Intelligent Biological Networks: Improving Anti-Microbial Resistance Resilience through Nutritional Interventions to Understand Protozoal Gut Infections
Abstract
1. Introduction

| Name | Transmission Mode | Health Symptoms | Hosts | Disinfection Resistance | Outbreaks/Cases | References |
|---|---|---|---|---|---|---|
| Cryptosporidium spp. | Water (drinking and recreational), fecal-oral route | Moderate/diarrhea. Mostly asymptomatic, diagnosed during clinical presentation | Humans, cattle, rodents, wild animals | Very high/ozone (4 ppm/10 min); >3% hypochlorite | 239/65,540 (2004–2014) | [2,3,6,8] |
| Giardia spp. | Moderate/diarrhea, gas, bloating, anorexia. Mostly asymptomatic, diagnosed during clinical presentation | Human, cattle, wild animals | High/fenbendazole (5 mg/kg); ozone (0.3 ppm/3 min); 1% sodium hypochlorite | 142/1110 (2007–2014) | [1,3,8,9] | |
| Entamoeba histolytica | Severe/colitis, dysentery, diarrhea, liver abscess | Humans, non-human primates | High/chlorine (5 ppm, pH 7, 5 min), 1% sodium hypochlorite | 15/9.41 million (2000–2015) | [2,4,9,10] |
2. Research Methodology
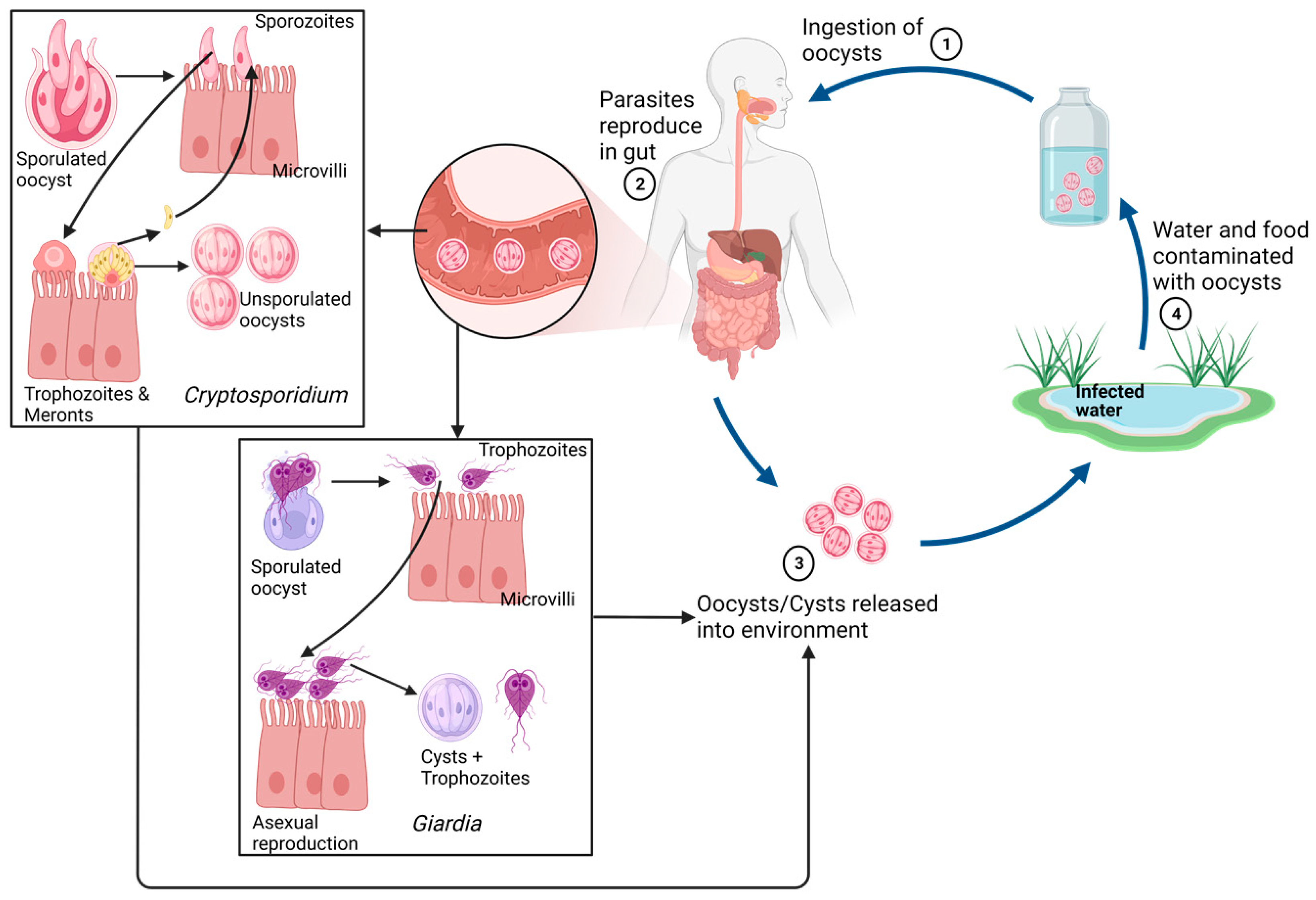
3. Life Cycle and Infection Mechanism
3.1. Life Cycle
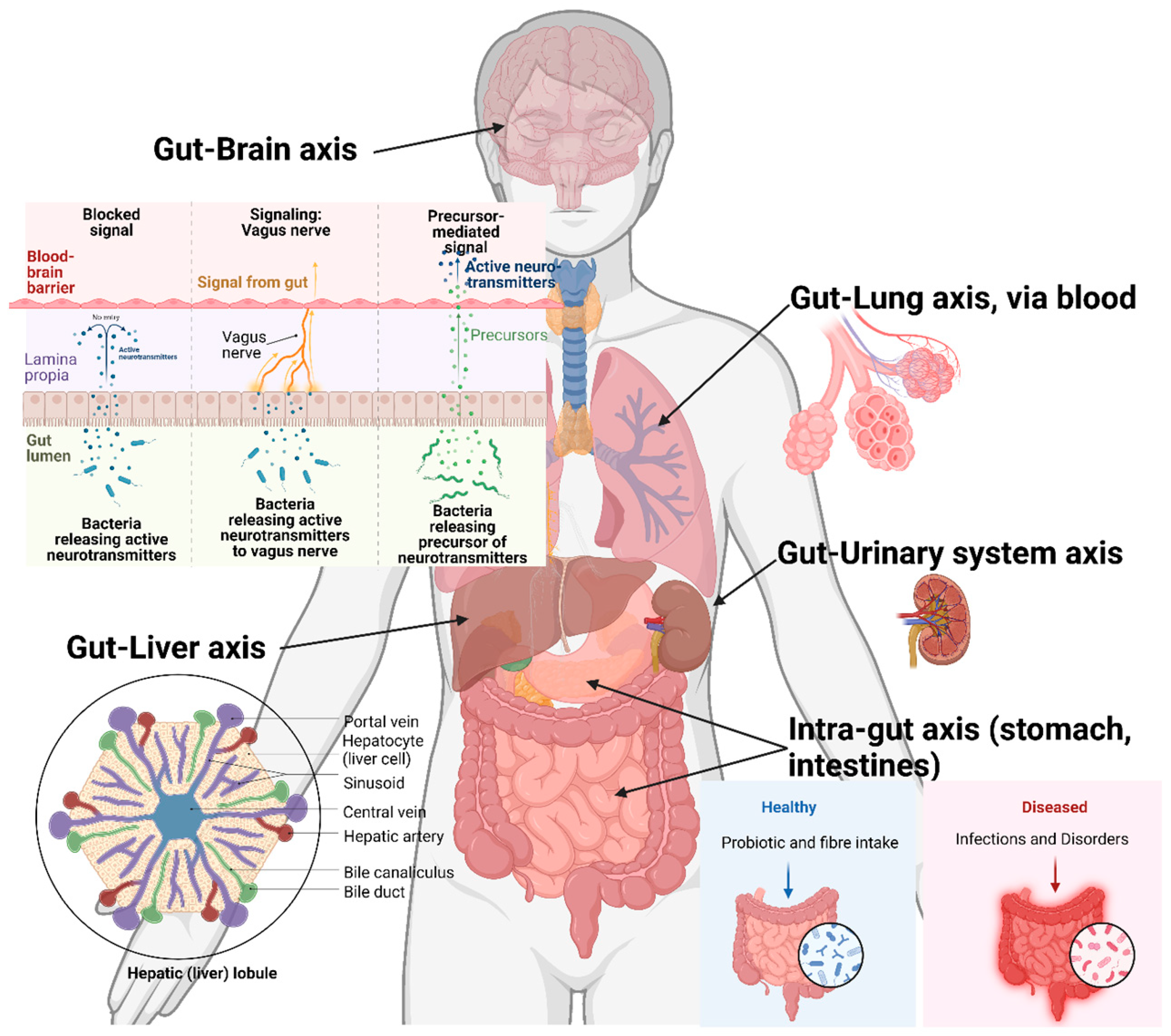
3.2. Dysbiosis and Target Organs
Dysbiosis
4. Cross-Organ Impacts
4.1. Gut–Liver Axis
4.2. Gut–Lung Axis
5. Nutritional Interventions
5.1. Prebiotics, Probiotics, and Synbiotics Supplementation
5.2. Postbiotics and Microbiome Modulation to Improve MDR Resilience
6. Application of Multiomics in High-Throughput Analysis of Gut Microbiome Health and Inter-Organ Axes
6.1. Multiomics Approaches
6.2. Application of Artificial Intelligence and Machine Learning (AIML) and Future Aspects
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Petri, W.A.; Miller, M.; Binder, H.J.; Levine, M.M.; Dillingham, R.; Guerrant, R.L. Enteric infections, diarrhea, and their impact on function and development. J. Clin. Investig. 2008, 118, 1277–1290. [Google Scholar] [CrossRef]
- WHO. Global Health Observatory data repository: Diarrhoeal diseases. Available online: http://www.who.int/mediacentre/factsheets/fs310/en/ (accessed on 17 January 2023).
- Efstratiou, A.; Ongerth, J.E.; Karanis, P. Waterborne transmission of protozoan parasites: Review of worldwide outbreaks—An update 2011–2016. Water Res. 2017, 114, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Berger, S. Amoebiasis: Global Status; GIDEON Informatics Inc.: Los Angeles, CA, USA, 2017. [Google Scholar]
- Berger, S. Giardiasis: Global Status; GIDEON Informatics Inc.: Los Angeles, CA, USA, 2017. [Google Scholar]
- Berger, S. Cryptosporidiosis: Global Status; GIDEON Informatics Inc.: Los Angeles, CA, USA, 2017. [Google Scholar]
- Dadonaite, B.; Ritchie, H.; Roser, M. Diarrheal Diseases. Available online: https://ourworldindata.org/diarrheal-diseases (accessed on 27 June 2023).
- Betancourt, W.Q.; Rose, J.B. Drinking water treatment processes for removal of Cryptosporidium and Giardia. Vet. Parasitol. 2004, 126, 219–234. [Google Scholar] [CrossRef] [PubMed]
- Jarroll, E.L.; Hoff, J.C. Effect of disinfectants on Giardia cysts. Crit. Rev. Environ. Sci. Technol. 1988, 18, 1–28. [Google Scholar]
- Rubin, A.J.; Engel, J.P.; Sproul, O.J. Disinfection of amoebic cysts in water with free chlorine. J. Water Pollut. Control. Fed. 1983, 55, 1174–1182. [Google Scholar]
- Chalmers, R.M. Chapter Sixteen—Cryptosporidium. In Microbiology of Waterborne Diseases, 2nd ed.; Academic Press: London, UK, 2014; pp. 287–326. [Google Scholar]
- Lane, S.; Lloyd, D. Current trends in research into the waterborne parasite Giardia. Crit. Rev. Microbiol. 2002, 28, 123–147. [Google Scholar] [CrossRef]
- Chalmers, R.M. Chapter Eighteen—Entamoeba histolytica. In Microbiology of Waterborne Diseases, 2nd ed.; Academic Press: London, UK, 2014; pp. 355–373. [Google Scholar]
- Duncan, H.E.; Edberg, S.C. Host-Microbe Interaction in the Gastrointestinal Tract. Crit. Rev. Microbiol. 1995, 21, 85–100. [Google Scholar] [CrossRef]
- Macfarlane, S.; Dillon, J.F. Microbial biofilms in the human gastrointestinal tract. J. Appl. Microbiol. 2007, 102, 1187–1196. [Google Scholar] [CrossRef]
- Swidsinski, A.; Ung, V.; Sydora, B.C.; Loening-Baucke, V.; Doerffel, Y.; Verstraelen, H.; Fedorak, R.N. Bacterial overgrowth and inflammation of small intestine after carboxymethylcellulose ingestion in genetically susceptible mice. Inflamm. Bowel Dis. 2009, 15, 359–364. [Google Scholar] [CrossRef]
