Nasal Methicillin-Resistant Staphylococcus aureus Colonization in Patients with Type 1 Diabetes in Taiwan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Clinical Data Collection
2.2. Sampling
2.3. Antibiotic Susceptibility
2.4. Molecular Typing
2.5. Statistical Analysis
3. Results
3.1. Colonization and Patient Characteristics
3.2. Antibiotic Susceptibility
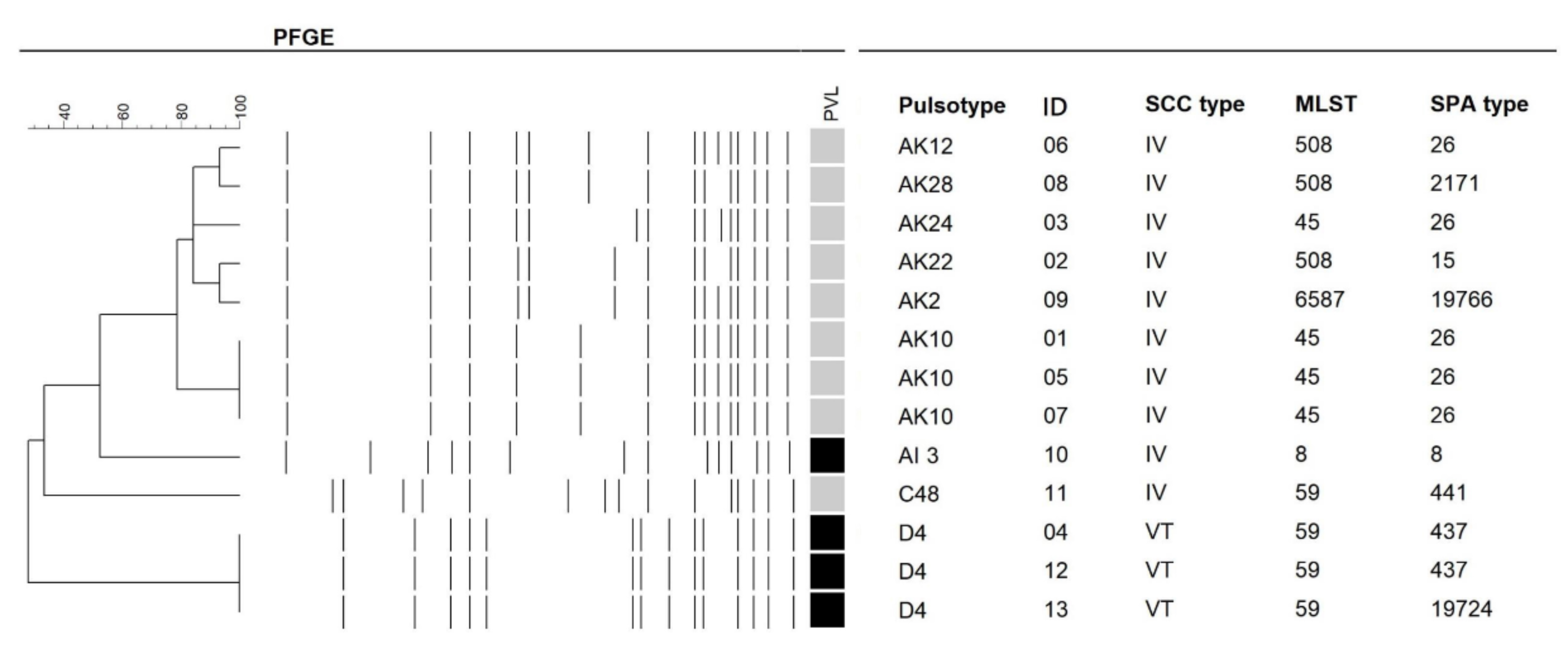
3.3. Molecular Characteristics
3.4. Factor Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lowy, F.D. Staphylococcus aureus infections. N. Engl. J. Med. 1998, 339, 520–532. [Google Scholar] [CrossRef]
- Tong, S.Y.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G., Jr. Staphylococcus aureus infections: Epidemiology, pathophysiology, clinical manifestations, and management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, D.; Harper, L.; Shopsin, B.; Torres, V.J. Staphylococcus aureus pathogenesis in diverse host environments. Pathog. Dis. 2017, 75. [Google Scholar] [CrossRef] [PubMed]
- Genovese, C.; D’Angeli, F.; Bellia, F.; Distefano, A.; Spampinato, M.; Attanasio, F.; Nicolosi, D.; Di Salvatore, V.; Tempera, G.; Lo Furno, D.; et al. In Vitro Antibacterial, Anti-Adhesive and Anti-Biofilm Activities of Krameria lappacea (Dombey) Burdet & B.B. Simpson Root Extract against Methicillin-Resistant Staphylococcus aureus Strains. Antibiotics 2021, 10, 428. [Google Scholar] [CrossRef] [PubMed]
- Tam, K.; Torres, V.J. Staphylococcus aureus Secreted Toxins and Extracellular Enzymes. Microbiol. Spectr. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- von Eiff, C.; Becker, K.; Machka, K.; Stammer, H.; Peters, G. Nasal carriage as a source of Staphylococcus aureus bacteremia. Study Group. N. Engl. J. Med. 2001, 344, 11–16. [Google Scholar] [CrossRef]
- Coates, T.; Bax, R.; Coates, A. Nasal decolonization of Staphylococcus aureus with mupirocin: Strengths, weaknesses and future prospects. J. Antimicrob. Chemother. 2009, 64, 9–15. [Google Scholar] [CrossRef]
- Barber, M. Methicillin-resistant staphylococci. J. Clin. Pathol. 1961, 14, 385–393. [Google Scholar] [CrossRef]
- Turner, N.A.; Sharma-Kuinkel, B.K.; Maskarinec, S.A.; Eichenberger, E.M.; Shah, P.P.; Carugati, M.; Holland, T.L.; Fowler, V.G., Jr. Methicillin-resistant Staphylococcus aureus: An overview of basic and clinical research. Nat. Rev. Microbiol. 2019, 17, 203–218. [Google Scholar] [CrossRef]
- Lee, A.S.; de Lencastre, H.; Garau, J.; Kluytmans, J.; Malhotra-Kumar, S.; Peschel, A.; Harbarth, S. Methicillin-resistant Staphylococcus aureus. Nat. Rev. Dis. Primers 2018, 4, 18033. [Google Scholar] [CrossRef]
