Computer-Aided Biomedical Imaging of Periiliac Adipose Tissue Identifies Perivascular Fat as a Marker of Disease Complexity in Patients with Lower Limb Ischemia
Abstract
:1. Introduction
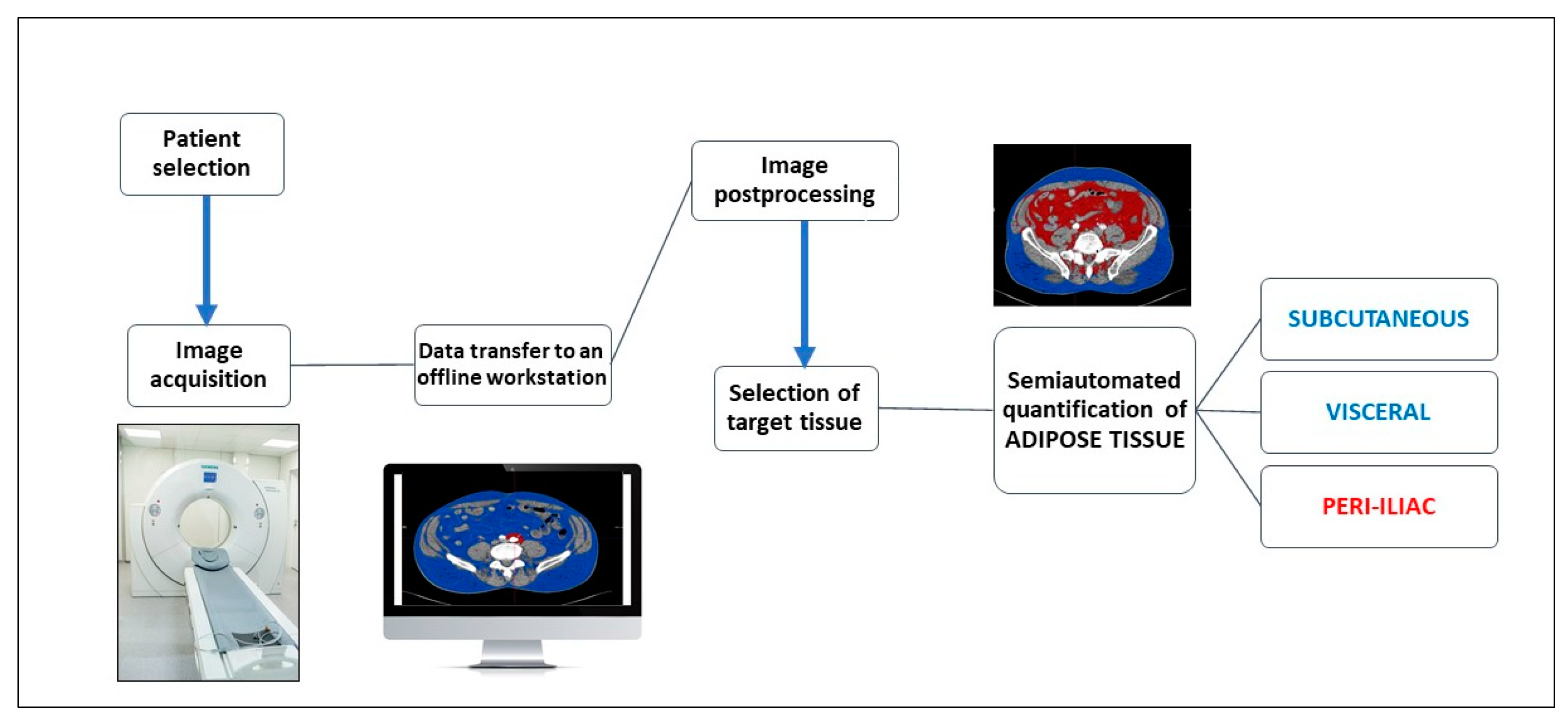
2. Materials and Methods
2.1. CT Acquisition
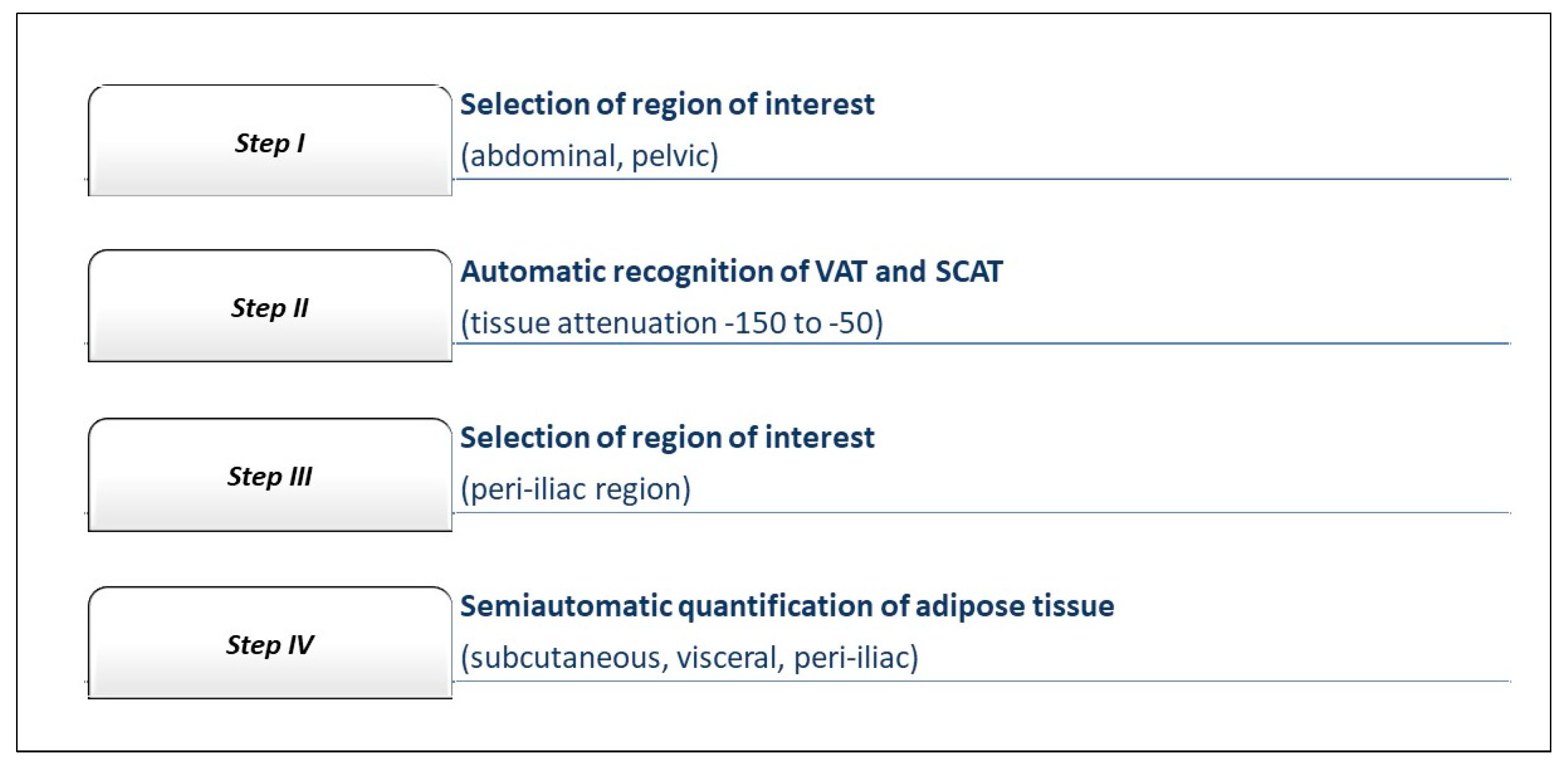
2.2. Computer-Aided CT Image Postprocessing
