Machine Learning-Based Predictive Model of Aortic Valve Replacement Modality Selection in Severe Aortic Stenosis Patients
Abstract
:1. Introduction
2. Materials and Methods
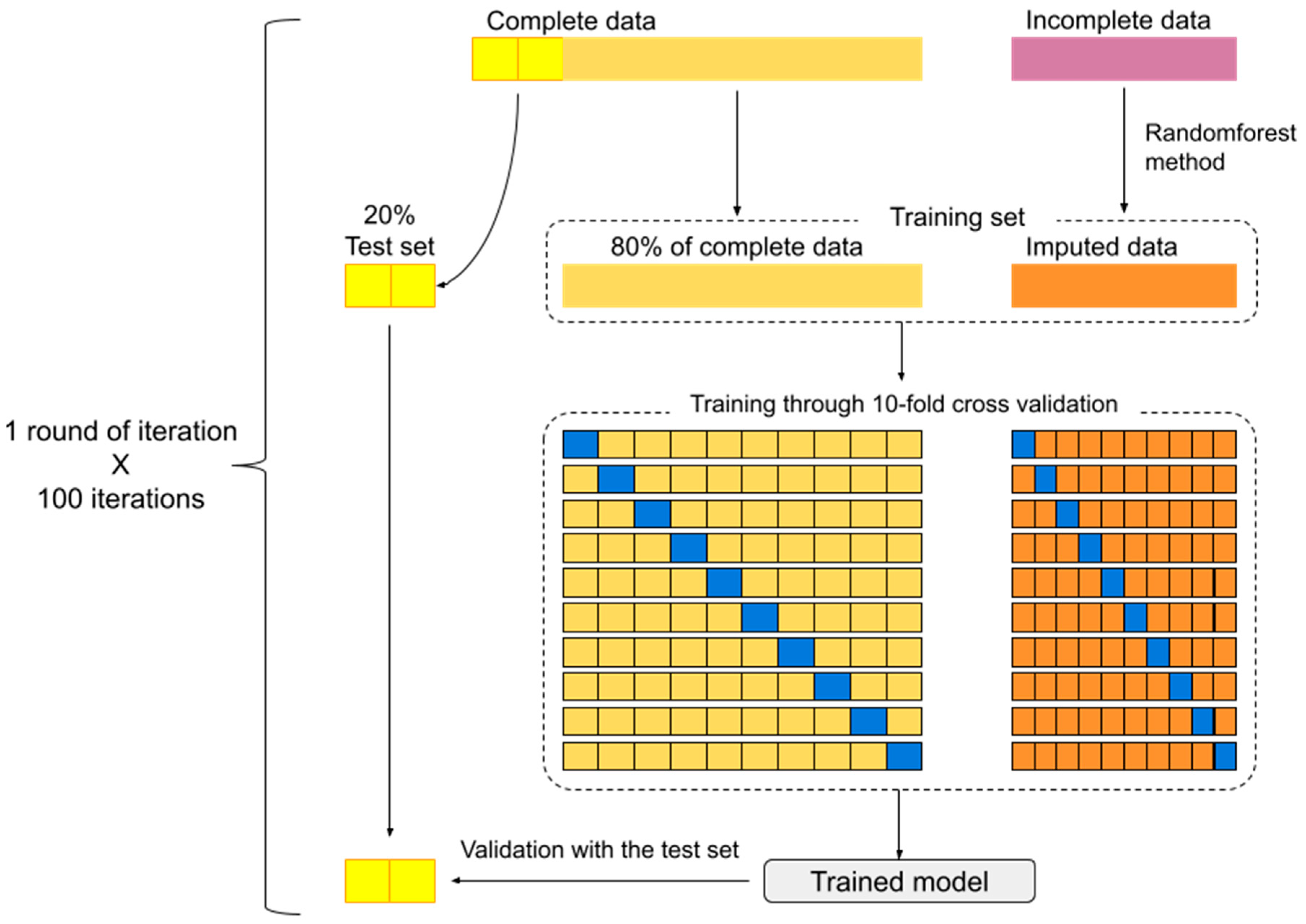
2.1. Treatment of Missing Data
2.2. Model Selection and Creation
2.3. Outcomes
3. Results
3.1. Study Population
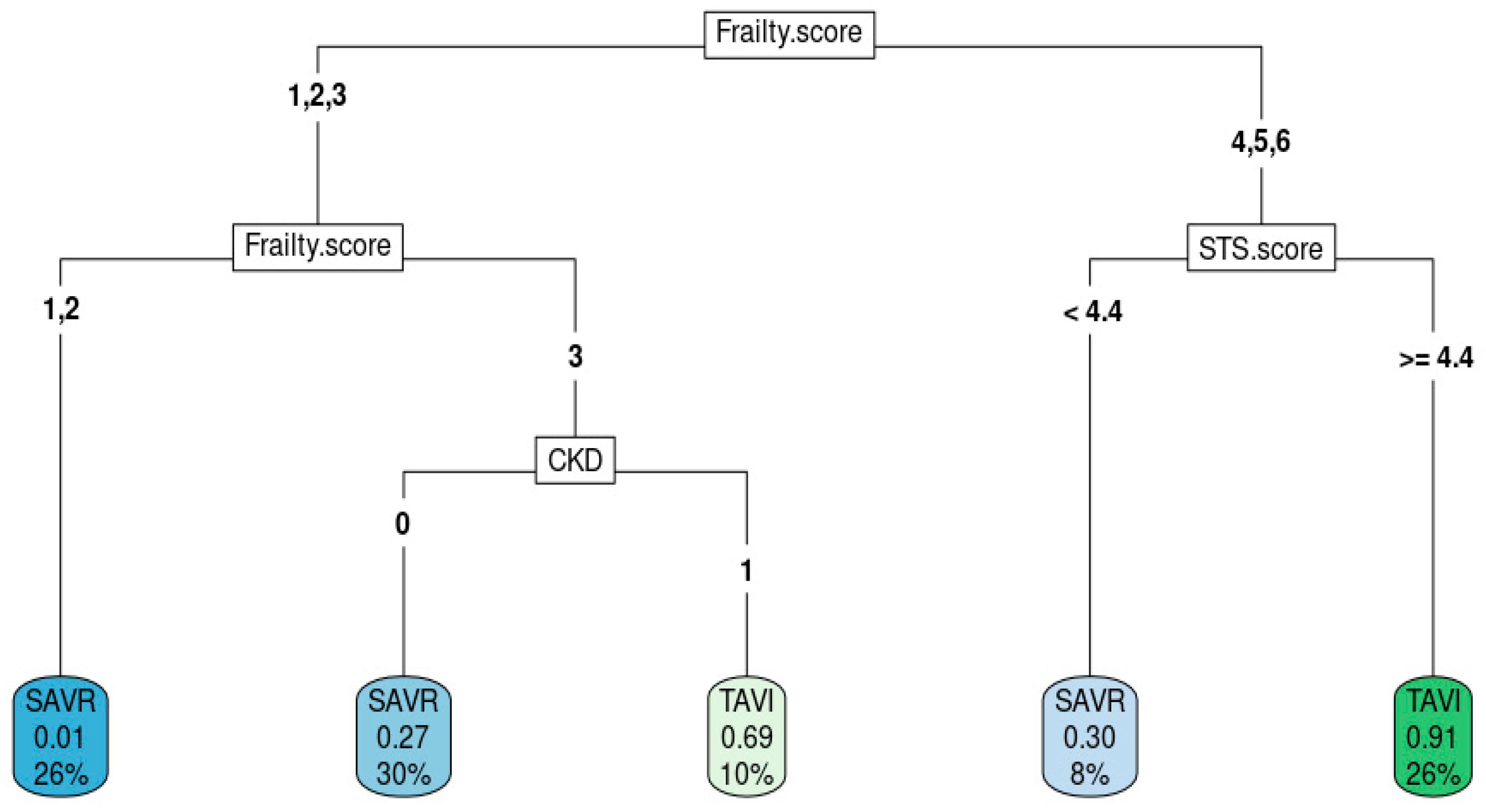
3.2. Model Derivation
Model Validation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coffey, S.; Roberts-Thomson, R.; Brown, A.; Carapetis, J.; Chen, M.; Enriquez-Sarano, M.; Zuhlke, L.; Prendergast, B.D. Global epidemiology of valvular heart disease. Nat. Rev. Cardiol. 2021, 18, 853–864. [Google Scholar] [CrossRef] [PubMed]
- Siemieniuk, R.A.; Agoritsas, T.; Manja, V.; Devji, T.; Chang, Y.; Bala, M.M.; Thabane, L.; Guyatt, G.H. Transcatheter versus surgical aortic valve replacement in patients with severe aortic stenosis at low and intermediate risk: Systematic review and meta-analysis. BMJ 2016, 354, i5130. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., 3rd; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, e72–e227. [Google Scholar] [PubMed]
- Siontis, G.C.M.; Overtchouk, P.; Cahill, T.J.; Modine, T.; Prendergast, B.; Praz, F.; Pilgrim, T.; Petrinic, T.; Nikolakopoulou, A.; Salanti, G.; et al. Transcatheter aortic valve implantation vs. surgical aortic valve replacement for treatment of symptomatic severe aortic stenosis: An updated meta-analysis. Eur. Heart J. 2019, 40, 3143–3153. [Google Scholar] [CrossRef] [PubMed]
- Prasitlumkum, N.; Kewcharoen, J.; Kanitsoraphan, C.; Rattanawong, P.; Mekritthikrai, R.; Gillaspie, E.A.; Mao, M.A.; Cheungpasitporn, W. Previous coronary artery bypass graft is not associated with higher mortality in transcatheter aortic valve replacement: Systemic review and meta-analysis. Acta Cardiol. 2020, 75, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Tarantini, G.; Nai Fovino, L.; D’Errigo, P.; Rosato, S.; Barbanti, M.; Tamburino, C.; Ranucci, M.; Santoro, G.; Badoni, G.; Seccareccia, F.; et al. Factors influencing the choice between transcatheter and surgical treatment of severe aortic stenosis in patients younger than 80 years: Results from the OBSERVANT study. Catheter. Cardiovasc. Interv. 2020, 95, E186–E195. [Google Scholar] [CrossRef] [PubMed]
