Salivary Redox Biomarkers in the Course of Caries and Periodontal Disease
Abstract
1. Saliva
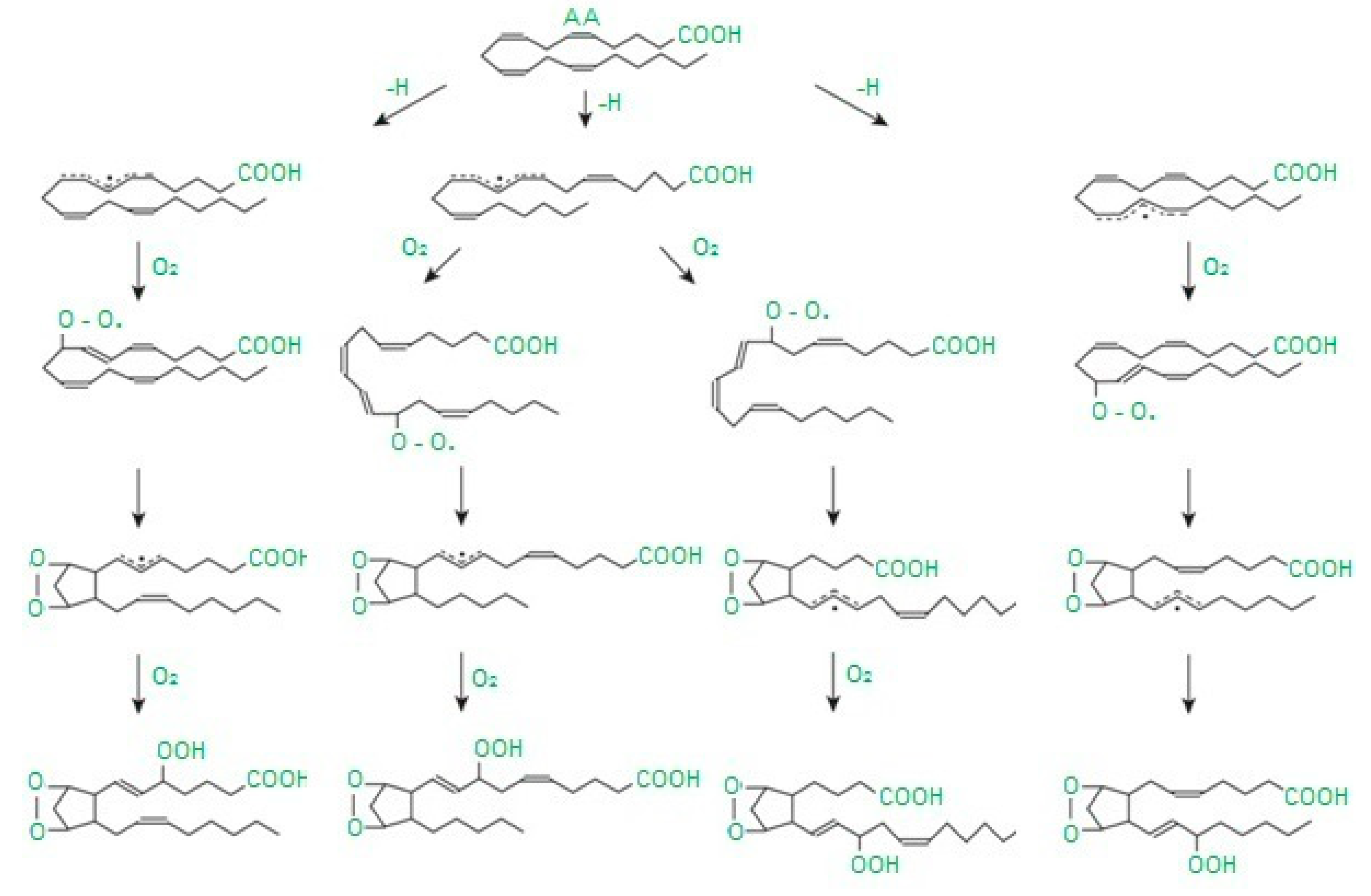
2. Oxidative Stress
3. Oxidative Stress Biomarkers
4. Antioxidant Defense
5. Materials and Methods
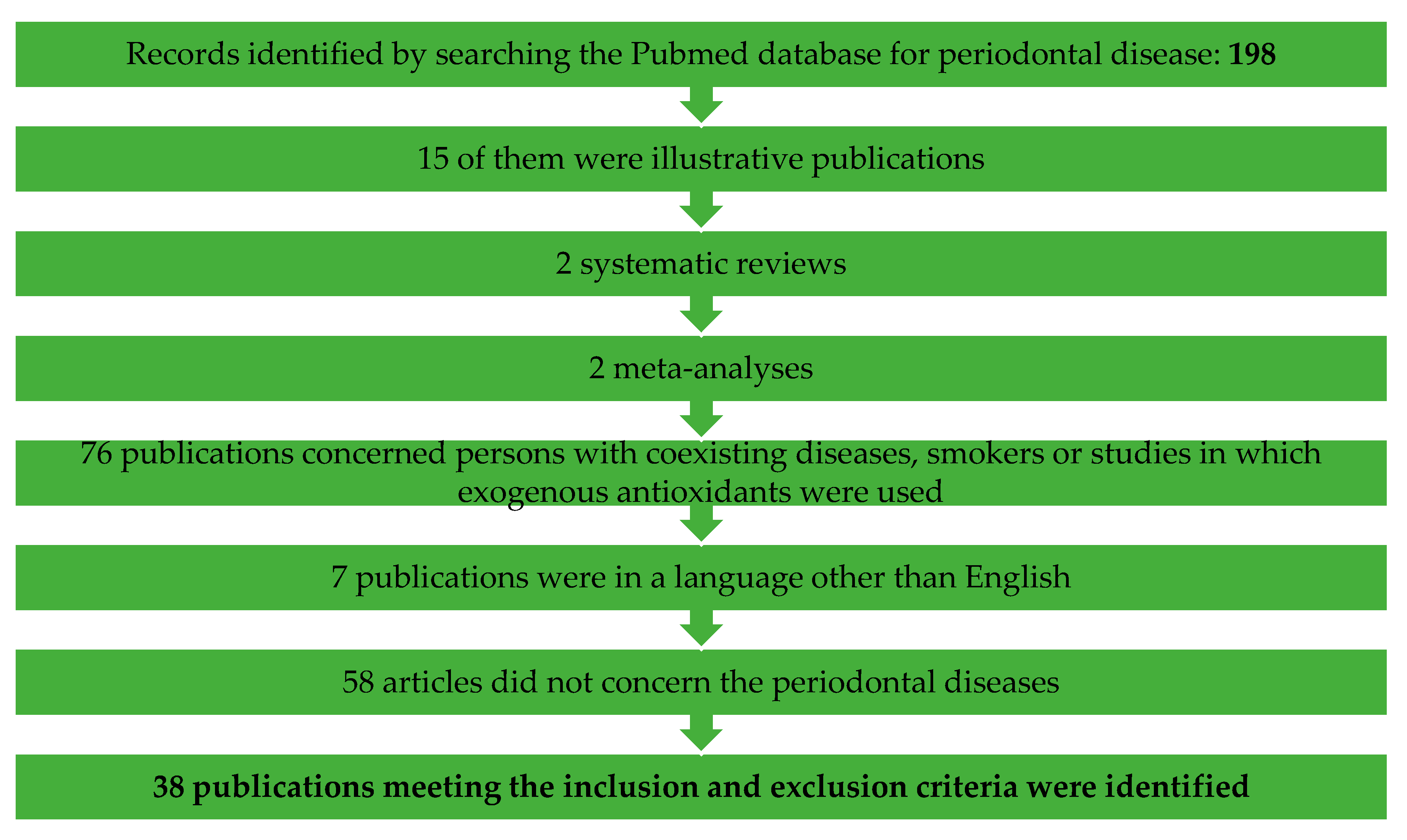
5.1. Searching Strategy
5.2. Inclusion and Exclusion Criteria
- the study group consisting of individuals with caries/periodontitis;
- subjects of the study refrained from taking antibiotics, antioxidants or any other medicines;
- evaluation of at least one oxidative stress biomarker in the saliva;
- the control group consisting of caries-free/periodontally healthy individuals;
- individuals qualified for both the study and control group were generally healthy;
5.3. Variables Recorded
6. Results
7. Caries
8. Periodontitis
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Klimiuk, A.; Maciejczyk, M.; Choromańska, M.; Fejfer, K.; Waszkiewicz, N.; Zalewska, A. Salivary Redox Biomarkers in Different Stages of Dementia Severity. J. Clin. Med. 2019, 8, 840. [Google Scholar] [CrossRef] [PubMed]
- Skutnik-Radziszewska, A.; Maciejczyk, M.; Fejfer, K.; Krahel, J.; Flisiak, I.; Kołodziej, U.; Zalewska, A. Salivary Antioxidants and Oxidative Stress in Psoriatic Patients: Can Salivary Total Oxidant Status and Oxidative Status Index Be a Plaque Psoriasis Biomarker? Oxidative Med. Cell. Longev. 2020, 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Choromańska, M.; Klimiuk, A.; Kostecka-Sochoń, P.; Wilczyńska, K.; Kwiatkowski, M.; Okuniewska, N.; Waszkiewicz, N.; Zalewska, A.; Maciejczyk, M. Antioxidant Defence, Oxidative Stress and Oxidative Damage in Saliva, Plasma and Erythrocytes of Dementia Patients. Can Salivary AGE be a Marker of Dementia? Int. J. Mol. Sci. 2017, 18, 2205. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Żebrowska, E.; Zalewska, A.; Chabowski, A. Redox Balance, Antioxidant Defense, and Oxidative Damage in the Hypothalamus and Cerebral Cortex of Rats with High Fat Diet-Induced Insulin Resistance. Oxidative Med. Cell. Longev. 2018, 2018, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Maciejczyk, M.; Zalewska, A.; Ładny, J.R. Salivary Antioxidant Barrier, Redox Status, and Oxidative Damage to Proteins and Lipids in Healthy Children, Adults, and the Elderly. Oxidative Med. Cell. Longev. 2019, 2019, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kołodziej, U.; Maciejczyk, M.; Niklińska, W.; Waszkiel, D.; Żendzian-Piotrowska, M.; Żukowski, P.; Zalewska, A. Chronic high-protein diet induces oxidative stress and alters the salivary gland function in rats. Arch. Oral Boil. 2017, 84, 6–12. [Google Scholar] [CrossRef]
- Ahmadi-Motamayel, F.; Goodarzi, M.T.; Hendi, S.; Kasraei, S.; Moghimbeigi, A. Total antioxidant capacity of saliva and dental caries. Med. Oral Patol. Oral y Cir. Bucal 2013, 18, e553–e556. [Google Scholar] [CrossRef]
- Evelyn, R.; Javier, M.; Gustavo, M.; Miguel, N.; Patricia, P.; Valeria, G.; Oyarzo, J.F.; Yevenes, I. Caries-free subjects have high levels of urease and arginine deiminase activity. J. Appl. Oral Sci. 2014, 22, 235–240. [Google Scholar]
- Krawczyk, D.; Sikorska, M.; Mielnik-Błaszczak, M.; Pasternak, K.; Kapeć, E.; Sztanke, M. Dental caries and total antioxidant status of unstimulated mixed whole saliva in patients aged 16–23 years. Adv. Med. Sci. 2012, 57, 163–168. [Google Scholar] [CrossRef]
- Hartenbach, F.A.R.R.; Velasquez, É.; Nogueira, F.C.; Domont, G.B.; Ferreira, E.D.O.; Colombo, A.P.V. Proteomic analysis of whole saliva in chronic periodontitis. J. Proteom. 2020, 213, 103602. [Google Scholar] [CrossRef]
- Rovera, A.; Rovera, G.; Alzahrani, A.; Hector, M.; Anderson, P. Correlation between parotid saliva composition and dental caries using 31P-NMR and ICDAS score. Arch. Oral Boil. 2020, 111, 104651. [Google Scholar] [CrossRef]
- Anusuya, S.; Prabhuji, M.L.; Lazarus, F.; Bhavikatti, S.K.; Babrawala, I.S. Estimation of 8-Hydroxy-deoxyguanosine (8-OHdG) in Saliva as a Marker of Oxidative Stress in Patients with Chronic Periodontitis: Preliminary Data. J. Int. Acad. Periodontol. 2017, 19, 95–100. [Google Scholar] [PubMed]
- Acquier, A.B.; De Couto Pita, A.K.; Busch, L.; Sánchez, G.A. Parameters of oxidative stress in saliva from patients with aggressive and chronic periodontitis. Redox Rep. 2016, 22, 119–126. [Google Scholar] [CrossRef]
- Jankowska, A.K.; Waszkiel, D.; Kowalczyk, A. Ślina jako główny składnik ekosystemu jamy ustnej, Część, I. Mechanizm wydzielania i funkcje. Wiadomości Lek. 2007, 60, 148–154. [Google Scholar]
- Jankowska, A.K.; Waszkiel, D.; Kobus, A.; Zwierz, K. Ślina jako główny składnik ekosystemu jamy ustnej, Część II. Mechanizmy odpornościowe. Wiadomości Lek. 2007, 60, 253–257. [Google Scholar]
- Jankowska, A.; Waszkiel, D.; Kobus, A.; Szajda, S.D.; Łuczaj- Cepowicz, E.; Błahuszewska, K.; Snarska, J.; Zwierz, K. The differences in salivary lysozyme concentration in caries resistant and caries-susceptible young men and women adults. In Środowiskowe Źródła Zagrożeń Zdowotnych; Kaczor, A., Borzécki, A., Iskra, M., Eds.; Wydawnictwo AM: Nałęczów, Polska, 2007; pp. 1451–1454. [Google Scholar]
- Żukowski, P.; Maciejczyk, M.; Waszkiel, D. Sources of free radicals and oxidative stress in the oral cavity. Arch. Oral Boil. 2018, 92, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Balaji, T.M.; Vasanthi, H.R.; Rao, S.R. Gingival, Plasma and Salivary Levels of Melatonin in Periodontally Healthy Individuals and Chronic Periodontitis Patients: A Pilot Study. J. Clin. Diagn. Res. 2015, 9, ZC23–ZC25. [Google Scholar] [CrossRef]
- Zalewska, A.; Knaś, M.; Kuźmiuk, A.; Waszkiewicz, N.; Niczyporuk, M.; Waszkiel, D.; Zwierz, K. Salivary innate defense system in type 1 diabetes mellitus in children with mixed and permanent dentition. Acta Odontol. Scand. 2013, 71, 1493–1500. [Google Scholar] [CrossRef]
- Ahmadi-Motamayel, F.; Goodarzi, M.T.; Mahdavinezhad, A.; Jamshidi, Z.; Darvishi, M. Salivary and Serum Antioxidant and Oxidative Stress Markers in Dental Caries. Caries Res. 2018, 52, 565–569. [Google Scholar] [CrossRef]
- Almerich-Silla, J.M.; Montiel-Company, J.M.; Pastor, S.; Serrano, F.; Puig-Silla, M.; Dasí, F. Oxidative Stress Parameters in Saliva and Its Association with Periodontal Disease and Types of Bacteria. Dis. Markers 2015, 2015, 1–7. [Google Scholar] [CrossRef]
- Araujo, H.C.; Nakamune, A.C.M.S.; Garcia, W.G.; Pessan, J.P.; Antoniali, C. Carious Lesion Severity Induces Higher Antioxidant System Activity and Consequently Reduces Oxidative Damage in Children’s Saliva. Oxidative Med. Cell. Longev. 2020, 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Babiuch, K.; Bednarczyk, A.; Gawlik, K.; Pawlica-Gosiewska, D.; Kęsek, B.; Darczuk, D.; Stępień, P.; Chomyszyn-Gajewska, M.; Kaczmarzyk, T. Evaluation of enzymatic and non-enzymatic antioxidant status and biomarkers of oxidative stress in saliva of patients with oral squamous cell carcinoma and oral leukoplakia: A pilot study. Acta Odontol. Scand. 2019, 77, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Baltacioglu, E.; Sukuroglu, E. Protein carbonyl levels in serum, saliva and gingival crevicular fluid in patients with chronic and aggressive periodontitis. Saudi Dent. J. 2018, 31, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Govindaraj, J.; Govindaraj, K.; Selvaraj, J.; Ramalingam, M.; Padmavathy, K.; Sumathy, G. 8-Hydroxy deoxyguanosine—A potential biomarker in periodontitis. Drug Invent. Today 2019, 11, 1027–1032. [Google Scholar]
- Srivastava, K.C. Comparative Evaluation of Saliva’s Oxidant-Antioxidant Status in Patients with Different Clinicopathological Types of Oral Leukoplakia. J. Int. Soc. Prev. Community Dent. 2019, 9, 396–402. [Google Scholar] [CrossRef]
- Thekiso, M.; Yengopal, V.; Rudolph, M.J.; Bhayat, A. Caries status among children in the West Rand District of Gauteng Province, South Africa. SADJ 2012, 67, 318–320. [Google Scholar]
- Borys, J.; Maciejczyk, M.; Antonowicz, B.; Sidun, J.; Świderska, M.; Zalewska, A. Free radical production, inflammation and apoptosis in patients treated with titanium mandibular fixations—An observational study. Front. Immunol. 2019, 10, 2662. [Google Scholar] [CrossRef]
- Lushchak, V.I. Free radicals, reactive oxygen species, oxidative stress and its classification. Chem. Biol. Interact. 2014, 224, 164–175. [Google Scholar] [CrossRef] [PubMed]
- Pietrucha, B.; Heropolitańska-Pliszka, E.; Maciejczyk, M.; Car, H.; Sawicka-Powierza, J.; Motkowski, R.; Karpinska, J.; Hryniewicka, M.; Zalewska, A.; Pac, M.; et al. Comparison of Selected Parameters of Redox Homeostasis in Patients with Ataxia-Telangiectasia and Nijmegen Breakage Syndrome. Oxidative Med. Cell. Longev. 2017, 2017, 1–8. [Google Scholar] [CrossRef]