- Koh, W.; Clode, P.L.; Monis, P.; Thompson, R.A. Multiplication of the waterborne pathogen Cryptosporidium parvum in an aquatic biofilm system. Parasites Vectors 2013, 6, 270. [Google Scholar] [CrossRef]
- McKenney, E.A.; Greene, L.K.; Drea, C.M.; Yoder, A.D. Down for the count: Cryptosporidium infection depletes the gut microbiome in Coquerel’s sifakas. Microb. Ecol. Health Dis. 2017, 28, 1335165. [Google Scholar] [CrossRef] [PubMed]
- Certad, G.; Viscogliosi, E.; Chabé, M.; Cacciò, S.M. Pathogenic Mechanisms of Cryptosporidium and Giardia. Trends Parasitol. 2017, 33, 561–576. [Google Scholar] [CrossRef] [PubMed]
- Karpe, A.V.; Hutton, M.L.; Mileto, S.J.; James, M.L.; Evans, C.; Shah, R.M.; Ghodke, A.B.; Hillyer, K.E.; Metcalfe, S.S.; Liu, J.-W.; et al. Cryptosporidiosis Modulates the Gut Microbiome and Metabolism in a Murine Infection Model. Metabolites 2021, 11, 380. [Google Scholar] [CrossRef]
- Berrilli, F.; Di Cave, D.; Cavallero, S.; D’Amelio, S. Interactions between parasites and microbial communities in the human gut. Front. Cell. Infect. Microbiol. 2012, 2, 141. [Google Scholar] [CrossRef]
- Dwyer, D.M.; Chang, K.P. Surface membrane carbohydrate alterations of a flagellated protozoan mediated by bacterial endosymbiotes. Proc. Natl. Acad. Sci. USA 1976, 73, 852–856. [Google Scholar] [CrossRef]
- Torres, M.F.; Uetanabaro, A.P.T.; Costa, A.F.; Alves, C.A.; Farias, L.M.; Bambirra, E.A.; Penna, F.J.; Vieira, E.C.; Nicoli, J.R. Influence of bacteria from the duodenal microbiota of patients with symptomatic giardiasis on the pathogenicity of Giardia duodenalis in gnotoxenic mice. J. Med. Microbiol. 2000, 49, 209–215. [Google Scholar] [CrossRef]
- Mirelman, D.; Feingold, C.; Wexler, A.; Bracha, R. Interactions between Entamoeba histolytica, bacteria and intestinal cells. In Cytopathology of Parasitic Disease; Pitman Books: London, UK, 1983; Volume 99, pp. 2–30. [Google Scholar]
- Galván-Moroyoqui, J.M.; Del Carmen Dominguez-Robles, M.; Franco, E.; Meza, I. The interplay between Entamoeba and enteropathogenic bacteria modulates epithelial cell damage. PLoS Neglected Trop. Dis. 2008, 2, e266. [Google Scholar] [CrossRef] [PubMed]
- Gerbaba, T.K.; Gupta, P.; Rioux, K.; Hansen, D.; Buret, A.G. Giardia duodenalis-induced alterations of commensal bacteria kill Caenorhabditis elegans: A new model to study microbial-microbial interactions in the gut. Am. J. Physiol.-Gastrointest. Liver Physiol. 2015, 308, G550–G561. [Google Scholar] [CrossRef] [PubMed]
- Wallace, J.L.; Blackler, R.W.; Chan, M.V.; Da Silva, G.J.; Elsheikh, W.; Flannigan, K.L.; Gamaniek, I.; Manko, A.; Wang, L.; Motta, J.-P. Anti-inflammatory and cytoprotective actions of hydrogen sulfide: Translation to therapeutics. Antioxid. Redox Signal. 2015, 22, 398–410. [Google Scholar] [CrossRef] [PubMed]
- Karpe, A.V.; Hutton, M.L.; Mileto, S.J.; James, M.L.; Evans, C.; Ghodke, A.B.; Shah, R.M.; Metcalfe, S.S.; Liu, J.-W.; Walsh, T.; et al. Gut microbial perturbation and host response induce redox pathway upregulation along the Gut-Liver axis during giardiasis in C57BL/6J mouse model. Int. J. Mol. Sci. 2023, 24, 1636. [Google Scholar] [CrossRef]
- Kedia, S.; Rampal, R.; Paul, J.; Ahuja, V. Gut microbiome diversity in acute infective and chronic inflammatory gastrointestinal diseases in North India. J. Gastroenterol. 2016, 51, 660–671. [Google Scholar] [CrossRef] [PubMed]
- Partida-Rodríguez, O.; Serrano-Vázquez, A.; Nieves-Ramírez, M.E.; Moran, P.; Rojas, L.; Portillo, T.; González, E.; Hernández, E.; Finlay, B.B.; Ximenez, C. Human intestinal microbiota: Interaction between parasites and the host immune response. Arch. Med. Res. 2017. [Google Scholar] [CrossRef] [PubMed]
- Zermeño, V.; Ximénez, C.; Morán, P.; Valadez, A.; Valenzuela, O.; Rascón, E.; Diaz, D.; Cerritos, R. Worldwide genealogy of Entamoeba histolytica: An overview to understand haplotype distribution and infection outcome. Infect. Genet. Evol. 2013, 17, 243–252. [Google Scholar] [CrossRef]
- Guzmán-Silva, M.A.; Santos, H.L.C.; Peralta, R.S.; Peralta, J.M.; de Macedo, H.W. Experimental amoebic liver abscess in hamsters caused by trophozoites of a Brazilian strain of Entamoeba dispar. Exp. Parasitol. 2013, 134, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Dolabella, S.S.; Serrano-Luna, J.; Navarro-García, F.; Cerritos, R.; Ximénez, C.; Galván-Moroyoqui, J.M.; Silva, E.F.; Tsutsumi, V.; Shibayama, M. Amoebic liver abscess production by Entamoeba dispar. Parasite 2012, 13, 15. [Google Scholar] [CrossRef]
