Congenital Sepsis with Candida albicans—A Rare Event in the Neonatal Period: Report of Two Cases and Literature Review
Abstract
:1. Introduction
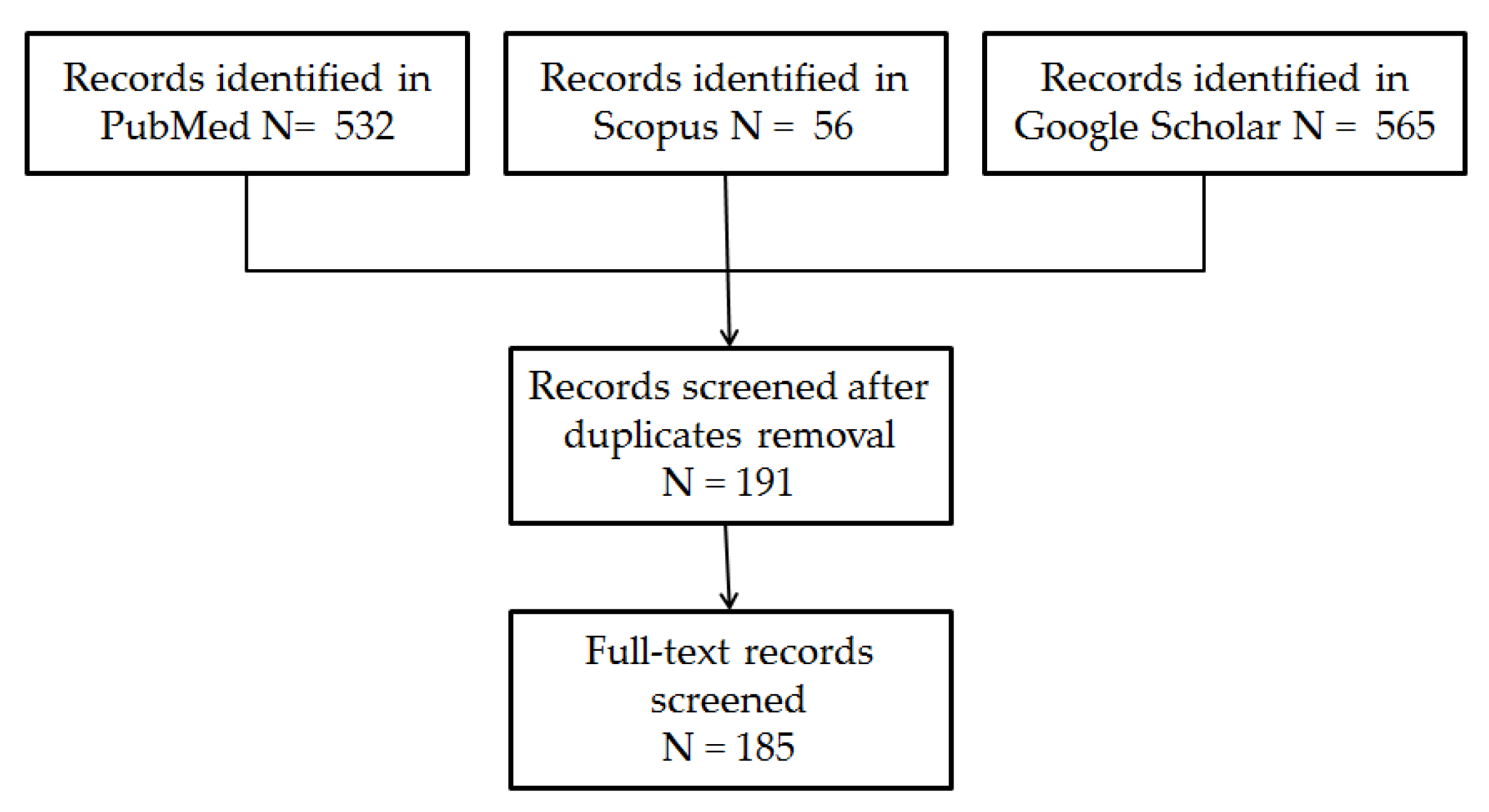
2. Material and Methods
2.1. Case Reports
2.1.1. Case Report 1
Medical History
Initial Assessment, Hematology, and Radiology Investigations
Microbiology Investigations, Treatment
Clinical Course and Outcome
2.1.2. Case Report 2
Medical History
Initial Assessment, Investigations, and Management
Microbiology Investigations and Treatment
Clinical Course, Complications, and Outcome
2.2. Review of the Literature
3. Discussion
3.1. General Aspects
3.1.1. Epidemiological Aspects
3.1.2. Classification
3.1.3. Etiology
3.1.4. Risk Factors
3.1.5. Risk Factors for Invasive Congenital Candidiasis
3.1.6. Comments on Reported Cases
3.2. Physiopathology
3.2.1. Transmission Pathways
3.2.2. Comments on Reported Cases
3.3. Clinical Aspects
3.3.1. Cutaneous Involvement
3.3.2. Systemic Involvement
3.3.3. Comments on Reported Cases
3.4. Diagnosis
3.4.1. Suspected Candidiasis at Birth
3.4.2. Blood Culture
3.4.3. Other Laboratory Investigations
3.4.4. Imaging
3.4.5. Differential Diagnosis
3.4.6. Comments on Reported Cases
3.5. Treatment
3.5.1. General Aspects
3.5.2. Antifungals
3.5.3. Supportive Treatment
3.5.4. Comments on Reported Cases
3.6. Clinical Course and Complications
3.6.1. General Aspects
3.6.2. Comments on Reported Cases
3.7. Prevention
4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, L.; Johnson, H.L.; Cousens, S.; Perin, J.; Scott, S.; Lawn, J.E.; Rudan, I.; Campbell, H.; Cibulskis, R.; Li, M.; et al. Child Health Epidemiology Reference Group of WHO and UNICEF. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet 2012, 379, 2151–2161. [Google Scholar] [CrossRef] [PubMed]
- Odabasi, I.O.; Bulbul, A. Neonatal Sepsis. Sisli Etfal Hastan. Tip Bul. 2020, 54, 142–158. [Google Scholar] [CrossRef]
- Cohen-Wolkowiez, M.; Moran, C.; Benjamin, D.K.; Cotten, C.M.; Clark, R.H.; Benjamin, D.K., Jr.; Smith, P.B. Early and late onset sepsis in late preterm infants. Pediatr. Infect. Dis. J. 2009, 28, 1052–1056. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Sánchez, P.J.; Faix, R.G.; Poindexter, B.B.; Van Meurs, K.P.; Bizzarro, M.J.; Goldberg, R.N.; Frantz, I.D., 3rd; Hale, E.C.; et al. Early onset neonatal sepsis: The burden of group B Streptococcal and E. coli disease continues. Pediatrics 2011, 127, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Turhan, E.E.; Gürsoy, T.; Ovalı, F. Factors which affect mortality in neonatal sepsis. Turk Pediatri Ars. 2015, 50, 170–175. [Google Scholar] [CrossRef]
- Johansson Gudjónsdóttir, M.; Elfvin, A.; Hentz, E.; Adlerberth, I.; Tessin, I.; Trollfors, B. Changes in incidence and etiology of early-onset neonatal infections 1997–2017—A retrospective cohort study in western Sweden. BMC Pediatr. 2019, 19, 490. [Google Scholar] [CrossRef]
- Sousa, R.A.; Martins Oliveira Diniz, L.; Lapa Marinho, F.E.; Gonçalves Rezende, L.; Machado Carelos, E.; de castro Romanelli, R.M. Risk factors for candidemia in neonates: Systematic review and meta-analysis. J. Neonatal Nurs. 2022, 28, 83–92. [Google Scholar] [CrossRef]
- Benjamin, D.K., Jr.; Stoll, B.J.; Gantz, M.G.; Walsh, M.C.; Sánchez, P.J.; Das, A.; Shankaran, S.; Higgins, R.D.; Auten, K.J.; Miller, N.A.; et al. Neonatal candidiasis: Epidemiology, risk factors, and clinical judgment. Pediatrics 2010, 126, e865–e873. [Google Scholar] [CrossRef] [PubMed]
- Klinger, G.; Levy, I.; Sirota, L.; Boyko, V.; Reichman, B.; Lerner-Geva, L.; Israel Neonatal Network. Epidemiology and risk factors for early onset sepsis among very-low-birthweight infants. Am. J. Obstet. Gynecol. 2009, 201, 38.e1–38.e6. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Padilla, A.P.; Valencia-Herrera, A.M.; Toledo-Bahena, M.E.; Mena-Cedillos, C.A.; Duarte-Abdala, M.; Salazar-García, M.; Bonifaz, A. Congenital Cutaneous Candidiasis: Uncommon Entity or Underdiagnosed? Curr. Fungal. Infect. Rep. 2019, 13, 175–180. [Google Scholar] [CrossRef]