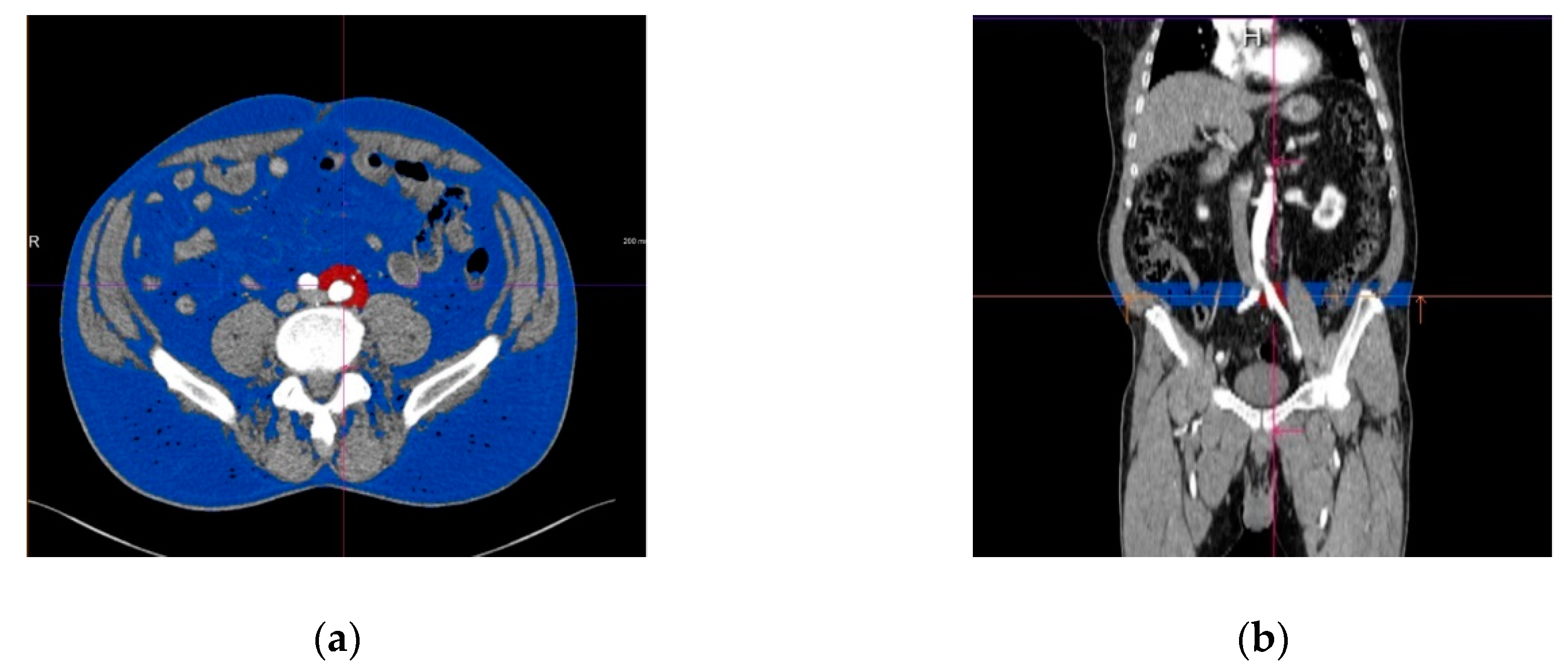
2.3. Assessment of the Periiliac Adipose Tissue
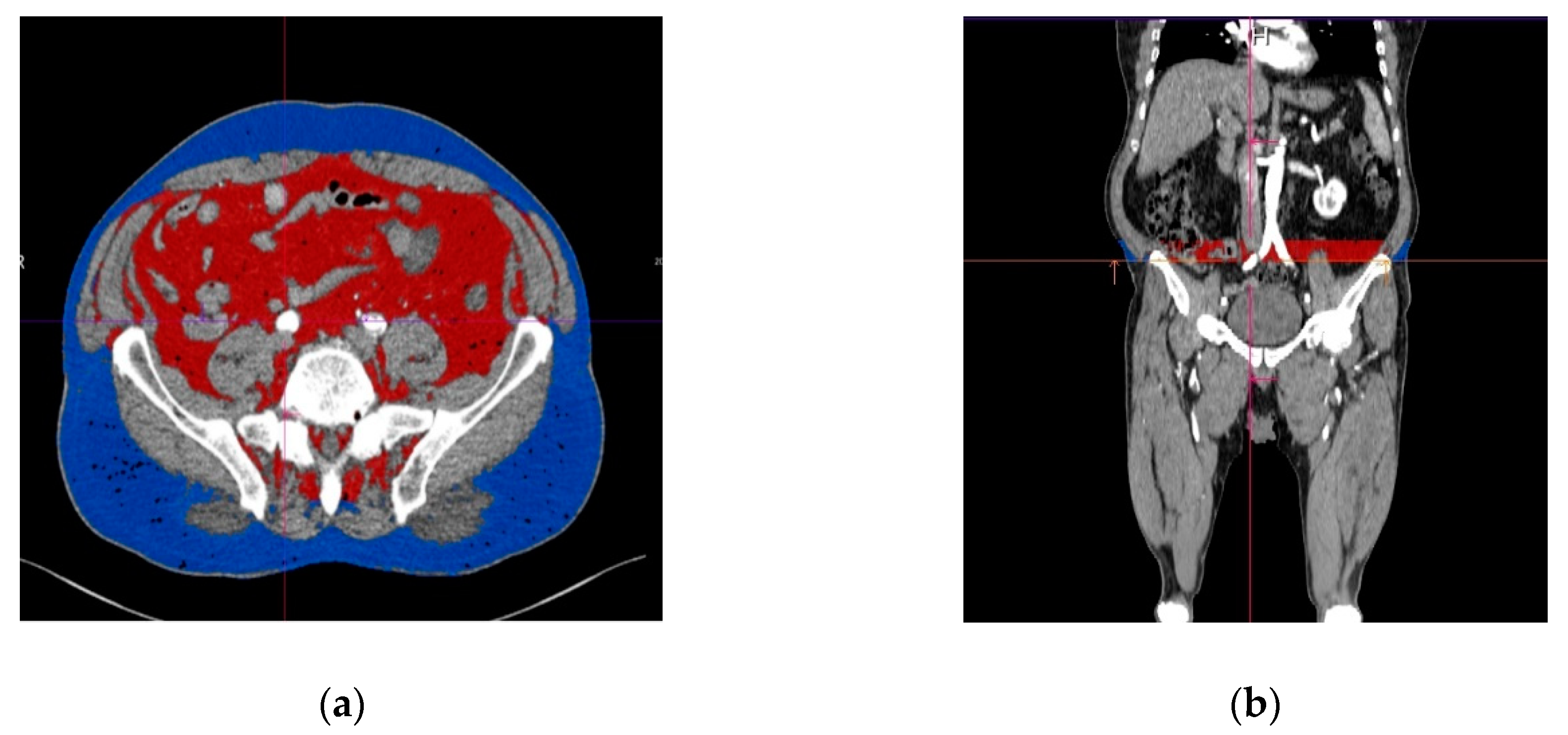
2.4. Assessment of The Subcutaneous and Visceral Adipose Tissue
- -
- complexity of the peripheral artery disease, expressed by TASC (Trans-Atlantic Inter-Society Consensus) class, in which TASC A represents the less complex and TASC D the most complex disease, according to the CT angiographic aspect of the iliac atherosclerotic lesions [12];
- -
- traditional cardiovascular risk factors and co-morbidities;
- -
- the amount of other computer-aided imaging biomarkers characterizing adipose tissue distribution, including the visceral and subcutaneous fat measured at the level of the common iliac arteries.
