Mechanisms Affecting the Acquisition, Persistence and Transmission of Francisella tularensis in Ticks
Abstract
:1. Introduction
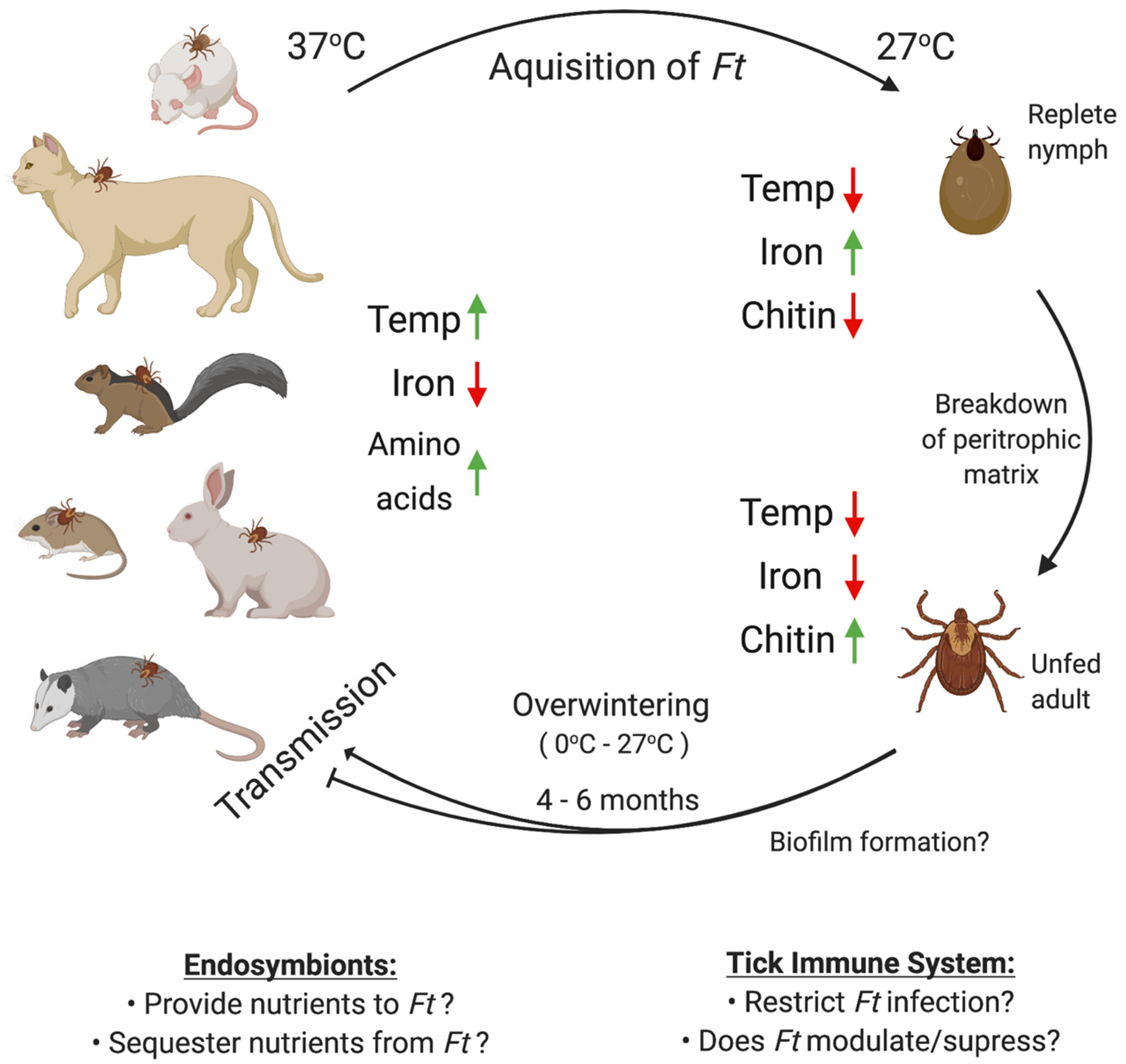
2. Epidemiology of F. tularensis Transmission by Ticks in the U.S.
3. Factors that Affect F. tularensis Infections of Ticks
4. F. tularensis Persistence and Transmission in Ticks
5. F. tularensis Biofilms
6. F. tularensis Chitin Utilization
7. Tick Endosymbionts
8. The Tick Immune System and Antimicrobial Activities
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rosenberg, R.; Lindsey, N.P.; Fischer, M.; Gregory, C.J.; Hinckley, A.F.; Mead, P.S.; Paz-Bailey, G.; Waterman, S.H.; Drexler, N.A.; Kersh, G.J.; et al. Vital Signs: Trends in Reported Vectorborne Disease Cases United States and Territories, 2004–2016. Mmwr Morb. Mortal. Wkly. Rep. 2018, 67, 496–501. [Google Scholar] [CrossRef] [Green Version]
- Ostfeld, R.S.; Canham, C.D.; Oggenfuss, K.; Winchcombe, R.J.; Keesing, F. Climate, deer, rodents, and acorns as determinants of variation in lyme-disease risk. PLoS Biol. 2006, 4, e145. [Google Scholar] [CrossRef]
- Molaei, G.; Little, E.A.H.; Williams, S.C.; Stafford, K.C. Bracing for the Worst-Range Expansion of the Lone Star Tick in the Northeastern United States. N. Engl. J. Med. 2019, 381, 2189–2192. [Google Scholar] [CrossRef] [PubMed]
- Sonenshine, D.E. Range Expansion of Tick Disease Vectors in North America: Implications for Spread of Tick-Borne Disease. Int. J. Environ. Res. Public Health 2018, 15, 478. [Google Scholar] [CrossRef] [Green Version]
- Reif, K.E.; Ujczo, J.K.; Alperin, D.C.; Noh, S.M. Francisella tularensis novicida infection competence differs in cell lines derived from United States populations of Dermacentor andersoni and Ixodes scapularis. Sci. Rep. 2018, 8, 12685. [Google Scholar] [CrossRef] [PubMed]
- Molins, C.R.; Delorey, M.J.; Yockey, B.M.; Young, J.W.; Sheldon, S.W.; Reese, S.M.; Schriefer, M.E.; Petersen, J.M. Virulence differences among Francisella tularensis subsp. tularensis clades in mice. PLoS ONE 2010, 5, e10205. [Google Scholar] [CrossRef]
- Ellis, J.; Oyston, P.C.; Green, M.; Titball, R.W. Tularemia. Clin. Microbiol. Rev. 2002, 15, 631–646. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oyston, P.C.; Quarry, J.E. Tularemia vaccine: Past, present and future. Antonie Van Leeuwenhoek 2005, 87, 277–281. [Google Scholar] [PubMed]
- Eigelsbach, H.T.; Downs, C.M. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J. Immunol. 1961, 87, 415–425. [Google Scholar]
- Kingry, L.C.; Petersen, J.M. Comparative review of Francisella tularensis and Francisella novicida. Front. Cell. Infect. Microbiol. 2014, 4, 35. [Google Scholar] [CrossRef] [PubMed]
- Dennis, D.T.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Friedlander, A.M.; Hauer, J.; Layton, M.; et al. Tularemia as a biological weapon: Medical and public health management. JAMA 2001, 285, 2763–2773. [Google Scholar] [CrossRef] [PubMed]
- Zellner, B.; Huntley, J.F. Ticks and Tularemia: Do We Know What We Don’t Know? Front. Cell. Infect. Microbiol. 2019, 9, 146. [Google Scholar] [CrossRef] [PubMed]
- Larssen, K.W.; Bergh, K.; Heier, B.T.; Vold, L.; Afset, J.E. All-time high tularaemia incidence in Norway in 2011: Report from the national surveillance. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 1919–1926. [Google Scholar] [CrossRef]
- Hennebique, A.; Boisset, S.; Maurin, M. Tularemia as a waterborne disease: A review. Emerg. Microbes Infect. 2019, 8, 1027–1042. [Google Scholar] [CrossRef] [PubMed]
- Dryselius, R.; Hjertqvist, M.; Makitalo, S.; Lindblom, A.; Lilja, T.; Eklof, D.; Lindstrom, A. Large outbreak of tularaemia, central Sweden, July to September 2019. Eurosurveillance 2019, 24. [Google Scholar] [CrossRef]