- Georgescu, T.A.; Lisievici, A.C.; Munteanu, O.; Furtunescu, F.L.; Bratu, O.G.; Berceanu, C.; Bohîlţea, R.E. Congenital systemic candidiasis: A comprehensive literature review and meta-analysis of 44 cases. Rom. J. Morphol. Embryol. 2020, 61, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Benirschke, K.; Raphael, S.I. Candida albicans infection of the amniotic sac. Am. J. Obstet. Gynecol. 1958, 75, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Barton, M.; Shen, A.; O’Brien, K.; Robinson, J.L.; Davies, H.D.; Simpson, K.; Asztalos, E.; Langley, J.; Le Saux, N.; Sauve, R.; et al. Early-Onset Invasive Candidiasis in Extremely Low Birth Weight Infants: Perinatal Acquisition Predicts Poor Outcome. Clin. Infect. Dis. 2017, 64, 921–927. [Google Scholar] [CrossRef]
- Kaufman, D.A. Challenging issues in neonatal candidiasis. Curr. Med. Res. Opin. 2010, 26, 1769–1778. [Google Scholar] [CrossRef]
- Chitnis, A.S.; Magill, S.S.; Edwards, J.R.; Chiller, T.M.; Fridkin, S.K.; Lessa, F.C. Trends in Candida central line-associated bloodstream infections among NICUs, 1999–2009. Pediatrics 2012, 130, e46–e52. [Google Scholar] [CrossRef]
- Kaufman, D.A. “Getting to Zero”: Preventing invasive Candida infections and eliminating infection-related mortality and morbidity in extremely preterm infants. Early Hum. Dev. 2012, 88 (Suppl. S2), S45–S49. [Google Scholar] [CrossRef]
- Kaufman, D.A. Fungal Infections in Preterm Infants. 27 December 2020. Available online: https://emedicine.medscape.com/article/980487-overview?st=fpf&scode=msp&socialSite=google&form=fpf&icd=login_success_gg_mismatch_fpf (accessed on 10 July 2024).
- Feng, Y.; Lu, H.; Whiteway, M.; Jiang, Y. Understanding fluconazole tolerance in Candida albicans: Implications for effective treatment of candidiasis and combating invasive fungal infections. J. Glob. Antimicrob. Resist. 2023, 35, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Năstase, L.; Rădulescu, L.; Luminos, M.L.; Merisescu, M.M.; Jugulete, G.; Stoicescu, S.M. Severe Modifications of Biological Markers in Late Neonatal Sepsis in a Very Low Birth Weight Due to Candida lusitaniae. Rev. Chim. 2019, 70, 393–397. [Google Scholar] [CrossRef]
- Nouri-Merchaoui, S.; Mahdhaoui, N.; Fekih, M.; Adouani, M.; Zakhama, R.; Methlouthi, J.; Ghith, A.; Seboui, H. Candidose congénitale systémique, forme rare de candidose néonatale: À propos d’une observation chez un nouveau-né prématuré [Systemic congenital candidiasis, a rare condition in neonates: Case report in a premature infant]. Arch. Pediatr. 2011, 18, 303–307. (In French) [Google Scholar] [CrossRef]
- Fernández-Ruiz, M.; Mosqueda-Peña, R.; Pérez-Ayala, A.; Blázquez-Gamero, D. Congenital cutaneous candidiasis associated with maternal peripartum candidemia. Rev. Iberoam. Micol. 2020, 37, 68–71. [Google Scholar] [CrossRef]
- Hammoud, M.S.; Al-Taiar, A.; Fouad, M.; Raina, A.; Khan, Z. Persistent candidemia in neonatal care units: Risk factors and clinical significance. Int. J. Infect. Dis. 2013, 17, e624–e628. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.M.; Hsu, C.H.; Chang, J.H. Congenital candidiasis. Pediatr. Neonatol. 2008, 49, 94–96. [Google Scholar] [CrossRef] [PubMed]
- Aruna, C.; Seetharam, K. Congenital candidiasis. Indian. Dermatol. Online J. 2014, 5 (Suppl. S1), S44–S47. [Google Scholar] [CrossRef] [PubMed]
- Shope, C.; Ritter, A.; Karlin, S.; Lee, L.W.; Cotton, C.H. Congenital Cutaneous Candidiasis in Preterm Infants. Neoreviews 2023, 24, e175–e180. [Google Scholar] [CrossRef]
- Pradeepkumar, V.K.; Rajadurai, V.S.; Tan, K.W. Congenital candidiasis: Varied presentations. J. Perinatol. 1998, 18, 311–316. [Google Scholar] [PubMed]
- Pfaller, M.A.; Diekema, D.J. Epidemiology of invasive candidiasis: A persistent public health problem. Clin. Microbiol. Rev. 2007, 20, 133–163. [Google Scholar] [CrossRef]
- Sanni, U.A.; Lawal, T.O.; Na’uzo, A.M.; Audu, L.I. Invasive Fungal Infection Presenting as Early-Onset Neonatal Sepsis: A Case Report from Northern Nigeria. J. Clin. Neonatol. 2023, 12, 38–41. [Google Scholar] [CrossRef]
- Jung, Y.J. Early- and late-onset candidemia in very low birth weight infants in the Korean neonatal network, 2013–2017. Pediatr. Neonatol. 2024. [Google Scholar] [CrossRef]
