Abstract
Muscle architectural parameters play a crucial role in the rate of force development, strength, and sports performance. On the other hand, deteriorated muscle architectural parameters are associated with injuries, sarcopenia, mortality, falls, and fragility. With the development of technology, exergames have emerged as a complementary tool for physical therapy programs. The PRISMA 2020 statement was followed during the systematic review and meta-analysis. CENTRAL, CINAHL, PROQUEST, PubMed, and OpenGrey databases were searched last time on 22 September 2021. In total, five controlled trials were included in the systematic review. Twelve weeks of virtual dance exercise (Dance Central game for Xbox 360®) showed a medium effect on the improvement of hamstrings (g = 0.55, 95% CI (−0.03, 1.14), I2 = 0%) and the quadriceps femoris muscle cross-sectional area (g = 0.58, 95% CI (0.1, 1.00), I2 = 0%) in community-dwelling older women. Additionally, a four-week virtual balance-training program (the ProKin System) led to significant increments in the cross-sectional areas of individual paraspinal muscles (14.55–46.81%). However, previously investigated exergame programs did not show any medium or large effects on the architectural parameters of the medial gastrocnemius muscle in community-dwelling older women. Distinct exergame programs can be used as a complementary therapy for different prevention and rehabilitation programs.
1. Introduction
Muscle architecture is a comprehensive term comprising fascicle geometry (fascicle length and pennation angle) and muscle size (anatomical and physiological cross-sectional areas, muscle thickness, and muscle length) [1]. Larger muscle sizes are strongly associated with higher muscle strength [2,3,4,5,6,7,8,9,10,11,12]. Additionally, longer fascicle lengths and larger muscle sizes increase the rate of force development, power generation, and sprint and walking performances [10,13,14,15,16,17,18,19,20,21,22]. On the other hand, shorter fascicle lengths, smaller muscle sizes, and muscle size ratios are associated with sport and orthopaedic injuries of the lower extremity [23,24,25,26,27,28,29,30,31,32]. Furthermore, significant adverse alterations in the muscle size, fascicle length, and pennation angle occur due to ageing [33,34]. The decrements in muscle size and muscle functionality have been defined as sarcopenia [35,36], which is significantly associated with an increased risk of falling, and consequently mortality and morbidity in the elderly or people suffering from other health conditions [35,37,38,39,40]. Similarly, decrements in muscle size were also detected due to the disuse of muscles after bed rest [41,42] or exposure to microgravity [43]. These muscle atrophies might lead to reduced contractile performance and metabolic dysregulations [44]. Therefore, muscle architectural parameters should also be monitored during rehabilitation and prevention programs, such as the prevention of falls in the elderly or the prevention of hamstring injuries in athletes, etc.
Virtual games (exergames) have emerged as a complementary tool to enhance physical activity and exercise with the development of technology [45]. Due to its motivating and interactive features, it has been stated that exergames might increase commitment to exercise [46,47,48,49]. Exergames, which mimic cycling, dancing, running, walking, playing a sport modality, and resistance training, have become commercially available [50,51,52,53,54,55,56]. Nowadays, exergames have been used in various rehabilitation programs for cerebral palsy, Parkinson’s disease, stroke, obesity, or sarcopenia [57]. A review article pointed out that using exergames in physical therapy resulted in similar improvements as with conventional therapy in most cases [57].
Numerous systematic reviews have focused on the effects of exergames on several outcomes, including anxiety level [53], balance [58,59,60,61], cardiac rehabilitation [62,63], childhood obesity [64,65], cognition [66,67,68,69,70,71], depression [70,72,73], exercise behaviour [74], motor skills [75,76,77], muscle strength [54], musculoskeletal pain [78], physical activity [32,79,80,81], postural control [82,83], psychological effects [84], quality of life [85], respiratory conditions [78], social effects [86], and walking capacity [87].
Despite the crucial importance of the muscle architectural parameters, however, there is no systematic review investigating the effects of exergames on skeletal muscle architecture in the literature. Exploring the impacts of exergames on the architecture of skeletal muscles can be a reference point for future directions of the development of exergames and rehabilitation programs for people who need improvements in muscle architectural parameters, such as the elderly, injured people, and patients exposed to long-term bed rest. Therefore, this systematic review aimed to examine studies investigating exergames-induced architectural alterations in the skeletal muscle architecture in humans, and to find out the effect size of exergames on the stimulation of improvements in the architectural parameters of individual muscles in humans.
2. Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) 2020 statement [88] was used as the guideline of this review. The PRISMA 2020 checklist, which consists of a 27-item checklist and focuses on the introduction, methods, results, and discussion sections of a systematic review, is presented in the Supplementary Table S1. Before this review, a systematic review protocol was registered on INPLASY (INPLASY202140054) and is fully available online [89].
2.1. Information Sources
Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, ProQuest, PubMed, and OpenGrey databases were searched first on 10 April 2021 for all dates without applying a time limitation, and last on 22 September 2021. Additionally, reference lists of eligible studies were screened in order to avoid publication bias caused by grey literature as an addition to the OpenGrey database search. Database search histories are shown in the Supplementary Table S2.
2.2. Database Search Strategy, Eligibility Criteria, and Study Selection Process
Databases were searched by the first (N.S.) and second (G.Y.) authors, using a combination of the following key terms: (“Active video gaming” OR Avatar OR AVG OR “Commercial game” OR “Computer-based” OR “Computer based” OR “Computer feedback” OR “Computer game” OR “Dance dance revolution” OR “Digital game” OR “Digital-game” OR Exergam* OR “Game training” OR “Game exercise” OR “Game-based” OR “health game” OR IREX OR Kinect OR “Lower limb power rehabilitation” OR Nintendo OR “Play station” OR “Play-station” OR SensBalance OR “Serious game” OR “Serious gaming” OR “Sony EyeToy” OR “Video game” OR “Video-game” OR “Videogame” OR “Video gaming” OR “Video based” OR videobased OR “Video-based” OR “Virtual reality” OR VRT OR Wii OR Wobble OR Xavi* OR XBOX OR X-box) AND (“Muscle architecture” OR “Cross sectional area” OR “Cross-sectional area” OR Fascic* OR “Fiber length” OR “Fibre length” OR “Muscle length” OR “Muscle structure” OR “Muscle thickness” OR “Muscle volume” OR Pennat* OR Pinnat*).
The eligibility criteria included studies (1) investigating the effects of an exergame intervention; (2) presenting magnetic resonance imaging (MRI) or ultrasound measured alterations in one or more specifically defined muscle architectural parameter(s) as an outcome; (3) that were a full-text journal article; (4) written in the English language.
Duplicate records were removed by using the EndNote X9 computer program [90]. After the removal of duplicates, the remaining records were independently screened by the first (N.S.) and second authors (G.Y.) in a blinded status via Rayyan—a web and mobile app for systematic reviews [91]. Similarly, data extraction of the eligible studies was independently performed by the lead (N.S.) and second (G.Y.) authors. Disagreements about selecting the studies and extracting data were solved by discussion between the lead (N.S.) and second (G.Y.) authors, and the third author (T.Y.) was considered as referee in the case of unsolved disagreements. The first and second authors were blind to each other’s decisions during the whole screening process. In the case of the absence of full-text versions of the articles, the articles were obtained by contacting the Bangor University and Tokyo Metropolitan University libraries.
2.3. Outcome Measures
Exergames-induced changes in the architectural parameters of individually defined muscles, including the anatomical cross-sectional area, fascicle length, muscle thickness, pennation angle, and the physiological cross-sectional area, were the constituted outcome measures of this systematic review.
2.4. Quality Assessment of Eligible Studies
The Downs and Black checklist [92], which consisted of a 27-item checklist, was used for quality of assessment of both non-randomised and randomised trials. This systematic review used the following classifications for the quality of evidence: 26–28 = excellent, 20–25 = good, 15–19: fair, and ≤14 = poor quality, based on the previous systematic reviews [93,94]. The first (N.S.) and second authors (G.Y.) independently assessed the quality level of the eligible studies. Any conflicts that arose with regard to the assessment of quality was solved by a discussion between the first and second authors, and the third author (T.Y.) was considered the referee for the unsolved conflicts. In addition to the quality assessment of eligible studies, the risk of bias of included studies was independently assessed by the first and second authors via The Cochrane Collaboration’s tool for assessing the risk of bias in randomised trials [95]. Included studies were examined based on random sequence generation, allocation concealment, blinding participants and personnel, blinding outcome assessment, incomplete outcome data, selective reporting, and other bias. Each risk of bias assessment category ranked selected studies as having “low risk of bias”, “unclear risk of bias”, or “high risk of bias”. The risk of bias summary—review authors’ judgements about each risk of bias item for each included analysis, and the risk of bias graph—review authors’ conclusions about each risk of bias item presented as percentages across all included studies, were created via the RevMan 5.4.1 computer program [96].
2.5. Data Extraction
The extracted data included the following information: author, year, groups, number of participants, participant characteristics, type of exercises allocated to groups, materials used for exercise interventions, total weeks, sessions, sets, repetitions, measured muscle, measurement device and regions, type of the muscle architectural parameter, and results of the eligible studies.
2.6. Meta-Analysis
Quantitative analyses were completed using the Review Manager (RevMan 5.4.1) program [96]. For an exercise intervention group, a placebo or control group was considered a comparator. As summary statistics, Hedge’s (adjusted) g effect size (the standardised mean difference (SMD)) was estimated for each meta-analysis by using RevMan [96]. The difference between Hedge’s (adjusted) g and Cohen’s d is that Hedge’s (adjusted) g corrects a potential estimation bias when the sample size is smaller than 20 participants [97]. The effect sizes of the exergame interventions were interpreted as small (0.2), medium (0.5), or large (0.8), which were generally used for interpreting the Cohen’s d [98] and Hedges’ g [99] effect sizes [100].
For a case of a missing standard deviation (SD) from the baseline score, which is commonly seen in continuous data-carrying studies [101], the following formula was used for calculations [101,102]:
In this formula, SDchange represents the SD of the mean changes from the baseline, SDbaseline represents the SD of the pre-test, SDfinal corresponds to the SD of the post-test, and the r represents the correlations between the SDfinal and SDbaseline measurements.
