Knockdown of Gonadotropin-Releasing Hormone II Receptor Impairs Ovulation Rate, Corpus Luteum Development, and Progesterone Production in Gilts
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Growth, Pubertal Development, and Cyclicity
2.3. Blood Collection
2.4. Tissue Collection
2.5. Digital Droplet PCR
2.6. Histological Analysis
2.7. Mass Spectrometry
2.8. Statistical Analysis
3. Results
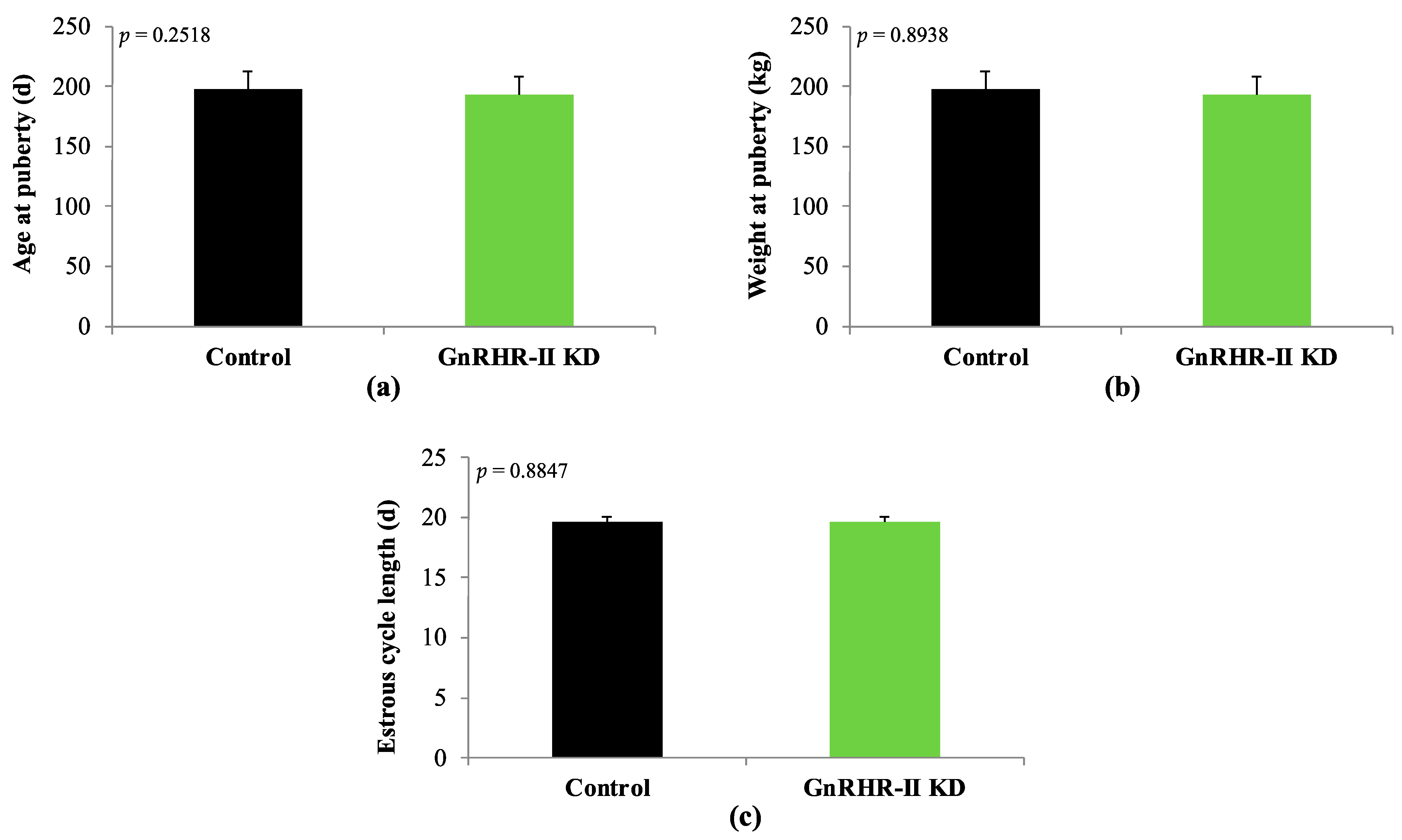
3.1. Growth, Pubertal Development, and Estrous Cyclicity
3.2. Corticosteroids in Circulation
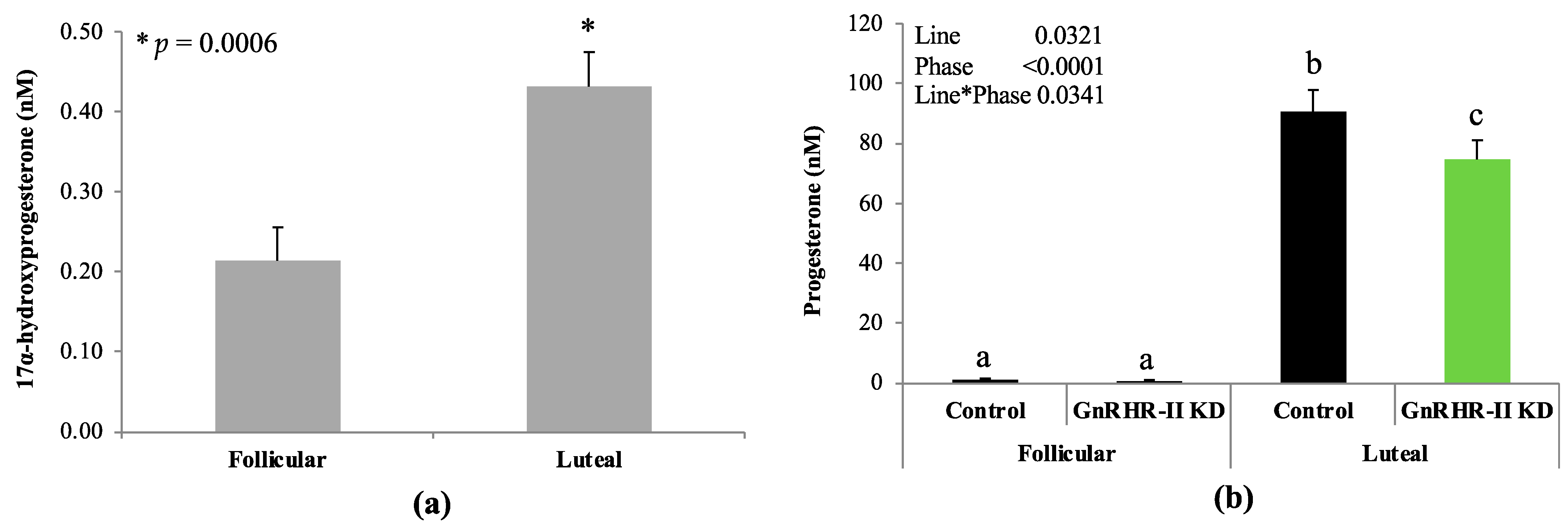
3.3. Progestogens in Circulation
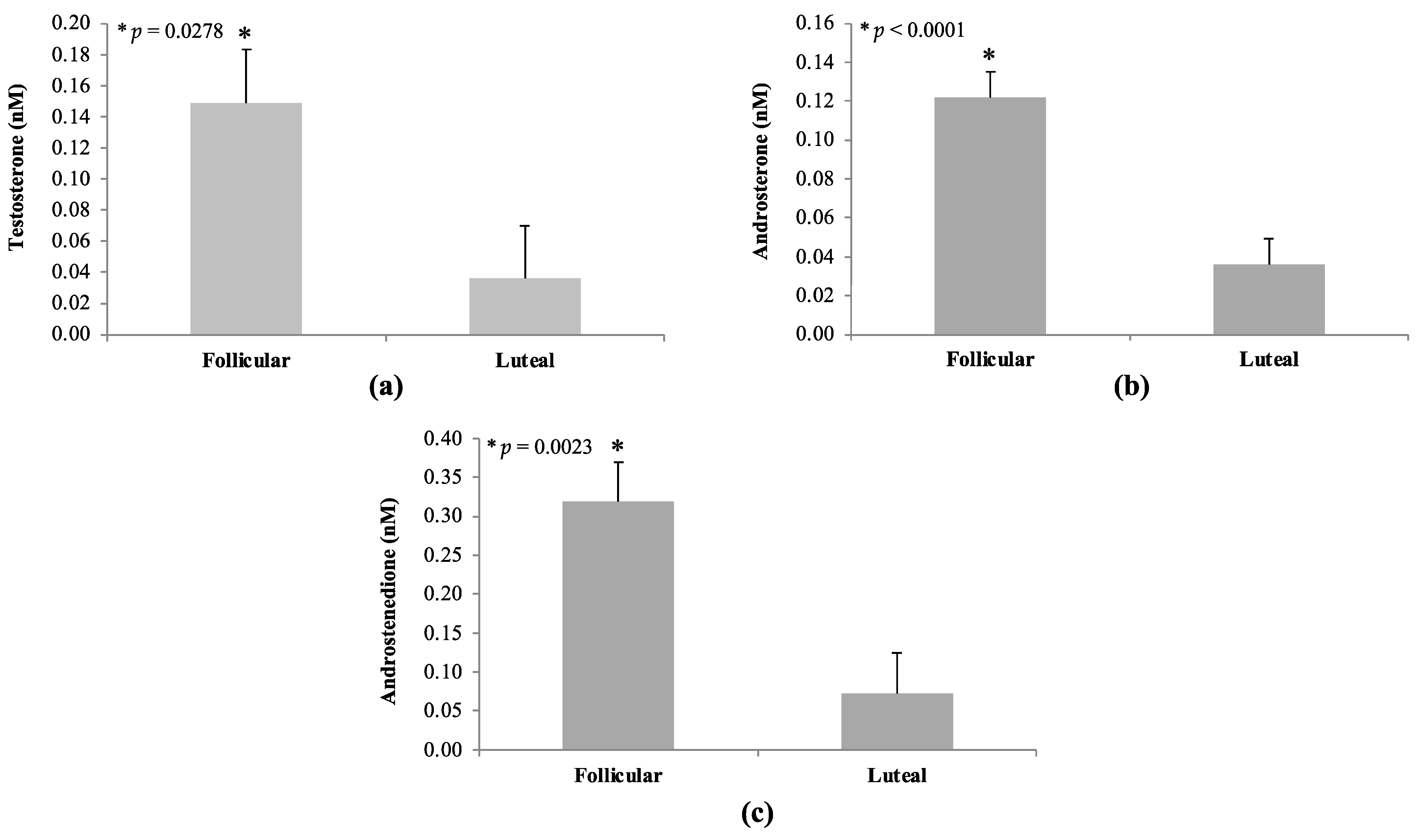
3.4. Androgens in Circulation
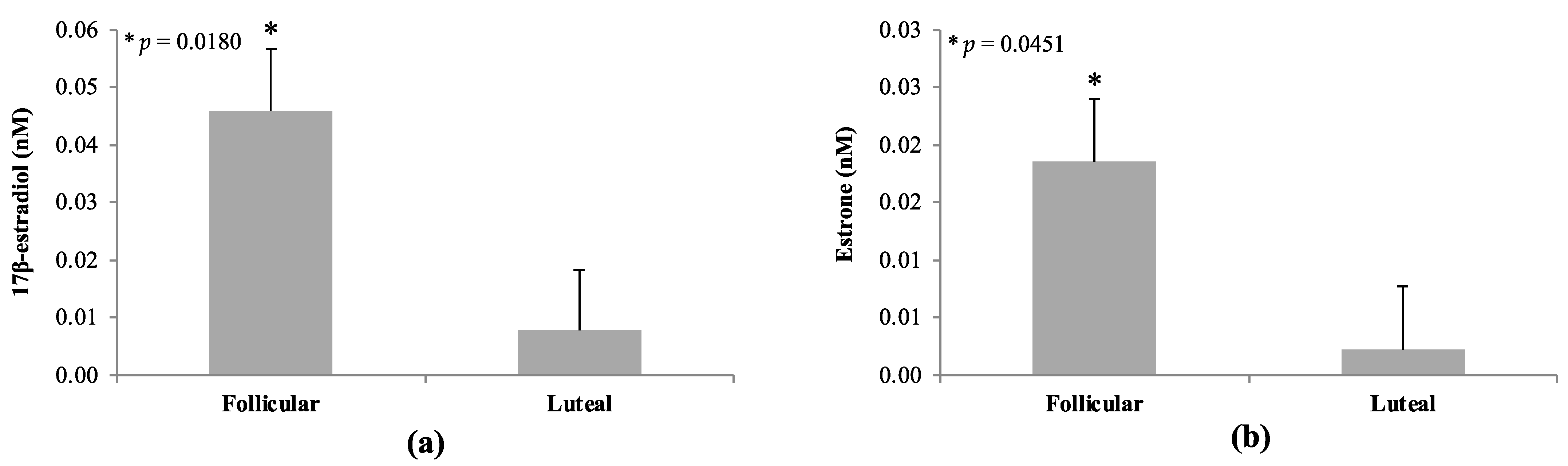
3.5. Estrogens in Circulation
3.6. Corpus luteum Metrics and GnRHR-II Quantification
3.7. Steroids within the Corpus luteum
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lopes, T.P.; Sanchez-Osorio, J.; Bolarin, A.; Martinez, E.A.; Roca, J. Relevance of ovarian follicular development to the seasonal impairment of fertility in weaned sows. Vet. J. 2014, 199, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Schally, A.V.; Arimura, A.; Baba, Y.; Nair, R.M.; Matsuo, H.; Redding, T.W.; Debeljuk, L. Isolation and properties of the FSH and LH-releasing hormone. Biochem. Biophys. Res. Commun. 1971, 43, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, H.; Baba, Y.; Nair, R.M.; Arimura, A.; Schally, A.V. Structure of the porcine LH- and FSH-releasing hormone. I. The proposed amino acid sequence. Biochem. Biophys. Res. Commun. 1971, 43, 1334–1339. [Google Scholar] [CrossRef] [PubMed]
- Baba, Y.; Matsuo, H.; Schally, A.V. Structure of the porcine LH- and FSH-releasing hormone. II. Confirmation of the proposed structure by conventional sequential analyses. Biochem. Biophys. Res. Commun. 1971, 44, 459–463. [Google Scholar] [CrossRef] [PubMed]
- White, R.B.; Eisen, J.A.; Kasten, T.L.; Fernald, R.D. Second gene for gonadotropin-releasing hormone in humans. Proc. Natl. Acad. Sci. USA 1998, 95, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Fernald, R.D.; White, R.B. Gonadotropin-releasing hormone genes: Phylogeny, structure, and functions. Front. Neuroendocrinol. 1999, 20, 224–240. [Google Scholar] [CrossRef] [PubMed]
