Needle Transportable Semi-Automatic Hair Follicle Implanter and Image-Based Hair Density Estimation for Advanced Hair Transplantation Surgery
Abstract
:1. Introduction
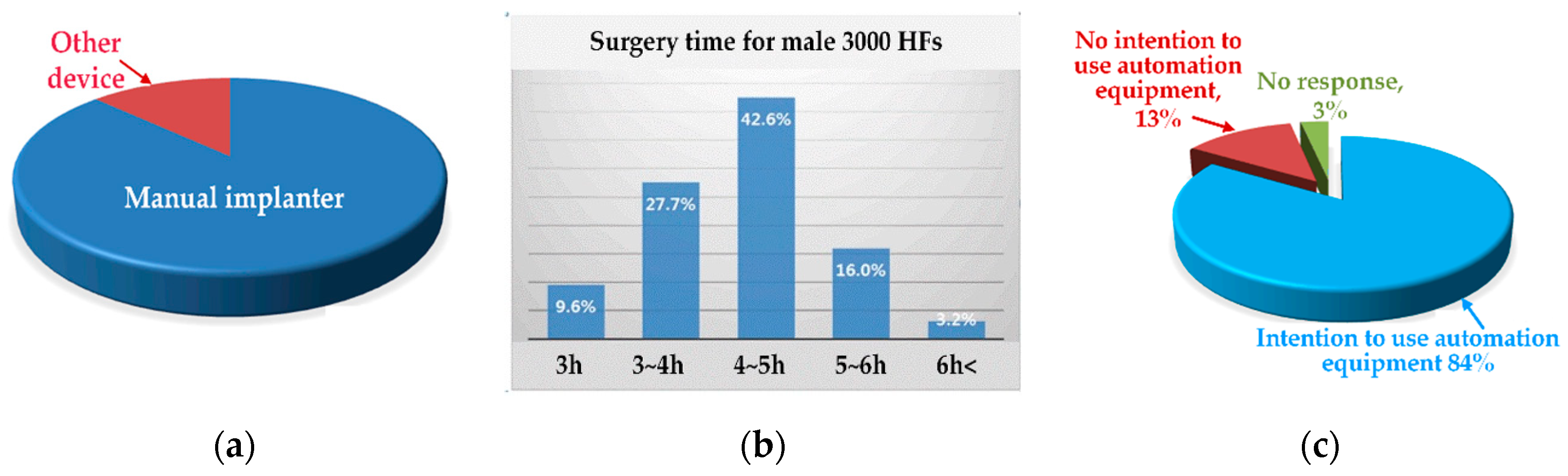
2. Background and Motivation
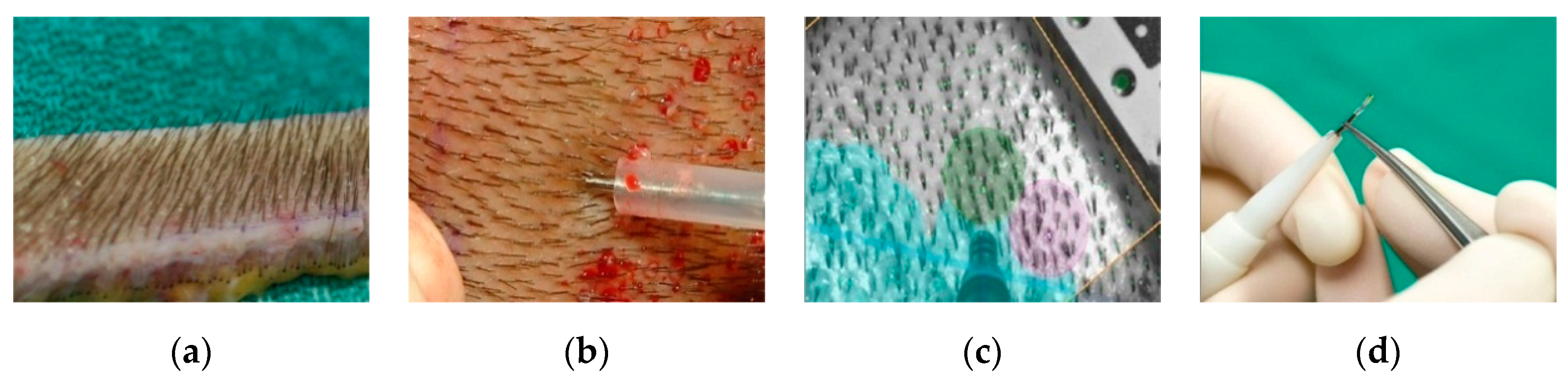
2.1. Current Hair Transplant Procedure
2.2. Operation Principle of the Manual Implanter
3. Materials and Methods
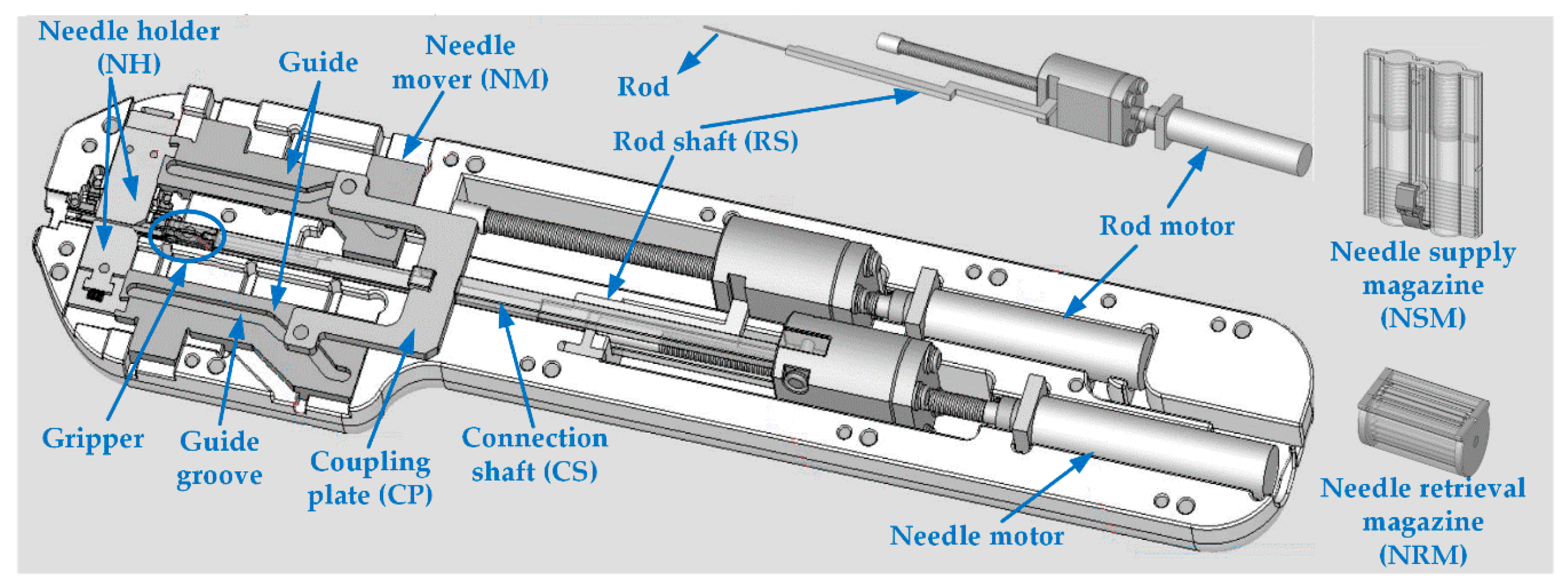
3.1. Structure of the Proposed Semi-Automatic Implementation
3.2. Operation Flowchart of Continuous Needle Supply