- Tóthová, L.; Celec, P. Oxidative Stress and Antioxidants in the Diagnosis and Therapy of Periodontitis. Front. Physiol. 2017, 8, 1055. [Google Scholar] [CrossRef]
- Sena, L.A.; Chandel, N.S. Physiological Roles of Mitochondrial Reactive Oxygen Species. Mol. Cell 2012, 48, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Lushchak, V.I. Classification of oxidative stress based on its intensity. EXCLI J. 2014, 13, 922–937. [Google Scholar] [PubMed]
- Stadtman, E.R.; Levine, R.L. Free radical-mediated oxidation of free amino acids and amino acid residues in proteins. Amino Acids 2003, 25, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Cadet, J.; Douki, T.; Gasparutto, D.; Ravanat, J.L. Oxidative damage to DNA: Formation, measurement and biochemical features. Mutat. Res. Fundam. Mol. Mech. Mutagen. 2003, 531, 5–23. [Google Scholar] [CrossRef] [PubMed]
- Sayre, L.M.; Lin, D.; Yuan, Q.; Zhu, X.; Tang, X. Protein Adducts Generated from Products of Lipid Oxidation: Focus on HNE and ONE. Drug Metab. Rev. 2006, 38, 651–675. [Google Scholar] [CrossRef] [PubMed]
- Zhong, H.; Yin, H. Role of lipid peroxidation derived 4-hydoxynonenal (4-HNE) in cancer: Focusing on mitochondria. Redox Biol. 2015, 4, 193–199. [Google Scholar] [CrossRef]
- Grosicka-Maciąg, E. Biological consequences of oxidative stress induced by pesticides. Postępy Hig. Med. Dośw. 2001, 65, 357–366. [Google Scholar] [CrossRef]
- Knaś, M.; Maciejczyk, M.; Daniszewska, I.; Klimiuk, A.; Matczuk, J.; Kołodziej, U.; Waszkiel, D.; Ładny, J.R.; Żendzian-Piotrowska, M.; Zalewska, A. Oxidative Damage to the Salivary Glands of Rats with Streptozotocin-Induced Diabetes-Temporal Study: Oxidative Stress and Diabetic Salivary Glands. J. Diabetes Res. 2016, 2016, 1–13. [Google Scholar] [CrossRef]
- Ayala, A.; Muñoz, M.F.; Arguelles, S. Lipid Peroxidation: Production, Metabolism, and Signaling Mechanisms of Malondialdehyde and 4-Hydroxy-2-Nonenal. Oxidative Med. Cell. Longev. 2014, 2014, 1–31. [Google Scholar] [CrossRef]
- Jaganjac, M.; Tirosh, O.; Cohen, G.; Sasson, S.; Zarkovic, N. Reactive aldehydes—Second messengers of free radicals in diabetes mellitus. Free Radic. Res. 2013, 47, 39–48. [Google Scholar] [CrossRef]
- Green, E.A.; Flavell, R.A. The initiation of autoimmune diabetes. Curr. Opin. Immunol. 1999, 11, 663–669. [Google Scholar] [CrossRef]
- Ibuki, F.K.; Simões, A.; Nogueira, F.N. Antioxidant enzymatic defense in salivary glands of streptozotocin-induced diabetic rats: A temporal study. Cell Biochem. Funct. 2010, 28, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, F.N.; Carvalho, A.M.; Yamaguti, P.M.; Nicolau, J. Antioxidant parameters and lipid peroxidation in salivary glands of streptozotocin-induced diabetic rats. Clin. Chim. Acta 2005, 353, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Waddington, R.J.; Moseley, R.; Embery, G. Periodontal Disease Mechanisms: Reactive oxygen species: A potential role in the pathogenesis of periodontal diseases. Oral Dis. 2000, 6, 138–151. [Google Scholar] [CrossRef]
- Bartosz, G. Druga Twarz Tlenu. Wolne Rodniki w Przyrodzie; Wydawnictwo Naukowe PWN: Warsow, Poland, 2003. [Google Scholar]
- Gruber, B. Enzymy chroniące organizm przed reaktywnymi postaciami tlenu. Farm Pol 1996, 52, 263–271. [Google Scholar]
- De Groot, H.; Hegi, U.; Sies, H. Loss of α-tocopherol upon exposure to nitric oxide or the sydnonimine SIN-1. FEBS Lett. 1993, 315, 139–142. [Google Scholar] [CrossRef]
- Lardinois, O.M. Reactions of Bovine Liver Catalase with Superoxide Radicals and Hydrogen Peroxide. Free Radic. Res. 1995, 22, 251–274. [Google Scholar] [CrossRef]
- Tainer, J.A.; Getzoff, E.D.; Richardson, J.S.; Richardson, D.C. Structure and mechanism of copper, zinc superoxide dismutase. Nature 1983, 306, 284–287. [Google Scholar] [CrossRef]
- Antunes, F.; Cadenas, E. Estimation of H2O2 gradients across biomembranes. FEBS Lett. 2000, 475, 121–126. [Google Scholar] [CrossRef]
- Safo, M.K.; Musayev, F.N.; Wu, S.-H.; Abraham, N.J.; Ko, T.-P. Structure of tetragonal crystals of human erythrocyte catalase. Acta Crystallogr. Sect. D Biol. Crystallogr. 2001, 57, 1–7. [Google Scholar] [CrossRef]
- Lledías, F.; Rangel, P.; Hansberg, W.; Lledías, F. Oxidation of Catalase by Singlet Oxygen. J. Boil. Chem. 1998, 273, 10630–10637. [Google Scholar] [CrossRef]
- Cadenas, E. Mechanisms of Antioxidant Action. Free Radicals, Oxidative Stress, and Antioxidants; Springer: Boston, MA, USA, 1997; pp. 237–251. [Google Scholar]
- Von Ossowski, I.; Hausner, G.; Loewen, P.C. Molecular evolutionary analysis based on the amino acid sequence of catalase. J. Mol. Evol. 1993, 37, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Battino, M.; Ferreiro, M.S.; Gallardo, I.; Newman, H.N.; Bullon, P. The antioxidant capacity of saliva. J. Clin. Periodontol. 2002, 29, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Kanehira, T.; Shibata, K.; Kashiwazaki, H.; Inoue, N.; Morita, M. Comparison of antioxidant enzymes in saliva of elderly smokers and non-smokers. Gerodontology 2006, 23, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Bartosz, G. Superoxide Dismutases and Catalase. In Oxidants and Antioxidant Defense Systems; Springer: Berlin/Heidelberg, Germany, 2005; pp. 109–149. [Google Scholar]
- Reznick, A.Z.; Klein, I.; Eiserich, J.P.; Cross, C.E.; Nagler, R. Inhibition of oral peroxidase activity by cigarette smoke: In vivo and in vitro studies. Free Radic. Boil. Med. 2003, 34, 377–384. [Google Scholar] [CrossRef]
- Matczuk, J.; Zalewska, A.; Łukaszuk, B.; Garbowska, M.; Chabowski, A.; Żendzian-Piotrowska, M.; Kurek, K. Effect of streptozotocin-induced diabetes on lipids metabolism in the salivary glands. Prostaglandins Other Lipid Mediat. 2016, 126, 9–15. [Google Scholar] [CrossRef]
- Clancy, R.M.; Levartovsky, D.; Leszczynska-Piziak, J.; Yegudin, J.; Abramson, S.B. Nitric oxide reacts with intracellular glutathione and activates the hexose monophosphate shunt in human neutrophils: Evidence for S-nitrosoglutathione as a bioactive intermediary. Proc. Natl. Acad. Sci. USA 1994, 91, 3680–3684. [Google Scholar] [CrossRef]
- Anders, M.W. Chemical Toxicology of Reactive Intermediates Formed by the Glutathione-Dependent Bioactivation of Halogen-Containing Compounds. Chem. Res. Toxicol. 2008, 21, 145–159. [Google Scholar] [CrossRef]
- Liu, L.; Yan, Y.; Zeng, M.; Zhang, J.; Hanes, M.A.; Ahearn, G.; McMahon, T.J.; Dickfeld, T.; Marshall, H.E.; Que, L.G.; et al. Essential Roles of S-Nitrosothiols in Vascular Homeostasis and Endotoxic Shock. Cell 2004, 116, 617–628. [Google Scholar] [CrossRef]
- Maxwell, S.R.J.; Thomason, H.; Sandler, D.; Leguen, C.; Baxter, M.A.; Thorpe, G.H.G.; Jones, A.F.; Barnett, A.H. Antioxidant status in patients with uncomplicated insulin-dependent and non-insulin-dependent diabetes mellitus. Eur. J. Clin. Investig. 1997, 27, 484–490. [Google Scholar] [CrossRef]
- Pablos, M.I.; Reiter, R.J.; Chuang, J.-I.; Ortiz, G.G.; Guerrero, J.M.; Sewerynek, E.; Agapito, M.T.; Melchiorri, D.; Lawrence, R.; Deneke, S.M. Acutely administered melatonin reduces oxidative damage in lung and brain induced by hyperbaric oxygen. J. Appl. Physiol. 1997, 83, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Gilad, E.; Cuzzocrea, S.; Zingarelli, B.; Salzman, A.L.; Szabo, C. Melatonin is a scavenger of peroxynitrite. Life Sci. 1997, 60, PL169–PL174. [Google Scholar] [CrossRef]
- Reiter, R.J. Oxidative damage in the central nervous system: Protection by melatonin. Prog. Neurobiol. 1998, 56, 359–384. [Google Scholar] [CrossRef]
- Gitto, E.; Tan, D.-X.; Reiter, R.J.; Karbownik, M.; Manchester, L.C.; Cuzzocrea, S.; Fulia, F.; Barberi, I. Individual and synergistic antioxidative actions of melatonin: Studies with vitamin E, vitamin C, glutathione and desferrrioxamine (desferoxamine) in rat liver homogenates. J. Pharm. Pharmacol. 2001, 53, 1393–1401. [Google Scholar] [CrossRef] [PubMed]
- Usha, C.; Sathyanarayanan, R. Dental caries—A complete changeover (Part I). J. Conserv. Dent. 2009, 12, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Leonora, J.; Tjäderhane, L.; Tieche, J.-M. Parotid gland function and dentin apposition in rat molars. J. Dent. Res. 2002, 81, 259–264. [Google Scholar] [CrossRef]
- Da Silva, P.V.; Troiano, J.A.; Nakamune, A.C.M.; Pessan, J.P.; Antoniali, C. Increased activity of the antioxidants systems modulate the oxidative stress in saliva of toddlers with early childhood caries. Arch. Oral Boil. 2016, 70, 62–66. [Google Scholar] [CrossRef]
- Jurczak, A.; Kościelniak, D.; Skalniak, A.; Papież, M.A.; Vyhouskaya, P.; Krzyściak, W. The role of the saliva antioxidant barrier to reactive oxygen species with regard to caries development. Redox Rep. 2017, 22, 524–533. [Google Scholar] [CrossRef]
- Mahjoub, S.; Ghasempour, M.; Gharage, A.; Bijani, A.; Masrourroudsari, J. Comparison of Total Antioxidant Capacity in Saliva of Children with Severe Early Childhood Caries and Caries-Free Children. Caries Res. 2014, 48, 271–275. [Google Scholar] [CrossRef]