- Ryden, P.; Bjork, R.; Schafer, M.L.; Lundstrom, J.O.; Petersen, B.; Lindblom, A.; Forsman, M.; Sjostedt, A.; Johansson, A. Outbreaks of tularemia in a boreal forest region depends on mosquito prevalence. J. Infect. Dis. 2012, 205, 297–304. [Google Scholar] [CrossRef] [Green Version]
- Eliasson, H.; Broman, T.; Forsman, M.; Back, E. Tularemia: Current epidemiology and disease management. Infect. Dis. Clin. N. Am. 2006, 20, 289–311. [Google Scholar] [CrossRef]
- Ma, Y.; Bring, A.; Kalantari, Z.; Destouni, G. Potential for Hydroclimatically Driven Shifts in Infectious Disease Outbreaks: The Case of Tularemia in High-Latitude Regions. Int. J. Environ. Res. Public Health 2019, 16, 3717. [Google Scholar] [CrossRef] [Green Version]
- Lopes de Carvalho, I.; Toledo, A.; Carvalho, C.L.; Barandika, J.F.; Respicio-Kingry, L.B.; Garcia-Amil, C.; Garcia-Perez, A.L.; Olmeda, A.S.; Ze-Ze, L.; Petersen, J.M.; et al. Francisella species in ticks and animals, Iberian Peninsula. Ticks Tick Borne Dis. 2016, 7, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Appelt, S.; Koppen, K.; Radonic, A.; Drechsel, O.; Jacob, D.; Grunow, R.; Heuner, K. Genetic Diversity and Spatial Segregation of Francisella tularensis Subspecies holarctica in Germany. Front. Cell. Infect. Microbiol. 2019, 9, 376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haulrig, M.B.; Mathiasen, G.; Nielsen, R.M.; Kromann, C.B.; Krogfelt, K.A.; Wiese, L. Two cases of tick-borne transmitted tularemia on Southern Zealand, Denmark. APMIS 2020, 128, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Wojcik-Fatla, A.; Zajac, V.; Sawczyn, A.; Cisak, E.; Sroka, J.; Dutkiewicz, J. Occurrence of Francisella spp. in Dermacentor reticulatus and Ixodes ricinus ticks collected in eastern Poland. Ticks Tick Borne Dis. 2015, 6, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Bielawska-Drozd, A.; Cieslik, P.; Zakowska, D.; Glowacka, P.; Wlizlo-Skowronek, B.; Zieba, P.; Zdun, A. Detection of Coxiella burnetii and Francisella tularensis in Tissues of Wild-living Animals and in Ticks of North-west Poland. Pol. J. Microbiol. 2018, 67, 529–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forminska, K.; Wolkowicz, T.; Brodzik, K.; Stefanoff, P.; Golab, E.; Masny, A.; Osiak, B.; Cieslik, P.; Bielawska-Drozd, A.; Zasada, A.A. Genetic diversity of Francisella tularensis in Poland with comments on MLVA genotyping and a proposition of a novel rapid v4-genotyping. Ticks Tick Borne Dis. 2020, 11, 101322. [Google Scholar] [CrossRef]
- Michelet, L.; Joncour, G.; Devillers, E.; Torina, A.; Vayssier-Taussat, M.; Bonnet, S.I.; Moutailler, S. Tick species, tick-borne pathogens and symbionts in an insular environment off the coast of Western France. Ticks Tick Borne Dis. 2016, 7, 1109–1115. [Google Scholar] [CrossRef] [PubMed]
- Janse, I.; Maas, M.; Rijks, J.M.; Koene, M.; van der Plaats, R.Q.; Engelsma, M.; van der Tas, P.; Braks, M.; Stroo, A.; Notermans, D.W.; et al. Environmental surveillance during an outbreak of tularaemia in hares, the Netherlands, 2015. Eurosurveillance 2017, 22, 30607. [Google Scholar] [CrossRef] [Green Version]
- Parker, R.R.; Spencer, R.R.; Francis, E. Tularæmia: XI. Tularæmia Infection in Ticks of the Species Dermacentor Andersoni Stiles in the Bitterroot Valley, Mont. Public Health Rep. (1896–1970) 1924, 39, 1057–1073. [Google Scholar] [CrossRef]
- Eisen, L. A call for renewed research on tick-borne Francisella tularensis in the Arkansas-Missouri primary national focus of tularemia in humans. J. Med. Entomol. 2007, 44, 389–397. [Google Scholar] [CrossRef]
- Nagamori, Y.; Payton, M.; Coburn, L.; Thomas, J.E.; Reichard, M. Nymphal engorgement weight predicts sex of adult Amblyomma americanum, Amblyomma maculatum, Dermacentor andersoni, Dermacentor variabilis, and Rhipicephalus sanguineus ticks. Exp. Appl. Acarol. 2019, 77, 401–410. [Google Scholar] [CrossRef]