2.5. Patient Groups
3. Results
3.1. Baseline Characteristics of the Study Population
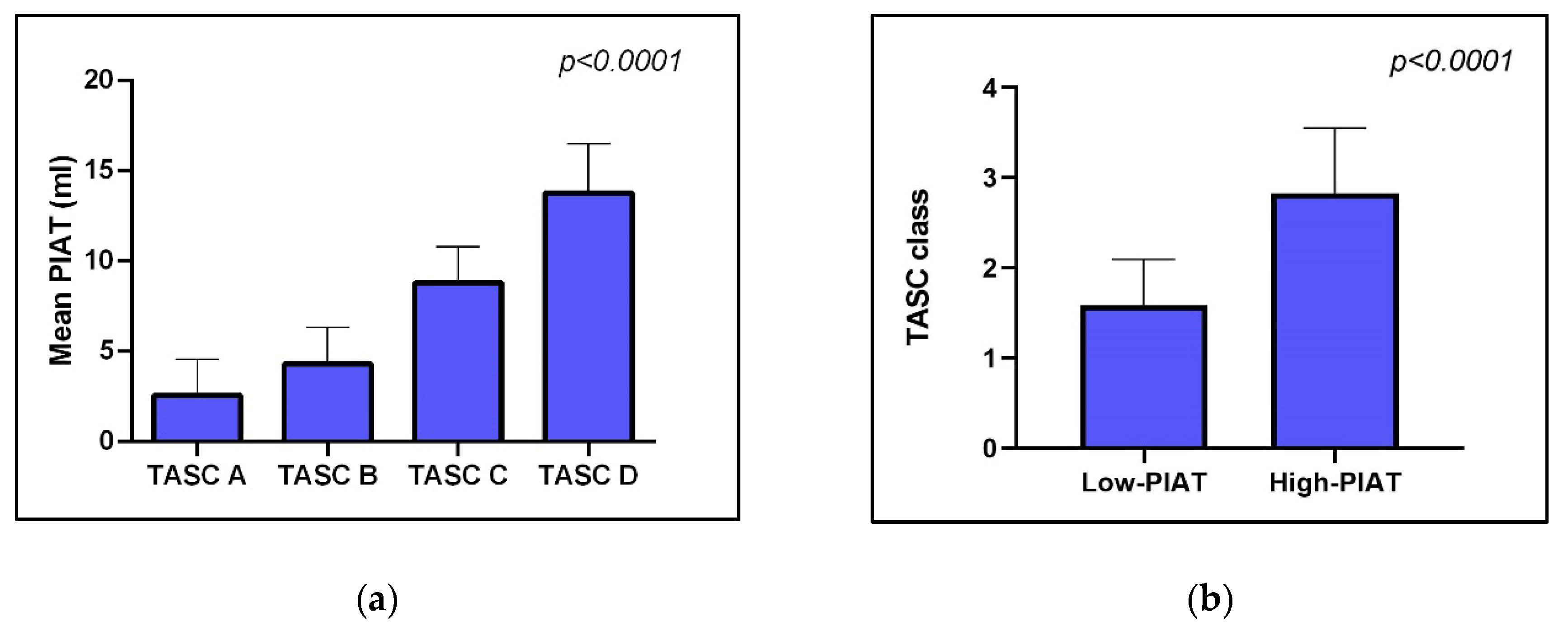
3.2. PIAT Volume and Severity of Peripheral Arterial Disease
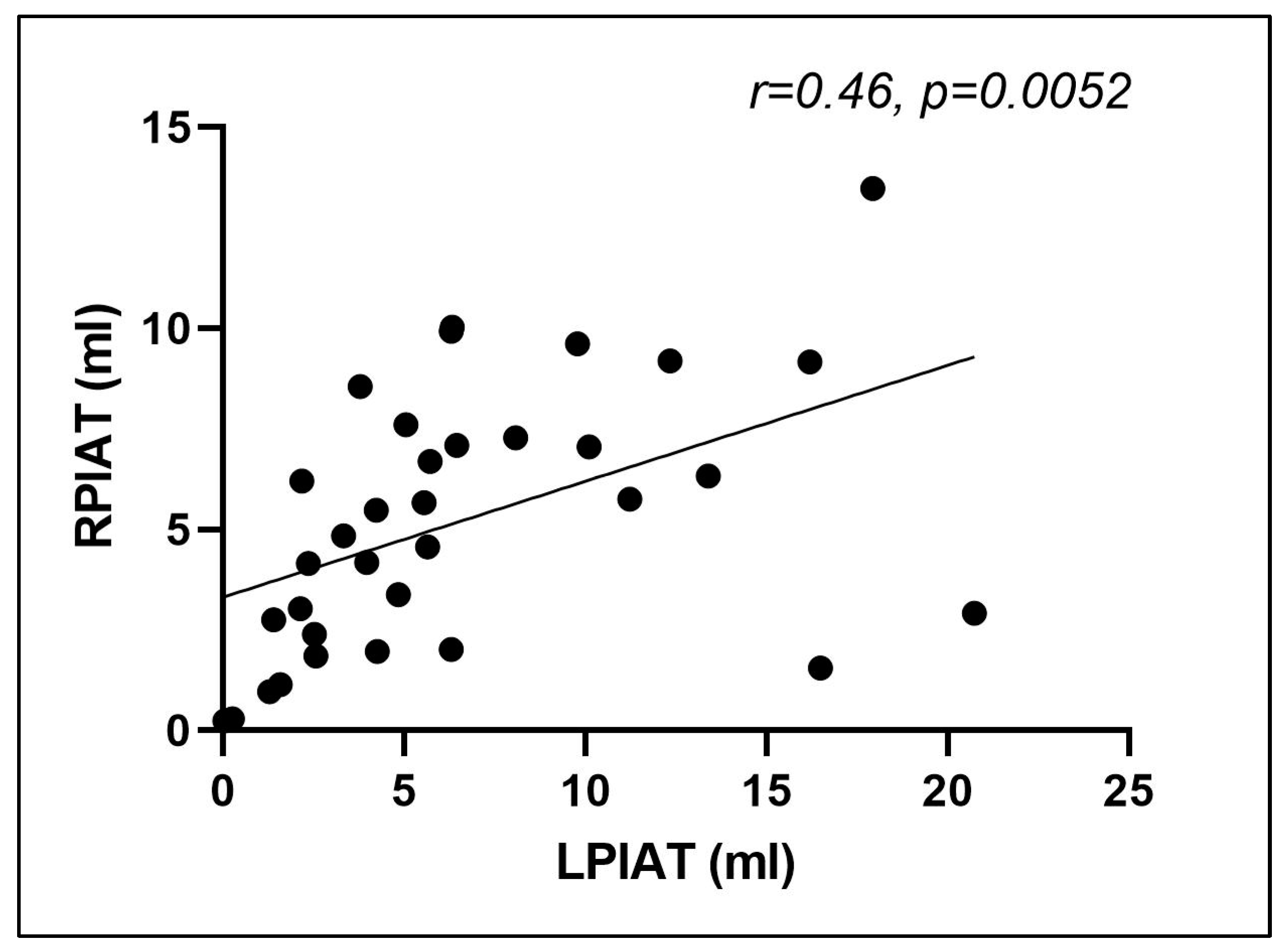
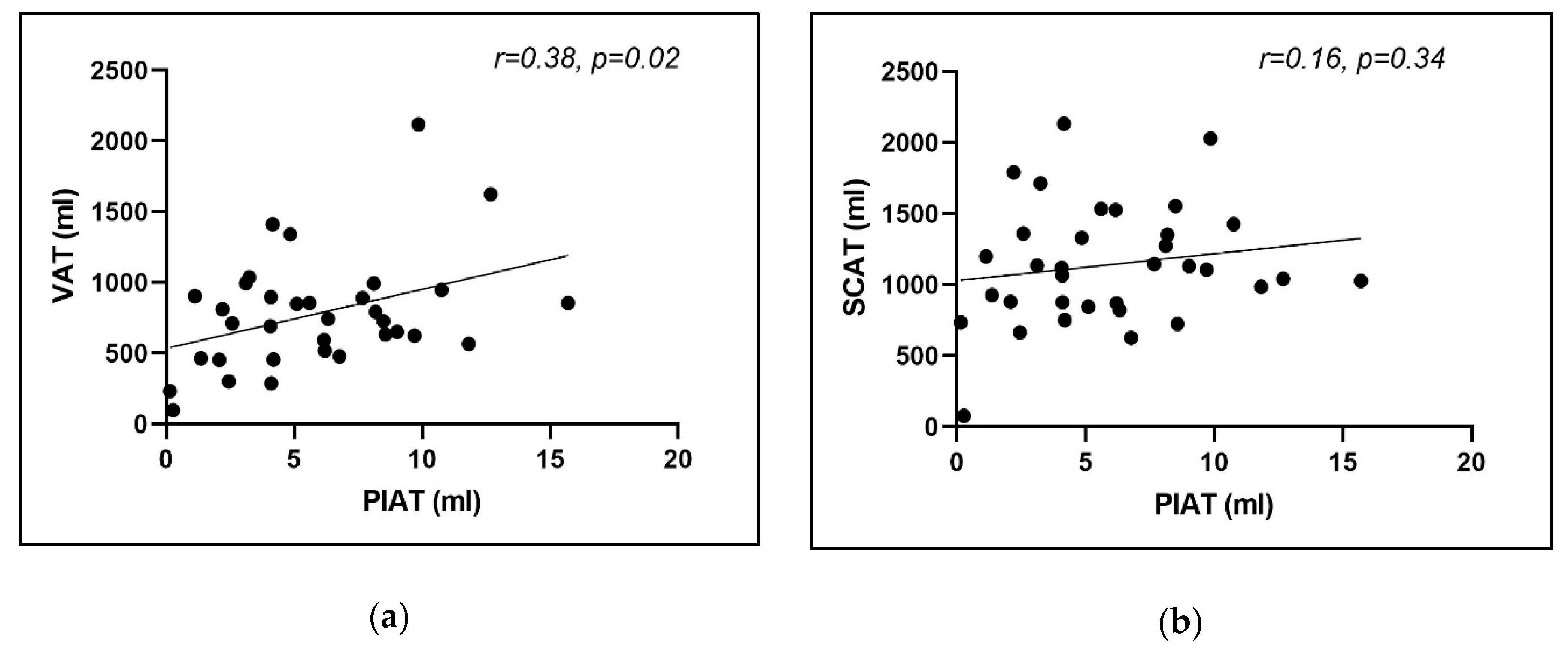
3.3. Computer-Aided Imaging Biomarkers Characterizing Adipose Tissue Distribution
4. Discussion
4.1. Study Limitations
4.2. Future Developments
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hicks, C.W.; Yang, C.; Ndumele, E.C.; Folsom, R.A.; Heiss, G.; Black, H.J.; Selvin, E.; Matsushita, K. Associations of Obesity With Incident Hospitalization Related to Peripheral Artery Disease and Critical Limb Ischemia in the ARIC Study. J. Am. Heart Assoc. 2018, 7, e008644. [Google Scholar] [CrossRef]
- Ratiu, M.; Rat, N.; Nyulas, T.; Moldovan, G.; Rus, V.; Benedek, T.; Benedek, I. Coronary Plaque Geometry and Thoracic Fat Distribution in Patients with Acute Chest Pain—A CT Angiography Study. J. Cardiovasc. Emergencies 2019, 5, 18–24. [Google Scholar] [CrossRef] [Green Version]
- Britton, K.A.; Fox, C.S. Perivascular Adipose Tissue and Vascular Disease. Clin. Lipidol. 2011, 6, 79–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yucel, N.; Arany, Z. Fat, Obesity, and the Endothelium. Curr. Opin. Physiol. 2019, 12, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, K.; Drosos, I.; Konstantinides, S. Perivascular Adipose Tissue: Epiphenomenon or Local Risk Factor? Int. J. Obes. (Lond) 2017, 41, 1311–1323. [Google Scholar] [CrossRef] [PubMed]
- Brown, N.K.; Zhou, Z.; Zhang, J. Perivascular Adipose Tissue in Vascular Function and Disease: A Review of Current Research and Animal Models. Arter. Thromb. Vasc. Biol. 2014, 34, 1621–1630. [Google Scholar] [CrossRef] [Green Version]
- Karastergioua, K.; Mohamed-Ali, V. The Autocrine and Paracrine Roles of Adipokines. Mol. Cell Endocrinol. 2010, 318, 69–78. [Google Scholar] [CrossRef] [Green Version]
- Trujillo, E.M.; Lee, M.J.; Sullivan, S.; Feng, J.; Schneider, H.S.; Greenberg, S.A.; Fried, K.S. Tumor Necrosis Factor and Glucocorticoid Synergistically Increase Leptin Production in Human Adipose Tissue: Role for p38 Mitogen-Activated Protein Kinase. J. Clin. Endocrinol. Metab. 2006, 91, 1484–1490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iikuni, N.; Lam, Q.L.; Lu, L.; Matarese, G.; La Cava, A. Leptin and Inflammation. Curr. Immunol. Rev. 2008, 4, 70–79. [Google Scholar] [CrossRef]
