Abstract
Proximal femoral varization osteotomy is a well-established surgical procedure in children with severe hip problems. This study aimed to evaluate the fixation stability and stiffness of two new implant systems. A biomechanical testing model was created with a total of 12 synthetic femora. Proximal femoral varization osteotomy was performed in every femur, and the synthetic femora were fixed with two different implant systems (PediLoc Locking Proximal Femur Plate System versus PediLoc Locking Cannulated Blade Plate System; OrthoPediatrics, Warsaw, IN, USA). The average torsional stiffness of the locking plate group was higher than for the cannulated blade plate group. Differences in internal and external rotations were seen between the two groups, but they were not significant. Using the tested implants in severe osteoporotic bones might show other results. Therefore, it might be helpful to use the locking plate system in osteoporotic bones and in cases of revision operations where stability is of critical focus.
1. Introduction
Proximal femoral varization osteotomy is a well-established surgical procedure in children with different hip problems, such as developmental dysplasia of the hip (DDH), containment in Perthes disease, and hip dislocation or subluxation in severe cerebral palsy (CP) [1,2,3,4,5,6,7,8,9]. In the literature, older implant systems had higher complication rates and longer time to bone union [8].
To simplify the procedure and to stabilize the fixation, new blade plate systems were developed [9]. Given the low complication rates and postoperative mobilization under full weight bearing, fixed-angle blade plates became the most used implant over time [2,4,5,6].
Clinical studies with the new implant systems comparing blade plate and screw-side plate show generally good results [2,10,11,12]. Jain et al. described a rate of implant-related fractures of 2.5% in all patients, and they found no significant difference between the blade plate and screw-side plate [11]. Trainee surgeons had preference for cannulated blade plate when learning proximal femoral osteotomy, analyzing cannulated blade plate versus fixed angled blade plate. The fixed angled blade plate group had a higher prevalence of technical errors. However, radiological results were similar regarding migration and neck shaft angle [12]. In contrast, little is known about the biomechanical stability of the new implant systems used in proximal femoral varization osteotomy [1,2,3].
Synthetic bones are often used as a substitute for human tissue in biomechanical in vitro investigations. In certain applications, they show good agreement in terms of macroscopic mechanical properties and anatomy [13]. A further advantage is their standardization and the associated low variance.
This study aimed to evaluate fixation stability and stiffness of two new implant systems (PediLoc Locking Proximal Femur Plate System versus PediLoc Locking Cannulated Blade Plate System) using a synthetic bone model.
2. Materials and Methods
2.1. Specimens
A total of 12 synthetic femora with medium-sized and left-side geometry (#3403, 4th generation, Sawbone, Pacific Research Laboratories Inc., Vashon, WA, USA) bones were used for the study. The specimens were divided into two groups of patients using PediLoc Locking Proximal Femur Plate System (F-PL group) and PediLoc Locking Cannulated Blade Plate System (G-CBP group).
On every femur, proximal femoral varization osteotomy was performed by a surgeon and in accordance to the user manual. The closing was 10° from the medial side: five femora were fixed with a PediLoc Locking Proximal Femur Plate (size 90° × 3.5-mm plate, 12-mm offset, 3 holes, OrthoPediatrics, Warsaw, IN, USA) and seven with a PediLoc Locking Cannulated Blade Plate System (size 90° − 50 × 10 × 3, OrthoPediatrics, Warsaw, IN, USA). The proximal end of the prepared specimens was embedded into a metal shell using cold-curing three-component resin (Rencast FC52/53 Isocyanate, FC53 Polyol, Füller DT 082, gössl&pfaff GmbH, Karlskron/Braulach, Germany).
