Is Perpendicular Double Two-Hole Plates Fixation Superior to Single Four-Hole Plate Fixation to Treat Mandibular Symphysis Fracture?—A Finite Element Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
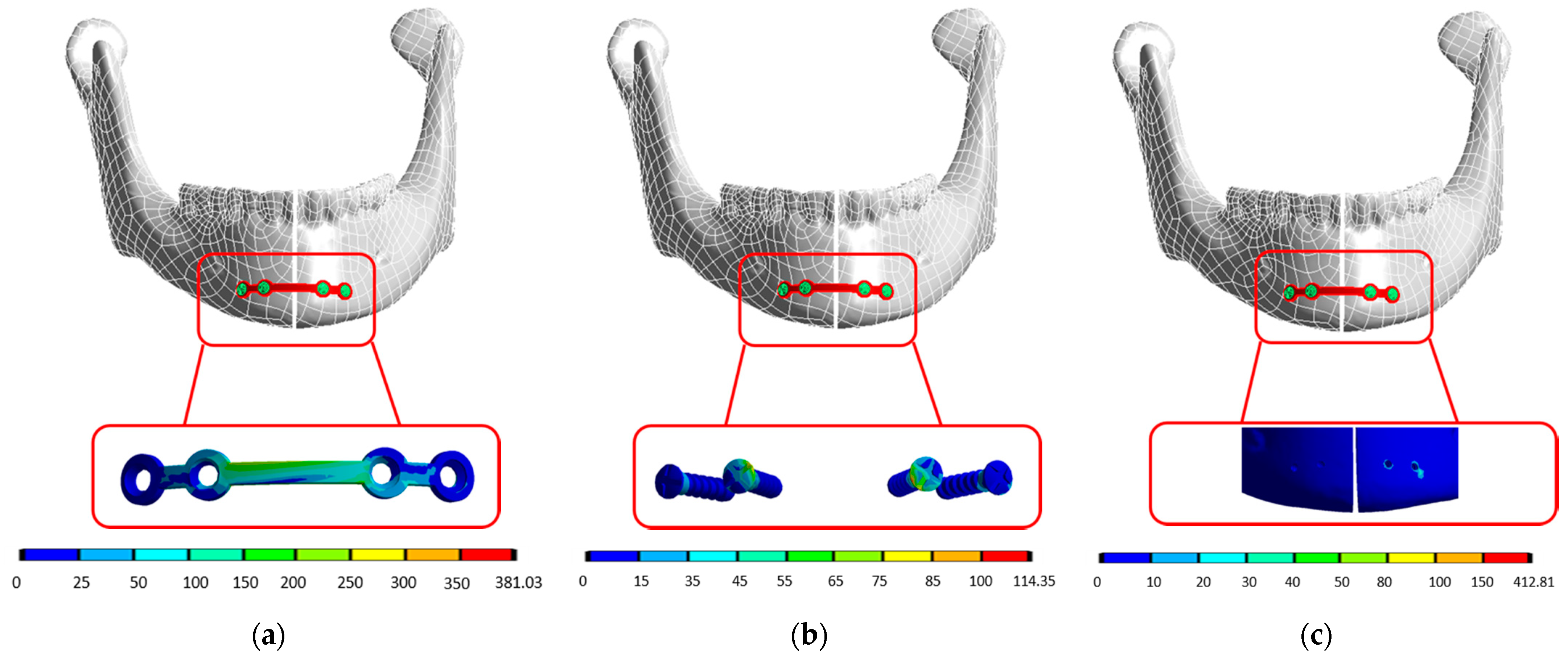
3.1. S4HP Group
3.2. Per4H2HP
3.3. PerD2HP
4. Discussion
4.1. Stress Shift on Plates
4.2. Stress Shift on Screws
4.3. Stress Shift on Screw Holes
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Erol, B.; Tanrikulu, R.; Görgün, B. Maxillofacial Fractures. Analysis of demographic distribution and treatment in 2901patients (25-year experience). J. Cranio-Maxillofac. Surg. 2004, 32, 308–313. [Google Scholar] [CrossRef]
- Haug, R.H.; Prather, J.; Thomas Indresano, A. An epidemiologic survey of facial fractures and concomitant injuries. J. Oral Maxillofac. Surg. 1990, 48, 926–932. [Google Scholar] [CrossRef]
- Ahmed, H.E.A.; Jaber, M.A.; Abu Fanas, S.H.; Karas, M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: A review of 230 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2004, 98, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Boole, J.R.; Holtel, M.; Amoroso, P.; Yore, M. 5196 mandible fractures among 4381 active duty army soldiers, 1980 to 1998. Laryngoscope 2001, 111, 1691–1696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brasileiro, B.F.; Passeri, L.A. Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2006, 102, 28–34. [Google Scholar] [CrossRef]
- Martini, M.Z.; Takahashi, A.; Oliveira Neto, H.G.d.; Carvalho Júnior, J.P.d.; Curcio, R.; Shinohara, E.H. Epidemiology of mandibular fractures treated in a Brazilian level I trauma public hospital in the city of São Paulo, Brazil. Braz. Dent. J. 2006, 17, 243–248. [Google Scholar] [CrossRef]
- Lamphier, J.; Ziccardi, V.; Ruvo, A.; Janel, M. Complications of mandibular fractures in an urban teaching center. J. Oral Maxillofac. Surg. 2003, 61, 745–749. [Google Scholar] [CrossRef]
- Søballe, K. Hydroxyapatite ceramic coating for bone implant fixation: Mechanical and histological studies in dogs. Acta Orthop. Scand. 1993, 64, 1–58. [Google Scholar] [CrossRef] [PubMed]