In the meta-analyses, statistical heterogeneity was calculated via chi-squared (χ2, or Chi2) statistics, and the level of the statistical heterogeneity was assessed by I2 statistics, which defines the percentage ratio of the variability in effect calculations due to heterogeneity rather than chance [103]. The I2 values were classified as low (25%), moderate (50%), and high (75%) [104]. A more conservative random effect (RE) model, 95% confidence interval, continuous data, and inverse variance features of a meta-analysis were applied during the quantitative analyses [105]. The RE model was defined as a better tool that accounts for statistical and methodological heterogeneities by a recent meta-analytic study [106].
3. Results
3.1. Study Selection
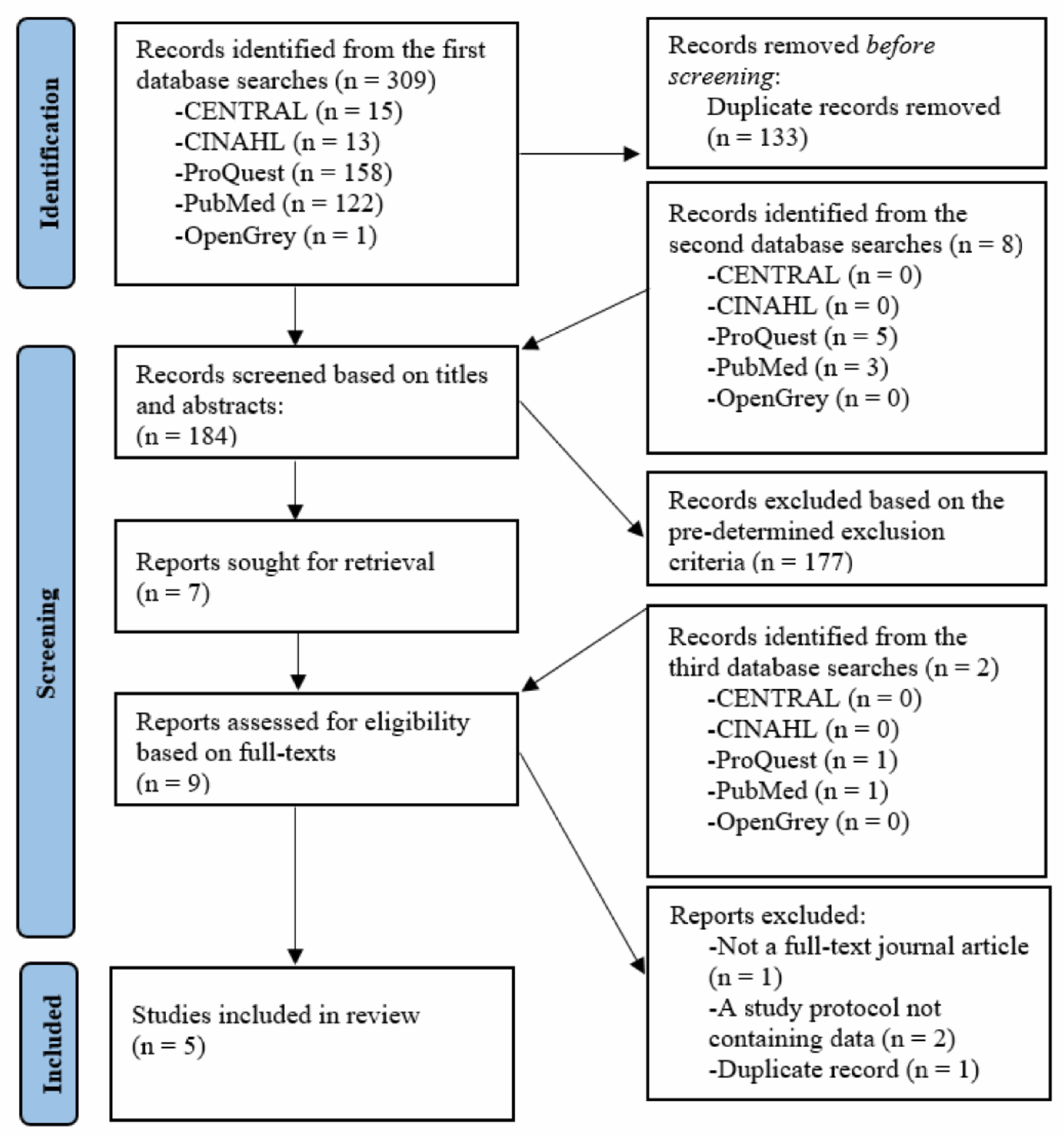
After the removal of duplicate records, a total of 184 records were independently screened based on titles and abstracts. One hundred seventy-seven records were excluded based on the exclusion criteria, and seven records were included based on the pre-determined eligibility criteria. The seven records and an additional two records, which were retrieved throughout the third database searches, were independently screened based on the full text. Eventually, five studies [107,108,109,110,111] were found eligible and included in this systematic review. The process of selecting eligible studies is presented in the PRISMA 2020 flow chart in Figure 1.
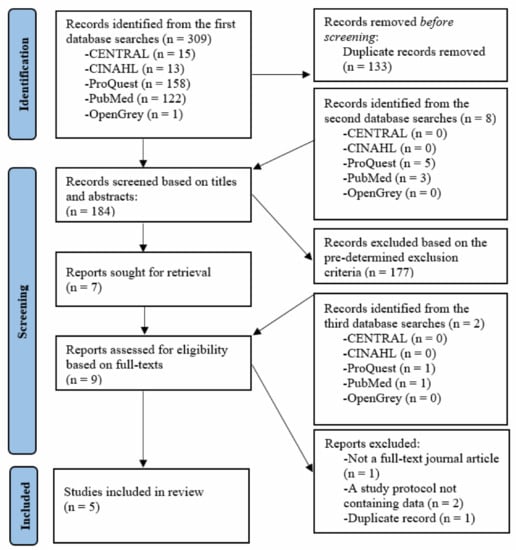
Figure 1.
PRISMA 2020 flow diagram.
3.2. Quality Assessment of Included Studies
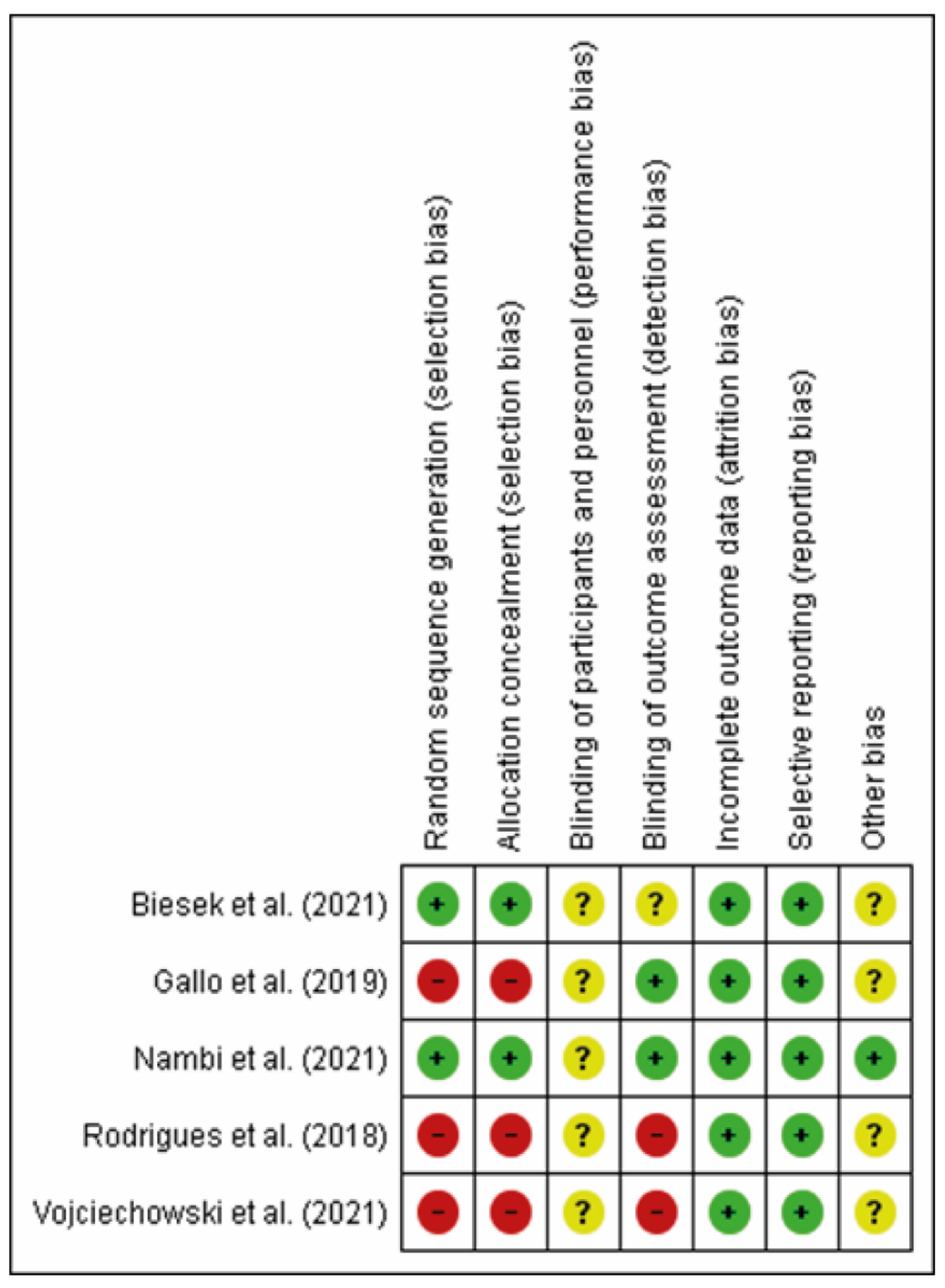
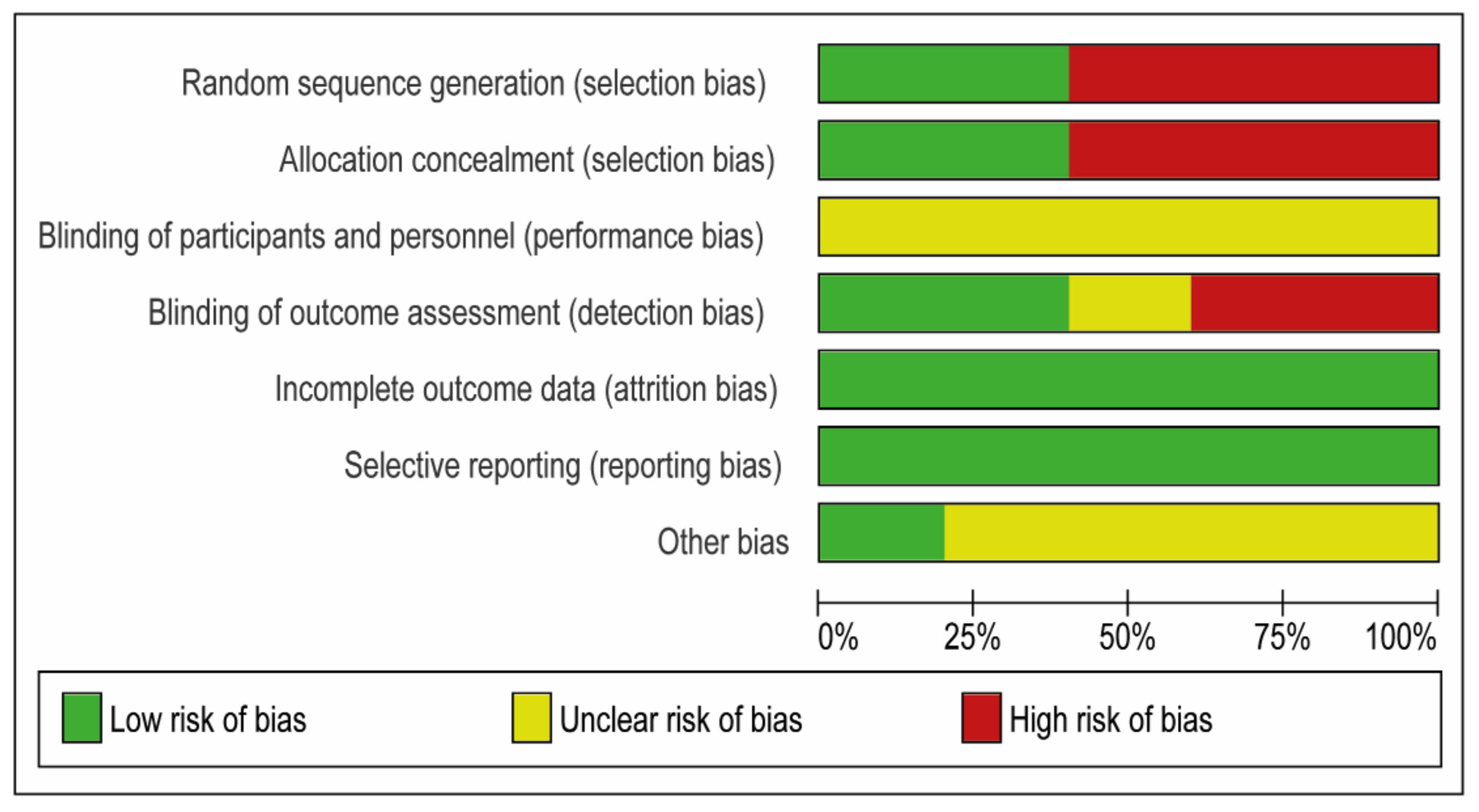
Once the first and second authors had independently assessed the evidence level of both randomised and non-randomised studies via the Downs and Black checklist [92], and the risk of bias of included studies by using The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials [95], any disagreements were solved by discussion between the first (N.S.) and second (G.Y.) authors, and the third author (T.Y.) was considered a referee in the case of unsolved disagreements. Consequently, the evidence levels of three studies were detected as having a “fair level” [108,110,111]. The evidence levels of the other studies were assigned the “good level” [107,109]. The quality assessments of each study are shown in detail in Table 1, a risk of bias summary—review authors’ judgements about each risk of bias item for each included study is presented in Figure 2, and a risk of bias graph—review authors’ judgements about each risk of bias item presented as percentages across all included studies is presented in Figure 3.

