Sana: A Gamified Rehabilitation Management System for Anterior Cruciate Ligament Reconstruction Recovery
Abstract
1. Introduction
1.1. Post-Operative ACLR Surgery
1.2. Related Work
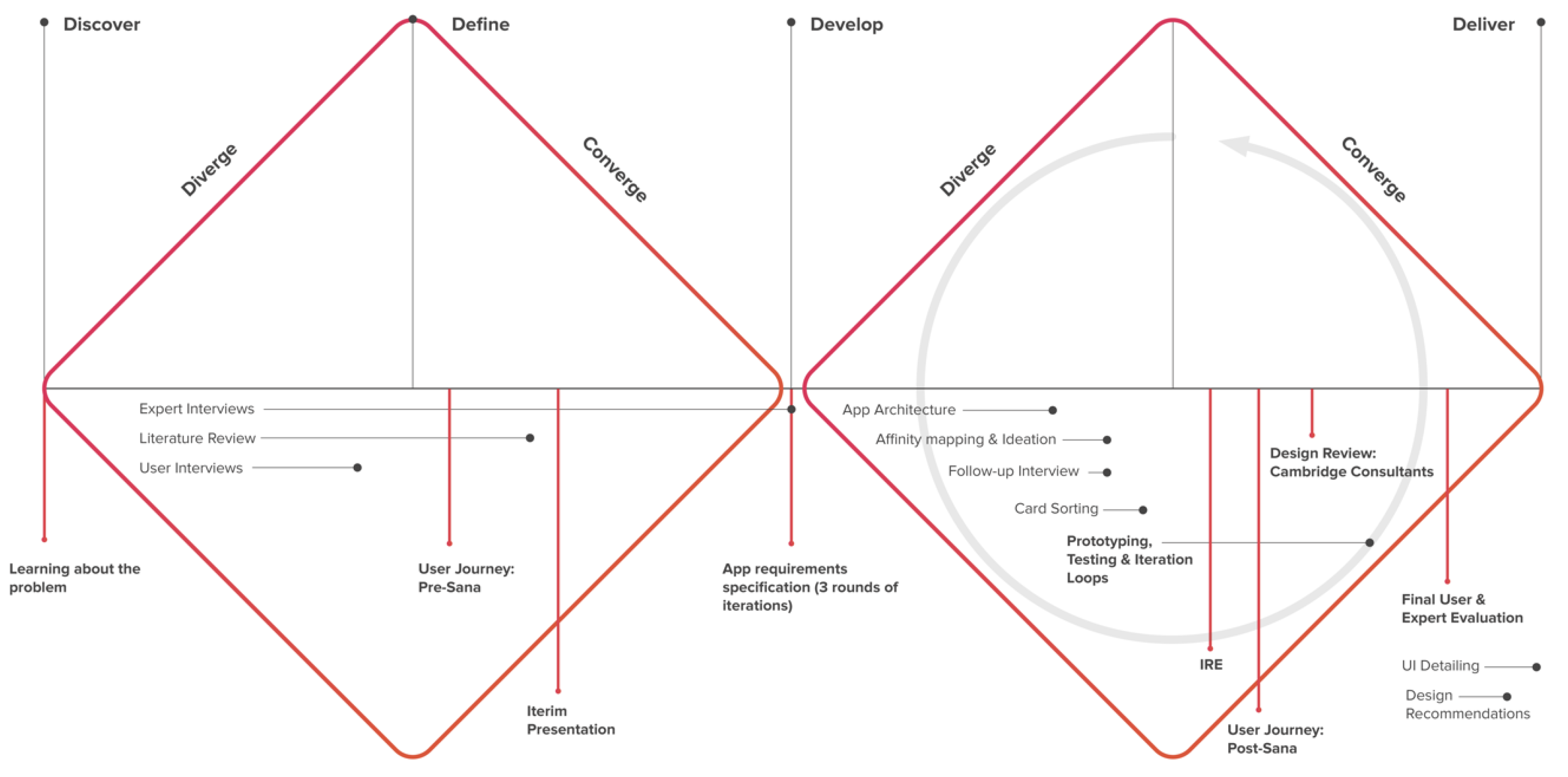
2. Methods
2.1. Discover and Define Phases
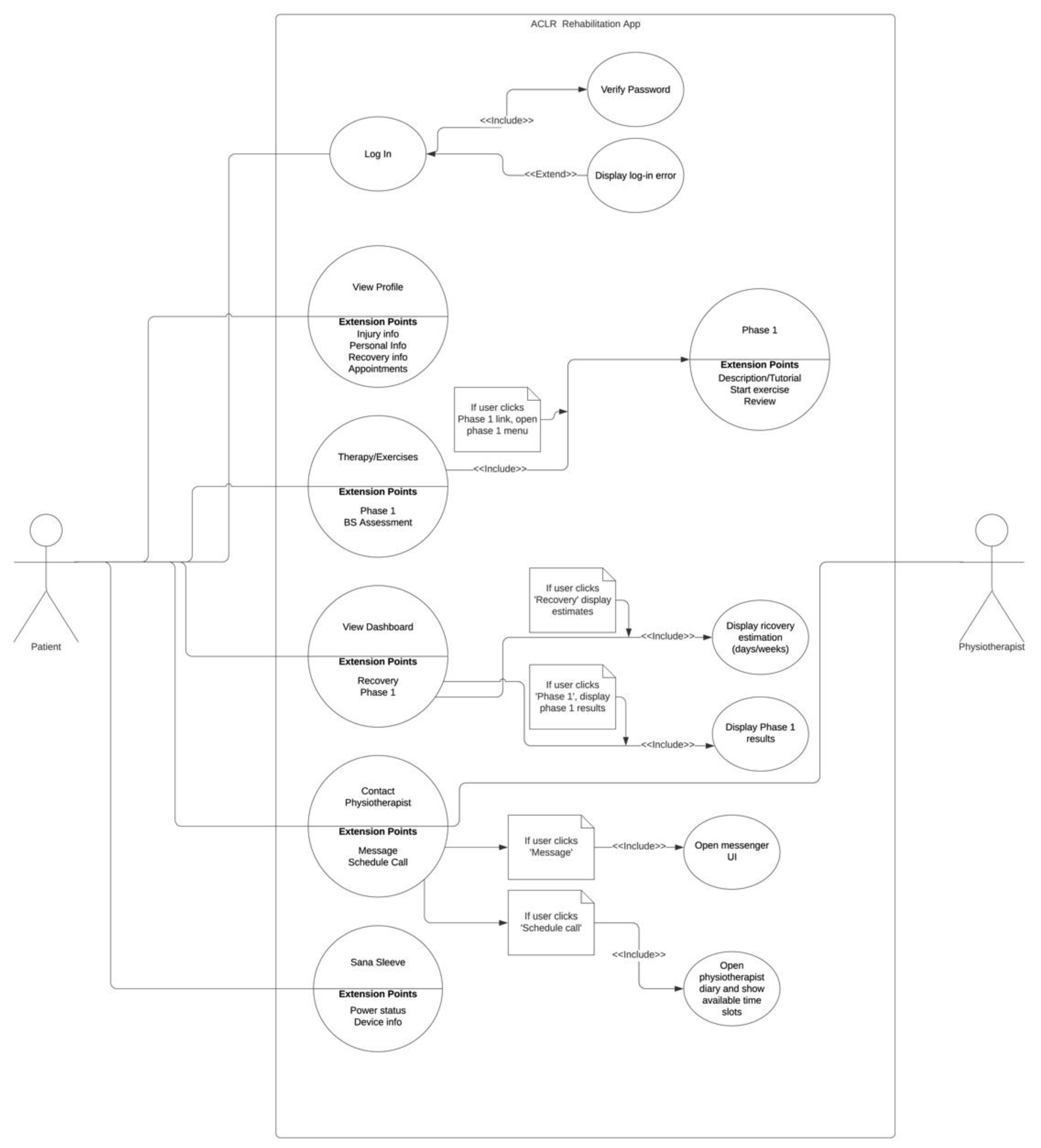
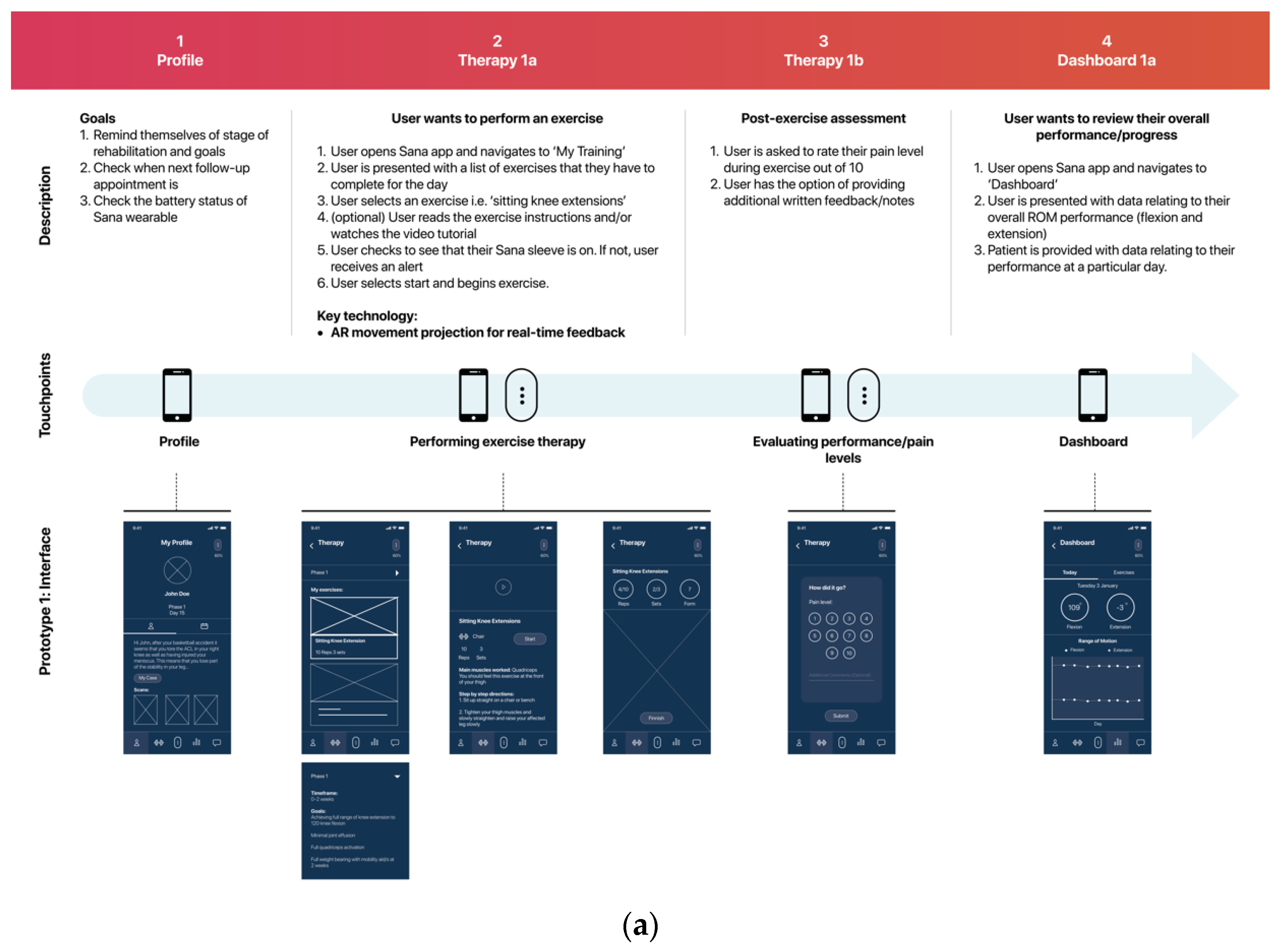
2.2. Develop Phase
2.3. Deliver Phase
3. Results
3.1. Discover Phase
- Self-efficacy: Issues related to self-efficacy resulted from patients having an unclear or no indication of progress and improvement during rehabilitation. Patients commonly stated that they often questioned the effectiveness of their therapy and had limited engagement with the exercises they were performing. There was an overall interest in being able to visualize the effects their therapy was having on their recovery and be able to track progress at each stage of rehabilitation. One interviewee stated, “It is easy to notice the pain, but I cannot see the improvement or progress”.