- Weber, C.; Koutero, M.; Dillies, M.-A.; Varet, H.; Lopez-Camarillo, C.; Coppée, J.Y.; Hon, C.-C.; Guillén, N. Extensive transcriptome analysis correlates the plasticity of Entamoeba histolytica pathogenesis to rapid phenotype changes depending on the environment. Sci. Rep. 2016, 6, 35852. [Google Scholar] [CrossRef]
- Rigothier, M.-C.; Khun, H.; Tavares, P.; Cardona, A.; Huerre, M.; Guillén, N. Fate of Entamoeba histolytica during establishment of amoebic liver abscess analyzed by quantitative radioimaging and histology. Infect. Immun. 2002, 70, 3208–3215. [Google Scholar] [CrossRef]
- Stanley, S.L. Pathophysiology of amoebiasis. Trends Parasitol. 2001, 17, 280–285. [Google Scholar] [CrossRef]
- Tsutsumi, V.; Mena-Lopez, R.; Anaya-Velazquez, F.; Martinez-Palomo, A. Cellular bases of experimental amebic liver abscess formation. Am. J. Pathol. 1984, 117, 81. [Google Scholar]
- Ungar, B.L.; Burris, J.A.; Quinn, C.A.; Finkelman, F.D. New mouse models for chronic Cryptosporidium infection in immunodeficient hosts. Infect. Immun. 1990, 58, 961–969. [Google Scholar] [CrossRef]
- Astiazaran-Garcia, H.; Lopez-Teros, V.; Valencia, M.E.; Vazquez-Ortiz, F.; Sotelo-Cruz, N.; Quihui-Cota, L. Giardia lamblia infection and its implications for vitamin a liver stores in school children. Ann. Nutr. Metab. 2010, 57, 228–233. [Google Scholar] [CrossRef]
- Swann, J.; Jamshidi, N.; Lewis, N.E.; Winzeler, E.A. Systems analysis of host–parasite interactions. Wiley Interdiscip. Rev. Syst. Biol. Med. 2015, 7, 381–400. [Google Scholar] [CrossRef]
- Zakaria, A.; Al-Share, B.; Al Asad, K. Primary Pulmonary Amebiasis Complicated with Multicystic Empyema. Case Rep. Pulmonol. 2016, 2016, 4. [Google Scholar] [CrossRef]
- Goh, L.M.L.; Marrone, J.R. Entamoeba histolytica meningoencephalitis diagnosed by trophozoites in cerebrospinal fluid. New Microbes New Infect. 2013, 1, 16–17. [Google Scholar] [CrossRef] [PubMed]
- Reina, F.T.R.; Ribeiro, C.A.; Araújo, R.S.D.; Matté, M.H.; Castanho, R.E.P.; Tanaka, I.I.; Viggiani, A.M.F.S.; Martins, L.P.A. Intestinal and Pulmonary Infection by Cryptosporidium parvum in Two Patients with HIV/AIDS. Rev. Inst. Med. Trop. São Paulo 2016, 58, 21. [Google Scholar] [CrossRef] [PubMed]
- López-Vélez, R.; Tarazona, R.; Camacho, A.G.; Gomez-Mampaso, E.; Guerrero, A.; Moreira, V.; Villanueva, R. Intestinal and extraintestinal cryptosporidiosis in AIDS patients. Eur. J. Clin. Microbiol. Infect. Dis. 1995, 14, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Clavel, A.; Arnal, A.C.; Sánchez, E.C.; Castillo, F.J.; Varea, M.; Gómez-Lus, R.; Cuesta, J.; Letona, S.; Amiguet, J.A. Respiratory cryptosporidiosis: Case series and review of the literature. Infection 1996, 24, 341–346. [Google Scholar] [CrossRef]
- Burgess, S.L.; Lu, M.; Ma, J.Z.; Naylor, C.; Donowitz, J.R.; Kirkpatrick, B.D.; Haque, R.; Petri, W.A., Jr. Inflammatory markers predict episodes of wheezing during the first year of life in Bangladesh. Respir. Med. 2015, 110, 53–57. [Google Scholar] [CrossRef]
- Braamskamp, M.J.A.M.; Dolman, K.M.; Tabbers, M.M. Clinical practice. Eur. J. Pediatr. 2010, 169, 1179–1185. [Google Scholar] [CrossRef]
- Wypych, T.P.; Wickramasinghe, L.C.; Marsland, B.J. The influence of the microbiome on respiratory health. Nat. Immunol. 2019, 20, 1279–1290. [Google Scholar] [CrossRef]
- Trompette, A.; Gollwitzer, E.S.; Yadava, K.; Sichelstiel, A.K.; Sprenger, N.; Ngom-Bru, C.; Blanchard, C.; Junt, T.; Nicod, L.P.; Harris, N.L.; et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat. Med. 2014, 20, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Cait, A.; Hughes, M.R.; Antignano, F.; Cait, J.; Dimitriu, P.A.; Maas, K.R.; Reynolds, L.A.; Hacker, L.; Mohr, J.; Finlay, B.B.; et al. Microbiome-driven allergic lung inflammation is ameliorated by short-chain fatty acids. Mucosal Immunol. 2018, 11, 785–795. [Google Scholar] [CrossRef] [PubMed]
- Thorburn, A.N.; McKenzie, C.I.; Shen, S.; Stanley, D.; Macia, L.; Mason, L.J.; Roberts, L.K.; Wong, C.H.Y.; Shim, R.; Robert, R.; et al. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nat. Commun. 2015, 6, 7320. [Google Scholar] [CrossRef] [PubMed]
- Trompette, A.; Gollwitzer, E.S.; Pattaroni, C.; Lopez-Mejia, I.C.; Riva, E.; Pernot, J.; Ubags, N.; Fajas, L.; Nicod, L.P.; Marsland, B.J. Dietary Fiber Confers Protection against Flu by Shaping Ly6c− Patrolling Monocyte Hematopoiesis and CD8+ T Cell Metabolism. Immunity 2018, 48, 992–1005.e8. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.L.F.; Rudan, I.; Liu, L.; Nair, H.; Theodoratou, E.; Bhutta, Z.A.; O’Brien, K.L.; Campbell, H.; Black, R.E. Global burden of childhood pneumonia and diarrhoea. Lancet 2013, 381, 1405–1416. [Google Scholar] [CrossRef]
