Video Game-Based Therapy on Balance and Gait of Patients with Stroke: A Systematic Review
Abstract
1. Introduction
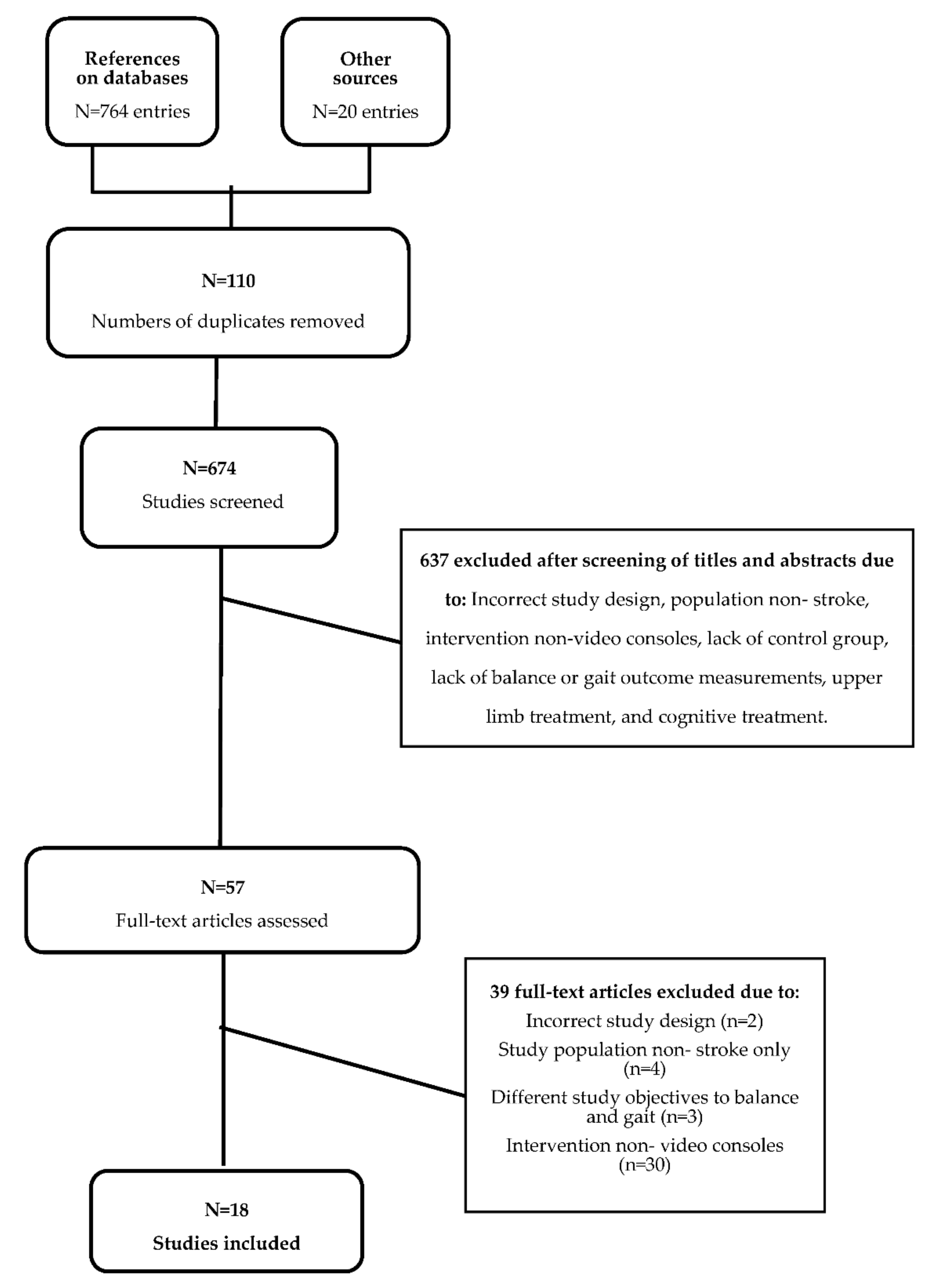
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Extracting Information and Managing Data
2.5. Assessing the Quality of Evidence
3. Results
3.1. Characteristics of the Included Studies
3.1.1. Participants
3.1.2. Intervention
3.1.3. Outcomes
3.1.4. Main Results
3.2. Quality of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO MONICA Project Principal Investigators. The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): A major international collaboration. WHO MONICA Project Principal Investigators. J. Clin. Epidemiol. 1988, 41, 105–114. [Google Scholar] [CrossRef]
- World Heart Organization Stroke. Neurological Disorders: Public Health Challenges; World Heart Organization Stroke: Geneva, Switzerland, 2006; pp. 151–163. [Google Scholar]
- Federación Española de Ictus. Código Ictus. Available online: https://ictusfederacion.es/infoictus/codigo-ictus/ (accessed on 23 June 2020).
- Ordahan, B.; Ay, K.; Basaran, A.; Turkoglu, G.; Kucuksarac, S.; Cubukcu, M.; Tekin, L.; Polat, A.D.; Kuran, B. Impact of exercises administered to stroke patients with balance trainer on reha-bilitation results: A randomized controlled study. Hippokratia 2015, 19, 125–130. [Google Scholar] [PubMed]
- Latham, N.K.; Jette, D.U.; Slavin, M.; Richards, L.G.; Procino, A.; Smout, R.J.; Horn, S.D. Physical therapy during stroke rehabilitation for people with different walking abilities. Arch. Phys. Med. Rehabil. 2005, 86, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Weiss, P.L.; Kizony, R.; Feintuch, U.; Katz, N. Virtual reality in neurorehabilitation. In Textbook of Neural Repair and Rehabilitation; Selzer, M., Clarke, S., Cohen, L., Duncan, P., Gage, F., Eds.; Cambridge University Press: Cambridge, UK, 2010; pp. 182–197. [Google Scholar]
- Olguín Carbajal, M.; Rivera Zárate, I.; Hernández Montañez, E. Introducción a la Realidad Virtual. Polibits 2006, 33, 11–15. [Google Scholar] [CrossRef]
- Bayón, M.; Martínez, J. Rehabilitación del ictus mediante realidad virtual. Rehabilitacion 2010, 44, 256–260. [Google Scholar] [CrossRef]
- Deutsch, J.E.; Lewis, J.A.; Burdea, G. Technical and patient performance using a virtual reality-integrated Telerehabilitation system: Preliminary finding. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 30–35. [Google Scholar] [CrossRef]
- Piron, L.; Turolla, A.; Agostini, M.; Zucconi, C.; Cortese, F.; Zampolini, M.; Zannini, M.; Dam, M.; Ventura, L.; Battauz, M.; et al. Exercises for paretic upper limb after stroke: A combined virtual-reality and telemedicine approach. J. Rehabil. Med. 2009, 41, 1016–1020. [Google Scholar] [CrossRef]
- Grigoras, A.V.; Matei, D.; Ignat, E.B. Non-Immersive Virtual Reality for Upper Limb Rehabilitation in Stroke Survivors-A Feasibility Study. Balneo Res. J. 2018, 9, 232–239. [Google Scholar] [CrossRef]
- Törnbom, K.; Danielsson, A. Experiences of treadmill walking with non-immersive virtual reality after stroke or acquired brain injury—A qualitative study. PLoS ONE 2018, 13, e0209214. [Google Scholar] [CrossRef]
- Cortés-Pérez, I.; Nieto-Escamez, F.A.; Obrero-Gaitán, E. Immersive Virtual Reality in Stroke Patients as a New Approach for Reducing Postural Disabilities and Falls Risk: A Case Series. Brain Sci. 2020, 10, 296. [Google Scholar] [CrossRef]
- Laver, K.; George, S.; Thomas, S.; Deutsch, J.; Crotty, M. Virtual reality for stroke rehabilitation (Review) summary of findings for the main comparison. Virtual Real. Stroke Rehabil. 2017, 80, 57–62. [Google Scholar]
- Li, Z.; Han, X.-G.; Sheng, J.; Ma, S.J. Virtual reality for improving balance in patients after stroke: A systematic review and meta-analysis. Clin. Rehabil. 2015, 30, 432–440. [Google Scholar] [CrossRef]
- Maier, M.; Rubio Ballester, B.; Duff, A.; Duarte Oller, E.; Verschure, P.F.M.J. Effect of Specific Over Nonspecific VR-Based Rehabilitation on Poststroke Motor Recovery: A Systematic Meta-analysis. Neurorehabil. Neural Repair 2019, 33, 112–129. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Castilla Alvarez, L. Buenas Prácticas de Accesibilidad en Videojuegos, 1st ed.; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2012. [Google Scholar]
- Deutsch, J.E.; Borbely, M.; Filler, J.; Huhn, K.; Guarrera-Bowlby, P. Use of a Low-Cost, Commercially Available Gaming Console (Wii) for Rehabilitation of an Adolescent With Cerebral Palsy. Phys. Ther. 2008, 88, 1196–1207. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.W.; McNeill, M.D.J.; Charles, D.K.; Morrow, P.J.; Crosbie, J.H.; McDonough, S.M. Optimising engagement for stroke rehabilitation using serious games. Vis. Comput. 2009, 25, 1085–1099. [Google Scholar] [CrossRef]
- Cheok, G.; Tan, D.; Low, A.; Hewitt, J. Is Nintendo Wii an Effective Intervention for Individuals with Stroke? A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2015, 16, 923–932. [Google Scholar] [CrossRef]
- Corbetta, D.; Imeri, F.; Gatti, R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: A systematic review. J. Physiother. 2015, 61, 117–124. [Google Scholar] [CrossRef]
- Lohse, K.R.; Hilderman, C.G.E.; Cheung, K.L.; Tatla, S.; Van der Loos, H.F.M. Virtual Reality Therapy for Adults Post-Stroke: A Systematic Review and Meta-Analysis Exploring Virtual Environments and Commercial Games in Therapy. PLoS ONE 2014, 9, e93318. [Google Scholar] [CrossRef]
