Influence of Examiners’ Experience and Region of Interest Location on Semiquantitative Elastography Validity and Reliability
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
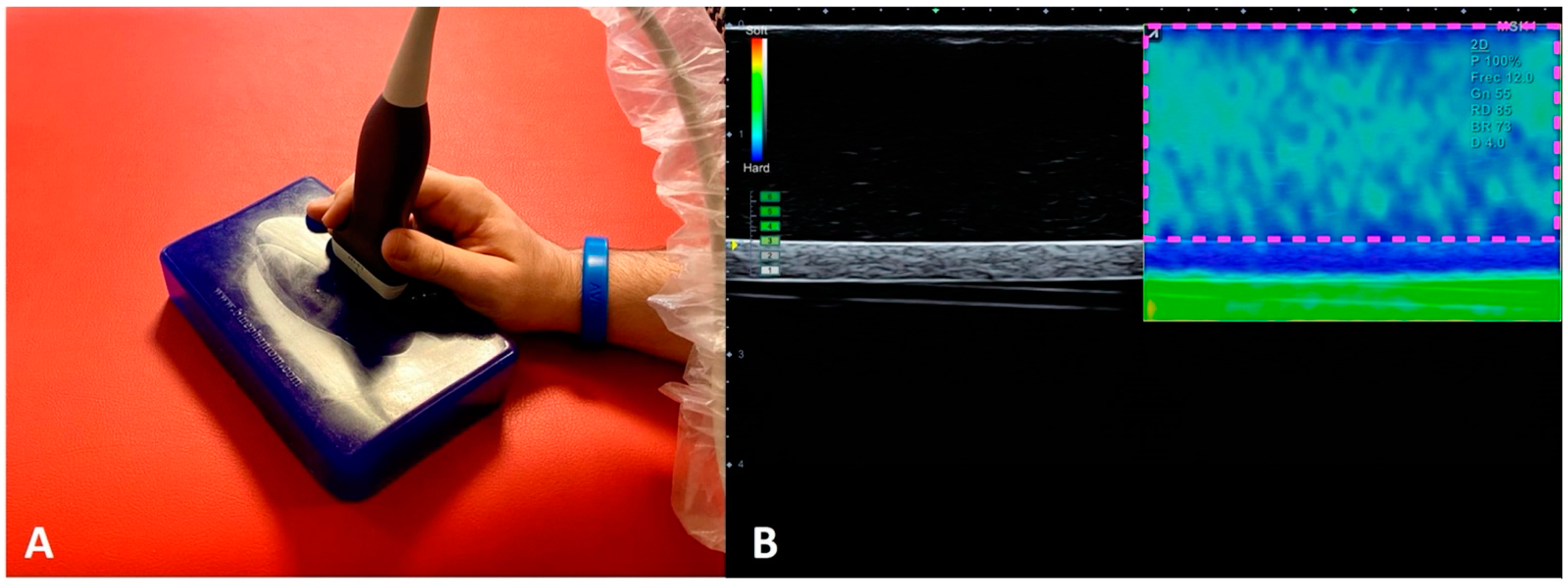
2.2. Imaging Acquisition Procedures
2.3. Measurement Assessment Procedures
- (1)
- Lateral areas of the image: First, the caliper was used to measure 1 cm from the top right corner of the image to the left. Then the area selector tool was utilized to contour a rectangle with 1 cm width and a height equal to the distance between the most superficial limit of the phantom to the most superficial limit of the cylindrical structure. Finally, another rectangle with same measurements (height and width) was placed in the top left corner of the image to obtain the SR.
- (2)
- Central areas of the image: Within the central 2 cm that were not included in the previous measurement, the distance from the surface of the phantom and the upper limit of the cylindrical structure was divided by 2. Following this, a rectangle was contoured with a width of 2 cm and the upper half of the distance previously calculated from the surface to the fake vessel. Finally, the SR between the upper rectangle and the lower rectangle was calculated.