- Shane, A.L.; Sánchez, P.J.; Stoll, B.J. Neonatal sepsis. Lancet 2017, 390, 1770–1780. [Google Scholar] [CrossRef]
- Melville, C.; Kempley, S.; Graham, J.; Berry, C.L. Early onset systemic Candida infection in extremely preterm neonates. Eur. J. Pediatr. 1996, 155, 904–906. [Google Scholar] [CrossRef]
- Trofa, D.; Gácser, A.; Nosanchuk, J.D. Candida parapsilosis, an emerging fungal pathogen. Clin. Microbiol. Rev. 2008, 21, 606–625. [Google Scholar] [CrossRef] [PubMed]
- Daniel, K.; Greenberg, R.G.; Boutzoukas, A.; Katakam, L. Updated Perspectives on the Diagnosis and Management of Neonatal Invasive Candidiasis. Res. Rep. Neonatol. 2023, 13, 45–63. [Google Scholar] [CrossRef]
- Weimer, K.E.D.; Smith, P.B.; Puia-Dumitrescu, M.; Aleem, S. Invasive fungal infections in neonates: A review. Pediatr. Res. 2022, 91, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, K.A.; Anderson-Berry, A.L.; Delair, S.F.; Davies, H.D. Early-onset neonatal sepsis. Clin. Microbiol. Rev. 2014, 27, 21–47. [Google Scholar] [CrossRef]
- Messina, A.; Mariani, A.; Brandolisio, R.; Tavella, E.; Germano, C.; Lipari, G.; Leo, L.; Masturzo, B.; Manzoni, P. Candidiasis in Pregnancy: Relevant Aspects of the Pathology for the Mother and the Fetus and Therapeutic Strategies. Trop. Med. Infect. Dis. 2024, 9, 114. [Google Scholar] [CrossRef]
- Waguespack-LaBiche, J.; Chen, S.H.; Yen, A. Disseminated congenital candidiasis in a premature infant. Arch. Dermatol. 1999, 135, 510–512. [Google Scholar] [CrossRef]
- Krallis, N.; Tzioras, S.; Giapros, V.; Leveidiotou, S.; Paschopoulos, M.; Stefanou, D.; Andronikou, S. Congenital candidiasis caused by different Candida species in a dizygotic pregnancy. Pediatr. Infect. Dis. J. 2006, 25, 958–959. [Google Scholar] [CrossRef]
- Arai, H.; Goto, R.; Matsuda, T.; Saito, S.; Hirano, H.; Sanada, H.; Sato, A.; Takada, G. Case of congenital infection with Candida glabrata in one infant in a set of twins. Pediatr. Int. 2002, 44, 449–450. [Google Scholar] [CrossRef]
- Pineda, C.; Kaushik, A.; Kest, H.; Wickes, B.; Zauk, A. Maternal sepsis, chorioamnionitis, and congenital Candida kefyr infection in premature twins. Pediatr. Infect. Dis. J. 2012, 31, 320–322. [Google Scholar] [CrossRef]
- Nichols, A.; Khong, T.Y.; Crowther, C.A. Candida tropicalis chorioamnionitis. Am. J. Obstet. Gynecol. 1995, 172, 1045–1047. [Google Scholar] [CrossRef]
- Chen, W.Y.; Chen, S.J.; Tsai, S.F.; Tsao, P.C.; Tang, R.B.; Soong, W.J. Congenital Systemic Fungus Infection in Twin Prematurity-A Case Report and Literature Review. AJP Rep. 2015, 5, e46–e50. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Cabrera, J.R.; Meléndrez-Vásquez, D.; Moreno, D.M.; Prieto-Jure, R. Congenital cutaneous candidiasis in a premature neonate: A case report. Clin. Case Rep. 2022, 10, e05773. [Google Scholar] [CrossRef]
- Kumar, M.; Saadaoui, M.; Al Khodor, S. Infections and Pregnancy: Effects on Maternal and Child Health. Front. Cell Infect. Microbiol. 2022, 12, 873253. [Google Scholar] [CrossRef]
- Maki, Y.; Fujisaki, M.; Sato, Y.; Sameshima, H. Candida Chorioamnionitis Leads to Preterm Birth and Adverse Fetal-Neonatal Outcome. Infect. Dis. Obstet. Gynecol. 2017, 2017, 9060138. [Google Scholar] [CrossRef] [PubMed]
- Disha, T.; Haque, F. Prevalence and Risk Factors of Vulvovaginal Candidosis during Pregnancy: A Review. Infect. Dis. Obstet. Gynecol. 2022, 2022, 6195712. [Google Scholar] [CrossRef]
- Shazniza Shaaya, E.; Halim, S.A.A.; Leong, K.W.; Ku, K.B.P.; Lim, P.S.; Tan, G.C.; Wong, Y.P. Candida Chorioamnionitis in Mothers with Gestational Diabetes Mellitus: A Report of Two Cases. Int. J. Environ. Res. Public Health 2021, 18, 7450. [Google Scholar] [CrossRef] [PubMed]
- Salusti-Simpson, M.; Marghoob, N.; Greene, L.; Morley, K. Congenital cutaneous candidiasis in a full-term neonate. Pediatr. Dermatol. 2022, 39, 952–954. [Google Scholar] [CrossRef]
- Pammi, M. Candida Infections in Neonates: Epidemiology, Clinical Manifestations, and Diagnosis. 22 May 2024. Available online: https://www.uptodate.com/contents/candida-infections-in-neonates-epidemiology-clinical-manifestations-and-diagnosis (accessed on 25 July 2024).