- Wolfenden, L.; Jones, J.; Williams, C.M.; Finch, M.; Wyse, R.J.; Kingsland, M.; Tzelepis, F.; Wiggers, J.; Williams, A.J.; Seward, K.; et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst. Rev. 2016, 2016, 1–639. [Google Scholar] [CrossRef]
- Hutton, B.; Catalá-López, F.; Moher, D. La extensión de la declaración PRISMA para revisiones sistemáticas que incorporan metaanálisis en red: PRISMA-NMA. Med. Clin. 2016, 147, 262–266. [Google Scholar] [CrossRef]
- Barcala, L.; Grecco, L.A.C.; Colella, F.; Lucareli, P.R.G.; Salgado, A.S.I.; Oliveira, C.S. Visual Biofeedback Balance Training Using Wii Fit after Stroke: A Randomized Controlled Trial. J. Phys. Ther. Sci. 2013, 25, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Bower, K.J.; Clark, R.A.; McGinley, J.L.; Martin, C.L.; Miller, K.J. Clinical feasibility of the Nintendo WiiTM for balance training post-stroke: A phase II randomized controlled trial in an inpatient setting. Clin. Rehabil. 2014, 28, 912–923. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.H.; Lee, K.J.; Song, C.H. Virtual-Reality Balance Training with a Video-Game System Improves Dynamic Balance in Chronic Stroke Patients. Tohoku J. Exp. Med. 2012, 228, 69–74. [Google Scholar] [CrossRef]
- Hung, J.W.; Chou, C.X.; Chang, H.F.; Wu, W.C.; Hsieh, Y.W.; Chen, P.C.; Yu, M.Y.; Chang, C.C.; Lin, J.R. Cognitive effects of weight-shifting controlled exergames in patients with chronic stroke: A pilot randomized comparison trial. Eur. J. Phys. Rehabil. Med. 2017, 53, 694–702. [Google Scholar] [PubMed]
- Hung, J.W.; Chou, C.X.; Hsieh, Y.W.; Wu, W.C.; Yu, M.Y.; Chen, P.C.; Chang, H.F.; Ding, S.E. Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Arch. Phys. Med. Rehabil. 2014, 95, 1629–1637. [Google Scholar] [CrossRef]
- Kannan, L.; Vora, J.; Bhatt, T.; Hughes, S.L. Cognitive-motor exergaming for reducing fall risk in people with chronic stroke: A randomized controlled trial. NeuroRehabilitation 2019, 44, 493–510. [Google Scholar] [CrossRef]
- Karasu, A.U.; Batur, E.B.; Karatas, G.K. Effectiveness of WII-based rehabilitation in stroke: A randomized controlled study. J. Rehabil. Med. 2018, 50, 406–412. [Google Scholar] [CrossRef]
- Kim, E.K.; Kang, J.H.; Park, J.S.; Jung, B.H. Clinical Feasibility of Interactive Commercial Nintendo Gaming for Chronic Stroke Rehabilitation. J. Phys. Ther. Sci. 2012, 24, 901–903. [Google Scholar] [CrossRef]
- Lee, H.Y.; Kim, Y.L.; Lee, S.M. Effects of virtual reality-based training and task-oriented training on balance performance in stroke patients. J. Phys. Ther. Sci. 2015, 27, 1883–1888. [Google Scholar] [CrossRef]
- Lee, H.-C.; Huang, C.-L.; Ho, S.-H.; Sung, W.-H. The Effect of a Virtual Reality Game Intervention on Balance for Patients with Stroke: A Randomized Controlled Trial. Games Health J. 2017, 6, 303–311. [Google Scholar] [CrossRef]
- Lee, M.; Shin, D.; Song, C. Canoe game-based virtual reality training to improve trunk postural stability, balance, and upper limb motor function in subacute stroke patients: A randomized controlled pilot study. J. Phys. Ther. Sci. 2016, 28, 2019–2024. [Google Scholar] [CrossRef] [PubMed]
- Morone, G.; Tramontano, M.; Iosa, M.; Shofany, J.; Iemma, A.; Musicco, M.; Paolucci, S.; Caltagirone, C. The efficacy of balance training with video game-based therapy in subacute stroke patients: A randomized controlled trial. Biomed Res. Int. 2014, 2014, 580861. [Google Scholar] [CrossRef] [PubMed]
- Park, D.S.; Lee, D.G.; Lee, K.; Lee, G.C. Effects of Virtual Reality Training using Xbox Kinect on Motor Function in Stroke Survivors: A Preliminary Study. J. Stroke Cerebrovasc. Dis. 2017, 26, 2313–2319. [Google Scholar] [CrossRef] [PubMed]
- Pedreira da Fonseca, E.; Ribeiro da Silva, N.M.; Pinto, E.B. Therapeutic Effect of Virtual Reality on Post-Stroke Patients: Randomized Clinical Trial. J. Stroke Cerebrovasc. Dis. 2016, 26, 94–100. [Google Scholar] [CrossRef]
- Rajaratnam, B.S.; Gui KaiEn, J.; Lee JiaLin, K.; SweeSin, K.; Sim FenRu, S.; Enting, L.; Ang YiHsia, E.; KeatHwee, N.; Yunfeng, S.; Woo YingHowe, W.; et al. Does the Inclusion of Virtual Reality Games within Conventional Rehabilitation Enhance Balance Retraining after a Recent Episode of Stroke? Rehabil. Res. Pract. 2013, 2013, 649561. [Google Scholar] [CrossRef]
- Singh, D.K.A.; Mohd Nordin, N.A.; Aziz, N.A.A.; Lim, B.K.; Soh, L.C. Effects of substituting a portion of standard physiotherapy time with virtual reality games among community-dwelling stroke survivors. BMC Neurol. 2013, 13, 199. [Google Scholar] [CrossRef]
- Song, G.b.; Park, E. cho Effect of virtual reality games on stroke patients’ balance, gait, depression, and interpersonal relationships. J. Phys. Ther. Sci. 2015, 27, 2057–2060. [Google Scholar] [CrossRef]
- Yatar, G.I.; Yildirim, S.A. Wii Fit balance training or progressive balance training in patients with chronic stroke: A randomised controlled trial. J. Phys. Ther. Sci. 2015, 27, 1145–1151. [Google Scholar] [CrossRef]
- Cho, K.H.; Kim, M.K.; Lee, H.J.; Lee, W.H. Virtual Reality Training with Cognitive Load Improves Walking Function in Chronic Stroke Patients. Tohoku J. Exp. Med. 2015, 236, 273–280. [Google Scholar] [CrossRef]
- You, S.H.; Jang, S.H.; Kim, Y.H.; Hallett, M.; Ahn, S.H.; Kwon, Y.H.; Kim, J.H.; Lee, M.Y. Virtual reality-induced cortical reorganization and associated locomotor recovery in chronic stroke: An experimenter-blind randomized study. Stroke 2005, 36, 1166–1171. [Google Scholar] [CrossRef]
- Wang, C.-Y.; Hwang, W.-J.; Fang, J.-J.; Sheu, C.-F.; Leong, I.-F.; Ma, H.-I. Comparison of Virtual Reality Versus Physical Reality on Movement Characteristics of Persons With Parkinson’s Disease: Effects of Moving Targets. Arch. Phys. Med. Rehabil. 2011, 92, 1238–1245. [Google Scholar] [CrossRef] [PubMed]