- Desaulniers, A.T.; Cederberg, R.A.; Lents, C.A.; White, B.R. Expression and role of gonadotropin-releasing hormone 2 and its receptor in mammals. Front. Endocrinol. 2017, 8, 269. [Google Scholar] [CrossRef] [PubMed]
- Stewart, A.J.; Katz, A.A.; Millar, R.P.; Morgan, K. Retention and silencing of prepro-GnRH-II and type II GnRH receptor genes in mammals. Neuroendocrinology 2009, 90, 416–432. [Google Scholar] [CrossRef]
- Neill, J.D. GnRH and GnRH receptor genes in the human genome. Endocrinology 2002, 143, 737–743. [Google Scholar] [CrossRef]
- Desaulniers, A.T.; Cederberg, R.A.; Mills, G.A.; Ford, J.J.; Lents, C.A.; White, B.R. LH-independent testosterone secretion is mediated by the interaction between GnRH2 and its receptor within porcine testes. Biol. Reprod. 2015, 93, 45. [Google Scholar] [CrossRef] [PubMed]
- Millar, R.; Lowe, S.; Conklin, D.; Pawson, A.; Maudsley, S.; Troskie, B.; Ott, T.; Millar, M.; Lincoln, G.; Sellar, R.; et al. A novel mammalian receptor for the evolutionarily conserved type II GnRH. Proc. Natl. Acad. Sci. USA 2001, 98, 9636–9641. [Google Scholar] [CrossRef] [PubMed]
- Rissman, E.F.; Alones, V.E.; Craig-Veit, C.B.; Millam, J.R. Distribution of chicken-II gonadotropin-releasing hormone in mammalian brain. J. Comp. Neurol. 1995, 357, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Millar, R.P.; Milton, R.C.; Follett, B.K.; King, J.A. Receptor binding and gonadotropin-releasing activity of a novel chicken gonadotropin-releasing hormone ([His5, Trp7, Tyr8]GnRH) and a D-Arg6 analog. Endocrinology 1986, 119, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Okada, Y.; Murota-Kawano, A.; Kakar, S.S.; Winters, S.J. Evidence that gonadotropin-releasing hormone (GnRH) II stimulates luteinizing hormone and follicle-stimulating hormone secretion from monkey pituitary cultures by activating the GnRH I receptor. Biol. Reprod. 2003, 69, 1356–1361. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, K.; Hasegawa, Y.; Nomura, M.; Igarashi, M.; Kangawa, K.; Matsuo, H. Identification of the second gonadotropin-releasing hormone in chicken hypothalamus: Evidence that gonadotropin secretion is probably controlled by two distinct gonadotropin-releasing hormones in avian species. Proc. Natl. Acad. Sci. USA 1984, 81, 3874–3878. [Google Scholar] [CrossRef] [PubMed]