- Halliez, M.C.M.; Buret, A.G. Extra-intestinal and long term consequences of Giardia duodenalis infections. World J. Gastroenterol. WJG 2013, 19, 8974–8985. [Google Scholar] [CrossRef]
- Buret, A.G.; Reti, K. Acute Enteric Infections Alter Commensal Microbiota: New Mechanisms in Post-Infectious Intestinal Inflammatory Disorders; Old Herborn University Foundation: Herborn-Dill, Germany, 2014; pp. 87–100. [Google Scholar]
- Hanevik, K. Long-Term Consequences of Cryptosporidium and Giardia Gastroenteritis. Curr. Trop. Med. Rep. 2016, 3, 89–93. [Google Scholar] [CrossRef]
- Barbara, G.; Grover, M.; Bercik, P.; Corsetti, M.; Ghoshal, U.C.; Ohman, L.; Rajilić-Stojanović, M. Rome Foundation Working Team Report on Post-Infection Irritable Bowel Syndrome. Gastroenterology 2019, 156, 46–58.e7. [Google Scholar] [CrossRef]
- Allen, S.J.; Martinez, E.G.; Gregorio, G.V.; Dans, L.F. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst. Rev. 2010, CD003048. [Google Scholar] [CrossRef]
- Depoorter, L.; Vandenplas, Y. Chapter 21—Probiotics in pediatrics. In Probiotics; Brandelli, A., Ed.; Academic Press: Cambridge, MA, USA, 2022; pp. 425–450. [Google Scholar]
- Su, G.L.; Ko, C.W.; Bercik, P.; Falck-Ytter, Y.; Sultan, S.; Weizman, A.V.; Morgan, R.L. AGA Clinical Practice Guidelines on the Role of Probiotics in the Management of Gastrointestinal Disorders. Gastroenterology 2020, 159, 697–705. [Google Scholar] [CrossRef]
- Di Nardo, G.; Cremon, C.; Staiano, A.; Stanghellini, V.; Borrelli, O.; Strisciuglio, C.; Romano, C.; Mallardo, S.; Scarpato, E.; Marasco, G.; et al. Role of inflammation in pediatric irritable bowel syndrome. Neurogastroenterol. Motil. 2023, 35, e14365. [Google Scholar] [CrossRef] [PubMed]
- Nocerino, R.; Di Costanzo, M.; Bedogni, G.; Cosenza, L.; Maddalena, Y.; Di Scala, C.; Della Gatta, G.; Carucci, L.; Voto, L.; Coppola, S.; et al. Dietary Treatment with Extensively Hydrolyzed Casein Formula Containing the Probiotic Lactobacillus rhamnosus GG Prevents the Occurrence of Functional Gastrointestinal Disorders in Children with Cow’s Milk Allergy. J. Pediatr. 2019, 213, 137–142.e2. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.C.; Lacy, B.E.; Talley, N.J. Irritable Bowel Syndrome. N. Engl. J. Med. 2017, 376, 2566–2578. [Google Scholar] [CrossRef] [PubMed]
- Shinde, T.; Perera, A.P.; Vemuri, R.; Gondalia, S.V.; Beale, D.J.; Karpe, A.V.; Shastri, S.; Basheer, W.; Southam, B.; Eri, R. Synbiotic supplementation with prebiotic green banana resistant starch and probiotic Bacillus coagulans spores ameliorates gut inflammation in mouse model of inflammatory bowel diseases. Eur. J. Nutr. 2020, 59, 3669–3689. [Google Scholar] [CrossRef]
- Vitali, B.; Ndagijimana, M.; Cruciani, F.; Carnevali, P.; Candela, M.; Guerzoni, M.E.; Brigidi, P. Impact of a synbiotic food on the gut microbial ecology and metabolic profiles. BMC Microbiol. 2010, 10, 4. [Google Scholar] [CrossRef]
- Pettersson, J.; Karlsson, P.C.; Göransson, U.; Rafter, J.J.; Bohlin, L. The Flavouring Phytochemical 2-Pentanone Reduces Prostaglandin Production and COX-2 Expression in Colon Cancer Cells. Biol. Pharm. Bull. 2008, 31, 534–537. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.K.; Beckett, J.M.; Kalpurath, K.; Ishaq, M.; Ahmad, T.; Eri, R.D. Synbiotics as Supplemental Therapy for the Alleviation of Chemotherapy-Associated Symptoms in Patients with Solid Tumours. Nutrients 2023, 15, 1759. [Google Scholar] [CrossRef]
- Boger, M.C.L.; Bueren, A.L.v.; Dijkhuizen, L. Cross-Feeding among Probiotic Bacterial Strains on Prebiotic Inulin Involves the Extracellular exo-Inulinase of Lactobacillus paracasei Strain W20. Appl. Environ. Microbiol. 2018, 84, e01539-18. [Google Scholar] [CrossRef]
- Gomez Quintero, D.F.; Kok, C.R.; Hutkins, R. The Future of Synbiotics: Rational Formulation and Design. Front. Microbiol. 2022, 13, 919725. [Google Scholar] [CrossRef]
- Ribeiro, C.M.; Costa, V.M.; Gomes, M.I.F.V.; Golim, M.A.; Modolo, J.R.; Langoni, H. Effects of synbiotic-based Bifidobacterium animalis in female rats experimentally infected with Toxoplasma gondii. Comp. Immunol. Microbiol. Infect. Dis. 2011, 34, 111–114. [Google Scholar] [CrossRef]
- Emery, S.J.; Baker, L.; Ansell, B.R.E.; Mirzaei, M.; Haynes, P.A.; McConville, M.J.; Svärd, S.G.; Jex, A.R. Differential protein expression and post-translational modifications in metronidazole-resistant Giardia duodenalis. GigaScience 2018, 7, giy024. [Google Scholar] [CrossRef]