- Oliver, J.D.; Dusty Loy, J.; Parikh, G.; Bartholomay, L. Comparative analysis of hemocyte phagocytosis between six species of arthropods as measured by flow cytometry. J. Invertebr. Pathol. 2011, 108, 126–130. [Google Scholar] [CrossRef]
- Duron, O.; Binetruy, F.; Noel, V.; Cremaschi, J.; McCoy, K.D.; Arnathau, C.; Plantard, O.; Goolsby, J.; Perez de Leon, A.A.; Heylen, D.J.A.; et al. Evolutionary changes in symbiont community structure in ticks. Mol. Ecol. 2017, 26, 2905–2921. [Google Scholar] [CrossRef] [Green Version]
- Hopla, C.E. Experimental studies on tick transmission of tularemia organisms. Am. J. Hyg. 1953, 58, 101–118. [Google Scholar] [CrossRef] [PubMed]
- Mani, R.J.; Metcalf, J.A.; Clinkenbeard, K.D. Amblyomma americanum as a Bridging Vector for Human Infection with Francisella tularensis. PLoS ONE 2015, 10, e0130513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coburn, J.; Maier, T.; Casey, M.; Padmore, L.; Sato, H.; Frank, D.W. Reproducible and quantitative model of infection of Dermacentor variabilis with the live vaccine strain of Francisella tularensis. Appl. Environ. Microbiol. 2015, 81, 386–395. [Google Scholar] [CrossRef] [Green Version]
- Brown, V.R.; Adney, D.R.; Bielefeldt-Ohmann, H.; Gordy, P.W.; Felix, T.A.; Olea-Popelka, F.J.; Bowen, R.A. Pathogenesis and Immune Responses of Francisella Tularensis Strains in Wild-Caught Cottontail Rabbits (Sylvilagus Spp.). J. Wildl. Dis. 2015, 51, 564–575. [Google Scholar] [CrossRef]
- Parker, R.R.; Brooks, C.S.; Marsh, H. The Occurrence of Bacterium tularense in the Wood Tick, Dermacentor occidentalis, in California. Public Health Rep. (1896–1970) 1929, 44, 328–335. [Google Scholar] [CrossRef]
- Reese, S.M.; Petersen, J.M.; Sheldon, S.W.; Dolan, M.C.; Dietrich, G.; Piesman, J.; Eisen, R.J. Transmission efficiency of Francisella tularensis by adult american dog ticks (Acari: Ixodidae). J. Med. Entomol. 2011, 48, 884–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reif, K.E.; Palmer, G.H.; Ueti, M.W.; Scoles, G.A.; Margolis, J.J.; Monack, D.M.; Noh, S.M. Dermacentor andersoni transmission of Francisella tularensis subsp. novicida reflects bacterial colonization, dissemination, and replication coordinated with tick feeding. Infect. Immun. 2011, 79, 4941–4946. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kugeler, K.J.; Mead, P.S.; Janusz, A.M.; Staples, J.E.; Kubota, K.A.; Chalcraft, L.G.; Petersen, J.M. Molecular Epidemiology of Francisella tularensis in the United States. Clin. Infect. Dis. 2009, 48, 863–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goethert, H.K.; Shani, I.; Telford, S.R., III. Genotypic diversity of Francisella tularensis infecting Dermacentor variabilis ticks on Martha’s Vineyard, Massachusetts. J. Clin. Microbiol. 2004, 42, 4968–4973. [Google Scholar] [CrossRef] [Green Version]
- Goethert, H.K.; Telford, S.R., III. A new Francisella (Beggiatiales: Francisellaceae) inquiline within Dermacentor variabilis say (Acari: Ixodidae). J. Med. Entomol. 2005, 42, 502–505. [Google Scholar] [CrossRef] [Green Version]
- Goethert, H.K.; Telford, S.R., III. Nonrandom distribution of vector ticks (Dermacentor variabilis) infected by Francisella tularensis. PloS Pathog. 2009, 5, e1000319. [Google Scholar] [CrossRef]
- Goethert, H.K.; Telford, S.R., III. Quantum of infection of Francisella tularensis tularensis in host-seeking Dermacentor variabilis. Ticks Tick Borne Dis. 2010, 1, 66–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montales, M.T.; Beebe, A.; Chaudhury, A.; Haselow, D.; Patil, S.; Weinstein, S.; Taffner, R.; Patil, N. A Clinical Review of Tick-Borne Diseases in Arkansas. J. Ark. Med. Soc. 2016, 112, 254–258. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention: Tularemia: Statistics. Available online: https://www.cdc.gov/tularemia/statistics/index.html (accessed on 23 September 2020).