3.3. Grip and Release of Needles by Gripper
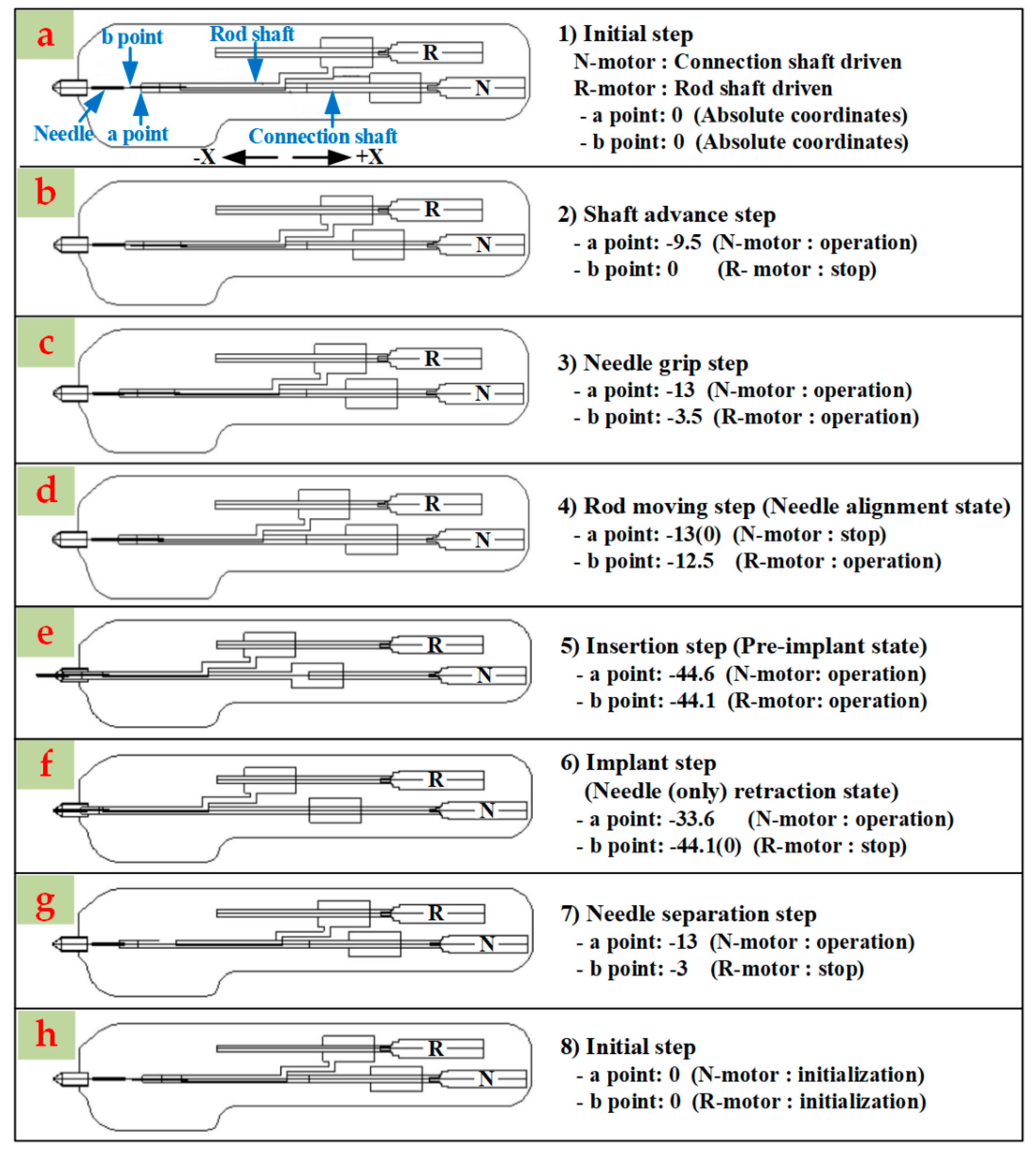
3.4. Automation of the Transplantation Procedure
3.5. Guide Structure for Needle Transfer
3.6. Driving Environment
- Initially, the driving motor is homed by the motor control EPOS2 program.
- The transplant speed is adjusted by the setting of the number of rotations, rotation speed, and acceleration and/or deceleration of the needle motor and the rod motor.
- The range of the rotation speed of the driving motor (DCX10L) is 0–32,256 rpm; the rotation speed for each transplant stroke can be changed according to the surgeon’ s preference.
- Both motors operate at 1350 rpm by default. However, in the case of the rod motor, the rotation speed is 1350 rpm or more in two strokes: the insertion of the rod into the needle when moving forward (the fourth stroke) and the rapid release of the rod out of the needle when moving backward (the sixth stroke).
- The motor-related setting values are entered in the order of movement of the needle and rod described in Section 3.4, but they can be adjusted within the confidence error.
