Picosecond Q-Switched 1064/532 nm Laser in Tattoo Removal: Our Single Center Experience
Abstract
:1. Introduction
2. Materials and Methods
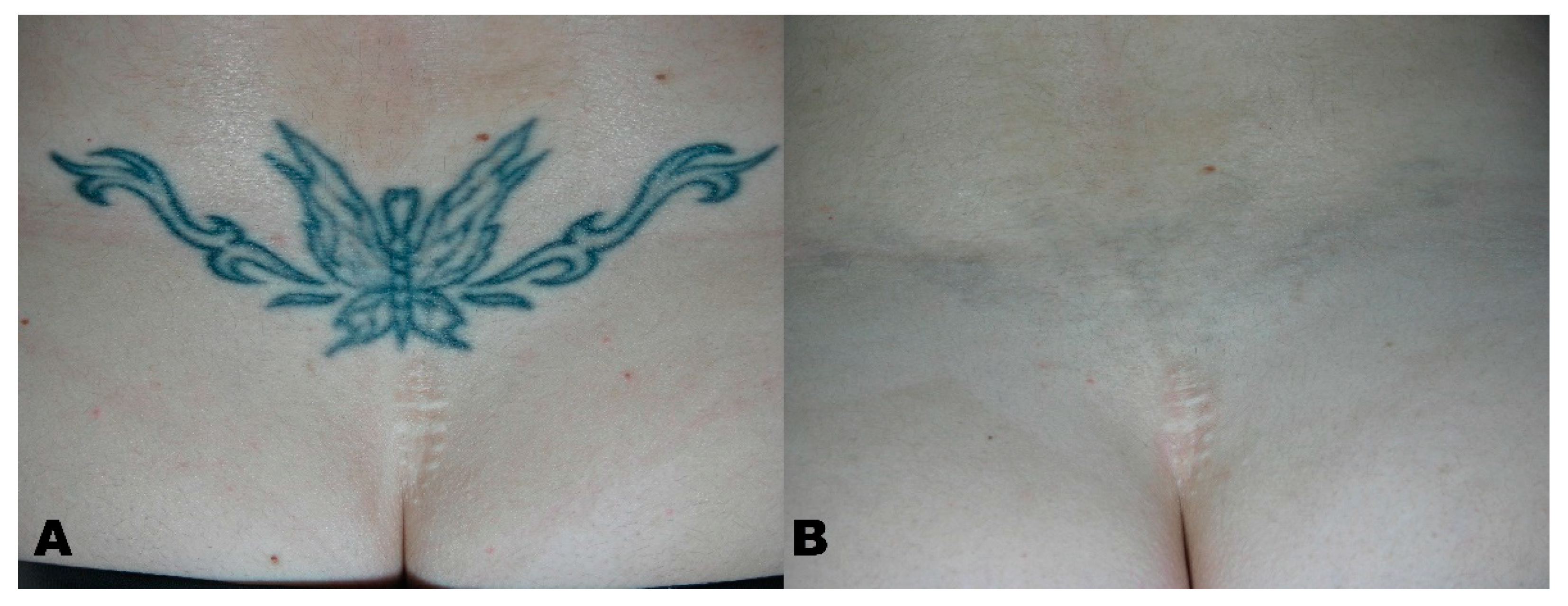
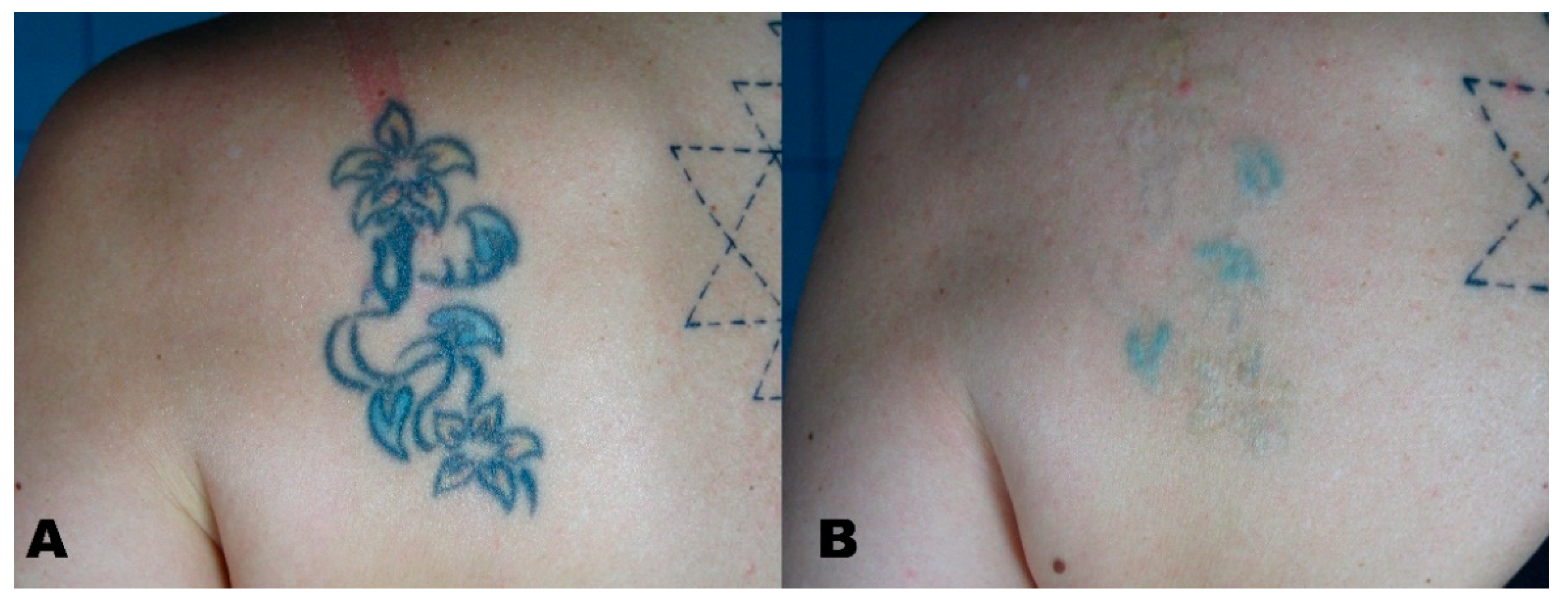
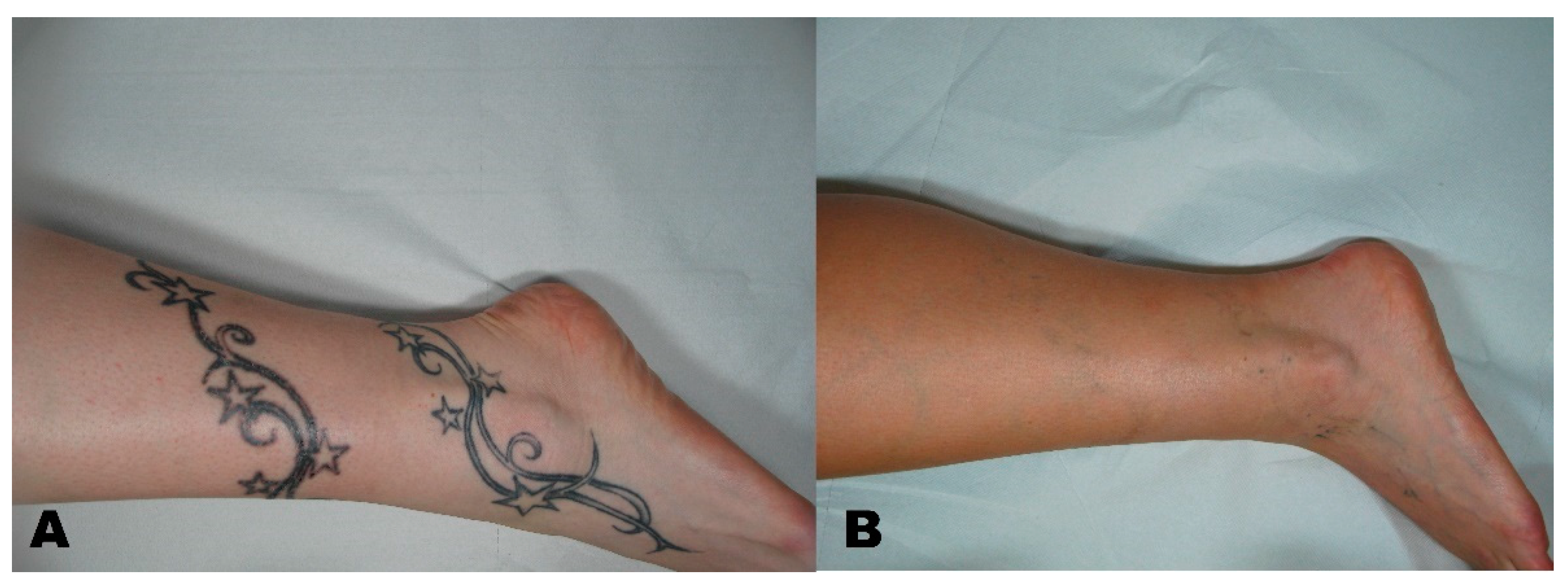
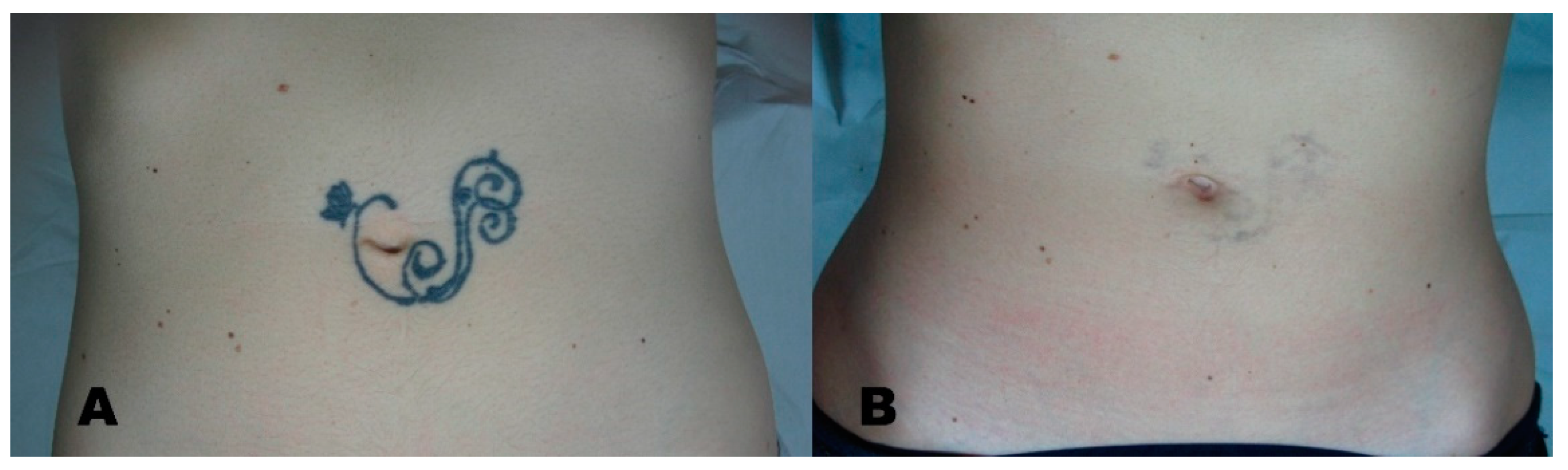
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Witkoś, J.; Hartman-Petrycka, M. Gender Differences in Subjective Pain Perception during and after Tattooing. Int. J. Environ. Res. Public Health 2020, 17, 9466. [Google Scholar] [CrossRef] [PubMed]
- Kluger, N.; Misery, L.; Seité, S.; Taieb, C. Regrets after tattooing and tattoo removal in the general population of France. J. Eur. Acad. Dermatol. Venereol. 2019, 33, e157–e159. [Google Scholar] [CrossRef] [PubMed]
- Zhitny, V.P.; Iftekhar, N. Tattoo Removal: A Practice from Ancient Times. Dermatology 2020, 236, 390–392. [Google Scholar] [CrossRef] [PubMed]
- Qu, Y.; Wang, L.; Zhou, P.; Zhang, W. Efficient Picosecond Laser for Tattoo Removal in Rat Models. Med. Sci. Monit. 2020, 26, e924583. [Google Scholar] [CrossRef] [PubMed]
- Laub, D.R.; Yules, R.B.; Arras, M.; Murray, D.E.; Crowley, L.; Chase, R.A. Preliminary histopathological observation of Q-switched ruby laser radiation on dermal tattoo pigment in man. J. Surg. Res. 1968, 8, 220–224. [Google Scholar] [CrossRef]
- Kim, M.; Park, S.; Lee, H.U.; Kang, H.W. Quantitative Monitoring of Tattoo Contrast Variations after 755-nm Laser Treatments in In Vivo Tattoo Models. Sensors 2020, 20, 285. [Google Scholar] [CrossRef] [Green Version]
- Mercuri, S.R.; Brianti, P.; Dattola, A.; Bennardo, L.; Silvestri, M.; Schipani, G.; Nisticò, S.P. CO2 laser and photodynamic therapy: Study of efficacy in periocular BCC. Dermatol. Ther. 2018, 31, e12616. [Google Scholar] [CrossRef]