- Education: All interviewees stated that they were issued a paper-based treatment program detailing a summary of their injury and rehabilitation procedure. Users reported limited engagement with this information, reporting that the initial exercise demonstrations provided by their caregivers were more effective in reinforcing the correct exercise technique than static images. One interviewee noted that YouTube videos on exercises were beneficial. Overall, the key takeaway from this was that patients responded better to information that was presented in an engaging manner. Subsequent design concepts must explore ways that this can be achieved. One interviewee stated, “I had no level of engagement with my exercises… I did not even know if what I was doing was correct.”
- Engagement with the primary caregiver: There was a shared view amongst users that they felt they had just been left to their own devices once discharged from the ward. Feedback would often be provided during patient follow-up; however, this was commonly described as either being ‘monotonous’, ‘disengaging’ or ‘useless.’ One interviewee remarked that something as simple as being told she was making small improvements by her caregiver would have been enough to motivate her to be persistent with therapy. In addition, one interviewee stated, “It would have been nice to have a follow-up with a healthcare specialist who understood the challenges I was having and gave useful advice. The feedback I was provided was often always the same”.
3.2. Define Phase
3.3. Develop Phase
- Profile: What information, if any, is a patient required to know regarding their injury? How often is a patient called up for follow-up treatment? What kind of advice or medication will a patient be given regarding pain and swelling management?
- Therapy and exercises: Will a patient be provided additional exercise equipment? If so, what are some examples of this equipment? How often do patients engage in exercise? How much input, if any, should a patient have in terms of deciding what exercises? Should patients be given a range of alternative exercises to perform if they are struggling? Is diet something patients need to regularly monitor during rehabilitation?
