, D.; Bedin, M.; Piccirillo, A. Pet and captive birds as potential reservoirs of zoonotic bacteria. J. Exot. Pet Med. 2018, 27, 17–20. [Google Scholar] [CrossRef]
- Botti, V.; Navillod, F.V.; Domenis, L.; Orusa, R.; Pepe, E.; Robetto, S.; Guidetti, C. Salmonella spp. and antibiotic-resistant strains in wild mammals and birds in north-western Italy from 2002 to 2010. Vet. Ital. 2013, 49, 195–202. [Google Scholar]
- Grimont, P.A.D.; Weill, F.-X. WHO Collaborating Centre for Reference and Research on Salmonella Antigenic Formulae of the Salmonella serovars, 9th ed.; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Graziani, C.; Losasso, C.; Luzzi, I.; Ricci, A.; Scavia, G.; Pasquali, P. Chapter 5—Salmonella. In Foodborne Diseases, 3rd ed.; Academic Press: Cambridge, MA, USA, 2017; pp. 133–169. ISBN 9780123850072. [Google Scholar]
- Issenhuth-Jeanjean, S.; Roggentin, P.; Mikoleit, M.; Guibourdenche, M.; De Pinna, E.; Nair, S.; Fields, P.I.; Weill, F.X. Supplement 2008-2010 (no. 48) to the White-Kauffmann-Le Minor scheme. Res. Microbiol. 2014, 165, 526–530. [Google Scholar] [CrossRef]
- Pulford, C.V.; Wenner, N.; Redway, M.L.; Rodwell, E.V.; Webster, H.J.; Escudero, R.; Kröger, C.; Canals, R.; Rowe, W.; Lopez, J.; et al. The diversity, evolution and ecology of Salmonella in venomous snakes. PLoS Negl. Trop. Dis. 2019, 13, e0007169. [Google Scholar] [CrossRef]
- Vila Nova, M.; Durimel, K.; La, K.; Felten, A.; Bessières, P.; Mistou, M.Y.; Mariadassou, M.; Radomski, N. Genetic and metabolic signatures of Salmonella enterica subsp. enterica associated with animal sources at the pangenomic scale. BMC Genom. 2019, 20, 814. [Google Scholar] [CrossRef] [PubMed]
- Lamas, A.; Miranda, J.M.; Regal, P.; Vázquez, B.; Franco, C.M.; Cepeda, A. A comprehensive review of non-enterica subspecies of Salmonella enterica. Microbiol. Res. 2018, 206, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Peruzy, M.F.; Proroga, Y.T.R.; Capuano, F.; Mancusi, A.; Montone, A.M.I.; Cristiano, D.; Balestrieri, A.; Murru, N. Occurrence and distribution of Salmonella serovars in carcasses and foods in southern Italy: Eleven-year monitoring (2011–2021). Front. Microbiol. 2022, 13, 1005035. [Google Scholar] [CrossRef]
- European Food Safety Authority and European Centre for Disease Prevention and Control (EFSA and ECDC). The European Union One Health 2022 Zoonoses Report. EFSA J. 2023, 21, e8442. [Google Scholar] [CrossRef] [PubMed]
- Sakaridis, I.; Soultos, N.; Iossifidou, E.; Koidis, P.; Ambrosiadis, I. Prevalence and antimicrobial resistance of Salmonella serovars from chicken carcasses in Northern Greece. J. Food Saf. 2011, 31, 203–210. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA); European Centre for Disease Prevention and Control (ECDC). The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2021–2022. EFSA J. 2024, 22, e8583. [Google Scholar] [CrossRef] [PubMed]
- Alba, P.; Leekitcharoenphon, P.; Carfora, V.; Amoruso, R.; Cordaro, G.; Matteo, P.D.; Ianzano, A.; Iurescia, M.; Diaconu, E.L.; ENGAGE-EURL-AR Network Study Group; et al. Molecular epidemiology of Salmonella Infantis in Europe: Insights into the success of the bacterial host and its parasitic pESI-like megaplasmid. Microb. Genom. 2020, 6, e000365. [Google Scholar] [CrossRef] [PubMed]
- World Organisation for Animal Health (WOAH) Salmonellosis. Manual of Diagnostic Tests and Vaccines for Terrestrial Animals; World Organisation for Animal Health: Paris, France, 2022. [Google Scholar]