3.7. Item Approval of the Medical Device
- Performance testing of the semi-automatic implanter by the KCTL
- Performance testing of the needle used in the semi-automatic implanter by the Korea Testing Laboratory [30]
- Biological stability (dermal reaction) test of the needle by Korea Conformity Laboratories [31] and
- Needle asepsis (sterilization validation) and needle validation test by Greenpiatech incorp [32].
3.8. Image Processing for the Estimation of Hair Root and Hair Density
4. Results
4.1. Animal Experiment
4.2. Clinical Experiment
4.2.1. Preparation
4.2.2. Institutional Review Board (IRB) and Subject Recruitment
4.2.3. Experiment Method
4.2.4. Evaluation of the HF Engraftment Rate
4.2.5. Evaluation of VSA and Adverse Events
4.3. Detection Results of Hair Root
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Okuda, S. The study of clinical experiments of hair transplantation. Jpn. J. Dermatol. Urol. 1939, 46, 135–138. [Google Scholar]
- Unger, W.P. Delineating the safe donor area for hair transplanting. Am. J. Cosmet. Surg. 1994, 11, 239–243. [Google Scholar] [CrossRef]
- Unger, W.P.; Shapiro, R.; Unger, R.; Unger, M. Hair Transplantation, 5th ed.; CRC Press: Florida, FL, USA, 2011; pp. 247–251. [Google Scholar]
- Lee, I.J.; Jung, J.H.; Lee, Y.R.; Kim, J.C.; Hwang, S.T. Guidelines on hair restoration for east asian patients. Dermatol. Surg. 2016, 42, 883–892. [Google Scholar] [CrossRef]
- ISHRS 2015 Data: Hair Transplants Up 76% from 2006. Available online: https://www.plasticsurgerypractice.com/client-objectives/rejuvenation/hair-transplant/ishrs-2015-data-hair-transplants-76-2006 (accessed on 23 October 2019).
- Orentreich, N. Autografts in alopecias and other selected dermatological conditions. Ann. N. Y. Acad. Sci. 1959, 83, 463–479. [Google Scholar] [CrossRef] [PubMed]
- Robert, M.; Bernstein, M.D.; William, R.; Rassman, M.D. Follicular unit transplantation. Dermatol. Clin. 2005, 23, 393–414. [Google Scholar]
- Lam, S.M.; Williams, K.L. Hair Transplant 360: Follicular Unit Extraction (FUE), 1st ed.; Jaypee Brothers Medical Pub: London, UK, 2016; pp. 453–464. [Google Scholar]
- Rassman, W.R.; Bernstein, R.M.; McClellan, R.; Jones, R.; Worton, E.; Uyttendaele, H. Follicular unit extraction: Minimally invasive surgery for hair transplantation. Dermatol. Surg. 2002, 28, 720–727. [Google Scholar] [CrossRef] [PubMed]
- Dua, A.; Dua, K. Follicular unit extraction hair transplant. J. Cutan. Aesthet. Surg. 2010, 3, 76–81. [Google Scholar] [PubMed]
- Rassman, W.R.; Carson, S. Micrografting in extensive quantities: The ideal hair restoration procedure. Dermatol. Surg. 1995, 21, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Rashid, R.M.; Morgan, B.L.T. Follicular unit extraction hair transplant automation: Options in overcoming challenges of the latest technology in hair restoration with the goal of avoiding the line scar. Dermatol. Online J. 2012, 18, 12. [Google Scholar] [PubMed]
- Onda, M.; Igawa, H.H.; Inoue, K.; Tanino, R. Novel technique of follicular unit extraction hair transplantation with a powered punching device. Dermatol. Surg. 2008, 34, 1683–1688. [Google Scholar]
- FUE Hair Transplant Procedure. Available online: http://www.bosley.com/solutions/follicular_unit_extraction.php (accessed on 23 October 2019).
- Qureshi, S.A.; Bodduluri, M. System and Method for Classifying Follicular Units. U.S. Patent US7477782B2, 13 January 2009. Available online: http://www.google.tl/patents/US7477782 (accessed on 23 October 2019).