- Nyulas, T.; Morariu, M.; Rat, N.; Marton, E.; Rus, V.A.; Ratiu, M.; Benedek, T.; Benedek, I. Epicardial Adipose Tissue Role as a Marker of Higher Vulnerability in Patients with Coronary Artery Disease. J. Interdiscip. Med. 2018, 3, 77–83. [Google Scholar] [CrossRef] [Green Version]
- Kim, W.H.; Kim, C.G.; Kim, D.W. Optimal CT Number Range for Adipose Tissue When Determining Lean Body Mass in Whole-Body F-18 FDG PET/CT Studies. Nucl. Med. Mol. Imaging. 2012, 46, 294–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.R.G. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J. Vasc. Surg. 2007, 45, S5–S67. [Google Scholar] [CrossRef] [Green Version]
- Iozzo, P. Myocardial, Perivascular, and Epicardial Fat. Diabetes Care 2011, 34 (Suppl. 2), S371–S379. [Google Scholar] [CrossRef] [Green Version]
- Demir, E.; Harmankaya, N.Ö.; Utku, K.I. The Relationship between Epicardial Adipose Tissue Thickness and Serum Interleukin-17a Level in Patients with Isolated Metabolic Syndrome. Biomolecules 2019, 9, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talman, A.H.; Psaltis, P.J.; Cameron, J.D.; Meredith, I.T.; Seneviratne, S.K.; Wong, D.T. Epicardial Adipose Tissue: Far More than a Fat Depot. Cardiovasc. Diagn. 2014, 4, 416–429. [Google Scholar] [CrossRef]
- Opincariu, D.; Chitu, M. Atrial Fibrillation and Acute Myocardial Infarction—An Inflammation-mediated Association. J. Cardiovasc. Emergencies 2018, 4, 123–132. [Google Scholar] [CrossRef] [Green Version]
- Cinteza, M.; Benedek, I. Epicardial Adipose Tissue—A New Biomarker of Cardiovascular Risk. J. Cardiovasc. Emergencies 2016, 2, 4–6. [Google Scholar] [CrossRef] [Green Version]
- Hung, P.H.; Tsai, H.B.; Lin, C.H.; Hung, K.Y. Abdominal Obesity is Associated with Peripheral Artery Disease in Hemodialysis Patients. PLoS ONE 2013, 8, e67555. [Google Scholar] [CrossRef]
- Jakovljević, B.; Stojanov, V.; Lović, D.; Paunović, K.; Radosavljević, V.; Tutić, I. Obesity and Fat Distribution as Predictors of Aortoiliac Peripheral Arterial Disease in Middle-aged Men. Eur. J. Intern. Med. 2011, 22, 84–88. [Google Scholar] [CrossRef]
- Lee, J.J.; Pedley, A.; Weinberg, I. Relation of Iliac Artery Calcium With Adiposity Measures and Peripheral Artery Disease. Am. J. Cardiol. 2017, 119, 1217–1223. [Google Scholar] [CrossRef] [Green Version]
