Bacterial Meningitis in Children: Neurological Complications, Associated Risk Factors, and Prevention
Abstract
:1. Introduction
2. Epidemiology and Etiology
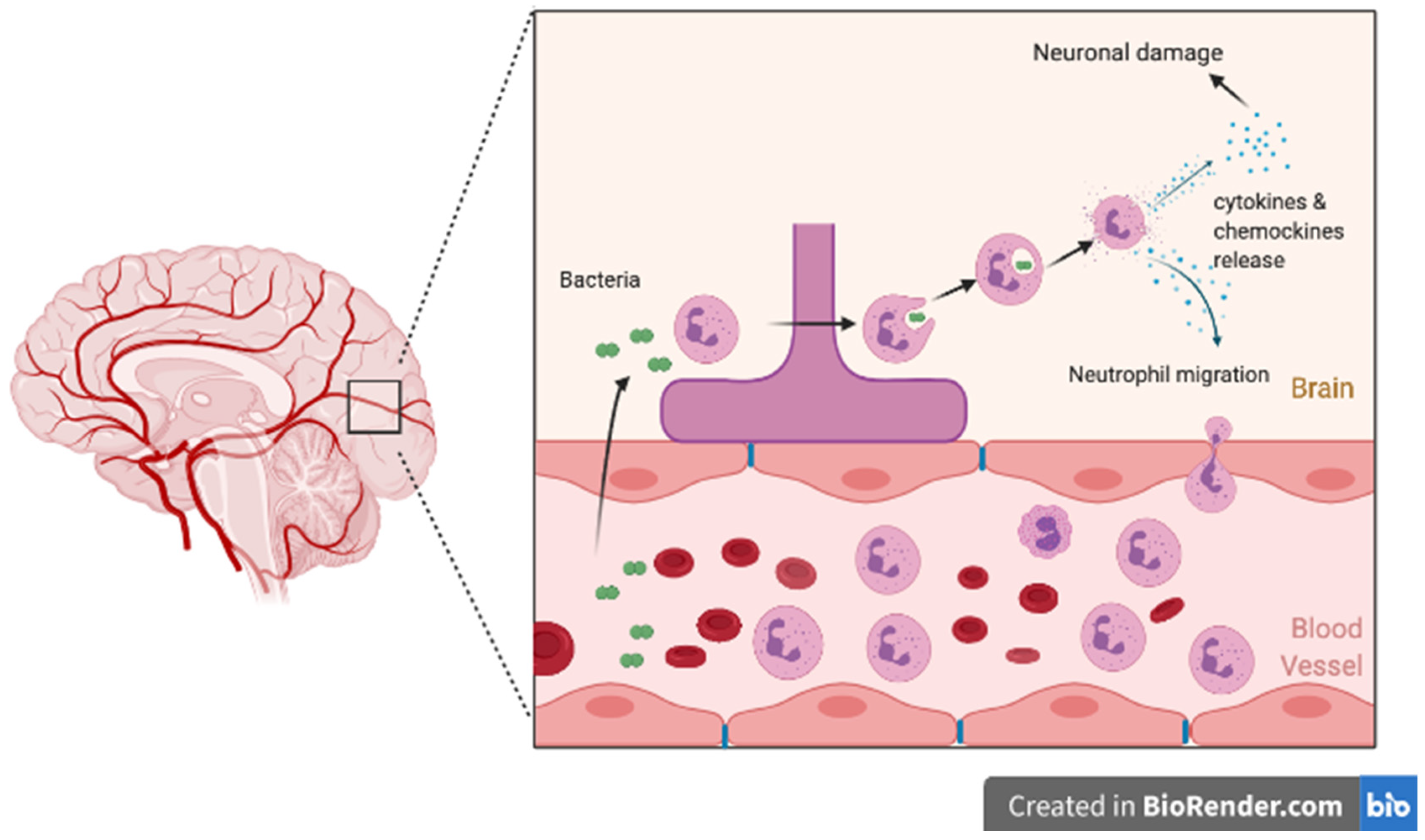
3. Pathophysiology of Bacterial Meningitis
4. Bacterial Meningitis Complications
4.1. Short-Term Complications
4.1.1. Subdural Effusion
4.1.2. Focal Neurological Deficit
4.2. Long-Term Complications
4.2.1. Hearing Loss
4.2.2. Cognitive Impairment
4.2.3. Seizures and Epilepsy
4.2.4. Hydrocephalus
5. Risk Factors
6. Prevention of Neurological Complication
6.1. Primary Prevention
6.2. Secondary Prevention of Complications
6.2.1. Antibiotic Therapy
6.2.2. Corticosteroids
7. Long-Term Follow Up
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grandgirard, D.; Leib, S.L. Strategies to prevent neuronal damage in paediatric bacterial meningitis. Curr. Opin. Pediatr. 2006, 18, 112–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sonko, A.M.; Dube, F.S.; Okoi, C.B.; Diop, A.; Thiongane, A.; Senghore, M.; Ndow, P.; Worwui, A.; Faye, P.M.; Dieye, B.; et al. Changes in the Molecular Epidemiology of Pediatric Bacterial Meningitis in Senegal after Pneumococcal Conjugate Vaccine Introduction. Clin. Infect. Dis. 2019, 69, S156–S163. [Google Scholar] [CrossRef] [PubMed]
- Shieh, H.H.; Ragazzi, S.L.B.; Gilio, A.E. Risk factors for neurological complications and sequelae in childhood acute bacterial meningitis. J. Pediatr. 2012, 88, 184. [Google Scholar] [CrossRef] [Green Version]
- Thigpen, M.C.; Whitney, C.G.; Messonnier, N.E.; Zell, E.R.; Lynfield, R.; Hadler, J.L.; Harrison, L.H.; Farley, M.M.; Reingold, A.; Bennett, N.M.; et al. Bacterial Meningitis in the United States, 1998–2007. N. Engl. J. Med. 2011, 364, 2016–2025. [Google Scholar] [CrossRef]
- Yogev, R.; A Guzmancottrill, J. Bacterial Meningitis in Children. Drugs 2005, 65, 1097–1112. [Google Scholar] [CrossRef]
- Pelkonen, T.; Roine, I.; Monteiro, L.; Correia, M.; Pitkäranta, A.; Bernardino, L.; Peltola, H. Risk Factors for Death and Severe Neurological Sequelae in Childhood Bacterial Meningitis in Sub-Saharan Africa. Clin. Infect. Dis. 2009, 48, 1107–1110. [Google Scholar] [CrossRef] [Green Version]
- Lucas, M.J.; Brouwer, M.C.; van de Beek, D. Neurological sequelae of bacterial meningitis. J. Infect. 2016, 73, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Namani, S.A.; Koci, B.M.; Milenković, Z.; Koci, R.; Qehaja-Buçaj, E.; Ajazaj, L.; Mehmeti, M.; Ismaili-Jaha, V. Early neurologic complications and long-term sequelae of childhood bacterial meningitis in a limited-resource country (Kosovo). Child’s Nerv. Syst. 2012, 29, 275–280. [Google Scholar] [CrossRef]
- Namani, S.; Milenković, Z.; Koci, B. A prospective study of risk factors for neurological complications in childhood bacterial meningitis. J. Pediatr. 2013, 89, 256–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ispahani, P.; Slack, R.C.B.; Donald, E.F.; Weston, V.C.; Rutter, N. Twenty year surveillance of invasive pneumococcal disease in Nottingham: Serogroups responsible and implications for immunisation. Arch. Dis. Child. 2004, 89, 757–762. [Google Scholar] [CrossRef]
- Softić, I.; Tahirović, H.; Hasanhodžić, M. Neonatal bacterial meningitis: Results from a cross-sectional hospital based study. Acta Med. Acad. 2015, 44, 117–123. [Google Scholar]