Table 1.
Quality assessment of eligible studies.
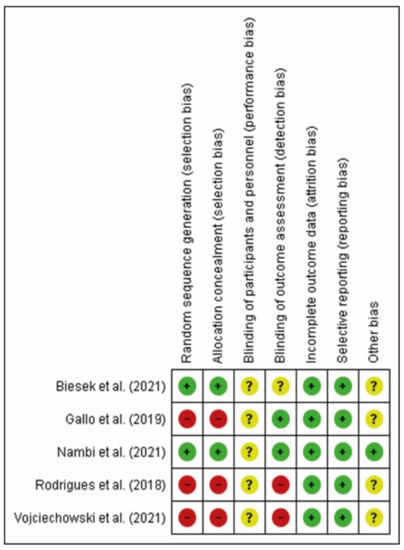
Figure 2.
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study (created via RevMan 5.4.1).
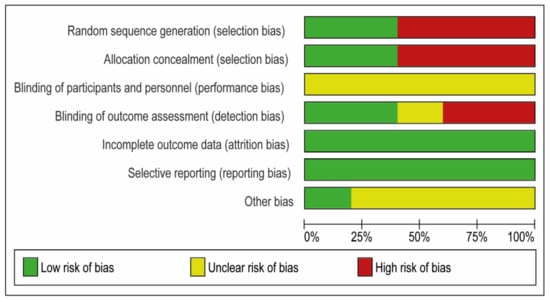
Figure 3.
Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
3.3. Characteristics of Included Studies
Participants’ age, population type, physical activity levels, and intervention and measurement characteristics of the included studies are illustrated in Table 2. Two studies [107,109] were classified as randomised controlled, and three studies [108,110,111] were classified as non-randomised controlled studies. Two studies [107,108] examined the effects of twelve-week exergame interventions on the medial gastrocnemius muscle architecture, while two studies [109,110] focused on the effects of twelve-week exergame interventions on the quadriceps femoris muscle cross-sectional area of community-dwelling older women. Additionally, one study [110] assessed the impacts of a twelve-week exergame training on the hamstring cross-sectional area of community-dwelling older women, and another study [109] measured the effects of four weeks of exergame intervention on the multifidus muscle thickness and the paraspinal muscle cross-sectional area in football players.

Table 2.
Characteristics of included studies.
3.4. Meta-Analyses
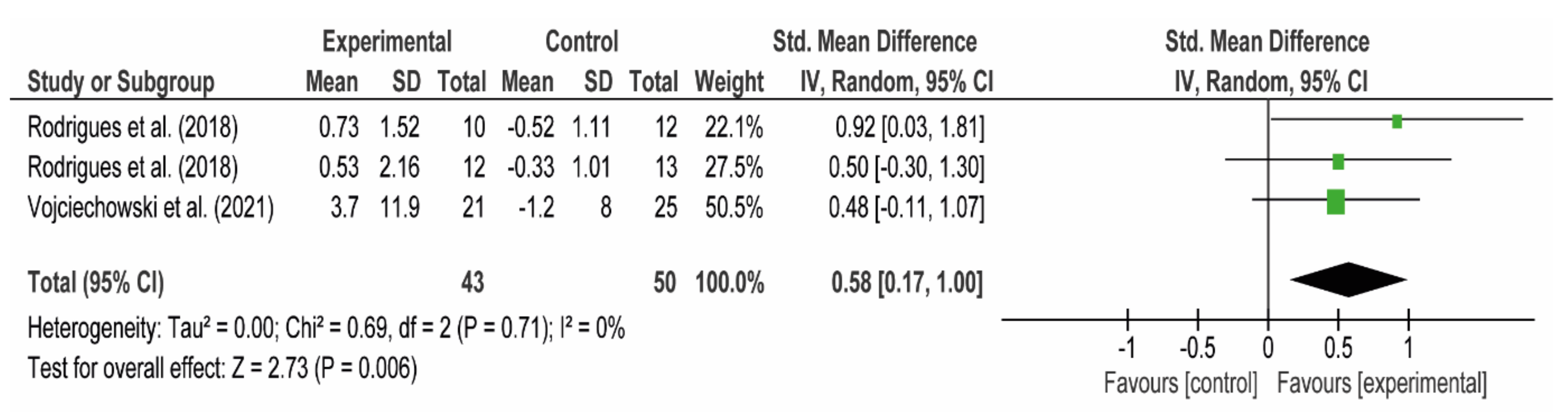
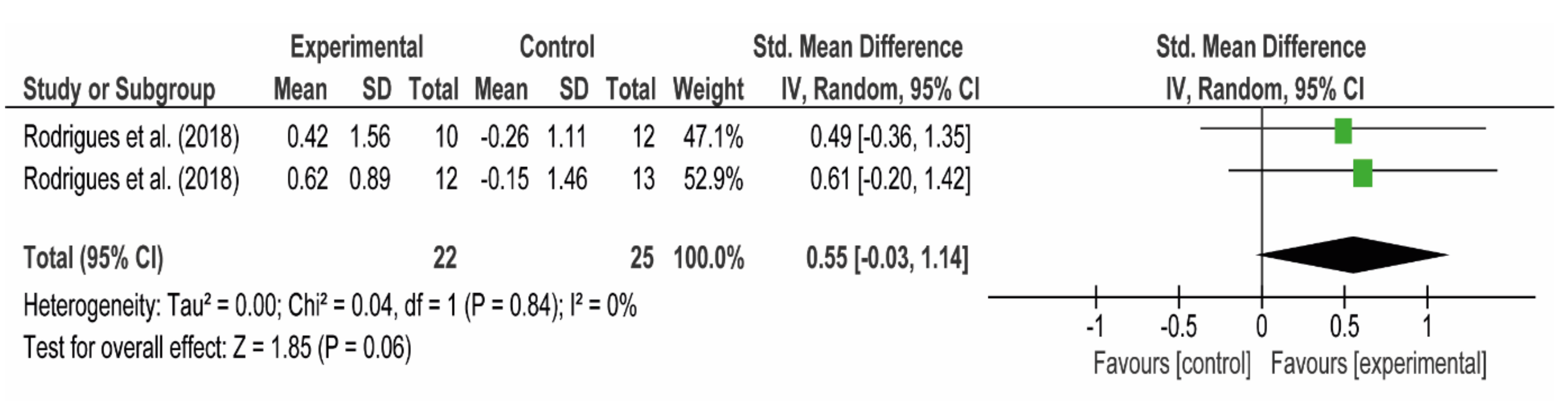
In total, four studies were included in the meta-analyses [107,108,110,111]. Firstly, two studies [110,111] were included in the meta-analysis assessing the effects of twelve-week virtual dance training (Dance Central game for Xbox 360® and Kinect) on the quadriceps femoris cross-sectional area in community-dwelling older women (Figure 4 ). Secondly, study subgroups of another study [110] were included in the meta-analysis measuring the effects of twelve-week virtual dance training (Dance Central game for Xbox 360® and Kinect) on the hamstrings cross-sectional area in community-dwelling older women (Figure 5). In both cases, twelve-week virtual dance training (Dance Central game for Xbox 360® and Kinect) showed a medium effect on the improvement of hamstrings (g = 0.55, 95% CI (−0.03, 1.14), I2 = 0%) and the quadriceps femoris (g = 0.58, 95% CI (0.17, 1.00), I2 = 0%) muscle cross-sectional areas without statistical heterogeneity in community-dwelling older women.