- Tams, J.; Van Loon, J.-P.; Otten, B.; Bos, R.R.M. A computer study of biodegradable plates for internal fixation of mandibular angle fractures. J. Oral Maxillofac. Surg. 2001, 59, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Arora, L.; Bhardwaj, S.; Hashmi, G.S.; Anwar, S.F.; Rahman, S.A. Finite Element Analysis (FEA) of Perpendicular Plating Versus Conventional Plating in Mandibular Symphysis Fracture. J. Maxillofac. Oral Surg. 2020, 19, 143–148. [Google Scholar] [CrossRef]
- Arbag, H.; Korkmaz, H.H.; Ozturk, K.; Uyar, Y. Comparative Evaluation of Different Miniplates for Internal Fixation of Mandible Fractures Using Finite Element Analysis. J. Oral Maxillofac. Surg. 2008, 66, 1225–1232. [Google Scholar] [CrossRef]
- Ji, B.; Wang, C.; Liu, L.; Long, J.; Tian, W.; Wang, H. A biomechanical analysis of titanium miniplates used for treatment of mandibular symphyseal fractures with the finite element method. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 109, e21–e27. [Google Scholar] [CrossRef]
- Madsen, M.J.; McDaniel, C.A.; Haug, R.H. A Biomechanical Evaluation of Plating Techniques Used for Reconstructing Mandibular Symphysis/Parasymphysis Fractures. J. Oral Maxillofac. Surg. 2008, 66, 2012–2019. [Google Scholar] [CrossRef]
- Tams, J.; van Loon, J.P.; Otten, E.; Rozema, F.R.; Bos, R.R.M. A three-dimensional study of bending and torsion moments for different fracture sites in the mandible: An in vitro study. Int. J. Oral Maxillofac. Surg. 1997, 26, 383–388. [Google Scholar] [CrossRef]
- Lovald, S.; Baack, B.; Gaball, C.; Olson, G.; Hoard, A. Biomechanical Optimization of Bone Plates Used in Rigid Fixation of Mandibular Symphysis Fractures. J. Oral Maxillofac. Surg. 2010, 68, 1833–1841. [Google Scholar] [CrossRef]
- Tams, J.; van Loon, J.P.; Rozema, F.R.; Otten, E.; Bos, P.R.M. A three-dimensional study of loads across the fracture for different fracture sites of the mandible. Br. J. Oral Maxillofac. Surg. 1996, 34, 400–405. [Google Scholar] [CrossRef]