- Baud, O.; Aujard, Y. Neonatal Bacterial Meningitis; Elsevier: Amsterdam, The Netherlands, 2013; Volume 112, pp. 1109–1113. [Google Scholar]
- Molyneux, E.M.; Walsh, A.L.; Forsyth, H.; Tembo, M.; Mwenechanya, J.; Kayira, K.; Bwanaisa, L.; Njobvu, A.; Rogerson, S.; Malenga, G. Dexamethasone treatment in childhood bacterial meningitis in Malawi: A randomised controlled trial. Lancet 2002, 360, 211–218. [Google Scholar] [CrossRef]
- Zunt, J.R.; Kassebaum, N.J.; Blake, N.; Glennie, L.; Wright, C.; Nichols, E.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; A Adamu, A.; et al. Global, regional, and national burden of meningitis, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 1061–1082. [Google Scholar] [CrossRef] [Green Version]
- McIntyre, P.B.; O’Brien, K.L.; Greenwood, B.; van de Beek, D. Effect of vaccines on bacterial meningitis worldwide. Lancet 2012, 380, 1703–1711. [Google Scholar] [CrossRef]
- McAlpine, A.; Sadarangani, M. Meningitis vaccines in children. Curr. Opin. Infect. Dis. 2019, 32, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Mwenda, J.M.; Soda, E.; Weldegebriel, G.; Katsande, R.; Biey, J.N.-M.; Traore, T.; De Gouveia, L.; Du Plessis, M.; Von Gottberg, A.; Antonio, M.; et al. Pediatric Bacterial Meningitis Surveillance in the World Health Organization African Region Using the Invasive Bacterial Vaccine-Preventable Disease Surveillance Network, 2011–2016. Clin. Infect. Dis. 2019, 69, 49–57. [Google Scholar] [CrossRef] [Green Version]
- Bettinger, J.A.; Scheifele, D.W.; Kellner, J.D.; Halperin, S.A.; Vaudry, W.; Law, B.; Tyrrell, G. The effect of routine vaccination on invasive pneumococcal infections in Canadian children, Immunization Monitoring Program, Active 2000–2007. Vaccine 2010, 28, 2130–2136. [Google Scholar] [CrossRef] [PubMed]
- Bettinger, J.A.; Scheifele, D.W.; Halperin, S.A.; Kellner, J.D.; Vanderkooi, O.G.; Schryvers, A.; De Serres, G.; Alcantara, J. Evaluation of meningococcal serogroup C conjugate vaccine programs in Canadian children: Interim analysis. Vaccine 2012, 30, 4023–4027. [Google Scholar] [CrossRef] [PubMed]
- Leal, J.; Vanderkooi, O.G.; Church, D.L.; MacDonald, J.; Tyrrell, G.J.; Kellner, J.D. Eradication of Invasive Pneumococcal Disease due to the Seven-valent Pneumococcal Conjugate Vaccine Serotypes in Calgary, Alberta. Pediatr. Infect. Dis. J. 2012, 31, e169–e175. [Google Scholar] [CrossRef] [PubMed]
- Gaschignard, J.; Levy, C.; Romain, O.; Cohen, R.; Bingen, E.; Aujard, Y.; Boileau, P. Neonatal Bacterial Meningitis. Pediatr. Infect. Dis. J. 2011, 30, 212–217. [Google Scholar] [CrossRef]
- Smith, P.B.; Garges, H.P.; Cotton, C.M.; Walsh, T.J.; Clark, R.H.; Benjamin, D.K.; Cotten, C.M. Meningitis in Preterm Neonates: Importance of Cerebrospinal Fluid Parameters. Am. J. Perinatol. 2008, 25, 421–426. [Google Scholar] [CrossRef] [Green Version]
- McCormick, D.W.; Wilson, M.L.; Mankhambo, L.; Phiri, A.; Chimalizeni, Y.; Kawaza, K.; Denis, B.; Carrol, E.D.; Molyneux, E.M. Risk Factors for Death and Severe Sequelae in Malawian Children with Bacterial Meningitis, 1997–2010. Pediatr. Infect. Dis. J. 2013, 32, e54–e61. [Google Scholar] [CrossRef] [Green Version]