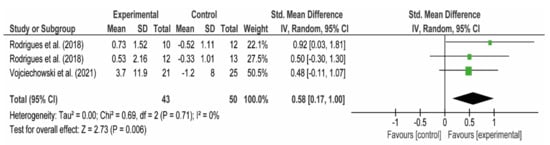
Figure 4.
The effects of twelve weeks exergames on the quadriceps femoris muscle cross-sectional area in community-dwelling older women. Note: The first line of Rodrigues et al. [110] represents fallers, and the second line represents non-fallers. This forest plot was created via RevMan [96].
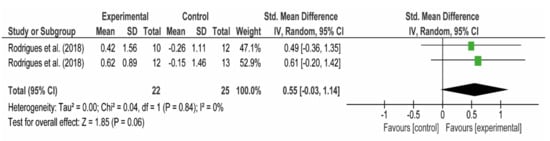
Figure 5.
The effects of twelve weeks of exergames on the hamstring muscle cross-sectional area of community-dwelling older women. Note: The first line of Rodrigues et al. [110] represents fallers, and the second line represents non-fallers. This forest plot was created via RevMan [96].
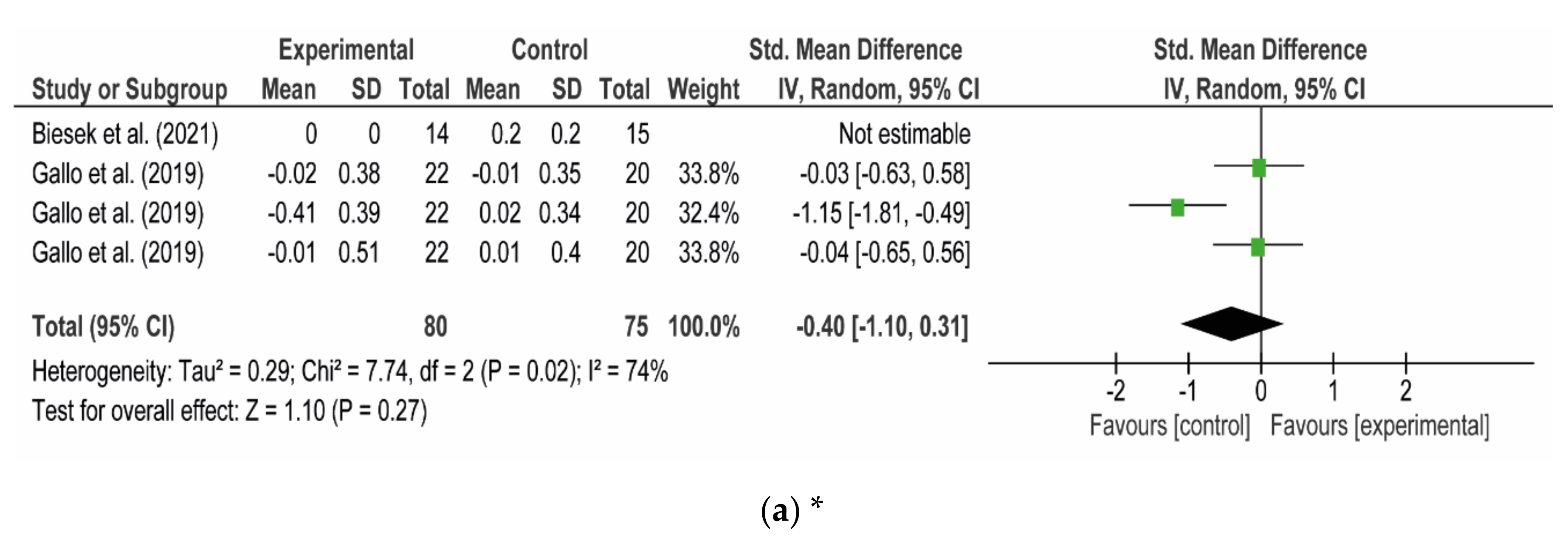
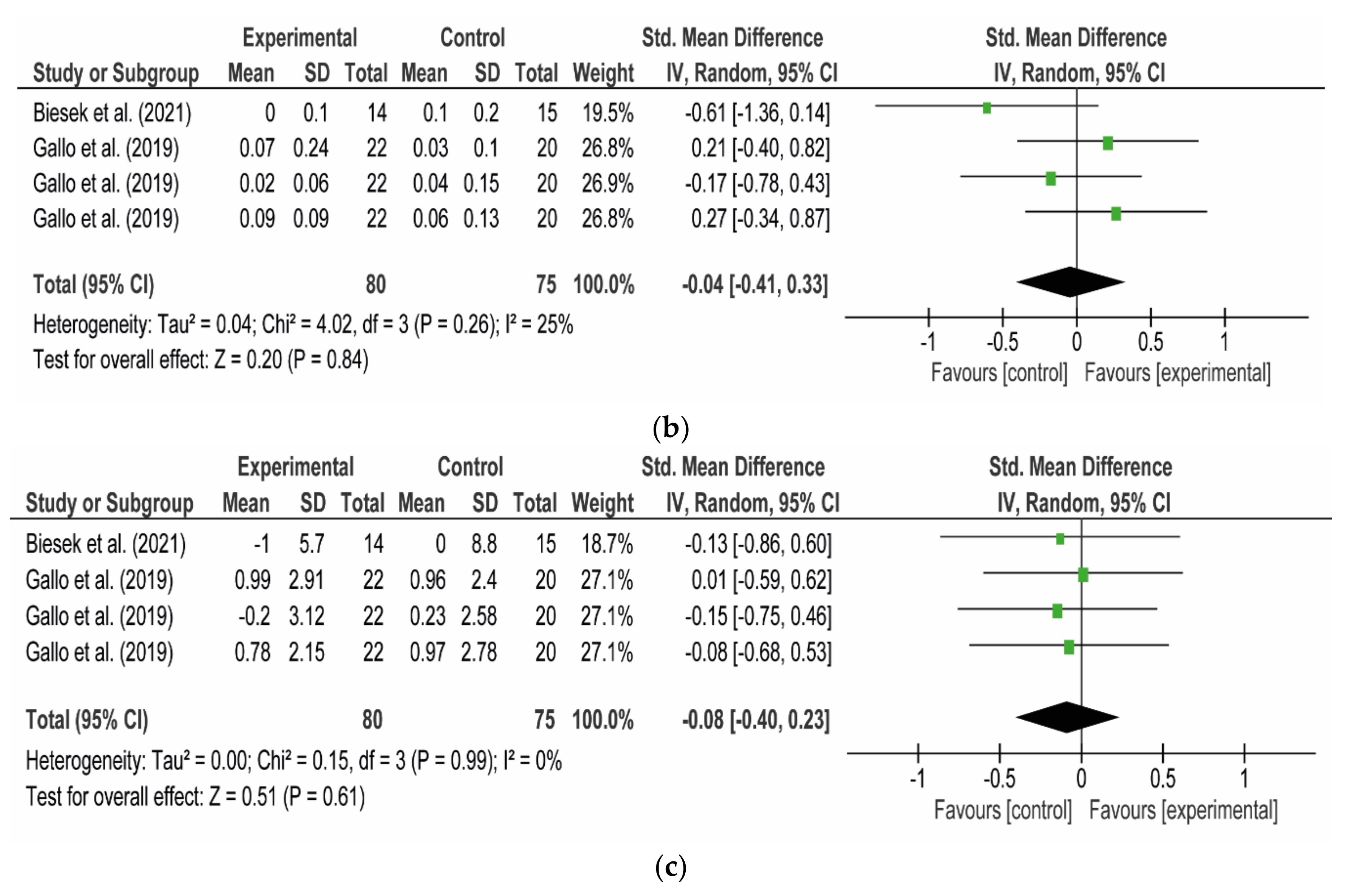
Thirdly, two studies [107,108] were included in meta-analyses assessing the impacts of twelve weeks of exergame interventions (Nintendo Wii Fit Plus® + balance platform [107] and Dance Central game for Xbox 360® + Kinect [108]) on the gastrocnemius muscle architectural parameters, including fascicle length, muscle thickness, and pennation angle, in community-dwelling older women. Individually or as combined in the meta-analyses, these exergames had no positive medium or large effects on increasing medial gastrocnemius fascicle length (g = −0.40, 95% CI (−1.10, 0,31), I2 = 74% (Figure 6a)), muscle thickness (g = −0.04, 95% CI (−0.41, 0.33), I2 = 25% (Figure 6b)), or pennation angle (g = −0.08, 95% CI (−0.40, 0.23), I2 = 0% (Figure 6c)).