- Balik, A.; Jindrichova, M.; Bhattacharyya, S.; Zemkova, H. GnRH-I and GnRH-II-induced calcium signaling and hormone secretion in neonatal rat gonadotrophs. Physiol. Res. 2009, 58, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Millar, R.P. GnRH II and type II GnRH receptors. Trends Endocrinol. Metab. 2003, 14, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Neill, J.D.; Duck, L.W.; Sellers, J.C.; Musgrove, L.C. A gonadotropin-releasing hormone (GnRH) receptor specific for GnRH II in primates. Biochem. Biophys. Res. Commun. 2001, 282, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Morgan, K.; Conklin, D.; Pawson, A.J.; Sellar, R.; Ott, T.R.; Millar, R.P. A transcriptionally active human type II gonadotropin-releasing hormone receptor gene homolog overlaps two genes in the antisense orientation on chromosome 1q.12. Endocrinology 2003, 144, 423–436. [Google Scholar] [CrossRef] [PubMed]
- Neill, J.D.; Duck, L.W.; Musgrove, L.C. GnRH II receptor is encoded in genomes of human, monkey, and pig but not mouse. In Abstracts of the 84th Annual Meeting of the Endocrine Society; The Endocrine Society: San Francisco, CA, USA, 2002; p. 74.9. [Google Scholar]
- Gault, P.M.; Morgan, K.; Pawson, A.J.; Millar, R.P.; Lincoln, G.A. Sheep exhibit novel variations in the organization of the mammalian type II gonadotropin-releasing hormone receptor gene. Endocrinology 2004, 145, 2362–2374. [Google Scholar] [CrossRef] [PubMed]
- Pawson, A.J.; Morgan, K.; Maudsley, S.R.; Millar, R.P. Type II gonadotrophin-releasing hormone (GnRH-II) in reproductive biology. Reproduction 2003, 126, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Desaulniers, A.T.; Cederberg, R.A.; Mills, G.A.; Lents, C.A.; White, B.R. Production of a gonadotropin-releasing hormone 2 receptor knockdown (GNRHR2 KD) swine line. Transgenic Res. 2017, 26, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Lents, C.A.; Thorson, J.F.; Desaulniers, A.T.; White, B.R. RFamide-related peptide 3 and gonadotropin-releasing hormone-II are autocrine-paracrine regulators of testicular function in the boar. Mol. Reprod. Dev. 2017, 84, 994–1003. [Google Scholar] [CrossRef] [PubMed]