2.2. Mechanical Testing
Biomechanical investigations were carried out on a servohydraulic material testing machine (MTS MiniBionix I, Model 858, Eden Prairie, MN, USA) and a custom-made experimental setup. Two different loading scenarios were selected. First, the torsional stiffness of all specimens was investigated without harming them. After axial torsion, the so-called Hayes fall investigations were carried out. The experimental setup allowed measuring the force applied to fracture the proximal femur or damage the implant, and was based on the Hayes fall [14,15].
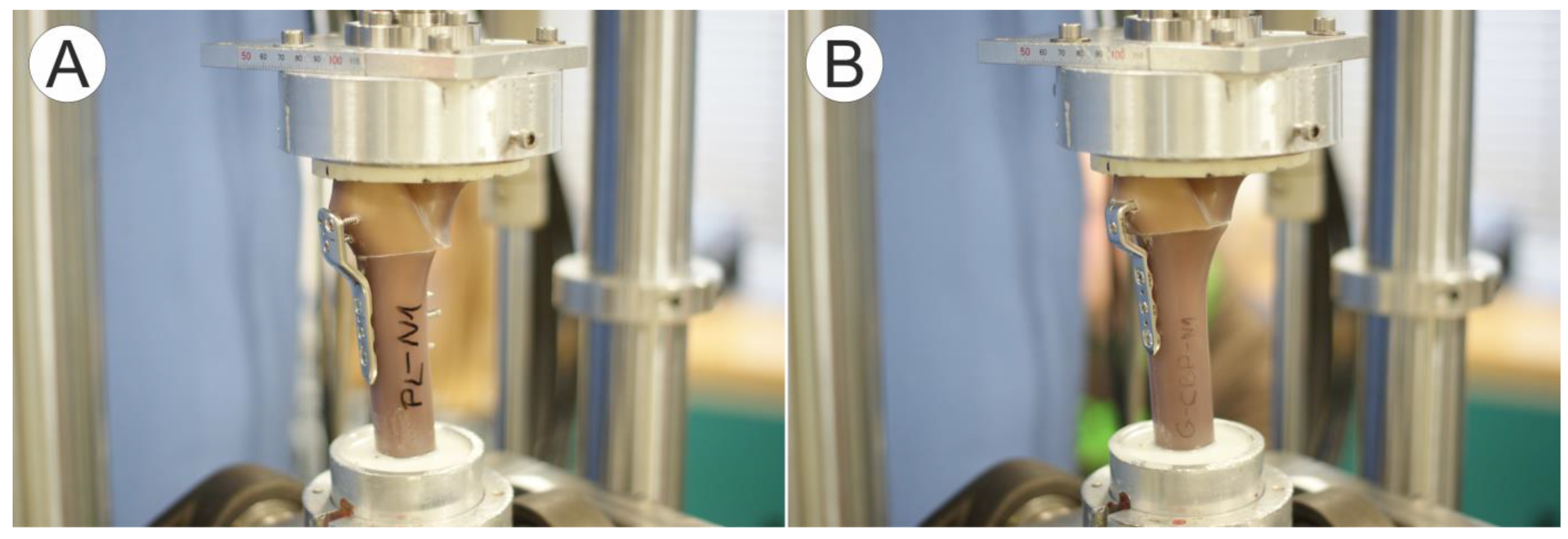
2.3. Axial Torsion
The synthetic femora were mounted between two universal joints to apply a purely torsional load (Figure 1). The distal part of the specimens was fixed to the lower cardan joint. The load was applied to the specimen via the second cardan joint at the top. The specimens were axially loaded with a static force (compression) of 100 N. First, a cyclic internal rotation was performed by introducing a torsional moment of 0 to 3 Nm into the proximal end of the specimens. After 100 cycles of internal rotation, an external rotation with 100 cycles was performed with the same load. The specimens were not harmed during the torsional test. Time, cycles, angle, torque, and force were recorded with a sampling rate of 1 kHz.