- Schuchat, A.; Robinson, K.; Wenger, J.D.; Harrison, L.H.; Farley, M.; Reingold, A.L.; Lefkowitz, L.; Perkins, B.A. Bacterial Meningitis in the United States in 1995. N. Engl. J. Med. 1997, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Cockcroft, D.W.; Nair, P. Methacholine test and the diagnosis of asthma. J. Allergy Clin. Immunol. 2012, 130, 556–557. [Google Scholar] [CrossRef]
- Ceyhan, M.; Gürler, N.; Ozsurekci, Y.; Keser, M.; Aycan, A.E.; Gurbuz, V.; Salman, N.; Camcioglu, Y.; Dinleyici, E.C.; Ozkan, S.; et al. Meningitis caused by Neisseria Meningitidis, Hemophilus Influenzae Type B and Streptococcus Pneumoniae during 2005–2012 in Turkey. Hum. Vaccines Immunother. 2014, 10, 2706–2712. [Google Scholar] [CrossRef] [Green Version]
- Duke, T.; Curtis, N.; Fuller, D.G. The management of bacterial meningitis in children. Expert Opin. Pharmacother. 2003, 4, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Phares, C.R.; Lynfield, R.; Farley, M.M.; Mohle-Boetani, J.; Harrison, L.H.; Petit, S.; Craig, A.S.; Schaffner, W.; Zansky, S.M.; Gershman, K.; et al. Epidemiology of Invasive Group B Streptococcal Disease in the United States, 1999–2005. JAMA 2008, 299, 2056–2065. [Google Scholar] [CrossRef]
- Edmond, K.M.; Kortsalioudaki, C.; Scott, S.; Schrag, S.J.; Zaidi, A.K.; Cousens, S.; Heath, P.T. Group B streptococcal disease in infants aged younger than 3 months: Systematic review and meta-analysis. Lancet 2012, 379, 547–556. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.S. Pathogenesis of bacterial meningitis: From bacteraemia to neuronal injury. Nat. Rev. Neurosci. 2003, 4, 376–385. [Google Scholar] [CrossRef]
- Koedel, U.; Klein, M.; Pfister, H.-W. New understandings on the pathophysiology of bacterial meningitis. Curr. Opin. Infect. Dis. 2010, 23, 217–223. [Google Scholar] [CrossRef]
- Scheld, W.M.; Koedel, U.; Nathan, B.; Pfister, H. Pathophysiology of Bacterial Meningitis: Mechanism (s) of Neuronal Injury. J. Infect. Dis. 2002, 186, 225–233. [Google Scholar] [CrossRef]
- Barichello, T.; Generoso, J.S.; Simões, L.R.; Goularte, J.A.; Petronilho, F.; Saigal, P.; Badawy, M.; Quevedo, J. Role of Microglial Activation in the Pathophysiology of Bacterial Meningitis. Mol. Neurobiol. 2016, 53, 1770–1781. [Google Scholar] [CrossRef]
- Hoffman, O.; Weber, J.R. Review: Pathophysiology and treatment of bacterial meningitis. Ther. Adv. Neurol. Disord. 2009, 2, 401–412. [Google Scholar] [CrossRef] [Green Version]
- Mook-Kanamori, B.B.; Geldhoff, M.; Van Der Poll, T.; Van De Beek, D. Pathogenesis and Pathophysiology of Pneumococcal Meningitis. Clin. Microbiol. Rev. 2011, 24, 557–591. [Google Scholar] [CrossRef] [Green Version]
- Chaudhuri, A. Adjunctive dexamethasone treatment in acute bacterial meningitis. Lancet Neurol. 2004, 3, 54–62. [Google Scholar] [CrossRef]
- Baraff, L.J.; Lee, S.I.; Schriger, D.L. Outcome of Bacterial Meningitis in Children a Meta-Analysis. Pediatr. Infect. Dis. J. 1993, 12, 389–394. [Google Scholar] [CrossRef]
- Mahmoudi, S.; Zandi, H.; Pourakbari, B.; Ashtiani, M.T.H.; Mamishi, S. Acute Bacterial Meningitis among Children Admitted into an Iranian Referral Children’s Hospital. Jpn. J. Infect. Dis. 2013, 66, 503–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, A.; Bradley, A.; Wall, R.; McPherson, B.; Secka, A.; Dunn, D.; Greenwood, B. Sequelae of epidemic meningococcal meningitis in Africa. Trans. R. Soc. Trop. Med. Hyg. 1988, 82, 312–320. [Google Scholar] [CrossRef]