- James, A.M.; Burdett, C.; McCool, M.J.; Fox, A.; Riggs, P. The geographic distribution and ecological preferences of the American dog tick, Dermacentor variabilis (Say), in the U.S.A. Med. Vet. Entomol. 2015, 29, 178–188. [Google Scholar] [CrossRef]
- Monzon, J.D.; Atkinson, E.G.; Henn, B.M.; Benach, J.L. Population and Evolutionary Genomics of Amblyomma americanum, an Expanding Arthropod Disease Vector. Genome Biol. Evol. 2016, 8, 1351–1360. [Google Scholar] [CrossRef] [Green Version]
- Kollars, T.M., Jr.; Oliver, J.H., Jr.; Durden, L.A.; Kollars, P.G. Host association and seasonal activity of Amblyomma americanum (Acari: Ixodidae) in Missouri. J. Parasitol. 2000, 86, 1156–1159. [Google Scholar] [CrossRef]
- Calhoun, E.L. Natural occurrence of tularemia in the lone star tick, Amblyomma americanus (Linn.), and in dogs in Arkansas. Am. J. Trop. Med. Hyg. 1954, 3, 360–366. [Google Scholar] [CrossRef]
- Whitten, T.; Demontigny, C.; Bjork, J.; Foss, M.; Peterson, M.; Scheftel, J.; Neitzel, D.; Sullivan, M.; Smith, K. Prevalence of Francisella tularensis in Dermacentor variabilis Ticks, Minnesota, 2017. Vector Borne Zoonotic Dis. 2019, 19, 596–603. [Google Scholar] [CrossRef]
- Dykstra, E.A.; Oltean, H.N.; Kangiser, D.; Marsden-Haug, N.; Rich, S.M.; Xu, G.; Lee, M.K.; Morshed, M.G.; Graham, C.B.; Eisen, R.J. Ecology and Epidemiology of Tickborne Pathogens, Washington, USA, 2011–2016. Emerg. Infect. Dis. 2020, 26, 648–657. [Google Scholar] [CrossRef] [Green Version]
- McCoy, G. A plague-like disease of rodents. Public Health Bull. 1911, 19, 61–72. [Google Scholar]
- Jellison, W.L. Tularemia; geographical distribution of deerfly fever and the biting fly, Chrysops discalis Williston. Public Health Rep. 1950, 65, 1321–1329. [Google Scholar] [CrossRef]
- Vonkavaara, M.; Telepnev, M.V.; Ryden, P.; Sjostedt, A.; Stoven, S. Drosophila melanogaster as a model for elucidating the pathogenicity of Francisella tularensis. Cell. Microbiol. 2008, 10, 1327–1338. [Google Scholar] [CrossRef]
- Murfin, K.E.; Kleinbard, R.; Aydin, M.; Salazar, S.A.; Fikrig, E. Borrelia burgdorferi chemotaxis toward tick protein Salp12 contributes to acquisition. Ticks Tick Borne Dis. 2019, 10, 1124–1134. [Google Scholar] [CrossRef]
- Galletti, M.F.; Fujita, A.; Rosa, R.D.; Martins, L.A.; Soares, H.S.; Labruna, M.B.; Daffre, S.; Fogaca, A.C. Virulence genes of Rickettsia rickettsii are differentially modulated by either temperature upshift or blood-feeding in tick midgut and salivary glands. Parasites Vectors 2016, 9, 331. [Google Scholar] [CrossRef] [Green Version]
- Keim, P.; Johansson, A.; Wagner, D.M. Molecular epidemiology, evolution, and ecology of Francisella. Ann. N. Y. Acad. Sci. 2007, 1105, 30–66. [Google Scholar] [CrossRef]
- Brooks, C.S.; Hefty, P.S.; Jolliff, S.E.; Akins, D.R. Global analysis of Borrelia burgdorferi genes regulated by mammalian host-specific signals. Infect. Immun. 2003, 71, 3371–3383. [Google Scholar] [CrossRef] [Green Version]
- Carroll, J.A.; Cordova, R.M.; Garon, C.F. Identification of 11 pH-regulated genes in Borrelia burgdorferi localizing to linear plasmids. Infect. Immun. 2000, 68, 6677–6684. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.F.; Pal, U.; Alani, S.M.; Fikrig, E.; Norgard, M.V. Essential role for OspA/B in the life cycle of the Lyme disease spirochete. J. Exp. Med. 2004, 199, 641–648. [Google Scholar] [CrossRef] [Green Version]
- Pal, U.; Li, X.; Wang, T.; Montgomery, R.R.; Ramamoorthi, N.; Desilva, A.M.; Bao, F.; Yang, X.; Pypaert, M.; Pradhan, D.; et al. TROSPA, an Ixodes scapularis receptor for Borrelia burgdorferi. Cell 2004, 119, 457–468. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Goldberg, M.S.; Popova, T.G.; Schoeler, G.B.; Wikel, S.K.; Hagman, K.E.; Norgard, M.V. Interdependence of environmental factors influencing reciprocal patterns of gene expression in virulent Borrelia burgdorferi. Mol. Microbiol. 2000, 37, 1470–1479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celli, J.; Zahrt, T.C. Mechanisms of Francisella tularensis intracellular pathogenesis. Cold Spring Harb. Perspect. Med. 2013, 3, a010314. [Google Scholar] [CrossRef] [PubMed]
- Steiner, D.J.; Furuya, Y.; Jordan, M.B.; Metzger, D.W. Protective Role for Macrophages in Respiratory Francisella tularensis Infection. Infect. Immun. 2017, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canton, J.; Khezri, R.; Glogauer, M.; Grinstein, S. Contrasting phagosome pH regulation and maturation in human M1 and M2 macrophages. Mol. Biol. Cell. 2014, 25, 3330–3341. [Google Scholar] [CrossRef]
- KuoLee, R.; Zhao, X.; Austin, J.; Harris, G.; Conlan, J.W.; Chen, W. Mouse model of oral infection with virulent type A Francisella tularensis. Infect. Immun. 2007, 75, 1651–1660. [Google Scholar] [CrossRef] [Green Version]
