Biomechanical Comparison of Different Volar Screw Placements for Horizontal Oblique Scaphoid Fractures
Abstract
:1. Introduction
2. Materials and Methods
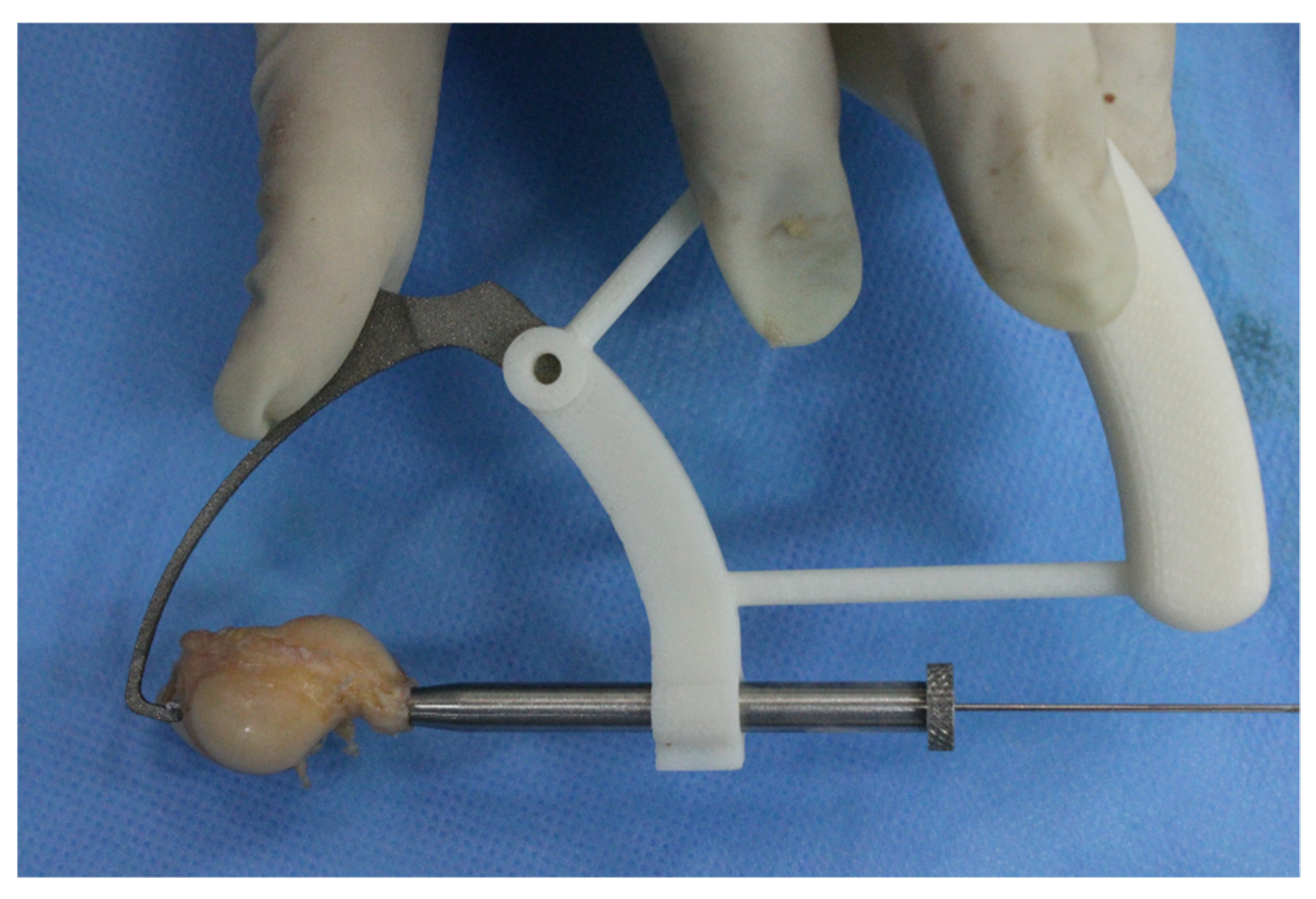
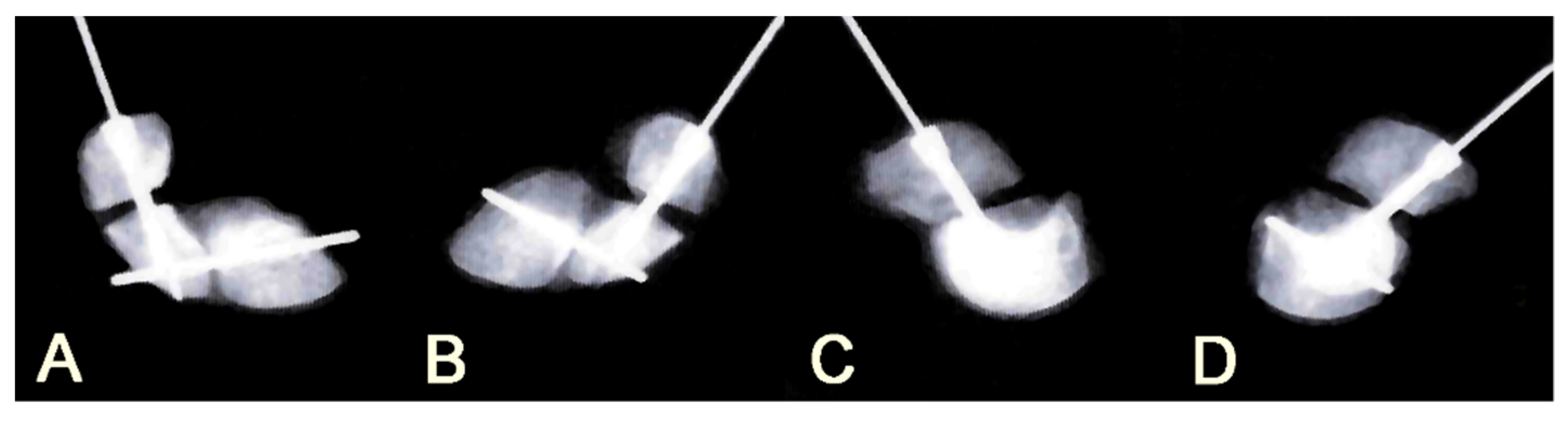
2.1. Surgical Procedures
2.2. Biomechanical Testing of Fixation Stability
2.3. Statistical Analysis
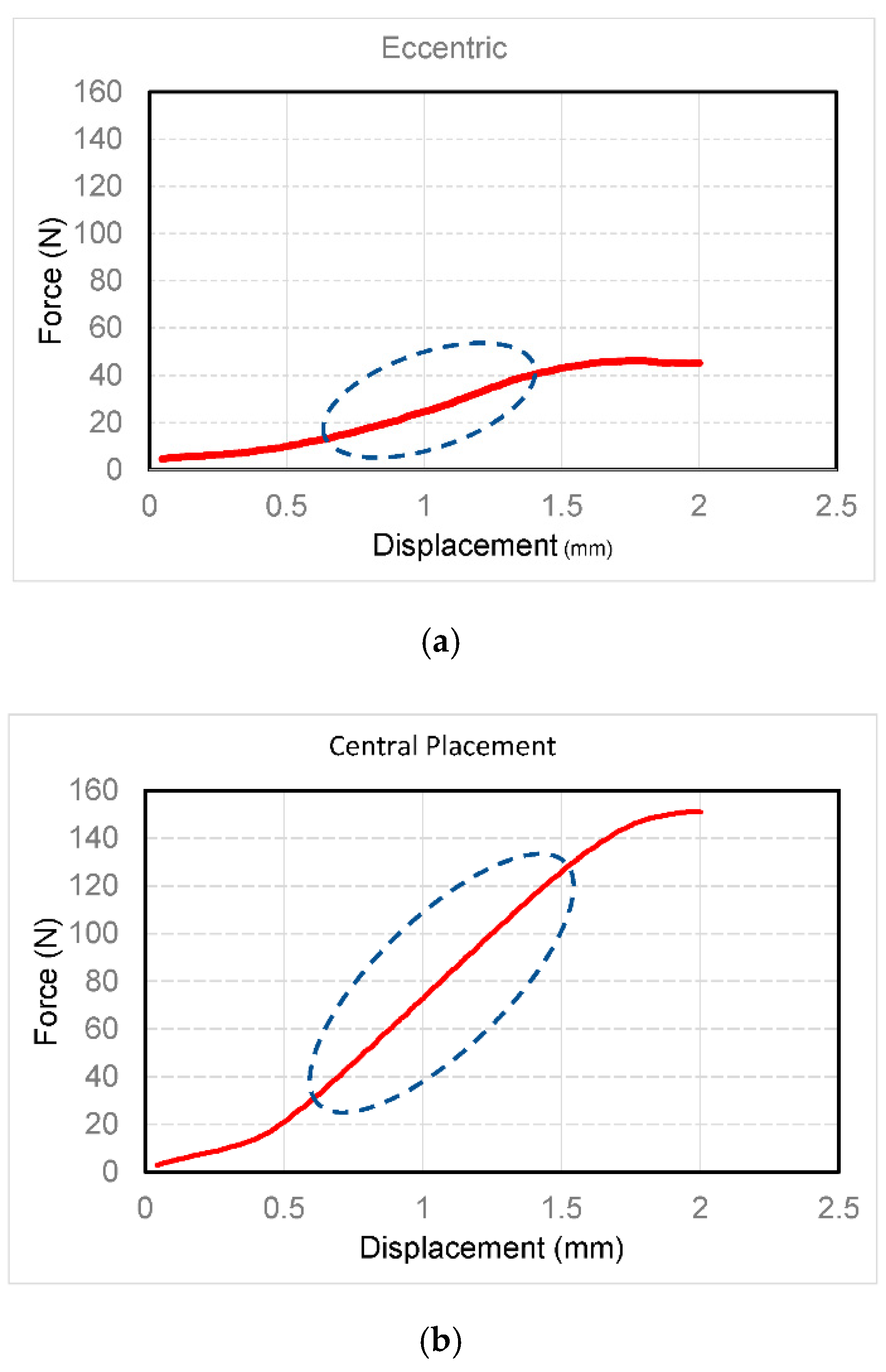
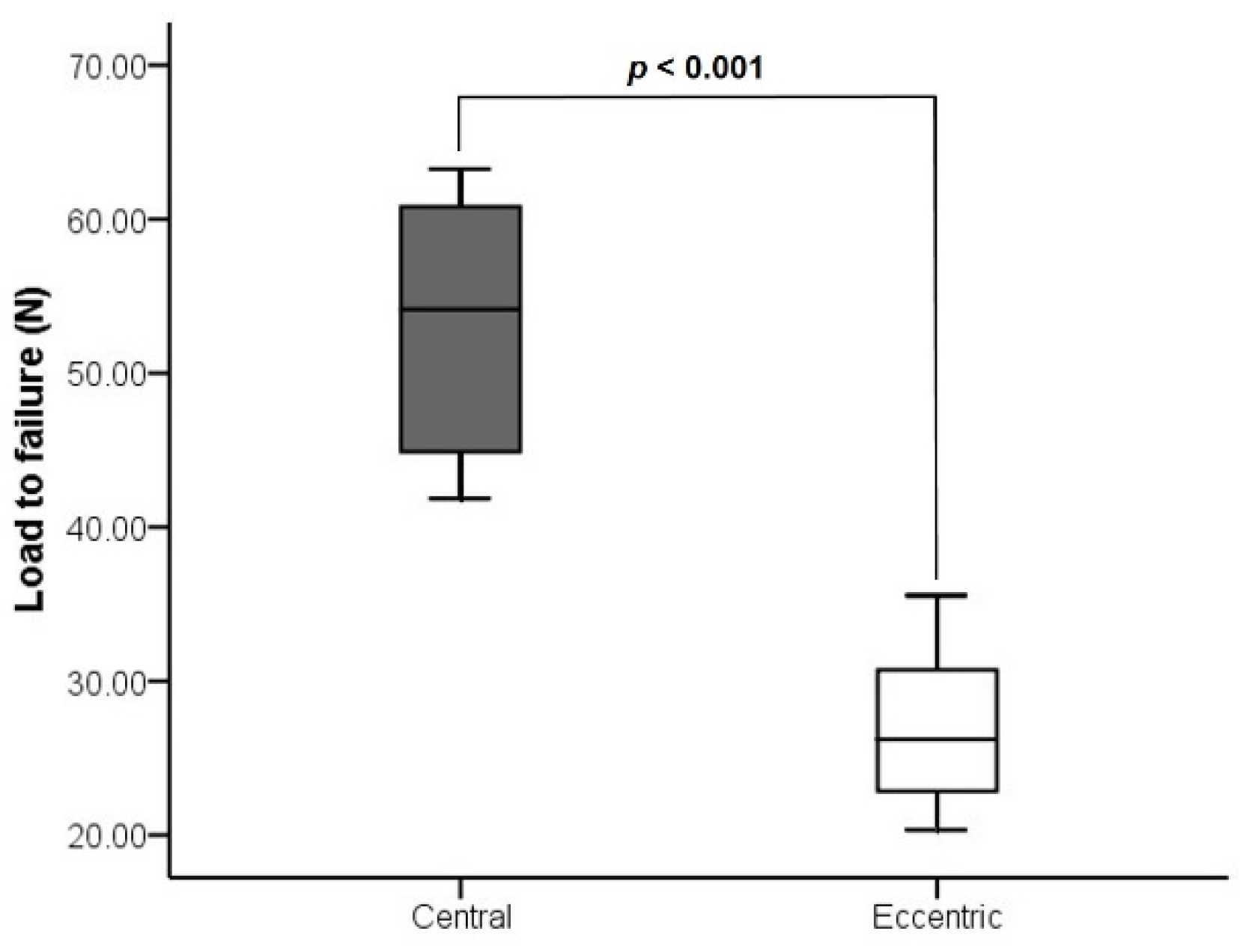
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Haddad, F.S.; Goddard, N.J. Acute percutaneous scaphoid fixation. J. Bone Joint Surg. Br. 1998, 80-B, 95–99. [Google Scholar] [CrossRef]
- Bond, C.D.; Shin, A.Y.; McBride, M.T.; Dao, K.D. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J. Bone Joint Surg. Am. 2001, 83, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Geissler, W.B.; Adams, J.E.; Bindra, R.R.; Lanzinger, W.D.; Slutsky, D.J. Scaphoid fractures: What’s hot, what’s not. J. Bone Joint Surg. Am. 2012, 94, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Merrell, G.; Slade, J. Technique for percutaneous fixation of displaced and nondisplaced acute scaphoid fractures and select nonunions. J. Hand Surg. Am. 2008, 33, 966–973. [Google Scholar] [CrossRef] [PubMed]
- Slade, J.F.; Grauer, J.N.; Mahoney, J.D. Arthroscopic Reduction and Percutaneous Fixation of Scaphoid Fractures With a Novel Dorsal Technique. Orthop. Clin. N. Am. 2001, 32, 247–261. [Google Scholar] [CrossRef]