- Cannarozzo, G.; Bennardo, L.; Negosanti, F.; Nisticò, S.P. CO2 Laser Treatment in Idiopathic Scrotal Calcinosis: A Case Series. J. Lasers Med. Sci. 2020, 11, 500–501. [Google Scholar] [CrossRef]
- Nistico, S.P.; Silvestri, M.; Zingoni, T.; Tamburi, F.; Bennardo, L.; Cannarozzo, G. Combination of Fractional CO2 Laser and Rhodamine-Intense Pulsed Light in Facial Rejuvenation: A Randomized Controlled Trial. Photobiomodul. Photomed. Laser Surg. 2021, 39, 113–117. [Google Scholar] [CrossRef]
- Lodi, G.; Sannino, M.; Caterino, P.; Cannarozzo, G.; Bennardo, L.; Nisticò, S.P. Fractional CO2 laser-assisted topical rifamycin drug delivery in the treatment of pediatric cutaneous leishmaniasis. Pediatr. Dermatol. 2021, 38, 717–720. [Google Scholar] [CrossRef] [PubMed]
- Lajevardi, V.; Mahmoudi, H.; Karimi, F.; Kalantari, Y.; Etesami, I. Comparing QS Nd:YAG laser alone with its combination with fractional ablative Er:YAG in tattoo removal. J. Cosmet. Dermatol. 2021. [Google Scholar] [CrossRef]
- Kurniadi, I.; Tabri, F.; Madjid, A.; Anwar, A.I.; Widita, W. Laser tattoo removal: Fundamental principles and practical approach. Dermatol. Ther. 2021, 34, e14418. [Google Scholar] [CrossRef] [PubMed]
- Goldust, M.; Wollina, U. Periorbital Hyperpigmentation—Dark Circles under the Eyes; Treatment Suggestions and Combining Procedures. Cosmetics 2021, 8, 26. [Google Scholar] [CrossRef]
- Del Duca, E.; Zingoni, T.; Bennardo, L.; Di Raimondo, C.; Garofalo, V.; Sannino, M.; Petrini, N.; Cannarozzo, G.; Bianchi, L.; Nisticò, S.P. Long-Term Follow-Up for Q-Switched Nd:YAG Treatment of Nevus of Ota: Are High Number of Treatments Really Required? A Case Report. Photobiomodul. Photomed. Laser Surg. 2021, 39, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Cannarozzo, G.; Negosanti, F.; Sannino, M.; Santoli, M.; Bennardo, L.; Banzola, N.; Negosanti, L.; Nisticò, S.P. Q-switched Nd:YAG laser for cosmetic tattoo removal. Dermatol. Ther. 2019, 32, e13042. [Google Scholar] [CrossRef]