- Casella, E.B.; Cypel, S.; Osmo, A.A.; Okay, Y.; Lefèvre, B.H.; Lichtig, I.; Marques-Dias, M.J. Sequelae from meningococcal meningitis in children: A critical analysis of dexamethasone therapy. Arq. Neuro-Psiquiatr. 2004, 62, 421–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Østergaard, C.; Konradsen, H.B.; Samuelsson, S. Clinical presentation and prognostic factors of Streptococcus pneumoniae meningitis according to the focus of infection. BMC Infect. Dis. 2005, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klobassa, D.S.; Zoehrer, B.; Paulke-Korinek, M.; Gruber-Sedlmayr, U.; Pfurtscheller, K.; Strenger, V.; Sonnleitner, A.; Kerbl, R.; Ausserer, B.; Arocker, W.; et al. The burden of pneumococcal meningitis in Austrian children between 2001 and 2008. Eur. J. Nucl. Med. Mol. Imaging 2014, 173, 871–878. [Google Scholar] [CrossRef]
- Saha, S.K.; Khan, N.Z.; Ahmed, A.S.M.N.U.; Amin, M.R.; Hanif, M.; Mahbub, M.; Anwar, K.S.; Qazi, S.A.; Kilgore, P.; Baqui, A.H.; et al. Neurodevelopmental Sequelae in Pneumococcal Meningitis Cases in Bangladesh: A Comprehensive Follow-up Study. Clin. Infect. Dis. 2009, 48, 90–96. [Google Scholar] [CrossRef]
- Arditi, M.; Mason, E.O.; Bradley, J.S.; Tan, T.Q.; Barson, W.J.; Schutze, G.E.; Wald, E.R.; Givner, L.B.; Kim, K.S.; Yogev, R.; et al. Three-Year Multicenter Surveillance of Pneumococcal Meningitis in Children: Clinical Characteristics, and Outcome Related to Penicillin Susceptibility and Dexamethasone Use. Pediatrics 1998, 102, 1087–1097. [Google Scholar] [CrossRef] [PubMed]
- Karppinen, M.; Pelkonen, T.; Roine, I.; Cruzeiro, M.L.; Peltola, H.; Pitkäranta, A. Hearing impairment after childhood bacterial meningitis dependent on etiology in Luanda, Angola. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 1820–1826. [Google Scholar] [CrossRef] [PubMed]
- King, B.; Richmond, P. Pneumococcal meningitis in Western Australian children: Epidemiology, microbiology and outcome. J. Paediatr. Child Health 2004, 40, 611–615. [Google Scholar] [CrossRef] [PubMed]
- Osuorah, D.; Shah, B.; Manjang, A.; Secka, E.; Ekwochi, U.; Ebenebe, J. Outbreak of serotype W135 Neisseria meningitidis in central river region of the Gambia between February and June 2012: A hospital-based review of paediatric cases. Niger. J. Clin. Pr. 2014, 18, 41–47. [Google Scholar]
- Koomen, I.; Grobbee, D.; Jennekens-Schinkel, A.; Roord, J.; Furth, A. Parental perception of educational, behavioural and general health problems in school-age survivors of bacterial meningitis. Acta Paediatr. 2007, 92, 177–185. [Google Scholar] [CrossRef]
- Roed, C.; Omland, L.H.; Skinhoj, P.; Rothman, K.J.; Sorensen, H.T.; Obel, N. Educational Achievement and Economic Self-sufficiency in Adults after Childhood Bacterial Meningitis. JAMA 2013, 309, 1714–1721. [Google Scholar] [CrossRef] [Green Version]
- Taylor, H.G.; Schatschneider, C.; Minich, N.M. Longitudinal outcomes of Haemophilus influenzae meningitis in school-age children. Neuropsychology 2000, 14, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Snedeker, J.D.; Kaplan, S.L.; Dodge, P.R.; Holmes, S.J.; Feigin, R.D. Subdural effusion and its relationship with neurologic sequelae of bacterial meningitis in infancy: A prospective study. Pediatrics 1990, 86, 163–170. [Google Scholar]