- Chen, M.L.; Chang, S.C.; Pan, H.J.; Hsueh, P.R.; Yang, L.S.; Ho, S.W.; Luh, K.T. Longitudinal analysis of methicillin-resistant Staphylococcus aureus isolates at a teaching hospital in Taiwan. J. Formos Med. Assoc. 1999, 98, 426–432. [Google Scholar] [PubMed]
- Chen, C.J.; Huang, Y.C.; Chiu, C.H.; Su, L.H.; Lin, T.Y. Clinical features and genotyping analysis of community-acquired methicillin-resistant Staphylococcus aureus infections in Taiwanese children. Pediatr. Infect. Dis. J. 2005, 24, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Chen, C.J. Community-associated meticillin-resistant Staphylococcus aureus in children in Taiwan, 2000s. Int. J. Antimicrob. Agents 2011, 38, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.J.; Huang, Y.C. New epidemiology of Staphylococcus aureus infection in Asia. Clin. Microbiol. Infect. 2014, 20, 605–623. [Google Scholar] [CrossRef] [PubMed]
- Maffi, P.; Secchi, A. The Burden of Diabetes: Emerging Data. Dev. Ophthalmol. 2017, 60, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, M.A.; Eisenbarth, G.S.; Michels, A.W. Type 1 diabetes. Lancet 2014, 383, 69–82. [Google Scholar] [CrossRef]
- Ceccarelli, F.; Perricone, C.; Olivieri, G.; Cipriano, E.; Spinelli, F.R.; Valesini, G.; Conti, F. Staphylococcus aureus Nasal Carriage and Autoimmune Diseases: From Pathogenic Mechanisms to Disease Susceptibility and Phenotype. Int. J. Mol. Sci. 2019, 20, 5624. [Google Scholar] [CrossRef]
- Pavlović, M.D.; Milenković, T.; Dinić, M.; Misović, M.; Daković, D.; Todorović, S.; Daković, Z.; Zecevi, R.D.; Doder, R. The prevalence of cutaneous manifestations in young patients with type 1 diabetes. Diabetes Care 2007, 30, 1964–1967. [Google Scholar] [CrossRef]
- Szablewski, L. Role of immune system in type 1 diabetes mellitus pathogenesis. Int. Immunopharmacol. 2014, 22, 182–191. [Google Scholar] [CrossRef]
- Wertheim, H.F.; Melles, D.C.; Vos, M.C.; van Leeuwen, W.; van Belkum, A.; Verbrugh, H.A.; Nouwen, J.L. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 2005, 5, 751–762. [Google Scholar] [CrossRef]
- Casqueiro, J.; Casqueiro, J.; Alves, C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J. Endocrinol Metab. 2012, 16 (Suppl. S1), S27–S36. [Google Scholar] [CrossRef]
- Taiwan National Health Insurance Adminstration, Ministry of Health and Welfare. Patients with Chronic Diseases (Refill Prescriptions). Available online: https://www.nhi.gov.tw/english/Content_List.aspx?n=8499F575B188B17E&topn=1D1ECC54F86E9050 (accessed on 28 March 2021).