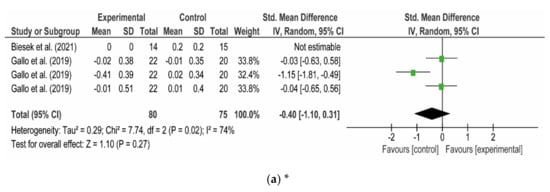
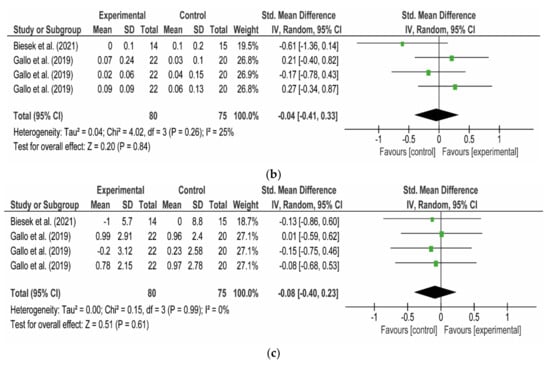
Figure 6.
The effects of twelve weeks of exergames on the medial gastrocnemius muscle architecture in community-dwelling older women: (a) fascicle length; (b) muscle thickness; (c) pennation angle. * In this meta-analysis, the given data in the study of Biesek et al. [107] was not calculable by RevMan [96]. Note: The first, second, and third Gallo et al. in each forest plot respectively represent the measurements taken from 20%, 30%, and 40% distances in the relevant study [108]. These forest plots were created via RevMan [96].
Lastly, one study [109] was not included in the meta-analyses due to the absence of other methodologically similar studies investigating the same topic. In this study, Nambi et al. [109] examined the effects of four-week virtual reality balance training (the ProKin system) on multifidus muscle thickness and paraspinal muscles, including multifidus again, cross-sectional area in university-level football players with chronic lower back pain.
As a result, Nambi and colleagues reported significant increments in the paraspinal muscle cross-sectional areas (psoas major: 25.58–26.19%, quadratus lumborum: 41.67–46.81%, multifidus: 44.23–43.40%, erector spinae: 14.55–14.63%) and 6.4–8.46% increments in multifidus muscle thickness (Supplementary Table S3).
4. Discussion
To the authors’ knowledge, this systematic review is the first systematic review focusing particularly on the effects of exergames on the architectural parameters of the skeletal muscles in humans. Based on studies identified to have a fair level of quality [110,111], 12 weeks of virtual dance exercises (Dance Central game for Xbox 360®) has a medium effect on increasing the quadriceps femoris muscle cross-sectional area. Likewise, 12 weeks of virtual dance exercises (Dance Central game for Xbox 360®) has a medium effect on increasing the quadriceps femoris muscle cross-sectional area based on a study with fair-level quality [110]. Additionally, a good-quality study [109] pointed out that four weeks of virtual balance training (via using the ProKin system) was significantly more effective than home-based balance training with the Swiss ball and conventional balance training in increasing paraspinal muscle size at the L3–L4 level and multifidus muscle size at the L4–L5 level in football players with chronic lower back pain. More specifically, the four weeks of virtual balance training [109] led to 14.55–46.81% increments in the paraspinal muscle cross-sectional areas (psoas major: 25.58–26.19%, quadratus lumborum: 41.67–46.81%, multifidus: 44.23–43.40%, erector spinae: 14.55-14.63%) and 6.4–8.46% increments in multifidus muscle thickness (Supplementary Table S3). On the other hand, meta-analyses measuring the impacts of twelve weeks of exergame interventions (Nintendo Wii Fit Plus® + balance platform [107] and Dance Central game for Xbox 360® + Kinect [108]) on gastrocnemius muscle architectural parameters, including fascicle length, muscle thickness, and pennation angle, in community-dwelling older women could not detect any positive medium or large effects of these exergames on the medial gastrocnemius muscle architectural parameters based on the fair–good-level studies [107,108].
From the perspective of the effects of 12 weeks of virtual dance exercises (Dance Central game for Xbox 360®), medium effects on the increase in muscle size of the quadriceps femoris and hamstrings of community-dwelling older women were detected by the meta-analyses of this study. Moreover, the effect size of 12 weeks of virtual dance exercises on quadricep muscle size increments in community-dwelling older and faller women was large (g = 0.92) (Figure 4). When considering older people, falling is one of the major reasons for mortality, loss of independence, or severe health problems [112,113,114]. Thirty per cent of community-dwelling people 65 years old or older fall every year [115,116]. Small muscle size was defined as an indicator of a higher risk of falls in community-dwelling older people [39,40,117,118]. Therefore, 12 weeks of virtual dance exercises (Dance Central game for Xbox 360®) can be used as a complementary therapy in fall prevention programs for the elderly due to its medium to large effects on increasing cross-sectional areas of the hamstrings and quadriceps femoris.
Additionally, Nambi and colleagues [109] found significantly favourable increments in the paraspinal and multifidus muscle sizes from the virtual balance training as compared to combined physical rehabilitation, which included balance exercises using a Swiss Ball, or conventional balance training. Previously, balance training with a Swiss Ball was considered the golden standard for balance training and enhancing the strength of core muscles [119]. However, four weeks of virtual reality balance training using the ProKin system led to percentage increments approximately two times higher in the cross-sectional areas of the individual paraspinal muscles (erector spinae, multifidus, psoas major, and quadratus lumborum) than four weeks of combined physical therapy, which included a Swiss Ball balance training (Supplementary Table S3). Hence, virtual reality balance training might be used as an alternative tool to improve the sizes of the paraspinal muscles. More studies may wish to confirm the effects of virtual reality balance training on core muscles. Furthermore, lower back pain is prevalent in many sports [120] and might reduce the size of core muscles, including multifidus and psoas major [121]. Decreased multifidus muscle size has previously been found to be associated with lower extremity injuries in sports [23,24,25,26,27]. Therefore, a future randomised controlled trial can examine the effects of virtual balance training on the multifidus muscle size in athletes without lower back pain.
Despite the comprehensive database searches, the main limitation of this systematic review is its use of only five eligible studies. Having more eligible studies might have allowed this systematic review to have more precise conclusions about more skeletal muscles. However, to the authors’ knowledge, this systematic review retrieved all the relevant studies. Additionally, all the eligible studies were published in the last three years. This fact could indicate that the quantity of studies investigating the effects of exergames on muscle architecture might increase in the future. Therefore, this systematic review might be updated in the future in order to explore the effects of exergames on the architecture of other muscles. An additional limitation of this study is the lack of publication bias assessments or meta-regression analyses since there were less than ten studies used. The Cochrane Handbook for Systematic Review of Interventions clearly states that there should be at least ten studies in a meta-analysis for detecting publication bias in funnel plots or meta-regression analyses [122]. Thus, differences in the training interventions and populations are considered to be other confounding factors in the meta-analysis. Future studies might be conducted on the effects of exergames on other muscle architectures in order to obtain an overall idea of the effectiveness of exergames in improving the architectural parameters of human skeletal muscles.
5. Conclusions
Twelve weeks of virtual dance exercise (Dance Central game for Xbox 360®) showed a medium effect on improving the hamstrings and the quadriceps femoris muscle cross-sectional area of community-dwelling older women. Additionally, a four-week virtual balance training program (the ProKin System) led to significant increments in the size of paraspinal muscles. However, one twelve-week virtual dance exercise program (Dance Central game for Xbox 360®) [108] or another twelve-week exergame training program (Nintendo Wii Fit Plus® + balance platform) [107] did not show any medium or large effects on the increase of the medial gastrocnemius muscle architectural parameters in community-dwelling older women. These results should be interpreted cautiously due to the small number of eligible studies.
In conclusion, twelve weeks of virtual dance exercise (Dance Central game for Xbox 360®) might be used as a complementary therapy in fall and fragility prevention programs for community-dwelling older women due to its positive effects on increasing hamstrings and quadricep femoris muscle sizes. Additionally, a four-week virtual balance training program (the ProKin System) can be included in rehabilitation programs for chronic lower back pain in university-level football players to increase the paraspinal muscle cross-sectional area in football players with chronic lower back pain. Moreover, the exergames which showed positive effects on increasing muscle sizes, e.g., the virtual dance game and the virtual balance training, can also be used as complementary therapies for home-based rehabilitation programs. Consequently, more studies are needed to have an overall idea of the effects of exergames on muscle architectural parameters in humans.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/app112110325/s1, Table S1: The PRISMA 2020 Statement Checklist, Table S2: Database Search Histories, Table S3: Training-induced percentage changes in muscle architectural parameters in the study of Nambi and colleagues.
Author Contributions
N.S. was involved in designing the review, independently screened the citations obtained through database searches, independently performed the quality assessment of the eligible studies, independently extracted data from eligible studies, and contributed to the writing process of the manuscript. G.Y. was involved in designing the review, performed the database searches, independently screened the citations obtained through database searches, independently performed the quality assessment of eligible studies, independently extracted data from eligible studies, and contributed to the writing process of the manuscript. T.Y. was involved in designing the review, acted as a referee in the case of an unsolved discussion. Conceptualization, N.S., G.Y., and T.Y.; methodology, N.S., G.Y., and T.Y.; software, N.S. and G.Y.; formal analysis, N.S. and G.Y.; formal analysis, N.S. and G.Y.; investigation, N.S. and G.Y.; resources, N.S. and G.Y.; data curation, N.S. and G.Y.; writing—original draft preparation, N.S. and G.Y.; writing—review and editing, N.S. and G.Y.; visualization, N.S. and G.Y.; supervision, T.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This systematic review did not receive any particular funding. The second author, Gokhan Yagiz, is sponsored for his postgraduate studies by the Republic of Turkey, Ministry of National Education: YLSY-40409183010. However, the funder did not play any role in any process of preparing or writing this manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The relevant data used in the systematic review were contained in the tables and figures in the main text and Supplementary Materials.
Conflicts of Interest
Nami Shida, Gokhan Yagiz, and Takumi Yamada declare that they have no conflict of interest in the content of this systematic review. The second author, Gokhan Yagiz, is sponsored for his postgraduate studies by the Republic of Turkey, Ministry of National Education: YLSY-4040918310. However, the funder did not play any role in any process of preparing or writing this manuscript.