- Olarte, L.; Barson, W.J.; Barson, R.M.; Lin, P.L.; Romero, J.R.; Tan, T.Q.; Givner, L.B.; Bradley, J.S.; Hoffman, J.A.; Hultén, K.G.; et al. Impact of the 13-Valent Pneumococcal Conjugate Vaccine on Pneumococcal Meningitis in US Children. Clin. Infect. Dis. 2015, 61, 767–775. [Google Scholar] [CrossRef] [Green Version]
- Wippold, F.J. Focal neurologic deficit. Am. J. Neuroradiol. 2008, 29, 1998–2000. [Google Scholar] [PubMed]
- Dunbar, M.; Shah, H.; Shinde, S.; Vayalumkal, J.; Vanderkooi, O.G.; Wei, X.-C.; Kirton, A. Stroke in Pediatric Bacterial Meningitis: Population-Based Epidemiology. Pediatr. Neurol. 2018, 89, 11–18. [Google Scholar] [CrossRef]
- Tibussek, D.; Sinclair, A.; Yau, I.; Teatero, S.; Fittipaldi, N.; Richardson, S.E.; Mayatepek, E.; Jahn, P.; Askalan, R. Late-Onset Group B Streptococcal Meningitis Has Cerebrovascular Complications. J. Pediatr. 2015, 166, 1187–1192. [Google Scholar] [CrossRef] [PubMed]
- Masri, A.; Alassaf, A.; Khuri-Bulos, N.; Zaq, I.; Hadidy, A.; Bakri, F.G. Recurrent meningitis in children: Etiologies, outcome, and lessons to learn. Child’s Nerv. Syst. 2018, 34, 1541–1547. [Google Scholar] [CrossRef]
- Unhanand, M.; Mustafa, M.M.; McCracken, G.H.; Nelson, J.D. Gram-negative enteric bacillary meningitis: A twenty-one-year experience. J. Pediatr. 1993, 122, 15–21. [Google Scholar] [CrossRef]
- Brouwer, M.C.; Wijdicks, E.F.M.; Van De Beek, D. What’s new in bacterial meningitis. Intensiv. Care Med. 2016, 42, 415–417. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Liu, X.; Wang, Y.; Liu, Q.; Kong, C.; Xu, G. Meta-analysis of adjunctive dexamethasone to improve clinical outcome of bacterial meningitis in children. Child’s Nerv. Syst. 2017, 34, 217–223. [Google Scholar] [CrossRef]
- Dodge, P.R.; Davis, H.; Feigin, R.D.; Holmes, S.J.; Kaplan, S.L.; Jubelirer, D.P.; Stechenberg, B.W.; Hirsh, S.K. Prospective Evaluation of Hearing Impairment as a Sequela of Acute Bacterial Meningitis. N. Engl. J. Med. 1984, 311, 869–874. [Google Scholar] [CrossRef]
- Sáez-Llorens, X.; McCracken, G.H. Acute Bacterial Meningitis beyond the Neonatal Period; Elsevier: Amsterdam, The Netherlands, 2008; pp. 284–291. [Google Scholar]
- Yoshinaga-Itano, C.; Sedey, A.L.; Coulter, D.K.; Mehl, A.L. Language of Early- and Later-identified Children with Hearing Loss. Pediatrics 1998, 102, 1161–1171. [Google Scholar] [CrossRef] [Green Version]
- Hall, W.C.; Li, N.; Dye, T.D.V. Influence of Hearing Loss on Child Behavioral and Home Experiences. Am. J. Public Health 2018, 108, 1079–1081. [Google Scholar] [CrossRef] [PubMed]
- Kostenniemi, U.J.; Bazan, A.; Karlsson, L.; Silfverdal, S.-A. Psychiatric Disabilities and Other Long-term Consequences of Childhood Bacterial Meningitis. Pediatr. Infect. Dis. J. 2020, 40, 26–31. [Google Scholar] [CrossRef]
- Kostenniemi, U.J.; Norman, D.; Borgström, M.; Silfverdal, S.A. The clinical presentation of acute bacterial meningitis varies with age, sex and duration of illness. Acta Paediatr. 2015, 104, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Curtis, S.; Stobart, K.; VanderMeer, B.; Simel, D.L.; Klassen, T. Clinical Features Suggestive of Meningitis in Children: A Systematic Review of Prospective Data. Pediatrics 2010, 126, 952–960. [Google Scholar] [CrossRef]