- Kirby, W.; Desai, A.; Desai, T. The Kirby-Desai Scale: A proposed scale to assess tattoo removal treatments. J. Clin. Aesthet. Dermatol. 2009, 2, 32–37. [Google Scholar] [PubMed]
- Kato, H.; Doi, K.; Kanayama, K.; Araki, J.; Nakatsukasa, S.; Chi, D.; Mori, M.; Fuse, Y.; Sakae, Y.; Uozumi, T. Combination of Dual Wavelength Picosecond and Nanosecond Pulse Width Neodymium-Doped Yttrium-Aluminum-Garnet Lasers for Tattoo Removal. Lasers Surg. Med. 2020, 52, 515–522. [Google Scholar] [CrossRef]
- Lorgeou, A.; Perrillat, Y.; Gral, N.; Lagrange, S.; Lacour, J.P.; Passeron, T. Comparison of two picosecond lasers to a nanosecond laser for treating tattoos: A prospective randomized study on 49 patients. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 265–270. [Google Scholar] [CrossRef]
- Cannarozzo, G.; Nisticò, S.P.; Zappia, E.; Del Duca, E.; Provenzano, E.; Patruno, C.; Negosanti, F.; Sannino, M.; Bennardo, L. Q-Switched 1064/532 nm Laser with Nanosecond Pulse in Tattoo Treatment: A Double-Center Retrospective Study. Life 2021, 11, 699. [Google Scholar] [CrossRef]
- Karsai, S. Removal of Tattoos by Q-Switched Nanosecond Lasers. Curr. Probl. Dermatol. 2017, 52, 105–112. [Google Scholar] [CrossRef]
- Islam, P.S.; Chang, C.; Selmi, C.; Generali, E.; Huntley, A.; Teuber, S.S.; Gershwin, M.E. Medical Complications of Tattoos: A Comprehensive Review. Clin. Rev. Allergy Immunol. 2016, 50, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Pinto, F.; Große-Büning, S.; Karsai, S.; Weiß, C.; Bäumler, W.; Hammes, S.; Felcht, M.; Raulin, C. Neodymium-doped yttrium aluminium garnet (Nd:YAG) 1064-nm picosecond laser vs. Nd:YAG 1064-nm nanosecond laser in tattoo removal: A randomized controlledsingle-blind clinical trial. Br. J. Dermatol. 2017, 176, 457–464. [Google Scholar] [CrossRef] [PubMed]
