Impact of Multidrug-Resistant Organisms on Severe Acquired Brain Injury Rehabilitation: An Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Sources and Measurements
2.3. Statistical Methods
3. Results
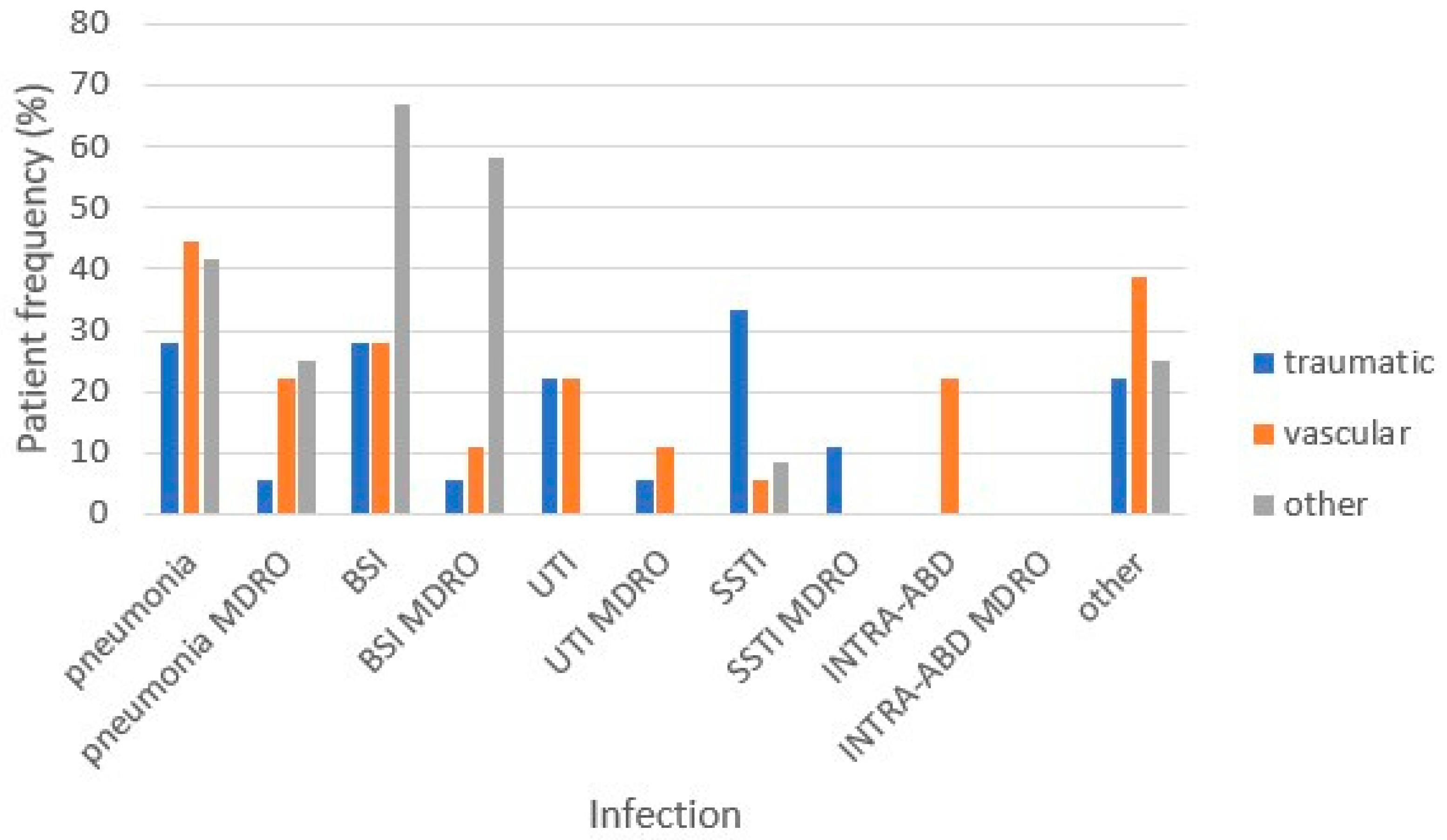
3.1. HAI Incidence
3.2. HAI Incidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ceravolo, M.G.; de Sire, A.; Andrenelli, E.; Negrini, F.; Negrini, S. Systematic rapid “living” review on rehabilitation needs due to COVID-19: Update to March 31st, 2020. Eur. J. Phys. Rehabil. Med. 2020, 56, 347–353, Update in Eur. J. Phys. Rehabil. Med. 2020, 56, 354–360; Update in Eur. J. Phys. Rehabil. Med. 2020, 56, 508–514. [Google Scholar] [CrossRef] [PubMed]
- OECD. Stemming the Superbug Tide: Just a Few Dollars More. In OECD Health Policy Studies; OECD Publishing: Paris, France, 2018. [Google Scholar] [CrossRef]
- Available online: https://www.who.int/news-room/detail/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 12 April 2024).