- European Food Safety Authority (EFSA); Amore, G.; Beloeil, P.; Fierro, R.G.; Guerra, B.; Papanikolaou, A.; Rizzi, V.; Stoicescu, A. Manual for reporting 2021 antimicrobial resistance data within the framework of Directive 2003/99/EC and Decision 2020/1729/EU. EFSA Support. Publ. 2021, 18, 6652E. [Google Scholar] [CrossRef]
- De Bene, A.F.; Russini, V.; Corradini, C.; Vita, S.; Pecchi, S.; De Marchis, M.L.; Terracciano, G.; Focardi, C.; Montemaggiori, A.; Zuffi, M.A.L.; et al. An extremely rare serovar of Salmonella enterica (Yopougon) discovered in a Western Whip Snake (Hierophis viridiflavus) from Montecristo Island, Italy: Case report and review. Arch. Microbiol. 2024, 206, 49. [Google Scholar] [CrossRef]
- Zhou, Z.; Alikhan, N.-F.; Sergeant, M.J.; Luhmann, N.; Vaz, C.; Francisco, A.P.; Carriço, J.A.; Achtman, M. GrapeTree: Visualization of core genomic relationships among 100,000 bacterial pathogens. Genome Res. 2018, 28, 1395–1404. [Google Scholar] [CrossRef]
- Bharat, A.; Petkau, A.; Avery, B.P.; Chen, J.C.; Folster, J.P.; Carson, C.A.; Kearney, A.; Nadon, C.; Mabon, P.; Thiessen, J.; et al. Correlation between Phenotypic and In Silico Detection of Antimicrobial Resistance in Salmonella enterica in Canada Using Staramr. Microorganisms 2022, 10, 292. [Google Scholar] [CrossRef] [PubMed]
- Carattoli, A.; Zankari, E.; García-Fernández, A.; Voldby Larsen, M.; Lund, O.; Villa, L.; Møller Aarestrup, F.; Hasman, H. In Silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob. Agents Chemother. 2014, 58, 3895–3903. [Google Scholar] [CrossRef] [PubMed]
- Alba, P.; Carfora, V.; Feltrin, F.; Diaconu, E.L.; Sorbara, L.; Dell’Aira, E.; Cerci, T.; Ianzano, A.; Donati, V.; Franco, A.; et al. Evidence of structural rearrangements in ESBL-positive pESI(like) megaplasmids of S. Infantis. FEMS Microbiol. Lett. 2023, 370, fnad014. [Google Scholar] [CrossRef] [PubMed]
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic local alignment search tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Alikhan, N.-F.; Petty, N.K.; Ben Zakour, N.L.; Beatson, S.A. BLAST Ring Image Generator (BRIG): Simple prokaryote genome comparisons. BMC Genom. 2011, 12, 402. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Alali, W.Q.; Harrison, M.A.; Hofacre, C.L. Prevalence of Salmonella in Neck Skin and Bone of Chickens. J. Food Prot. 2014, 77, 1193–1197. [Google Scholar] [CrossRef] [PubMed]
- Iannetti, L.; Neri, D.; Santarelli, G.A.; Cotturone, G.; Podaliri Vulpiani, M.; Salini, R.; Antoci, S.; Di Serafino, G.; Di Giannatale, E.; Pomilio, F.; et al. Animal welfare and microbiological safety of poultry meat: Impact of different at-farm animal welfare levels on at-slaughterhouse Campylobacter and Salmonella contamination. Food Control 2020, 109, 106921. [Google Scholar] [CrossRef]
- Perilli, M.; Scattolini, S.; Telera, G.C.; Cornacchia, A.; Tucci, P.; Sacchini, F.; Sericola, M.; Romantini, R.; Marotta, F.; Di Provvido, A.; et al. Distribution of Salmonella spp. Serotypes Isolated from Poultry in Abruzzo and Molise Regions (Italy) during a 6-Year Period. Microorganisms 2022, 10, 199. [Google Scholar] [CrossRef] [PubMed]
- Moore, J. Comparison of phenotypic and genotypic characteristics of Salmonella Bredeney associated with a poultry-related outbreak of gastroenteritis in Northern Ireland. J. Infect. 2003, 47, 33–39. [Google Scholar] [CrossRef]
- Flórez, N.Y.; Arévalo, S.A.; Rodríguez, E.C.; Guerrero, J.; Valverde, K.P.; Díaz, P.L.; Montaño, L.A.; Gartner, D.M.; Duarte, C.; Moreno, J.E. Brote de Salmonella enterica subsp. enterica serovar Give asociado con enfermedad transmitida por alimentos en Vichada, Colombia, 2015. Biomédica 2021, 41, 41–51. [Google Scholar] [CrossRef]