- White, B.R.; Cederberg, R.A.; Elsken, D.H.; Ross, C.E.; Lents, C.A.; Desaulniers, A.T. Role of gonadotropin-releasing hormone-II and its receptor in swine reproduction. Mol. Reprod. Dev. 2023, 90, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Millar, R.P.; Rissman, E.F. An evolutionarily conserved form of gonadotropin-releasing hormone coordinates energy and reproductive behavior. Endocrinology 2003, 144, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.S.; Rissman, E.F. A critical role for the evolutionarily conserved gonadotropin-releasing hormone II: Mediation of energy status and female sexual behavior. Endocrinology 2004, 145, 3639–3646. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.S. Emerging functions of gonadotropin-releasing hormone II in mammalian physiology and behaviour. J. Neuroendocrinol. 2004, 16, 794–806. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.S.; Wills, A.; Millar, R.P.; Rissman, E.F. Evidence that the type-2 gonadotrophin-releasing hormone (GnRH) receptor mediates the behavioural effects of GnRH-II on feeding and reproduction in musk shrews. J. Neuroendocrinol. 2005, 17, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.S.; Bojkowska, K.; Wills, A.; Rissman, E.F. Gonadotropin-releasing hormone-II messenger ribonucleic acid and protein content in the mammalian brain are modulated by food intake. Endocrinology 2006, 147, 5069–5077. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.S.; Rissman, E.F. The evolutionarily conserved gonadotropin-releasing hormone II modifies food intake. Endocrinology 2004, 145, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Siler-Khodr, T.M.; Grayson, M. Action of chicken II GnRH on the human placenta. J. Clin. Endocrinol. Metab. 2001, 86, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.S.; Beristain, A.G.; MacCalman, C.D.; Leung, P.C. Cellular localization of gonadotropin-releasing hormone (GnRH) I and GnRH II in first-trimester human placenta and decidua. J. Clin. Endocrinol. Metab. 2004, 89, 1459–1466. [Google Scholar] [CrossRef] [PubMed]