- Dashboard: What are the different milestones that patients have during phase 1 of rehabilitation? What kind of data do caregivers need to collect about patients? How do patients currently determine whether treatment is working? What are the commonly used metrics to determine a patient’s rate of recovery?
- Contact: How much flexibility do patients have in scheduling appointments themselves?
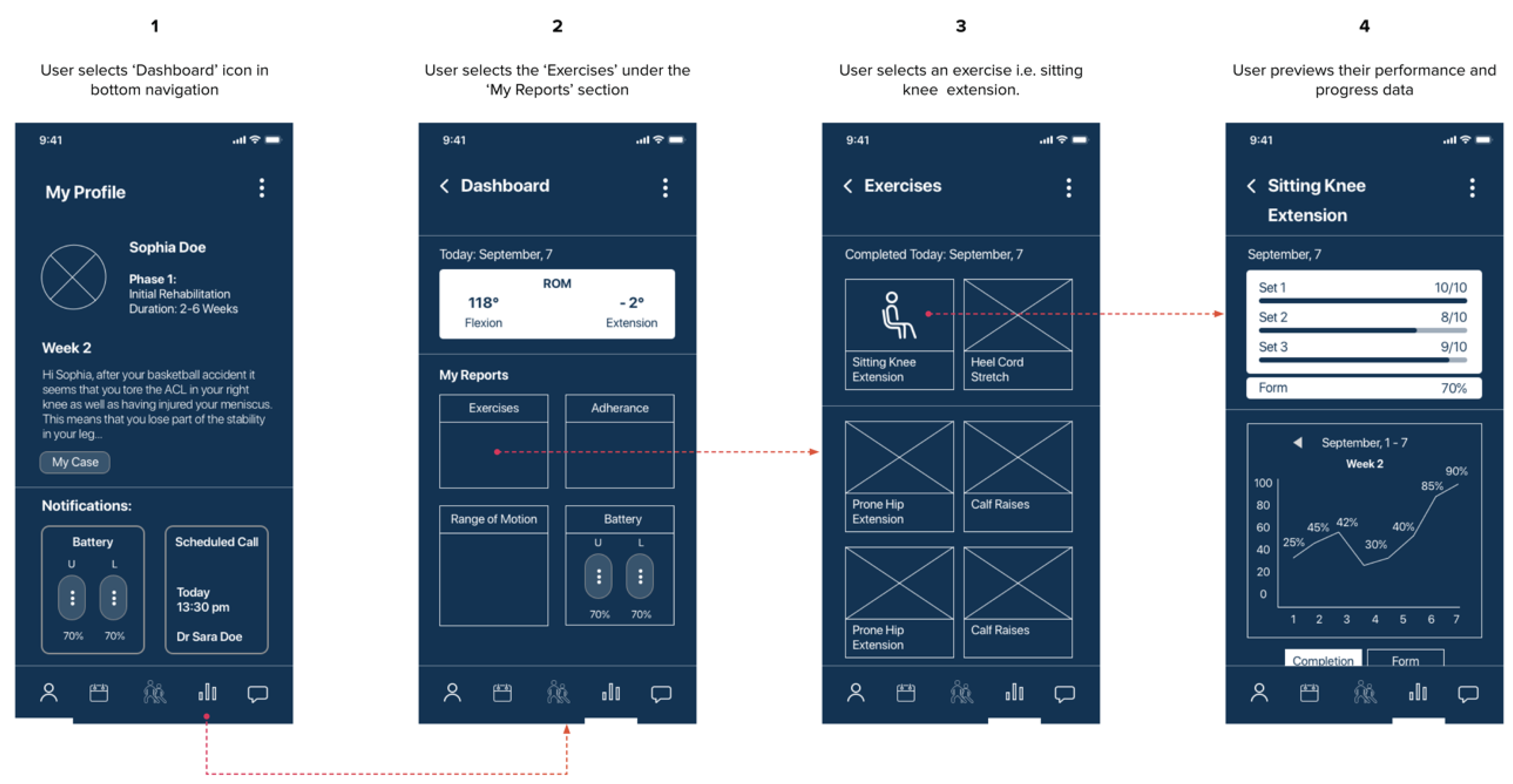
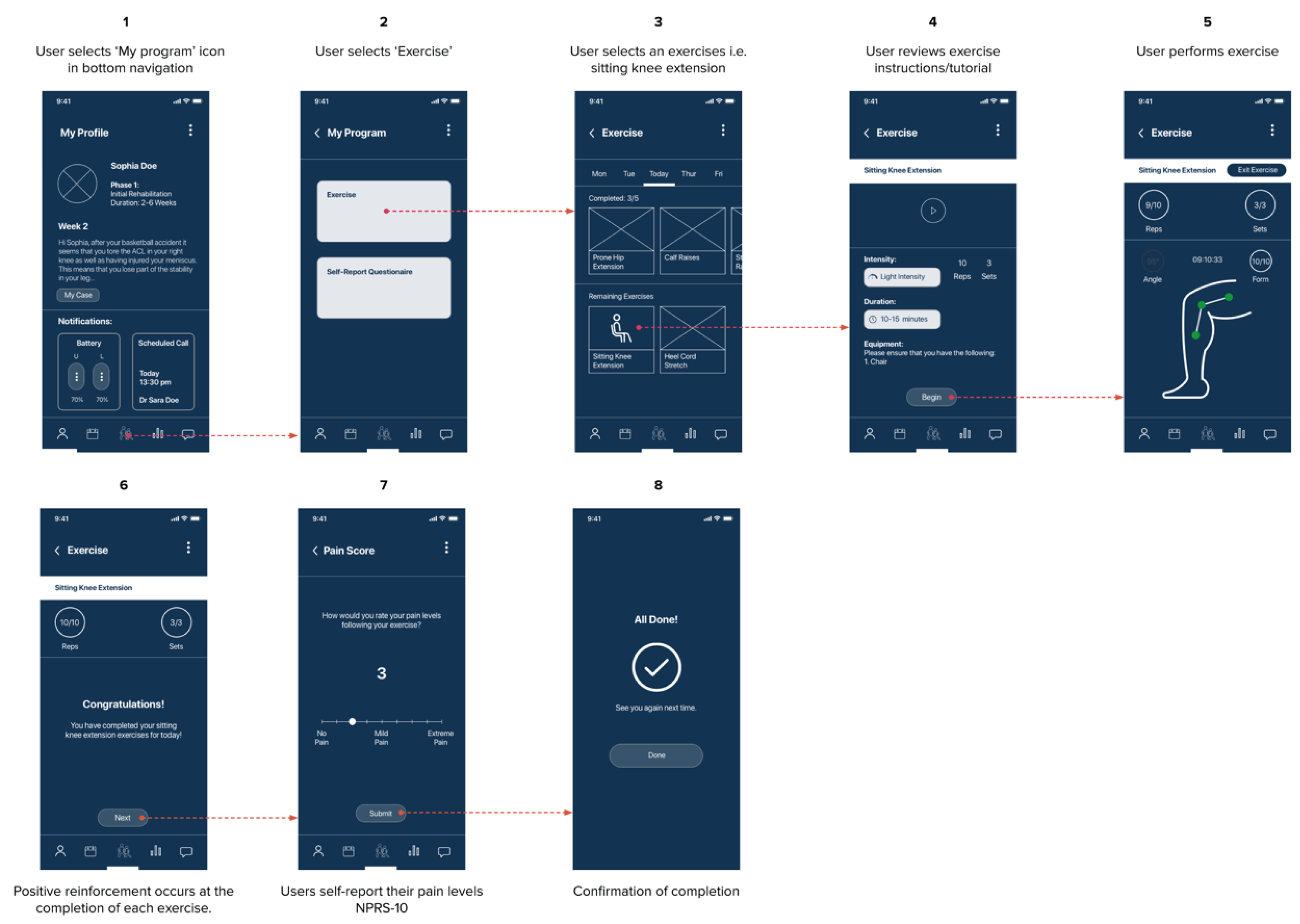
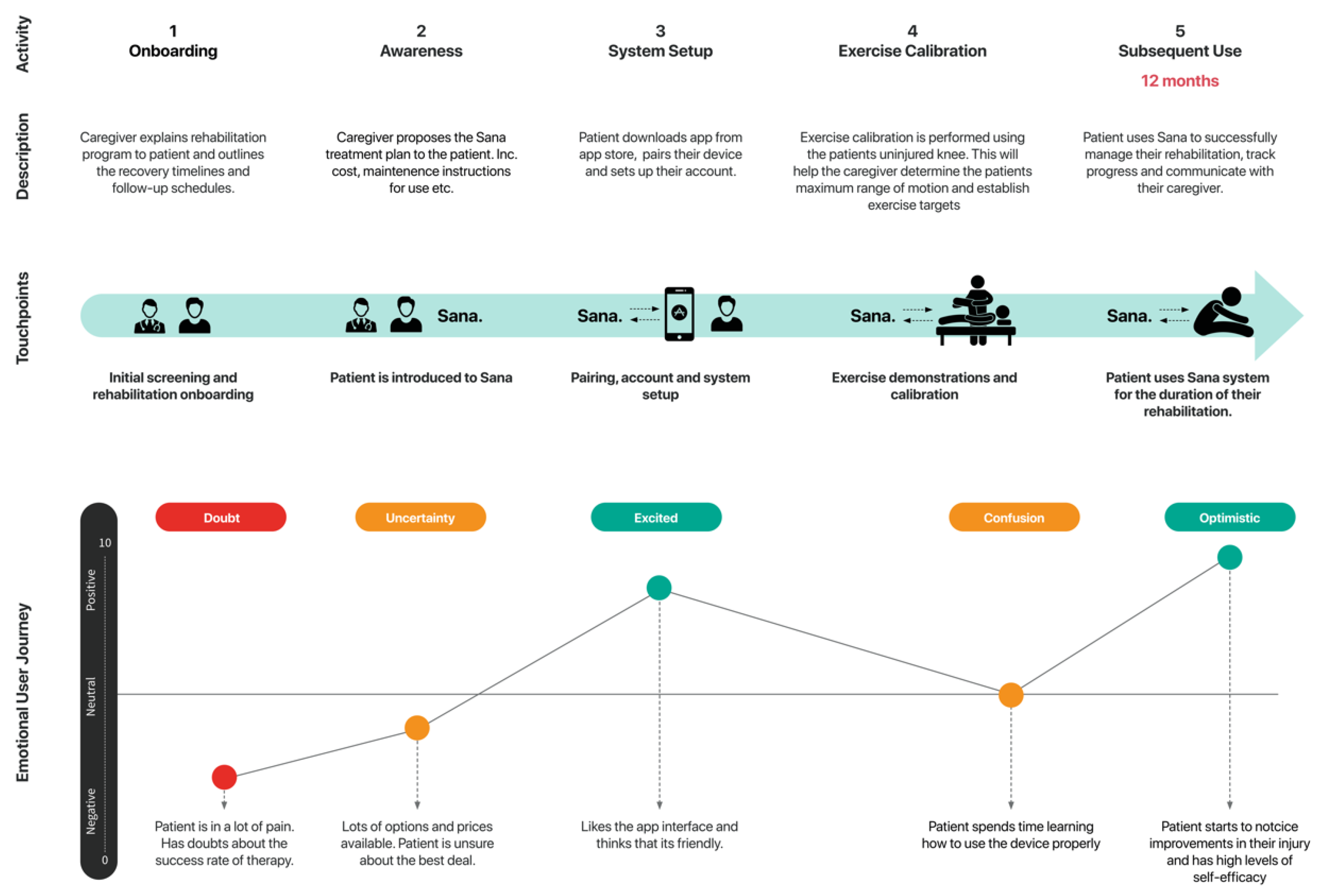
Patient User Journey: Post-Sana
- Action 1: Dashboard workflow: Prioritize one dashboard feature for the final system (i.e., exercise reports, range of motion reports or adherence reports) and produce sketch concepts.
- Action 2: Exercise workflow: Refine exercise workflow with an emphasis on AR visualization, gamification, and positive feedback. Feedback on the system’s interface was also provided, which was implemented in the next prototype iteration. The comments mainly centered around content hierarchy, navigation, and clarity of information presented within the interface.