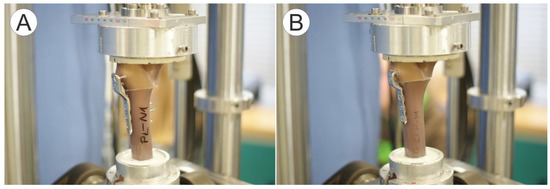
Figure 1.
Test setup for axial torsion on the material test machine with mounted synthetic femora specimen: (A) F-PL with PediLoc Locking Proximal Femur Plate and (B) G-CBP with PediLoc Locking Cannulated Blade Plate System.
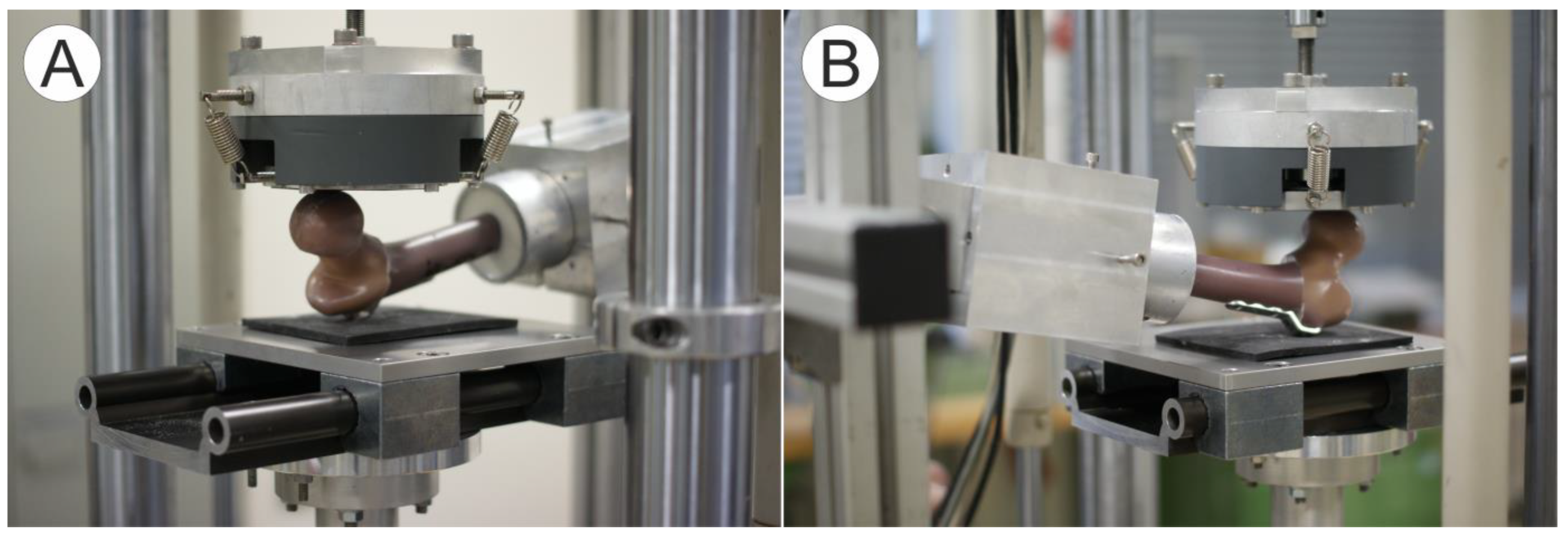
2.4. Proximal Femoral Strength
The proximal strength of the osteotomized synthetic femora was determined using a custom-made setup designed to simulate a sideways fall onto the greater trochanter region [14,15]. The distal embedding was free to rotate around the mediolateral axis. The specimens were positioned in the assembly with 15° internal rotation and 10° adduction (Figure 2). Proximally, the trochanter lay on a 6-mm thick rubber mat. The table under the rubber mat can be moved in the proximal-distal direction. The force and torque sensors of the material testing machine were located below the table. The force was applied directly to the femoral head via a sliding plate that permitted translational movements in the frontal plane of the femur. A position-controlled test protocol was used. First, a preload of 20 N was applied. The actuator then moved downward at a traversing speed of 0.5 mm/s. The abort criterion was manual after the failure of the sample. The transversal position, force, and time were recorded at 1 kHz.