- Suárez, J.A.G.; Calumby, R.J.N.; Silva, D.P.; Barbosa, V.T.; Maranhão, F.C.A.; Moreira, I.F.; Melhem, M.S.C.; Moreira, R.T.F. Neonatal innate immunity response in invasive candidiasis. Braz. J. Biol. 2024, 84, e275155. [Google Scholar] [CrossRef]
- Michalski, C.; Kan, B.; Lavoie, P.M. Antifungal Immunological Defenses in Newborns. Front. Immunol. 2017, 8, 281. [Google Scholar] [CrossRef]
- Mahieu, L.M.; Van Gasse, N.; Wildemeersch, D.; Jansens, H.; Ieven, M. Number of sites of perinatal Candida colonization and neutropenia are associated with nosocomial candidemia in the neonatal intensive care unit patient. Pediatr. Crit. Care Med. 2010, 11, 240–245. [Google Scholar] [CrossRef]
- Roqué, H.; Abdelhak, Y.; Young, B.K. Intra amniotic candidiasis. Case report and meta-analysis of 54 cases. J. Perinat. Med. 1999, 27, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Jagtap, S.A.; Saple, P.P.; Dhaliat, S.B. Congenital cutaneous candidiasis: A rare and unpredictable disease. Indian. J. Dermatol. 2011, 56, 92–93. [Google Scholar] [CrossRef] [PubMed]
- Blomberg, L.; Backman, K.; Kirjavainen, P.V.; Karvonen, A.M.; Harju, M.; Keski-Nisula, L. Vulvovaginal yeast infections, gestational diabetes and pregnancy outcome. BMC Pregnancy Childbirth 2023, 23, 70. [Google Scholar] [CrossRef]
- Ognean, M.L.; Muntean, A.; Pavel, A.; Boanta, O.; Olariu, E.; Todor, M. Maternal Diabetes Mellitus—Is it a Risk Factor for Congenital Candidiasis? Neonatology 2010, II, 47–52. [Google Scholar]
- Rasti, S.; Asadi, M.A.; Taghriri, A.; Behrashi, M.; Mousavie, G. Vaginal candidiasis complications on pregnant women. Jundishapur J. Microbiol. 2014, 7, e10078. [Google Scholar] [CrossRef]
- Drummond, R.A.; Lionakis, M.S. Candidiasis of the Central Nervous System in Neonates and Children with Primary Immunodeficiencies. Curr. Fungal Infect. Rep. 2018, 12, 92–97. [Google Scholar] [CrossRef]
- Bider, D.; Ben-Rafael, Z.; Barkai, G.; Mashiach, S. Intrauterine fetal death apparently due to Candida chorioamnionitis. Arch. Gynecol. Obstet. 1989, 244, 175–177. [Google Scholar] [CrossRef]
- Guzel, A.B.; Ilkit, M.; Burgut, R.; Urunsak, I.F.; Ozgunen, F.T. An evaluation of risk factors in pregnant women with Candida vaginitis and the diagnostic value of simultaneous vaginal and rectal sampling. Mycopathologia 2011, 172, 25–36. [Google Scholar] [CrossRef]
- Roberts, C.L.; Rickard, K.; Kotsiou, G.; Morris, J.M. Treatment of asymptomatic vaginal candidiasis in pregnancy to prevent preterm birth: An open-label pilot randomized controlled trial. BMC Pregnancy Childbirth 2011, 11, 18. [Google Scholar] [CrossRef] [PubMed]
- Stronati, M.; Decembrino, L. Neonatal invasive candidiasis. Minerva Pediatr. 2006, 58, 537–549. [Google Scholar] [PubMed]
- Torres-Alvarez, B.; Hernandez-Blanco, D.; Ehnis-Perez, A.; Castanedo-Cazares, J.P. Cutaneous congenital candidiasis in a full-term newborn from an asymptomatic mother. Dermatol. Online J. 2013, 19, 18967. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, B.; Ferreira, C.; Alves, C.T.; Henriques, M.; Azeredo, J.; Silva, S. Vulvovaginal candidiasis: Epidemiology, microbiology and risk factors. Crit. Rev. Microbiol. 2016, 42, 905–927. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Tang, R.; Deng, J.; Cai, T.; He, P.; Wu, J.; Cao, Y. Effects of oestrogen on vulvovaginal candidosis. Mycoses 2022, 65, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Vasant, B.; Mathur, A.; De, M. A study of neonatal sepsis due to Candida species. Bombay Hosp. J. 2011, 53, 524–528. [Google Scholar]
- Saiman, L.; Ludington, E.; Pfaller, M.; Rangel-Frausto, S.; Wiblin, R.T.; Dawson, J.; Blumberg, H.M.; Patterson, J.E.; Rinaldi, M.; Edwards, J.E.; et al. Risk factors for candidemia in Neonatal Intensive Care Unit patients. The National Epidemiology of Mycosis Survey study group. Pediatr. Infect. Dis. J. 2000, 19, 319–324. [Google Scholar] [CrossRef]
- Prinsloo, B.; Weldhagen, G.F.; Blaine, R.W. Candida famata central nervous system infection. S. Afr. Med. J. 2003, 93, 601–602. [Google Scholar] [PubMed]
- Manzoni, P.; Farina, D.; Galletto, P.; Leonessa, M.; Priolo, C.; Arisio, R.; Gomirato, G. Type and number of sites colonized by fungi and risk of progression to invasive fungal infection in preterm neonates in neonatal intensive care unit. J. Perinat. Med. 2007, 35, 220–226. [Google Scholar] [CrossRef]
- Darmstadt, G.L.; Dinulos, J.G.; Miller, Z. Congenital cutaneous candidiasis: Clinical presentation, pathogenesis, and management guidelines. Pediatrics 2000, 105, 438–444. [Google Scholar] [CrossRef]
- Arsenault, A.B.; Bliss, J.M. Neonatal Candidiasis: New Insights into an Old Problem at a Unique Host-Pathogen Interface. Curr. Fungal Infect. Rep. 2015, 9, 246–252. [Google Scholar] [CrossRef]