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Clinical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Whittaker, J.L.; Teyhen, D.S.; Elliott, J.M.; Cook, K.; Langevin, H.M.; Dahl, H.H.; Stokes, M. Rehabilitative Ultrasound Imaging: Understanding the Technology and Its Applications. J. Orthop. Sports Phys. Ther. 2007, 37, 434–449. [Google Scholar] [CrossRef]
- Valera-Calero, J.A.; Sánchez-Jorge, S.; Alvarez-González, J.; Ortega-Santiago, R.; Cleland, J.A.; Fernández-De-Las-Peñas, C.; Arias-Buría, J.L. Intra-rater and inter-rater reliability of rehabilitative ultrasound imaging of cervical multifidus muscle in healthy people: Imaging capturing and imaging calculation. Musculoskelet. Sci. Pract. 2020, 48, 102158. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A.; Gallego-Sendarrubias, G.; Fernández-De-Las-Peñas, C.; Cleland, J.A.; Ortega-Santiago, R.; Arias-Buría, J.L. Cross-Sectional Area of the Cervical Extensors assessed with Panoramic Ultrasound Imaging: Preliminary Data in Healthy People. Musculoskelet. Sci. Pract. 2020, 50, 102257. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A.; Arias-Buría, J.L.; Fernández-De-Las-Peñas, C.; Cleland, J.A.; Gallego-Sendarrubias, G.M.; Cimadevilla-Fernández-Pola, E. Echo-intensity and fatty infiltration ultrasound imaging measurement of cervical multifidus and short rotators in healthy people: A reliability study. Musculoskelet. Sci. Pract. 2021, 53, 102335. [Google Scholar] [CrossRef]
- Gennisson, J.-L.; Deffieux, T.; Fink, M.; Tanter, M. Ultrasound elastography: Principles and techniques. Diagn. Interv. Imaging 2013, 94, 487–495. [Google Scholar] [CrossRef]
- Sigrist, R.M.; Liau, J.; El Kaffas, A.; Chammas, M.C.; Willmann, J.K. Ultrasound Elastography: Review of Techniques and Clinical Applications. Theranostics 2017, 7, 1303–1329. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.H.; Kim, J.Y.; Kim, D.H.; Kim, Y.I.; Cho, J.H. Sonoelastography on Supraspinatus Muscle-Tendon and Long Head of Biceps Tendon in Korean Professional Baseball Pitchers. Korean J. Sports Med. 2016, 34, 28–35. [Google Scholar] [CrossRef] [Green Version]
- Franchi-Abella, S.; Elie, C.; Correas, J.-M. Performances and Limitations of Several Ultrasound-Based Elastography Techniques: A Phantom Study. Ultrasound Med. Biol. 2017, 43, 2402–2415. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, R.; Suga, M.; Koyama, A.; Omatsu, T.; Tachibana, Y.; Ebner, D.K.; Obata, T. Measuring shear-wave speed with point shear-wave elastography and MR elastography: A phantom study. BMJ Open 2017, 7, e013925. [Google Scholar] [CrossRef]
- Ozturk, A.; Grajo, J.R.; Dhyani, M.; Anthony, B.W.; Samir, A.E. Principles of ultrasound elastography. Abdom. Radiol. 2018, 43, 773–785. [Google Scholar] [CrossRef]
- Mulabecirovic, A.; Vesterhus, M.; Gilja, O.H.; Havre, R.F. In Vitro Comparison of Five Different Elastography Systems for Clinical Applications, Using Strain and Shear Wave Technology. Ultrasound Med. Biol. 2016, 42, 2572–2588. [Google Scholar] [CrossRef] [Green Version]
- Valera-Calero, J.; Sánchez-Jorge, S.; Buffet-García, J.; Varol, U.; Gallego-Sendarrubias, G.; Álvarez-González, J. Is Shear-Wave Elastography a Clinical Severity Indicator of Myofascial Pain Syndrome? An Observational Study. J. Clin. Med. 2021, 10, 2895. [Google Scholar] [CrossRef] [PubMed]
- Carlsen, J.F.; Ewertsen, C.; Saftoiu, A.; Lönn, L.; Nielsen, M.B. Accuracy of Visual Scoring and Semi-Quantification of Ultrasound Strain Elastography—A Phantom Study. PLoS ONE 2014, 9, e88699. [Google Scholar] [CrossRef]
- Kimberlin, C.L.; Winterstein, A.G. Validity and reliability of measurement instruments used in research. Am. J. Health-Syst. Pharm. 2008, 65, 2276–2284. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, D.; De Vet, H.C.W.; et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015, 351, h5527. [Google Scholar] [CrossRef] [Green Version]