- Bhattacharyya, S. Herbal, Nutritional, and Traditional Remedies for Giardiasis. In Neglected Tropical Diseases and Phytochemicals in Drug Discovery; Wiley: Hoboken, NJ, USA, 2021; pp. 135–169. [Google Scholar]
- Anthony, J.P.; Fyfe, L.; Stewart, D.; McDougall, G.J.; Smith, H.V. The effect of blueberry extracts on Giardia duodenalis viability and spontaneous excystation of Cryptosporidium parvum oocysts, in vitro. Methods 2007, 42, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.; Attia, R.; Said, S.; Ibraheim, Z. Ginger and cinnamon: Can this household remedy treat giardiasis? Parasitological and histopathological studies. Iran. J. Parasitol. 2014, 9, 530–540. [Google Scholar] [PubMed]
- de Almeida, C.R.; Bezagio, R.C.; Colli, C.M.; Romera, L.I.L.; Ferrari, A.; Gomes, M.L. Elimination of Giardia duodenalis BIV in vivo using natural extracts in microbiome and dietary supplements. Parasitol. Int. 2022, 86, 102484. [Google Scholar] [CrossRef]
- Gaber, M.; Galal, L.A.A.; Farrag, H.M.M.; Badary, D.M.; Alkhalil, S.S.; Elossily, N. The Effects of Commercially Available Syzygium aromaticum, Anethum graveolens, Lactobacillus acidophilus LB, and Zinc as Alternatives Therapy in Experimental Mice Challenged with Cryptosporidium parvum. Infect. Drug Resist. 2022, 15, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Popovic, A.; Bourdon, C.; Wang, P.W.; Guttman, D.S.; Soofi, S.; Bhutta, Z.A.; Bandsma, R.H.J.; Parkinson, J.; Pell, L.G. Micronutrient supplements can promote disruptive protozoan and fungal communities in the developing infant gut. Nat. Commun. 2021, 12, 6729. [Google Scholar] [CrossRef]
- Salminen, S.; Collado, M.C.; Endo, A.; Hill, C.; Lebeer, S.; Quigley, E.M.M.; Sanders, M.E.; Shamir, R.; Swann, J.R.; Szajewska, H.; et al. The International Scientific Association of Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of postbiotics. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 649–667. [Google Scholar] [CrossRef]
- Shinde, T.; Vemuri, R.; Shastri, S.; Perera, A.P.; Gondalia, S.V.; Beale, D.J.; Karpe, A.V.; Eri, R.; Stanley, R. Modulating the microbiome and immune responses using whole plant fibre in synbiotic combination with fibre-digesting probiotic attenuates chronic colonic inflammation in spontaneous colitic mice model of IBD. Nutrients 2020, 12, 2380. [Google Scholar] [CrossRef]
- Kobayashi, J. D-amino acids and lactic acid bacteria. Microorganisms 2019, 7, 690. [Google Scholar] [CrossRef]
- Sasabe, J.; Miyoshi, Y.; Rakoff-Nahoum, S.; Zhang, T.; Mita, M.; Davis, B.M.; Hamase, K.; Waldor, M.K. Interplay between microbial d-amino acids and host d-amino acid oxidase modifies murine mucosal defence and gut microbiota. Nat. Microbiol. 2016, 1, 1–7. [Google Scholar] [CrossRef]
- Sencio, V.; Barthelemy, A.; Tavares, L.P.; Machado, M.G.; Soulard, D.; Cuinat, C.; Queiroz-Junior, C.M.; Noordine, M.-L.; Salomé-Desnoulez, S.; Deryuter, L.; et al. Gut Dysbiosis during Influenza Contributes to Pulmonary Pneumococcal Superinfection through Altered Short-Chain Fatty Acid Production. Cell Rep. 2020, 30, 2934–2947.e6. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, A.; Lam, L.; Rajendram, M.; Tamburini, F.; Honeycutt, J.; Pham, T.; Van Treuren, W.; Pruss, K.; Stabler, S.R.; Lugo, K.; et al. A Gut Commensal-Produced Metabolite Mediates Colonization Resistance to Salmonella Infection. Cell Host Microbe 2018, 24, 296–307.e7. [Google Scholar] [CrossRef] [PubMed]
- Vemuri, R.; Gundamaraju, R.; Shinde, T.; Perera, A.P.; Basheer, W.; Southam, B.; Gondalia, S.V.; Karpe, A.V.; Beale, D.J.; Tristram, S.; et al. Lactobacillus acidophilus DDS-1 Modulates Intestinal-Specific Microbiota, Short-Chain Fatty Acid and Immunological Profiles in Aging Mice. Nutrients 2019, 11, 1297. [Google Scholar] [CrossRef] [PubMed]
- Hochbaum, A.I.; Kolodkin-Gal, I.; Foulston, L.; Kolter, R.; Aizenberg, J.; Losick, R. Inhibitory effects of D-amino acids on Staphylococcus aureus biofilm development. J. Bacteriol. 2011, 193, 5616–5622. [Google Scholar] [CrossRef]
- Sassone-Corsi, M.; Nuccio, S.-P.; Liu, H.; Hernandez, D.; Vu, C.T.; Takahashi, A.A.; Edwards, R.A.; Raffatellu, M. Microcins mediate competition among Enterobacteriaceae in the inflamed gut. Nature 2016, 540, 280–283. [Google Scholar] [CrossRef]
- Upatissa, S.; Mitchell, R.J. The “Cins” of Our Fathers: Rejuvenated Interest in Colicins to Combat Drug Resistance. J. Microbiol. 2023, 61, 145–158. [Google Scholar] [CrossRef]