References
- Blazevich, A. Effects of Physical Training and Detraining, Immobilisation, Growth and Aging on Human Fascicle Geometry. Sports Med. 2006, 36, 1003–1017. [Google Scholar] [CrossRef] [PubMed]
- Abe, T.; Kojima, K.; Stager, J.M. Skeletal muscle mass and muscular function in master swimmers is related to training distance. Rejuvenation Res. 2014, 17, 415–421. [Google Scholar] [CrossRef]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S. Morphological and functional relationships with ultrasound measured muscle thickness of the lower extremity: A brief review. Ultrasound 2015, 23, 166–173. [Google Scholar] [CrossRef]
- Akima, H.; Kano, Y.; Enomoto, Y.; Ishizu, M.; Okada, M.; Oishi, Y.; Katsuta, S.; Kuno, S. Muscle function in 164 men and women aged 20–84 yr. Med. Sci. Sports Exerc. 2001, 33, 220–226. [Google Scholar] [CrossRef]
- Freilich, R.J.; Kirsner, R.L.; Byrne, E. Isometric strength and thickness relationships in human quadriceps muscle. Neuromuscul. Disord. 1995, 5, 415–422. [Google Scholar] [CrossRef]
- Fukunaga, T.; Roy, R.R.; Shellock, F.G.; Hodgson, J.A.; Edgerton, V.R. Specific tension of human plantar flexors and dorsiflexors. J. Appl. Physiol. 1996, 80, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Ikai, M.; Fukunaga, T. Calculation of muscle strength per unit cross-sectional area of human muscle by means of ultrasonic measurement. Int. Z. Angew. Physiol. Einschl. Arb. 1968, 26, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Lieber, R.L. Skeletal Muscle Structure and Function; Williams and Wilkins: Baltimore, Maryland, USA, 1992. [Google Scholar]
- Maughan, R.J.; Watson, J.S.; Weir, J. Strength and cross-sectional area of human skeletal muscle. J. Physiol. 1983, 338, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Moreau, N.G.; Simpson, K.N.; Teefey, S.A.; Damiano, D.L. Muscle architecture predicts maximum strength and is related to activity levels in cerebral palsy. Phys. Ther. 2010, 90, 1619–1630. [Google Scholar] [CrossRef] [PubMed]
- Narici, M.V.; Landoni, L.; Minetti, A.E. Assessment of human knee extensor muscles stress from in vivo physiological cross-sectional area and strength measurements. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 65, 438–444. [Google Scholar] [CrossRef]
- Shephard, R.J.; Bouhlel, E.; Vandewalle, H.; Monod, H. Muscle mass as a factor limiting physical work. J. Appl. Physiol. 1988, 64, 1472–1479. [Google Scholar] [CrossRef]
- Abe, T.; Fukashiro, S.; Harada, Y.; Kawamoto, K. Relationship between sprint performance and muscle fascicle length in female sprinters. J. Physiol. Anthropol. Appl. Hum. Sci. 2001, 20, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Brechue, W.F.; Abe, T. The role of FFM accumulation and skeletal muscle architecture in powerlifting performance. Eur. J. Appl. Physiol. 2002, 86, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Ikebukuro, T.; Kubo, K.; Okada, J.; Yata, H.; Tsunoda, N. The relationship between muscle thickness in the lower limbs and competition performance in weightlifters and sprinters. Jpn. J. Phys. Fit. Sports Med. 2011, 60, 401–411. [Google Scholar] [CrossRef]
- Kumagai, K.; Abe, T.; Brechue, W.; Ryushi, T.; Takano, S.; Mizuno, M. Sprint performance is related to muscle fascicle length in male 100-m sprinters. J. Appl. Physiol. 2000, 88, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Mangine, G.T.; Fukuda, D.H.; LaMonica, M.B.; Gonzalez, A.M.; Wells, A.J.; Townsend, J.R.; Jajtner, A.R.; Fragala, M.S.; Stout, J.R.; Hoffman, J.R. Influence of gender and muscle architecture asymmetry on jump and sprint performance. J. Sports Sci. Med. 2014, 13, 904–911. [Google Scholar] [PubMed]
- Mangine, G.T.; Fukuda, D.H.; Townsend, J.R.; Wells, A.J.; Gonzalez, A.M.; Jajtner, A.R.; Bohner, J.D.; LaMonica, M.; Hoffman, J.R.; Fragala, M.S.; et al. Sprinting performance on the Woodway Curve 3.0TM is related to muscle architecture. Eur. J. Sport Sci. 2015, 15, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Nasirzade, A.; Ehsanbakhsh, A.; Argavani, H.; Sobhkhiz, A.; Aliakbari, M. Selected anthropometrical, muscular architecture, and biomechanical variables as predictors of 50-m performance of front crawl swimming in young male swimmers. Sci. Sports 2014, 29, e75–e81. [Google Scholar] [CrossRef]
- Nasirzade, A.; Ehsanbakhsh, A.; Ilbeygi, S.; Sobhkhiz, A.; Argavani, H.; Aliakbari, M. Relationship between sprint performance of front crawl swimming and muscle fascicle length in young swimmers. J. Sports Sci. Med. 2014, 13, 550–556. [Google Scholar]
- Nimphius, S.; McGuigan, M.R.; Newton, R.U. Changes in muscle architecture and performance during a competitive season in female softball players. J. Strength Cond. Res. 2012, 26, 2655–2666. [Google Scholar] [CrossRef]
- Zaras, N.D.; Stasinaki, A.N.; Methenitis, S.K.; Krase, A.A.; Karampatsos, G.P.; Georgiadis, G.V.; Spengos, K.M.; Terzis, G.D. Rate of Force Development, Muscle Architecture, and Performance in Young Competitive Track and Field Throwers. J. Strength Cond. Res. 2016, 30, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Hides, J.; Frazer, C.; Blanch, P.; Grantham, B.; Sexton, C.; Mendis, M.D. Clinical utility of measuring the size of the lumbar multifidus and quadratus lumborum muscles in the Australian football league setting: A prospective cohort study. Phys. Ther. Sport 2020, 46, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Hides, J.A.; Brown, C.T.; Penfold, L.; Stanton, W.R. Screening the lumbopelvic muscles for a relationship to injury of the quadriceps, hamstrings, and adductor muscles among elite Australian Football League players. J. Orthop. Sports Phys. Ther. 2011, 41, 767–775. [Google Scholar] [CrossRef]
- Hides, J.A.; Stanton, W.R. Can motor control training lower the risk of injury for professional football players? Med. Sci. Sports Exerc. 2014, 46, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Hides, J.A.; Stanton, W.R. Predicting football injuries using size and ratio of the multifidus and quadratus lumborum muscles. Scand. J. Med. Sci. Sports 2017, 27, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Hides, J.A.; Stanton, W.R.; Mendis, M.D.; Franettovich Smith, M.M.; Sexton, M.J. Small Multifidus Muscle Size Predicts Football Injuries. Orthop. J. Sports Med. 2014, 2, 2325967114537588. [Google Scholar] [CrossRef]
- Jeon, J.Y.; Kang, H.W.; Kim, D.Y.; Kim, Y.T.; Lee, D.Y.; Lee, D.-O. Relationship between calf muscle cross-sectional area and ankle fracture. Foot Ankle Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lindström, M.; Strandberg, S.; Wredmark, T.; Felländer-Tsai, L.; Henriksson, M. Functional and muscle morphometric effects of ACL reconstruction. A prospective CT study with 1 year follow-up. Scand. J. Med. Sci. Sports 2013, 23, 431–442. [Google Scholar] [CrossRef]
- Mangine, G.T.; Hoffman, J.R.; Gonzalez, A.M.; Jajtner, A.R.; Scanlon, T.; Rogowski, J.P.; Wells, A.J.; Fragala, M.S.; Stout, J.R. Bilateral differences in muscle architecture and increased rate of injury in national basketball association players. J. Athl. Train. 2014, 49, 794–799. [Google Scholar] [CrossRef] [PubMed]
- Timmins, R.G.; Bourne, M.N.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): A prospective cohort study. Br. J. Sports Med. 2016, 50, 1524–1535. [Google Scholar] [CrossRef] [PubMed]
- Wieschhoff, G.G.; Mandell, J.C.; Czuczman, G.J.; Nikac, V.; Shah, N.; Smith, S.E. Acute non-contact anterior cruciate ligament tears are associated with relatively increased vastus medialis to semimembranosus cross-sectional area ratio: A case-control retrospective MR study. Skelet. Radiol. 2017, 46, 1469–1475. [Google Scholar] [CrossRef]
- Doherty, T.J. Invited review: Aging and sarcopenia. J. Appl. Physiol. 2003, 95, 1717–1727. [Google Scholar] [CrossRef]
- Narici, M.V.; Maganaris, C.N.; Reeves, N.D.; Capodaglio, P. Effect of aging on human muscle architecture. J. Appl. Physiol. 2003, 95, 2229–2234. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M. Sarcopenia: European consensus on definition and diagnosisReport of the European Working Group on Sarcopenia in Older PeopleA. J. Cruz-Gentoft et al. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Kulmala, J.-P.; Korhonen, M.T.; Kuitunen, S.; Suominen, H.; Heinonen, A.; Mikkola, A.; Avela, J. Which muscles compromise human locomotor performance with age? J. R. Soc. Interface 2014, 11, 20140858. [Google Scholar] [CrossRef] [PubMed]
- Arango-Lopera, V.E.; Arroyo, P.; Gutiérrez-Robledo, L.M.; Perez-Zepeda, M.U.; Cesari, M. Mortality as an adverse outcome of sarcopenia. J. Nutr. Health Aging 2013, 17, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Englesbe, M.J.; Patel, S.P.; He, K.; Lynch, R.J.; Schaubel, D.E.; Harbaugh, C.; Holcombe, S.A.; Wang, S.C.; Segev, D.L.; Sonnenday, C.J. Sarcopenia and Mortality after Liver Transplantation. J. Am. Coll. Surg. 2010, 211, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Cruz-Jentoft, A.J.; Liperoti, R.; Russo, A.; Giovannini, S.; Tosato, M.; Capoluongo, E.; Bernabei, R.; Onder, G. Sarcopenia and mortality risk in frail older persons aged 80 years and older: Results from ilSIRENTE study. Age Ageing 2013, 42, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Van Ancum, J.M.; Pijnappels, M.; Jonkman, N.H.; Scheerman, K.; Verlaan, S.; Meskers, C.G.M.; Maier, A.B. Muscle mass and muscle strength are associated with pre- and post-hospitalization falls in older male inpatients: A longitudinal cohort study. BMC Geriatr. 2018, 18, 116. [Google Scholar] [CrossRef] [PubMed]