- Teasell, R.; Bayona, N.; Marshall, S.; Cullen, N.; Bayley, M.; Chundamala, J.; Villamere, J.; Mackie, D.; Rees, L.; Hartridge, C.; et al. A systematic review of the rehabilitation of moderate to severe acquired brain injuries. Brain Inj. 2007, 21, 107–112. [Google Scholar] [CrossRef]
- Grabljevec, K.; Singh, R.; Denes, Z.; Angerova, Y.; Nunes, R.; Boldrini, P.; Delargy, M.; Laxe, S.; Kiekens, C.; Varela Donoso, E.; et al. Evidence-based position paper on Physical and Rehabilitation Medicine professional practice for Adults with Acquired Brain Injury. The European PRM position (UEMS PRM Section). Eur. J. Phys. Rehabil. Med. 2018, 54, 971–979. [Google Scholar] [CrossRef]
- Kourbeti, I.S.; Vakis, A.F.; Papadakis, J.A.; Karabetsos, D.A.; Bertsias, G.; Filippou, M.; Ioannou, A.; Neophytou, C.; Anastasaki, M.; Samonis, G. Infections in traumatic brain injury patients. Clin. Microbiol. Infect. 2012, 18, 359–364. [Google Scholar] [CrossRef]
- Godbolt, A.K.; Stenberg, M.; Jakobsson, J.; Sorjonen, K.; Krakau, K.; Stålnacke, B.M.; Nygren DeBoussard, C. Subacute complications during recovery from severe traumatic brain injury: Frequency and associations with outcome. BMJ Open 2015, 5, e007208. [Google Scholar] [CrossRef]
- Dziedzic, T.; Slowik, A.; Szczudlik, A. Nosocomial infections and immunity: Lesson from brain-injured patients. Crit. Care 2004, 8, 266–270. [Google Scholar] [CrossRef]
- Rollnik, J.D. Outcome of MRSA carriers in neurological early rehabilitation. BMC Neurol. 2014, 14, 34. [Google Scholar] [CrossRef]
- Filozov, A.; Visintainer, P.; Carbonaro, C.; Aguero-Rosenfeld, M.; Wormser, G.P.; Montecalvo, M.A. Epidemiology of an outbreak of antibiotic-resistant Klebsiella pneumoniae at a tertiary care medical center. Am. J. Infect. Control 2009, 37, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Valsdottir, F.; Elfarsdottir Jelle, A.; Gudlaugsson, O.; Hilmarsdottir, I. Long-lasting outbreak due to CTX-M-15-producing Klebsiella pneumoniae ST336 in a rehabilitation ward: Report and literature review. J. Hosp. Infect. 2017, 97, 42–51. [Google Scholar] [CrossRef]
- Flannery, J.; Land, K. Teaching acute care nurses cognitive assessment using LOCFAS: What’s the best method? J. Neurosci. Nurs. 2001, 33, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Galeoto, G.; Turriziani, S.; Berardi, A.; Sansoni, J.; Santilli, V.; Mascio, M.; Paoloni, M. Levels of Cognitive Functioning Assessment Scale: Italian cross-cultural adaptation and validation. Ann. Ig. Med. Prev. Comunità 2020, 32, 16–26. [Google Scholar] [CrossRef]
- Rappaport, M.; Hall, K.M.; Hopkins, K.; Belleza, T.; Cope, D.N. Disability rating scale for severe head trauma: Coma to community. Arch. Phys. Med. Rehabil. 1982, 63, 118–123. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute Care Hospitals—Protocol Version 5.3; ECDC: Stockholm, Sweden, 2016. [Google Scholar]
- Castellani, G.B.; Maietti, E.; Leonardi, G.; Bertoletti, E.; Trapani, F.; Battistini, A.; Tedeschi, S.; Piperno, R.; Viale, P. Healthcare-associated infections and antimicrobial resistance in severe acquired brain injury: A retrospective multicenter study. Front. Neurol. 2023, 14, 1219862. [Google Scholar] [CrossRef]