- Jarosz-Chobot, P.; Nowakowska, M.; Polanska, J. Seeking the factors predisposing to local skin inflammatory state development in children with type 1 diabetes (T1DM) treated with continuous subcutaneous insulin infusion (CSII). Exp. Clin. Endocrinol. Diabetes 2007, 115, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.Y.; Lo, F.S.; Wang, J.P.; Yeh, L.K.; Wu, A.L.; Tseng, Y.J.; Yeh, C.T.; Liu, L.; Chen, K.J.; Wu, W.C.; et al. Nomogram for prediction of non-proliferative diabetic retinopathy in juvenile-onset type 1 diabetes: A cohort study in an Asian population. Sci. Rep. 2018, 8, 12164. [Google Scholar] [CrossRef]
- Wang, N.K.; Lai, C.C.; Wang, J.P.; Wu, W.C.; Liu, L.; Yeh, L.K.; Tseng, H.J.; Chang, C.J.; Lo, F.S.; Chang Gung Juvenile Diabetes Eye Study, G. Risk factors associated with the development of retinopathy 10 yr after the diagnosis of juvenile-onset type 1 diabetes in Taiwan: A cohort study from the CGJDES. Pediatr. Diabetes 2016, 17, 407–416. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute. M100 Performance Standards for Antimicrobial Susceptibility Testing, 31th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2021. [Google Scholar]
- Kang, Y.C.; Tai, W.C.; Yu, C.C.; Kang, J.H.; Huang, Y.C. Methicillin-resistant Staphylococcus aureus nasal carriage among patients receiving hemodialysis in Taiwan: Prevalence rate, molecular characterization and de-colonization. BMC Infect. Dis. 2012, 12, 284. [Google Scholar] [CrossRef]
- Enright, M.C.; Day, N.P.; Davies, C.E.; Peacock, S.J.; Spratt, B.G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 2000, 38, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, D.C.; de Lencastre, H. Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2002, 46, 2155–2161. [Google Scholar] [CrossRef]
- Strommenger, B.; Braulke, C.; Heuck, D.; Schmidt, C.; Pasemann, B.; Nübel, U.; Witte, W. Spa Typing of Staphylococcus aureus as a frontline tool in epidemiological typing. J. Clin. Microbiol. 2008, 46, 574–581. [Google Scholar] [CrossRef]
- Huang, Y.C.; Ho, C.F.; Chen, C.J.; Su, L.H.; Lin, T.Y. Comparative molecular analysis of community-associated and healthcare-associated methicillin-resistant Staphylococcus aureus isolates from children in northern Taiwan. Clin. Microbiol. Infect. 2008, 14, 1167–1172. [Google Scholar] [CrossRef]
- Huang, Y.C.; Hwang, K.P.; Chen, P.Y.; Chen, C.J.; Lin, T.Y. Prevalence of methicillin-resistant Staphylococcus aureus nasal colonization among Taiwanese children in 2005 and 2006. J. Clin. Microbiol. 2007, 45, 3992–3995. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wu, C.J.; Ko, W.C.; Ho, M.W.; Lin, H.H.; Yang, Y.L.; Lin, J.N.; Huang, I.W.; Wang, H.Y.; Lai, J.F.; Shiau, Y.R.; et al. Prevalence of and risk factors for methicillin-resistant Staphylococcus aureus colonization among human immunodeficient virus-infected outpatients in Taiwan: Oral Candida colonization as a comparator. J. Oral Microbiol. 2017, 9, 1322446. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.T.; Liao, C.H.; Fang, C.T.; Chie, W.C.; Lai, M.S.; Lauderdale, T.L.; Lee, W.S.; Huang, J.H.; Chang, S.C. Prevalence of and risk factors for colonization by methicillin-resistant Staphylococcus aureus among adults in community settings in Taiwan. J. Clin. Microbiol. 2009, 47, 2957–2963. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.Y.; Chang, F.Y.; Cheng, C.C.; Lee, K.D.; Huang, Y.C. Methicillin-resistant Staphylococcus aureus nasal colonization among adult patients visiting emergency department in a medical center in Taiwan. PLoS ONE 2011, 6, e18620. [Google Scholar] [CrossRef]
- Lin, S.Y.; Lin, N.Y.; Huang, Y.Y.; Hsieh, C.C.; Huang, Y.C. Methicillin-resistant Staphylococcus aureus nasal carriage and infection among patients with diabetic foot ulcer. J. Microbiol. Immunol. Infect. 2020, 53, 292–299. [Google Scholar] [CrossRef]
- Tsai, M.S.; Chen, C.J.; Lin, T.Y.; Huang, Y.C. Nasal methicillin-resistant Staphylococcus aureus colonization among otherwise healthy children aged between 2 months and 5 years in northern Taiwan, 2005–2010. J. Microbiol. Immunol. Infect. 2018, 51, 756–762. [Google Scholar] [CrossRef]
- Chen, C.J.; Hsu, K.H.; Lin, T.Y.; Hwang, K.P.; Chen, P.Y.; Huang, Y.C. Factors associated with nasal colonization of methicillin-resistant Staphylococcus aureus among healthy children in Taiwan. J. Clin. Microbiol. 2011, 49, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Gesualdo, F.; Bongiorno, D.; Rizzo, C.; Bella, A.; Menichella, D.; Stefani, S.; Tozzi, A.E. MRSA nasal colonization in children: Prevalence meta-analysis, review of risk factors and molecular genetics. Pediatr. Infect. Dis. J. 2013, 32, 479–485. [Google Scholar] [CrossRef]
- Lin, J.; Peng, Y.; Xu, P.; Zhang, T.; Bai, C.; Lin, D.; Ou, Q.; Yao, Z. Methicillin-Resistant Staphylococcus aureus Nasal Colonization in Chinese Children: A Prevalence Meta-Analysis and Review of Influencing Factors. PLoS ONE 2016, 11, e0159728. [Google Scholar] [CrossRef] [PubMed]
- Karadag-Oncel, E.; Gonc, N.; Altay, O.; Cengiz, A.B.; Ozon, A.; Pinar, A.; Ceyhan, M.; Alikasifoglu, A.; Akyon, Y.; Kandemir, N.; et al. Prevalence of nasal carriage of methicillin-resistant Staphylococcus aureus in children with diabetes mellitus: Trends between 2005 and 2013. Am. J. Infect. Control. 2015, 43, 1015–1017. [Google Scholar] [CrossRef] [PubMed]
- Genc, O.; Arikan, I. The relationship between hand hygiene practices and nasal Staphylococcus aureus carriage in healthcare workers. Med. Lav. 2020, 111, 54–62. [Google Scholar] [CrossRef]
- Kilic, A.; Mert, G.; Senses, Z.; Bedir, O.; Aydogan, H.; Basustaoglu, A.C.; Appelbaum, P.C. Molecular characterization of methicillin-resistant Staphylococcus aureus nasal isolates from Turkey. Antonie van Leeuwenhoek 2008, 94, 615–619. [Google Scholar] [CrossRef] [PubMed]
- Pino, S.C.; Kruger, A.J.; Bortell, R. The role of innate immune pathways in type 1 diabetes pathogenesis. Curr. Opin. Endocrinol. Diabetes Obes. 2010, 17, 126–130. [Google Scholar] [CrossRef]