- Fox, C.S.; Massaro, J.M.; Schlett, C.L. Periaortic Fat Deposition is Associated with Peripheral Arterial Disease: The Framingham Heart Study. Circ. Cardiovasc. Imaging 2010, 3, 515–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takaoka, M.; Suzuki, H.; Shioda, S. Endovascular Injury Induces Rapid Phenotypic Changes in Perivascular Adipose Tissue. Arter. Thromb. Vasc. Biol. 2010, 30, 1576–1582. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Loscalzo, J.; Ridker, P.M.; Farkouh, M.E.; Hsue, P.Y.; Fuster, V.; Hasan, A.A.; Amar, S. Inflammation, Immunity, and Infection in Atherothrombosis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2018, 72, 2071–2081. [Google Scholar] [CrossRef]
- Antoniades, C.; Kotanidis, C.P.; Berman, D.S. State-of-the-art review article. Atherosclerosis affecting fat: What can we learn by imaging perivascular adipose tissue? J. Cardiovasc. Comput. Tomogr. 2019, 13, 288–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, K.; Masataka, S. Roles of Perivascular Adipose Tissue in the Pathogenesis of Atherosclerosis. Front. Physiol. 2018, 9, 3. [Google Scholar] [CrossRef] [Green Version]
- Stone, P.A.; Yacoub, M. Inflammatory biomarkers in peripheral arterial disease. Semin. Vasc. Surg. 2014, 27, 148–151. [Google Scholar] [CrossRef]
- Ozaki, Y.; Imanishi, T.; Akasaka, T. Inflammatory Biomarkers in Peripheral Artery Disease: Diagnosis, Prognosis, and Therapeutic Challenges. Curr. Med. Chem. 2015, 22, 2744–2753. [Google Scholar] [CrossRef]
- Antonopoulos, A.S.; Sanna, F.; Sabharwal, N.; Thomas, S.; Oikonomou, E.K.; Herdman, L.; Margaritis, M.; Shirodaria, C.; Kampoli, A.M.; Akoumianakis, I.; et al. Detecting human coronary inflammation by imaging perivascular fat. Sci. Transl. Med. 2017, 9, eaal2658. [Google Scholar] [CrossRef] [Green Version]
- Oikonomou, E.K.; Marwan, M.; Desai, M.Y.; Mancio, J.; Alashi, A.; Hutt Centeno, E.; Thomas, S.; Herdman, L.; Kotanidis, C.P.; Thomas, K.E.; et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): A post-hoc analysis of prospective outcome data. Lancet 2018, 392, 929–939. [Google Scholar] [CrossRef] [Green Version]
| Parameter | Group 1 (Low Mean Periiliac Fat Volume) n = 17 | Group 2 (High Mean Periiliac Fat Volume) n = 17 | 95% CI | p-Value |
|---|---|---|---|---|
| Age (years) | 69.59 +/− 12.12 | 69 +/− 7.99 | 95% CI −3.760 to 10.58 | p = 0.33 |
| Gender, male (n,%) | 10 (58.82%) | 15 (88.23%) | 95% CI −0.5937 to 0.0054 | p = 0.054 |
| Cholesterol (mg/dl) | 149.8+/−52.68 | 224.1 +/− 76.09 | 95% CI −126.3 to −22.24 | p = 0.007 |
| Creatinine (mg/dl) | 1.1 +/−0.47 | 0.93 +/− 0.19 | 95% CI −0.4854 to 0.137 | p = 0.25 |