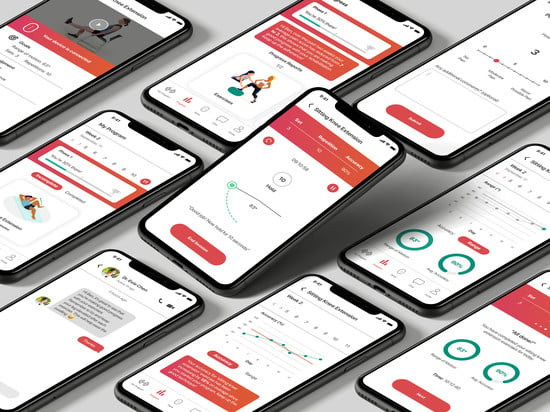
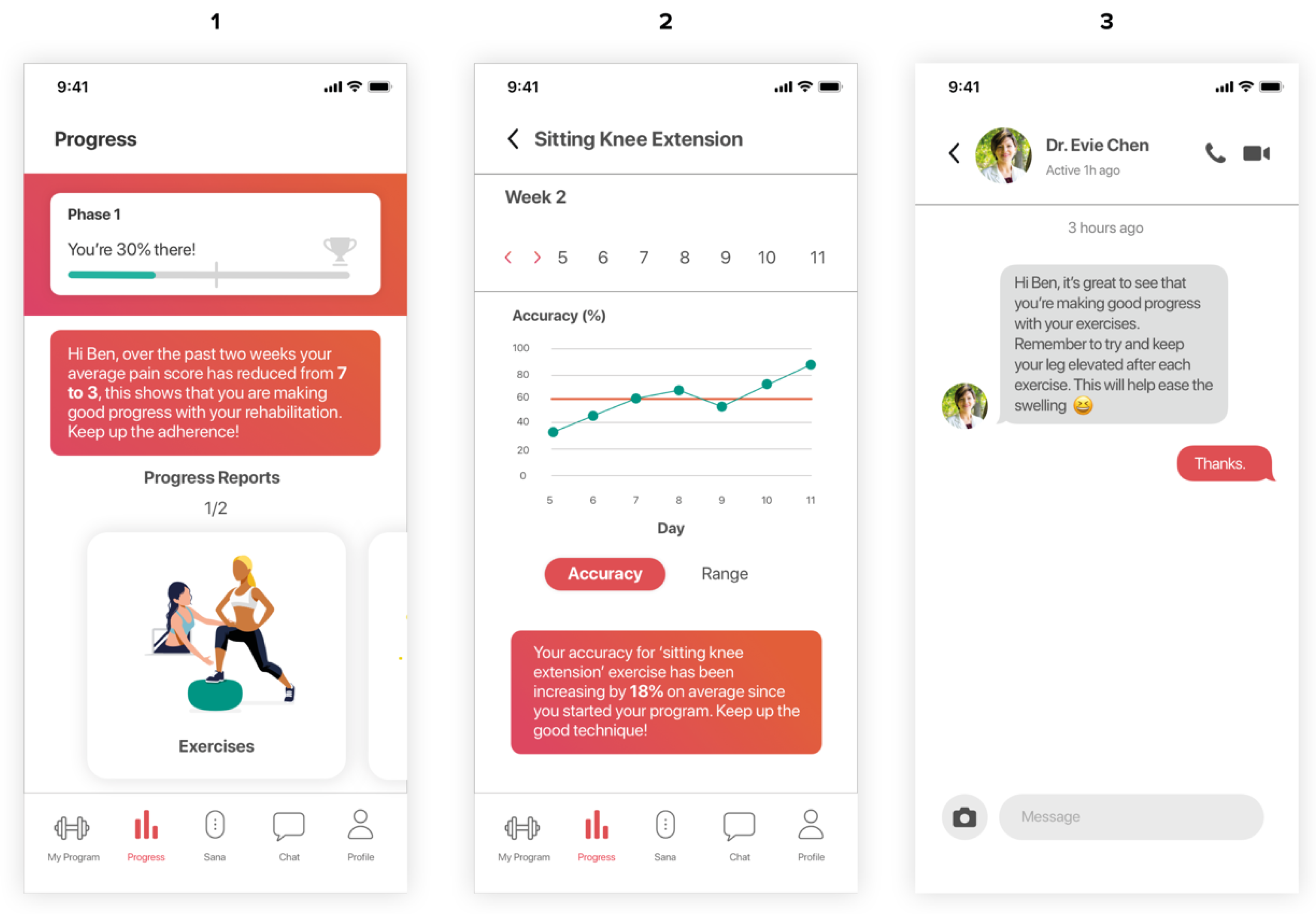
4. The Proposed System: Sana
4.1. Exercise Calibration
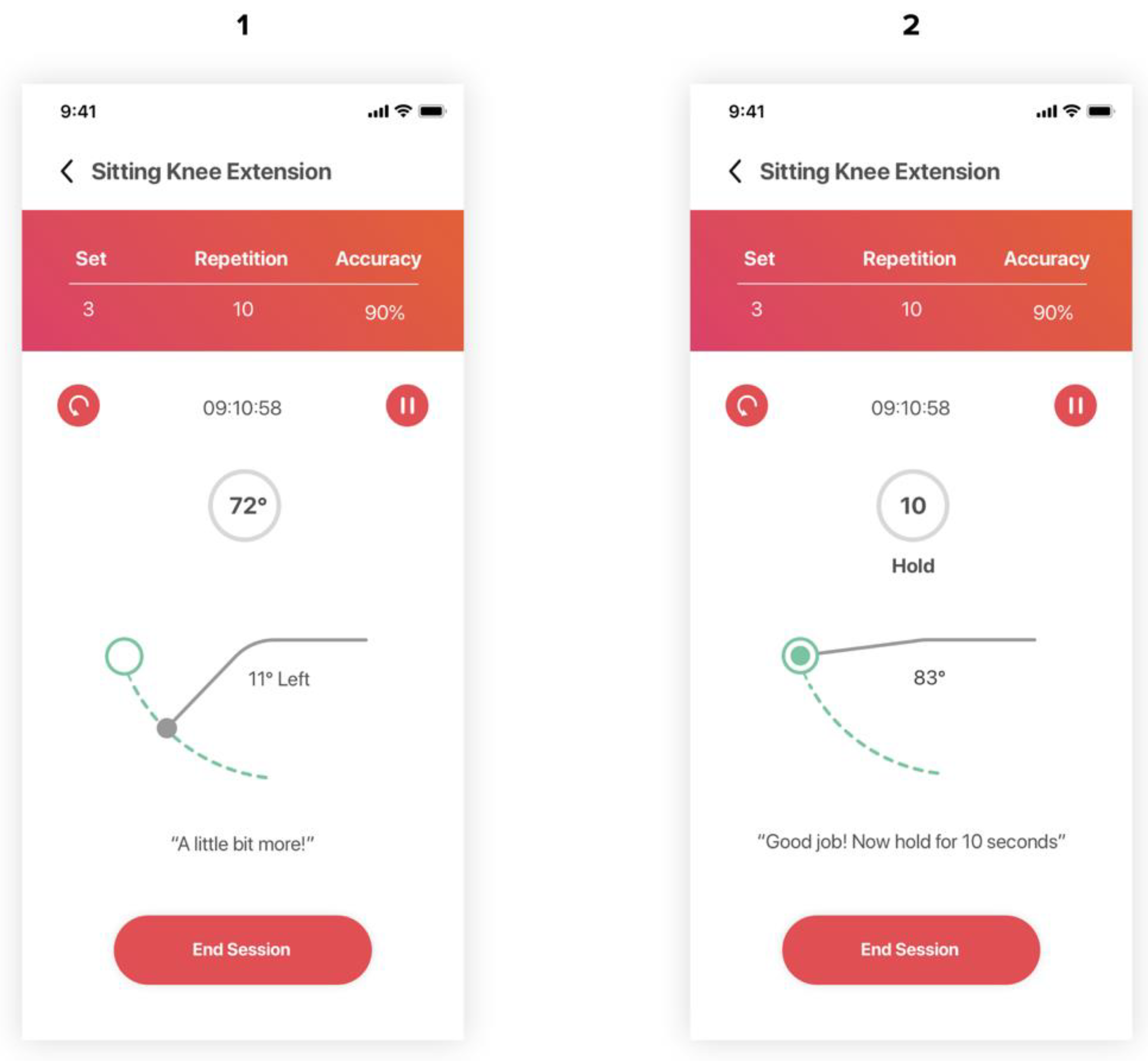
4.2. Integration of AR and Exercise Gamification
4.3. Progress and Performance Feedback
5. Conclusions
5.1. Study Limitations
5.2. Future Developments
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Joseph, A.; Collins, C.; Henke, N.; Yard, E.; Fields, S.; Comstock, R. A Multisport Epidemiologic Comparison of Anterior Cruciate Ligament Injuries in High School Athletics. J. Athl. Train. 2013, 48, 810–817. [Google Scholar] [CrossRef] [PubMed]
- Essery, R.; Geraghty, A.; Kirby, S.; Yardley, L. Predictors of adherence to home-based physical therapies: A systematic review. Disabil. Rehabil. 2016, 39, 519–534. [Google Scholar] [CrossRef] [PubMed]
- Comparison of the Clinical and Cost Effectiveness of Two Management Strategies for Non-Acute Anterior Cruciate Ligament (ACL) Injury: Rehabilitation Versus Surgical Reconstruction. Available online: https://ichgcp.net/clinical-trials-registry/NCT02980367 (accessed on 25 April 2020).