- Chan, K.W.; McAdams, T.R. Central screw placement in percutaneous screw scaphoid fixation: A cadaveric comparison of proximal and distal techniques. J. Hand Surg. Am. 2004, 29, 74–79. [Google Scholar] [CrossRef]
- Meermans, G.; Verstreken, F. Influence of screw design, sex, and approach in scaphoid fracture fixation. Clin. Orthop. Relat Res. 2012, 470, 1673–1681. [Google Scholar] [CrossRef] [Green Version]
- Acar, B.; Kose, O.; Kati, Y.A.; Egerci, O.F.; Turan, A.; Yuksel, H.Y. Comparison of volar versus dorsal screw fixation for scaphoid waist fractures: A finite element analysis. Orthop. Traumatol. Surg. Res. 2018, 104, 1107–1113. [Google Scholar] [CrossRef]
- Bushnell, B.D.; McWilliams, A.D.; Messer, T.M. Complications in dorsal percutaneous cannulated screw fixation of nondisplaced scaphoid waist fractures. J. Hand Surg. Am. 2007, 32, 827–833. [Google Scholar] [CrossRef]
- Meermans, G.; Van Glabbeek, F.; Braem, M.J.; van Riet, R.P.; Hubens, G.; Verstreken, F. Comparison of two percutaneous volar approaches for screw fixation of scaphoid waist fractures: Radiographic and biomechanical study of an osteotomy-simulated model. J. Bone Joint Surg. Am. 2014, 96, 1369–1376. [Google Scholar] [CrossRef]