- Vieira e Oliveira, T.R.; Passeri, L.A. Mechanical Evaluation of Different Techniques for Symphysis Fracture Fixation—An In Vitro Polyurethane Mandible Study. J. Oral Maxillofac. Surg. 2011, 69, e141–e146. [Google Scholar] [CrossRef] [PubMed]
- Kimura, A.; Nagasao, T.; Kaneko, T.; Miyamoto, J.; Nakajima, T. A comparative study of most suitable miniplate fixation for mandibular symphysis fracture using a finite element model. Keio J. Med. 2006, 55, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Zhang, Y.; An, J.G.; He, Y. Use of two 2.0 mini-plates for width-controlling fixation of symphyseal/parasymphyseal fractures associated with bilateral condylar fractures: A retrospective investigation of 45 cases. Int. J. Oral Maxillofac. Surg. 2015, 44, e27–e28. [Google Scholar] [CrossRef]
- Prein, J.; Lüscher, N.J. Anatomic Approaches. In Manual of Internal Fixation in the Cranio-Facial Skeleton: Techniques Recommended by the AO/ASIF Maxillofacial Group; Prein, J., Ed.; Springer: Berlin/Heidelberg, Germany, 1998; pp. 51–56. [Google Scholar]
- Peterson, L.J. Peterson’s Principles of Oral and Maxillofacial Surgery; PMPH-USA: Shelton, CT, USA, 2012; Volume 1. [Google Scholar]
- Kharmanda, G.; Kharma, M.-Y. Evaluating the Effect of Minimizing Screws on Stabilization of Symphysis Mandibular Fracture by 3D Finite Element Analysis. J. Maxillofac. Oral Surg. 2017, 16, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.-S.; Tsai, F.-D.; Chen, C.-Y.; Lin, L.-W. Factorial analysis of variables affecting bone stress adjacent to the orthodontic anchorage mini-implant with finite element analysis. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 182–189. [Google Scholar] [CrossRef]
- Manafi Khajeh Pasha, A.; Mahmoudi Sheykhsarmast, R.; Manafi Khajeh Pasha, S.; Khashabi, E. Influence of Treatment Plans on Stress and Deformation Distribution in Mandibular Implant-Supported Overdenture and Mandibular Bone under Traumatic Load: A 3D FEA. J. Med. Biol. Eng. 2021, 41, 543–557. [Google Scholar] [CrossRef]