- Pietrosimone, B.; Seeley, M.K.; Johnston, C.; Pfeiffer, S.J.; Spang, J.T.; Blackburn, J.T. Walking Ground Reaction Force Post-ACL Reconstruction: Analysis of Time and Symptoms. Med. Sci. Sports Exerc. 2019, 51, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Tanwar, S.; Parekh, K.; Evans, R. Blockchain-based electronic healthcare record system for healthcare 4.0 applications. J. Inf. Secur. Appl. 2020, 50, 102407. [Google Scholar] [CrossRef]
- Kungwengwe, T. Business Model. BA Industrial Design and Technology; Brunel University London: London, UK, 12 May 2020. [Google Scholar]
- Adherence to Home Exercise Programs. Available online: https://www.physio-pedia.com/Adherence_to_Home_Exercise_Programs#cite_note-Wright-7 (accessed on 25 April 2020).
- Magee, D.J.; Zachazewski, J.; Quillen, W.; Manske, R.A. Pathology and Intervention in Musculoskeletal Rehabilitation, 2nd ed.; Elsevier Inc.: London, UK, 2016; pp. 16–19. [Google Scholar]
- Henderson, K.; Cole, J. The effects of exercise rehabilitation on perceived self-efficacy. Aust. J. Physiother. 1992, 38, 195–201. [Google Scholar] [CrossRef]
- Anterior Cruciate Ligament (ACL) Reconstruction. Available online: https://www.bupa.co.uk/health-information/knee-clinic/treatment-and-care/anterior-cruciate-ligament-acl-reconstruction (accessed on 25 April 2020).
- Rehabilitation Guidelines for Patients Undergoing Anterior Cruciate Ligament Repair (ACL). Available online: https://www.rnoh.nhs.uk/services/rehabilitation-guidelines (accessed on 17 November 2019).
- Brown, M.; O’Neill, N.; van Woerden, H.; Eslambolchilar, P.; Jones, M.; John, A. Gamification and Adherence to Web-Based Mental Health Interventions: A Systematic Review. JMIR Ment. Health 2016, 3, e39. [Google Scholar] [CrossRef] [PubMed]
- Tannous, H.; Istrate, D.; Benlarbi-Delai, A.; Sarrazin, J.; Idriss, M.; Tho, M.; Dao, T. Exploring various orientation measurement approaches applied to a serious game system for functional rehabilitation. In Proceedings of the 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Orlando, FL, USA, 16–20 August 2016; IEEE: New York, NY, USA, 2016; p. 16395741. [Google Scholar]
- Idriss, M.; Tannous, H.; Istrate, D.; Perrochon, A.; Salle, J.; Ho Ba Tho, M.; Dao, T. Rehabilitation- Oriented Serious Game Development and Evaluation Guidelines for Musculoskeletal Disorders. JMIR Serious Games 2017, 5, e14. [Google Scholar] [CrossRef] [PubMed]
- Mubin, O.; Alnajjar, F.; Jishtu, N.; Alsinglawi, B.; Al Mahmud, A. Exoskeletons with Virtual Reality, Augmented Reality, and Gamification for Stroke Patients’ Rehabilitation: Systematic Review. JMIR Rehabil. Assist. Technol. 2019, 6, e12010. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Man Li, K.; Neoh, E.; Zhang, H.; Khaw, X.; Fan, X.; Miao, C. Fun-Knee™: A Novel Smart Knee Sleeve for Total-Knee-Replacement Rehabilitation with Gamification. In Proceedings of the IEEE 5th International Conference on Serious Games and Applications for Health, Perth, Australia, 2–4 April 2017; IEEE: New York, NY, USA, 2017; p. 16946151. [Google Scholar]
- Egan, A.; Mahmood, W.; Fenton, R.; Redziniak, N.; Kyaw Tun, T.; Sreenan, S.; McDermott, J. Barriers to exercise in obese patients with type 2 diabetes. QJM 2013, 106, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Gunaydin, T.; Arslan, R.; Birik, B.; Cirak, Y.; Durustkan Elbasi, N. A Surface Electromyography Based Serious Game for Increasing Patient Participation to Physiotherapy and Rehabilitation Treatment Following Anterior Cruciate and Medial Collateral Ligaments Operations. In Proceedings of the IEEE 31st International Symposium on Computer-Based Medical Systems, Karlstad, Sweden, 18–21 June 2018; IEEE: New York, NY, USA, 2018; p. 17936736. [Google Scholar]
- Clausen, J.; Nahen, N.; Horstmann, H.; Lasch, F.; Krutsch, W.; Krettek, C.; Weber-Spickschen, T. Improving Maximal Strength in the Initial Postoperative Phase After Anterior Cruciate Ligament Reconstruction Surgery: Randomized Controlled Trial of an App-Based Serious Gaming Approach. JMIR Serious Games 2020, 8, e14282. [Google Scholar] [CrossRef] [PubMed]
- Deacon, M.; Parsons, J.; Mathieson, S.; Davies, T. Can Wii Balance? Evaluating a Stepping Game for Older Adults. IEEE Trans. Neural. Syst. Rehabil. Eng. 2018, 26, 1783–1793. [Google Scholar] [CrossRef] [PubMed]
- Cugelman, B. Gamification: What It Is and Why It Matters to Digital Health Behavior Change Developers. JMIR Serious Games 2013, 1, e3. [Google Scholar] [CrossRef] [PubMed]
- Tech Trends 2012: Elevate IT for Digital Business. Available online: https://www2.deloitte.com/content/dam/Deloitte/au/Documents/technology/deloitte-au-technology-tech-trends-2012.pdf (accessed on 9 May 2020).
- Exploitationware: On the Rhetoric of Gamification. From My “Persuasive Games” Column at Gamasutra. Available online: http://bogost.com/writing/exploitationware/ (accessed on 9 May 2020).
- Gliddon, E.; Lauder, S.; Berk, L.; Cosgrove, V.; Grimm, D.; Dodd, S.; Suppes, T.; Berk, M. Evaluating discussion board engagement in the MoodSwings online self-help program for bipolar disorder: Protocol for an observational prospective cohort study. BMC Psychiatry 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Digital NHS. Available online: https://digital.nhs.uk/ (accessed on 12 May 2020).
- How to Conduct Design Review Meetings That don’t Get Derailed. Available online: https://uxdesign.cc/how-to-conduct-design-review-meetings-that-dont-get-derailed (accessed on 10 April 2020).