- Zlotolow, D.A.; Knutsen, E.; Yao, J. Optimization of volar percutaneous screw fixation for scaphoid waist fractures using traction, positioning, imaging, and an angiocatheter guide. J. Hand Surg. Am. 2011, 36, 916–921. [Google Scholar] [CrossRef] [PubMed]
- Meermans, G.; Verstreken, F. Percutaneous transtrapezial fixation of acute scaphoid fractures. J. Hand Surg. Eur. Vol. 2008, 33, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Luria, S.; Schwarcz, Y.; Wollstein, R.; Emelife, P.; Zinger, G.; Peleg, E. 3-dimensional analysis of scaphoid fracture angle morphology. J. Hand Surg. Am. 2015, 40, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Fowler, J.R.; Ilyas, A.M. Headless compression screw fixation of scaphoid fractures. Hand Clin. 2010, 26, 351–361. [Google Scholar] [CrossRef]
- McCallister, W.V.; Knight, J.; Kaliappan, R.; Trumble, T.E. Central placement of the screw in simulated fractures of the scaphoid waist: A biomechanical study. J. Bone Joint Surg. Am. 2003, 85, 72–77. [Google Scholar] [CrossRef]
- Luria, S.; Lenart, L.; Lenart, B.; Peleg, E.; Kastelec, M. Optimal fixation of oblique scaphoid fractures: A cadaver model. J. Hand Surg. Am. 2012, 37, 1400–1404. [Google Scholar] [CrossRef]
- Smith, D.K.; Cooney, W.P., 3rd; An, K.N.; Linscheid, R.L.; Chao, E.Y. The effects of simulated unstable scaphoid fractures on carpal motion. J. Hand Surg. Am. 1989, 14, 283–291. [Google Scholar] [CrossRef]