| Triglycerides (mg/dl) | 140.7+/− 50.49 | 134.78 +/− 40.06 | 95% CI −43.95 to 38.19 | p = 0.88 |
| Hematocrit (%) | 36.52 +/−6.63 | 40.71 +/− 3.55 | 95% CI −0.3348 to 8.71 | p = 0.068 |
| Hemoglobin (g/dl) | 12.51+/− 2.18 | 13.47 +/− 1.52 | 95% CI −0.6303 to 2.551 | p = 0.22 |
| Previous AMI (n,%) | 3 (17.64%) | 2 (11.76%) | 95% CI −0.3130 to 0.1954 | p = 0.64 |
| Hypertension (n,%) | 16 (94.11%) | 17 (100%) | 95% CI −0.061 to 0.1786 | p = 0.32 |
| Diabetes | 6 (35.29%) | 6 (35.29%) | 95% CI −0.3442 to 0.3442 | p = 0.99 |
| History of stroke (n,%) | 1 (5.8%) | 2 (11.7%) | 95% CI −0.1443 to 0.2620 | p = 0.55 |
| Coronary artery disease (n,%) | 5 (29.4%) | 2 (11.7%) | 95% CI −0.5962 to 0.3270 | p = 0.54 |
| Parameter | Group 1 (Low-PIAT Volume) n = 17 | Group 2 (High-PIAT Volume) n = 17 | 95% CI | p-value |
|---|---|---|---|---|
| TASC class | TASC A: 7 (41.17%) TASC B: 10 (58.83%) | TASC A: 1 (5.88%) TASC B: 3 (17.64%) TASC C: 11 (64.7%) TASC D: 2 (11.76%) | 95% CI 0.7971 to 1.673 | p < 0.0001 |
| Fontaine class | Fontaine 2:5 (29.4%) Fontaine 3:7 (41.1%) Fontaine 4:5 (29.4%) | Fontaine 2:8 (47.05%) Fontaine 3:1 (5.88%) Fontaine 4:8 (47.05%) | 95% CI −0.6298 to 0.6298 | p = 0.99 |
| Rutherford class | Rutherford 2:2 (11.7%) Rutherford 3:3 (17.6%) Rutherford 4:7 (41.1%) Rutherford 5:3 (17.6%) Rutherford 6:2 (11.7%) | Rutherford 3:8 (47%) Rutherford 4:1 (5.8%) Rutherford 5:1 (5.8%) Rutherford 6:7 (41.1%) | 95% CI −0.5134 to 1.337 | p = 0.37 |
| Patient No. | SCAT LCIA (mL) | SCAT RCIA (mL) | VAT LCIA (mL) | VAT RCIA (mL) | PIAT LCIA (mL) | PIAT RCIA (mL) |
|---|---|---|---|---|---|---|
| 1 | 627.27 | 839.52 | 202.79 | 261.94 | 0.05 | 0.24 |
| 2 | 92.72 | 57.4 | 112.43 | 82.25 | 0.25 | 0.29 |
| 3 | 1204.86 | 1195.03 | 895.22 | 909.31 | 1.28 | 0.97 |
| 4 | 1075.22 | 776.13 | 557.45 | 371.28 | 1.58 | 1.15 |
| 5 | 1076.4 | 684.68 | 550.18 | 358.08 | 1.4 | 2.76 |
| 6 | 2011.81 | 1570.1 | 897.57 | 725.89 | 2.56 | 1.86 |
| 7 | 691.36 | 634.01 | 317.53 | 286.17 | 2.52 | 2.39 |
| 8 | 1361.22 | 1356.32 | 709.16 | 714.06 | 2.13 | 3.03 |
| 9 | 1196.26 | 1071.03 | 1011.07 | 978.79 | 4.26 | 1.97 |
| 10 | 1711.49 | 1714.39 | 1038.44 | 1035.54 | 2.36 | 4.15 |
| 11 | 1103.31 | 1133.02 | 680.07 | 699.7 | 3.96 | 4.18 |
| 12 | 1173.05 | 960.16 | 968.05 | 825.52 | 3.33 | 4.85 |
| 13 | 840.15 | 914.01 | 276.95 | 294.3 | 4.84 | 3.38 |
| 14 | 2108 | 2158 | 1395.56 | 1425.88 | 6.3 | 2.02 |
| 15 | 800.32 | 702.41 | 477.99 | 430.46 | 2.18 | 6.21 |