- De las Alas, J.M.; Siripunvarapon, A.H.; Dofitas, B.L. Pulsed dye laser for the treatment of keloid and hypertrophic scars: A systematic review. Expert Rev. Med. Devices 2012, 9, 641–650. [Google Scholar] [CrossRef] [PubMed]
- Cannarozzo, G.; Silvestri, M.; Tamburi, F.; Sicilia, C.; Del Duca, E.; Scali, E.; Bennardo, L.; Nisticò, S. A new 675-nm laser device in the treatment of acne scars: An observational study. Lasers Med. Sci. 2021, 36, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Naga, L.I.; Alster, T.S. Laser Tattoo Removal: An Update. Am. J. Clin. Dermatol. 2017, 18, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Serup, J.; Bäumler, W. Guide to Treatment of Tattoo Complications and Tattoo Removal. Curr. Probl. Dermatol. 2017, 52, 132–138. [Google Scholar] [CrossRef]
- Hsu, V.M.; Aldahan, A.S.; Mlacker, S.; Shah, V.V.; Nouri, K. The picosecond laser for tattoo removal. Lasers Med. Sci. 2016, 31, 1733–1737. [Google Scholar] [CrossRef]
- Hutton Carlsen, K.; Esmann, J.; Serup, J. Tattoo removal by Q-switched yttrium aluminium garnet laser: Client satisfaction. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 904–909. [Google Scholar] [CrossRef]
- Silvestri, M.; Bennardo, L.; Zappia, E.; Tamburi, F.; Cameli, N.; Cannarozzo, G.; Nisticò, S.P. Q-Switched 1064/532 nm Laser with Picosecond Pulse to Treat Benign Hyperpigmentations: A Single-Center Retrospective Study. Appl. Sci. 2021, 11, 7478. [Google Scholar] [CrossRef]
- Pedrelli, V.; Azzopardi, E.; Azzopardi, E.; Tretti Clementoni, M. Picosecond laser versus historical responses to Q-switched lasers for tattoo treatment. J. Cosmet. Laser Ther. 2020, 22, 210–214. [Google Scholar] [CrossRef]
- Bolookat, E.R.; Rich, L.J.; Paragh, G.; Colegio, O.R.; Singh, A.K.; Seshadri, M. Photoacoustic Imaging of Tattoo Inks: Phantom and Clinical Evaluation. Appl. Sci. 2020, 10, 1024. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Group | Description |