- Brown, A.F.; Leech, J.M.; Rogers, T.R.; McLoughlin, R.M. Staphylococcus aureus Colonization: Modulation of Host Immune Response and Impact on Human Vaccine Design. Front. Immunol. 2014, 4, 507. [Google Scholar] [CrossRef]
- David, M.Z.; Daum, R.S. Community-associated methicillin-resistant Staphylococcus aureus: Epidemiology and clinical consequences of an emerging epidemic. Clin. Microbiol. Rev. 2010, 23, 616–687. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Huang, K.A.; Huang, Y.C.; Chi, H.; Lu, C.Y.; Chang, L.Y.; Ho, Y.H.; Chi, C.Y.; Liu, C.C.; Huang, L.M.; et al. Prevalence and molecular characterizations of Staphylococcus aureus nasal colonization among patients in pediatric intensive care units in Taiwan. Antimicrob. Resist. Infect. Control. 2020, 9, 41. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.Y.; Huang, Y.C. Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Asia. Lancet Infect. Dis. 2013, 13, 698–708. [Google Scholar] [CrossRef]
- Feng, Y.; Chen, H.L.; Chen, C.J.; Chen, C.L.; Chiu, C.H. Genome comparisons of two Taiwanese community-associated methicillin-resistant Staphylococcus aureus ST59 clones support the multi-origin theory of CA-MRSA. Infect. Genet. Evol. 2017, 54, 60–65. [Google Scholar] [CrossRef]
- Wang, H.K.; Huang, C.Y.; Huang, Y.C. Clinical features and molecular characteristics of childhood community-associated methicillin-resistant Staphylococcus aureus infection in a medical center in northern Taiwan, 2012. BMC Infect. Dis. 2017, 17, 470. [Google Scholar] [CrossRef]
- Chen, K.H.; Chuang, W.C.; Wong, W.K.; Chuang, C.H.; Chen, C.J.; Huang, Y.C. Nasal Methicillin-Resistant Staphylococcus aureus Carriage Among Foreign Workers Recruited to Taiwan from Southeastern Asian Countries. Open Forum Infect. Dis. 2021, 8, ofaa586. [Google Scholar] [CrossRef]
- Lee, Y.T.; Lin, D.B.; Wang, W.Y.; Tsao, S.M.; Yu, S.F.; Wei, M.J.; Yang, S.F.; Lu, M.C.; Chiou, H.L.; Chen, S.C.; et al. First identification of methicillin-resistant Staphylococcus aureus MLST types ST5 and ST45 and SCCmec types IV and Vt by multiplex PCR during an outbreak in a respiratory care ward in central Taiwan. Diagn.. Microbiol. Infect. Dis. 2011, 70, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.J.; Siu, L.K.; Lin, J.C.; Wang, C.H.; Lu, P.L. Molecular typing and characterization of nasal carriage and community-onset infection methicillin-susceptible Staphylococcus aureus isolates in two Taiwan medical centers. BMC Infect. Dis. 2012, 12, 343. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Chen, C.J.; Lauderdale, T.Y. Detection, spread and phylogeny of meticillin-resistant Staphylococcus aureus sequence type 45 in Taiwan. Microb. Genom. 2021, 7. [Google Scholar] [CrossRef]
- Ajao, A.O.; Harris, A.D.; Johnson, J.K.; Roghmann, M.C.; Perencevich, E.N.; Schweizer, M.L.; Zhan, M.; Chen, W.H.; Furuno, J.P. Association between methicillin-resistant Staphylococcus aureus colonization and infection may not differ by age group. Infect. Control. Hosp. Epidemiol. 2013, 34, 93–95. [Google Scholar] [CrossRef]