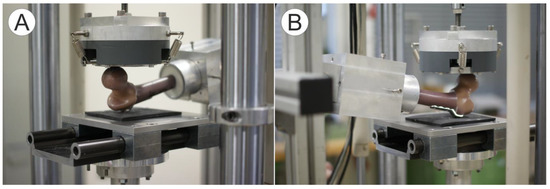
Figure 2.
Test setup for the determination of the proximal femoral strength on the material test machine with mounted synthetic femora specimen. (A) Experimental setup to determine the proximal femoral strength based on the Hayes fall. The force is applied on the femoral head via a sliding plate that permits translational movements. The greater trochanter lies on a 6-mm thick rubber mat. The table under the rubber mat can be moved in the proximal–distal direction. (B) In the left part of the picture, the aluminum shell with the distal embedding is shown. The embedding can be rotated about the mediolateral axis. The specimens are positioned with internal rotation of 15° and an adduction of 10°.
2.5. Statistics
Due to the small sample size of the groups, the statistics were carried out with a Mann–Whitney U test for unrelated samples using R software (R version 3.5.1, The R Foundation for Statistical Computing, Vienna, Austria). A significance level of α = 0.05 was applied.
3. Results
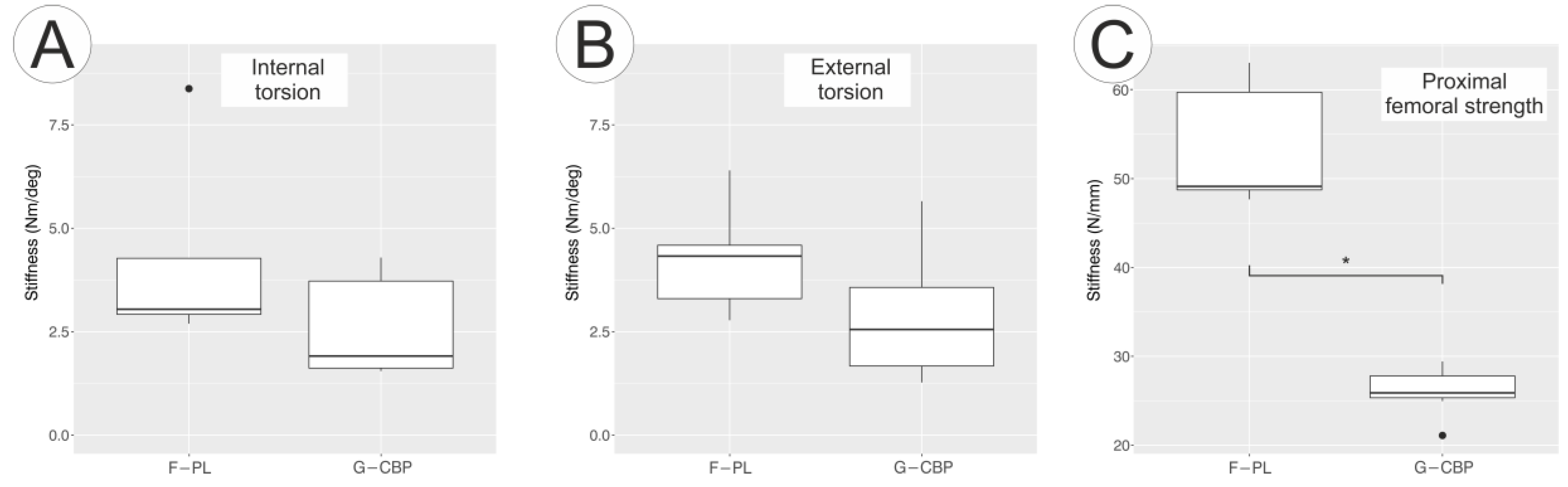
3.1. Axial Torsion
All synthetic femora could be tested for axial torsion without causing damage. The average torsional stiffness of the F-PL group was 4.26 ± 2.38 Nm/deg for internal rotation and 4.28 ± 1.40 Nm/deg for external rotation (Figure 3A). For the G-CBP group, the average torsional stiffness was 2.63 ± 1.23 Nm/deg for internal rotation and 2.85 ± 1.61 Nm/deg for external rotation (Figure 3B). The differences for internal and external rotations were not significant between the two groups.