- Kulkarni, R.W.; Wollstein, R.; Tayar, R.; Citron, N. Patterns of healing of scaphoid fractures. The importance of vascularity. J. Bone Joint Surg. Br. 1999, 81, 85–90. [Google Scholar] [CrossRef]
- Amirfeyz, R.; Bebbington, A.; Downing, N.D.; Oni, J.A.; Davis, T.R. Displaced scaphoid waist fractures: The use of a week 4 CT scan to predict the likelihood of union with nonoperative treatment. J. Hand Surg. Eur. Vol. 2011, 36, 498–502. [Google Scholar] [CrossRef]
- Patel, S.; Giugale, J.; Tiedeken, N.; Debski, R.E.; Fowler, J.R. Impact of Screw Length on Proximal Scaphoid Fracture Biomechanics. J. Wrist Surg. 2019, 8, 360–365. [Google Scholar] [CrossRef] [Green Version]
- Ma, C.H.; Wu, C.H.; Tu, Y.K.; Lin, T.S. Metaphyseal locking plate as a definitive external fixator for treating open tibial fractures--clinical outcome and a finite element study. Injury 2013, 44, 1097–1101. [Google Scholar] [CrossRef] [PubMed]
- Dodds, S.D.; Panjabi, M.M.; Slade, J.F., 3rd. Screw fixation of scaphoid fractures: A biomechanical assessment of screw length and screw augmentation. J. Hand Surg. Am. 2006, 31, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Trumble, T.E.; Gilbert, M.; Murray, L.W.; Smith, J.; Rafijah, G.; McCallister, W.V. Displaced scaphoid fractures treated with open reduction and internal