- Zhou, M.; Shi, Q.; Zhang, X.; Mei, L.; Ye, Y.; Fang, C.; Shang, S. Salmonella enterica subsp. diarizonae Harboring ST233, ST1263, and ST1845 in Children. Front. Cell. Infect. Microbiol. 2021, 11, 727811. [Google Scholar] [CrossRef] [PubMed]
- Reche, M.P.; Jiménez, P.A.; Alvarez, F.; García De Los Ríos, J.E.; Rojas, A.M.; De Pedro, P. Incidence of Salmonellae in Captive and Wild Free-Living Raptorial Birds in Central Spain. J. Vet. Med. Ser. B 2003, 50, 42–44. [Google Scholar] [CrossRef] [PubMed]
- Molina-Lopez, R.A.; Valverdú, N.; Martin, M.; Mateu, E.; Obon, E.; Cerdà-Cuéllar, M.; Darwich, L. Wild raptors as carriers of antimicrobial-resistant Salmonella and Campylobacter strains. Vet. Rec. 2011, 168, 565. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo, A.; Fioretti, A.; Russo, T.P.; Varriale, L.; Rampa, L.; Paone, S.; De Luca Bossa, L.M.; Raia, P.; Dipineto, L. Occurrence of enteropathogenic bacteria in birds of prey in Italy. Lett. Appl. Microbiol. 2018, 66, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, R.; Tavares, L.; Oliveira, M. Antimicrobial Resistance and Virulence Potential of Bacterial Species from Captive Birds of Prey—Consequences of Falconry for Public Health. Animals 2024, 14, 856. [Google Scholar] [CrossRef] [PubMed]
- Nagai, K.; Tokita, K.; Ono, H.; Uchida, K.; Sakamoto, F.; Higuchi, H. Hindgut Bacterial Flora Analysis in Oriental Honey Buzzard (Pernis ptilorhynchus). Zoolog. Sci. 2019, 36, 77. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, B.C.M.; Murray, M.; Tseng, F.; Widmer, G. The fecal microbiota of wild and captive raptors. Anim. Microbiome 2020, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Alba, C.; Sansano-Maestre, J.; Cid Vázquez, M.D.; Martínez-Herrero, M.D.C.; Garijo-Toledo, M.M.; Azami-Conesa, I.; Moraleda Fernández, V.; Gómez-Muñoz, M.T.; Rodríguez, J.M. Captive Breeding and Trichomonas gallinae Alter the Oral Microbiome of Bonelli’s Eagle Chicks. Microb. Ecol. 2023, 85, 1541–1551. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.R.; Ridgeway, S.; Shibl, A.A.; Idaghdour, Y.; Jha, A.R. Falcon gut microbiota is shaped by diet and enriched in Salmonella. PLoS ONE 2024, 19, e0293895. [Google Scholar] [CrossRef]
- Chattaway, M.A.; Langridge, G.C.; Wain, J. Salmonella nomenclature in the genomic era: A time for change. Sci. Rep. 2021, 11, 7494. [Google Scholar] [CrossRef]
- Polat, İ.; Şen, B.; Onurdağ, F.K. Salmonella enterica serotypes isolated for the first time in laying hens, and their susceptibility to antibiotics. Poult. Sci. 2024, 103, 103180. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Alikhan, N.-F.; Mohamed, K.; Fan, Y.; Agama Study Group; Achtman, M. The EnteroBase user’s guide, with case studies on Salmonella transmissions, Yersinia pestis phylogeny, and Escherichia core genomic diversity. Genome Res. 2020, 30, 138–152. [Google Scholar] [CrossRef] [PubMed]
- Achtman, M.; Zhou, Z.; Alikhan, N.-F.; Tyne, W.; Parkhill, J.; Cormican, M.; Chiou, C.-S.; Torpdahl, M.; Litrup, E.; Prendergast, D.M.; et al. Genomic diversity of Salmonella enterica-The UoWUCC 10K genomes project. Wellcome Open Res. 2021, 5, 223. [Google Scholar] [CrossRef] [PubMed]
- Mattock, J.; Chattaway, M.A.; Hartman, H.; Dallman, T.J.; Smith, A.M.; Keddy, K.; Petrovska, L.; Manners, E.J.; Duze, S.T.; Smouse, S.; et al. A One Health Perspective on Salmonella enterica Serovar Infantis, an Emerging Human Multidrug-Resistant Pathogen. Emerg. Infect. Dis. 2024, 30, 701–710. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO List of Medically Important Antimicrobials A Risk Management Tool for Mitigating Antimicrobial Resistance Due to Non-Human Use; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- Jibril, A.H.; Okeke, I.N.; Dalsgaard, A.; Menéndez, V.G.; Olsen, J.E. Genomic Analysis of Antimicrobial Resistance and Resistance Plasmids in Salmonella Serovars from Poultry in Nigeria. Antibiotics 2021, 10, 99. [Google Scholar] [CrossRef]