- Aldana-Valenzuela, C.; Morales-Marquec, M.; Castellanos-Martínez, J.; Deanda-Gómez, M. Congenital candidiasis: A rare and unpredictable disease. J. Perinatol. 2005, 25, 680–682. [Google Scholar] [CrossRef]
- Zhao, H.H.; Zhou, Z.; Lu, L.; Zhao, Y.Z.; Yang, L.J.; Ding, Y.X. Congenital candidiasis in a full-term infant: A case report. J. Int. Med. Res. 2023, 51, 3000605231158015. [Google Scholar] [CrossRef] [PubMed]
- Ito, F.; Okubo, T.; Yasuo, T.; Mori, T.; Iwasa, K.; Iwasaku, K.; Kitawaki, J. Premature delivery due to intrauterine Candida infection that caused neonatal congenital cutaneous candidiasis: A case report. J. Obstet. Gynaecol. Res. 2013, 39, 341–343. [Google Scholar] [CrossRef] [PubMed]
- Ganer Herman, H.; Mevorach Zussman, N.; Krajden Haratz, K.; Bar, J.; Sagiv, R. Candida glabrata Chorioamnionitis following in vitro Fertilization: Review of the Literature. Gynecol. Obstet. Investig. 2015, 80, 145–147. [Google Scholar] [CrossRef]
- Obermair, H.M.; Bhagwanani, G.; Caldas, R.; Doyle, H.; Smoleniec, J.; Adno, A. Candida chorioamnionitis associated with late stillbirth: A case report. Case Rep. Womens Health 2020, 27, e00239. [Google Scholar] [CrossRef] [PubMed]
- Diana, A.; Epiney, M.; Ecoffey, M.; Pfister, R.E. “White dots on the placenta and red dots on the baby”: Congential cutaneous candidiasis--a rare disease of the neonate. Acta Paediatr. 2004, 93, 996–999. [Google Scholar] [CrossRef]
- Blanc, W.A. Pathways of fetal and early neonatal infection. Viral placentitis, bacterial and fungal chorioamnionitis. J. Pediatr. 1961, 59, 473–496. [Google Scholar] [CrossRef]
- Jin, Y.; Endo, A.; Shimada, M.; Minato, M.; Takada, M.; Takahashi, S.; Harada, K. Congenital systemic candidiasis. Pediatr. Infect. Dis. J. 1995, 14, 818–820. [Google Scholar]
- Paul, A.A.; Hoffman, K.L.; Hagan, J.L.; Sampath, V.; Petrosino, J.F.; Pammi, M. Fungal cutaneous microbiome and host determinants in preterm and term neonates. Pediatr. Res. 2020, 88, 225–233. [Google Scholar] [CrossRef]
- Miras, I.; Vierge, E.; García, M.; Arruza, L.; Criado, E.; Ramos, J.T.; Martínez-Orgado, J. Congenital Cutaneous Candidiasis with Systemic Dissemination in a Preterm Infant. Pediatr. Infect. Dis. J. 2021, 40, e230–e233. [Google Scholar] [CrossRef]
- Colantonio, S.; Hedin, E.; Li, H.O.; Gavigan, G. Management of congenital cutaneous candidiasis in a healthy term baby: A case report. SAGE Open Med. Case Rep. 2019, 7, 2050313X19876707. [Google Scholar] [CrossRef]
- Almeida Santos, L.; Beceiro, J.; Hernandez, R.; Salas, S.; Escriba, R.; Garcia Frias, E.; Perez Rodriguez, J.; Quero, J. Congenital cutaneous candidiasis: Report of four cases and review of the literature. Eur. J. Pediatr. 1991, 150, 336–338. [Google Scholar] [CrossRef] [PubMed]
- Kucinskiene, V.; Sutkute, A.; Valiukeviciene, S. Cutaneous fungal infection in a neonatal intensive care unit patient: A case report and literature review. Pediatr. Dermatol. 2014, 31, 267–270. [Google Scholar] [CrossRef]
- Korting, H.C.; Patzak, U.; Schaller, M.; Maibach, H.I. A model of human cutaneous candidosis based on reconstructed human epidermis for the light and electron microscopic study of pathogenesis and treatment. J. Infect. 1998, 36, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Scheffler, E.; Miller, G.G.; Classen, D.A. Zygomycotic infection of the neonatal upper extremity. J. Pediatr. Surg. 2003, 38, E16–E17. [Google Scholar] [CrossRef]
- Smolinski, K.N.; Shah, S.S.; Honig, P.J.; Yan, A.C. Neonatal cutaneous fungal infections. Curr. Opin. Pediatr. 2005, 17, 486–493. [Google Scholar] [CrossRef]
- Smith, P.B.; Steinbach, W.J.; Benjamin, D.K., Jr. Neonatal candidiasis. Infect. Dis. Clin. N. Am. 2005, 19, 603–615. [Google Scholar] [CrossRef]
- Ng, P.C.; Siu, Y.K.; Lewindon, P.J.; Wong, W.; Cheung, K.L.; Dawkins, R. Congenital Candida pneumonia in a preterm infant. J. Paediatr. Child Health 1994, 30, 552–554. [Google Scholar] [CrossRef]
- Carmo, K.B.; Evans, N.; Isaacs, D. Congenital candidiasis presenting as septic shock without rash. Arch. Dis. Child. 2007, 92, 627–628. [Google Scholar] [CrossRef] [PubMed]
- Tezer, H.; Canpolat, F.E.; Dilmen, U. Invasive fungal infections during the neonatal period: Diagnosis, treatment and prophylaxis. Expert Opin. Pharmacother. 2012, 13, 193–205. [Google Scholar] [CrossRef]
- Barone, S.R.; Krilov, L.R. Neonatal candidal meningitis in a full-term infant with congenital cutaneous candidiasis. Clin. Pediatr. 1995, 34, 217–219. [Google Scholar] [CrossRef]
- Baradkar, V.P.; Taklikar, S.M. Meningitis caused by Candida albicans in a premature neonate. J. Pediatr. Neurosci. 2007, 2, 90–91. [Google Scholar] [CrossRef]