|---|---|
| Dark Tattoos | Qualified professionals tattooed the patient using mostly black-colored ink |
| Red Tattoos | Qualified professionals tattooed the patient using mostly red-colored ink |
| Mixed-Color Tattoos | Qualified professionals tattooed the patient using a variety of colors |
| Amateur | Unqualified professionals tattooed the patient |
| Medical | Usually blue superficial tattoos before radiotherapy |
| Traumatic | Caused by traumatic events |
| Cosmetic | Performed by professionals; Usually ferric oxide is present |
| Patient No. | 34 |
| Female (%) | 17 (50%) |
| Male (%) | 17 (50%) |
| Mean age ± SD [years] | 43.6 ± 11 |
| Age range [years] | 26–58 |
| Fitzpatrick phototype: | |
| II (%) | 10 (29.4%) |
| III (%) | 13 (38.2%) |
| IV (%) | 11 (32.4%) |
| Tattoo Type: 1 | |
| Professional (%), out of which: | 15 (44.1%) |
| Dark tattoos (%) | 7 (20.6%) |
| Red tattoos (%) | 6 (17.6%) |
| Mixed-color group (%) | 2 (5.9%) |
| Amateur (%) | 9 (26.5%) |
| Medical (%) | 2 (5.9%) |
| Traumatic (%) | 4 (11.8%) |
| Cosmetic (%) | 4 (11.8%) |
| Tattoo location: | |
| Face/head (%) | 8 (23.5%) |
| Upper trunk/shoulder (%) | 9 (26.5%) |
| Lower trunk/upper leg (%) | 8 (23.5%) |
| Lower arm/leg (%) | 8 (23.5%) |
| Wrist/hand/ankle/foot (%) | 1 (2.9%) |
| No. Patients (%) | Mean No. Sessions ± SD | No. Sessions Range | |
|---|---|---|---|
| Total | 34 (100%) | 3.3 ± 2.0 | 1–7 |
| Tattoo removal scores | |||
| 3 (60–80%) | 20 (58.8%) | 3.3 ± 1.9 | 1–6 |
| 4 (80–100%) | 14 (41.2%) | 3.3 ± 2.3 | 1–7 |
| Mean No. Sessions ± SD | No. Sessions Range | Tattoo Removal Score 3 (60–80%) [n; %] | Tattoo Removal Score 4 (80–100%) [n; %] | |
|---|---|---|---|---|
| Fitzpatrick phototype: | ||||
| II | 3.6 ± 2.0 | 1–6 | 7 (70%) | 3 (30%) |
| III | 3.0 ± 2.1 | 1–7 | 5 (38.5%) | 8 (61.5%) |
| IV | 3.4 ± 2.2 | 1–7 | 8 (72.7%) | 3 (27.3%) |