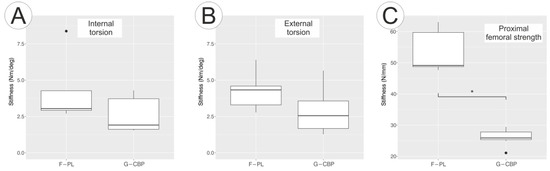
Figure 3.
Box plots of the torsional stiffness for (A) internal, (B) external rotations, and (C) proximal femoral strength for both subgroups.
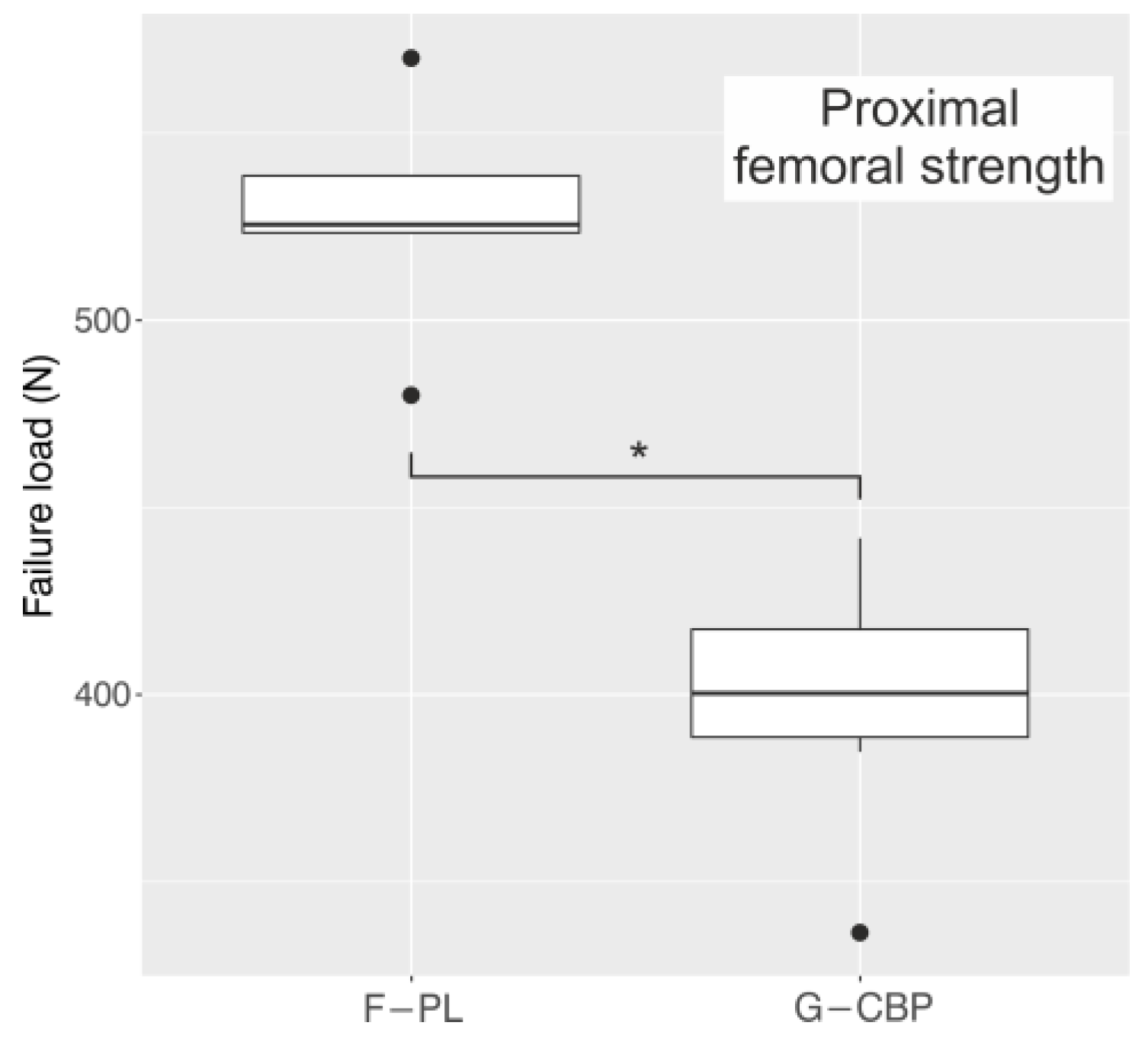
3.2. Proximal Femoral Strength
All specimens of both groups showed plastic deformation of the osteosynthesis plates at the end of the tests. The bone screws did not tear out, and the synthetic bones were not fractured.
The mean stiffness of the F-PL group was 53.9 ± 6.4 N/mm and that of the G-CBP group was 26.1 ± 2.7 N/mm (Figure 3C). This difference was also significant (p = 0.018). The mean force for the F-PL group and G-CBP group where implant failure occurred was 554 ± 71 N and 399 ± 33 N, respectively (Figure 4). This difference was significant (p = 0.003).
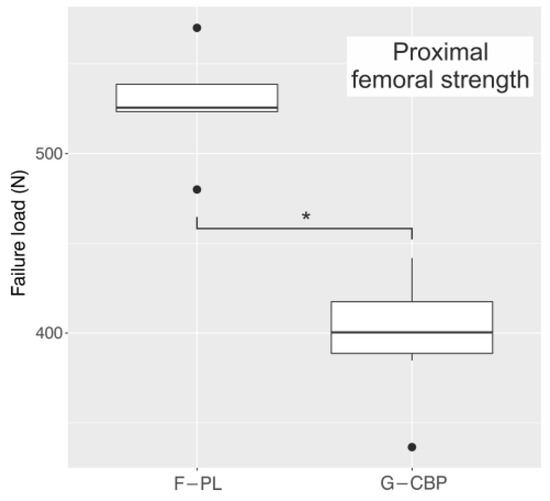
Figure 4.
Box plots of the load to failure of the proximal femora for both tested groups.
4. Discussion
In this biomechanical comparative study, we investigated the torsional stiffness for internal and external rotations and the proximal strength of the osteotomized synthetic femora for two implant systems (PL and CBP). The average torsional stiffness of the F-PL group was higher than that for the G-CBP group. Differences in internal and external rotations were found between the two both groups. However, this difference was not significant (Figure 3A,B). Moreover, the F-PL system has proximal locking screws to ensure that bending moments were further reduced during loading.
The proximal femoral strength of the osteotomized synthetic femora was tested with a setup to simulate a sideways fall onto the great trochanteric region. All specimens (both groups) showed plastic deformation of the implants at the end of the testing. No fractured synthetic bones or torn screws were seen in any group. The mean force where implant failure occurred was significantly higher in the F-PL group than in the G-CBP group. That the F-PL plate has a significantly higher rigidity and load to failure can be due to its construction. With 19 mm, the F-PL is 8 mm wider in the proximal and highly stressed gap area than the G-CBP. Both plates have approximately the same 3-mm thickness. This results in a higher moment of inertia of the F-PL, which is reflected in the results of the proximal strength. That there were no significant differences in torsion can be due to the fact that the G-CBP has a cannulated blade plate.