- Ben Said, L.; Emond-Rheault, J.-G.; Soltani, S.; Telhig, S.; Zirah, S.; Rebuffat, S.; Diarra, M.S.; Goodridge, L.; Levesque, R.C.; Fliss, I. Phenomic and genomic approaches to studying the inhibition of multiresistant Salmonella enterica by microcin J25. Environ. Microbiol. 2020, 22, 2907–2920. [Google Scholar] [CrossRef]
- Martin-Gómez, H.; Jorba, M.; Albericio, F.; Viñas, M.; Tulla-Puche, J. Chemical Modification of Microcin J25 Reveals New Insights on the Stereospecific Requirements for Antimicrobial Activity. Int. J. Mol. Sci. 2019, 20, 5152. [Google Scholar] [CrossRef]
- Guesdon, W.; Pezier, T.; Menard, S.; Nicolosi, A.; Le Vern, Y.; Silvestre, A.; Diana, J.; Laurent, F.; Lacroix-Lamandé, S. Cryptosporidium parvum Subverts Antimicrobial Activity of CRAMP by Reducing Its Expression in Neonatal Mice. Microorganisms 2020, 8, 1635. [Google Scholar] [CrossRef]
- Sabiá Júnior, E.F.; Menezes, L.F.S.; de Araújo, I.F.S.; Schwartz, E.F. Natural Occurrence in Venomous Arthropods of Antimicrobial Peptides Active against Protozoan Parasites. Toxins 2019, 11, 563. [Google Scholar] [CrossRef]
- Mahdavi Abhari, F.; Pirestani, M.; Dalimi, A. Anti-amoebic activity of a cecropin-melittin hybrid peptide (CM11) against trophozoites of Entamoeba histolytica. Wien. Klin. Wochenschr. 2019, 131, 427–434. [Google Scholar] [CrossRef]
- Yang, J.-Y.; Kim, M.-S.; Kim, E.; Cheon, J.H.; Lee, Y.-S.; Kim, Y.; Lee, S.-H.; Seo, S.-U.; Shin, S.-H.; Choi, S.S.; et al. Enteric Viruses Ameliorate Gut Inflammation via Toll-like Receptor 3 and Toll-like Receptor 7-Mediated Interferon-β Production. Immunity 2016, 44, 889–900. [Google Scholar] [CrossRef] [PubMed]
- Tsigalou, C.; Konstantinidis, T.; Stavropoulou, E.; Bezirtzoglou, E.E.; Tsakris, A. Potential elimination of human gut resistome by exploiting the benefits of functional foods. Front. Microbiol. 2020, 11, 50. [Google Scholar] [CrossRef] [PubMed]
- Nath, A.; Bhattacharjee, R.; Nandi, A.; Sinha, A.; Kar, S.; Manoharan, N.; Mitra, S.; Mojumdar, A.; Panda, P.K.; Patro, S.; et al. Phage delivered CRISPR-Cas system to combat multidrug-resistant pathogens in gut microbiome. Biomed. Pharmacother. 2022, 151, 113122. [Google Scholar] [CrossRef]
- Zhang, Y.; Lin, Y.; Galgano, S.; Houdijk, J.; Xie, W.; Jin, Y.; Lin, J.; Song, W.; Fu, Y.; Li, X.; et al. Recent Progress in Phage Therapy to Modulate Multidrug-Resistant Acinetobacter baumannii, including in Human and Poultry. Antibiotics 2022, 11, 1406. [Google Scholar] [PubMed]
- Jeon, J.; Kim, J.-w.; Yong, D.; Lee, K.; Chong, Y. Complete Genome Sequence of the Podoviral Bacteriophage YMC/09/02/B1251 ABA BP, Which Causes the Lysis of an OXA-23-Producing Carbapenem-Resistant Acinetobacter baumannii Isolate from a Septic Patient. J. Virol. 2012, 86, 12437–12438. [Google Scholar] [CrossRef]
- Wu, M.; Hu, K.; Xie, Y.; Liu, Y.; Mu, D.; Guo, H.; Zhang, Z.; Zhang, Y.; Chang, D.; Shi, Y. A novel phage PD-6A3, and its endolysin Ply6A3, with extended lytic activity against Acinetobacter baumannii. Front. Microbiol. 2019, 9, 3302. [Google Scholar] [CrossRef]
- Wang, R.; Shu, X.; Zhao, H.; Xue, Q.; Liu, C.; Wu, A.; Cheng, F.; Wang, L.; Zhang, Y.; Feng, J.; et al. Associate toxin-antitoxin with CRISPR-Cas to kill multidrug-resistant pathogens. Nat. Commun. 2023, 14, 2078. [Google Scholar] [CrossRef]
- Gencay, Y.E.; Jasinskytė, D.; Robert, C.; Semsey, S.; Martínez, V.; Petersen, A.Ø.; Brunner, K.; de Santiago Torio, A.; Salazar, A.; Turcu, I.C.; et al. Engineered phage with antibacterial CRISPR–Cas selectively reduce E. coli burden in mice. Nat. Biotechnol. 2023. [Google Scholar] [CrossRef]
- Roson-Calero, N.; Ballesté-Delpierre, C.; Fernández, J.; Vila, J. Insights on Current Strategies to Decolonize the Gut from Multidrug-Resistant Bacteria: Pros and Cons. Antibiotics 2023, 12, 1074. [Google Scholar] [CrossRef]
- Strati, F.; Lattanzi, G.; Amoroso, C.; Facciotti, F. Microbiota-targeted therapies in inflammation resolution. Semin. Immunol. 2022, 59, 101599. [Google Scholar] [CrossRef] [PubMed]
- Pinu, F.R.; Beale, D.J.; Paten, A.M.; Kouremenos, K.; Swarup, S.; Schirra, H.J.; Wishart, D. Systems Biology and Multi-Omics Integration: Viewpoints from the Metabolomics Research Community. Metabolites 2019, 9, 76. [Google Scholar] [CrossRef] [PubMed]
- Balvočiūtė, M.; Huson, D.H. SILVA, RDP, Greengenes, NCBI and OTT—How do these taxonomies compare? BMC Genom. 2017, 18, 114. [Google Scholar] [CrossRef] [PubMed]
- Nagarajan, M. Metagenomics: Perspectives, methods, and applications. In Metagenomics; Academic Press: London, UK, 2018. [Google Scholar]
- Antoine, L.; Bruno, D. Advances in high-resolution accurate mass spectrometry application to targeted proteomics. PROTEOMICS 2015, 15, 880–890. [Google Scholar] [CrossRef]