- Baram, Y.; Miller, A. Virtual reality cues for improvement of gait in patients with multiple sclerosis. Neurology 2006, 66, 178–181. [Google Scholar] [CrossRef]
- Chang, W.H.; Sohn, M.K.; Lee, J.; Kim, D.Y.; Lee, S.G.; Shin, Y.I.; Oh, G.J.; Lee, Y.S.; Joo, M.C.; Han, E.Y.; et al. Predictors of functional level and quality of life at 6 months after a first-ever stroke: The KOSCO study. J. Neurol. 2016, 263, 1166–1177. [Google Scholar] [CrossRef]
- Murie-Fernández, M.; Irimia, P.; Martínez-Vila, E.; John Meyer, M.; Teasell, R. Neurorrehabilitación tras el ictus. Neurologia 2010, 25, 189–196. [Google Scholar] [CrossRef]
- De Moya, P.; Bertomeu, B.; Broseta, V. Evaluación y rehabilitación del equilibrio mediante posturografía. Rehabilitacion 2005, 39, 315–323. [Google Scholar] [CrossRef]
- Balaguer García, R.; Pitarch Corresa, S.; Baydal Bertomeu, J.M.; Morales Suárez-Varela, M.M. Posturografía estática con pruebas dinámicas. Utilidad de los parámetros biomecánicos en la valoración del paciente vestibular. Acta Otorrinolaringol. Esp. 2012, 63, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Hernández, J.G.; Saldaña, L.M.; Rodríguez, M.P.; Almeida, A.M.; Tejero, J.P.; Alted, C.G. Relación entre las pruebas de funcionalidad de la marcha en personas con daño cerebral adquirido en fase subaguda. AGON Int. J. Sport Sci. 2012, 2, 6–16. [Google Scholar]
- Bogle Thorbahn, L.D.; Newton, R.A. Use of the Berg Balance Test to predict falls in elderly persons. Phys. Ther. 1996, 76, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Berg, K. Measuring balance in the elderly: Preliminary development of an instrument. Physiother. Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Blum, L.; Korner-Bitensky, N. Usefulness of the Berg Balance Scale in Stroke Rehabilitation: A Systematic Review. Phys. Ther. 2008, 88, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Wan, B.; Huang, R.; Xiong, W.; Miao, C.; Zhang, F. Meta-analysis of clinical efficacy of postoperative rehabilitation nursing for patients with cerebral hemorrhage. Acta Microsc. 2020, 29, 820–829. [Google Scholar]
- Hugues, A.; Di Marco, J.; Ribault, S.; Ardaillon, H.; Janiaud, P.; Xue, Y.; Zhu, J.; Pires, J.; Khademi, H.; Rubio, L.; et al. Limited evidence of physical therapy on balance after stroke: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0221700. [Google Scholar] [CrossRef] [PubMed]
- Dee, M.; Lennon, O.; O’Sullivan, C. A systematic review of physical rehabilitation interventions for stroke in low and lower-middle income countries. Disabil. Rehabil. 2020, 42, 473–501. [Google Scholar] [CrossRef] [PubMed]
- Kwakkel, G. Intensity of practice after stroke: More is better. Schweiz. Arch. Neurol. Psychiatr. 2009, 160, 295–298. [Google Scholar]
- Adamovich, S.V.; Fluet, G.G.; Tunik, E.; Merians, A.S. Sensorimotor training in virtual reality: A review. NeuroRehabilitation 2009, 25, 29–44. [Google Scholar] [CrossRef]

| CINAHL Complete |
| #1 (MM “Stroke”) |
| #2 (TX “Cerebrovascular accident”) |
| #3 #1 OR #2 |
| #4 (MH “Virtual reality”) |
| #5 (MM “Virtual reality exposure therapy”) |
| #6 (MM “Video games”) |
| #7 (TX “Commercial gaming devices”) |
| #8 (TX “gaming”) |
| #9 (TX “console”) |
| #10 (TX “console games”) |
| #11 (TX “Wii”) |
| #12 (TX “Play Station”) |
| #13 (TX “Xbox”) |
| #14 (TX “Kinect”) |
| #15 (TX “Nintendo Switch”) |
| #16 (TX “Play station virtual reality”) |
| #17 (TX “Eye toy”) |
| #18 #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 |
| #19 (MM “Balance, Postural”) |
| #20 (MM “Gait”) |
| #21 (MM “Gait Disorders, Neurologic”) |
| #22 (MM “Gait Training”) |
| #23 (TX “Berg Balance Scale”) |
| #24 (TX “Timed Up and Go “) |
| #25 (TX “6 min walk test”) |
| #26 (TX “10 metre walk test” |
| #27 (TX “Functional reach test”) |
| #28 (TX “Posturography”) |
| #29 #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 |
| #30 #3 AND #18 AND #29 |
| Number of results obtained in CINAHL |
| 153 |
| Medline |
| #1 (MM “Stroke”) |
| #2 (TX “Cerebrovascular accident”) |
| #3 #1 OR #2 |
| #4 (MH “Virtual reality”) |
| #5 (MM “Virtual reality exposure therapy”) |
| #6 (MM “Video games”) |
| #7 (TX “Commercial gaming devices”) |
| #8 (TX “gaming”) |
| #9 (TX “console”) |
| #10 (TX “console games”) |
| #11 (TX “Wii”) |
| #12 (TX “Play Station”) |
| #13 (TX “Xbox”) |
| #14 (TX “Kinect”) |
| #15 (TX “Nintendo Switch”) |
| #16 (TX “Play station virtual reality”) |
| #17 (TX “Eye toy”) |
| #18 #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 |
| #19 (MM “Postural Balance”) |
| #20 (TX “Postural Balance”) |
| #21 (MM “Gait”) |
| #22 (MM “Gait Disorders, Neurologic”) |
| #23 (TX “Berg Balance Scale”) |
| #24 (TX “Timed Up and Go “) |
| #25 (TX “6 min walk test”) |
| #26 (TX “10 metre walk test” |
| #27 (TX “Functional reach test”) |
| #28 (TX “Posturography”) |
| #29 #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 |
| #30 #3 AND #18 AND #29 |
| Number of results obtained in Medline |
| 152 |
| PubMed |
| #1 “Stroke”[MeSH Terms] |
| #2 “cerebrovascular accident”[Title/Abstract] |
| #3 #1 OR #2 |
| #4 “Virtual reality”[MeSH Terms] |
| #5 “Virtual Reality Exposure Therapy”[MeSH Terms] |
| #6 “Virtual reality”[Title/Abstract] |
| #7 “Video games”[Title/Abstract] |
| #8 “Commercial gaming devices”[Title/Abstract] |
| #9 “gaming”[Text Word] |
| #10 “Commercial gaming devices”[Text Word] |
| #11 “console”[Text Word] |