- Liu, S.H.; Mitchell, H.; Nasser Al-Rawahi, G. Epidemiology and associated risk factors for candidemia in a Canadian tertiary paediatric hospital: An 11-year review. J. Assoc. Med. Microbiol. Infect. Dis. Can. 2023, 8, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Kopanou Taliaka, P.; Tsantes, A.G.; Konstantinidi, A.; Houhoula, D.; Tsante, K.A.; Vaiopoulos, A.G.; Piovani, D.; Nikolopoulos, G.K.; Bonovas, S.; Iacovidou, N.; et al. Risk Factors, Diagnosis, and Treatment of Neonatal Fungal Liver Abscess: A Systematic Review of the Literature. Life 2023, 13, 167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meizoso, T.; Rivera, T.; Fernández-Aceñero, M.J.; Mestre, M.J.; Garrido, M.; Garaulet, C. Intrauterine candidiasis: Report of four cases. Arch. Gynecol. Obstet. 2008, 278, 173–176. [Google Scholar] [CrossRef]
- Qureshi, F.; Jacques, S.M.; Bendon, R.W.; Faye-Peterson, O.M.; Heifetz, S.A.; Redline, R.; Sander, C.M. Candida funisitis: A clinicopathologic study of 32 cases. Pediatr. Dev. Pathol. 1998, 1, 118–124. [Google Scholar] [CrossRef]
- Aliaga, S.; Clark, R.H.; Laughon, M.; Walsh, T.J.; Hope, W.W.; Benjamin, D.K.; Kaufman, D.; Arrieta, A.; Benjamin, D.K., Jr.; Smith, P.B. Changes in the incidence of candidiasis in neonatal intensive care units. Pediatrics 2014, 133, 236–242. [Google Scholar] [CrossRef]
- Ellepola, A.N.; Morrison, C.J. Laboratory diagnosis of invasive candidiasis. J. Microbiol. 2005, 43, 65–84. [Google Scholar] [PubMed]
- Clancy, C.J.; Nguyen, M.H. Finding the “missing 50%” of invasive candidiasis: How nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin. Infect. Dis. 2013, 56, 1284–1292. [Google Scholar] [CrossRef]
- Fleiss, N.; Schwabenbauer, K.; Randis, T.M.; Polin, R.A. What’s new in the management of neonatal early-onset sepsis? Arch. Dis. Child. Fetal Neonatal Ed. 2023, 108, 10–14. [Google Scholar] [CrossRef]
- Celik, I.H.; Hanna, M.; Canpolat, F.E.; Pammi, M. Diagnosis of neonatal sepsis: The past, present and future. Pediatr. Res. 2022, 91, 337–350. [Google Scholar] [CrossRef]
- Schelonka, R.L.; Moser, S.A. Time to positive culture results in neonatal Candida septicemia. J. Pediatr. 2003, 142, 564–565. [Google Scholar] [CrossRef] [PubMed]
- Oeser, C.; Pond, M.; Butcher, P.; Bedford Russell, A.; Henneke, P.; Laing, K.; Planche, T.; Heath, P.T.; Harris, K. PCR for the detection of pathogens in neonatal early onset sepsis. PLoS ONE 2020, 15, e0226817. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, R.G.; Benjamin, D.K., Jr. Neonatal candidiasis: Diagnosis, prevention, and treatment. J. Infect. 2014, 69 (Suppl. S1), S19–S22. [Google Scholar] [CrossRef] [PubMed]
- Stein, A.; Soukup, D.; Rath, P.M.; Felderhoff-Müser, U. Diagnostic Accuracy of Multiplex Polymerase Chain Reaction in Early Onset Neonatal Sepsis. Children 2023, 10, 1809. [Google Scholar] [CrossRef]
- Aittakorpi, A.; Kuusela, P.; Koukila-Kähkölä, P.; Vaara, M.; Petrou, M.; Gant, V.; Mäki, M. Accurate and rapid identification of Candida spp. frequently associated with fungemia by using PCR and the microarray-based Prove-it Sepsis assay. J. Clin. Microbiol. 2012, 50, 3635–3640. [Google Scholar] [CrossRef]
- Innings, A.; Ullberg, M.; Johansson, A.; Rubin, C.J.; Noreus, N.; Isaksson, M.; Herrmann, B. Multiplex real-time PCR targeting the RNase P RNA gene for detection and identification of Candida species in blood. J. Clin. Microbiol. 2007, 45, 874–880. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kosmeri, C.; Giapros, V.; Serbis, A.; Baltogianni, M. Application of Advanced Molecular Methods to Study Early-Onset Neonatal Sepsis. Int. J. Mol. Sci. 2024, 25, 2258. [Google Scholar] [CrossRef]
- Shabaan, A.E.; Elbaz, L.M.; El-Emshaty, W.M.; Shouman, B. Role of serum (1,3)-β-d-glucan assay in early diagnosis of invasive fungal infections in a neonatal intensive care unit. J. Pediatr. 2018, 94, 559–565. [Google Scholar] [CrossRef]
- Warris, A.; Lehrnbecher, T. Progress in the Diagnosis of Invasive Fungal Disease in Children. Curr. Fungal Infect. Rep. 2017, 11, 35–44. [Google Scholar] [CrossRef]
- Manzoni, P.; Mostert, M.; Galletto, P.; Gastaldo, L.; Gallo, E.; Agriesti, G.; Farina, D. Is thrombocytopenia suggestive of organism-specific response in neonatal sepsis? Pediatr. Int. 2009, 51, 206–210. [Google Scholar] [CrossRef]
- Wolach, B.; Bogger-Goren, S.; Whyte, R. Perinatal hematological profile of newborn infants with candida antenatal infections. Biol. Neonate 1991, 59, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Tasneem, F.; Hossain, M.M.; Mahmud, S.; Ahmed, S.S. Clinical profile of fungal sepsis in new born: A tertiary centre experience from Bangladesh. J. Pediatr. Neonatal Care 2020, 10, 170–173. [Google Scholar] [CrossRef]