| Tattoo Type: | ||||
| Professional: | ||||
| Dark tattoos | 5.0 ± 0.8 | 4–6 | 5 (71.4%) | 2 (28.6%) |
| Red tattoos | 5.3 ± 0.8 | 4–6 | 4 (66.7%) | 2 (33.3%) |
| Mixed-color tattoos | 7.0 ± 0.0 | 7 | 0 (0%) | 2 (100%) |
| Amateur | 1.7 ± 0.5 | 1–2 | 6 (66.7%) | 3 (33.3%) |
| Medical | 1.5 ± 0.7 | 1–2 | 1 (50%) | 1 (50%) |
| Traumatic | 1.8 ± 0.5 | 1–2 | 2 (50%) | 2 (50%) |
| Cosmetic | 1.5 ± 0.6 | 1–2 | 2 (50%) | 2 (50%) |
| Tattoo location: | ||||
| Face/head | 1.6 ± 0.5 | 1–2 | 4 (50%) | 4 (50%) |
| Upper trunk/shoulder | 3.3 ± 1.7 | 1–6 | 6 (66.7%) | 3 (33.3%) |
| Lower trunk/upper leg | 4.9 ±1.9 | 2–7 | 5 (62.5%) | 3 (37.5%) |
| Lower arm/leg | 3.5 ± 2.5 | 1–7 | 4 (50%) | 4 (50%) |
| Wrist/hand/ankle/foot | 2 (n = 1) | 2 (n = 1) | 1 (100%) | 0 (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bennardo, L.; Cannarozzo, G.; Tamburi, F.; Patruno, C.; Provenzano, E.; Nisticò, S.P. Picosecond Q-Switched 1064/532 nm Laser in Tattoo Removal: Our Single Center Experience. Appl. Sci. 2021, 11, 9712. https://doi.org/10.3390/app11209712
Bennardo L, Cannarozzo G, Tamburi F, Patruno C, Provenzano E, Nisticò SP. Picosecond Q-Switched 1064/532 nm Laser in Tattoo Removal: Our Single Center Experience. Applied Sciences. 2021; 11(20):9712. https://doi.org/10.3390/app11209712
Chicago/Turabian StyleBennardo, Luigi, Giovanni Cannarozzo, Federica Tamburi, Cataldo Patruno, Eugenio Provenzano, and Steven Paul Nisticò. 2021. "Picosecond Q-Switched 1064/532 nm Laser in Tattoo Removal: Our Single Center Experience" Applied Sciences 11, no. 20: 9712. https://doi.org/10.3390/app11209712
APA StyleBennardo, L., Cannarozzo, G., Tamburi, F., Patruno, C., Provenzano, E., & Nisticò, S. P. (2021). Picosecond Q-Switched 1064/532 nm Laser in Tattoo Removal: Our Single Center Experience. Applied Sciences, 11(20), 9712. https://doi.org/10.3390/app11209712