- Fuller, J.R.; Kijek, T.M.; Taft-Benz, S.; Kawula, T.H. Environmental and intracellular regulation of Francisella tularensis ripA. BMC Microbiol. 2009, 9, 216. [Google Scholar] [CrossRef] [Green Version]
- Chong, A.; Wehrly, T.D.; Nair, V.; Fischer, E.R.; Barker, J.R.; Klose, K.E.; Celli, J. The early phagosomal stage of Francisella tularensis determines optimal phagosomal escape and Francisella pathogenicity island protein expression. Infect. Immun. 2008, 76, 5488–5499. [Google Scholar] [CrossRef] [Green Version]
- Pan, X.; Tamilselvam, B.; Hansen, E.J.; Daefler, S. Modulation of iron homeostasis in macrophages by bacterial intracellular pathogens. BMC Microbiol. 2010, 10, 64. [Google Scholar] [CrossRef] [Green Version]
- Ouyang, Z.; Deka, R.K.; Norgard, M.V. BosR (BB0647) controls the RpoN-RpoS regulatory pathway and virulence expression in Borrelia burgdorferi by a novel DNA-binding mechanism. Plos Pathog. 2011, 7, e1001272. [Google Scholar] [CrossRef] [Green Version]
- Deng, K.; Blick, R.J.; Liu, W.; Hansen, E.J. Identification of Francisella tularensis genes affected by iron limitation. Infect. Immun. 2006, 74, 4224–4236. [Google Scholar] [CrossRef] [Green Version]
- Horzempa, J.; Carlson, P.E., Jr.; O’Dee, D.M.; Shanks, R.M.; Nau, G.J. Global transcriptional response to mammalian temperature provides new insight into Francisella tularensis pathogenesis. BMC Microbiol. 2008, 8, 172. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Powell, D.A.; Shaffer, S.A.; Rasko, D.A.; Pelletier, M.R.; Leszyk, J.D.; Scott, A.J.; Masoudi, A.; Goodlett, D.R.; Wang, X.; et al. LPS remodeling is an evolved survival strategy for bacteria. Proc. Natl. Acad. Sci. USA 2012, 109, 8716–8721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connat, J.L. Demonstration of regurgitation of gut content during blood meals of the tick Ornithodoros moubata. Possible role in the transmission of pathogenic agents. Parasitol. Res. 1991, 77, 452–454. [Google Scholar] [CrossRef]
- Sojka, D.; Franta, Z.; Horn, M.; Caffrey, C.R.; Mares, M.; Kopacek, P. New insights into the machinery of blood digestion by ticks. Trends Parasitol. 2013, 29, 276–285. [Google Scholar] [CrossRef]
- Meibom, K.L.; Charbit, A. Francisella tularensis metabolism and its relation to virulence. Front. Microbiol. 2010, 1, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papanikolaou, G.; Pantopoulos, K. Iron metabolism and toxicity. Toxicol. Appl. Pharmacol. 2005, 202, 199–211. [Google Scholar] [CrossRef]
- Mohapatra, N.P.; Soni, S.; Rajaram, M.V.; Strandberg, K.L.; Gunn, J.S. Type A Francisella tularensis acid phosphatases contribute to pathogenesis. PLoS ONE 2013, 8, e56834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ren, G.; Champion, M.M.; Huntley, J.F. Identification of disulfide bond isomerase substrates reveals bacterial virulence factors. Mol. Microbiol. 2014, 94, 926–944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Bian, G.; Pan, W.; Feng, T.; Dai, J. Molecular characterization of a defensin gene from a hard tick, Dermacentor silvarum. Parasites Vectors 2015, 8, 25. [Google Scholar] [CrossRef] [Green Version]
- Martins, L.A.; Malossi, C.D.; Galletti, M.; Ribeiro, J.M.; Fujita, A.; Esteves, E.; Costa, F.B.; Labruna, M.B.; Daffre, S.; Fogaca, A.C. The Transcriptome of the Salivary Glands of Amblyomma aureolatum Reveals the Antimicrobial Peptide Microplusin as an Important Factor for the Tick Protection Against Rickettsia rickettsii Infection. Front. Physiol. 2019, 10, 529. [Google Scholar] [CrossRef]
- Galay, R.L.; Umemiya-Shirafuji, R.; Mochizuki, M.; Fujisaki, K.; Tanaka, T. Iron metabolism in hard ticks (Acari: Ixodidae): The antidote to their toxic diet. Parasitol. Int. 2015, 64, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Zolnik, C.P.; Falco, R.C.; Daniels, T.J.; Kolokotronis, S.O. Transient influence of blood meal and natural environment on blacklegged tick bacterial communities. Ticks Tick Borne Dis. 2018, 9, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Mani, R.J.; Reichard, M.V.; Morton, R.J.; Kocan, K.M.; Clinkenbeard, K.D. Biology of Francisella tularensis subspecies holarctica live vaccine strain in the tick vector Dermacentor Variabilis. PloS ONE 2012, 7, e35441. [Google Scholar] [CrossRef] [PubMed]
- Alhede, M.; Bjarnsholt, T.; Givskov, M.; Alhede, M. Pseudomonas aeruginosa biofilms: Mechanisms of immune evasion. Adv. Appl. Microbiol. 2014, 86, 1–40. [Google Scholar] [CrossRef]
- Guilhen, C.; Miquel, S.; Charbonnel, N.; Joseph, L.; Carrier, G.; Forestier, C.; Balestrino, D. Colonization and immune modulation properties of Klebsiella pneumoniae biofilm-dispersed cells. Npj Biofilms Microbiomes 2019, 5, 25. [Google Scholar] [CrossRef]