| #12 “console games”[Text Word] |
| #13 “Wii”[Text Word] |
| #14 “play station”[Text Word] |
| #15 ”Xbox”[Text Word] |
| #16 “Kinect”[Text Word]13 |
| #17 “Nintendo switch”[Text Word] |
| #18 “Play station virtual reality”[Text Word] |
| #19 “Eye toy”[Text Word] |
| #20 #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR # |
| 13 OR #14 OR #15 OR #16 OR #17 OR #19 |
| #21 “Postural Balance”[MeSH Terms] |
| #22 “Gait”[MeSH Terms] |
| #23 “Gait Disorders, Neurologic”[MeSH Terms] |
| #24 “Gait training”[Text Word] |
| #25 “Berg Balance Scale”[Text Word] |
| #26 “Timed Up and Go”[Text Word] |
| #27 “6 min walk test”[Text Word] |
| #28 “10 metre walk test”[Text Word] |
| #29 “Posturography”[Text Word] |
| #30 “Functional reach test”[Text Word] |
| #31 “Balance” [Title/Abstract] |
| #32 #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 |
| #33 #3 AND #20 AND #32 |
| Number of results obtained in PubMed |
| 430 |
| PEDro |
| #”Stroke” “virtual reality” “gait” “balance” |
| Number of results obtained in PEDro |
| 24 |
| Scopus |
| #1 Tittle-Abs (“Stroke”) |
| #2 Tittle-Abs (“Virtual reality”) |
| #3 Tittle-Abs (“video games”) |
| #4 #2 OR #3 |
| #5 Tittle-Abs (“Physical Therapy”) |
| #6 Tittle-Abs (“Rehabilitation”) |
| #7 #5 OR #6 |
| #8 Tittle-Abs (“Balance”) |
| #9 Tittle-Abs (“Gait”) |
| #10 Tittle-Abs (“Postural Balance”) |
| #11 Tittle-Abs (“Postural Control”) |
| #12 #8 OR #9 OR #10 OR #11 |
| #13 #1 AND #4 and #7 and #12 |
| Number of results obtained in Scopus |
| 5 |
|
| Study | Sample Size | Mean Age ± SD | EG Intervention | N° of Sessions | Sessions/Week | Duration (Weeks) | CG Intervention | Video Console | Video Games in EG | PEDro |
|---|---|---|---|---|---|---|---|---|---|---|
| Barcala et al. [25] | N = 20 EG = 10 CG = 10 | 64.35 ± 1.20 | 60′ conventional physiotherapy + 30′ Wii® | 10 | 2 | 5 | 60’ conventional physiotherapy | Nintendo Wii® | Wii Fit® | 8/10 |
| Bower et al. [26] | N = 30 EG = 17 CG = 13 | 63.9 ± 0.82 | Conventional rehabilitation + 45’ Wii® in bipedestations | 9 | 3 | 3 | Conventional rehabilitation + 45’ Wii® in sitting position | Nintendo Wii® | Wii Fit Plus® | 6/10 |
| Cho et al. [27] | N = 22 EG = 11 CG = 11 | 64.19 ± 1.50 | 60’/90’standard rehabilitation + 30’Wii® | 18 | 3 | 6 | 60’/90’ standard rehabilitation | Nintendo Wii® | Wii Fit® | 6/10 |
| Hung et al. [28] | N = 24 EG = 12 CG = 12 | Standard rehabilitation + 30’ Wii® | 24 | 2 | 12 | Standard rehabilitation + 30’ load transfer | Nintendo Wii® | Wii Fit Plus® | 8/10 | |
| Hung et al. [29] | N = 28 EG = 13 CG = 15 | 54.39 ± 1.40 | Standard outpatient rehabilitation + 30’ Wii® | 24 | 2 | 12 | Standard outpatient rehabilitation + 30’ load transfer | Nintendo Wii® | Wii Fit Plus® | 8/10 |
| Kannan et al. [30] | N = 20 EG = 10 CG = 10 | 59.25 ± 2.47 | 90’Wii® + cognitive tasks simultaneously | 20 | 6 | 90’ standard rehabilitation | Nintendo Wii® | Wii Fit® | 6/10 | |
| Karasu et al. [31] | N = 23 EG = 12 CG = 11 | 63.2 ± 1.27 | 120’/180’standard rehabilitation + 20’ Wii® | 20 | 5 | 4 | 120’/180’standard rehabilitation | Nintendo Wii® | Wii Fit® | 7/10 |
| Kim et al. [32] | N = 17 EG = 10 CG = 7 | 48.15 ± 9.68 | 30’general exercises + 15’ electric stimulation + 30’ Wii® | 9 | 3 | 3 | 30’ general exercises + 15’ electric stimulation | Nintendo Wii® | Wii Sports® | 6/10 |
| Lee et al. [33] | N = 24 EG = 12 CG = 12 | 47.53 ± 2.29 | 60’ therapeutic exercise with physiotherapy + 30’ Wii® | 18 | 3 | 6 | 60’ therapeutic exercise + 30’ functional task treatment | Nintendo Wii® | Wii Fit Plus® | 6/10 |
| Lee et al. [34] | N = 47 EG = 26 CG = 21 | 57.55 ± 2.53 | 45’ conventional rehabilitation + 45’ Xbox® | 12 | 2 | 6 | 60’ conventional rehabilitation + 30’ balance training | Kinect-Xbox® | Kinect Sport® + Kinect Sport Season2® + Kinect Adventures® + Kinect Your Shape: Fitness Evolved® | 7/10 |
| Lee et al. [35] | N = 10 EG = 5 CG = 5 | 65.7 ± 0.5 | 135’ conventional rehabilitation + 30’ Wii® | 12 | 3 | 4 | 135’ conventional rehabilitation | Nintendo Wii® | Wii Sports Resort® | 7/10 |
| Morone et al. [36] | N = 50 EG = 25 CG = 25 | 60.16 ± 10.04 | Conventional physiotherapy + 20’ Wii® | 12 | 3 | 4 | Conventional physiotherapy + 20’ balance exercises | Nintendo Wii® | Wii Fit® | 8/10 |
| Park et al. [37] | N = 20 EG = 10 CG = 10 | 63.65 ± 2.33 | 30’ conventional physiotherapy + 30’ Xbox® | 42 | 7 | 6 | 30’ conventional physiotherapy | Kinect-Xbox® | Kinect Sport® + Kinect Sport Season2® | 8/10 |
| Pedreira da Fonseca et al. [38] | N = 27 EG = 14 CG = 13 | 52.4 ± 8.9 | 15’ conventional physiotherapy + 45’ Wii® | 20 | 2 | 10 | 60’ conventional physiotherapy | Nintendo Wii® | Wii Sports® | 7/10 |
| Rajaratnam et al. [39] | N = 19 EG = 10 CG = 9 | 61.6 ± 7.8 | 40’ conventional rehabilitation + 20’ VR (Wii®/Xbox®) | 15 | 60’ conventional rehabilitation | Nintendo Wii®/Kinect-Xbox® | Wii Fit®/Kinect Adventures® | 7/10 | ||
| Singh et al. [40] | N = 28 EG = 15 CG = 13 | 66.2 ± 1.13 | 90’ standard group physiotherapy + 30’ VR (15’ Wii® + 15’ Xbox®) | 12 | 2 | 6 | 120’ standard group physiotherapy | Nintendo Wii® + Kinect-Xbox® | Wii Fit Plus® + Kinect Adventures | 5/10 |
| Song & Park [41] | N = 40 EG = 20 CG = 20 | 50.73 ± 0.89 | 30’ Xbox® | 40 | 5 | 8 | 30’ ergometric bike MOTOmed | Kinect-Xbox® | Kinect Sport® + Kinect Sport Season2® + Kinect Adventures® + Kinect Grunstringer® | 6/10 |
| Yatar & Yildrim [42] | N = 30 EG = 15 CG = 15 | 59.7 ± 4.38 | 30’ Neurodevelopment + 30’ Wii® | 12 | 3 | 4 | 30’ Neurodevelopment + 30’ balance training | Nintendo Wii® | Wii Fit Plus® | 4/10 |