- Šimunič, B.; Koren, K.; Rittweger, J.; Lazzer, S.; Reggiani, C.; Rejc, E.; Pišot, R.; Narici, M.; Degens, H. Tensiomyography detects early hallmarks of bed-rest-induced atrophy before changes in muscle architecture. J. Appl. Physiol. 2019, 126, 815–822. [Google Scholar] [CrossRef]
- Wall, B.T.; Dirks, M.L.; Snijders, T.; Senden, J.M.G.; Dolmans, J.; van Loon, L.J.C. Substantial skeletal muscle loss occurs during only 5 days of disuse. Acta Physiol. 2014, 210, 600–611. [Google Scholar] [CrossRef]
- Winnard, A.; Scott, J.; Waters, N.; Vance, M.; Caplan, N. Effect of Time on Human Muscle Outcomes during Simulated Microgravity Exposure without Countermeasures—Systematic Review. Front. Physiol. 2019, 10, 1046. [Google Scholar] [CrossRef]
- Narici, M.V.; de Boer, M.D. Disuse of the musculo-skeletal system in space and on earth. Eur. J. Appl. Physiol. 2011, 111, 403–420. [Google Scholar] [CrossRef]
- Van Diest, M.; Lamoth, C.J.; Stegenga, J.; Verkerke, G.J.; Postema, K. Exergaming for balance training of elderly: State of the art and future developments. J. Neuroeng. Rehabil. 2013, 10, 101. [Google Scholar] [CrossRef]
- Fung, V.; So, K.; Park, E.; Ho, A.; Shaffer, J.; Chan, E.; Gomez, M. The utility of a video game system in rehabilitation of burn and nonburn patients: A survey among occupational therapy and physiotherapy practitioners. J. Burn Care Res. 2010, 31, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, M.G.; Laessoe, U.; Hendriksen, C.; Nielsen, O.B.F.; Aagaard, P. Efficacy of Nintendo Wii training on mechanical leg muscle function and postural balance in community-dwelling older adults: A randomized controlled trial. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2013, 68, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Studenski, S.; Perera, S.; Hile, E.; Keller, V.; Spadola-Bogard, J.; Garcia, J. Interactive video dance games for healthy older adults. J. Nutr. Health Aging 2010, 14, 850–852. [Google Scholar] [CrossRef] [PubMed]
- Taylor, L.M.; Kerse, N.; Frakking, T.; Maddison, R. Active video games for improving physical performance measures in older people: A meta-analysis. J. Geriatr. Phys. Ther. 2018, 41, 108. [Google Scholar] [CrossRef]
- Graves, L.E.; Ridgers, N.D.; Williams, K.; Stratton, G.; Atkinson, G.; Cable, N.T. The physiological cost and enjoyment of Wii Fit in adolescents, young adults, and older adults. J. Phys. Act. Health 2010, 7, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Morais, N.S.; Viana, R.B.; Silva, W.F.; Santos, D.A.; Costa, T.G.; Campos, M.H.; Vieira, C.A.; Vancini, R.L.; Andrade, M.S.; Gentil, P.; et al. Effect of both dance exergame and a traditional exercise on state anxiety and enjoyment in women. J. Sports Med. Phys. Fit. 2021. [Google Scholar] [CrossRef]
- Viana, R.B.; Alves, C.L.; Vieira, C.A.; Vancini, R.L.; Campos, M.H.; Gentil, P.; Andrade, M.S.; de Lira, C.A.B. Anxiolytic Effects of a Single Session of the Exergame Zumba® Fitness on Healthy Young Women. Games Health J. 2017, 6, 365–370. [Google Scholar] [CrossRef]
- Viana, R.B.; Dankel, S.J.; Loenneke, J.P.; Gentil, P.; Vieira, C.A.; Andrade, M.D.S.; Vancini, R.L.; de Lira, C.A.B. The effects of exergames on anxiety levels: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 1100–1116. [Google Scholar] [CrossRef]
- Viana, R.B.; de Oliveira, V.N.; Dankel, S.J.; Loenneke, J.P.; Abe, T.; da Silva, W.F.; Morais, N.S.; Vancini, R.L.; Andrade, M.S.; de Lira, C.A.B. The effects of exergames on muscle strength: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2021. [Google Scholar] [CrossRef] [PubMed]
- Viana, R.B.; Vancini, R.L.; Vieira, C.A.; Gentil, P.; Campos, M.H.; Andrade, M.S.; de Lira, C.A.B. Profiling exercise intensity during the exergame Hollywood Workout on XBOX 360 Kinect®. PeerJ 2018, 6, e5574. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.T.; Wu, W.L.; Chu, I.H. Energy Expenditure and Intensity in Healthy Young Adults during Exergaming. Am. J. Health Behav. 2015, 39, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Bonnechère, B.; Jansen, B.; Omelina, L.; Van Sint Jan, S. The use of commercial video games in rehabilitation: A systematic review. Int. J. Rehabil. Res. 2016, 39, 277–290. [Google Scholar] [CrossRef]
- Fang, Q.; Ghanouni, P.; Anderson, S.E.; Touchett, H.; Shirley, R.; Fang, F.; Fang, C. Effects of Exergaming on Balance of Healthy Older Adults: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Games Health J. 2020, 9, 11–23. [Google Scholar] [CrossRef]
- Harris, D.M.; Rantalainen, T.; Muthalib, M.; Johnson, L.; Teo, W.P. Exergaming as a Viable Therapeutic Tool to Improve Static and Dynamic Balance among Older Adults and People with Idiopathic Parkinson’s Disease: A Systematic Review and Meta-Analysis. Front. Aging Neurosci. 2015, 7, 167. [Google Scholar] [CrossRef]
- Laufer, Y.; Dar, G.; Kodesh, E. Does a Wii-based exercise program enhance balance control of independently functioning older adults? A systematic review. Clin. Interv. Aging 2014, 9, 1803–1813. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, T.B.F.; de Medeiros, C.S.P.; de Oliveira, V.H.B.; Vieira, E.R.; de Cavalcanti, F.A.C. Effectiveness of exergames for improving mobility and balance in older adults: A systematic review and meta-analysis. Syst. Rev. 2020, 9, 163. [Google Scholar] [CrossRef]
- García-Bravo, S.; Cuesta-Gómez, A.; Campuzano-Ruiz, R.; López-Navas, M.J.; Domínguez-Paniagua, J.; Araújo-Narváez, A.; Barreñada-Copete, E.; García-Bravo, C.; Flórez-García, M.T.; Botas-Rodríguez, J.; et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review. Disabil. Rehabil. 2021, 43, 448–457. [Google Scholar] [CrossRef]
- Ruivo, J.A. Exergames and cardiac rehabilitation: A review. J. Cardiopulm. Rehabil. Prev. 2014, 34, 2–20. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Chen, S. Are field-based exergames useful in preventing childhood obesity? A systematic review. Obes. Rev. 2014, 15, 676–691. [Google Scholar] [CrossRef] [PubMed]
- Lamboglia, C.M.; da Silva, V.T.; de Vasconcelos Filho, J.E.; Pinheiro, M.H.; Munguba, M.C.; Silva Júnior, F.V.; de Paula, F.A.; da Silva, C.A. Exergaming as a strategic tool in the fight against childhood obesity: A systematic review. J. Obes. 2013, 2013, 438364. [Google Scholar] [CrossRef][Green Version]
- Fang, Q.; Aiken, C.A.; Fang, C.; Pan, Z. Effects of Exergaming on Physical and Cognitive Functions in Individuals with Autism Spectrum Disorder: A Systematic Review. Games Health J. 2019, 8, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Mura, G.; Carta, M.G.; Sancassiani, F.; Machado, S.; Prosperini, L. Active exergames to improve cognitive functioning in neurological disabilities: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2018, 54, 450–462. [Google Scholar] [CrossRef]
- Stanmore, E.; Stubbs, B.; Vancampfort, D.; de Bruin, E.D.; Firth, J. The effect of active video games on cognitive functioning in clinical and non-clinical populations: A meta-analysis of randomized controlled trials. Neurosci. Biobehav. Rev. 2017, 78, 34–43. [Google Scholar] [CrossRef]
- Stojan, R.; Voelcker-Rehage, C. A Systematic Review on the Cognitive Benefits and Neurophysiological Correlates of Exergaming in Healthy Older Adults. J. Clin. Med. 2019, 8, 734. [Google Scholar] [CrossRef] [PubMed]
- Yen, H.Y.; Chiu, H.L. Virtual Reality Exergames for Improving Older Adults’ Cognition and Depression: A Systematic Review and Meta-Analysis of Randomized Control Trials. J. Am. Med Dir. Assoc. 2021. [Google Scholar] [CrossRef]
- Zhao, Y.; Feng, H.; Wu, X.; Du, Y.; Yang, X.; Hu, M.; Ning, H.; Liao, L.; Chen, H.; Zhao, Y. Effectiveness of Exergaming in Improving Cognitive and Physical Function in People With Mild Cognitive Impairment or Dementia: Systematic Review. JMIR Serious Games 2020, 8, e16841. [Google Scholar] [CrossRef]
- Drazich, B.F.; LaFave, S.; Crane, B.M.; Szanton, S.L.; Carlson, M.C.; Budhathoki, C.; Taylor, J.L. Exergames and Depressive Symptoms in Older Adults: A Systematic Review. Games Health J. 2020, 9, 339–345. [Google Scholar] [CrossRef]