- Abdel-Nour, M.; Duncan, C.; Low, D.E.; Guyard, C. Biofilms: The stronghold of Legionella pneumophila. Int. J. Mol. Sci. 2013, 14, 21660–21675. [Google Scholar] [CrossRef] [Green Version]
- Lutz, C.; Erken, M.; Noorian, P.; Sun, S.; McDougald, D. Environmental reservoirs and mechanisms of persistence of Vibrio cholerae. Front. Microbiol. 2013, 4, 375. [Google Scholar] [CrossRef] [Green Version]
- Jarrett, C.O.; Deak, E.; Isherwood, K.E.; Oyston, P.C.; Fischer, E.R.; Whitney, A.R.; Kobayashi, S.D.; DeLeo, F.R.; Hinnebusch, B.J. Transmission of Yersinia pestis from an infectious biofilm in the flea vector. J. Infect. Dis. 2004, 190, 783–792. [Google Scholar] [CrossRef] [Green Version]
- Telford, S.R., III; Goethert, H.K. Toward an understanding of the perpetuation of the agent of tularemia. Front. Microbiol. 2010, 1, 150. [Google Scholar] [CrossRef] [Green Version]
- Dergousoff, S.J.; Anstead, C.A.; Chilton, N.B. Identification of bacteria in the Rocky Mountain wood tick, Dermacentor andersoni, using single-strand conformation polymorphism (SSCP) and DNA sequencing. Exp. Appl. Acarol. 2020, 80, 247–256. [Google Scholar] [CrossRef]
- Merzendorfer, H.; Zimoch, L. Chitin metabolism in insects: Structure, function and regulation of chitin synthases and chitinases. J. Exp. Biol. 2003, 206, 4393–4412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Margolis, J.J.; El-Etr, S.; Joubert, L.M.; Moore, E.; Robison, R.; Rasley, A.; Spormann, A.M.; Monack, D.M. Contributions of Francisella tularensis subsp. novicida chitinases and Sec secretion system to biofilm formation on chitin. Appl. Environ. Microbiol. 2010, 76, 596–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durham-Colleran, M.W.; Verhoeven, A.B.; van Hoek, M.L. Francisella novicida forms in vitro biofilms mediated by an orphan response regulator. Microb. Ecol. 2010, 59, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Zogaj, X.; Wyatt, G.C.; Klose, K.E. Cyclic di-GMP stimulates biofilm formation and inhibits virulence of Francisella novicida. Infect. Immun. 2012, 80, 4239–4247. [Google Scholar] [CrossRef] [Green Version]
- Champion, A.E.; Catanzaro, K.C.F.; Bandara, A.B.; Inzana, T.J. Formation of the Francisella tularensis Biofilm is Affected by Cell Surface Glycosylation, Growth Medium, and a Glucan Exopolysaccharide. Sci. Rep. 2019, 9, 12252. [Google Scholar] [CrossRef]
- Chung, M.C.; Dean, S.; Marakasova, E.S.; Nwabueze, A.O.; van Hoek, M.L. Chitinases are negative regulators of Francisella novicida biofilms. PLoS ONE 2014, 9, e93119. [Google Scholar] [CrossRef] [Green Version]
- Tilly, K.; Elias, A.F.; Errett, J.; Fischer, E.; Iyer, R.; Schwartz, I.; Bono, J.L.; Rosa, P. Genetics and regulation of chitobiose utilization in Borrelia burgdorferi. J. Bacteriol. 2001, 183, 5544–5553. [Google Scholar] [CrossRef] [Green Version]
- Gall, C.A.; Reif, K.E.; Scoles, G.A.; Mason, K.L.; Mousel, M.; Noh, S.M.; Brayton, K.A. The bacterial microbiome of Dermacentor andersoni ticks influences pathogen susceptibility. ISME J. 2016, 10, 1846–1855. [Google Scholar] [CrossRef] [Green Version]
- Gerhart, J.G.; Moses, A.S.; Raghavan, R. A Francisella-like endosymbiont in the Gulf Coast tick evolved from a mammalian pathogen. Sci. Rep. 2016, 6, 33670. [Google Scholar] [CrossRef]
- Brinkerhoff, R.J.; Clark, C.; Ocasio, K.; Gauthier, D.T.; Hynes, W.L. Factors affecting the microbiome of Ixodes scapularis and Amblyomma americanum. PLoS ONE 2020, 15, e0232398. [Google Scholar] [CrossRef]
- Trout Fryxell, R.T.; DeBruyn, J.M. The Microbiome of Ehrlichia-Infected and Uninfected Lone Star Ticks (Amblyomma americanum). PLoS ONE 2016, 11, e0146651. [Google Scholar] [CrossRef] [Green Version]
- Lado, P.; Luan, B.; Allerdice, M.E.J.; Paddock, C.D.; Karpathy, S.E.; Klompen, H. Integrating population genetic structure, microbiome, and pathogens presence data in Dermacentor variabilis. PeerJ 2020, 8, e9367. [Google Scholar] [CrossRef] [PubMed]
- Clay, K.; Klyachko, O.; Grindle, N.; Civitello, D.; Oleske, D.; Fuqua, C. Microbial communities and interactions in the lone star tick, Amblyomma americanum. Mol. Ecol. 2008, 17, 4371–4381. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Mao, L.; Sun, Y.; Wang, Z.; Zhang, J.; Zhang, J.; Peng, Y.; Xia, L. A Novel Francisella-Like Endosymbiont in Haemaphysalis longicornis and Hyalomma asiaticum, China. Vector Borne Zoonotic Dis. 2018, 18, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Pavanelo, D.B.; Schroder, N.C.H.; Pin Viso, N.D.; Martins, L.A.; Malossi, C.D.; Galletti, M.; Labruna, M.B.; Daffre, S.; Farber, M.; Fogaca, A.C. Comparative analysis of the midgut microbiota of two natural tick vectors of Rickettsia rickettsii. Dev. Comp. Immunol. 2020, 106, 103606. [Google Scholar] [CrossRef] [PubMed]