| Study | Outcomes | Mean Values EG (Mean ± SD) | Mean Values CG (Mean ± SD) | Main Results | Effect Size (Cohen’s d) | Time × Group Interaction (F/P) |
|---|---|---|---|---|---|---|
| Barcala et al. [25] | Posturography (peak plantar pressure and oscillation in different sensorial conditions) BBS TUG | Peak plantar pressure on affected leg, g/cm2: pre: 1138.2 ± 333.3; post: 1309.5 ± 260.1; p < 0.05 Peak plantar pressure on non-affected leg, g/cm2: pre: 1465.7 ± 285.2; post: 1350.4 ± 243.6; p < 0.05 ML oscillation EO, cm: pre: 4.55 ± 0.55; post:2.87 ± 0.93; p < 0.05 ML oscillation EC, cm: pre: 5.40 ± 0.51; post: 3.97 ± 0.94; p < 0.05 AP oscillation EO, cm: pre: 1.18 ± 0.06; post: 1.13 ± 0.08; p < 0.05 AP oscillation EC, cm: pre: 1.48 ± 0.27; post: 1.35 ± 0.27; p < 0.05 BBS, score: Pre: 39.6 ± 6.43; post: 41.9 ± 6.91; p < 0.05 TUG, s: Pre: 27.9 ± 8.22; post: 24.3± 8.64; p < 0.05 | Peak plantar pressure on affected leg, g/cm2: pre: 1232.1 ± 182.1 post: 1319.7 ± 194.6 p < 0.05 Peak plantar pressure on non-affected leg, g/cm2: pre: 1490.9 ± 196.1; post: 1357.0 ± 185.4; p < 0.05 ML oscillation EO, cm: pre: 4.3 ± 1.69; post: 3.13 ± 1.81; p < 0.05 ML oscillation EC, cm: pre: 5.17 ± 2.07; post: 3.64 ± 1.97; p < 0.05 AP oscillation EO, cm: pre: 1.18 ± 0.13; post: 1.12 ± 0.08; p < 0.05 AP oscillation EC, cm: pre: 1.26 ± 0.15; post: 1.18 ± 0.07; p < 0.05 BBS, score: Pre: 37.2 ± 5.22 post: 42.2 ± 4.80 p < 0.05 TUG, s: Pre: 28.1 ± 3.10; post: 25.2 ± 2.78; p < 0.05 | Statistically significant improvements in both groups after intervention in all the variables (the variables recorded by posturography, BBS and TUG) (p < 0.05), although without significant statistical differences between groups. | NR | NR |
| Bower et al. [26] | Wii Balance Board® (displacement velocity in different sensorial conditions and weight shifting) Steptest FRT TUG FES-I | EO COP velocity, cm/s: pre: 1.90 ± 0.76; post: 1.59 ± 0.49; p > 0.05 EO ML COP velocity, cm/s: pre: 0.94 ± 0.45; post: 0.71 ± 0.27; p > 0.05 EO AP velocity, cm/s: Pre: 1.45 ± 0.60; post: 1.28 ± 0.41; p > 0.05 EC COP velocity, cm/s: pre: 2.89 ± 1.30; post: 2.29 ± 0.70; p > 0.05 EC ML COP velocity, cm/s: pre: 1.38 ± 0.99; post: 0.94 ± 0.38; p > 0.05 EC AP velocity, cm/s: pre: 2.21 ± 0.84; post: 1.91 ± 0.60; p > 0.05 ML weight shifting, n: pre: 7.2 ± 3.5; post: 10.9 ± 4.0; p > 0.05 Steptest (affected), score: pre: 2.7 ± 3.8; post: 8.9 ± 5.4; p > 0.05 Steptest (unaffected), score: pre: 4.2 ± 3.1; post:9.0 ± 4.2; p > 0.05 FRT, cm: pre: 28.1 ± 6.4; post: 31.1 ± 6.5; p > 0.05 TUG, s: Pre: 30.3 ± 15.9; post: 19.2 ± 15.5; p > 0.05 FES-I, score: pre: 16.6 ± 4.8; post: 11.3 ± 3.2; p > 0.05 | EO COP velocity, cm/s: pre: 1.54 ± 0.38; post: 1.54 ± 0.42; p > 0.05 EO ML COP velocity: pre: 0.60 ± 0.13; post: 0.59 ± 0.16; p > 0.05 EO AP velocity, cm/s: Pre: 1.29 ± 0.33; post: 1.31 ± 0.38; p > 0.05 EC COP velocity, cm/s: pre: 2.62 ± 0.82; post: 2.36 ± 0.67; p > 0.05 EC ML COP velocity, cm/s: pre: 0.89 ± 0.34; post: 0.76 ± 0.22; p > 0.05 EC AP velocity, cm/s: pre: 2.27 ± 0.70; post: 2.12 ± 0.61; p > 0.05 ML weight shifting, n: pre: 8.1 ± 3.4; post: 10.1 ± 2.3; p > 0.05 Steptest (affected), score: pre: 7.4 ± 6.0; post: 8.9 ± 5.4; p > 0.05 Steptest (unaffected, score): pre:6.1 ± 5.8; post:9.7 ± 4.7; p > 0.05 FRT, cm: pre: 28.3 ± 9.6; post: 31.1 ± 9.0; p > 0.05 TUG, s: Pre: 32.0 ± 32.2; Post: 16.0 ± 11.9; p > 0.05 FES-I, score: pre: 19.3 ± 7.0; post: 13.0 ± 3.4; p > 0.05 | Clinical improvements in both groups after intervention in all the variables (the variables recorded by Wii Balance Board®, Steptest, FRT, TUG, FES-I), but not statistically significant improvements (p > 0.05). Not statistic and clinically significant differences between groups in any variable after intervention. | EO COP velocity: −0.93 EO ML COP velocity: −1 EO AP velocity: −0.69 EC COP velocity: −0.46 EC ML COP velocity: −0.58 EC AP velocity: −0.30 ML weight shifting: 0.71 Steptest (affected): 1.54 Steptest (unaffected): 0.41 FRT: 0.03 TUG: 0.29 FES-I: 0.19 | Steptest NR/0.002 FRT: NR/0.066 NR in the other variables |
| Cho et al. [27] | Posturography (Postural Sway Velocity in different sensorial conditions) BBS TUG | PSV AP EO, mm/s: Pre: 7.37 ± 2.20; Post: 6.20 ± 1.70; p > 0.05 PSV AP EC, mm/s: Pre: 9.97 ± 2.69; Post:9.18 ± 1.75; p > 0.05 PSV ML EO, mm/s: Pre: 11.40 ± 2.24; Post: 11.22 ± 2.06; p > 0.05 PSV ML EC, mm/s: Pre: 16.78 ± 2.25; Post: 15.50 ± 3.59; p > 0.05 BBS, score: Pre: 39.09 ± 5.66; Post: 43.09 ± 4.80; p < 0.001 TUG, s: Pre: 21.74 ± 3.41; Post: 20.40 ± 3.19; p < 0.001 | PSV AP EO, mm/s: Pre: 6.01 ± 1.85; post: 5.64 ± 1.57; p > 0.05 PSV AP EC, mm/s: Pre: 9.67 ± 2.72; Post:9.14 ± 2.31; p > 0.05 PSV ML EO, mm/s: Pre: 9.92 ± 1.28; Post:9.82 ± 1.20; p > 0.05 PSV ML EC, mm/s: Pre: 14.41 ± 4.08; Post: 14.12 ± 4.01; p > 0.05 BBS, score: Pre: 41.09 ± 4.01; Post: 43.90 ± 4.06; p < 0.001 TUG, s: Pre: 19.60 ± 4.42; Post: 19.08 ± 4.52; p < 0.01 | Statistically significant improvements in both groups after intervention in BBS and TUG (p < 0.01); statistic improvements were significantly higher in the EG (p < 0.05). The variables recorded by posturography presented no significant statistical differences in any group after intervention (p > 0.05). | NR | NR |
| Hung et al. [28] | BBS | BBS, score: Pre: 46.58 ± 5.16; Post: 48.83 ± 5.02; p > 0.05 | BBS, score: Pre: 48.25 ± 3.91; Post: 50.42 ± 3.99; p > 0.05 | Clinical improvements in both groups after intervention in BBS, but not statistically significant (p > 0.05) Not significant statistical differences between groups in BBS after intervention. | NR | NR |