- Namani, S.A.; Kuchar, E.; Koci, R.; Mehmeti, M.; Dedushi, K. Early symptomatic and late seizures in Kosovar children with bacterial meningitis. Child’s Nerv. Syst. 2011, 27, 1967–1971. [Google Scholar] [CrossRef] [PubMed]
- Murthy, J.M.K.; Prabhakar, S. Bacterial meningitis and epilepsy. Epilepsia 2008, 49, 8–12. [Google Scholar] [CrossRef]
- Preux, P.-M.; Druet-Cabanac, M. Epidemiology and aetiology of epilepsy in sub-Saharan Africa. Lancet Neurol. 2005, 4, 21–31. [Google Scholar] [CrossRef]
- Pomeroy, S.L.; Holmes, S.J.; Dodge, P.R.; Feigin, R.D. Seizures and Other Neurologic Sequelae of Bacterial Meningitis in Children. N. Engl. J. Med. 1990, 323, 1651–1657. [Google Scholar] [CrossRef]
- De Jonge, R.C.; Van Furth, A.M.; Wassenaar, M.; Gemke, R.J.; Terwee, C.B. Predicting sequelae and death after bacterial meningitis in childhood: A systematic review of prognostic studies. BMC Infect. Dis. 2010, 10, 232. [Google Scholar] [CrossRef] [Green Version]
- Pong, A.; Bradley, J.S. Bacterial Meningitis and the Newborn Infant. Infect. Dis. Clin. N. Am. 1999, 13, 711–733. [Google Scholar] [CrossRef]
- Ouchenir, L.; Renaud, C.; Khan, S.; Bitnun, A.; Boisvert, A.-A.; McDonald, J.; Bowes, J.; Brophy, J.; Barton, M.; Ting, J.; et al. The Epidemiology, Management, and Outcomes of Bacterial Meningitis in Infants. Pediatrics 2017, 140, e20170476. [Google Scholar] [CrossRef] [Green Version]
- Huo, L.; Fan, Y.; Jiang, C.; Gao, J.; Yin, M.; Wang, H.; Yang, F.; Cao, Q. Clinical Features of and Risk Factors for Hydrocephalus in Childhood Bacterial Meningitis. J. Child Neurol. 2018, 34, 11–16. [Google Scholar] [CrossRef]
- Tamber, M.S.; Klimo, P.; Mazzola, C.A.; Flannery, A.M. Pediatric hydrocephalus: Systematic literature review and evidence-based guidelines. Part 8: Management of cerebrospinal fluid shunt infection. J. Neurosurg. Pediatr. 2014, 14, 60–71. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, D.C.; Diniz, L.M.O.; Guimarães, N.S.; Moreira, H.M.D.A.S.; Teixeira, C.C.; Romanelli, R.M.D.C. Risk factors associated with the outcomes of pediatric bacterial meningitis: A systematic review. J. Pediatr. 2020, 96, 159–167. [Google Scholar] [CrossRef]
- Feavers, I.; Pollard, A.J.; Sadarangani, M. Handbook of Meningococcal Disease Management; Springer International Publishing: Berlin/Heidelberg, Germany, 2016. [Google Scholar] [CrossRef]
- Pace, D.; Pollard, A.J. Meningococcal disease: Clinical presentation and sequelae. Vaccine 2012, 30, B3–B9. [Google Scholar] [CrossRef]
- Aku, F.Y.; Lessa, F.C.; Asiedu-Bekoe, F.; Balagumyetime, P.; Ofosu, W.; Farrar, J.; Ouattara, M.; Vuong, J.T.; Issah, K.; Opare, J.; et al. Meningitis Outbreak Caused by Vaccine-Preventable Bacterial Pathogens—Northern Ghana, 2016. Morb. Mortal. Wkly. Rep. 2017, 66, 806–810. [Google Scholar] [CrossRef] [Green Version]
- Greenwood, B. Editorial: 100 years of epidemic meningitis in West Africa—Has anything changed? Trop. Med. Int. Health 2006, 11, 773–780. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services Center for Disease Control and Prevention. Haemophilus Influenzae Type b (Hib) Vaccine: What You Need to Know Hib Vaccine. 2019. Available online: https://www.cdc.gov/vaccines/hcp/vis/vis-statements/hib.html (accessed on 2 January 2021).