- Kumar, D.; Pandey, R.K.; Agrawal, D.; Agrawal, D. An estimation and evaluation of total antioxidant capacity of saliva in children with severe early childhood caries. Int. J. Paediatr. Dent. 2011, 21, 459–464. [Google Scholar] [CrossRef]
- Muchandi, S.; Walimbe, H.; Bijle, M.N.A.; Nankar, M.; Chaturvedi, S.; Karekar, P. Comparative Evaluation and Correlation of Salivary Total Antioxidant Capacity and Salivary pH in Caries-free and Severe Early Childhood Caries Children. J. Contemp. Dent. Pract. 2015, 16, 234–237. [Google Scholar] [CrossRef]
- Tóthová, L.; Celecová, V.; Celec, P. Salivary Markers of Oxidative Stress and Their Relation to Periodontal and Dental Status in Children. Dis. Markers 2013, 34, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Subramanyam, D.; Gurunathan, D.; Gaayathri, R.; Priya, V.V. Comparative evaluation of salivary malondialdehyde levels as a marker of lipid peroxidation in early childhood caries. Eur. J. Dent. 2018, 12, 067–070. [Google Scholar] [CrossRef] [PubMed]
- Syed, M.; Sachdev, V.; Chopra, R. Intercomparison of salivary nitric oxide as a biomarker of dental caries risk between caries-active and caries-free children. Eur. Arch. Paediatr. Dent. 2016, 17, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Han, D.-H.; Kim, M.-J.; Jun, E.-J.; Kim, J.-B. The role of glutathione metabolism in cariogenic bacterial growth and caries in Korean children. Arch. Oral Boil. 2013, 58, 493–499. [Google Scholar] [CrossRef]
- Preethi, B.P.; Reshma, D.; Anand, P. Evaluation of Flow Rate, pH, Buffering Capacity, Calcium, Total Proteins and Total Antioxidant Capacity Levels of Saliva in Caries Free and Caries Active Children: An In Vivo Study. Indian J. Clin. Biochem. 2010, 25, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Dodwad, R.; Betigeri, A.V.; Preeti, B.P. Estimation of total antioxidant capacity levels in saliva of caries-free and caries-active children. Contemp. Clin. Dent. 2011, 2, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P.; Reddy, N.V.; Rao, V.A.P.; Saxena, A.; Chaudhary, C.P. Estimation of salivary flow rate, pH, buffer capacity, calcium, total protein content and total antioxidant capacity in relation to dental caries severity, age and gender. Contemp. Clin. Dent. 2015, 6, S65–S71. [Google Scholar] [CrossRef]
- Pyati, S.A.; Naveen Kumar, R.; Kumar, V.; Praveen Kumar, N.H.; Parveen Reddy, K.M. Salivary Flow Rate, pH, Buffering Capacity, Total Protein, Oxidative Stress and Antioxidant Capacity in Children with and without Dental Caries. J. Clin. Pediatr. Dent. 2018, 42, 445–449. [Google Scholar] [CrossRef]
- Banda, N.R.; Singh, G.; Markam, V. Evaluation of total antioxidant level of saliva in modulation of caries occurrence and progression in children. J. Indian Soc. Pedod. Prev. Dent. 2016, 34, 227. [Google Scholar] [CrossRef]
- Alanazi, G.S.; Pani, S.C.; AlKabbaz, H.J. Salivary antioxidant capacity of children with severe early childhood caries before and after complete dental rehabilitation. Arch. Oral Boil. 2018, 95, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, M.; Ghoorchi, V.; Rezaei, F.; Raygani, A.V. Evaluation of Total Antioxidant Capacity of Saliva in High School Students. Glob. J. Health Sci. 2015, 8, 89–94. [Google Scholar] [CrossRef]
- Hegde, M.N.; Hegde, N.D.; Ashok, A.; Shetty, S. Evaluation of total antioxidant capacity of saliva and serum in caries-free and caries-active adults: An in-vivo study. Indian J. Dent. Res. 2013, 24, 164. [Google Scholar] [CrossRef] [PubMed]
- Sarode, G.; Shelar, A.; Sarode, S.; Bagul, N. Association between Dental Caries and Lipid Peroxidation in Saliva. Int. J. Oral. Maxillofac. Pathol. 2012, 3, 2–4. [Google Scholar]
- Hendi, S.; Goodarzi, M.T.; Moghimbeigi, A.; Ahmadi-Motamayel, F. Evaluation of the status of salivary antioxidants in dental caries. Infect. Disord. Drug Targets 2019, 19. [Google Scholar] [CrossRef]
- Hegde, M.N.; Hegde, N.D.; Ashok, A.; Shetty, S. Biochemical Indicators of Dental Caries in Saliva: An in vivo Study. Caries Res. 2014, 48, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, L.; Furuncuoğlu, H.; Atala, M.; Uluköylü, O.; Akyüz, S.; Yarat, A. Association between dental-oral health in young adults and salivary glutathione, lipid peroxidation and sialic acid levels and carbonic anhydrase activity. Braz. J. Med. Boil. Res. 2008, 41, 956–959. [Google Scholar] [CrossRef]
- Tulunoglu, Ö.; Demirtas, S.; Tulunoglu, I. Total antioxidant levels of saliva in children related to caries, age, and gender. Int. J. Paediatr. Dent. 2006, 16, 186–191. [Google Scholar] [CrossRef]
- Celecová, V.; Kamodyova, N.; Tóthová, L.; Kúdela, M.; Celec, P. Salivary markers of oxidative stress are related to age and oral health in adult non-smokers. J. Oral Pathol. Med. 2012, 42. [Google Scholar] [CrossRef]
- Ahmadi-Motamayel, F.; Hendi, S.S.; Goodarzi, M.T. Evaluation of Salivary Lipid Peroxidation End Product Level in Dental Caries. Infect. Disord. Drug Targets 2020, 20, 65–68. [Google Scholar] [CrossRef]
- Rice-Evans, C.A. DAT. Techniques in Free Radical Research. In Laboratory Techniques in Biochemistry and Molecular Biology; Elsevier Science: London, UK, 1991; pp. 1–291. [Google Scholar]
- Pisoschi, A.M.; Pop, A. The role of antioxidants in the chemistry of oxidative stress: A review. Eur. J. Med. Chem. 2015, 97, 55–74. [Google Scholar] [CrossRef] [PubMed]
- Zalewska, A.; Knaś, M.; Żendzian-Piotrowska, M.; Waszkiewicz, N.; Szulimowska, J.; Prokopiuk, S.; Waszkiel, D.; Car, H. Antioxidant profile of salivary glands in high fat diet-induced insulin resistance rats. Oral Dis. 2013, 20, 560–566. [Google Scholar] [CrossRef]
- Zalewska, A.; Knaś, M.; Maciejczyk, M.; Waszkiewicz, N.; Klimiuk, A.; Choromańska, M.; Matczuk, J.; Waszkiel, D.; Car, H. Antioxidant profile, carbonyl and lipid oxidation markers in the parotid and submandibular glands of rats in different periods of streptozotocin induced diabetes. Arch. Oral Boil. 2015, 60, 1375–1386. [Google Scholar] [CrossRef]
- Aparna, A.; Shilpa, S.; Surgery, M. Salivary Nitric Oxide (No2+No3) As Biomarker of Dental Caries in Adults: An Invivo Study. Int. Res. J. Pharm. 2012, 3, 100–102. [Google Scholar]
- Maciejczyk, M.; Szulimowska, J.; Taranta-Janusz, K.; Werbel, K.; Wasilewska, A.; Zalewska, A. Salivary FRAP as A Marker of Chronic Kidney Disease Progression in Children. Antioxidants 2019, 8, 409. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Szulimowska, J.; Skutnik-Radziszewska, A.; Taranta-Janusz, K.; Wasilewska, A.; Wiśniewska, N.; Zalewska, A. Salivary Biomarkers of Oxidative Stress in Children with Chronic Kidney Disease. J. Clin. Med. 2018, 7, 209. [Google Scholar] [CrossRef] [PubMed]
- Skutnik-Radziszewska, A.; Maciejczyk, M.; Flisiak, I.; Krahel, J.; Kołodziej, J.K.U.; Kotowska-Rodziewicz, A.; Klimiuk, A.; Zalewska, A. Enhanced Inflammation and Nitrosative Stress in the Saliva and Plasma of Patients with Plaque Psoriasis. J. Clin. Med. 2020, 9, 745. [Google Scholar] [CrossRef]
- Zalewska, A.; Knaś, M.; Waszkiewicz, N.; Klimiuk, A.; Litwin, K.; Sierakowski, S.; Waszkiel, D.; Gindzienska-Sieskiewicz, E. Salivary antioxidants in patients with systemic sclerosis. J. Oral Pathol. Med. 2013, 43, 61–68. [Google Scholar] [CrossRef]
- Gao, X.; Qi, L.; Qiao, N.; Choi, H.K.; Curhan, G.; Tucker, K.L.; Ascherio, A. Intake of Added Sugar and Sugar-Sweetened Drink and Serum Uric Acid Concentration in US Men and Women. Hypertension 2007, 50, 306–312. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, R.; Bagewadi, N.; Krishnan, N. A study to correlate dental caries experience with total antioxidant levels of saliva among adolescents in Mangalore. J. Indian Assoc. Public Health Dent. 2015, 13, 122. [Google Scholar] [CrossRef]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal diseases. Nat. Rev. Dis. Prim. 2017, 3, 17038. [Google Scholar] [CrossRef] [PubMed]
- Paredes-Sánchez, E.; Montiel-Company, J.M.; Iranzo-Cortés, J.E.; Almerich-Torres, T.; Bellot-Arcís, C.; Almerich-Silla, J.M. Meta-Analysis of the Use of 8-OHdG in Saliva as a Marker of Periodontal Disease. Dis. Markers 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tatakis, D.N.; Kumar, P.S. Etiology and pathogenesis of periodontal diseases. Dent Clin. North Am. 2005, 49, 491–516. [Google Scholar] [CrossRef]
- Martínez-Herrera, M.; López-Domènech, S.; Silvestre-Rangil, J.; Bañuls, C.; Víctor, V.M.; Rocha, M. Chronic periodontitis impairs polymorphonuclear leucocyte–endothelium cell interactions and oxidative stress in humans. J. Clin. Periodontol. 2018, 45, 1429–1439. [Google Scholar] [CrossRef] [PubMed]
