Medical Robotic Bed to Prevent Pressure Sores
Abstract
:1. Introduction
2. Developed Robot Bed System
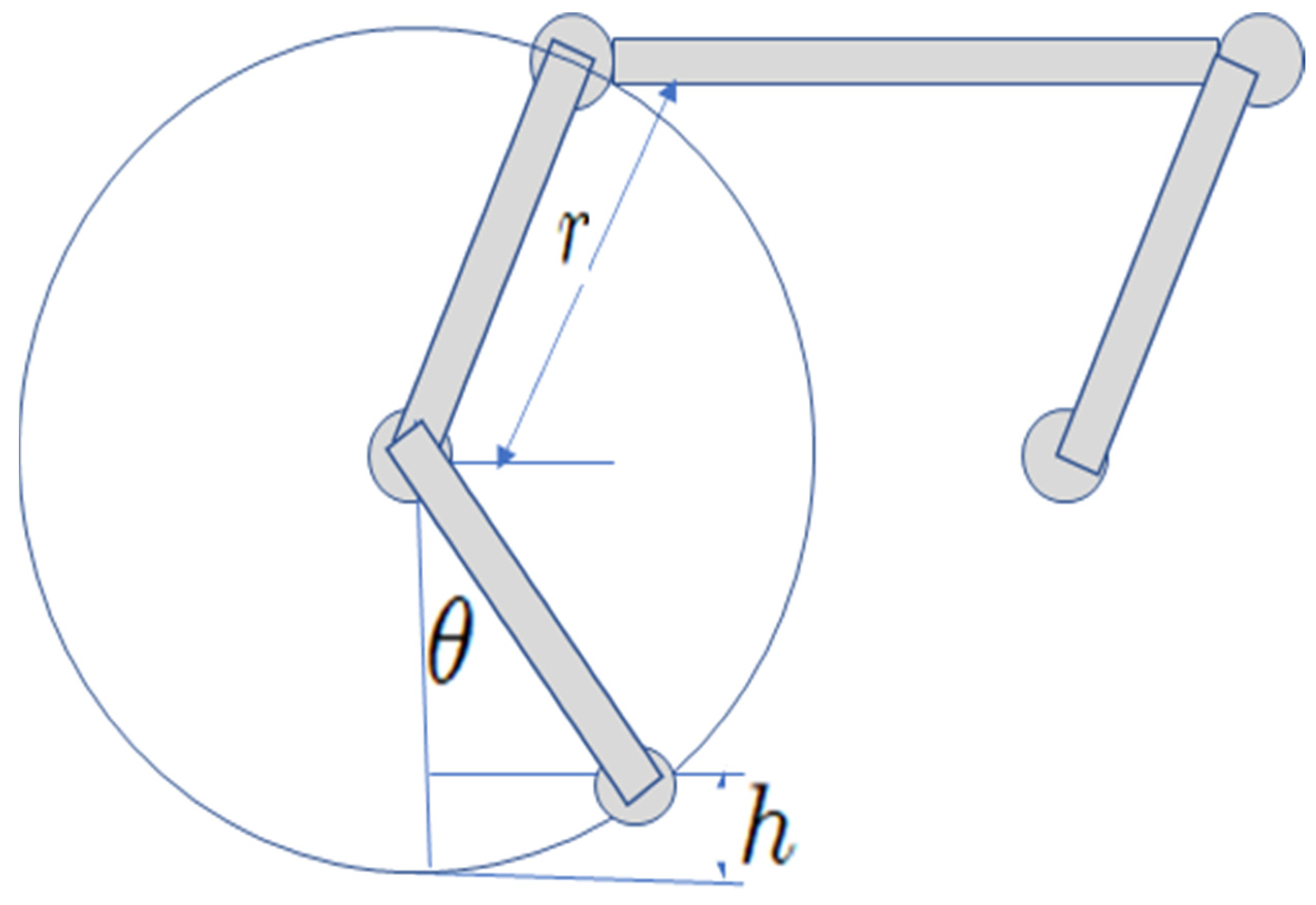
2.1. Robotic Bed Mechanism Design
2.2. Pressure Sensor
2.3. Control Laws
2.3.1. Closed-Loop Control Mode
2.3.2. Open-Loop Control Mode
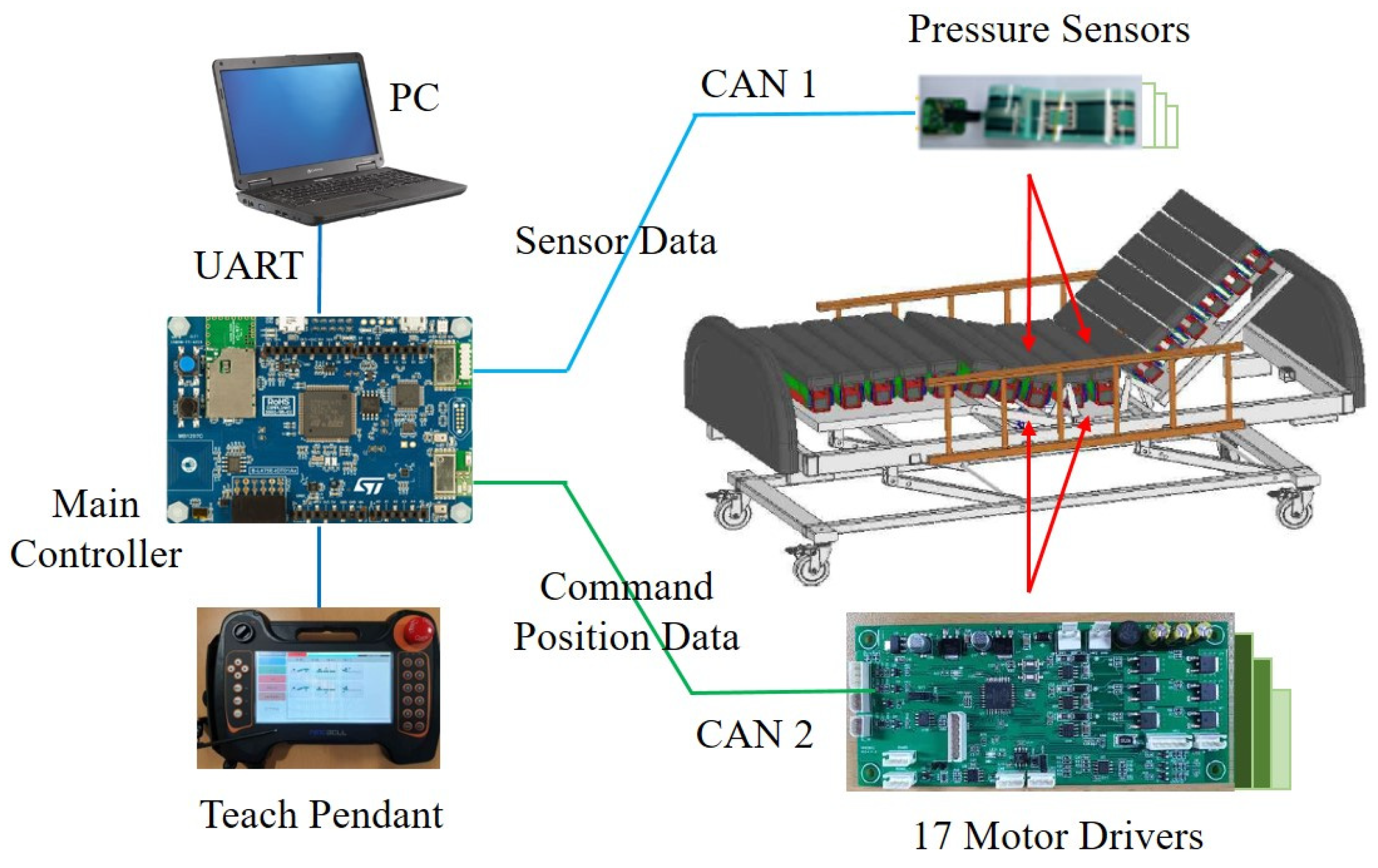
2.4. Integrated System
3. Experiments
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Kapusta, A.S.; Grice, P.M.; Clever, H.M.; Chitalia, Y.; Park, D.; Kemp, C.C. A system for bedside assistance that integrates a robotic bed and a mobile manipulator. PLoS ONE 2019, 14, e0221854. [Google Scholar] [CrossRef] [PubMed]
- Seo, K.; Oh, C.; Choi, T.; Lee, J. Bed-type robotic system for the bedridden. In Proceedings of the IEEE/ASME International Conference on Advanced Intelligent Mechatronics, Monterey, CA, USA, 24–28 July 2005; pp. 1170–1175. [Google Scholar] [CrossRef]
- Van der Loos, H.M.; Ullrich, N.; Kobayashi, H. Development of Sensate and Robotic Bed Technologies for Vital Signs Monitoring and Sleep Quality Improvement. Auton. Robot. 2003, 15, 67–79. [Google Scholar] [CrossRef]
- Wei, C.; Tung, T.; Hsiao, S.; Chen, W.; Chiu, Y.; Tu, K.; Yeh, C.; Chen, K. Hospital Bed with Auxiliary Functions of Lateral Positioning and Transferring for Immobilized Patients. In Proceedings of the IECON, Taipei, Taiwan, 5–8 November 2007; pp. 2991–2995. [Google Scholar] [CrossRef]
- Ning, M.; Ren, M.; Fan, Q.; Zhang, L. Mechanism design of a robotic chair/bed system for bedridden aged. Adv. Mech. Eng. 2017, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y. Evaluation of a pressure ulcer risk assessment tool. Korean Acad. Soc. Adult Nurs. 1997, 9, 272–285. [Google Scholar]
- Higgins, N. Management of a Pressure Ulcer in the Presence of Arterial Disease and MRSA Infection. Wound Pract. Res. J. Aust. Wound Manag. Assoc. 2008, 16, 166–168. [Google Scholar]
- Bennett, G.; Dealey, C.; Posnett, J. The cost of pressure ulcers in the UK. Age Ageing 2004, 33, 230–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russo, C.A.; Steiner, C.; Spector, W. Hospitalizations Related to Pressure Ulcers Among Adults 18 Years and Older, 2006: Statistical Brief #64. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2006. [Google Scholar]
- Hahn, M.; Klyscz, T. Synchronous measurement of blood pressure and red blood cell velocity in capillaries of human skin. J. Investig. Dermatol. 1996, 106, 1256–1259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soreless Bed. Available online: https://www.youtube.com/watch?v=wh56qajNYR8&feature=youtu.be (accessed on 9 August 2021).