- US Department of Health and Human Services Center for Disease Control and Prevention. Pneumococcal Polysaccharide Vaccine (PPSV23): What You Need to Know. 2019. Available online: https://www.cdc.gov/vaccines/hcp/vis/vis-statements/ppv.html (accessed on 2 January 2021).
- Bijlsma, M.W.; Brouwer, M.C.; Spanjaard, L.; Van De Beek, D.; Van Der Ende, A. A Decade of Herd Protection after Introduction of Meningococcal Serogroup C Conjugate Vaccination. Clin. Infect. Dis. 2014, 59, 1216–1221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitney, C.G.; Farley, M.M.; Hadler, J.; Harrison, L.H.; Bennett, N.M.; Lynfield, R.; Reingold, A.; Cieslak, P.R.; Pilishvili, T.; Jackson, D.; et al. Decline in Invasive Pneumococcal Disease after the Introduction of Protein–Polysaccharide Conjugate Vaccine. N. Engl. J. Med. 2003, 348, 1737–1746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nigrovic, L.E.; Kuppermann, N.; Malley, R. For the Bacterial Meningitis Study Group of the Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics Children with Bacterial Meningitis Presenting to the Emergency Department during the Pneumococcal Conjugate Vaccine Era. Acad. Emerg. Med. 2008, 15, 522–528. [Google Scholar] [CrossRef]
- Ngocho, J.S.; Magoma, B.; Olomi, G.A.; Mahande, M.J.; Msuya, S.E.; De Jonge, M.I.; Mmbaga, B.T. Effectiveness of pneumococcal conjugate vaccines against invasive pneumococcal disease among children under five years of age in Africa: A systematic review. PLoS ONE 2019, 14, e0212295. [Google Scholar] [CrossRef]
- Kaplan, S.L.; O Mason, E.; Wald, E.R.; Schutze, G.E.; Bradley, J.S.; Tan, T.Q.; Hoffman, J.A.; Givner, L.B.; Yogev, R.; Barson, W.J. Decrease of invasive pneumococcal infections in children among 8 children’s hospitals in the United States after the introduction of the 7-valent pneumococcal conjugate vaccine. Pediatrics 2004, 113, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Singleton, R.J.; Hennessy, T.W.; Bulkow, L.R.; Hammitt, L.L.; Zulz, T.; Hurlburt, D.A.; Butler, J.C.; Rudolph, K.; Parkinson, A. Invasive Pneumococcal Disease Caused by Nonvaccine Serotypes among Alaska Native Children with High Levels of 7-Valent Pneumococcal Conjugate Vaccine Coverage. JAMA 2007, 297, 1784–1792. [Google Scholar] [CrossRef] [PubMed]
- Bozio, C.H.; Vuong, J.; Dokubo, E.K.; Fallah, M.P.; A McNamara, L.; Potts, C.C.; Doedeh, J.; Gbanya, M.; Retchless, A.C.; Patel, J.C.; et al. Outbreak of Neisseria meningitidis serogroup C outside the meningitis belt—Liberia, 2017: An epidemiological and laboratory investigation. Lancet Infect. Dis. 2018, 18, 1360–1367. [Google Scholar] [CrossRef]
- Wall, E.C.; Everett, D.B.; Mukaka, M.; Bar-Zeev, N.; Feasey, N.; Jahn, A.; Moore, M.; Van Oosterhout, J.J.; Pensalo, P.; Baguimira, K.; et al. Bacterial Meningitis in Malawian Adults, Adolescents, and Children during the Era of Antiretroviral Scale-up and Haemophilus influenzae Type b Vaccination, 2000–2012. Clin. Infect. Dis. 2014, 58, e137–e145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peterson, E.M.; Li, Y.; Bita, A.; Moureau, A.; Nair, H.; Kyaw, M.H.; Abad, R.; Bailey, F.; Garcia, I.D.L.F.; Decheva, A.; et al. Meningococcal serogroups and surveillance: A systematic review and survey. J. Glob. Health 2018, 9, 010409. [Google Scholar] [CrossRef]
- Mustapha, M.M.; Harrison, L.H. Vaccine prevention of meningococcal disease in Africa: Major advances, remaining challenges. Hum. Vaccines Immunother. 2018, 14, 1107–1115. [Google Scholar] [CrossRef] [Green Version]
- Le Saux, N. Guidelines for the management of suspected and confirmed bacterial meningitis in Canadian children older than one month of age. Paediatr. Child Health 2014, 19, 141–146. [Google Scholar] [CrossRef] [Green Version]
- NICE UK. Meningitis (Bacterial) and Meningococcal Septicaemia in under 16s: Recognition, Diagnosis and Management. 2010. Available online: https://www.nice.org.uk/guidance/CG102/chapter/1-Guidance#pre-hospital-management-of-suspected-bacterial-meningitis-and-meningococcal-septicaemia (accessed on 14 January 2021).