| 16 | 1313.68 | 1347.71 | 1349.08 | 1332.92 | 4.23 | 5.48 |
| 17 | 818.35 | 870.67 | 839.27 | 860.25 | 5.65 | 4.57 |
| 18 | 1702.37 | 1363.44 | 947.94 | 761.77 | 5.55 | 5.67 |
| 19 | 1422.25 | 1627.94 | 559.81 | 626.21 | 3.79 | 8.56 |
| 20 | 828.78 | 911.2 | 494.94 | 539.79 | 5.71 | 6.69 |
| 21 | 814.13 | 829.39 | 768.86 | 714.69 | 5.05 | 7.61 |
| 22 | 619.45 | 634.31 | 470.04 | 485.82 | 6.45 | 7.09 |
| 23 | 1136.8 | 1151.41 | 897.53 | 882.92 | 8.07 | 7.28 |
| 24 | 1498.29 | 1050.45 | 1175.88 | 810.86 | 6.3 | 9.93 |
| 25 | 1409.38 | 1293.81 | 862.58 | 724.8 | 6.33 | 10.03 |
| 26 | 1715.19 | 1391.49 | 1337.09 | 115.86 | 11.23 | 5.75 |
| 27 | 716.63 | 729.95 | 611.98 | 652.08 | 10.1 | 7.05 |
| 28 | 1202.97 | 1058.36 | 702.6 | 599.78 | 16.49 | 1.56 |
| 29 | 861.24 | 1348.97 | 481.68 | 767.56 | 9.79 | 9.62 |
| 30 | 1956.01 | 2101.88 | 2086.93 | 2147.19 | 13.4 | 6.33 |
| 31 | 1421.26 | 1430.29 | 952.03 | 943 | 12.34 | 9.19 |
| 32 | 1019.01 | 949.97 | 591.27 | 537.99 | 20.74 | 2.92 |
| 33 | 890.27 | 1189.86 | 1413.37 | 1833.53 | 16.2 | 9.17 |
| 34 | 1070.25 | 982.73 | 910.61 | 798.8 | 17.94 | 13.48 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rapolti, E.; Opincariu, D.; Benedek, I.; Kovacs, I.; Ratiu, M.; Rat, N.; Benedek, T. Computer-Aided Biomedical Imaging of Periiliac Adipose Tissue Identifies Perivascular Fat as a Marker of Disease Complexity in Patients with Lower Limb Ischemia. Appl. Sci. 2020, 10, 4456. https://doi.org/10.3390/app10134456
Rapolti E, Opincariu D, Benedek I, Kovacs I, Ratiu M, Rat N, Benedek T. Computer-Aided Biomedical Imaging of Periiliac Adipose Tissue Identifies Perivascular Fat as a Marker of Disease Complexity in Patients with Lower Limb Ischemia. Applied Sciences. 2020; 10(13):4456. https://doi.org/10.3390/app10134456
Chicago/Turabian StyleRapolti, Emese, Diana Opincariu, Imre Benedek, Istvan Kovacs, Mihaela Ratiu, Nora Rat, and Theodora Benedek. 2020. "Computer-Aided Biomedical Imaging of Periiliac Adipose Tissue Identifies Perivascular Fat as a Marker of Disease Complexity in Patients with Lower Limb Ischemia" Applied Sciences 10, no. 13: 4456. https://doi.org/10.3390/app10134456
APA StyleRapolti, E., Opincariu, D., Benedek, I., Kovacs, I., Ratiu, M., Rat, N., & Benedek, T. (2020). Computer-Aided Biomedical Imaging of Periiliac Adipose Tissue Identifies Perivascular Fat as a Marker of Disease Complexity in Patients with Lower Limb Ischemia. Applied Sciences, 10(13), 4456. https://doi.org/10.3390/app10134456