- Islami, D.; Bischof, P.; Chardonnens, D. Possible interactions between leptin, gonadotrophin-releasing hormone (GnRH-I and II) and human chorionic gonadotrophin (hCG). Eur. J. Obstet. Gynecol. Reprod. Biol. 2003, 110, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Islami, D.; Chardonnens, D.; Campana, A.; Bischof, P. Comparison of the effects of GnRH-I and GnRH-II on HCG synthesis and secretion by first trimester trophoblast. Mol. Hum. Reprod. 2001, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Cheon, K.W.; Lee, H.S.; Parhar, I.S.; Kang, I.S. Expression of the second isoform of gonadotrophin-releasing hormone (GnRH-II) in human endometrium throughout the menstrual cycle. Mol. Hum. Reprod. 2001, 7, 447–452. [Google Scholar] [CrossRef]
- Eicke, N.; Gunthert, A.R.; Viereck, V.; Siebold, D.; Behe, M.; Becker, T.; Emons, G.; Grundker, C. GnRH-II receptor-like antigenicity in human placenta and in cancers of the human reproductive organs. Eur. J. Endocrinol. 2005, 153, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Siler-Khodr, T.M.; Yu, F.Q.; Wei, P.; Tao, S.X.; Liu, Y.X. Contraceptive action of a gonadotropin-releasing hormone II analog in the rhesus monkey. J. Clin. Endocrinol. Metab. 2004, 89, 4513–4520. [Google Scholar] [CrossRef] [PubMed]
- Emons, G.; Grundker, C.; Gunthert, A.R.; Westphalen, S.; Kavanagh, J.; Verschraegen, C. GnRH antagonists in the treatment of gynecological and breast cancers. Endocr. Relat. Cancer 2003, 10, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Fister, S.; Gunthert, A.R.; Aicher, B.; Paulini, K.W.; Emons, G.; Grundker, C. GnRH-II antagonists induce apoptosis in human endometrial, ovarian, and breast cancer cells via activation of stress-induced MAPKs P38 and JNK and proapoptotic protein Bax. Cancer Res. 2009, 69, 6473–6481. [Google Scholar] [CrossRef]
- Eidne, K.A.; Flanagan, C.A.; Millar, R.P. Gonadotropin-releasing hormone binding sites in human breast carcinoma. Science 1985, 229, 989–991. [Google Scholar] [CrossRef]
- Grundker, C.; Fost, C.; Fister, S.; Nolte, N.; Gunthert, A.R.; Emons, G. Gonadotropin-releasing hormone type II antagonist induces apoptosis in MCF-7 and triple-negative MDA-MB-231 human breast cancer cells in vitro and in vivo. Breast Cancer Res. 2010, 12, R49. [Google Scholar] [CrossRef] [PubMed]