- Heyer, R.; Schallert, K.; Zoun, R.; Becher, B.; Saake, G.; Benndorf, D. Challenges and perspectives of metaproteomic data analysis. J. Biotechnol. 2017, 261, 24–36. [Google Scholar] [CrossRef]
- Bi, H.; Krausz, K.; Manna, S.; Li, F.; Johnson, C.; Gonzalez, F. Optimization of harvesting, extraction, and analytical protocols for UPLC-ESI-MS-based metabolomic analysis of adherent mammalian cancer cells. Anal. Bioanal. Chem. 2013, 405, 5279–5289. [Google Scholar] [CrossRef]
- Marcinowska, R.; Trygg, J.; Wolf-Watz, H.; Mortiz, T.; Surowiec, I. Optimization of a sample preparation method for the metabolomic analysis of clinically relevant bacteria. J. Microbiol. Meth. 2011, 87, 24–31. [Google Scholar] [CrossRef]
- Beale, D.; Barratt, R.; Marlow, D.; Dunn, M.; Palombo, E.; Morrison, P.; Key, C. Application of metabolomics to understanding biofilms in water distribution systems: A pilot study. Biofouling 2013, 29, 283–294. [Google Scholar] [CrossRef]
- Beale, D.; Karpe, A.; Ahmed, W.; Cook, S.; Morrison, P.; Staley, C.; Sadowsky, M.; Palombo, E. A community multi-omics approach towards the assessment of surface water quality in an urban river system. Int. J. Environ. Res. Public Health 2017, 14, 303. [Google Scholar] [CrossRef]
- Beale, D.J.; Morrison, P.D.; Palombo, E.A. Detection of Listeria in milk using non-targeted metabolic profiling of Listeria monocytogenes: A proof-of-concept application. Food Control 2014, 42, 343–346. [Google Scholar] [CrossRef]
- Meijer, S.; Otero, J.; Olivares, R.; Andersen, M.R.; Olsson, L.; Nielsen, J. Overexpression of isocitrate lyase—Glyoxylate bypass influence on metabolism in Aspergillus niger. Metab. Eng. 2009, 11, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Maier, K.; Hofmann, U.; Bauer, A.; Niebel, A.; Vacun, G.; Reuss, M.; Mauch, K. Quantification of statin effects on hepatic cholesterol synthesis by transient 13C-flux analysis. Metab. Eng. 2009, 11, 292–309. [Google Scholar] [CrossRef] [PubMed]
- Niklas, J.; Schneider, K.; Heinzle, E. Metabolic flux analysis in eukaryotes. Curr. Opin. Biotech. 2010, 21, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Beale, D.J.; Morrison, P.D.; Karpe, A.V.; Dunn, M.S. Chemometric Analysis of Lavender Essential Oils Using Targeted and Untargeted GC-MS Acquired Data for the Rapid Identification and Characterization of Oil Quality. Molecules 2017, 22, 1339. [Google Scholar] [CrossRef] [PubMed]
- Driouch, H.; Melzer, G.; Wittmann, C. Integration of in vivo and in silico metabolic fluxes for improvement of recombinant protein production. Metab. Eng. 2012, 14, 47–58. [Google Scholar] [CrossRef]
- Pedersen, H.; Carlsen, M.; Nielsen, J. Identification of enzymes and quantification of metabolic fluxes in the wild type and in a recombinant Aspergillus oryzae strain. Appl. Environ. Microb. 1999, 65, 11–19. [Google Scholar] [CrossRef]
- Beale, D.J.; Kouremenos, K.A.; Palombo, E.A. Microbial Metabolomics; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar]
- Jinawath, N.; Bunbanjerdsuk, S.; Chayanupatkul, M.; Ngamphaiboon, N.; Asavapanumas, N.; Svasti, J.; Charoensawan, V. Bridging the gap between clinicians and systems biologists: From network biology to translational biomedical research. J. Transl. Med. 2016, 14, 324. [Google Scholar] [CrossRef]
- Douglas, G.M.; Maffei, V.J.; Zaneveld, J.R.; Yurgel, S.N.; Brown, J.R.; Taylor, C.M.; Huttenhower, C.; Langille, M.G. PICRUSt2 for prediction of metagenome functions. Nat. Biotechnol. 2020, 38, 685–688. [Google Scholar] [CrossRef]
- McNally, C.P.; Eng, A.; Noecker, C.; Gagne-Maynard, W.C.; Borenstein, E. BURRITO: An interactive multi-omic tool for visualizing taxa–function relationships in microbiome data. Front. Microbiol. 2018, 9, 365. [Google Scholar] [CrossRef]
- Chong, J.; Soufan, O.; Li, C.; Caraus, I.; Li, S.; Bourque, G.; Wishart, D.S.; Xia, J. MetaboAnalyst 4.0: Towards more transparent and integrative metabolomics analysis. Nucleic Acids Res. 2018, 46, W486–W494. [Google Scholar] [CrossRef]
- Karpe, A.V.; Liu, J.-W.; Shah, A.; Koloski, N.; Holtmann, G.; Beale, D.J. Utilising lipid and, arginine and proline metabolism in blood plasma to differentiate the biochemical expression in functional dyspepsia (FD) and irritable bowel syndrome (IBS). Metabolomics 2022, 18, 38. [Google Scholar] [CrossRef] [PubMed]
- Karpe, A.V.; Nguyen, T.V.; Shah, R.M.; Au, G.G.; McAuley, A.J.; Marsh, G.A.; Riddell, S.; Vasan, S.S.; Beale, D.J. A Time-Series Metabolomic Analysis of SARS-CoV-2 Infection in a Ferret Model. Metabolites 2022, 12, 1151. [Google Scholar] [CrossRef] [PubMed]
