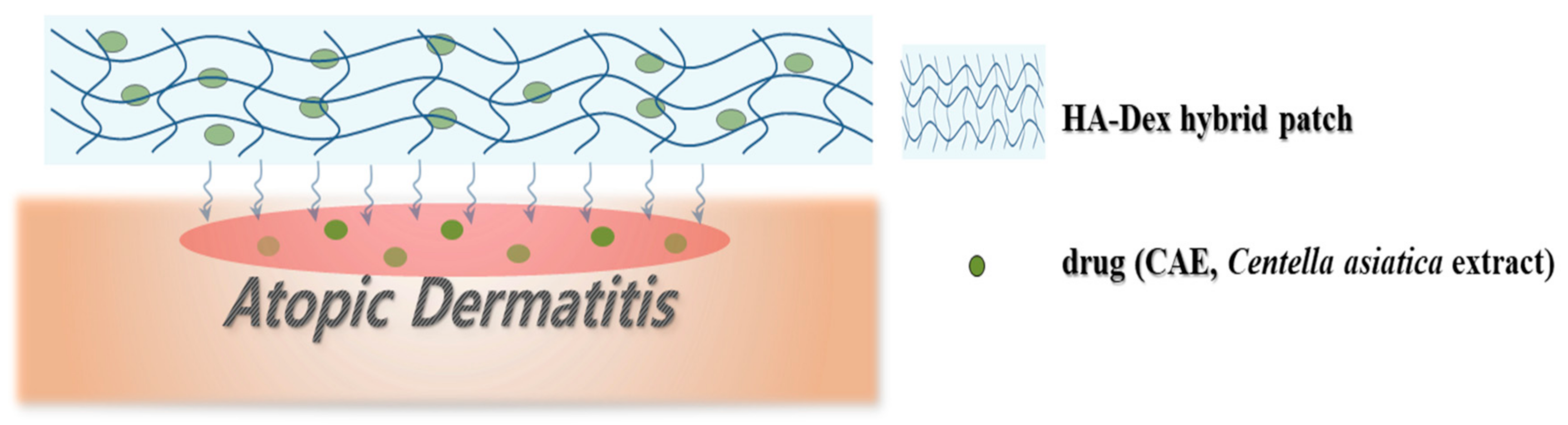
Development of a Natural Matrix Hybrid Hydrogel Patch and Evaluation of Its Efficacy against Atopic Dermatitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Manufacturing Method
2.2. Evaluation af Physical and Chemical Properties
2.3. Analysis of the Gelation Rate and Swelling Ratio
2.4. Analysis of CAE Release Profile
2.5. Cell Compatibility Analysis
2.6. Analysis of In Vitro Wound Closure
2.7. Statistical Analysis
3. Results and Discussion
3.1. Physical and Chemical Evaluation
3.2. Evaluation of Gelation Rate and Swelling Ratio
3.3. Evaluation of the CAE Release Profile
3.4. Biocompatibility Evaluation
3.5. Evaluation of In Vitro Wound Healing
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Park, Y.M. Advances in the pathophysiology of atopic dermatitis. Pediatr. Allergy Respir. Dis. 2006, 16, 189–196. [Google Scholar]
- Patrizi, A.; Raone, B.; Raboni, R.; Neri, I. Efficacy and tolerability of a cream containing AR-GG27® (sorbityl furfural palmitate) in the treatment of mild/moderate childhood atopic dermatitis associated with pityriasis alba. A double-blind, placebo-controlled clinical trial. G. Ital. Dermatol. Venereol. 2012, 147, 1–8. [Google Scholar]
- Garg, N.; Silverberg, J.I. Epidemiology of childhood atopic dermatitis. Clin. Dermatol. 2015, 33, 281–288. [Google Scholar] [CrossRef]
- Myles, I.A.; Earland, N.J.; Anderson, E.D.; Moore, I.N.; Kieh, M.D.; Williams, K.W.; Saleem, A.; Fontecilla, N.M.; Welch, P.A.; Darnell, D.A.; et al. First-in-human topical microbiome transplantation with Roseomonas mucosa for atopic dermatitis. JCI Insight 2018, 3, 120608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kyllönen, H.; Remitz, A.; Mandelin, J.M.; Elg, P.; Reitamo, S. Effects of 1-year intermittent treatment with topical tacrolimus monotherapy on skin collagen synthesis in patients with atopic dermatitis. Br. J. Dermatol. 2004, 150, 1174–1181. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, R. Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Int. J. Mol. Sci. 2017, 18, 606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, H.T.; Choi, H.J. Clinical efficacy of functional herbal extracts liquid in atopic dermatitis patient. Korean J. Food Nutr. 2005, 18, 380–384. [Google Scholar]
- Shon, M.Y.; Nam, S.H. Effect of Eucommia ulmoides extracts on allergic contact dermatitis and oxidative damage induced by repeat elicitation of DNCB. J. Korean Soc. Food Sci. Nutr. 2007, 36, 1517–1522. [Google Scholar] [CrossRef] [Green Version]
- Adtani, P.N.; Narasimhan, M.; Punnoose, A.M.; Kambalachenu, H.R. Antifibrotic effect of Centella asiatica Linn and asiatic acid on arecoline-induced fibrosis in human buccal fibroblasts. J. Investig. Clin. Dent. 2017, 8, 12208. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Choi, H.K.; N’deh, K.P.U.; Choi, Y.; Fan, M.; Kim, E.K.; Chung, K.H.; An, J.H. Inhibitory effect of Centella asiatica extract on DNCB-Induced atopic dermatitis in HaCaT cells and BALB/c mice. Nutrients 2020, 12, 411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.H.; Yeo, I.J.; Jang, J.S.; Kim, K.C.; Park, M.H.; Lee, H.P.; Han, S.B.; Hong, J.T. Combination effect of titrated extract of Centella asiatica and astaxanthin in a mouse model of phthalic anhydride-induced atopic dermatitis. Allergy Asthma Immunol. Res. 2019, 11, 548–559. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.F.; Conic, R.R.Z.; Kim, I.; Rowland, D.Y.; Nedorost, S.T. Atopy and sensitization to allergens known to cause systemic contact dermatitis. Dermatitis 2019, 30, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S.; Lee, Y.J.; Ryoo, W.S.; Noh, S.K. Preparation of high molecular weight atactic poly(vinyl alcohol) hydrogel by electron beam irradiation technique. Polymer (Korea) 2008, 32, 587–592. [Google Scholar]
- Chen, J.; Jo, S.; Park, K. Polysaccharide hydrogels for protein drug delivery. Carbohydr. Polym. 1995, 28, 69–76. [Google Scholar] [CrossRef]
- Hong, I.R.; Kim, Y.J. Self-Aggregated nanoparticles of lipoic acid conjugated hyaluronic acid. Polymer (Korea) 2008, 32, 561–565. [Google Scholar]
- Kim, K.T.; Kim, Y.H.; Kim, J.G.; Han, C.S.; Park, S.H.; Kim, K.H. Preparation of oligo hyaluronic acid by hydrolysis and its application as a cosmetic ingredient. J. Soc. Cosmet. Sci. Korea 2007, 33, 189. [Google Scholar]
- Wiegand, C.; Heinze, T.; Hipler, U.-C. Comparative in vitro study on cytotoxicity, antimicrobial activity, and binding capacity for pathophysiological factors in chronic wounds of alginate and silver-containing alginate. Wound Repair Regen. 2009, 17, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Grammatikos, A.P. The genetic and environmental basis of atopic diseases. Ann. Med. 2008, 40, 482–495. [Google Scholar] [CrossRef] [PubMed]









| Samples Weight Ratio (W/W) | HA-Dex Hybrid Patch * | CAE |
|---|---|---|
| Control | 10.0 | 0 |
| a | 9.8 | 0.2 |
| b | 9.6 | 0.4 |
| c | 9.4 | 0.6 |
| d | 9.2 | 0.8 |
| e | 9.0 | 1.0 |
| Patch Type | Total Intrusion Volume (Ml/G) | Total Pore Area (M2/G) | Median Pore Diameter (Volume/Nm) | Median Pore Diameter (Area/Nm) | Average Pore Diameter (4V/A) Nm | Porosity(%) |
|---|---|---|---|---|---|---|
| a | 1.6388 | 4.930 | 85,324.9 | 14.0 | 1329.6 | 68.2117 |
| b | 0.4233 | 0.943 | 16,078.3 | 77.7 | 1795.0 | 42.5677 |
| c | 0.4328 | 0.156 | 12,349.2 | 10,966.7 | 11,109.2 | 41.5143 |
| d | 0.3350 | 5.695 | 132,087.9 | 6.6 | 235.3 | 32.2406 |
| e | 0.2199 | 0.861 | 12,196.2 | 90.2 | 1021.8 | 26.5290 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, G.S.; Choi, J.Y.; Suh, J.S.; Lim, J.O.; Choi, J.H. Development of a Natural Matrix Hybrid Hydrogel Patch and Evaluation of Its Efficacy against Atopic Dermatitis. Appl. Sci. 2020, 10, 8759. https://doi.org/10.3390/app10238759
Hong GS, Choi JY, Suh JS, Lim JO, Choi JH. Development of a Natural Matrix Hybrid Hydrogel Patch and Evaluation of Its Efficacy against Atopic Dermatitis. Applied Sciences. 2020; 10(23):8759. https://doi.org/10.3390/app10238759
Chicago/Turabian StyleHong, Gyeong Sik, Jeong Yeon Choi, Jang Soo Suh, Jeong Ok Lim, and Jin Hyun Choi. 2020. "Development of a Natural Matrix Hybrid Hydrogel Patch and Evaluation of Its Efficacy against Atopic Dermatitis" Applied Sciences 10, no. 23: 8759. https://doi.org/10.3390/app10238759
APA StyleHong, G. S., Choi, J. Y., Suh, J. S., Lim, J. O., & Choi, J. H. (2020). Development of a Natural Matrix Hybrid Hydrogel Patch and Evaluation of Its Efficacy against Atopic Dermatitis. Applied Sciences, 10(23), 8759. https://doi.org/10.3390/app10238759