- Woods, S.; Beiter, E.; Drake, B.; Engel, A. The prevalence of asymptomatic methicillin-resistant Staphylococcus aureus in school-age children. East. J. Med. 2011, 16, 18–20. [Google Scholar]
- Balder, J.W.; Lansberg, P.J.; Hof, M.H.; Wiegman, A.; Hutten, B.A.; Kuivenhoven, J.A. Pediatric lipid reference values in the general population: The Dutch lifelines cohort study. J. Clin. Lipidol. 2018, 12, 1208–1216. [Google Scholar] [CrossRef]
- Delekta, P.C.; Shook, J.C.; Lydic, T.A.; Mulks, M.H.; Hammer, N.D. Staphylococcus aureus Utilizes Host-Derived Lipoprotein Particles as Sources of Fatty Acids. J. Bacteriol. 2018, 200. [Google Scholar] [CrossRef]
- Surewaard, B.G.; Nijland, R.; Spaan, A.N.; Kruijtzer, J.A.; de Haas, C.J.; van Strijp, J.A. Inactivation of staphylococcal phenol soluble modulins by serum lipoprotein particles. PLoS Pathog. 2012, 8, e1002606. [Google Scholar] [CrossRef]
- Bhakdi, S.; Tranum-Jensen, J.; Utermann, G.; Füssle, R. Binding and partial inactivation of Staphylococcus aureus alpha-toxin by human plasma low density lipoprotein. J. Biol. Chem. 1983, 258, 5899–5904. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.M.; Mack, J.L.; Hall, P.R.; Alsup, A.A.; Alexander, S.M.; Sully, E.K.; Sawires, Y.S.; Cheung, A.L.; Otto, M.; Gresham, H.D. Apolipoprotein B Is an innate barrier against invasive Staphylococcus aureus infection. Cell Host Microbe 2008, 4, 555–566. [Google Scholar] [CrossRef]
- Chen, C.H.; Kuo, K.C.; Hwang, K.P.; Lin, T.Y.; Huang, Y.C. Risk factors for and molecular characteristics of methicillin-resistant Staphylococcus aureus nasal colonization among healthy children in southern Taiwan, 2005–2010. J. Microbiol. Immunol. Infect. 2019, 52, 929–936. [Google Scholar] [CrossRef] [PubMed]
| Variates | Non-MRSA (n = 232) | MRSA (n = 13) | Total (n = 245) | p Value * |
|---|---|---|---|---|
| Male (no.) (%) | 112 (48.3) | 4 (30.8) | 116 (47.3) | 0.219 |
| Age (year) (mean ± SD) | 22.9 ± 6.5 | 14.4 ± 8.4 | 22.4 ± 6.8 | <0.001 |
| Age ≤ 10 years (%) | 13 (5.6) | 6 (46.2) | 19 (7.8) | 0.001 |
| Age > 10 years (%) | 219 (94.4) | 7 (53.8) | 226 (92.2) | |
| Diabetes duration (year) (mean ± SD) | 14.8 ± 6.0 | 8.4 ± 6.6 | 14.4 ± 6.2 | <0.001 |
| HbA1c (%) (mean ± SD) | 8.6 ± 2.0 | 8.4 ± 1.3 | 8.6 ± 2.0 | 0.714 |
| Body weight (kg) (mean ± SD) | 59.6 ± 14.1 | 42.5 ± 16.0 | 58.8 ± 14.6 | <0.001 |
| Height (cm) (mean ± SD) | 161.5 ± 12.7 | 141.7 ± 18.6 | 160.4 ± 13.7 | 0.002 |
| Body mass index (kg/m2) (mean ± SD) | 22.9 ± 0.3 | 19.6 ± 1.1 | 22.8 ± 5.6 | 0.037 |
| Hypertension (no.) (%) | 38 (16.4) | 1 (7.7) | 39 (15.9) | 0.699 |
| Serum creatinine (mg/dL) (mean ± SD) | 0.64 ± 0.16 | 0.45 ± 0.12 | 0.63 ± 0.16 | <0.001 |
| Serum HDL-C (mg/dL) (mean ± SD) | 62.6 ± 15.5 | 70.5 ± 16.6 | 63.0 ± 15.6 | 0.073 |
| Serum LDL-C (mg/dL) (mean ± SD) | 111.0 ± 34.1 | 95.5 ± 29.6 | 110.2 ± 34.0 | 0.110 |
| Serum total cholesterol (mg/dL) (mean ± SD) | 187.0 ± 42.0 | 181.2 ± 33.8 | 186.7 ± 41.6 | 0.625 |
| Serum triglyceride (mg/dL) (mean ± SD) | 81.4 ± 61.4 | 63.5 ± 41.3 | 80.5 ± 60.6 | 0.301 |