- Qureshi, S.A.; Bodduluri, M. System and Method for Classifying Follicular Units. U.S. Patent US7627157B2, 1 December 2009. Available online: https://www.google.com/patents/US7627157 (accessed on 23 October 2019).
- Bodduluri, M.; Gildenberg, P.L.; Caddes, D.E. System and Methods for Aligning a Tool with a Desired Location or Object. U.S. Patent US7962192B2, 14 June 2011. Available online: https://www.google.com/patents/US7962192 (accessed on 23 October 2019).
- ARTAS Robotic Hair Restoration. Available online: http://restorationrobotics.com (accessed on 23 October 2019).
- Shin, J.W.; Kwon, S.H.; Kim, S.A.; Kim, J.Y.; Na, J.I.; Park, K.C.; Huh, C.H. Characteristics of robotically harvested hair follicles in Koreans. J. Am. Acad. Dermatol. 2015, 72, 146–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.C. Hair Transplanter. U.S. Patent US6461369B1, 8 October 2002. Available online: https://www.google.ch/patents/US6461369 (accessed on 23 October 2019).
- Lee, S.J.; Lee, H.J.; Hwang, S.J.; Kim, D.W.; Jun, J.B.; Chung, S.L.; Kim, J.C. Evaluation of survival rate after follicular unit transplantation using the KNU implanter. Dermatol. Surg. 2001, 27, 716–720. [Google Scholar] [PubMed]
- Lee, D.Y.; Lee, J.H.; Yang, J.M.; Lee, E.S. New instrument for hair transplant: Multichannel hair transplanter. Dermatol. Surg. 2005, 31, 379. [Google Scholar] [CrossRef] [PubMed]
- Pathomvanich, D.; Imagawa, K. Hair Restoration Surgery in Asians; Springer: Berlin, Germany, 2010; pp. 169–171. [Google Scholar]
- KNU Implanter. Available online: http://www.hairmedical.co.kr/eng/c03/c03_03.html (accessed on 23 October 2019).
- Bae, T.W.; Jung, Y.C.; Kim, K.H.; Kim, M.K.; Kim, J.C.; Suh, J.W.; Lee, H.S.; Choi, E.C.; Kim, D.S.; Hong, C.H. Manual Follicle-Transplanting Hair Transplanter for Increasing Graft Survival Rate. U.S. Patent US10251674B2, 9 April 2019. Available online: https://patents.justia.com/patent/10251674 (accessed on 11 June 2020).
- Bae, T.W.; Kim, K.H.; Kim, M.K.; Kim, J.C.; Suh, J.W.; Lee, S.I.; Lee, H.S.; Jung, Y.C.; Choi, E.C.; Kim, D.S.; et al. Automatic Hair Transplanter for Transplanting Follicles. U.S. Patent US 20170020565A1, 1 January 2017. Available online: https://www.freshpatents.com/-dt20170126ptan20170020565.php (accessed on 23 October 2019).
- EPOS2 Digital Positioning Controller. Available online: https://www.maxongroup.com/maxon/view/product/control/Positionierung/367676 (accessed on 23 October 2019).
- Korea Compliance Testing Laboratories. Available online: www.kctl.co.kr (accessed on 23 October 2019).
- Korea Testing Certification. Available online: https://www.ktc.re.kr (accessed on 23 October 2019).
- Korea Testing Laboratory. Available online: https://www.ktl.re.kr (accessed on 23 October 2019).
- Korea Conformity Laboratories. Available online: https://www.kcl.re.kr (accessed on 23 October 2019).
- Medical Device Information & Technology Assistance Center. Available online: https://www.greenpiatech.com (accessed on 23 October 2019).
- Korea Testing & Research Institute. Available online: www.ktr.or.kr (accessed on 23 October 2019).
- Medical Device Information & Technology Assistance Center. Available online: http://www.nids.or.kr (accessed on 23 October 2019).
- Daegu Regional Korea Food & Drug Administration. Available online: https://www.mfds.go.kr/wpge/m_154/de010728l001.do (accessed on 23 October 2019).