- Chang, M.-X.; Zhang, J.-F.; Sun, Y.-H.; Li, R.-S.; Lin, X.-L.; Yang, L.; Webber, M.A.; Jiang, H.-X. Contribution of Different Mechanisms to Ciprofloxacin Resistance in Salmonella spp. Front. Microbiol. 2021, 12, 663731. [Google Scholar] [CrossRef]


| Raptors Species | ID Code | 20 July 2021 | 5 August 2021 | 27 December 2021 | Serovar | NCBI Acc. No. |
|---|---|---|---|---|---|---|
| Bald Eagle (Haliaeetus leucocephalus) | A1 | + | / | − | Salmonella Infantis | SAMN40917614 |
| Bald Eagle (Haliaeetus leucocephalus) | A2 | + | / | − | Salmonella Bredeney | SAMN40917609 |
| Bald Eagle (Haliaeetus leucocephalus) | A3 | + | / | − | Salmonella Bredeney | SAMN40917606 |
| Bateleur (Terathopius ecaudatus) | B1 | + | / | − | Salmonella Bredeney | SAMN40917610 |
| Eurasian eagle-owl (Bubo bubo) | C1 | + | / | − | Salmonella Bredeney | SAMN40917608 |
| Crested caracara (Caracara plancus) | D1 | + | / | − | Salmonella Bredeney | SAMN40917607 |
| Crested caracara (Caracara plancus) | D2 | / | − | + | Salmonella Infantis | SAMN40917615 |
| African Fish Eagle (Haliaeetus vocifer) | E1 | + | / | − | Salmonella enterica subsp. diarizonae IIIb (50:r:1.5) O:50 (Z) | sequencing not performed |
| African Fish Eagle (Haliaeetus vocifer) | E2 | + | / | − | Salmonella enterica subsp. diarizonae IIIb (35:r:z35) O:35 (O) | sequencing not performed |
| Black-chested buzzard-eagle (Geranoaetus melanoleucus) | F1 | − | / | − | n/a | n/a |
| Hooded vulture (Necrosyrtes monachus) | G1 | − | − | / | n/a | n/a |
| Egyptian Vulture (Neophron percnopterus) | H1 | / | − | − | n/a | n/a |
| Barn Owl (Tyto alba) | I1 | / | − | − | n/a | n/a |
| Barn Owl (Tyto alba) | I2 | / | − | / | n/a | n/a |
| Barn Owl (Tyto alba) | I3 | / | − | / | n/a | n/a |
| Tawny owl (Strix aluco) | L1 | / | − | / | n/a | n/a |
| Black kite (Milvus migrans) | M1 | / | − | / | n/a | n/a |
| Harris’s hawk (Parabuteo unicinctus) | N1 | / | − | / | n/a | n/a |
| Feed Matrix | ID Code | 26 August 2021 | 7 September 2021 | 28 September 2021 | Serovar | NCBI Acc. No. |
|---|---|---|---|---|---|---|
| Chicken necks (Gallus gallus) | CN1 | + | / | / | Salmonella Bredeney | SAMN40917603 |
| Salmonella Infantis | SAMN40917611 | |||||
| CN1a | − | / | / | n/a | n/a | |
| CN2 | / | + | / | Salmonella Bredeney | SAMN40917604 | |
| Salmonella Infantis | SAMN40917612 | |||||
| CN3 | / | / | + | Salmonella Bredeney | SAMN40917605 | |
| Salmonella Infantis | SAMN40917613 | |||||
| Salmonella Give | sequencing not performed | |||||
| Carcasses of chicks (Gallus gallus) | CC1 | − | / | / | n/a | n/a |
| CC2 | − | / | / | n/a | n/a | |
| CC3 | − | / | / | n/a | n/a |
| Aminoglycoside | Aminocyclitol | Beta-Lactam | Phenicol | Folate Pathway Antagonist | (Fluoro)quinolone | Macrolide | Tetracycline | Plasmid | AMR Phenotype | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample ID | Origin | Serotype | MLST | cgMLST | aadA1 | aadA2 | aph(3′)-Ia | aph(3″)-Ib | aph(6)-Id | ant(3″)-Ia | blaCTX-M-1 | blaTEM-1B | cmlA1 | dfrA1 | dfrA12 | dfrA14 | sul1 | sul2 | sul3 | gyrA (D87G) | gyrA (D87Y) | parC (T57S) | qnrB19 | mef(B) | tet(A) | tet(B) | Col(pHAD28) | IncFIB(pN55391) | |
| Chicken neck CN1 | Food | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | + | − | − | + | + | − | NAL-CIP-SUL-TET |