- Bartolo, M.; Zucchella, C.; Aabid, H.; Valoriani, B.; Copetti, M.; Fontana, A.; Intiso, D.; Mancuso, M. Impact of healthcare-associated infections on functional outcome of severe acquired brain injury during inpatient rehabilitation. Sci. Rep. 2022, 12, 5245. [Google Scholar] [CrossRef]
- Giani, T.; Pini, B.; Arena, F.; Conte, V.; Bracco, S.; Migliavacca, R.; AMCLI-CRE Survey Participants; Pantosti, A.; Pagani, L.; Luzzaro, F.; et al. Epidemic diffusion of KPC carbapenemase-producing Klebsiella pneumoniae in Italy: Results of the first countrywide survey, 15 May to 30 June 2011. Euro Surveill. 2013, 18, 20489. [Google Scholar] [CrossRef]
- Tedeschi, S.; Trapani, F.; Liverani, A.; Tumietto, F.; Cristini, F.; Pignanelli, S.; Berlingeri, A.; Bonavita, J.; Belloni, G.P.; Bartoletti, M.; et al. The burden of colonization and infection by carbapenemase-producing Enterobacteriaceae in the neuro-rehabilitation setting: A prospective six-year experience. Infect. Control. Hosp. Epidemiol. 2019, 40, 368–371. [Google Scholar] [CrossRef]
- Zembower, N.R.; Zhu, A.; Malczynski, M.; Qi, C. Klebsiella pneumoniae carbapenemase-producing K. pneumoniae (KPC-KP) in brain and spinal cord injury patients: Potential for prolonged colonization. Spinal Cord 2017, 55, 390–395. [Google Scholar] [CrossRef]
- Bartolo, M.; Zucchella, C.; Aabid, H.; Valoriani, B.; Mancuso, M.; Intiso, D. Healthcare-Associated Infections in Subjects with Severe Acquired Brain Injury: The Effect of Microbial Colonization on the Functional Outcome. Data from a Multicenter Observational Study. Front. Neurol. 2020, 11, 563275. [Google Scholar] [CrossRef]
- Whyte, J.; Nordenbo, A.M.; Kalmar, K.; Merges, B.; Bagiella, E.; Chang, H.; Yablon, S.; Cho, S.; Hammond, F.; Khademi, A.; et al. Medical complications during inpatient rehabilitation among patients with traumatic disorders of consciousness. Arch. Phys. Med. Rehabil. 2013, 94, 1877–1883. [Google Scholar] [CrossRef] [PubMed]
- Westendorp, W.F.; Nederkoorn, P.J.; Vermeij, J.D.; Dijkgraaf, M.G.; van de Beek, D. Post-stroke infection: A systematic review and meta-analysis. BMC Neurol. 2011, 11, 110. [Google Scholar] [CrossRef] [PubMed]
- Helling, T.S.; Evans, L.L.; Fowler, D.L.; Hays, L.V.; Kennedy, F.R. Infectious complications in patients with severe head injury. J. Trauma 1988, 28, 1575–1577. [Google Scholar] [CrossRef]
- Zanaty, M.; Chalouhi, N.; Starke, R.M.; Clark, S.W.; Bovenzi, C.D.; Saigh, M.; Schwartz, E.; Kunkel, E.S.; Efthimiadis-Budike, A.S.; Jabbour, P.; et al. Complications following cranioplasty: Incidence and predictors in 348 cases. J. Neurosurg. 2015, 123, 182–188. [Google Scholar] [CrossRef]
- Di Stefano, C.; Sturiale, C.; Trentini, P.; Bonora, R.; Rossi, D.; Cervigni, G.; Piperno, R. Unexpected neuropsychological improvement after cranioplasty: A case series study. Br. J. Neurosurg. 2012, 26, 827–831. [Google Scholar] [CrossRef]