- Oh, J.W.; Kloepper, J.; Langan, E.A.; Kim, Y.; Yeo, J.; Kim, M.J.; His, T.C.; Rose, C.; Yoon, G.S.; Lee, S.J.; et al. A guide to studying human hair follicle cycling in vivo. J. Investig. Dermatol. 2016, 136, 34–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ISO 11137 Gamma & E-Beam Sterilization for Medical Devices. Available online: https://lso-inc.com/sterilization-validation-services/iso11137-gamma-ebeam-sterilization.html (accessed on 23 October 2019).
- Paired t-Tests. Available online: http://www.statstutor.ac.uk/resources/uploaded/paired-t-test.pdf (accessed on 23 October 2019).
- Data Analysis. Available online: http://learntech.uwe.ac.uk/da/Default.aspx?pageid=1442 (accessed on 23 October 2019).











| No. | Needle Motor (N-Motor) | Rod Motor (R-Motor) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Direction | No. of Rotations | Speed (rpm) | Acceleration (rad/s2) | Deceleration (rad/s2) | Direction | No. of Rotations | Speed (rpm) | Acceleration (rad/s2) | Deceleration (rad/s2) | |
| 1 | Forward | 9728 | 1350 | 20,000 | 20,000 | |||||
| 2 | Forward | 3584 | 1350 | 20,000 | 20,000 | Forward | 3584 | 1350 | 20,000 | 20,000 |
| 3 | Forward | 12,083 | 1350 | 20,000 | 20,000 | |||||
| 4 | Forward | 24,422 | 1350 | 20,000 | 20,000 | Forward | 25,221 | 1350 | 20,000 | 20,000 |
| 5 | Reverse | 6656 | 1350 | 20,000 | 20,000 | |||||
| 6 | Reverse | 17,766 | 1350 | 20,000 | 20,000 | Reverse | 28,088 | 1350 | 20,000 | 20,000 |
| 7 | Reverse | 12,800 | 1350 | 20,000 | 20,000 | |||||
| 8 | Reverse | 13,312 | 1350 | 20,000 | 20,000 | |||||
| Proposed Semi-Automatic Implanter | Manual Implanter | |||
|---|---|---|---|---|
| Mouse Number | Transplanted | Regrown | Transplanted | Regrown |
| No. 1. | 5 | 4 | 8 | 6 |
| No. 2. | 13 | 13 | 10 | 5 |