- Shameer, K.; Johnson, K.W.; Glicksberg, B.S.; Dudley, J.T.; Sengupta, P.P. Machine learning in cardiovascular medicine: Are we there yet? Heart 2018, 104, 1156–1164. [Google Scholar] [CrossRef] [PubMed]
- Krittanawong, C.; Johnson, K.W.; Rosenson, R.S.; Wang, Z.; Aydar, M.; Baber, U.; Min, J.K.; Tang, W.H.W.; Halperin, J.L.; Narayan, S.M. Deep learning for cardiovascular medicine: A practical primer. Eur. Heart J. 2019, 40, 2058–2073. [Google Scholar] [CrossRef] [PubMed]
- Attia, Z.I.; Friedman, P.A. Explainable AI for ECG-based prediction of cardiac resynchronization therapy outcomes: Learning from machine learning? Eur. Heart J. 2023, 44, 693–695. [Google Scholar] [CrossRef] [PubMed]
- Quer, G.; Arnaout, R.; Henne, M.; Arnaout, R. Machine Learning and the Future of Cardiovascular Care: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 77, 300–313. [Google Scholar] [CrossRef] [PubMed]
- Lertsanguansinchai, P.; Chokesuwattanaskul, R.; Petchlorlian, A.; Suttirut, P.; Buddhari, W.; Chula, T.T. Machine learning-based predictive risk models for 30-day and 1-year mortality in severe aortic stenosis patients undergoing transcatheter aortic valve implantation. Int. J. Cardiol. 2023, 374, 20–26. [Google Scholar] [CrossRef]
- Rockwood, K.; Theou, O. Using the Clinical Frailty Scale in Allocating Scarce Health Care Resources. Can. Geriatr. J. 2020, 23, 210–215. [Google Scholar] [CrossRef]