- Fister, S.; Schlotawa, L.; Gunthert, A.R.; Emons, G.; Grundker, C. Increase of doxorubicin-induced apoptosis after knock-down of gonadotropin-releasing hormone receptor expression in human endometrial, ovarian and breast cancer Cells. Gynecol. Endocrinol. 2008, 24, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.K.; Tai, C.J.; Nathwani, P.S.; Leung, P.C. Differential regulation of two forms of gonadotropin-releasing hormone messenger ribonucleic acid in human granulosa-luteal cells. Endocrinology 2001, 142, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Siler-Khodr, T.M.; Yu, F.Q.; Wei, P.; Tao, S.X.; Coulhart, S.; Mactyszczyk, S.; Lui, Y.X. Dose-related actions of GnRH II analog in the cycling rhesus monkey. Contraception 2006, 74, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Siler-Khodr, T.M.; Grayson, M.; Eddy, C.A. Action of gonadotropin-releasing hormone II on the baboon ovary. Biol. Reprod. 2003, 68, 1150–1156. [Google Scholar] [CrossRef] [PubMed]
- Desaulniers, A.T.; Cederberg, R.A.; Carreiro, E.P.; Gurumurthy, C.B.; White, B.R. A transgenic pig model expressing a CMV-ZsGreen1 reporter across an extensive array of tissues. J. Biomed. Res. 2020, 35, 163–173. [Google Scholar] [CrossRef] [PubMed]
- National Research Council (NRC). Nutrient Requirements of Swine, 11th ed.; National Academies Press: Washington, DC, USA, 2012; pp. 208–238. [Google Scholar] [CrossRef]
- American Veterinary Medical Association. AVMA Guidelines for the Euthanasia of Animals: 2020 Ed.; American Veterinary Medicine Association: Schaumburg, IL, USA, 2020; pp. 72–76. [Google Scholar]
- Cavzos, L.F.; Anderson, L.L.; Belt, W.D.; Henricks, D.M.; Kraeling, R.R.; Melampy, R.M. Fine Structure and Progesterone Levels in the Corpus Luteum of the Pig during the Estrous Cycle. Biol. Reprod. 1969, 1, 83–106. [Google Scholar] [CrossRef] [PubMed]
- Hindson, C.M.; Chevillet, J.R.; Briggs, H.A.; Gallichotte, E.N.; Ruf, I.K.; Hindson, B.J.; Vessella, R.L.; Tewari, M. Absolute quantification by droplet digital PCR versus analog real-time PCR. Nat. Methods 2013, 10, 1003–1005. [Google Scholar] [CrossRef] [PubMed]
- Koal, T.; Schmiederer, D.; Pham-Tuan, H.; Rohring, C.; Rauh, M. Standardized LC-MS/MS based steroid hormone profile-analysis. J. Steroid Biochem. Mol. Biol. 2012, 129, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Abedal-Majed, M.A.; Springman, S.A.; Sutton, C.M.; Snider, A.P.; Bell, B.E.; Hart, M.; Kurz, S.G.; Bergman, J.; Summers, A.F.; McFee, R.M.; et al. VEGFA165 can rescue excess steroid secretion, inflammatory markers and follicle arrest in the ovarian cortex of high A4 cows. Biol. Reprod. 2022, 106, 118–131. [Google Scholar] [CrossRef] [PubMed]