- Moiduddin, K. Implementation of Computer-Assisted Design, Analysis, and Additive Manufactured Customized Mandibular Implants. J. Med. Biol. Eng. 2018, 38, 744–756. [Google Scholar] [CrossRef]
- Chang, L.-R.; Chen, C.-C.; Jeng, S.F.; Chen, Y.-R.; Hwang, L.-C.; Lin, T.-S. Investigation of a Modified Novel Technique in Bilateral Sagittal Splitting Osteotomy Fixation: Finite Element Analysis and In Vitro Biomechanical Test. BioMed Res. Int. 2020, 2020, 8707389. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H. Biomechanical Analysis of Mandibular Symphyseal Fracture with Different Fixation Configurations. Master’s Thesis, I-Shou University, Kaohsiung, Taiwan, 2016. [Google Scholar]
- Ramos, A.; Completo, A.; Relvas, C.; Mesnard, M.; Simões, J.A. Straight, semi-anatomic and anatomic TMJ implants: The influence of condylar geometry and bone fixation screws. J. Cranio-Maxillofac. Surg. 2011, 39, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Kao, M.-H. Investigation of Intraoral Stability on Bilateral Sagittal Split Osteotomy with Various Fixation Configurations. Master’s Thesis, I-Shou University, Kaohsiung, Taiwan, 2013. [Google Scholar]
- Rudderman, R.H.; Mullen, R.L. Biomechanics Of The Facial Skeleton. Clin. Plast. Surg. 1992, 19, 11–29. [Google Scholar] [CrossRef]
- Schilli, W.; Stoll, P.; Bähr, W.; Prein, J. Mandibular Fractures. In Manual of Internal Fixation in the Cranio-Facial Skeleton: Techniques Recommended by the AO/ASIF Maxillofacial Group; Prein, J., Ed.; Springer: Berlin/Heidelberg, Germany, 1998; pp. 57–93. [Google Scholar]


| S4HP | Per4H2HP | PerD2HP |
|---|---|---|
 |  |  |
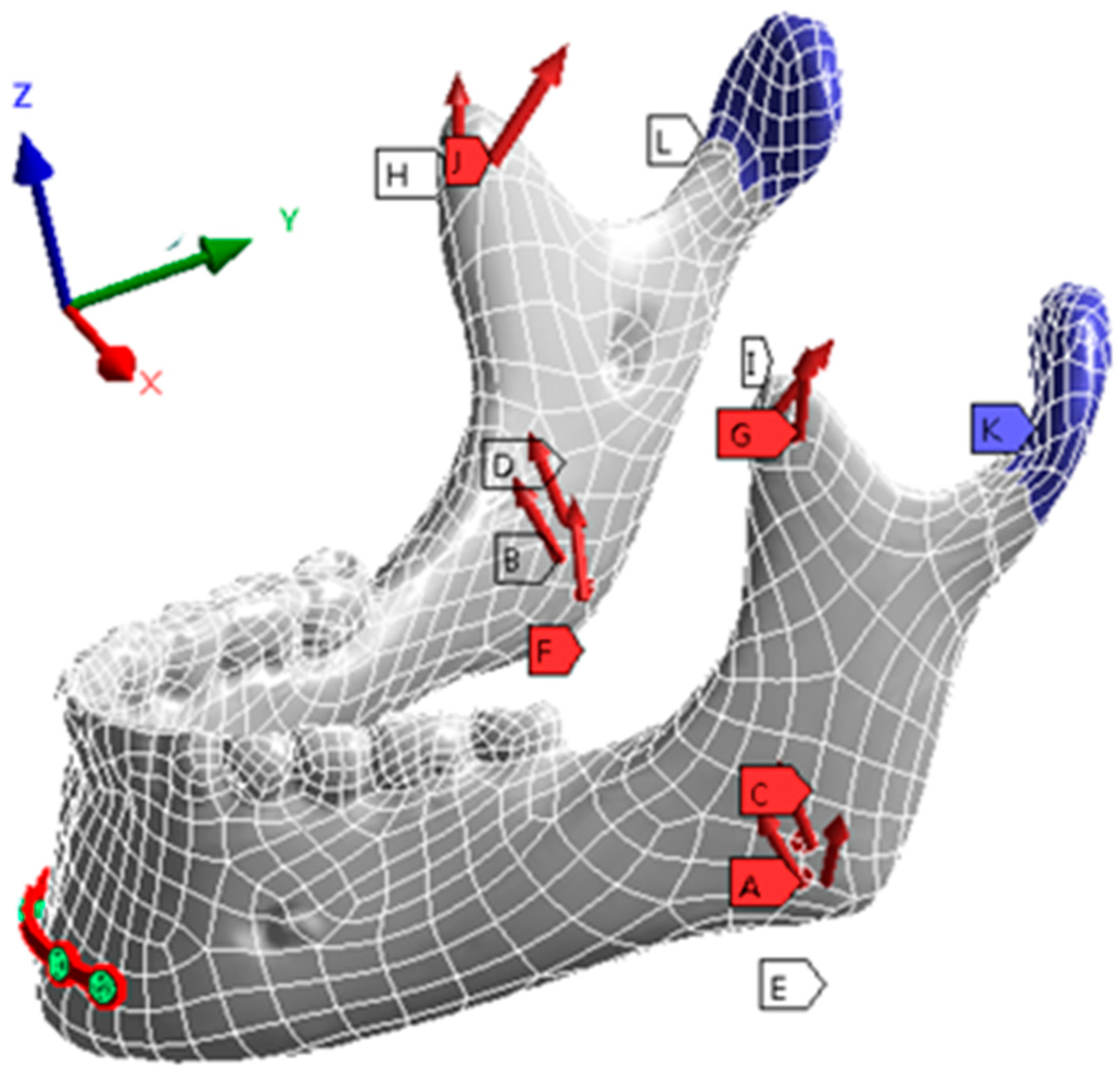
| Muscles Actions | Ref. | Loads (N) | ||
|---|---|---|---|---|
| X axis | Y axis | Z axis | ||
| Deep masseter | A, B | 7.776 | 127.23 | 22.68 |
| Superficial masseter | C, D | 12.873 | 183.5 | 12.11 |
| Medial pterygoid | E, F | 140.38 | 237.8 | −77.3 |
| Temporalis | G, H | 0.064 | 0.37 | −0.13 |
| Medial temporalis | I, J | 0.97 | 5.68 | −7.44 |
| S4HP | Per4H2HP | PerD2HP | |