| Hung et al. [29] | Posturography (Percentage of weight bearing on affected leg in different sensorial conditions, Stability index in different sensorial conditions) FRT TUG FES-I | Weight bearing on affected leg with head straight EO while standing on a solid surface, %: Pre: 42.31 ± 7.94; Post: 43.34 ± 6.03; p < 0.05 Follow-up: 42.08 ± 4.00; p > 0.05 Weight bearing on affected leg with head straight EC while standing on a solid surface, %: Pre: 43.58 ± 10.46; Post: 44.03 ± 6.76; P < 0.05 Follow-up: 42.23 ± 4.99; p > 0.05 Stability index in head straight EO while standing on a solid surface: Pre: 27.37 ± 12.52; Post: 28.40 ± 15.11; P < 0.05 Follow-up: 28.84 ± 10.25; p > 0.05 Stability index in head straight EC while standing on a solid surface: Pre: 43.34 ± 27.73; Post: 38.30 ± 17.82; P < 0.05 Follow-up: 38.52 ± 23.46; p > 0.05 FRT, cm: Pre: 21.62 ± 5.19; Post: 25.35 ± 3.92; p < 0.05 Follow-up: 24.63 ± 4.82; p < 0.05 TUG, s: Pre: 26.06 ± 12.05; Post: 20.88 ± 7.77; p < 0.05 Follow-up: 23.01± 7.89; p < 0.05 FES-I: Pre: 29.15 ± 6.85; Post: 25.38 ± 6.06; P < 0.05 Follow-up: 29.31 ± 9.81; p > 0.05 | Weight bearing on affected leg with head straight EO while standing on a solid surface, %: Pre: 40.81 ± 10.12; Post: 46.07 ± 6.39; p < 0.05 Follow-up: 46.72 ± 8.80; p > 0.05 Weight bearing on affected leg with head straight EC while standing on a solid surface, %: Pre: 41.10 ± 9.86; Post: 46.17 ± 6.95; P < 0.05 Follow-up: 45.86 ± 7.98; p > 0.05 Stability index in head straight EO while standing on a solid surface: Pre: 24.22 ± 9.81; Post: 25.69 ± 8.92; P < 0.05 Follow-up: 27.17 ± 12.37; p > 0.05 Stability index in head straight EC while standing on a solid surface: Pre: 35.17 ± 13.45; Post: 38.29 ± 18.94; P < 0.05 Follow-up: 36.86 ± 16.52; p > 0.05 FRT, cm: Pre: 21.73 ± 5.33; Post: 25.37 ± 4.99; p < 0.05 Follow-up: 25.82 ± 7.29; p < 0.05 TUG, s: Pre: 29.45± 16.22; Post: 26.61 ± 12.92; p < 0.05 Follow-up: 25.60 ± 13.79; p < 0.05 FES-I: Pre: 30.07 ± 4.76; Post: 26.20 ± 6.80; P < 0.05 Follow-up: 30.80 ± 11.42; p > 0.05 | Statistically significant improvements in both groups after intervention in the variables recorded by posturography, FRT, FES-I and TUG (p < 0.05). These results were maintained at 3-month follow-up in FRT and TUG but not in the variables recorded by posturography and FES-I. Not significant statistical differences between groups in any variable after intervention. | NR | Intervention effect Percentage of weight bearing on affected leg with head straight EO while standing on a solid surface: 3.61/0.07 Percentage of weight bearing on affected leg with head straight EC while standing on a solid surface: 2.61/0.12 Stability index in head straight EO while standing on a solid surface: 0.02/0.89 Stability index in head straight EC while standing on a solid surface: 1.71/0.20 FRT: 0.00/0.96 TUG: 0.57/0.46 FES-I: 0.00/0.97 Maintenance effect Percentage of weight bearing on affected leg with head straight EO while standing on a solid surface: 5.06/0.03 Percentage of weight bearing on affected leg with head straight EC while standing on a solid surface: 2.61/0.12 Stability index in head straight EO while standing on a solid surface: 0.18/0.67 Stability index in head straight EC while standing on a solid surface: 1.71/0.20 FRT: 0.16/0.69 TUG: 0.07/0.79 FES-I: 0.02/0.89 |
| Kannan et al. [30] | Posturography (MVL) BBS TUG 6 MWT | Data in graph, Not extractable | Data in graph, Not extractable | Statistically significant improvements after intervention in EG in MVL (p = 0.001). Statistically significant improvements in both groups after intervention in BBS, TUG and 6 MWT (p < 0.05). Not statistically significant differences between groups in any variable after intervention. | NR | MVL: 14.295/0.001 NR in the other variables |
| Karasu et al. [31] | Posturography (displacement of the centre of pressure in different sensorial conditions) BBS FRT SBI PASS TUG | displacement ML EO, cm: pre: 3.0 ± 1.3; post: 1.8 ± 0.5; p < 0.05 follow-up: 1.7 ± 0.5; p: NR displacement ML EC, cm: pre: 3.5 ± 1.4; post: 2.4 ± 0.7; p < 0.05 follow-up: 2.2 ± 0.7; p: NR displacement AP EO, cm pre: 3.0 ± 0.9; post: 2.4 ± 0.8; p < 0.05 follow-up: 2.05 ± 0.7; p: NR displacement AP EC, cm pre: 3.4 ± 0.9; post: 2.8± 0.8; p < 0.05 follow-up: 2.4 ± 0.6; p: NR BBS, score: pre: 38.8 ± 6.9; post: 48.9± 6.4; p < 0.05 follow-up: 48.7 ± 4.7; p: NR FRT, cm: pre: 16.4 ± 5.5; post: 25.2 ± 5.5; p < 0.05 follow-up: 23.6 ± 5.4; p: NR SBI, score: pre: 426.2 ± 285.3; post: 369.3 ± 301.5; p < 0.05 follow-up: 337 ± 282.8; p: NR PASS, score: pre: 28.8 ± 4.3; post: 32.5 ± 2.5; p < 0.05 follow-up: 32 ± 2.4; p: NR TUG, s: pre: 32.5 ± 21.2; post: 19.5 ± 9.8; p > 0.05 follow-up: 20.5 ± 8.3; p: NR | displacement ML EO, cm: pre: 2.7 ± 0.9; post: 2.4 ± 0.9; p < 0.05 follow-up: 2.5 ± 0.6; p: NR displacement ML EC, cm: pre: 3.1 ± 1.1; post: 2.9 ± 1.3; p < 0.05 follow-up: 3.1 ± 0.6; p: NR displacement AP EO, cm pre: 2.5 ± 0.8; post: 2.6 ± 1.4; p < 0.05 follow-up: 2.5 ± 0.5; p: NR displacement AP EC, cm pre: 3.1 ± 0.7; post: 3.2 ± 1.4; p < 0.05 follow-up: 3.3 ± 0.6; p: NR BBS, score: pre: 39.1 ± 6.9; post: 42.2 ± 6.4; p < 0.05 follow-up: 39.4 ± 5.7; p: NR FRT, cm: pre: 18.8 ± 3.3; post: 22.2 ± 5.1; p < 0.05 follow-up: 20 ± 3.14) p: NR SBI, score: pre: 412.4 ± 196.8; post: 314.2 ± 129.8; p < 0.05 follow-up: 399.7 ± 74.7; p: NR PASS, score: pre: 27.9 ± 5.2; post: 30.4 ± 4.1; p < 0.05 follow-up: 29.2 ± 3.5; p: NR TUG, s: pre: 27.4 ± 15.0; post: 24 ± 13.5; p > 0.05 follow-up: 29.6 ± 10.5; p: NR | Statistically significant improvements in both groups after intervention in variables recorded by posturography, BBS, FRT, SBI and PASS (p < 0.05). The improvements in BBS and FRT were statistical significantly higher in the EG (p < 0.001). TUG presented no significant statistical differences in any group after intervention (p > 0.05). | NR | Intervention effect Displacement ML EO: NR/0.034 displacement ML EC: NR/0.071 displacement AP EO: NR/0.012 displacement AP EC: NR/0.018 BBS: NR/<0.001 FRT: NR/<0.001 SBI: NR/0.068 PASS: NR/0.375 TUG: NR/0.078 Maintenance effect NR |