- Summers, A.F.; Pohlmeier, W.E.; Sargent, K.M.; Cole, B.D.; Vinton, R.J.; Kurz, S.G.; McFee, R.M.; Cushman, R.A.; Cupp, A.S.; Wood, J.R. Altered theca and cumulus oocyte complex gene expression, follicular arrest and reduced fertility in cows with dominant follicle follicular fluid androgen excess. PLoS ONE 2014, 9, e110683. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, Z.E.; Studer, J.M.; Chipman, A.L.; Adur, M.K.; Mainquist-Whigham, C.; Gabler, N.K.; Keating, A.F.; Ross, J.W. Circulating biomarkers associated with pelvic organ prolapse risk in late gestation sows. J. Anim. Sci. 2021, 99, skab207. [Google Scholar] [CrossRef] [PubMed]
- Meyer, A.E.; Pfeiffer, C.A.; Brooks, K.E.; Spate, L.D.; Benne, J.A.; Cecil, R.; Samuel, M.S.; Murphy, C.N.; Behura, S.; McLean, M.K.; et al. New perspective on conceptus estrogens in maternal recognition and pregnancy establishment in the pig. Biol. Reprod. 2019, 101, 148–161. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, S.; Leung, P.C. Differential regulation of gonadotropin-releasing hormone (GnRH)I and GnRHII messenger ribonucleic acid by gonadal steroids in human granulosa luteal cells. J. Clin. Endocrinol. Metab. 2003, 88, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Foxcroft, G.R.; Hunter, M.G. Basic physiology of follicular maturation in the pig. J. Reprod. Fertil. Suppl. 1985, 33, 1–19. [Google Scholar] [PubMed]
- Choi, J.H.; Gilks, C.B.; Auersperg, N.; Leung, P.C. Immunolocalization of gonadotropin-releasing hormone (GnRH)-I, GnRH-II, and type I GnRH receptor during follicular development in the human ovary. J. Clin. Endocrinol. Metab. 2006, 91, 4562–4570. [Google Scholar] [CrossRef] [PubMed]
- Knox, R.V. Recent advancements in the hormonal stimulation of ovulation in swine. Vet. Med. 2015, 6, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Abedel-Majed, M.A.; Romereim, S.M.; Davis, J.S.; Cupp, A.S. Perturbations in lineage specification of granulosa and theca cells may alter corpus luteum formation and function. Front. Endocrinol. 2019, 10, 832. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Tang, T.; Li, W.; Liu, Z.; Yang, X.; Shi, X.; Sun, G.; Liu, X.; Wang, M.; Liang, X.; et al. Bone morphogenetic protein 15 knockdown inhibits porcine ovarian follicular development and ovulation. Front. Cell. Dev. Biol. 2019, 7, 286. [Google Scholar] [CrossRef] [PubMed]