- Chandra, R.; Srinivas, G.; Reddy, A.A.; Reddy, B.H.; Reddy, C.; Nagarajan, S.; Naveen, A. Locally delivered antioxidant gel as an adjunct to nonsurgical therapy improves measures of oxidative stress and periodontal disease. J. Periodontal Implant. Sci. 2013, 43, 121–129. [Google Scholar] [CrossRef]
- Mathur, A.; Mathur, L.; Manohar, B.; Mathur, H.; Shankarapillai, R.; Shetty, N.; Bhatia, A. Antioxidant therapy as monotherapy or as an adjunct to treatment of periodontal diseases. J. Indian Soc. Periodontol. 2013, 17, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Raut, C.P.; Sethi, K.S. Comparative evaluation of co-enzyme Q10 and Melaleuca alternifolia as antioxidant gels in treatment of chronic periodontitis: A clinical study. Contemp. Clin. Dent. 2016, 7, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Sree, S.L.; Sethupathy, S. Evaluation of the efficacy of taurine as an antioxidant in the management of patients with chronic periodontitis. Dent. Res. J. (Isfahan) 2014, 11, 228–233. [Google Scholar]
- Tóthová, L.; Kamodyova, N.; Červenka, T.; Celec, P. Salivary markers of oxidative stress in oral diseases. Front. Microbiol. 2015, 5, 73. [Google Scholar] [CrossRef]
- Trivedi, S.; Lal, N.; Mahdi, A.; Singh, B.; Pandey, S. Association of Salivary Lipid Peroxidation Levels, Antioxidant Enzymes, and Chronic Periodontitis. Int. J. Periodontics Restor. Dent. 2015, 35, 14–19. [Google Scholar] [CrossRef]
- Miricescu, D.; Totan, A.; Calenic, B.; Mocanu, B.; Didilescu, A.; Mohora, M.; Spinu, T.; Greabu, M. Salivary biomarkers: Relationship between oxidative stress and alveolar bone loss in chronic periodontitis. Acta Odontol. Scand. 2013, 72, 42–47. [Google Scholar] [CrossRef]
- Karim, S.; Pratibha, P.K.; Kamath, S.; Bhat, G.S.; Kamath, U.; Dutta, B.; Sharma, N.; Archana, B.; Bhat, K.M.; Guddattu, V. Superoxide dismutase enzyme and thiol antioxidants in gingival crevicular fluid and saliva. Dent. Res. J. 2012, 9, 266–272. [Google Scholar]
- Villa-Correa, Y.A.; Isaza-Guzmán, D.M.; Tobón-Arroyave, S.I. Influence of Periodontal Clinical Status on Salivary Levels of Glutathione Reductase. J. Periodontol. 2016, 87, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Bazzichi, L.; Ciompi, M.L.; Betti, L.; Rossi, A.; Melchiorre, D.; Fiorini, M.; Giannaccini, G.; Lucacchini, A. Impaired gluthathione reductase activity and levels of collagenase and elastase in synovial fluid in rheumatoid arthritis. Clin. Exp. Rheumatol. 2002, 20, 761–766. [Google Scholar] [PubMed]
- Wei, D.; Zhang, X.-L.; Wang, Y.-Z.; Yang, C.-X.; Chen, G. Lipid peroxidation levels, total oxidant status and superoxide dismutase in serum, saliva and gingival crevicular fluid in chronic periodontitis patients before and after periodontal therapy. Aust. Dent. J. 2010, 55, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.-S.; Huang, W.-C.; Chen, S.-Y.; Chen, C.-H.; Lee, C.-Y.; Lin, C.-T.; Huang, Y.-K. Scaling-Stimulated Salivary Antioxidant Changes and Oral-Health Behavior in an Evaluation of Periodontal Treatment Outcomes. Sci. World J. 2014, 2014, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Meschiari, C.A.; Marcaccini, A.M.; Moura, B.C.S.; Zuardi, L.R.; Tanus-Santos, J.E.; Gerlach, R.F. Salivary MMPs, TIMPs, and MPO levels in periodontal disease patients and controls. Clin. Chim. Acta 2013, 421, 140–146. [Google Scholar] [CrossRef]
- Novaković, N.; Todorovic, T.; Rakic, M.; Milinkovic, I.; Dozic, I.; Jankovic, S.; Aleksic, Z.; Cakic, S. Salivary antioxidants as periodontal biomarkers in evaluation of tissue status and treatment outcome. J. Periodontal Res. 2013, 49, 129–136. [Google Scholar] [CrossRef]
- Lee, C.-Y.; Choy, C.S.; Lai, Y.-C.; Chang, C.-C.; Teng, N.-C.; Huang, W.-T.; Lin, C.-T.; Huang, Y.-K. A Cross-Sectional Study of Endogenous Antioxidants and Patterns of Dental Visits of Periodontitis Patients. Int. J. Environ. Res. Public Health 2019, 16, 180. [Google Scholar] [CrossRef]
- AlMughrabi, O.M.; Marzouk, K.M.; Hasanato, R.M.; Shafik, S.S. Melatonin levels in periodontal health and disease. J. Periodontal Res. 2012, 48, 315–321. [Google Scholar] [CrossRef]
- Srinath, R.; Acharya, A.B.; Thakur, S.L. Salivary and Gingival Crevicular Fluid Melatonin in Periodontal Health and Disease. J. Periodontol. 2010, 81, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Andrukhov, O.; Haririan, H.; Müller-Kern, M.; Liu, S.; Liu, Z.; Rausch-Fan, X. Total Antioxidant Capacity and Total Oxidant Status in Saliva of Periodontitis Patients in Relation to Bacterial Load. Front. Cell. Infect. Microbiol. 2016, 5, 97. [Google Scholar] [CrossRef] [PubMed]
- Baser, U.; Gamsiz-Isik, H.; Cifcibasi, E.; Ademoglu, E.; Yalcin, F. Plasma and salivary total antioxidant capacity in healthy controls compared with aggressive and chronic periodontitis patients. Saudi Med. J. 2015, 36, 856–861. [Google Scholar] [CrossRef]
- Baňasová, L.; Kamodyova, N.; Janšáková, K.; Tóthová, L.; Stanko, P.; Turna, J.; Celec, P. Salivary DNA and markers of oxidative stress in patients with chronic periodontitis. Clin. Oral Investig. 2014, 19, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Toczewska, J.; Maciejczyk, M.; Konopka, T.; Zalewska, A. Total Oxidant and Antioxidant Capacity of Gingival Crevicular Fluid and Saliva in Patients with Periodontitis: Review and Clinical Study. Antioxidants 2020, 9, 450. [Google Scholar] [CrossRef] [PubMed]
- Baltacıoğlu, E.; Yuva, P.; Aydın, G.; Alver, A.; Kahraman, C.; Karabulut, E.; Akalın, F.A. Lipid Peroxidation Levels and Total Oxidant/Antioxidant Status in Serum and Saliva From Patients With Chronic and Aggressive Periodontitis. Oxidative Stress Index: A New Biomarker for Periodontal Disease? J. Periodontol. 2014, 85, 1432–1441. [Google Scholar] [CrossRef]
- Önder, C.; Kurgan, Ş.; Altıngöz, S.M.; Bağış, N.; Uyanık, M.; Serdar, M.A.; Kantarcı, A.; Günhan, M. Impact of non-surgical periodontal therapy on saliva and serum levels of markers of oxidative stress. Clin. Oral Investig. 2016, 21, 1961–1969. [Google Scholar] [CrossRef]
- Ahmadi-Motamayel, F.; Goodarzi, M.T.; Jamshidi, Z.; Kebriaei, R. Evaluation of Salivary and Serum Antioxidant and Oxidative Stress Statuses in Patients with Chronic Periodontitis: A Case-Control Study. Front. Physiol. 2017, 8, 189. [Google Scholar] [CrossRef]
- Verma, A.; Tripathi, V.; Singh, S.T.; Singh, C.D.; Gill, J.S.; Sharma, V. Assessment of Lipid Peroxidation Levels and Total Antioxidant Status in Chronic and Aggressive Periodontitis Patients: An in vivo Study. J. Contemp. Dent. Pract. 2018, 19, 287–291. [Google Scholar] [CrossRef]
- Spite, M.; Summers, L.; Porter, T.; Srivastava, S.; Bhatnagar, A.; Serhan, C.N. Resolvin D1 controls inflammation initiated by glutathione-lipid conjugates formed during oxidative stress. Br. J. Pharmacol. 2009, 158, 1062–1073. [Google Scholar] [CrossRef]
- Sezer, U.; Çiçek, Y.; Çanakçi, C.F. Increased Salivary Levels of 8-Hydroxydeoxyguanosine May Be a Marker for Disease Activity for Periodontitis. Dis. Markers 2012, 32, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Perez, A.L.; Ortiz-García, Y.M.; Lazalde-Ramos, B.P.; Guerrero-Velázquez, C.; Gómez-Meda, B.C.; Ramírez-Aguilar, M.Á.; Zúñiga-González, G.M. Increased micronuclei and nuclear abnormalities in buccal mucosa and oxidative damage in saliva from patients with chronic and aggressive periodontal diseases. J. Periodontal Res. 2014, 50, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Villa-Correa, Y.A.; Isaza-Guzmán, D.M.; Tobón-Arroyave, S.I. Prognostic Value of 8-Hydroxy-2′-Deoxyguanosine and Human Neutrophil Elastase/α1-Proteinase Inhibitor Complex as Salivary Biomarkers of Oxidative Stress in Chronic Periodontitis. J. Periodontol. 2015, 86, 1260–1267. [Google Scholar] [CrossRef]
- Badea, V.; Balaban, D.P.; Amariei, C.; Nuca, C.; Bucur, L. Salivary 8-hidroxy-2-deoxy guanosine as oxidative stress biomarker for the diagnosis of periodontal disease. Farmacia 2010, 58, 660–670. [Google Scholar]
- Öngöz, D.F.; Özden, F.O.; Avci, B.; Avcı, B. 8-Hydroxy-Deoxyguanosine Levels in Gingival Crevicular Fluid and Saliva in Patients with Chronic Periodontitis after Initial Periodontal Treatment. J. Periodontol. 2013, 84, 821–828. [Google Scholar] [CrossRef]
- Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 2005, 38, 1103–1111. [Google Scholar] [CrossRef]
- Zalewska, A.; Maciejczyk, M.; Szulimowska, J.; Imierska, M.; Blachnio-Zabielska, A. High-Fat Diet Affects Ceramide Content, Disturbs Mitochondrial Redox Balance, and Induces Apoptosis in the Submandibular Glands of Mice. Biomolecules 2019, 9, 877. [Google Scholar] [CrossRef]
- Toczewska, J.; Konopka, T.; Zalewska, A.; Maciejczyk, M. Nitrosative Stress Biomarkers in the Non-Stimulated and Stimulated Saliva, as well as Gingival Crevicular Fluid of Patients with Periodontitis: Review and Clinical Study. Antioxidants 2020, 9, 259. [Google Scholar] [CrossRef]