- Ratridewi, I.; Amalia, K.; Huwae, T.E.; Putera, M.A.; Sulistijono, E. Systemic Candidosis Diagnostic Test with Candida Score and Monocyte Count in Premature Infants with Late-Onset Sepsis: Research in Low Resources Country. Russ. J. Infect. Immun. 2023, 13, 133–140. [Google Scholar] [CrossRef]
- Noyola, D.E.; Fernandez, M.; Moylett, E.H.; Baker, C.J. Ophthalmologic, visceral, and cardiac involvement in neonates with candidemia. Clin. Infect. Dis. 2001, 32, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef]
- Ruhnke, M.; Rickerts, V.; Cornely, O.A.; Buchheidt, D.; Glöckner, A.; Heinz, W.; Höhl, R.; Horré, R.; Karthaus, M.; Kujath, P.; et al. Diagnosis and therapy of Candida infections: Joint recommendations of the German Speaking Mycological Society and the Paul-Ehrlich-Society for Chemotherapy. Mycoses 2011, 54, 279–310. [Google Scholar] [CrossRef]
- Hope, W.W.; Castagnola, E.; Groll, A.H.; Roilides, E.; Akova, M.; Arendrup, M.C.; Arikan-Akdagli, S.; Bassetti, M.; Bille, J.; Cornely, O.A.; et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: Prevention and management of invasive infections in neonates and children caused by Candida spp. Clin. Microbiol. Infect. 2012, 18 (Suppl. S7), 38–52. [Google Scholar] [CrossRef]
- Vasileiou, E.; Apsemidou, A.; Vyzantiadis, T.A.; Tragiannidis, A. Invasive candidiasis and candidemia in pediatric and neonatal patients: A review of current guidelines. Curr. Med. Mycol. 2018, 4, 28–33. [Google Scholar] [CrossRef]
- Robbins, N.; Caplan, T.; Cowen, L.E. Molecular Evolution of Antifungal Drug Resistance. Annu. Rev. Microbiol. 2017, 71, 753–775. [Google Scholar] [CrossRef]
- Gharaghani, M.; Taghipour, S.; Halvaeezadeh, M.; Mahmoudabadi, A.Z. Candiduria; a review article with specific data from Iran. Turk. J. Urol. 2018, 44, 445–452. [Google Scholar] [CrossRef]
- Wade, K.C.; Benjamin, D.K., Jr.; Kaufman, D.A.; Ward, R.M.; Smith, P.B.; Jayaraman, B.; Adamson, P.C.; Gastonguay, M.R.; Barrett, J.S. Fluconazole dosing for the prevention or treatment of invasive candidiasis in young infants. Pediatr. Infect. Dis. J. 2009, 28, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Shrivastava, M.; Whiteway, M.; Jiang, Y. Candida albicans targets that potentially synergize with fluconazole. Crit. Rev. Microbiol. 2021, 47, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Berman, J.; Krysan, D.J. Drug resistance and tolerance in fungi. Nat. Rev. Microbiol. 2020, 18, 319–331. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, A.; Ene, I.V.; Bibi, M.; Zakin, S.; Segal, E.S.; Ziv, N.; Dahan, A.M.; Colombo, A.L.; Bennett, R.J.; Berman, J. Antifungal tolerance is a subpopulation effect distinct from resistance and is associated with persistent candidemia. Nat. Commun. 2018, 9, 2470. [Google Scholar] [CrossRef]
- Benjamin, D.K., Jr.; Stoll, B.J.; Fanaroff, A.A.; McDonald, S.A.; Oh, W.; Higgins, R.D.; Duara, S.; Poole, K.; Laptook, A.; Goldberg, R.; et al. Neonatal candidiasis among extremely low birth weight infants: Risk factors, mortality rates, and neurodevelopmental outcomes at 18 to 22 months. Pediatrics 2006, 117, 84–92. [Google Scholar] [CrossRef]
- de Haan, T.R.; Beckers, L.; de Jonge, R.C.; Spanjaard, L.; van Toledo, L.; Pajkrt, D.; van Wassenaer-Leemhuis, A.G.; van der Lee, J.H. Neonatal gram negative and Candida sepsis survival and neurodevelopmental outcome at the corrected age of 24 months. PLoS ONE 2013, 8, e59214. [Google Scholar] [CrossRef]
- Mendling, W.S.H. Antimykotische Therapie der Vaginalen Hefepilz-Kolonisation von Schwangeren zur Verhutung von Kandidamykosen beim Neugeborenen. AMWF 2008, 15, S1. [Google Scholar]
- Mantadakis, E.; Pana, Z.D.; Zaoutis, T. Candidemia in children: Epidemiology, prevention and management. Mycoses 2018, 61, 614–622. [Google Scholar] [CrossRef]

| Patient 1 | Patient 2 | |
|---|---|---|
| Gestational age | 39 weeks | 28 weeks |
| Birth weight | 3600 g | 1250 g |
| Maternal history | Vaginal discharge and genital itching one week before delivery | 132 h of membrane rupture, intravenous ampicillin for 5 days, associated with ceftriaxone at birth |
| Maternal vaginal cultures | No pathogen growth at admission in our unit (2nd day after delivery) | No pathogen growth 5 days before delivery, C. albicans was isolated in cultures sampled at birth |
| Clinical onset | At birth, with characteristic rash | The 4th day, respiratory distress syndrome |
| Clinical course | No other signs or symptoms suggestive of sepsis, rash entirely resolved by DOL 13 | Re-initiated respiratory support (after initial treatment for respiratory distress syndrome due to surfactant deficiency with Bubble CPAP and surfactant), weaned on HHHFNC on DOL 15, oxygen-independent at DOL 41 |