- Lee, G.; Chikwe, J.; Milojevic, M.; Wijeysundera, H.C.; Biondi-Zoccai, G.; Flather, M.; Gaudino, M.F.L.; Fremes, S.E.; Tam, D.Y. ESC/EACTS vs. ACC/AHA guidelines for the management of severe aortic stenosis. Eur. Heart J. 2023, 44, 796–812. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Niu, G.; Chen, Y.; Zhou, Z.; Feng, D.; Zhang, Y.; Wu, Y. Development and validation of a deep learning-based fully automated algorithm for pre-TAVR CT assessment of the aortic valvular complex and detection of anatomical risk factors: A retrospective, multicentre study. eBioMedicine 2023, 96, 104794. [Google Scholar] [CrossRef] [PubMed]
- Lachmann, M.; Rippen, E.; Schuster, T.; Xhepa, E.; von Scheidt, M.; Trenkwalder, T.; Pellegrini, C.; Rheude, T.; Hesse, A.; Stundl, A.; et al. Artificial intelligence-enabled phenotyping of patients with severe aortic stenosis: On the recovery of extra-aortic valve cardiac damage after transcatheter aortic valve replacement. Open Heart 2022, 9, e002068. [Google Scholar] [CrossRef] [PubMed]
- Maier, O.; Afzal, S.; Piayda, K.; Zeus, T.; Veulemans, V. Patient-Specific Computer Simulation in TAVR: Is Artificial Intelligence Superior to Human Experience in Interventional Cardiology? JACC Cardiovasc. Interv. 2020, 13, 2580–2581. [Google Scholar] [CrossRef] [PubMed]
- Hon, J.K.F.; Tay, E. Transcatheter aortic valve implantation in Asia. Ann. Cardiothorac. Surg. 2017, 6, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Sawa, Y.; Takayama, M.; Mitsudo, K.; Nanto, S.; Takanashi, S.; Komiya, T.; Kuratani, T.; Tobaru, T.; Goto, T. Clinical efficacy of transcatheter aortic valve replacement for severe aortic stenosis in high-risk patients: The PREVAIL JAPAN trial. Surg. Today 2015, 45, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, R.A.; O’Gara, P.T.; Bavaria, J.E.; Brindis, R.G.; Carroll, J.D.; Kavinsky, C.J.; Lindman, B.R.; Linderbaum, J.A.; Little, S.H.; Mack, M.J.; et al. 2019 AATS/ACC/ASE/SCAI/STS Expert Consensus Systems of Care Document: A Proposal to Optimize Care for Patients With Valvular Heart Disease: A Joint Report of the American Association for Thoracic Surgery, American College of Cardiology, American Society of Echocardiography, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 2019, 73, 2609–2635. [Google Scholar] [PubMed]