- Parwani, S.; Chitnis, P.; Parwani, R. Salivary nitric oxide levels in inflammatory periodontal disease—A case-control and interventional study. Int. J. Dent. Hyg. 2011, 10, 67–73. [Google Scholar] [CrossRef]
- Scarel-Caminaga, R.M.; Cera, F.F.; Pigossi, S.C.; Finoti, L.S.; Kim, Y.J.; Viana, A.C.; Secolin, R.; Montenegro, M.F.F.; Tanus-Santos, J.E.; Orrico, S.R.P.; et al. Inducible Nitric Oxide Synthase Polymorphisms and Nitric Oxide Levels in Individuals with Chronic Periodontitis. Int. J. Mol. Sci. 2017, 18, 1128. [Google Scholar] [CrossRef]
- Meschiari, C.A.; Zuardi, L.R.; Gomes, V.A.; De Almeida, G.R.C.; Novaes, A.B.; Gerlach, R.F.; Marcaccini, A.M. Salivary, blood and plasma nitrite concentrations in periodontal patients and healthy individuals before and after periodontal treatment. Clin. Chim. Acta 2015, 444, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Ozer, L.; Elgün, S.; Özdemir, B.; Pervane, B.; Özmeriç, N. Arginine–Nitric Oxide–Polyamine Metabolism in Periodontal Disease. J. Periodontol. 2011, 82, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Andrukhov, O.; Haririan, H.; Bertl, K.; Rausch, W.-D.; Bantleon, H.-P.; Moritz, A.; Rausch-Fan, X. Nitric oxide production, systemic inflammation and lipid metabolism in periodontitis patients: Possible gender aspect. J. Clin. Periodontol. 2013, 40, 916–923. [Google Scholar] [CrossRef] [PubMed]
- Topcu, A.O.; Akalin, F.A.; Sahbazoglu, K.B.; Yamalik, N.; Kilinç, K.; Karabulut, E.; Tözüm, T.F.; Ali, O.T. Nitrite and Nitrate Levels of Gingival Crevicular Fluid and Saliva in Subjects with Gingivitis and Chronic Periodontitis. J. Oral Maxillofac. Res. 2014, 5. [Google Scholar] [CrossRef]
- Ghasemi, A.; Zahediasl, S.; Mehrabi, Y.; Saadat, N.; Azizi, F. Serum nitric oxide metabolite levels in a general healthy population: Relation to sex and age. Life Sci. 2008, 83, 326–331. [Google Scholar] [CrossRef]
- Han, D.-H.; Kim, M.-S.; Shin, H.-S.; Park, K.P.; Kim, H.-D. Association between Periodontitis and Salivary Nitric Oxide Metabolites among Community Elderly Koreans. J. Periodontol. 2013, 84, 776–784. [Google Scholar] [CrossRef]
- Kurgan, Ş.; Onder, C.; Altıngöz, S.M.; Bagis, N.; Uyanik, M.; Serdar, M.A.; Kantarci, A. High sensitivity detection of salivary 8-hydroxy deoxyguanosine levels in patients with chronic periodontitis. J. Periodontal Res. 2015, 50, 766–774. [Google Scholar] [CrossRef]
- Katsuragi, H.; Ohtake, M.; Kurasawa, I.; Saito, K. Intracellular production and extracellular release of oxygen radicals by PMNs and oxidative stress on PMNs during phagocytosis of periodontopathic bacteria. Odontology 2003, 91, 13–18. [Google Scholar] [CrossRef]
- Huycke, M.M.; Abrams, V.; Moore, D.R.; Tavan, E.; Cayuela, C.; Antoine, J.-M.; Trugnan, G.; Chaugier, C.; Cassand, P. Enterococcus faecalis produces extracellular superoxide and hydrogen peroxide that damages colonic epithelial cell DNA. Carcinogenesis 2002, 23, 529–536. [Google Scholar] [CrossRef]
- Vlková, B.; Celec, P. Does Enterococcus faecalis contribute to salivary thiobarbituric acid-reacting substances? In Vivo (Brooklyn) 2009, 23, 343–345. [Google Scholar]




| Patients | Analyzed parameter | Results | Source |
|---|---|---|---|
| Study group: - 30 children with S-ECC (at the age of 0–3). Control group: - 30 caries-free children (at the age of 0–3) | Total protein concentration, MDA, TAC, SOD, UA | - ↑ total protein concentration, TAC, SOD, UA in NS of children with S-ECC vs. control (p < 0.01, p < 0.05, p < 0.05, p < 0.0001, respectively), - ↓ MDA in NS of children with S-ECC vs. control (p < 0.0001). | [71] |
| Study group: - group 1: 30 children with initial caries, - group 2: 30 children with moderate caries, - group 3: 30 children with extensive caries. Control group: - group 4: 30 children without caries. Age of study participants: 1–3 years. | Total protein concentration, MDA, TAC, UA, SOD | - ↑ total protein concentration, TAC, UA, SOD in NS of group 3 vs. groups 1, 2, 4 (p < 0.001, p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ total protein concentration, TAC, UA, SOD in NS of group 2 vs. groups 1, 4 (p < 0.001, p < 0.001, p < 0.001, p < 0.001, respectively) - n.s difference in total protein concentration, TAC, UA, SOD in NS of group 1 vs. group 4 (p > 0.05, p > 0.05, p > 0.05, p > 0.05, respectively), - ↓ MDA in NS of group 3 vs. groups 1, 2, 4 (p < 0.001), - ↓ MDA in NS of group 2 vs. groups 1, 4 (p < 0.001), - n.s difference in MDA level in NS of group 1 vs. group 4 (p > 0.05). | [22] |
| Study group: - 27 children with initial caries (at the age of 2.35 ± 1.09), - 27 children with advanced caries (at the age of 3.56 ± 1.25). Control group: - 27 caries-free children (at the age of 3.11 ± 1.19). | TAC, GSH, GSSG, GSH/GSSG | - ↑ TAC, GSH, GSSG, GSH/GSSG in NS of children with initial caries vs. control (p = 0.001, p = 0.001, p = 0.001, p = 0.001, respectively), - ↑ TAC, GSH, GSSG, GSH/GSSG in NS of children with advanced caries vs. control (p = 0.001, p = 0.001, p = 0.001, p = 0.001, respectively), - ↑ TAC, GSH, GSSG, GSH/GSSG in NS of children with initial caries vs. children with advanced caries (p = 0.001, p = 0.001, p = 0.001, p = 0.001, respectively). | [72] |
| Study group: - 40 children with S-ECC (at the age of 3–5). Control group: - 40 caries-free children (at the age of 3–5). | TAC | - ↑ TAC in NS of children with S-ECC vs. control (p = 0.025). | [73] |
| Study group: - 50 children with S-ECC (25 girls, 25 boys), at the age of 3–5. Control group: -50 caries-free children (24 girls, 26 boys), at the age of 3–5. | TAC | - ↑ TAC in NS of children with S-ECC vs. control (p < 0.001). | [74] |
| Study group: - 25 children with S-ECC (at the age of 3–5). Control group: -25 caries-free children (at the age of 3–5). | TAC | - ↑ TAC in NS of children with S-ECC vs. control (p < 0.0001). | [75] |
| Study group: - 30 children with S-ECC (at the age of 5) before treatment, including: * 28 children with S-ECC (at the age of 5), one week after treatment, * 20 children with S-ECC (at the age of 5), 3 months after treatment. Control group: - 30 caries-free children, at the age of 5. | TAC | - ↑ TAC in NS of children with S-ECC before treatment vs. control (p = 0.002), - n.s difference TAC in NS of children with S-ECC one week after treatment vs. control and 3 months after treatment vs. control (p = 0.086, p = 0.096, respectively), - ↓ TAC in NS of children with S-ECC one week after treatment vs. before treatment and 3 months after treatment vs. before treatment (p < 0.001, p < 0.001, respectively). | [85] |
| Study group: - 82 children (47 girls, 35 boys), at the age of 4–18 (13.4 ± 3.6), patients with different caries and periodontological status. | TBARS | - positive correlation between TBARS concentration and OHI and PBI indicators (p = 0.05, p = 0.04, respectively). | [76] |
| Study group: - 75 children with ECC, at the age of 6. Control group: - 75 caries-free children, at the age of 6. | MDA | - n.s difference in concentration of MDA in the NS and in serum of children with ECC vs. control (p = 0.13, p > 0.05, respectively). | [77] |
| Study group: - 50 children with active caries (DMFT/dmft ≥ 3), at the age of 6–12. Control group: - 50 caries-free children (DMFT/dmft = 0), at the age of 6–12. | NO | - ↓ NO in NS of children with active caries vs. control (p < 0.0001). | [78] |
| Study group: - 30 children with active caries (15 girls, 15 boys), DMFT/dmft ≥ 4. Control group: - 30 caries-free children (15 girls, 15 boys), DMFT/dmft = 0. Age of study participants: 6–12 years. | TAC | - ↑ TAC in NS of children with active caries vs. control (p < 0.0001). | [84] |
| Study group: - 77 children with active caries, at the age of 6–14. Control group: - 180 caries-free children, at the age of 6–14. | GSH, GSSG, GSH/GSSG | - ↑ GSH, GSSG in NS of children with active caries vs. control (p < 0.001, p = 0.012, respectively), - n.s difference ratio of GSH/GSSG in NS of children with active caries vs. control (p = 0.237). | [79] |
| Study group: - Ia girls with active caries (n = 15), at the age of 7–10, - Ib boys with active caries (n = 15), at the age of 7–10, - IIa girls with active caries (n = 15), at the age of 11–14, - IIb boys with active caries (n = 15), at the age of 11–14. Control group: - IIIa caries-free girls (n = 15), at the age of 7–10, - IIIb caries-free boys (n = 15), at the age of 7–10, - IVa caries-free girls (n = 15), at the age of 11–14, - IVb caries-free boys (n = 15), at the age of 11–14. | TAC | - ↑ TAC in NS of group Ia vs. group IIIa (p < 0.001), - ↑ TAC in NS of group B vs. group IIIb (p < 0.05), - ↑ TAC in NS of group IIa vs. IVa (p < 0.01), - ↑ TAC in NS of group IIb vs. IVb (p < 0.05). | [80] |