- Agrawal, S.; Nadel, S. Acute bacterial meningitis in infants and children: Epidemiology and management. Pediatr. Drugs. 2011, 13, 385–400. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed10&NEWS=N&AN=2011577682 (accessed on 16 December 2020). [CrossRef]
- Nudelman, Y.; Tunkel, A.R. Bacterial Meningitis. Drugs 2009, 69, 2577–2596. [Google Scholar] [CrossRef]
- Chaudhuri, A.; Martinez-Martin, P.; Kennedy, P.G.E.; Seaton, R.A.; Portegies, P.; Bojar, M.; Steiner, I.; EFNS Task Force. EFNS guideline on the management of community-acquired bacterial meningitis: Report of an EFNS Task Force on acute bacterial meningitis in older children and adults. Eur. J. Neurol. 2008, 15, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, M.C.; McIntyre, P.; Prasad, K.; Van De Beek, D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst. Rev. 2015, 2015, e004405. [Google Scholar] [CrossRef] [PubMed]
- Schaad, U.B.; Kaplan, S.L.; McCracken, J.G.H. Steroid Therapy for Bacterial Meningitis. Clin. Infect. Dis. 1995, 20, 685–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, K.; Nichani, J.; Hans, P.; Bruce, I.; Henderson, L.; Ramsden, R. C096 Cochlear implantation in profound hearing loss following bacterial meningitis in children. Int. J. Pediatr. Otorhinolaryngol. 2011, 75, 50. [Google Scholar] [CrossRef]
- Bille, J.; Ovesen, T. Cochlear implant after bacterial meningitis. Pediatr. Int. 2014, 56, 400–405. [Google Scholar] [CrossRef]
| Age Group | Most Common Organisms | References |
|---|---|---|
| Pre-term neonate | Escherichia coli, GBS * | [12,21,22] |
| Term neonate and infants < three months | GBS *, E. coli, Streptococcus pneumoniae, Listeria monocytogenes | [12] |
| Children ≥ three months to ten years | S. pneumoniae, Neisseria meningitidis, Haemophilus influenzae type b | [3,13,23,24] |
| Adolescent until 19 years old | N. meningitidis, S. pneumoniae | [4,25,26] |
| Pneumococcal Meningitis | Meningococcal Meningitis | References | |||
|---|---|---|---|---|---|
| LMICs | HICs | LMICs | HICs | ||
| Focal deficits | 12% | 3–14% | 2–4% | 3% | [13,39,40,41,42] |
| Hearing loss | 25% | 14–32% | 19–23% | 4% | [10,13,43,44,45] |
| Seizures | 45–63% | 15–48% | 17–33% | 2% | [40,45,46,47] |
| Cognitive impairment | 4–41% | N/A * | 4% | 12–19% | [10,13,43,48,49] |
| Risk Factor | % with Neurological Complications | References |
|---|---|---|
| Young Age (infants < 12 months) | 71% | [9] |
| Etiology: S. pneumoniae | 75% | [9] |
| Altered Level of Consciousness on Presentation | 82% | [9] |
| Delayed Presentation | N/A * | [6,9] |
| Delayed initiation of antibiotics | N/A * | [76] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zainel, A.; Mitchell, H.; Sadarangani, M. Bacterial Meningitis in Children: Neurological Complications, Associated Risk Factors, and Prevention. Microorganisms 2021, 9, 535. https://doi.org/10.3390/microorganisms9030535
Zainel A, Mitchell H, Sadarangani M. Bacterial Meningitis in Children: Neurological Complications, Associated Risk Factors, and Prevention. Microorganisms. 2021; 9(3):535. https://doi.org/10.3390/microorganisms9030535
Chicago/Turabian StyleZainel, Abdulwahed, Hana Mitchell, and Manish Sadarangani. 2021. "Bacterial Meningitis in Children: Neurological Complications, Associated Risk Factors, and Prevention" Microorganisms 9, no. 3: 535. https://doi.org/10.3390/microorganisms9030535
APA StyleZainel, A., Mitchell, H., & Sadarangani, M. (2021). Bacterial Meningitis in Children: Neurological Complications, Associated Risk Factors, and Prevention. Microorganisms, 9(3), 535. https://doi.org/10.3390/microorganisms9030535