| Kim et al. [32] | PASS MMAS | PASS, score: Pre: 25.8 ± 3.85; Post:30.3 ± 3.19; p < 0.05 MMAS, score: Pre: 29.8 ± 6.4; Post: 34.7 ± 6.2; p < 0.05 | PASS, score: Pre: 26.42 ± 1.98; Post: 28.0 ± 1.63; p < 0.05 MMAS, score: Pre: 31.71 ± 1.88; Post: 33.57 ± 1.51; p < 0.05 | Statistically significant improvements in both groups after intervention in PASS and MMAS (p < 0.05). These improvements were statistical significantly higher in the EG (p < 0.05). | NR | NR |
| Lee et al. [33] | Wii Balance Board® (COP path length and velocity in different sensorial conditions) FRT | COP path length EO, cm: Pre: 63.86 ± 33.53; Post: 51.25 ± 27.29; p < 0.05 COP path length EC, cm: Pre: 75.71 ± 37.61; Post: 75.71 ± 37.61; p < 0.001 COP velocity EO, cm/s: Pre: 2.12 ± 1.11; Post: 1.70 ± 0.90; p < 0.05 COP velocity EC, cm/s: Pre: 2.52 ± 1.25; Post: 1.99 ± 0.79; p < 0.05 FRT, cm: Pre: 15.84 ± 6.32; Post: 24.75 ± 7.44; p < 0.0001 | COP path length EO, cm: Pre: 60.65 ± 30.14; Post: 49.52 ± 18.50; p < 0.05 COP path length EC, cm: Pre: 65.85 ± 34.95; Post: 59.00 ± 24.88; p > 0.05 COP velocity EO, cm/s: Pre: 2.02 ± 1.00; Post: 1.65 ± 0.61; p < 0.05 COP velocity EC, cm/s: Pre: 2.19 ± 1.16; Post: 1.96 ± 0.82; p > 0.05 FRT, cm: Pre: 16.40 ± 5.91; Post: 21.39 ± 6.31; p < 0.0001 | Statistically significant improvements in both groups after intervention in variables recorded by Wii Balance Board® and FRT (p < 0.05). The improvements in FRT were statistical significantly higher in the EG (p < 0.0001), but not in variables recorded by Wii Balance Board® (p > 0.05). | NR | NR |
| Lee et al. [34] | BBS FRT TUG-cog | BBS, score: Pre: 43.35 ± 6.23; Post: 46.19 ± 5.57; P < 0.05 Follow-up: 46.31 ± 5.80; p < 0.05 FRT, cm: Pre: 21.43 ± 7.62; Post: 22.63 ± 5.07; P > 0.05 Follow-up: 22.48 ± 5.87; p > 0.05 TUG-cog, s: Pre: 27.18 ± 14.90; Post: 24.15 ± 10.87; p < 0.05 Follow-up: 23.52 ± 10.96; p < 0.05 | BBS, score: Pre: 43.48 ± 6.62; Post: 45.71 ± 6.64; p < 0.05 Follow-up: 45.00 ± 5.06; p < 0.05 FRT, cm: Pre: 22.05 ± 8.27; Post: 21.84 ± 7.46; p > 0.05 Follow-up: 18.74 ± 5.88; p > 0.05 TUG-cog, s: Pre: 32.13 ± 24.63; Post: 28.48 ± 21.53; p < 0.05 Follow-up: 28.67 ± 18.73; p < 0.05 | Statistically significant improvements in both groups after intervention and follow-up in BBS and TUG-cog (p < 0.05), although without significant differences between both groups. FRT presented no significant statistical differences in any group after intervention and follow up (p > 0.05). | NR | Intervention effect BBS: 0.705/0.497 FRT: 3.066/0.051 TUG-cog: NR Maintenance effect NR |
| Lee et al. [35] | BBS FRT TUG | BBS, score: Pre: 41.8 ± 4.2; Post: 46.2 ± 4.3; p: <0.05 FRT, cm: Pre: 20.4 ± 3.5; Post: 22.4 ± 3.9; p: <0.05 TUG, s: Pre: 16.6 ± 4.3; Post: 15.1 ± 4.0; p: <0.05 | BBS, score: Pre: 38.8 ± 3.7; Post: 41.2 ± 2.9; p: <0.05 FRT, cm: Pre: 17.8 ± 0.9; Post: 18.7 ± 0.9; p: <0.05 TUG, s: Pre: 18.1 ± 2.7; Post: 18.2 ± 1.5; p: >0.05 | Statistically significant improvements in both groups after intervention in BBS and FRT (p < 0.05). These improvements were significantly higher in the EG (p < 0.05). Statistically significant improvements after intervention in EG in TUG (p < 0.05). These improvements were statistically significant between both groups after intervention (p < 0.05) | NR | NR |
| Morone et al. [36] | BBS FAC 10 MWT | Data in graph, Not extractable | Data in graph, Not extractable | Statistically significant improvements in both groups after intervention in all variables (BBS, FAC and 10 MWT) (p < 0.001), the improvements in BBS and 10 MWT were statistically significantly higher in the EG (p < 0.05), but not in FAC (p > 0.05). These Statistically significant improvements were maintained in follow-up | NR | Intervention effect 10 MWT: NR/0.099 NR in the other variables Maintenance effect NR |
| Park et al. [37] | BBS TUG 10 MWT | BBS, score: Pre: 35.80 ± 8.61; Post: 50.00 ± 6.27; p: <0.05 TUG, s: Pre: 44.35 ± 33.49; Post: 44.93 ± 27.41; p: <0.05 10 MWT, m/s: Pre: 57.14 ± 22.61; Post: 44.73 ± 20.87; p: <0.05 | BBS, score: Pre: 37.30 ± 11.98; Post: 44.70 ± 7.47; p: <0.05 TUG, s: Pre: 44.93 ± 27.41; Post: 41.16 ± 27.68; p: <0.05 10 MWT, m/s: Pre: 53.90 ± 26.06; Post: 47.77 ± 22.98; p: <0.05 | Statistically significant improvements in both groups after intervention in all variables (BBS, TUG and 10 MWT) (p < 0.05) and statistically significantly higher in the EG (p < 0.05) | NR | NR |
| Pedreira da Fonseca et al. [38] | DGI | Data in graph, Not extractable | Data in graph, Not extractable | Statistically significant improvements in CG after intervention in DGI (p < 0.05). Clinical improvements in EG after intervention in DGI, but not statistically significant (p > 0.05) | NR | NR |