| Study group: - IA girls with active caries (n = 15), at the age of 7–10, - IB boys with active caries (n = 15), at the age of 7–10, - II A girls with active caries (n = 15), at the age of 11–14, - II B boys with active caries (n = 15), at the age of 11–14. Control group: - III A caries-free girls (n = 15), at the age of 7–10, - III B caries-free (n = 15), at the age of 7–10, - IV A caries-free girls (n = 15), at the age of 11–14, - IV B caries-free boys (n = 15), at the age of 11–14. | TAC | - ↑ TAC in NS of group IA vs. group III A (p < 0.001), - ↑ TAC in NS of group IB vs. group III B (p < 0.05), - ↑ TAC in NS of group II A vs. group IV A (p < 0.01), - ↑ TAC in NS group II B vs. group IV B (p < 0.05). | [81] |
| Study group: - Ia girls with active caries (n = 15), at the age of 7–10, - Ib boys with active caries (n = 15), at the age of 7–10, - IIa girls with active caries (n = 15), at the age of 11–15, - IIb boys with active caries (n = 15), at the age of 11–15. Control group: - IIIa caries-free girls (n = 15), at the age of 7–10, - IIIb caries-free boys (n = 15), at the age of 7–10, - IVa caries-free girls (n = 15), at the age of 11–15, - IVb caries-free boys (n = 15), at the age of 11–15. | TAC | - ↑ TAC in NS of group Ia vs. group IIIa (p < 0.05), - ↑ TAC in NS of group B vs. group IIIb (p < 0.05), - n.s difference in TAC level in NS of group IIa vs. group IVa (p > 0.05), - ↑ TAC in NS of group IIb vs. group IVb (p < 0.05). | [82] |
| Study group: - 50 children with active caries (DMFS/dfs ≥ 5), at the age of 6–12. Control group: - 50 caries-free children (DMFS/dfs = 0), at the age of 6–12. | TAC, MDA | - ↑ TAC, MDA in NS of children with active caries vs. control (p < 0.05, p < 0.05, respectively). | [83] |
| Study group: - 30 girls with active caries, - 30 boys with active caries. Control group: - 30 caries-free girls, - 30 caries-free boys. Age of study participants: 14–18 years. | TAC | - ↓ TAC in NS of girls with active caries vs. control (p < 0.001), - ↓ TAC in NS of boys with active caries vs. control (p < 0.001), - ↓ TAC in NS of patients with active caries (girls and boys) vs. control (p < 0.001). | [86] |
| Study group: - 50 people with active caries (25 women, 25 men), at the age of 15–17. Control group: - 50 caries-free people (25 women, 25 men), at the age of 15–17. | TAC | - ↑ TAC in NS of patients with active caries vs. control (p < 0.001). | [7] |
| Study group: - 50 people with active caries (25 women, 25 men). Control group: - 50 caries-free people (25 women, 25 men). Age of study participants: 15–17 years. | MDA | - ↑ MDA in NS of people with active caries vs. control (p < 0.001), - ↑ MDA in NS of women with active caries vs. caries-free women (p < 0.001), - ↑ MDA in NS of men with active caries vs. caries-free men (p < 0.001). | [94] |
| Study group: - 62 people with active caries, at the age of 15–19. Control group: - 57 caries-free people, at the age of 15–19. | TAC, MDA | - n.s difference in TAC level in NS and serum of people with active caries vs. control (p > 0.05, p > 0.05, respectively), - ↑ MDA in NS and serum of people with active caries vs. control (p = 0.001, p = 0.001, respectively). | [20] |
| Study group: - group I (n = 25) people with active caries, DMFT < 3, - group II (n = 25) people with active caries, DMFT < 10, - group III (n = 25) people with active caries, DMFT > 10. Control group: - 25 caries-free people, DMFT = 0. Age of study participants: 25–50 years. | TAC | - ↑ TAC in NS and serum of group I vs. control (p < 0.001, p < 0.001, respectively), - ↑ TAC in NS and serum of group II vs. control (p < 0.001, p < 0.001, respectively), - ↑ TAC in NS and serum of group III vs. control (p < 0.001, p < 0.001, respectively). | [87] |
| Study group: - 30 people with active caries (17 women, 13 men), at the age of 17–50. Control group: - 12 caries-free people (6 women, 6 men), at the age of 15–60. | MDA | - ↑ MDA in NS of people with active caries vs. control (p < 0.05). | [88] |
| Study group: - 50 people with active caries (25 women, 25 men). Control group: - 50 caries-free people (25 women, 25 men). Age of participants 15–17 years. | SOD, Px, GSH, CAT, UA | - n.s ↑ UA, Px, CAT in NS of people with active caries vs. control (p = 0.641, p = 0.072, p = 0.491, respectively), - ↑ GSH in NS of people with active caries vs. control (p = 0.004), - n.s ↓ SOD in NS of people with active caries vs. control (p = 0.935), - ↑ CAT in NS of men with active caries vs. women with active caries (p = 0.042), - ↑ SOD in NS of women with active caries vs. men with active caries (p < 0.0001). | [89] |
| Study group: - 60 people with active caries (DMFT > 10), at the age of 25–50. Control group: - 20 caries-free people (DMFT = 0), at the age of 25–50. | SOD | - ↑ SOD in NS of people with active caries vs. control (p < 0.0001). | [90] |
| Study group: - 204 people with different DMFT (128 women, 76 men), at the age of 19–83 (41.8 ± 14.5), including: * group I (CI = 0)—without caries (control group), * group II (CI = 1)—caries within the enamel and dentin, * group III (CI = 2)—extensive dentin caries. | AOPP | - n.s ↑ AOPP in NS of group II vs. group I (p > 0.05), - ↓ AOPP in NS of group III vs. group II (p < 0.05). | [93] |
| Patients | Analyzed Parameter | Results | Source |
|---|---|---|---|
| Study group: - 33 people with CP (14 women, 19 men), at the age of 41–45; - 16 people with gingivitis (12 women, 4 men), at the age of 35–43. Control group: - 37 generally healthy people (22 women, 15 men), at the age of 38–43. | 8-OHdG, GPx, TAC, SOD, MDA | - ↑ 8-OHdG, GPx, SOD, MDA in NS of people with CP vs. gingivitis (p < 0.05, p < 0.05, p < 0.05, p < 0.05, respectively), - ↑ 8-OHdG, GPx, TAC, SOD, MDA in NS of people with CP vs. control (p < 0.05, p < 0.05, p < 0.05, p < 0.05, p < 0.05, respectively). | [21] |
| Study group: - 15 people with AgP (13 women, 2 men), at the age of 22–29, - 36 people with CP (25 women, 11 men), at the age of 31–50. Control group: - No. 1 (matched to people with AgP) 21 generally healthy people (17 women, 4 men), at the age of 21–31, - No. 2 (matched to people with CP) 16 generally healthy people (10 women, 6 men), at the age of 32–50. | TAC | - ↓ TAC in NS of people with CP vs. control no. 2 (p < 0.05), - ↓ TAC in plasma of people with AgP vs. control no. 1 (p < 0.05), - ↓ TAC in plasma of people with CP vs. control no. 2 (p < 0.05). | [128] |
| Study group: - 35 people with CP (17 women, 18 men), at the age of 23–42, - 43 people with AgP (21 women, 22 men), at the age of 22–37. Control group: - 32 generally healthy people (15 women, 17 men), at the age of 26–38. | AOPP | - ↑ AOPP in NS and GCF of people with CP vs. AgP (p < 0.05, p < 0.05, respectively), - n.s ↑ AOPP in NS and serum of people with CP vs. control (p > 0.05, p > 0.05, respectively), - n.s ↑ AOPP in NS and serum of people with AgP vs. control (p > 0.05, p > 0.05, respectively), - ↑ AOPP in GCF of people with CP vs. control (p < 0.05), - ↑ AOPP in GCF of people with AgP vs. control (p < 0.05), - n.s ↑ AOPP in serum of people with CP vs. AgP (p > 0.05). | [24] |
| Study group: - 20 people with CP, at the age of 25–50. Control group: - 10 generally healthy people, at the age of 25–50. | 8-OHdG | - ↑ 8-OHdG in SS of people with CP vs. control (p ≤ 0.001), - ↓ 8-OHdG in SS of patients with CP after treatment vs. patients before treatment CP (p ≤ 0.001). | [12] |
| Study group: - 45 people with periodontitis (15 people with AgP, 30 people with CP), at the age of 45.2 ± 9.8. Control group: - 37 generally healthy people, at the age of 36.1 ± 10.3. | TAC, TOS | - ↓ TAC in NS of patients with periodontitis vs. control (p < 0.05), - n.s difference of TOS level in NS of patients with periodontitis vs. control (p > 0.05), - n.s difference of TAC and TOS level in NS of patients with AgP vs. CP (p > 0.05, p > 0.05, respectively). | [127] |
| Study group: - 55 people with CP, at the age of 30–50. Control group: - 55 generally healthy people, at the age of 30–50. | TAC, MDA | - ↑ MDA in NS and serum of people with CP vs. control (p = 0.0001, p = 0.0001, respectively). - n.s ↓ TAC in NS and serum of people with CP vs. control (p > 0.05, p > 0.05, respectively). | [133] |
| Study group: - 20 people with AgP, at the age of 17–23, - 20 people with CP, at the age of 32–40. Control group: - 20 generally healthy people, at the age of 17–23, - 20 generally healthy people, at the age of 32–40. | TAC, MDA | - ↑ TAC, MDA in NS of people with AgP vs. AgP control (p < 0.001, p < 0.001, respectively), - ↑ TAC, MDA in NS of people with CP vs. CP control (p < 0.001, p < 0.001, respectively), - ↑ TAC, MDA in NS of patients with CP vs. AgP (p < 0.001, p < 0.001, respectively). | [13] |