| No. 3. | 9 | 9 | 8 | 8 |
| No. 4. | 7 | 7 | 10 | 6 |
| Sum | 34 | 33 | 36 | 25 |
| Engraftment rate | 97% (33/34) | 70% (25/36) | ||
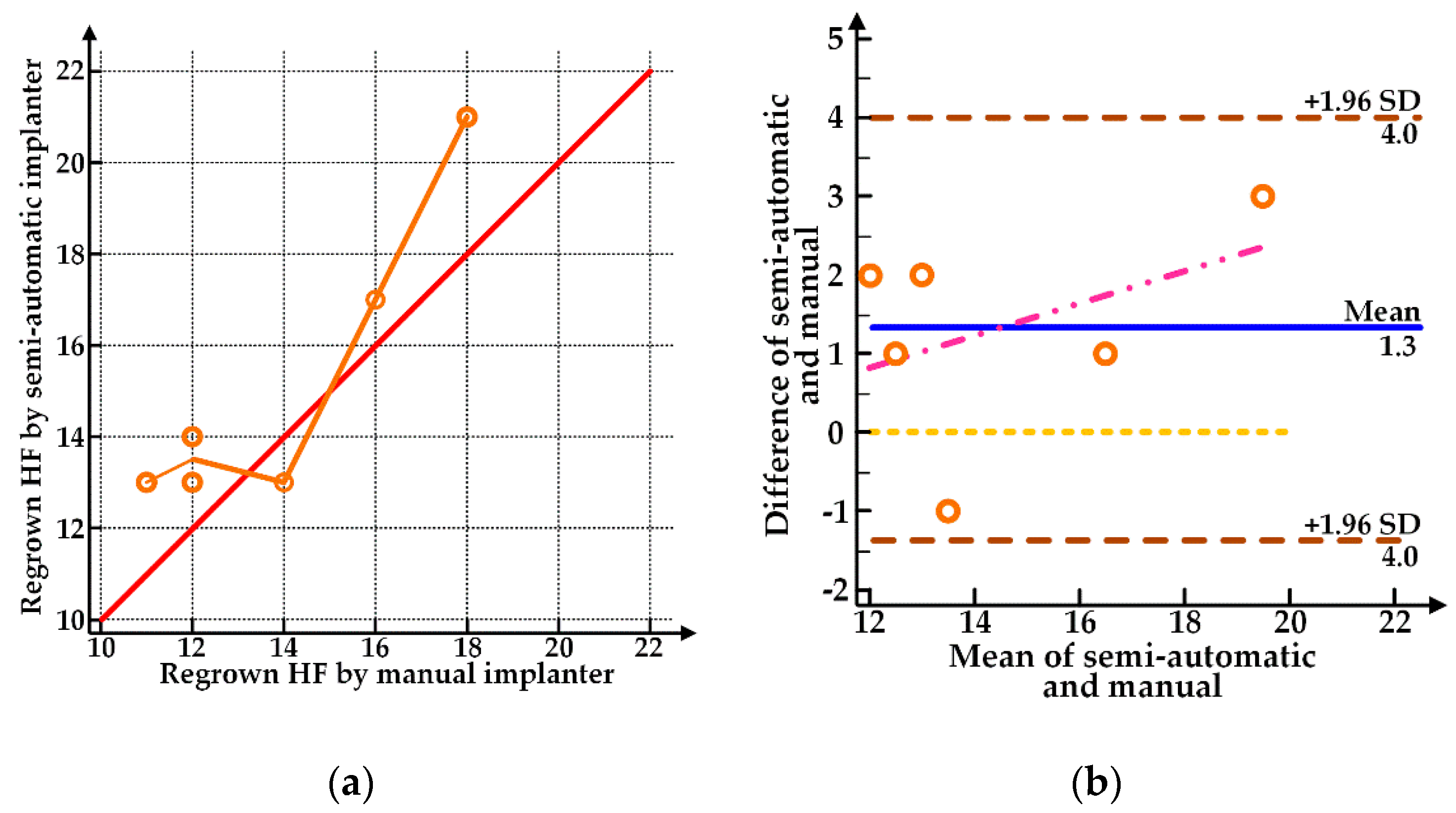
| No. | Manual Implanter | Semi-Automatic Implanter |
|---|---|---|
| 1 | 12 | 14 |
| 2 | 11 | 13 |
| 3 | 18 | 21 |
| 4 | 14 | 13 |
| 5 | 16 | 17 |
| 6 | 12 | 13 |
| Average number of regrown HFs (Mean ± SD) | 13.8 ± 2.7 | 15.2 ± 3.3 |
| Engraftment rate | 55% (83/150) | 61% (91/150) |
| Difference | Kolmogorov–Smirnov | ||
| Statistics 0.237 | Degree of Freedom 6 | Significance Probability 0.200 | |
| Shapiro–Wilk | |||
| Statistics 0.927 | Degree of Freedom 6 | Significance Probability 0.554 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, T.W.; Jung, Y.C.; Kim, K.H. Needle Transportable Semi-Automatic Hair Follicle Implanter and Image-Based Hair Density Estimation for Advanced Hair Transplantation Surgery. Appl. Sci. 2020, 10, 4046. https://doi.org/10.3390/app10114046
Bae TW, Jung YC, Kim KH. Needle Transportable Semi-Automatic Hair Follicle Implanter and Image-Based Hair Density Estimation for Advanced Hair Transplantation Surgery. Applied Sciences. 2020; 10(11):4046. https://doi.org/10.3390/app10114046
Chicago/Turabian StyleBae, Tae Wuk, Yong Chul Jung, and Kyu Hyung Kim. 2020. "Needle Transportable Semi-Automatic Hair Follicle Implanter and Image-Based Hair Density Estimation for Advanced Hair Transplantation Surgery" Applied Sciences 10, no. 11: 4046. https://doi.org/10.3390/app10114046
APA StyleBae, T. W., Jung, Y. C., & Kim, K. H. (2020). Needle Transportable Semi-Automatic Hair Follicle Implanter and Image-Based Hair Density Estimation for Advanced Hair Transplantation Surgery. Applied Sciences, 10(11), 4046. https://doi.org/10.3390/app10114046