A recent study has shown that the design of the blade plate is relevant for stability [16]. After the addition of a proximal screw, the pullout strength increased even if the axial loading properties of the blade plate did not increase [16]. Considering these and our results, we suspect that design modifications might influence biomechanical results, and we hypothesize that adding a screw to the blade plate will not necessarily lead to better results. Further investigation might be helpful.
The fourth-generation synthetic femoral sawbones were used for testing. In a previous study, these femoral sawbones showed generally good agreement in terms of mean anatomy and macroscopic mechanical properties [13]. They are standardized and have low variance because of their biomechanical behavior. As regards testing, we expect comparable good results in vivo, as previously described [4,9]. However, most varization operations are performed in growing children [8,11,12]. The diversity of the growing skeleton cannot be represented by the sawbones used. Due to ethical consideration, we would disclaim interventional clinical trials analyzing stability with pediatric patients. Further studies, for example, on failed implants after osteotomy of the femur (in vivo) might help us better understand the stability and stiffness of the implants used.
A typical indication for the operation is coxa valga and excessive anteversion in spastic CP [2,3,12]. In severe cases, the hip is subluxated or luxated, and additive soft tissue operation is necessary [3]. Younger patients are often between 4 and 8 years [3]. The synthetic femora used cannot be representative for this pathologic anatomic situation. Furthermore, these patients have osteoporotic bone and reduced state of health, causing problems during treatment. This has to be investigated further in vivo.
In this study, comparable results were described in both groups. Using the tested implants in severe osteoporotic bones might show other results. Torn screws or fractured bones might occur. Concerning our results, we decided to use the F-PL in osteoporotic bones and in cases of revision operations. However, further biomechanical and in vivo tests in osteoporotic bones are necessary.
One further limitation of the study is the simplification of the loads that actually affect the musculoskeletal system. No combined load scenarios were applied, which do not fully correspond to reality, but facilitates the interpretation and comprehensibility of the results. However, the simulation of a sideways fall on the greater trochanter region is a frequently used method to examine the load capacity in the area of the osteotomy gap [14,15].
The results of this study showed that it is not possible to make a statement about possible intra- and postoperative complications. Blood loss, operation time, delayed union, implant loosening, and wound infections are typical parameters that should be evaluated in further comparative in vivo studies. Radiographic analyses of changes in containment should also be evaluated. In regard to existing studies, we expect comparable good results for these parameters [9,11,12].
Implant-related fractures along the two different implant systems (blade plate versus screw side plate) have been evaluated [11]. A previous study showed that no observed significant differences [11] may support our results on stiffness and stability. Therefore, differences in the design of the plates do not necessarily lead to significant differences in stability, even if we must await further studies with our two implant systems in vivo before making a definitive statement.
The correlation between surgeon experience and operative results is well explored [12]. All osteotomies in this study were performed by a well-experienced senior surgeon to prevent learning curve effects.
In a study analyzing CBP versus fixed angled blade plate, trainee surgeons were found to have preference for CBP when learning proximal femoral osteotomy [11]. In the present study, we decided to use the CBP for our trainee surgeons in their first year. Severe cases, such as osteoporotic bones and the use of PL, are reserved to senior surgeons in our department.
In conclusion, the average torsional stiffness of the locking plate group was higher than for the cannulated blade plate group. Differences in internal and external rotations were seen between the two groups, but they were not significant. Using the tested implants in severe osteoporotic bones might show other results. Therefore, it might be helpful to use the locking plate system in osteoporotic bones and in cases of revision operations where stability is of critical focus.