| Study group: - 33 people with CP (17 women, 16 men), at the age of 6–42, - 35 people with AgP (17 women, 18 men), at the age of 22–36. Control group: - 30 generally healthy people (14 women, 16 men), at the age of 26–37. | MDA, TOS, TAC, OSI | - ↑ MDA TOS, OSI in NS of people with CP vs. control (p > 0.05, p > 0.05, p > 0.05, respectively), - ↑ MDA TOS, OSI in NS of people with AgP vs. control (p > 0.05, p > 0.05, p > 0.05, respectively), - ↑ TOS, OSI in NS of people with AgP vs. CP (p < 0.05, p < 0.05, respectively), - ↓ TAC in NS of people with CP vs. control (p < 0.05), - ↓ TAC in NS of people with AgP vs. control (p < 0.05), - ↓ TAC in NS of people with AgP vs. CP (p < 0.05), - ↑ TOS, OSI in plasma of people with CP vs. control (p < 0.05, p < 0.05, respectively), - ↑ TOS, OSI in plasma of people with AgP vs. control (p < 0.05, p < 0.05, respectively), - ↑ TOS, OSI in plasma of people with AgP vs. CP (p < 0.05, p < 0.05, respectively), - ↓ TAC in plasma of people with CP vs. control (p < 0.05), - ↓ TAC in plasma of people with AgP vs. control (p < 0.05). | [130] |
| Study group: - 20 people with CP (10 women, 10 men), at the age of 29–58, - 20 people with chronic gingivitis (10 women, 10 men), at the age of 29–58. Control group: - 20 generally healthy people (10 women, 10 men), at the age of 29–55. | 8-OHdG | - ↑ 8-OHdG in SS of people with CP vs. control (p < 0.001), - ↑ 8-OHdG in SS of people with CP vs. chronic gingivitis (p < 0.001), - n.s ↑ 8-OHdG in SS of patients with chronic gingivitis vs. control (p > 0.05). | [136] |
| Study group: - 25 people with CP (11 women, 14 men), at the age of 45.8 ± 5.1. Control group: - 26 generally healthy people (15 women, 11 men), at the age of 45 ± 6.6. | 8-OHdG, MDA, 4-HNE | - ↑ 8-OHdG, MDA in NS of patients with CP before treatment vs. control (p < 0.001, p < 0.001, respectively), - ↑ 8-OHdG in NS of patients with CP before treatment vs. people with CP after treatment (p < 0.001), - ↑ MDA in NS of patients with CP after treatment vs. control (p < 0.05), - ↑ 4-HNE in serum of people with CP before treatment vs. control (p < 0.001), - ↑ 4-HNE in serum of people with CP after treatment vs. control (p < 0.05). | [132] |
| Study group: - 23 people with CP (14 women, 9 men), at the age of 43 ± 7.6. Control group: - 19 generally healthy people (8 women, 11 men), at the age of 39.1 ± 8.8. | TBARS, AOPP, AGE, TAC, FRAP | - ↑ TBARS in NS of men with CP vs. generally healthy men (p < 0.01), - ↓ TAC, FRAP in NS of women with CP vs. generally healthy women (p < 0.01, p < 0.01, respectively), - n.s difference of AOPP and AGE concentration in NS of people with CP vs. control (p > 0.05, p > 0.05, respectively). | [129] |
| Study group: - 58 people with CP (38 women, 20 men), on average 42.21 years old, - 42 people with AgP (26 women, 16 men), on average 35.85 years old. Control group: - 60 generally healthy people (38 women, 22 men), on average age 40.13 years old. | 8-OHdG | - ↑ 8-OHdG in NS of patients with periodontitis (CP and AgP) vs. control (p = 0.001), - ↑ 8-OHdG in NS of patients with CP vs. control (p = 0.001), - ↑ 8-OHdG in NS of patients with AgP vs. control (p = 0.001), - ↑ 8-OHdG in NS of patients with AgP vs. CP (p = 0.02). | [137] |
| Study group: - 48 people with CP (21 women, 27 men), at the age of 40.1 ± 7.3. Control group: - 35 people (16 women, 19 men), at the age of 42.1 ± 7.7. | MDA, TOS, SOD | - n.s difference in concentration of MDA in NS and serum of people with CP vs. control (p > 0.05, p > 0.05, respectively), - ↑ TOS, SOD in NS of people with CP vs. control (p < 0.05, p < 0.05, respectively), - ↓ MDA TOS, SOD in NS of patients with CP after SRP vs. people with CP before treatment (p < 0.05, p < 0.05, p < 0.05, respectively), - ↑ MDA TOS, SOD in GCF of people with CP vs. control (p < 0.05, p < 0.05, p < 0.05, respectively), - ↓ MDA TOS, SOD in GCF of people with CP after SRP vs. people with CP before treatment (p < 0.05, p < 0.05, p < 0.05, respectively), - n.s difference in concentration of MDA in serum of people with CP after SRP vs. people with CP before treatment (p > 0.05), - ↑ TOS, SOD in serum of people with CP vs. control (p < 0.05, p < 0.05, respectively), - ↓ TOS, SOD in serum of people with CP after SRP vs. people with CP before treatment (p < 0.05, p < 0.05, respectively). | [120] |
| Study group: - 23 people with CP (8 women, 15 men), at the age of 46.1 ± 5.1. Control group: - 25 generally healthy people (15 women, 10 men), at the age of 44.9 ± 6.8. | 8-OHdG | - ↑ 8-OHdG in NS of patients with CP vs. control (p < 0.001), - ↓ 8-OHdG in NS of patients with CP after SRP vs. people with CP before treatment (p < 0.001). | [152] |
| Study group: - 30 people with CP (16 women, 14 men), at the age of 30.7 ± 5.3. Control group: - 30 generally healthy people (15 women, 15 men), at the age of 35.7 ± 5.9. | MDA, SOD, CAT, GR | - ↑ MDA in NS of patients with CP vs. control (p < 0.001), - ↓ SOD, CAT, GR in NS of people with CP vs. control (p < 0.001, p < 0.001, p < 0.001, respectively). | [115] |
| Study group: - 25 people with CP (14 women, 11 men), at the age of 51.26 ± 7.4. Control group: - 25 generally healthy people (20 women, 5 men), at the age of 18.66 ± 2.0. | 8-OHdG, MDA, UA, TAC, GPx | - ↑ 8-OHdG, MDA in NS of people with CP vs. control (p < 0.05, p < 0.05, respectively), - ↓ UA, TAC, GPx in NS of people with CP vs. control (p < 0.05, p < 0.05, p < 0.05, respectively). | [116] |
| Study group: - 24 people with gingivitis, - 23 people with periodontitis. Control group: - 23 generally healthy people. Age of study participants: 20–55 years. | SOD, thiol | - ↑ SOD, thiol in NS of generally healthy after treatment vs. before treatment (p < 0.05, p < 0.05, respectively), - ↑ SOD, thiol in NS of patients with gingivitis after treatment vs. before treatment (p < 0.05, p < 0.05, respectively), - ↑ SOD, thiol in NS of patients with periodontitis after treatment vs. before treatment (p < 0.05, p < 0.05, respectively). | [117] |
| Study group: - 121 people with CP (76 women, 45 men), at the age of 48.55 ± 10.42, - 18 people with AgP (11 women, 7 men), at the age of 34.11 ± 5.61. Control group: - 69 generally healthy people (46 women, 23 men), at the age of 31.57 ± 12.03. | GR | - ↑ GR in NS of people with CP vs. control (p < 0.001), - ↑ GR in NS of people with AgP vs. control (p < 0.001), - ↑ GR in NS of people with AgP vs. people with CP (p < 0.001). | [118] |
| Study group: - 22 people with CP including: * group A (n = 14)—patients who responded positively to SRP treatment, * group B (n = 8)—patients who did not respond to SRP treatment. Age of participants: 35–44 years. | SOD | - ↑ SOD in NS of group B after treatment vs. before treatment (p = 0.02). | [121] |
| Study group: - 23 people with CP. Control group: - 11 generally healthy people. Age of study participants: 35–55 years old. | MPO | - ↑ MPO in SS of patients with CP vs. control (p < 0.05). | [122] |
| Study group: - 42 people with CP including: * OHI group—21 people who have undergone only oral instruction, at the age of 38.1 ± 10, * SRP group—21 people undergoing SRP treatment, at the age of 39.2 ± 11.5. Control group: - 21 healthy people over 25 years of age. | ALB, UA, GPx, SOD, TAC | - n.s difference in concentration of ALB, UA, GPx, SOD, TAC in NS of OHI group after treatment vs. before treatment (p > 0.05, p > 0.05, p > 0.05, p > 0.05, p > 0.05, respectively), - ↑ ALB, UA, GPx, TAC in NS of SRP group after treatment vs. before treatment (p < 0.001, p < 0.001, p < 0.001, p < 0.005, respectively), - ↓ SOD in NS of SRP group after treatment vs. before treatment (p < 0.005), - ↓ ALB, GPx, TAC in NS of SRP group before treatment vs. control (p = 0.039, p < 0.0001, p = 0.001, respectively), - ↑ SOD in NS of SRP group before treatment vs. control (p = 0.021). | [123] |
| Study group: - 225 people with CP (122 women, 103 men). | Cu/Zn SOD, Mn SOD, CAT | - positive correlation between Cu/Zn SOD concentration in SS of persons with CP and BOP index and increase in PD value (p = 0.02, p = 0.04, respectively), - positive correlation between CAT concentration in SS of people with CP and PI and BOP index (p = 0.02, p = 0.02, respectively). | [124] |
| Study group: - 15 people with CP (7 women, 8 men), at the age of 41.18 ± 7.06. Control group: - 5 healthy people (2 women, 3 men), at the age of 29.6 ± 5.81. | Melatonin | - n.s difference in concentration of melatonin in NS and plasma of patients with CP vs. control (p = 0.266, p = 0.933, respectively), - ↓ concentration of melatonin in gingival tissue homogenates of people with CP vs. control (p = 0.015). | [18] |