| Chicken neck CN2 | Food | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | − | − | − | + | − | − | NAL-CIP-SUL-TET |
| Chicken neck CN3 | Food | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | − | − | − | + | − | − | SUL-TET |
| Bald Eagle (Haliaeetus leucocephalus) A3 | Droppings | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | + | − | − | + | + | − | NAL-CIP-SUL-TET |
| Crested caracara (Caracara plancus) D1 | Droppings | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | + | − | − | + | + | − | NAL-CIP-SUL-TET |
| Eurasian eagle-owl (Bubo bubo) C1 | Droppings | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | − | − | − | + | − | − | SUL-TET |
| Bald Eagle (Haliaeetus leucocephalus) A2 | Droppings | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | − | − | − | + | − | − | SUL-TET |
| Bateleur (Terathopius ecaudatus) B1 | Droppings | Bredeney | 897 | 201416 | − | − | + | + | + | − | − | − | − | − | − | − | − | + | − | − | − | + | − | − | − | + | − | − | SUL-TET |
| Chicken neck CN1 | Food | Infantis | 32 | 254768 | − | − | − | − | − | + | − | − | − | − | − | − | + | − | − | − | + | + | − | − | + | − | − | + | NAL-CIP-SUL-TET |
| Chicken neck CN2 | Food | Infantis | 32 | 93308 | + | + | + | − | − | − | − | + | + | + | + | + | + | − | + | + | − | + | − | + | + | − | − | + | AMP-CHL-NAL-CIP-SUL-TET-TMP |
| Chicken neck CN3 | Food | Infantis | 32 | 93308 | + | + | + | − | − | − | − | + | + | + | + | + | + | − | + | + | − | + | − | + | + | − | − | + | AMP-CHL-NAL-CIP-SUL-TET-TMP |
| Bald Eagle (Haliaeetus leucocephalus) A1 | Droppings | Infantis | 32 | 145963 | − | − | − | − | − | − | + | − | − | + | − | + | + | − | − | + | − | + | − | − | + | − | + | + | AMP-FOT-TAZ-NAL-CIP-SUL-TET-TMP |
| Crested caracara (Caracara plancus) D2 | Droppings | Infantis | 32 | 145963 | − | − | − | − | − | − | + | − | − | + | − | + | + | − | − | + | − | + | − | − | + | − | − | + | AMP-FOT-TAZ-NAL-CIP-SUL-TET-TMP |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corradini, C.; De Bene, A.F.; Russini, V.; Carfora, V.; Alba, P.; Cordaro, G.; Senese, M.; Terracciano, G.; Fabbri, I.; Di Sirio, A.; et al. Detection of Salmonella Reservoirs in Birds of Prey Hosted in an Italian Wildlife Centre: Molecular and Antimicrobial Resistance Characterisation. Microorganisms 2024, 12, 1169. https://doi.org/10.3390/microorganisms12061169
Corradini C, De Bene AF, Russini V, Carfora V, Alba P, Cordaro G, Senese M, Terracciano G, Fabbri I, Di Sirio A, et al. Detection of Salmonella Reservoirs in Birds of Prey Hosted in an Italian Wildlife Centre: Molecular and Antimicrobial Resistance Characterisation. Microorganisms. 2024; 12(6):1169. https://doi.org/10.3390/microorganisms12061169
Chicago/Turabian StyleCorradini, Carlo, Andrea Francesco De Bene, Valeria Russini, Virginia Carfora, Patricia Alba, Gessica Cordaro, Matteo Senese, Giuliana Terracciano, Ilaria Fabbri, Alessandro Di Sirio, and et al. 2024. "Detection of Salmonella Reservoirs in Birds of Prey Hosted in an Italian Wildlife Centre: Molecular and Antimicrobial Resistance Characterisation" Microorganisms 12, no. 6: 1169. https://doi.org/10.3390/microorganisms12061169
APA StyleCorradini, C., De Bene, A. F., Russini, V., Carfora, V., Alba, P., Cordaro, G., Senese, M., Terracciano, G., Fabbri, I., Di Sirio, A., Di Giamberardino, F., Boria, P., De Marchis, M. L., & Bossù, T. (2024). Detection of Salmonella Reservoirs in Birds of Prey Hosted in an Italian Wildlife Centre: Molecular and Antimicrobial Resistance Characterisation. Microorganisms, 12(6), 1169. https://doi.org/10.3390/microorganisms12061169