| Rajaratnam et al. [39] | Wii Balance Board® (COP) BBS FRT TUG | Data not extractable | Data not extractable | Statistically significant improvements after intervention in EG in FRT and TUG (p < 0.05) and in CG in TUG (p < 0.05). Variable recorded by Wii Balance Board® presented no significant statistical differences in any group after intervention (p > 0.05). No significant statistical differences between both groups in any variables after intervention (p > 0.05) | NR | NR |
| Singh et al. [40] | Posturography (OBS) TUG 10 MWT 6 MWT | OBS, score: Pre: 2.53 ± 1.02; Post: 2.70 ± 0.72; p: >0.05 TUG, s: Pre: 25.33 ± 14.38; Post: 23.07 ± 12.22; p: >0.05 10 MWT, m/s: Pre: 13.20 ± 7.46; Post: 12.17 ± 6.16; p: >0.05 6 MWT, m: Pre: 162.40 ± 78.97; Post: 165.27 ± 78.52; p: >0.05 | OBS, score: Pre: 3.25 ± 1.12; Post: 3.31 ± 1.39; p: >0.05 TUG, s: Pre: 23.27 ± 12.15; Post: 21.69 ± 12.29; p: >0.05 10 MWT, m/s: Pre: 14.80 ± 10.16; Post: 15.03 ± 9.35; p: >0.05 6 MWT, m: Pre: 209.92 ± 176.53; Post: 167.23 ± 103.85; p: >0.05 | No significant statistical differences were found in any group after intervention in any variable (p > 0.05) | NR | TUG: NR/0.02 10 MWT: NR/0.66 6 MWT: NR/0.59 OBS: NR |
| Song & Park [41] | Posturography (WB on the affected side, anterior and posterior LOS) TUG 10 MWT | Affected side WB, %: Pre: 42.8 ± 6.1; Post: 46.1 ± 4.3; p: <0.05 Forward LOS, mm: Pre: 2732.9 ± 3137.1; Post: 3311.7 ± 3786.5; p: <0.05 Backward LOS, mm: Pre: 2072.7 ± 2050.4; Post: 1895.9 ± 2097.5; p: <0.05 TUG, s: Pre: 21.17 ± 7.7; Post: 21.9 ± 7.9; p: <0.05 10 MWT, m/s: Pre: 18.3 ± 2.2; Post: 21.4 ± 8.9; p: <0.05 | Affected side WB, %: Pre: 42.1 ± 4.3; Post: 43.3 ± 4.9; p: <0.05 Forward LOS, mm: Pre: 5670.8 ± 4291.1; Post: 4322.6 ± 3565.5; p: <0.05 Backward LOS, mm: Pre: 3971.7 ± 2794.3; Post: 2889.7 ± 2769.7; p: <0.05 TUG, s: Pre:16.6 ± 4.7; Post: 19.5 ± 7.5; p: <0.05 10 MWT, m/s: Pre: 14.3 ± 2.1; Post: 19.1 ± 8.8; p: <0.05 | Statistically significant improvements in both groups after intervention in all variables (Variables recorded by posturography, TUG and 10 MWT) (p < 0.05) and statically significant higher in the EG (p < 0.05) | NR | NR |
| Yatar & Yildrim [42] | Wii Balance Board® (weight distribution) FRT BBS TUG DGI | Weight distribution, paretic side, %: Pre: 44.04 ± 7.47; Post: 48.00 ± 2.80; p: ≤0.05 Follow-up: 46.64 ± 4.40; p: >0.05 FRT, cm: Pre: 25.26 ± 5.92; Post: 29.40 ± 5.16; p: ≤0.05 Follow-up: 30.06 ± 5.16; p: >0.05 BBS, score: Pre: 45.60 ± 5.26; Post: 50.33 ± 4.09; P: ≤0.05 Follow-up: 50.33 ± 4.16; p: >0.05 TUG, s: Pre: 17. 96 ± 7.77; Post: 16.17 ± 8.23; P: ≤0.05 Follow-up: 15.95 ± 7.93; p: >0.05 DGI, score: Pre: 14.86 ± 4.12; Post: 16.86 ± 3.35; P: ≤0.05 Follow-up: 16.86 ± 3.33; p: >0.05 | Weight distribution, paretic, %: Pre: 47.54 ± 10.16; Post: 48.59 ± 8.38; p: >0.05 Follow-up: 48.14 ± 8.94; p: >0.05 FRT, cm: Pre: 24.20 ± 6.66; Post: 27.13 ± 6.19; p: ≤0.05 Follow-up: 26.80 ± 6.58; p: >0.05 BBS, score: Pre: 39.60 ± 9.31; Post: 44.80 ± 7.48; P: ≤0.05 Follow-up: 44.20 ± 7.77; p: ≤0.05 TUG, s: Pre: 26.36 ± 11.60; Post: 22.11 ± 11.88; P: ≤0.05 Follow-up: 22.73 ± 11.95; p: >0.05 DGI, score: Pre: 12.60 ± 3.96; Post: 14.46 ± 3.48; P: ≤0.05 Follow-up: 14.86 ± 4.06; p: >0.05 | Statistically significant improvements in both groups after intervention in FRT, BBS, TUG and DGI (p ≤ 0.05). Significant statistical differences between both groups in FRT, BBS, TUG and DGI (p ≤ 0.05), with better results in EG. Statistically significant improvements in EG after intervention in weight distribution recorded by Wii Balance Board® (p ≤ 0.05), but not in CG (P > 0.05) These improvements were maintained in CG in BBS and TUG in follow-up (p ≤ 0.05) | NR | NR |
| BIAS | ||||||
|---|---|---|---|---|---|---|
| REFERENCES | Selection | Performance | Detection | Wear | Notification | Others |
| Barcala et al. [25] | + | - | + | + | + | + |
| Bower et al. [26] | - | - | + | - | + | + |
| Cho et al. [27] | + | - | - | + | + | + |
| Hung et al. [28] | + | - | + | + | + | + |
| Hung et al. [29] | + | - | + | + | + | + |
| Kannan et al. [30] | + | - | - | + | + | + |
| Karasu et al. [31] | + | - | + | + | + | + |
| Kim et al. [32] | + | - | - | + | + | + |
| Lee et al. [33] | - | - | - | + | + | + |
| Lee et al. [34] | + | - | + | + | + | + |
| Lee et al. [35] | + | - | + | + | + | + |
| Morone et al. [36] | + | - | + | - | + | + |
| Park et al. [37] | + | - | + | + | + | + |
| Pedreira da Fonseca et al. [38] | + | - | + | + | + | + |
| Rajaratnam et al. [39] | + | + | + | + | - | + |
| Singh et al. [40] | - | - | + | + | + | + |
| Song & Park [41] | + | - | - | + | + | + |
| Yatar & Yildrim [42] | - | - | - | + | + | + |
| Advantages | Disadvantages |
|---|---|
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pintado-Izquierdo, S.; Cano-de-la-Cuerda, R.; Ortiz-Gutiérrez, R.M. Video Game-Based Therapy on Balance and Gait of Patients with Stroke: A Systematic Review. Appl. Sci. 2020, 10, 6426. https://doi.org/10.3390/app10186426
Pintado-Izquierdo S, Cano-de-la-Cuerda R, Ortiz-Gutiérrez RM. Video Game-Based Therapy on Balance and Gait of Patients with Stroke: A Systematic Review. Applied Sciences. 2020; 10(18):6426. https://doi.org/10.3390/app10186426
Chicago/Turabian StylePintado-Izquierdo, Silvia, Roberto Cano-de-la-Cuerda, and Rosa María Ortiz-Gutiérrez. 2020. "Video Game-Based Therapy on Balance and Gait of Patients with Stroke: A Systematic Review" Applied Sciences 10, no. 18: 6426. https://doi.org/10.3390/app10186426
APA StylePintado-Izquierdo, S., Cano-de-la-Cuerda, R., & Ortiz-Gutiérrez, R. M. (2020). Video Game-Based Therapy on Balance and Gait of Patients with Stroke: A Systematic Review. Applied Sciences, 10(18), 6426. https://doi.org/10.3390/app10186426