| Overall | SAVR | TAVI | p | |
|---|---|---|---|---|
| n | 415 | 238 | 177 | |
| Age (mean (SD)) | 78.41 (7.41) | 75.41 (6.50) | 82.44 (6.63) | <0.001 |
| Gender (%) | 220 (53.0) | 121 (50.8) | 99 (55.9) | 0.353 |
| STS.score (mean (SD)) | 5.63 (4.27) | 3.97 (1.73) | 7.89 (5.49) | <0.001 |
| Frailty.score (mean (SD)) | 3.26 (1.06) | 2.71 (0.78) | 4.01 (0.93) | <0.001 |
| Frailty score > 4 = TRUE (%) | 150 (36.1) | 31 (13.0) | 119 (67.2) | <0.001 |
| NYHA (%) | <0.001 | |||
| 0 | 2 (0.5) | 0 (0.0) | 2 (1.1) | |
| 1 | 4 (1.0) | 4 (1.7) | 0 (0.0) | |
| 2 | 196 (47.2) | 134 (56.3) | 62 (35.0) | |
| 3 | 192 (46.3) | 94 (39.5) | 98 (55.4) | |
| 4 | 20 (4.8) | 6 (2.5) | 14 (7.9) | |
| CAD (%) | 113 (27.2) | 55 (23.1) | 58 (32.8) | 0.038 |
| AF AFL (%) | 57 (13.7) | 19 (8.0) | 38 (21.5) | <0.001 |
| CKD (%) | 141 (34.0) | 27 (11.3) | 114 (64.4) | <0.001 |
| HF (%) | 234 (56.4) | 91 (38.2) | 143 (80.8) | <0.001 |
| COPD (%) | 33 (8.0) | 10 (4.2) | 23 (13.0) | 0.002 |
| Smoke (%) | 19 (4.6) | 7 (2.9) | 12 (6.8) | 0.107 |
| HT (%) | 339 (81.7) | 191 (80.3) | 148 (83.6) | 0.455 |
| DM (%) | 144 (34.7) | 73 (30.7) | 71 (40.1) | 0.058 |
| DLP (%) | 297 (71.6) | 162 (68.1) | 135 (76.3) | 0.085 |
| LVEF (mean (SD)) | 62.52 (15.83) | 63.18 (15.53) | 61.67 (16.23) | 0.343 |
| TVD (%) | 89 (21.4) | 45 (18.9) | 44 (24.9) | 0.168 |
| Calcify.Ao (%) | 22 (5.3) | 1 (0.4) | 21 (11.9) | <0.001 |
| CABG (%) | 38 (9.2) | 2 (0.8) | 36 (20.3) | <0.001 |
| RVSP (mean (SD)) | 22.22 (21.62) | 18.57 (21.35) | 26.83 (21.14) | <0.001 |
| mPAP (mean (SD)) | 1.52 (6.40) | 0.82 (4.73) | 2.19 (7.63) | 0.057 |
| MS…Mod (%) | 7 (1.7) | 1 (0.4) | 6 (3.4) | 0.007 |
| MR…Mod (%) | 35 (8.4) | 12 (5.0) | 23 (13.0) | 0.003 |
| MR…Severe (%) | 4 (1.0) | 1 (0.4) | 3 (1.7) | 0.05 |
| Best Model | Median | 1st Quartile | 3rd Quartile | Frequency | |
|---|---|---|---|---|---|
| Precision | 98.6% | 92.1% | 89.5% | 93.4% | - |
| Age | −0.0703 | −0.0903 | −0.1286 | −0.0697 | 100 |
| STS.score | −0.2019 | −0.2688 | −0.3731 | −0.1797 | 100 |