fixation with a cannulated screw. J. Bone Joint Surg. Am. 2000, 82, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Faucher, G.K.; Golden, M.L., 3rd; Sweeney, K.R.; Hutton, W.C.; Jarrett, C.D. Comparison of screw trajectory on stability of oblique scaphoid fractures: A mechanical study. J. Hand Surg. Am. 2014, 39, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Luria, S.; Hoch, S.; Liebergall, M.; Mosheiff, R.; Peleg, E. Optimal fixation of acute scaphoid fractures: Finite element analysis. J. Hand Surg. Am. 2010, 35, 1246–1250. [Google Scholar] [CrossRef] [PubMed]
- Russe, O. Fracture of the carpal navicular. Diagnosis, non-operative treatment, and operative treatment. J. Bone Joint Surg. Am. 1960, 42-a, 759–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volk, I.; Gal, J.; Peleg, E.; Almog, G.; Luria, S. Three-dimensional comparison of alternative screw positions versus actual fixation of scaphoid fractures. Injury 2017, 48, 1183–1189. [Google Scholar] [CrossRef]
- Hart, A.; Mansuri, A.; Harvey, E.J.; Martineau, P.A. Central versus eccentric internal fixation of acute scaphoid fractures. J. Hand Surg. Am. 2013, 38, 66–71. [Google Scholar] [CrossRef]


| Number | Age/Gender | Group | Side | Length (mm) | Number | Age/Gender | Group | Side | Length (mm) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 54/F | Central | L | 25.0 | 9 | 71/M | Central | R | 31.0 |