- Beale, D.J.; Shah, R.; Karpe, A.V.; Hillyer, K.E.; McAuley, A.J.; Au, G.G.; Marsh, G.A.; Vasan, S.S. Metabolic Profiling from an Asymptomatic Ferret Model of SARS-CoV-2 Infection. Metabolites 2021, 11, 327. [Google Scholar] [CrossRef] [PubMed]
- Attia, S.; Versloot, C.J.; Voskuijl, W.; van Vliet, S.J.; Di Giovanni, V.; Zhang, L.; Richardson, S.; Bourdon, C.; Netea, M.G.; Berkley, J.A.; et al. Mortality in children with complicated severe acute malnutrition is related to intestinal and systemic inflammation: An observational cohort study. Am. J. Clin. Nutr. 2016, 104, 1441–1449. [Google Scholar] [CrossRef]
- Calder, N.; Walsh, K.; Olupot-Olupot, P.; Ssenyondo, T.; Muhindo, R.; Mpoya, A.; Brignardello, J.; Wang, X.; McKay, E.; Morrison, D.; et al. Modifying gut integrity and microbiome in children with severe acute malnutrition using legume-based feeds (MIMBLE): A pilot trial. Cell Rep. Med. 2021, 2, 100280. [Google Scholar] [CrossRef]
- Muller Bark, J.; Karpe, A.V.; Doecke, J.D.; Leo, P.; Jeffree, R.L.; Chua, B.; Day, B.W.; Beale, D.J.; Punyadeera, C. A pilot study: Metabolic profiling of plasma and saliva samples from newly diagnosed glioblastoma patients. Cancer Med. 2023, 12, 11427–11437. [Google Scholar] [CrossRef]
- Durán, C.; Ciucci, S.; Palladini, A.; Ijaz, U.Z.; Zippo, A.G.; Sterbini, F.P.; Masucci, L.; Cammarota, G.; Ianiro, G.; Spuul, P.; et al. Nonlinear machine learning pattern recognition and bacteria-metabolite multilayer network analysis of perturbed gastric microbiome. Nat. Commun. 2021, 12, 1926. [Google Scholar] [CrossRef]
- Arnold, B.F.; van der Laan, M.J.; Hubbard, A.E.; Steel, C.; Kubofcik, J.; Hamlin, K.L.; Moss, D.M.; Nutman, T.B.; Priest, J.W.; Lammie, P.J. Measuring changes in transmission of neglected tropical diseases, malaria, and enteric pathogens from quantitative antibody levels. PLoS Neglected Trop. Dis. 2017, 11, e0005616. [Google Scholar] [CrossRef]
- Jain, H.A.; Agarwal, V.; Bansal, C.; Kumar, A.; Faheem; Mohammed, M.-U.-R.; Murugesan, S.; Simpson, M.M.; Karpe, A.V.; Chandra, R.; et al. CoviRx: A User-Friendly Interface for Systematic Down-Selection of Repurposed Drug Candidates for COVID-19. Data 2022, 7, 164. [Google Scholar] [CrossRef]
- Gouws, M. The Comparative Effects of Essential Oil Compounds and Monensin in the Diet of Pre-Weaned Calves on Animal Growth, Performance and the Prevalence of Antibiotic Resistant Escherichia coli and Salmonella spp.; Stellenbosch University: Stellenbosch, South Africa, 2023. [Google Scholar]
- Cunningham, M.; Azcarate-Peril, M.A.; Barnard, A.; Benoit, V.; Grimaldi, R.; Guyonnet, D.; Holscher, H.D.; Hunter, K.; Manurung, S.; Obis, D.; et al. Shaping the Future of Probiotics and Prebiotics. Trends Microbiol. 2021, 29, 667–685. [Google Scholar] [CrossRef]
- Gibbons, S.M.; Gurry, T.; Lampe, J.W.; Chakrabarti, A.; Dam, V.; Everard, A.; Goas, A.; Gross, G.; Kleerebezem, M.; Lane, J.; et al. Perspective: Leveraging the Gut Microbiota to Predict Personalized Responses to Dietary, Prebiotic, and Probiotic Interventions. Adv. Nutr. 2022, 13, 1450–1461. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Sood, U.; Kaur, J.; Anand, S.; Gupta, V.; Patil, K.S.; Lal, R. The rising dominance of microbiology: What to expect in the next 15 years? Microb. Biotechnol. 2022, 15, 110–128. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karpe, A.V.; Beale, D.J.; Tran, C.D. Intelligent Biological Networks: Improving Anti-Microbial Resistance Resilience through Nutritional Interventions to Understand Protozoal Gut Infections. Microorganisms 2023, 11, 1800. https://doi.org/10.3390/microorganisms11071800
Karpe AV, Beale DJ, Tran CD. Intelligent Biological Networks: Improving Anti-Microbial Resistance Resilience through Nutritional Interventions to Understand Protozoal Gut Infections. Microorganisms. 2023; 11(7):1800. https://doi.org/10.3390/microorganisms11071800
Chicago/Turabian StyleKarpe, Avinash V., David J. Beale, and Cuong D. Tran. 2023. "Intelligent Biological Networks: Improving Anti-Microbial Resistance Resilience through Nutritional Interventions to Understand Protozoal Gut Infections" Microorganisms 11, no. 7: 1800. https://doi.org/10.3390/microorganisms11071800
APA StyleKarpe, A. V., Beale, D. J., & Tran, C. D. (2023). Intelligent Biological Networks: Improving Anti-Microbial Resistance Resilience through Nutritional Interventions to Understand Protozoal Gut Infections. Microorganisms, 11(7), 1800. https://doi.org/10.3390/microorganisms11071800