| Complications | None | Hepatic and renal involvement |
| Discharge | DOL 24 | DOL 58 |
| Follow up | Normal growth and development at the age of 2 | Recently discharged, follow-up scheduled |
| Patient 1 | Patient 2 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 12 h | Day 1 | Day 3 | Day 12 | Day 17 | 12 h | Day 1 | Day 2 | 86 h | Day 5 | Day 10 | Day 15 | Day 20 | |
| Blood count and differential | |||||||||||||
| Platelets (103/µL) (range 150,000–400,000) ‡ | 434 | 412 | 389 | 354 | - | - | 374 | - | - | 331 | 356 | - | - |
| Leucocytes (/µL) (range 9000–26,000) ‡ | 17,440 | 14,430 | 11,280 | 9760 | - | - | 23,300 | - | - | 21,240 | 15,050 | - | - |
| Neutrophils (/µL) (range 2700–14,400) ‡ | 10,580 | 7540 | 6820 | 5730 | - | - | 15,090 | - | - | 14,350 | 9030 | - | - |
| Monocytes (%) (range 0–2%) ‡ | 1.4 | 12 | 12.5 | 4.1 | - | - | 8.4 | - | - | 9.5 | 5 | - | - |
| Inflammatory markers | |||||||||||||
| C-RP (mg/L) (normal value < 5 mg/L) | 19.38 | 8.3 | 7.4 | 1.6 | 3.1 | 2.1 | 1.3 | <1 | 41.4 | 36.6 | 14.3 | 12.5 | 2.9 |
| Biochemistry | |||||||||||||
| Blood glucose (mg/dL) (range 40–60 mg/dL 0–24 h, 40–100 mg/dL > 24 h of life) | 63.1 | 74 | 85 | - | - | 59 | 77 | 57 | 123 | 49 | 87 | 89 | 78 |
| AST (U/L) (range 11–70 U/L) | 38.4 | 34 | 29 | 27 | 15 | 29 | 29 | 114 | 107 | 87 | 20 | 27 | 28 |
| ALT (U/L) (range 0–70 U/L | 13.3 | 16 | 18 | 15 | 14 | <7 | <7 | 14 | 21 | 22 | 9 | 8 | 9 |
| Creatinine (mg/dL) (range 0.31–0.53 mg/mL) | 1.01 | 0.61 | 0.52 | 0.54 | 0.45 | 0.52 | 0.85 | 0.97 | 1.15 | 1.25 | 0.91 | 0.75 | 0.54 |
| BUN (mg/dL) (range 11–36 mg/mL) | 30.5 | 12 | 13 | 15 | 24 | 24 | 63 | 83 | 79 | 74 | 37 | 26 | 19 |
| Total bilirubin (mg/dL) § | 3.4 | 4.3 | 5.5 | 1.2 | 0.17 | 2.3 | 4.6 | 6.8 | 6.9 | 6.9 | 1.7 | - | - |
| Imaging | |||||||||||||
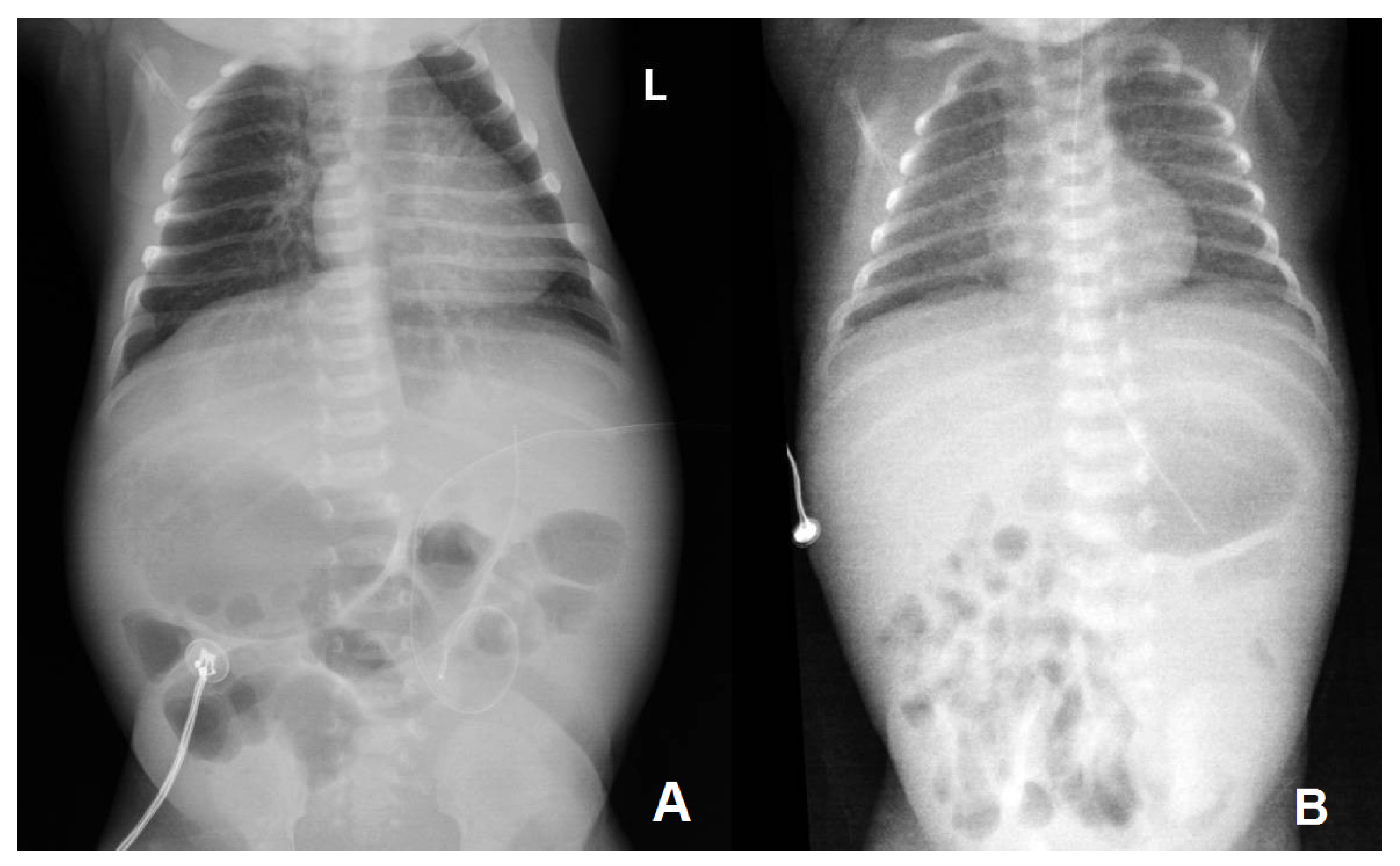
| Thoraco-abdominal radiography | No lung or abdominal involvement | Suggestive of respiratory distress syndrome due to surfactant deficiency on DOL 0; pronounced reticular, micronodular bilateral lung interstitium on DOL 5 | |||||||||||
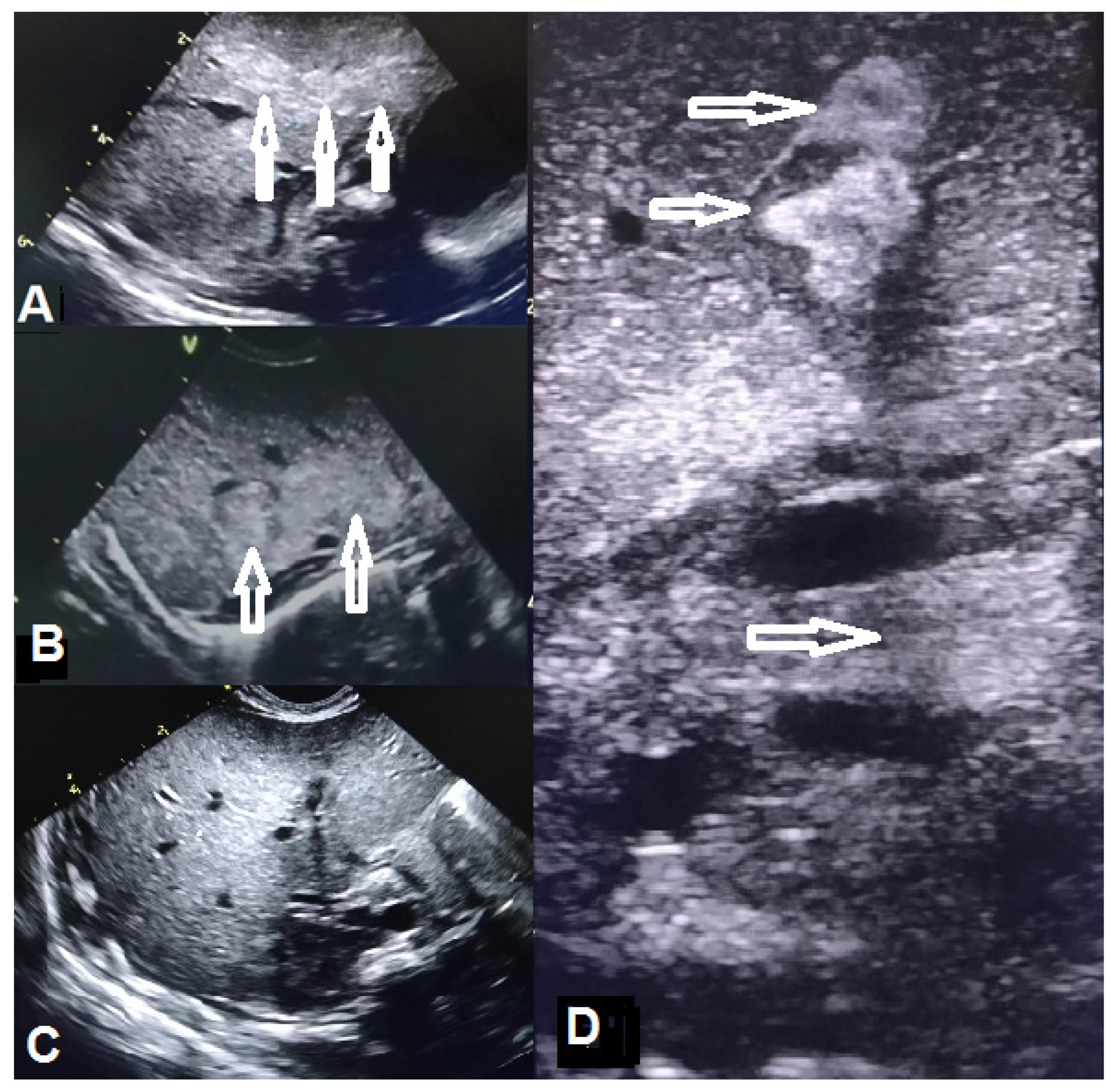
| Abdominal ultrasound | Abdominal situs inversus on DOL 2; no abdominal parenchymal involvement on DOL 2 and 10 | Gross, inhomogenous, patchy echogenic areas disseminated, almost throughout the entire liver on DOL 9; fine granular echogenic areas limited to the fourth hepatic segment by DOL6 14; normal hepatic ultrasound structure on DOL 45 | |||||||||||
| Doppler echocardiography | Small PDA, PFO, right-sided aortic arch (DOL 1) | Small PDA, PFO on DOL 4 and 14 | |||||||||||
| Microbiology | |||||||||||||
| Blood culture | Positive for C. albicans at admission, no growth at 14 days | Positive for C. albicans on DOL 0 and 11, negative on DOL 18 | |||||||||||
| Nasal swab culture | No pathogen identified | No pathogen identified on DOL 4 and 18 | |||||||||||
| Gastric aspirate | No pathogen identified | C. albicans isolated on DOL 0, and 4, no pathogen growth on DOL 18 | |||||||||||
| Pharyngeal culture | No pathogen identified | C. albicans isolated on DOL 4, no pathogen growth on DOL 18 | |||||||||||
| Umbilical line tip culture | C. albicans (in situ for 2 days) | C. albicans (in situ for 5 days) | |||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teacoe, D.A.; Cormoș, R.C.; Toma, D.A.; Ștef, L.; Cucerea, M.; Muțiu, I.; Chicea, R.; Popescu, D.; Chicea, E.D.; Boicean, A.G.; et al. Congenital Sepsis with Candida albicans—A Rare Event in the Neonatal Period: Report of Two Cases and Literature Review. Microorganisms 2024, 12, 1869. https://doi.org/10.3390/microorganisms12091869
Teacoe DA, Cormoș RC, Toma DA, Ștef L, Cucerea M, Muțiu I, Chicea R, Popescu D, Chicea ED, Boicean AG, et al. Congenital Sepsis with Candida albicans—A Rare Event in the Neonatal Period: Report of Two Cases and Literature Review. Microorganisms. 2024; 12(9):1869. https://doi.org/10.3390/microorganisms12091869
Chicago/Turabian StyleTeacoe, Dumitru Alin, Roxana Cristina Cormoș, Diana Adela Toma, Laura Ștef, Manuela Cucerea, Irina Muțiu, Radu Chicea, Dragoș Popescu, Eugen Dan Chicea, Adrian Gheorghe Boicean, and et al. 2024. "Congenital Sepsis with Candida albicans—A Rare Event in the Neonatal Period: Report of Two Cases and Literature Review" Microorganisms 12, no. 9: 1869. https://doi.org/10.3390/microorganisms12091869
APA StyleTeacoe, D. A., Cormoș, R. C., Toma, D. A., Ștef, L., Cucerea, M., Muțiu, I., Chicea, R., Popescu, D., Chicea, E. D., Boicean, A. G., Galiș, R., & Ognean, M. L. (2024). Congenital Sepsis with Candida albicans—A Rare Event in the Neonatal Period: Report of Two Cases and Literature Review. Microorganisms, 12(9), 1869. https://doi.org/10.3390/microorganisms12091869