| Frailty.score2 | 1.7302 | 2.2415 | 1.9649 | 2.6769 | 100 |
| Frailty.score4 [MU4] | −0.5575 | −0.9194 | −1.2795 | −0.6159 | 100 |
| CKD1 | −1.0407 | −1.7186 | −2.124 | −1.481 | 100 |
| Best Model | Median | 1st Quartile | 3rd Quartile | Frequency | |
|---|---|---|---|---|---|
| Precision | 93% | 86% | 83% | 88% | - |
| Age | 0.08 | 0.09 | 0.08 | 0.11 | 100 |
| CKD | 0.11 | 0.15 | 0.13 | 0.32 | 100 |
| Frailty score | 0.39 | 0.29 | 0.2 | 0.33 | 100 |
| STS.score | 0.23 | 0.2 | 0.18 | 0.22 | 100 |
| CABG | 0.03 | 0.04 | 0.02 | 0.05 | 86 |
| NYHA | 0.02 | 0.01 | 0 | 0.01 | 82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chokesuwattanaskul, R.; Petchlorlian, A.; Lertsanguansinchai, P.; Suttirut, P.; Prasitlumkum, N.; Srimahachota, S.; Buddhari, W. Machine Learning-Based Predictive Model of Aortic Valve Replacement Modality Selection in Severe Aortic Stenosis Patients. Med. Sci. 2024, 12, 3. https://doi.org/10.3390/medsci12010003
Chokesuwattanaskul R, Petchlorlian A, Lertsanguansinchai P, Suttirut P, Prasitlumkum N, Srimahachota S, Buddhari W. Machine Learning-Based Predictive Model of Aortic Valve Replacement Modality Selection in Severe Aortic Stenosis Patients. Medical Sciences. 2024; 12(1):3. https://doi.org/10.3390/medsci12010003
Chicago/Turabian StyleChokesuwattanaskul, Ronpichai, Aisawan Petchlorlian, Piyoros Lertsanguansinchai, Paramaporn Suttirut, Narut Prasitlumkum, Suphot Srimahachota, and Wacin Buddhari. 2024. "Machine Learning-Based Predictive Model of Aortic Valve Replacement Modality Selection in Severe Aortic Stenosis Patients" Medical Sciences 12, no. 1: 3. https://doi.org/10.3390/medsci12010003
APA StyleChokesuwattanaskul, R., Petchlorlian, A., Lertsanguansinchai, P., Suttirut, P., Prasitlumkum, N., Srimahachota, S., & Buddhari, W. (2024). Machine Learning-Based Predictive Model of Aortic Valve Replacement Modality Selection in Severe Aortic Stenosis Patients. Medical Sciences, 12(1), 3. https://doi.org/10.3390/medsci12010003