Author Contributions
Conceptualization, K.R. and F.G.; methodology, K.R., F.G., B.W., and M.E.; software, M.S. and B.W.; validation M.S. and B.W.; operation/implantation, F.G. and P.P.; biomechanical testing, M.S. and B.W.; data curation, B.W. and M.S.; writing—original draft preparation, K.R., B.W., and M.S.; writing—review and editing, K.R., B.W., and M.S.; visualization, B.W. and M.S.; supervision, B.W.; funding acquisition, F.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We thank Robert Martin from OrthoPediatrics (now NuVasive Germany GmbH, Bremen, Germany) for supporting our study with the used implants and sawbones. We acknowledge support by the German Research Foundation (DFG) and the Open Access Publication Fund of Hannover Medical School (MHH).
Conflicts of Interest
All authors declare that we received implants and sawbones from Robert Martin, OrthoPediatrics, Warsaw, IN, USA, for this study. The sponsors had no role in the design, execution, interpretation, or writing of the study.
References
- Thielemann, F.; Schneider, A. Long-term management results of Pemberton’s ilium osteotomy in combination with inter-trochanter derotation-varisation osteotomy in hip dysplasia of childhood. Z Orthop. Ihre Grenzgeb. 2003, 141, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Rutz, E.; Brunner, R. The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J. Pediatr. Orthop. 2010, 30, 726–731. [Google Scholar] [CrossRef] [PubMed]
- Eilert, R.E.; MacEwen, D. Varus derotational osteotomy of the femur in cerebral palsy. Clin. Orthop. Relat. Res. 1977, 125, 168–172. [Google Scholar] [CrossRef]
- Zhou, L.; Camp, M. Cannulated, locking blade plates for proximal femoral osteotomy in children and adolescents. J. Child. Orthop. 2015, 9, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Beauchesne, R.; Miller, F. Proximal femoral osteotomy using the AO fixed-angle blade plate. J. Pediatr. Orthop. 1992, 12, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Hau, R.; Dickens, D.R.V. Which implant for proximal femoral osteotomy in children? A comparison of the AO (ASIF) 90° fixed-angle blade plate and the Richards intermediate hip screw. J. Pediatr. Orthop. 2000, 20, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Maranho, D.A.; Pagnano, R.G. Tension band wiring for proximal femoral varus osteotomy fixation in children. Medicine 2014, 93, e61. [Google Scholar] [CrossRef] [PubMed]
- Canale, S.T.; Holand, R.W. Coventry screw fixation of osteotomies about the pediatric hip. J. Pediatr. Orthop. 1983, 3, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Grant, A.D.; Lehman, W.B. Cannulated blade plate for proximal femoral varus osteotomy. Clin. Orthop. Relat. Res. 1990, 259, 111–113. [Google Scholar] [CrossRef]
- Heiner, A.D.; Brown, T.D. Structural properties of a new design of composite replicate femurs and tibia. J. Biomech. 2001, 34, 773–781. [Google Scholar] [CrossRef]
- Jain, A.; Thompson, J.M. Implant-related fractures in children with proximal femoral osteotomy: Blade plate versus screw-side plate construct. J. Pediatr. Orthop. 2016, 36, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Camp, M. Proximal femoral osteotomy in children with cerebral palsy: The perspective of the trainee. J. Child. Orthop. 2017, 11, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.P.; Chong, A.C.M. Mechanical evaluation of large-size fourth-generation composite femur and tibia models. Ann. Biomed. Eng. 2010, 38, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Beckmann, J.; Ferguson, S.J. Femoroplasty-augmentation of the proximal femur with a composite bone cement-feasibility, biomechanical properties and osteosynthesis potential. Med. Eng. Phys. 2007, 29, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.G.; Lowet, G. Assessment of the strength of proximal femur in vitro: Relationship to femoral bone mineral density and femoral geometry. Bone 1997, 20, 213–218. [Google Scholar] [CrossRef]
- Ruzbarsky, J.J.; Swarup, I. Biomechanical comparison of two pediatric blade plate designs in proximal femoral osteotomies. HSS J. 2020, 16, 81–85. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).