- Rynkiewicz, E.C.; Hemmerich, C.; Rusch, D.B.; Fuqua, C.; Clay, K. Concordance of bacterial communities of two tick species and blood of their shared rodent host. Mol. Ecol. 2015, 24, 2566–2579. [Google Scholar] [CrossRef]
- Clow, K.M.; Weese, J.S.; Rousseau, J.; Jardine, C.M. Microbiota of field-collected Ixodes scapularis and Dermacentor variabilis from eastern and southern Ontario, Canada. Ticks Tick Borne Dis. 2018, 9, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, E.L.; Stone, N.E.; Scoles, G.A.; Hepp, C.M.; Busch, J.D.; Wagner, D.M. Range-wide genetic analysis of Dermacentor variabilis and its Francisella-like endosymbionts demonstrates phylogeographic concordance between both taxa. Parasit. Vectors 2018, 11, 306. [Google Scholar] [CrossRef] [Green Version]
- Macaluso, K.R.; Sonenshine, D.E.; Ceraul, S.M.; Azad, A.F. Rickettsial infection in Dermacentor variabilis (Acari: Ixodidae) inhibits transovarial transmission of a second Rickettsia. J. Med. Entomol. 2002, 39, 809–813. [Google Scholar] [CrossRef] [Green Version]
- Mohanty, I.; Rath, A.; Swain, S.P.; Pradhan, N.; Hazra, R.K. Wolbachia Population in Vectors and Non-vectors: A Sustainable Approach Towards Dengue Control. Curr. Microbiol. 2019, 76, 133–143. [Google Scholar] [CrossRef]
- Rivas, J.J.; Moreira-Soto, A.; Alvarado, G.; Taylor, L.; Calderon-Arguedas, O.; Hun, L.; Corrales-Aguilar, E.; Morales, J.A.; Troyo, A. Pathogenic potential of a Costa Rican strain of ‘Candidatus Rickettsia amblyommii’ in guinea pigs (Cavia porcellus) and protective immunity against Rickettsia rickettsii. Ticks Tick Borne Dis. 2015, 6, 805–811. [Google Scholar] [CrossRef] [PubMed]
- Billeter, S.A.; Blanton, H.L.; Little, S.E.; Levy, M.G.; Breitschwerdt, E.B. Detection of Rickettsia amblyommii in association with a tick bite rash. Vector Borne Zoonotic Dis. 2007, 7, 607–610. [Google Scholar] [CrossRef] [PubMed]
- Hajdusek, O.; Sima, R.; Ayllon, N.; Jalovecka, M.; Perner, J.; de la Fuente, J.; Kopacek, P. Interaction of the tick immune system with transmitted pathogens. Front. Cell. Infect. Microbiol. 2013, 3, 26. [Google Scholar] [CrossRef] [Green Version]
- Hernandez, E.P.; Talactac, M.R.; Fujisaki, K.; Tanaka, T. The case for oxidative stress molecule involvement in the tick-pathogen interactions-an omics approach. Dev. Comp. Immunol. 2019, 100, 103409. [Google Scholar] [CrossRef] [PubMed]
- Sonenshine, D.E.; Hynes, W.L. Molecular characterization and related aspects of the innate immune response in ticks. Front. Biosci. 2008, 13, 7046–7063. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johns, R.; Sonenshine, D.E.; Hynes, W.L. Control of bacterial infections in the hard tick Dermacentor variabilis (Acari: Ixodidae): Evidence for the existence of antimicrobial proteins in tick hemolymph. J. Med. Entomol. 1998, 35, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Ceraul, S.M.; Sonenshine, D.E.; Hynes, W.L. Resistance of the tick dermacentor variabilis (Acari: Ixodidae) following challenge with the bacterium Escherichia coli (Enterobacteriales: Enterobacteriaceae). J. Med. Entomol. 2002, 39, 376–383. [Google Scholar] [CrossRef] [Green Version]
- Eggenberger, L.R.; Lamoreaux, W.J.; Coons, L.B. Hemocytic encapsulation of implants in the tick Dermacentor variabilis. Exp. Appl. Acarol. 1990, 9, 279–287. [Google Scholar] [CrossRef]
- Mambie, A.; Wallet, F.; Scherman, L.; Armand, S.; Vervelle, C.; Faure, K.; Guery, B.; Titecat, M.; Loiez, C. Neither Neoplasia nor Tuberculosis, but Francisella. Open Forum Infect. Dis. 2016, 3, ofw080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bokhari, S.M.; Kim, K.J.; Pinson, D.M.; Slusser, J.; Yeh, H.W.; Parmely, M.J. NK cells and gamma interferon coordinate the formation and function of hepatic granulomas in mice infected with the Francisella tularensis live vaccine strain. Infect. Immun. 2008, 76, 1379–1389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasmussen, J.W.; Cello, J.; Gil, H.; Forestal, C.A.; Furie, M.B.; Thanassi, D.G.; Benach, J.L. Mac-1+ cells are the predominant subset in the early hepatic lesions of mice infected with Francisella tularensis. Infect. Immun. 2006, 74, 6590–6598. [Google Scholar] [CrossRef] [Green Version]
- Johns, R.; Sonenshine, D.E.; Hynes, W.L. Response of the tick Dermacentor variabilis (Acari: Ixodidae) to hemocoelic inoculation of Borrelia burgdorferi (Spirochetales). J. Med. Entomol. 2000, 37, 265–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.; Narasimhan, S.; Dai, J.; Zhang, L.; Cheng, G.; Fikrig, E. Ixodes scapularis salivary gland protein P11 facilitates migration of Anaplasma phagocytophilum from the tick gut to salivary glands. EMBO Rep. 2011, 12, 1196–1203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goddard, J. Experimental infection of lone star ticks, Amblyomma americanum (L.), with Rickettsia parkeri and exposure of guinea pigs to the agent. J. Med. Entomol. 2003, 40, 686–689. [Google Scholar] [CrossRef]