- Lewis, J.; Sauro, J. Revisiting the Factor Structure of the System Usability Scale. J. Usability Stud. 2017, 12, 184–192. [Google Scholar]
- Turning Usability Testing Data into Action without Going Insane. Available online: https://www.toptal.com/designers/usability/turning-usability-testing-data-into-action (accessed on 25 April 2020).
- Card Sorting: Uncover Users’ Mental Models for Better Information Architecture. Available online: https://www.nngroup.com/articles/card-sorting-definition/ (accessed on 17 January 2020).
- 10 Usability Heuristics for User Interface Design. Available online: https://www.nngroup.com/articles/ten-usability-heuristics/ (accessed on 10 May 2020).
- Haladjian, J.; Bredies, K.; Brügge, B. KneeHapp Textile: A Smart Textile System for Rehabilitation of Knee Injuries. In Proceedings of the IEEE 15th International Conference on Wearable and Implantable Body Sensor Networks, Las Vegas, NV, USA, 4–7 March 2018; IEEE: New York, NY, USA, 2018; p. 17681609. [Google Scholar]
- Pereira, A.; Folgado, D.; Nunes, F.; Almeida, J.; Sousa, I. Using Inertial Sensors to Evaluate Exercise Correctness in Electromyography-based Home Rehabilitation Systems. In Proceedings of the IEEE International Symposium on Medical Measurements and Applications, Istanbul, Turkey, 26–28 June 2019; IEEE: New York, NY, USA, 2019; p. 18970423. [Google Scholar]






| Phase 1 | Phase 2 | Phase 3 |
|---|---|---|
| Initial Rehabilitation Phase (Duration: 2–6 weeks) | Recovery Rehabilitation Phase (Duration: 6–12 weeks) | Intermediate–Final Rehabilitation Phase (Duration: 12 weeks–1 year) |
|
|
|
| Question | Comments | Additional Information |
|---|---|---|
| What specific information is a patient given regarding the nature of their injury during initial consultation? | Patients will often be given information relating to their goals for that rehabilitation phase and restrictions. | None. |
| How often are patients called up for follow-up treatment? | Physiotherapists see their patients more frequently during the acute rehabilitation phase (1), and less frequently after that. | Phase 1 is where caregivers need to ensure that the patient is doing everything correctly. |
| How often do ACL reconstruction patients have to engage in physical therapy? | Patients need to perform exercises consistently during the acute rehabilitation phase. | The type of exercises a patient engages in will depend on the type of injury, severity, and where the tissue is damaged. When physiotherapists are deciding on patient exercises, they need to think about the tissue, healing time frames, and clinical indicators (i.e., adequate quad strength, full range of motion and weight bearing). |
| What are the various types of equipment that patients will receive to support them with exercises? | This varies depending on the type of injury and the exercises that the physiotherapist wants patients to perform. | None. |
| Does diet have an impact on a patient’s rehabilitation success rate? | Yes. | Diet is subjective. Your system should focus on rehabilitation exercises, improving efficacy, and monitoring the quality of exercises performed. |
| What type of metrics need to be collected to show that a patient is recovering successfully? | Rotation, extension, bend, velocity, and power are important metrics. | The quantitative metrics we use are strength, range of motion, and swelling. Quality of movement is also important during exercises. Are they weight shifting evenly? It is also useful to keep track of whether a patient’s pain levels are going down. |
| Do patients schedule their own appointments or is this done by the healthcare provider? | No. In private healthcare settings, physiotherapists tend to have a treatment plan; this involves mapping out when the patient will need to visit for follow-up care. Treatment plans are always set in collaboration with the patient during the initial consultation. | None. |
| What kinds of advice/medication will a patient be given regarding pain and swelling management? | Patients will be given advice regarding swelling management (i.e., how long they need to apply an ice pack on their injury). | In the acute phase, it is important that the patient does not receive too much anti-inflammatory medication. |
| Are the different phases of recovery fixed for every single post-ACL reconstruction patient? | Depends on the patient’s level of injury. | Patients should not push too hard during exercise. It is important to perform exercises correctly rather than too fast and not use correct form. |
| How do patients monitor their own performance with rehabilitation? | They cannot. They only find out about their performance during follow-up consultation | None. |
| Cards/Potential System Features | Groupings and Labels | ||||
|---|---|---|---|---|---|
| Settings/Wearable Device/FAQs | Exercise/Rehabilitation/Therapy | Profile/About Me | Home Page | Dashboard | |
| Instructions on systems set-up | Providing feedback on my pain levels | Personal details | Setting exercise reminders | My exercise performance | |
| Syncing my Fitbit/fitness tracker | Guidance on how to complete an exercise | Prescribed medication and dosage information | View my rewards and achievements | Adherence levels to my rehabilitation program | |
| Detailed product information (e.g., battery life) | Congratulatory message that I have completed an exercise | Summary of my injury and expectations of recovery | |||
| Real-time performance feedback | Adherence levels to my rehabilitation program | ||||
| Challenges | Ideas and Improvements |
|
|
| Likes | Questions |
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kungwengwe, T.; Evans, R. Sana: A Gamified Rehabilitation Management System for Anterior Cruciate Ligament Reconstruction Recovery. Appl. Sci. 2020, 10, 4868. https://doi.org/10.3390/app10144868
Kungwengwe T, Evans R. Sana: A Gamified Rehabilitation Management System for Anterior Cruciate Ligament Reconstruction Recovery. Applied Sciences. 2020; 10(14):4868. https://doi.org/10.3390/app10144868
Chicago/Turabian StyleKungwengwe, Tanaka, and Richard Evans. 2020. "Sana: A Gamified Rehabilitation Management System for Anterior Cruciate Ligament Reconstruction Recovery" Applied Sciences 10, no. 14: 4868. https://doi.org/10.3390/app10144868
APA StyleKungwengwe, T., & Evans, R. (2020). Sana: A Gamified Rehabilitation Management System for Anterior Cruciate Ligament Reconstruction Recovery. Applied Sciences, 10(14), 4868. https://doi.org/10.3390/app10144868