- Zheng, F.; Xu, H.; von Spreckelsen, N.; Stavrinou, P.; Timmer, M.; Goldbrunner, R.; Cao, F.; Ran, Q.; Li, G.; Fan, R.; et al. Early or late cranioplasty following decompressive craniotomy for traumatic brain injury: A systematic review and meta-analysis. J. Int. Med. Res. 2018, 46, 2503–2512. [Google Scholar] [CrossRef]
- Hayden, M.K.; Lin, M.Y.; Lolans, K.; Weiner, S.; Blom, D.; Moore, N.M.; Fogg, L.; Henry, D.; Lyles, R.; Thurlow, C.; et al. Prevention of colonization and infection by Klebsiella pneumoniae carbapenemase-producing enterobacteriaceae in long-term acute-care hospitals. Clin. Infect. Dis. 2015, 60, 1153–1161. [Google Scholar] [CrossRef]
- Bellaviti, G.; Balsamo, F.; Iosa, M.; Vella, D.; Pistarini, C. Influence of systemic infection and comorbidities on rehabilitation outcomes in severe acquired brain injury. Eur. J. Phys. Rehabil. Med. 2021, 57, 69–77. [Google Scholar] [CrossRef]

| Study Sample | N = 48 |
|---|---|
| Male, n (%) | 30 (62.5%) |
| Age, mean ± SD | 52.4 ± 16.2 |
| Etiology, n (%) | |
| Traumatic | 18 (37.5%) |
| Associated trauma * | 16 (88.9%) |
| Vascular | 18 (37.5%) |
| Other (anoxic, metabolic, neoplastic and infective–inflammatory) | 12 (25%) |
| Comorbidity, n (%) | 10 (20.8%) |
| Pre-admission surgery | |
| No | 19 (39.6%) |
| Neurosurgery | 26 (54.2%) |
| Other (abdominal and skeletal surgery) | 3 (6.2%) |
| LCF upon admission, mean ± SD | 3.9 ± 1.7 |
| DRS upon admission, mean ± SD | 18.7 ± 6.2 |
| Transfers, n (%) | 23 (47.9%) |
| Surgery during hospitalization | |
| No | 26 (54.2%) |
| Neurosurgery | 15 (31.2%) |
| Other (abdominal and skeletal surgery) | 7 (14.6%) |
| CPE colonization, n (%) | |
| No | 17 (35.4%) |
| Upon admission | 15 (31.3%) |
| During hospitalization | 16 (33.3%) |
| Complications, n (%) | 37 (77.1%) |
| Length of stay, median (IQ range) | 206 (122–273) |
| Medical devices | |
| Indwelling catheter, n (%) | 45 (93.8%) |
| days, median (IQ range) | 71 (24–107) |
| Central venous catheter, n (%) | 27 (56.3%) |
| days, median (IQ range) | 41 (7–58) |
| Tracheotomy tube, n (%) | 41 (85.4%) |
| days, median (IQ range) | 135 (50–233) |
| PEG or PEJ, n (%) | 30 (62.5%) |
| days, median (IQ range) | 234 (122–299) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castellani, G.B.; Maietti, E.; Colombo, V.; Clemente, S.; Cassani, I.; Rucci, P. Impact of Multidrug-Resistant Organisms on Severe Acquired Brain Injury Rehabilitation: An Observational Study. Microorganisms 2024, 12, 830. https://doi.org/10.3390/microorganisms12040830
Castellani GB, Maietti E, Colombo V, Clemente S, Cassani I, Rucci P. Impact of Multidrug-Resistant Organisms on Severe Acquired Brain Injury Rehabilitation: An Observational Study. Microorganisms. 2024; 12(4):830. https://doi.org/10.3390/microorganisms12040830
Chicago/Turabian StyleCastellani, Giovanna Barbara, Elisa Maietti, Valentina Colombo, Stefano Clemente, Ivo Cassani, and Paola Rucci. 2024. "Impact of Multidrug-Resistant Organisms on Severe Acquired Brain Injury Rehabilitation: An Observational Study" Microorganisms 12, no. 4: 830. https://doi.org/10.3390/microorganisms12040830