- Jones, C.L.; Napier, B.A.; Sampson, T.R.; Llewellyn, A.C.; Schroeder, M.R.; Weiss, D.S. Subversion of host recognition and defense systems by Francisella spp. Microbiol. Mol. Biol. Rev. 2012, 76, 383–404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiner, D.J.; Furuya, Y.; Metzger, D.W. Detrimental Influence of Alveolar Macrophages on Protective Humoral Immunity during Francisella tularensis SchuS4 Pulmonary Infection. Infect. Immun. 2018, 86, e00787-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gulia-Nuss, M.; Nuss, A.B.; Meyer, J.M.; Sonenshine, D.E.; Roe, R.M.; Waterhouse, R.M.; Sattelle, D.B.; de la Fuente, J.; Ribeiro, J.M.; Megy, K.; et al. Genomic insights into the Ixodes scapularis tick vector of Lyme disease. Nat. Commun. 2016, 7, 10507. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Zhu, S. The defensin gene family expansion in the tick Ixodes scapularis. Dev. Comp. Immunol. 2011, 35, 1128–1134. [Google Scholar] [CrossRef]
- Ceraul, S.M.; Dreher-Lesnick, S.M.; Gillespie, J.J.; Rahman, M.S.; Azad, A.F. New tick defensin isoform and antimicrobial gene expression in response to Rickettsia montanensis challenge. Infect. Immun. 2007, 75, 1973–1983. [Google Scholar] [CrossRef] [Green Version]
- Ceraul, S.M.; Dreher-Lesnick, S.M.; Mulenga, A.; Rahman, M.S.; Azad, A.F. Functional characterization and novel rickettsiostatic effects of a Kunitz-type serine protease inhibitor from the tick Dermacentor variabilis. Infect. Immun. 2008, 76, 5429–5435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ceraul, S.M.; Chung, A.; Sears, K.T.; Popov, V.L.; Beier-Sexton, M.; Rahman, M.S.; Azad, A.F. A Kunitz protease inhibitor from Dermacentor variabilis, a vector for spotted fever group rickettsiae, limits Rickettsia montanensis invasion. Infect. Immun. 2011, 79, 321–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johns, R.; Sonenshine, D.E.; Hynes, W.L. Identification of a defensin from the hemolymph of the American dog tick, Dermacentor variabilis. Insect. Biochem. Mol. Biol. 2001, 31, 857–865. [Google Scholar] [CrossRef] [Green Version]
- Kocan, K.M.; de la Fuente, J.; Manzano-Roman, R.; Naranjo, V.; Hynes, W.L.; Sonenshine, D.E. Silencing expression of the defensin, varisin, in male Dermacentor variabilis by RNA interference results in reduced Anaplasma marginale infections. Exp. Appl. Acarol. 2008, 46, 17–28. [Google Scholar] [CrossRef] [Green Version]
- Kocan, K.M.; Zivkovic, Z.; Blouin, E.F.; Naranjo, V.; Almazan, C.; Mitra, R.; de la Fuente, J. Silencing of genes involved in Anaplasma marginale-tick interactions affects the pathogen developmental cycle in Dermacentor variabilis. BMC Dev. Biol. 2009, 9, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, T.K.; Tirloni, L.; Pinto, A.F.M.; Diedrich, J.K.; Moresco, J.J.; Yates, J.R., III; da Silva Vaz, I., Jr.; Mulenga, A. Time-resolved proteomic profile of Amblyomma americanum tick saliva during feeding. PloS Negl. Trop. Dis. 2020, 14, e0007758. [Google Scholar] [CrossRef] [Green Version]
- Larsson, P.; Oyston, P.C.; Chain, P.; Chu, M.C.; Duffield, M.; Fuxelius, H.H.; Garcia, E.; Halltorp, G.; Johansson, D.; Isherwood, K.E.; et al. The complete genome sequence of Francisella tularensis, the causative agent of tularemia. Nat. Genet. 2005, 37, 153–159. [Google Scholar] [CrossRef] [Green Version]
- Caimano, M.J.; Drecktrah, D.; Kung, F.; Samuels, D.S. Interaction of the Lyme disease spirochete with its tick vector. Cell. Microbiol. 2016, 18, 919–927. [Google Scholar] [CrossRef] [Green Version]
- Kung, F.; Anguita, J.; Pal, U. Borrelia burgdorferi and tick proteins supporting pathogen persistence in the vector. Future Microbiol. 2013, 8, 41–56. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tully, B.G.; Huntley, J.F. Mechanisms Affecting the Acquisition, Persistence and Transmission of Francisella tularensis in Ticks. Microorganisms 2020, 8, 1639. https://doi.org/10.3390/microorganisms8111639
Tully BG, Huntley JF. Mechanisms Affecting the Acquisition, Persistence and Transmission of Francisella tularensis in Ticks. Microorganisms. 2020; 8(11):1639. https://doi.org/10.3390/microorganisms8111639
Chicago/Turabian StyleTully, Brenden G., and Jason F. Huntley. 2020. "Mechanisms Affecting the Acquisition, Persistence and Transmission of Francisella tularensis in Ticks" Microorganisms 8, no. 11: 1639. https://doi.org/10.3390/microorganisms8111639
APA StyleTully, B. G., & Huntley, J. F. (2020). Mechanisms Affecting the Acquisition, Persistence and Transmission of Francisella tularensis in Ticks. Microorganisms, 8(11), 1639. https://doi.org/10.3390/microorganisms8111639