| Hormone (nM) # | Follicular | Luteal | SEM | p-Value |
|---|---|---|---|---|
| 11-deoxycortisol | 1.3 | 0.2 | 0.5 | 0.0320 |
| Corticosterone | 3.4 | 1.4 | 0.7 | 0.0103 |
| Cortisol | 56.2 | 28.9 | 9.1 | 0.0084 |
| Cortisone | 16.2 | 9.1 | 2.7 | 0.0081 |
| Hormone (fmol/mg Tissue) # | Control | GnRHR-II KD | SEM | p-Value |
|---|---|---|---|---|
| 11-Deoxycorticosterone | 15.6 | 13.4 | 1.9 | 0.4569 |
| 11-Deoxycortisol | 2.8 | 2.4 | 0.8 | 0.7100 |
| Corticosterone | 3.4 | 2.9 | 1.4 | 0.7991 |
| Cortisol | 6.6 | 6.7 | 2.3 | 0.9789 |
| Cortisone | 88.8 | 70.4 | 26.9 | 0.6452 |
| Hormone (fmol/mg Tissue) # | Control | GnRHR-II KD | SEM | p-Value |
|---|---|---|---|---|
| 17α-Hydroxyprogesterone | 169.1 | 79.4 | 48.9 | 0.2425 |
| Progesterone | 166,838 | 128,849 | 13,355 | 0.0910 |
| Dehydroepiandrosterone sulfate | 19.9 | 23.7 | 7.5 | 0.7328 |
| Androstenedione | 69.4 | 38.2 | 19.9 | 0.3104 |
| Testosterone | 3.6 | 3.3 | 1.3 | 0.8751 |
| Androsterone | 1.0 | 1.1 | 0.3 | 0.7165 |
| Estrone | 1.8 | 0.9 | 0.3 | 0.0914 |
| 17β-estradiol | 0.9 | 1.1 | 0.3 | 0.7630 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Desaulniers, A.T.; Cederberg, R.A.; Lents, C.A.; White, B.R. Knockdown of Gonadotropin-Releasing Hormone II Receptor Impairs Ovulation Rate, Corpus Luteum Development, and Progesterone Production in Gilts. Animals 2024, 14, 2350. https://doi.org/10.3390/ani14162350
Desaulniers AT, Cederberg RA, Lents CA, White BR. Knockdown of Gonadotropin-Releasing Hormone II Receptor Impairs Ovulation Rate, Corpus Luteum Development, and Progesterone Production in Gilts. Animals. 2024; 14(16):2350. https://doi.org/10.3390/ani14162350
Chicago/Turabian StyleDesaulniers, Amy T., Rebecca A. Cederberg, Clay A. Lents, and Brett R. White. 2024. "Knockdown of Gonadotropin-Releasing Hormone II Receptor Impairs Ovulation Rate, Corpus Luteum Development, and Progesterone Production in Gilts" Animals 14, no. 16: 2350. https://doi.org/10.3390/ani14162350