| Study group: - 20 people with gingivitis (2 women, 18 men), at the age of 18–40 (29.9 ± 7.0), - 20 people with CP (4 women, 16 men), at the age of 40–55 (47.2 ± 4.6), - 20 people with AgP (5 women, 15 men), at the age of 28–40 (34.7 ± 5.4). Control group: - 10 generally healthy people (3 women, 7 men), at the age of 20–44 (28.3 ± 6.7). | Melatonin | - ↓ melatonin in NS of patients with gingivitis vs. control (p < 0.05), - ↓ melatonin in NS of patients with CP vs. control (p < 0.05), - ↓ melatonin in NS of patients with AgP vs. control (p < 0.05). | [125] |
| Study group: - 15 people with gingivitis, - 15 people with CP. Control group: - 15 generally healthy people. Age of study participants: 20–45 years old. | Melatonin | - ↓ melatonin in NS and GCF of patients with CP vs. control (p < 0.05, p < 0.05, respectively), - n.s difference in concentration of melatonin in NS and GCF of people with gingivitis vs. control (p > 0.05, p > 0.05, respectively). | [126] |
| Study group: - 58 people with CP (group I + II), (29 women, 29 men), including: * group I (III stage of advancement CP), n = 34, (16 women, 18 men), * group II (IV stage of advancement CP), n = 24, (13 women, 11 men). Control group: - 29 generally healthy people, (17 women, 12 men). Age of study participants: 20–55 years. | TOS, TAC, OSI, FRAP | - ↑ TOS in NS, SS and GCF of group I vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ TOS in NS, SS and GCF of group II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ TOS in NS, SS and GCF of group I + II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↓ TAC in NS, SS and GCF of group I vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↓ TAC in NS, SS and GCF of group II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↓ TAC in NS, SS and GCF of group I + II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ OSI in NS, SS and GCF of group I vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ OSI in NS, SS and GCF of group II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ OSI in NS, SS and GCF of group I + II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↓ FRAP in NS and SS of group I vs. control (p < 0.001, p < 0.001, respectively), - ↓ FRAP in NS and SS of group II vs. control (p < 0.001, p < 0.001, respectively), - ↓ FRAP in NS and SS of group I + II vs. control (p < 0.001, p < 0.001, respectively), - n.s difference in concentration of FRAP in GCF of group I vs. control (p > 0.05), - n.s difference in concentration of FRAP in GCF of group II vs. control (p > 0.05), - n.s difference in concentration of FRAP in GCF of group I + II vs. control (p > 0.05). | [131] |
| Study group: - 82 children of different periodontological and carious status (47 girls, 35 boys), at the age of 4–18 (13.4 ± 3.6). | TAC, TBARS, AOPP, AGE | - positive correlation between TAC level and patient age (p = 0.03), - ↑ TBARS by 35% in boys vs. girls (p = 0.01), - positive correlation between TAC level and OHI, PBI index (p = 0.01, p = 0.001, respectively). | [76] |
| Study group: - 110 people with CP (71 women, 39 men), at the age of 48.34 ± 10.78. Control group: - 50 generally healthy people (35 women, 15 men), at the age of 31.80 ± 13.75. | 8-OHdG, 4-HNE | - ↑ 8-OHdG, 4-HNE in NS of people with CP vs. contol (p < 0.001, p = 0.001, respectively). | [138] |
| Study group: - 24 people with CP (12 women, 12 men), at the age of 30–55 (42.46 ± 6.70). Control group: - 24 generally healthy people (12 women, 12 men), at the age of 18–30 (24.92 ± 3.50). | 8-OHdG | - ↑ 8-OHdG in GCF of people with CP before treatment vs. control (p < 0.001), - n.s ↑ 8-OHdG in NS of patients with CP before treatment vs. control (p = 0.09), - ↓ 8-OHdG in GCF of people with CP after treatment vs. before treatment (p < 0.001), - n.s ↓ 8-OHdG in NS of patients with CP after treatment vs. before treatment (p = 0.076). | [140] |
| Study group: - 60 people with CP (group I + II), (30 women, 30 men), at the age of 20–55, including: * Group I (III stage of advancement CP), n = 36, (17 women, 19 men), at the age of 43.3 ± 8.99, * group II (IV stage of advancement CP), n = 24, (13 women, 11 men), at the age of 44.0 ± 8.03. Control group: - 30 generally healthy people (17 women, 13 men), at the age of 20–55 (40.3 ± 9.58). | NO, peroxynitrite, S-nitrosothiols | - ↑ NO in NS and SS of group I vs. control (p < 0.01, p < 0.01, respectively), - n.s ↑ NO in NS and GCF of group II vs. control (p > 0.05, p > 0.05, respectively), - ↑ NO in NS and SS of group I + II vs. control (p < 0.01, p < 0.001, respectively), - ↑ NO in SS of group II vs. control (p < 0.001), - n.s ↑ NO in GCF of group I vs. control (p > 0.05), - n.s ↑ NO in GCF of group I + II vs. control (p > 0.05), - ↑ peroxynitrite in NS, SS and GCF of group I vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ peroxynitrite in NS, SS and GCF of group II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ peroxynitrite in NS, SS and GCF of group I + II vs. control (p < 0.001, p < 0.001, p < 0.001, respectively), - ↑ S-nitrosothiols in NS and SS of group I vs. control (p < 0.05, p < 0.001, respectively), - n.s ↑ S-nitrosothiols in NS and GCF of group II vs. control (p > 0.05, p > 0.05, respectively), - ↑ S-nitrosothiols in NS of group I + II vs. control (p < 0.05, p < 0.001, respectively), - ↑ S-nitrosothiols in SS of group II vs. control (p < 0.001), - n.s ↑ S-nitrosothiols in GCF of group I vs. control (p > 0.05), - n.s ↑ S-nitrosothiols in GCF of group I + II vs. control (p > 0.05). | [143] |
| Study group: - 30 people with gingivitis, - 30 people with CP. Control group: - 30 generally healthy people. Age of study participants: 20–60 years. | NO | - ↑ NO in NS patients with gingivitis and CP before treatment vs. control (p < 0.0001, p < 0.0001, respectively), - ↓ NO in NS patients with gingivitis and CP after treatment vs. before treatment (p < 0.0001, p < 0.0001, respectively). | [144] |
| Study group: - 65 people with CP (38 women, 27 men), at the age of 41.84 ± 8.43. Control group: - 48 generally healthy people (23 women, 25 men), at the age of 35.74 ± 8.08. | NO | - ↑ NO in NS of patients with CP vs. control (p < 0.05). | [145] |
| Study group: - 22 people with CP. Control group: - 16 generally healthy people. | NO | - n.s ↓ NO in NS of patients with CP vs. control (p > 0.05). | [146] |
| Study group: - 9 people with gingivitis (8 women, 1 man), at the age of 23–41 (28.20 ± 7.24), - 15 people with CP (10 women, 5 men), at the age of 35–53 (44.30 ± 6.90). Control group: - 11 generally healthy people (10 women, 1 man), at the age of 23–45 (28.64 ± 9.47). | NO | - n.s difference in concentration of NO in NS of the patients with CP and gingivitis vs. control (p = 0.421, p = 0.184, respectively), - ↓ NO in NS of people with CP vs. people with gingivitis (p < 0.0001). | [147] |
| Study group: - 89 people with CP (36 women, 53 men), at the age of 42.2 ± 8.4. Control group: - 54 generally healthy people (29 women, 25 men), at the age of 34.3 ± 1.2. | NO | - ↓ NO in NS of people with CP vs. control (p < 0.01). | [148] |
| Study group: - 242 people with CP (151 women, 91 men), at the age of 48–93, including: * group I (I stage of advancement CP), n = 85, * group II (II stage of advancement CP), n = 79, * group III (III stage of advancement CP), n = 32, * group IV (IV stage of advancement CP), n = 23. | NO | - ↑ NO in NS of group IV vs. group I (p = 0.015). | [151] |
| Study group: - 20 people with gingivitis (12 women, 8 men), at the age of 33.9 ± 8.38, - 20 people with CP (11 women, 9 men), at the age of 42.65 ± 8.04. Control group: - 20 generally healthy people (10 women, 10 men), at the age of 29.9 ± 2.17. | Nitrite level, Nitrate level | - n.s difference in concentration of nitrite and nitrate in NS of people with gingivitis vs. control (p > 0.05, p > 0.05, respectively), - n.s difference in concentration of nitrite and nitrate in NS of people with CP vs. control (p > 0.05, p > 0.05, respectively), - ↑ nitrite level in GCF of people with gingivitis and CP vs. control (p < 0.001, p < 0.001, respectively) - n.s difference in concentration of nitrate in GCF of people with gingivitis and CP vs. control (p > 0.05, p > 0.05, respectively). | [149] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skutnik-Radziszewska, A.; Zalewska, A. Salivary Redox Biomarkers in the Course of Caries and Periodontal Disease. Appl. Sci. 2020, 10, 6240. https://doi.org/10.3390/app10186240
Skutnik-Radziszewska A, Zalewska A. Salivary Redox Biomarkers in the Course of Caries and Periodontal Disease. Applied Sciences. 2020; 10(18):6240. https://doi.org/10.3390/app10186240
Chicago/Turabian StyleSkutnik-Radziszewska, Anna, and Anna Zalewska. 2020. "Salivary Redox Biomarkers in the Course of Caries and Periodontal Disease" Applied Sciences 10, no. 18: 6240. https://doi.org/10.3390/app10186240
APA StyleSkutnik-Radziszewska, A., & Zalewska, A. (2020). Salivary Redox Biomarkers in the Course of Caries and Periodontal Disease. Applied Sciences, 10(18), 6240. https://doi.org/10.3390/app10186240