| 2 | 54/F | Eccentric | R | 25.5 | 10 | 71/M | Eccentric | L | 31.5 |
| 3 | 66/F | Central | L | 26.0 | 11 | 51/M | Central | L | 30.0 |
| 4 | 66/F | Eccentric | R | 26.5 | 12 | 51/M | Eccentric | R | 29.5 |
| 5 | 59/M | Central | R | 27.5 | 13 | 42/M | Central | R | 28.5 |
| 6 | 59/M | Eccentric | L | 27.5 | 14 | 42/M | Eccentric | L | 28.5 |
| 7 | 50/F | Central | L | 27.0 | 15 | 67/F | Central | R | 27.0 |
| 8 | 50/F | Eccentric | R | 26.5 | 16 | 67/F | Eccentric | L | 27.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, T.-S.; Ma, C.-H.; Wu, C.-H.; Yen, C.-Y.; Jou, I.-M.; Tu, Y.-K. Biomechanical Comparison of Different Volar Screw Placements for Horizontal Oblique Scaphoid Fractures. Appl. Sci. 2020, 10, 8592. https://doi.org/10.3390/app10238592
Lin T-S, Ma C-H, Wu C-H, Yen C-Y, Jou I-M, Tu Y-K. Biomechanical Comparison of Different Volar Screw Placements for Horizontal Oblique Scaphoid Fractures. Applied Sciences. 2020; 10(23):8592. https://doi.org/10.3390/app10238592
Chicago/Turabian StyleLin, Ting-Sheng, Ching-Hou Ma, Chin-Hsien Wu, Cheng-Yo Yen, I-Ming Jou, and Yuan-Kun Tu. 2020. "Biomechanical Comparison of Different Volar Screw Placements for Horizontal Oblique Scaphoid Fractures" Applied Sciences 10, no. 23: 8592. https://doi.org/10.3390/app10238592