| ID | CC | E | FA | LZD | P | SXT | TEC | VA | CIP | D |
|---|---|---|---|---|---|---|---|---|---|---|
| 01 | S | S | S | S | R | S | S | S | S | S |
| 02 | S | S | S | S | R | S | S | S | S | S |
| 03 | S | R | S | S | R | S | S | S | S | S |
| 04 | S | S | S | S | R | S | S | S | S | S |
| 05 | S | R | S | S | R | S | S | S | S | S |
| 06 | S | S | S | S | R | S | S | S | S | S |
| 07 | S | S | S | S | R | S | S | S | S | S |
| 08 | S | R | S | S | R | S | S | S | S | S |
| 09 | S | R | S | S | R | S | S | S | S | S |
| 10 | S | R | S | S | R | S | S | S | R | S |
| 11 | R | R | S | S | R | S | S | S | S | S |
| 12 | S | S | S | S | R | S | S | S | S | S |
| 13 | S | S | S | S | R | S | S | S | S | S |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p Value | Odds Ratio | 95% CI | p Value | |
| Male | 0.48 | 0.14–1.59 | 0.23 | |||
| Age | ||||||
| ≤10 years | 14.44 | 4.24–49.18 | <0.001 | 7.40 | 0.69–79.47 | 0.099 |
| >10 years | 0.07 | 0.02–0.24 | <0.001 | |||
| Body mass index | ||||||
| <18 kg/m2 | 7.10 | 2.21–22.79 | 0.001 | 0.63 | 0.06–6.36 | 0.698 |
| 19–24 kg/m2 | 0.43 | 0.14–1.37 | 0.153 | |||
| >24 kg/m2 | 0.44 | 0.10–2.03 | 0.292 | |||
| Diabetes duration | ||||||
| <10 years | 8.86 | 2.61–30.01 | <0.001 | 3.92 | 0.81–18.87 | 0.089 |
| ≥10 years | 0.12 | 0.03–0.39 | 0.001 | |||
| HbA1c | ||||||
| <7.0% | 0.74 | 0.16–3.43 | 0.696 | |||
| 7.0%–10.0% | 2.11 | 0.57–7.89 | 0.266 | |||
| >10% | 0.36 | 0.05–2.81 | 0.327 | |||
| Hypertension | 0.43 | 0.05–3.37 | 0.418 | |||
| Elevated LDL-C 1 | 0.27 | 0.08–0.89 | 0.032 | 0.29 | 0.08–1.10 | 0.068 |
| Elevated total cholesterol 2 | 0.93 | 0.30–2.94 | 0.907 | |||
| Elevated triglyceride 3 | 0.84 | 0.10–6.76 | 0.868 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, C.-Y.; Kang, E.Y.-C.; Lai, C.-C.; Lo, W.-C.; Chen, K.-J.; Wu, W.-C.; Liu, L.; Hwang, Y.-S.; Lo, F.-S.; Huang, Y.-C. Nasal Methicillin-Resistant Staphylococcus aureus Colonization in Patients with Type 1 Diabetes in Taiwan. Microorganisms 2021, 9, 1296. https://doi.org/10.3390/microorganisms9061296
Kang C-Y, Kang EY-C, Lai C-C, Lo W-C, Chen K-J, Wu W-C, Liu L, Hwang Y-S, Lo F-S, Huang Y-C. Nasal Methicillin-Resistant Staphylococcus aureus Colonization in Patients with Type 1 Diabetes in Taiwan. Microorganisms. 2021; 9(6):1296. https://doi.org/10.3390/microorganisms9061296
Chicago/Turabian StyleKang, Chun-Ya, Eugene Yu-Chuan Kang, Chi-Chun Lai, Wei-Che Lo, Kun-Jen Chen, Wei-Chi Wu, Laura Liu, Yih-Shiou Hwang, Fu-Sung Lo, and Yhu-Chering Huang. 2021. "Nasal Methicillin-Resistant Staphylococcus aureus Colonization in Patients with Type 1 Diabetes in Taiwan" Microorganisms 9, no. 6: 1296. https://doi.org/10.3390/microorganisms9061296
APA StyleKang, C.-Y., Kang, E. Y.-C., Lai, C.-C., Lo, W.-C., Chen, K.-J., Wu, W.-C., Liu, L., Hwang, Y.-S., Lo, F.-S., & Huang, Y.-C. (2021). Nasal Methicillin-Resistant Staphylococcus aureus Colonization in Patients with Type 1 Diabetes in Taiwan. Microorganisms, 9(6), 1296. https://doi.org/10.3390/microorganisms9061296