|---|---|---|---|
| Anterior lower border | 381.03 | 407.31 | 354.63 |
| Inferior border | 550.44 | 562.58 |
| Muscles Actions | Location | S4HP | Per4H2HP | PerD2HP | |
|---|---|---|---|---|---|
| Anterior lower border | Right | Outer hole | 32.897 | 111.18 | 140.4 |
| Medial hole | 107.66 | 155.79 | |||
| Left | Outer hole | 114.35 | 310.73 | 100.32 | |
| Medial hole | 88.145 | 98.197 | |||
| Inferior border | Right | 185.45 | 442.19 (+138.44%) | ||
| Left | 259.18 | 107.05 (−142.11%) | |||
| Muscles Actions | Location | S4HP | Per4H2HP | PerD2HP | |
|---|---|---|---|---|---|
| Anterior lower border | Right | Outer hole | 13.145 | 23.278 | 80.758 |
| Medial hole | 10.554 | 24.611 | |||
| Left | Outer hole | 14.16 | 35.14 | 31.519 | |
| Medial hole | 32.68 | 64.483 | |||
| Inferior border | Right | 58.582 | 132.03 (+125.38%) | ||
| Left | 98.035 | 39.189 (−60.02%) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, L.-R.; Hou, Y.-P.; Lin, T.-S. Is Perpendicular Double Two-Hole Plates Fixation Superior to Single Four-Hole Plate Fixation to Treat Mandibular Symphysis Fracture?—A Finite Element Study. Appl. Sci. 2021, 11, 8629. https://doi.org/10.3390/app11188629
Chang L-R, Hou Y-P, Lin T-S. Is Perpendicular Double Two-Hole Plates Fixation Superior to Single Four-Hole Plate Fixation to Treat Mandibular Symphysis Fracture?—A Finite Element Study. Applied Sciences. 2021; 11(18):8629. https://doi.org/10.3390/app11188629
Chicago/Turabian StyleChang, Li-Ren, Ya-Pei Hou, and Ting-Sheng Lin. 2021. "Is Perpendicular Double Two-Hole Plates Fixation Superior to Single Four-Hole Plate Fixation to Treat Mandibular Symphysis Fracture?—A Finite Element Study" Applied Sciences 11, no. 18: 8629. https://doi.org/10.3390/app11188629
APA StyleChang, L.-R., Hou, Y.-P., & Lin, T.-S. (2021). Is Perpendicular Double Two-Hole Plates Fixation Superior to Single Four-Hole Plate Fixation to Treat Mandibular Symphysis Fracture?—A Finite Element Study. Applied Sciences, 11(18), 8629. https://doi.org/10.3390/app11188629