- Smart Mattress. Available online: https://www.zdnet.co.kr/view/?no=20130726151317 (accessed on 9 August 2021). (In Korean).
- INSYDE. Available online: https://www.iis.fraunhofer.de/en/ff/sse/health/medical-sensors-and-analytics/prod/insyde.html (accessed on 9 August 2021).
- Yousefi, R.; Ostadabbas, S.; Faezipour, M.; Nourani, M.; Ng, V.; Tamil, L.; Bowling, A.; Behan, D.; Pompeo, M. A smart bed platform for monitoring & Ulcer prevention. In Proceedings of the International Conference on Biomedical Engineering and Informatics (BMEI), Shanghai, China, 15–17 October 2011; pp. 1362–1366. [Google Scholar] [CrossRef]
- Lee, K.-H.; Kwon, Y.-E.; Lee, H.; Lee, Y.; Seo, J.; Kwon, O.; Kang, S.-W.; Lee, D. Active Body Pressure Relief System with Time-of-Flight Optical Pressure Sensors for Pressure Ulcer Prevention. Sensors 2019, 19, 3862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misaki, A.; Imanishi, K.; Takasugi, S.; Wada, M.; Fukagawa, S.; Furue, M. Body pressure sensing mattress for bedsore prevention. SEI Tech. Rev. 2014, 78, 95–99. [Google Scholar]
- Lee, Y.; Kim, C.; Choi, M. Enhancement of 4 bar parallelogram linkage for a medical bed. J. Converg. Cult. Technol. 2020, 6, 515–520. [Google Scholar] [CrossRef]
- Lilly, J. Fuzzy Control and Identification; Wiley: Hoboken, NJ, USA, 2010. [Google Scholar]
- Seon, M.; Choi, J.; Lee, Y. Control Technique of a Medical Bed for Ulcer Prevention Equipped with Body Pressure Sensors. J. IIBC 2021, 21, 89–95. [Google Scholar] [CrossRef]
- Giovanelli, D.; Farella, E. Force sensing resistor and evaluation of technology for wearable body pressure sensing. J. Sens. 2016, 2016. [Google Scholar] [CrossRef] [Green Version]
















| Rule | If-Then |
|---|---|
| If e is ERR_LOW, then u is LOW | |
| If e is ERR_HIGH, then u is MEDIUM | |
| If e is ERR_VERYHIGH, then u is HIGH | |
| If e is ERR_TOOHIGH, then u is TOOHIGH |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seon, M.; Lee, Y.; Moon, C. Medical Robotic Bed to Prevent Pressure Sores. Appl. Sci. 2021, 11, 8459. https://doi.org/10.3390/app11188459
Seon M, Lee Y, Moon C. Medical Robotic Bed to Prevent Pressure Sores. Applied Sciences. 2021; 11(18):8459. https://doi.org/10.3390/app11188459
Chicago/Turabian StyleSeon, Minju, Youngdae Lee, and Chanwoo Moon. 2021. "Medical Robotic Bed to Prevent Pressure Sores" Applied Sciences 11, no. 18: 8459. https://doi.org/10.3390/app11188459
APA StyleSeon, M., Lee, Y., & Moon, C. (2021). Medical Robotic Bed to Prevent Pressure Sores. Applied Sciences, 11(18), 8459. https://doi.org/10.3390/app11188459