- Whittaker, J.L.; Ellis, R.; Hodges, P.W.; Osullivan, C.; Hides, J.; Carnero, S.F.; Arias-Buria, J.L.; Teyhen, D.S.; Stokes, M.J. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br. J. Sports Med. 2019, 53, 1447–1453. [Google Scholar] [CrossRef]
- Nicholls, J.; Alfuraih, A.; Hensor, E.M.A.; Robinson, P. Inter- and intra-reader reproducibility of shear wave elastography measurements for musculoskeletal soft tissue masses. Skelet. Radiol. 2020, 49, 779–786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, B.; Yan, F.; He, Y.; Wang, L.; Xiang, X.; Tang, Y.; Yang, Y.; Qiu, L. Evaluation of the healthy median nerve elasticity: Feasibility and reliability of shear wave elastography. Medicine 2018, 97, e12956. [Google Scholar] [CrossRef]
- Bachasson, D.; Dubois, G.J.; Allenbach, Y.; Benveniste, O.; Hogrel, J.Y. Muscle Shear Wave Elastography in Inclusion Body Myositis: Feasi-bility, Reliability and Relationships with Muscle Impairments. Ultrasound Med. Biol. 2018, 44, 1423–1432. [Google Scholar] [CrossRef]
- Hackett, M.; Aveledo, R.; Lam, P.H.; Murrell, G.A. Reliability of shear wave elastography ultrasound to assess the supraspinatus tendon: An intra and inter-rater in vivo study. Shoulder Elb. 2020, 12, 18–23. [Google Scholar] [CrossRef]
- Corrigan, P.; Zellers, J.A.; Balascio, P.; Silbernagel, K.G.; Cortes, D.H. Quantification of Mechanical Properties in Healthy Achilles Tendon Using Continuous Shear Wave Elastography: A Reliability and Validation Study. Ultrasound Med. Biol. 2019, 45, 1574–1585. [Google Scholar] [CrossRef]
- Thomas, L.; Low, J.; Chan, K.; Durbridge, G. Shear wave elastography of the cervical arteries: A novel approach to the assess-ment of cervical arterial wall stiffness. An investigation of psychometric properties and intra-rater reliability. Musculoskelet. Sci. Pract. 2019, 40, 96–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paluch, Ł.; Nawrocka-Laskus, E.; Wieczorek, J.; Mruk, B.; Frel, M.; Walecki, J. Use of Ultrasound Elastography in the Assessment of the Mus-culoskeletal System. Pol. J. Radiol. 2016, 81, 240–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drakonaki, E.E.; Allen, G.M.; Wilson, D.J. Real-time ultrasound elastography of the normal Achilles tendon: Reproducibility and pattern description. Clin. Radiol. 2009, 64, 1196–1202. [Google Scholar] [CrossRef]
- Klauser, A.S.; Faschingbauer, R.; Jaschke, W.R. Is sonoelastography of value in assessing tendons? Semin. Musculoskelet. Radiol. 2010, 14, 323–333. [Google Scholar] [CrossRef]
- Drakonaki, E.E.; Allen, G.M. Magnetic resonance imaging, ultrasound and real-time ultrasound elastography of the thigh muscles in congenital muscle dystrophy. Skelet. Radiol. 2010, 39, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Botar-Jid, C.; Damian, L.; Dudea, S.M.; Vasilescu, D.; Rednic, S.; Badea, R. The contribution of ultrasonography and sonoelastography in assessment of myositis. Med Ultrason. 2010, 12, 120–126. [Google Scholar]
- Yanagisawa, O.; Niitsu, M.; Kurihara, T.; Fukubayashi, T. Evaluation of human muscle hardness after dynamic exercise with ul-trasound real time tissue elastography: A feasibility study. Clin. Radiol. 2011, 66, 815–819. [Google Scholar] [CrossRef]
- Botanlioglu, H.; Kantarci, F.; Kaynak, G.; Unal, Y.; Ertan, S.; Aydingoz, O.; Erginer, R.; Unlu, M.C.; Mihmanli, I.; Babacan, M. Shear wave elastography properties of vastus lateralis and vastus me-dialis obliquus muscles in normal subjects and female patients with patellofemoral pain syndrome. Skelet. Radiol. 2013, 42, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Gerwin, R.D.; Shannon, S.; Hong, C.-Z.; Hubbard, D.; Gevirtz, R. Interrater reliability in myofascial trigger point examination. Pain 1997, 69, 65–73. [Google Scholar] [CrossRef]
- Sikdar, S.; Shah, J.P.; Gebreab, T.; Yen, R.H.; Gilliams, E.; Danoff, J.; Gerber, L.H. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Arch. Phys. Med. Rehabil. 2009, 90, 1829–1838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sikdar, S.; Ortiz, R.; Gebreab, T.; Gerber, L.H.; Shah, J.P. Understanding the vascular environment of myofascial trigger points using ultrasonic imaging and computational modeling. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; Volume 2010, pp. 5302–5305. [Google Scholar]
- Jafari, M.; Bahrpeyma, F.; Mokhtari-Dizaji, M.; Nasiri, A. Novel method to measure active myofascial trigger point stiffness using ultrasound imaging. J. Bodyw. Mov. Ther. 2018, 22, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Winn, N.; Lalam, R.; Cassar-Pullicino, V. Sonoelastography in the musculoskeletal system: Current role and future directions. World J. Radiol. 2016, 8, 868–879. [Google Scholar] [CrossRef] [PubMed]

| Examiner 1 (Experienced) (n = 50 Images) | Examiner 2 (Experienced) (n = 50 Images) | Examiner 3 (Novice) (n = 50 Images) | Examiner 4 (Novice) (n = 50 Images) | |
|---|---|---|---|---|
| Lateral areas of the image | ||||
| SR obtained † | 0.96 | 0.98 | 1.09 | 1.10 |
| 95% CI (Lower; upper limits) | 0.92; 1.00 | 0.90; 1.05 | 1.04; 1.14 | 1.03; 1.16 |
| Variability of the measurements (%) | 14.75 | 17.50 | 17.40 | 15.42 |
| Difference between examiners | 0.01 ± 0.04 a | 0.11 ± 0.05 d,† | ||
| 0.12 ± 0.03 b,† | 0.12 ± 0.04 e,† | |||
| 0.13 ± 0.04 c,† | 0.00 ± 0.04 f | |||
| Central area of the image | ||||
| SR obtained | 0.97 | 0.97 | 0.96 | 0.97 |
| 95% CI | 0.95; 0.98 | 0.95; 0.99 | 0.94; 0.98 | 0.94; 1.00 |
| Variability of the measurements (%) | 5.61 | 5.38 | 6.94 | 7.80 |
| Difference between examiners | 0.00 ± 0.01 a | 0.01 ± 0.01 d | ||
| 0.00 ± 0.01 b | 0.00 ± 0.01 e | |||
| 0.00 ± 0.02 c | 0.01 ± 0.02 f | |||
| Differences between measurement locations | ||||
| SR difference | 0.00 ± 0.02 | 0.00 ± 0.04 | 0.13 ± 0.02 * | 0.11 ± 0.03 * |
| Examiner 1 (Experienced) (n = 50 Images) | Examiner 2 (Experienced) (n = 50 Images) | Examiner 3 (Novice) (n = 50 Images) | Examiner 4 (Novice) (n = 50 Images) | |
|---|---|---|---|---|
| Lateral areas of the image | ||||
| SR obtained | 0.96 | 0.98 | 1.09 *,† | 1.10 *,† |
| Error | 0.03 ± 0.14 | 0.02 ± 0.17 | 0.09 ± 0.17 | 0.10 ± 0.15 |
| Absolute Error | 0.11 ± 0.09 | 0.14 ± 0.08 | 0.15 ± 0.12 | 0.14 ± 0.06 |
| Coefficient of Variation (%) | 0.14 | 0.17 | 0.15 | 0.13 |
| Percent Error (%) | 11.80 | 14.28 | 15.16 | 12.72 |
| Mean Error of Measurements | 0.14 ± 0.05 * | |||
| Central areas of the image | ||||
| SR obtained | 0.97 | 0.97 | 0.96 | 0.97 |
| Error | 0.02 ± 0.05 | 0.03 ± 0.06 | 0.03 ± 0.06 | 0.04 ± 0.06 |
| Absolute Error | 0.04 ± 0.03 | 0.05 ± 0.03 | 0.05 ± 0.05 | 0.06 ± 0.03 |
| Coefficient of Variation (%) | 0.05 | 0.06 | 0.06 | 0.06 |
| Percent Error (%) | 4.89 | 5.15 | 5.52 | 6.18 |
| Mean Error of Measurements | 0.05 ± 0.02 * | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valera-Calero, J.A.; Fernández-de-las-Peñas, C.; Fernández-Rodríguez, T.; Arias-Buría, J.L.; Varol, U.; Gallego-Sendarrubias, G.M. Influence of Examiners’ Experience and Region of Interest Location on Semiquantitative Elastography Validity and Reliability. Appl. Sci. 2021, 11, 9247. https://doi.org/10.3390/app11199247
Valera-Calero JA, Fernández-de-las-Peñas C, Fernández-Rodríguez T, Arias-Buría JL, Varol U, Gallego-Sendarrubias GM. Influence of Examiners’ Experience and Region of Interest Location on Semiquantitative Elastography Validity and Reliability. Applied Sciences. 2021; 11(19):9247. https://doi.org/10.3390/app11199247
Chicago/Turabian StyleValera-Calero, Juan Antonio, César Fernández-de-las-Peñas, Tomás Fernández-Rodríguez, José Luis Arias-Buría, Umut Varol, and Gracia María Gallego-Sendarrubias. 2021. "Influence of Examiners’ Experience and Region of Interest Location on Semiquantitative Elastography Validity and Reliability" Applied Sciences 11, no. 19: 9247. https://doi.org/10.3390/app11199247