- Li, J.; Theng, Y.L.; Foo, S. Effect of Exergames on Depression: A Systematic Review and Meta-Analysis. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Street, T.D.; Lacey, S.J.; Langdon, R.R. Gaming Your Way to Health: A Systematic Review of Exergaming Programs to Increase Health and Exercise Behaviors in Adults. Games Health J. 2017, 6, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Zeng, N.; McDonough, D.J.; Gao, Z. Effect of Active Video Games on Healthy Children’s Fundamental Motor Skills and Physical Fitness: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8264. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, P.D.; Capistrano, R.; Zequinão, M.A.; Silva, S.A.D.; Beltrame, T.S.; Cardoso, F.L. Exergames as a Tool for the Acquisition and Development of Motor Skills and Abilities: A systematic review. Rev. Paul. Pediatr. 2017, 35, 464–471. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Page, Z.E.; Barrington, S.; Edwards, J.; Barnett, L.M. Do active video games benefit the motor skill development of non-typically developing children and adolescents: A systematic review. J. Sci. Med. Sport 2017, 20, 1087–1100. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Merellano-Navarro, E.; Olivares, P.R.; García-Rubio, J.; Gusi, N. Effect of exergames on musculoskeletal pain: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2018, 28, 760–771. [Google Scholar] [CrossRef]
- Corregidor-Sánchez, A.I.; Segura-Fragoso, A.; Criado-Álvarez, J.J.; Rodríguez-Hernández, M.; Mohedano-Moriano, A.; Polonio-López, B. Effectiveness of Virtual Reality Systems to Improve the Activities of Daily Life in Older People. Int. J. Environ. Res. Public Health 2020, 17, 6283. [Google Scholar] [CrossRef]
- Molina, K.I.; Ricci, N.A.; de Moraes, S.A.; Perracini, M.R. Virtual reality using games for improving physical functioning in older adults: A systematic review. J. Neuroeng. Rehabil. 2014, 11, 156. [Google Scholar] [CrossRef]
- Ramírez-Granizo, I.A.; Ubago-Jiménez, J.L.; González-Valero, G.; Puertas-Molero, P.; San Román-Mata, S. The Effect of Physical Activity and the Use of Active Video Games: Exergames in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4243. [Google Scholar] [CrossRef]
- Alhasan, H.; Alshehri, M.A.; Wheeler, P.C.; Fong, D.T.P. Effects of Interactive Videogames on Postural Control and Risk of Fall Outcomes in Frail and Pre-frail Older Adults: A Systematic Review and Meta-Analysis. Games Health J. 2021, 10, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Tahmosybayat, R.; Baker, K.; Godfrey, A.; Caplan, N.; Barry, G. A systematic review and meta-analysis of outcome measures to assess postural control in older adults who undertake exergaming. Maturitas 2017, 98, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Andrade, A.; Correia, C.K.; Coimbra, D.R. The Psychological Effects of Exergames for Children and Adolescents with Obesity: A Systematic Review and Meta-Analysis. Cyberpsychology Behav. Soc. Netw. 2019, 22, 724–735. [Google Scholar] [CrossRef]
- Cugusi, L.; Prosperini, L.; Mura, G. Exergaming for Quality of Life in persons living with chronic diseases: A systematic review and meta-analysis. PM&R 2021, 13, 756–780. [Google Scholar] [CrossRef]
- Li, J.; Erdt, M.; Chen, L.; Cao, Y.; Lee, S.-Q.; Theng, Y.-L. The Social Effects of Exergames on Older Adults: Systematic Review and Metric Analysis. J. Med Internet Res. 2018, 20, e10486. [Google Scholar] [CrossRef]
- Corregidor-Sánchez, A.I.; Segura-Fragoso, A.; Rodríguez-Hernández, M.; Criado-Alvarez, J.J.; González-Gonzalez, J.; Polonio-López, B. Can exergames contribute to improving walking capacity in older adults? A systematic review and meta-analysis. Maturitas 2020, 132, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Shida, N.; Yagiz, G.; Yamada, T. The Effects of Exergames on Muscle Architecture: A systematic review and meta-analysis protocol. Int. Platf. Regist. Syst. Rev. Meta Anal. Protoc. 2021. [Google Scholar] [CrossRef]
- The EndNote Team. EndNote, EndNote X9; Clarivate: Philadelphia, PA, USA, 2013. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef]
- Da Cunha Nascimento, D.; Petriz, B.; da Cunha Oliveira, S.; Vieira, D.C.L.; Funghetto, S.S.; Silva, A.O.; Prestes, J. Effects of blood flow restriction exercise on hemostasis: A systematic review of randomized and non-randomized trials. Int. J. Gen. Med. 2019, 12, 91. [Google Scholar] [CrossRef]
- Hooper, P.; Jutai, J.W.; Strong, G.; Russell-Minda, E. Age-related macular degeneration and low-vision rehabilitation: A systematic review. Can. J. Ophthalmol. 2008, 43, 180–187. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- The Cochrane Collaboration. Review Manager [Computer Program], 5.4.1; The Nordic Cochrane Centre: Copenhagen, Danmark, 2020. [Google Scholar]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Hedges, L.V.; Olkin, I. Statistical Methods for Meta-Analysis; Academic Press: New York, USA, 2014. [Google Scholar]
- Brydges, C.R. Effect Size Guidelines, Sample Size Calculations, and Statistical Power in Gerontology. Innov. Aging 2019, 3, igz036. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 [updated March 2011]; The Cochrane Collaboration: Chichester, UK, 2011. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Effect Sizes Based on Means. In Introduction to Meta-Analysis; John Wiley & Sons Ltd: Chichester, UK, 2009; pp. 21–32. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions, version 5.0.2; Higgins, J.G.S., Ed.; The Cochrane Collaboration: Chichester, UK, 2011. [Google Scholar]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Green, B.; Bourne, M.N.; van Dyk, N.; Pizzari, T. Recalibrating the risk of hamstring strain injury (HSI): A 2020 systematic review and meta-analysis of risk factors for index and recurrent hamstring strain injury in sport. Br. J. Sports Med. 2020, 54, 1081. [Google Scholar] [CrossRef] [PubMed]
- Biesek, S.; Vojciechowski, A.S.; Filho, J.M.; Menezes Ferreira, A.C.R.; Borba, V.Z.C.; Rabito, E.I.; Gomes, A.R.S. Effects of Exergames and Protein Supplementation on Body Composition and Musculoskeletal Function of Prefrail Community-Dwelling Older Women: A Randomized, Controlled Clinical Trial. Int. J. Environ. Res. Public Health 2021, 18, 9324. [Google Scholar] [CrossRef]
- Gallo, L.H.; Rodrigues, E.V.; Melo Filho, J.; da Silva, J.B.; Harris-Love, M.O.; Gomes, A.R.S. Effects of virtual dance exercise on skeletal muscle architecture and function of community dwelling older women. J. Musculoskelet. Neuronal Interact. 2019, 19, 50. [Google Scholar] [PubMed]
- Nambi, G.; Abdelbasset, W.; Alqahtani, B. Radiological (Magnetic Resonance Image and Ultrasound) and biochemical effects of virtual reality training on balance training in football players with chronic low back pain: A randomized controlled study. J. Back Musculoskelet. Rehabil. 2020, 34, 1–9. [Google Scholar] [CrossRef]
- Rodrigues, E.V.; Gallo, L.H.; Guimarães, A.T.B.; Melo Filho, J.; Luna, B.C.; Gomes, A.R.S. Effects of dance exergaming on depressive symptoms, fear of falling, and musculoskeletal function in fallers and nonfallers community-dwelling older women. Rejuvenation Res. 2018, 21, 518–526. [Google Scholar] [CrossRef]
- Vojciechowski, A.S.; Silva, C.T.S.; Rodrigues, E.V.; Gallo, L.H.; Melo Filho, J.; Gomes, A.R.S. Does Physical Dance Training with Virtual Games Change Muscle Quality of Community-Dwelling Older Women? Games Health J. 2021. [Google Scholar] [CrossRef]
- Kwan, E.; Straus, S.E. Assessment and management of falls in older people. CMAJ 2014, 186, E610–E621. [Google Scholar] [CrossRef]
- Schoene, D.; Valenzuela, T.; Lord, S.R.; de Bruin, E.D. The effect of interactive cognitive-motor training in reducing fall risk in older people: A systematic review. BMC Geriatr. 2014, 14, 107. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.A.; Mahoney, J.E.; Ehrenreich, H. Circumstances and outcomes of falls among high risk community-dwelling older adults. Inj. Epidemiol. 2014, 1, 1–9. [Google Scholar] [CrossRef]
- Akyol, A.D. Falls in the elderly: What can be done? Int. Nurs. Rev. 2007, 54, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Ganz, D.A.; Bao, Y.; Shekelle, P.G.; Rubenstein, L.Z. Will my patient fall? Jama 2007, 297, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Liperoti, R.; Russo, A.; Giovannini, S.; Tosato, M.; Capoluongo, E.; Bernabei, R.; Onder, G. Sarcopenia as a risk factor for falls in elderly individuals: Results from the ilSIRENTE study. Clin. Nutr. 2012, 31, 652–658. [Google Scholar] [CrossRef]
- Szulc, P.; Beck, T.J.; Marchand, F.; Delmas, P.D. Low skeletal muscle mass is associated with poor structural parameters of bone and impaired balance in elderly men—The MINOS study. J. Bone Miner. Res. 2005, 20, 721–729. [Google Scholar] [CrossRef]
- Sekendiz, B.; Cuğ, M.; Korkusuz, F. Effects of Swiss-ball core strength training on strength, endurance, flexibility, and balance in sedentary women. J. Strength Cond. Res. 2010, 24, 3032–3040. [Google Scholar] [CrossRef] [PubMed]
- Trainor, T.J.; Trainor, M.A. Etiology of low back pain in athletes. Curr. Sports Med. Rep. 2004, 3, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Barker, K.L.; Shamley, D.R.; Jackson, D. Changes in the cross-sectional area of multifidus and psoas in patients with unilateral back pain: The relationship to pain and disability. Spine 2004, 29, E515–E519. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Tianjing, L.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions, version 6.2; The Cochrane Collaboration: Chichester, UK, 2021. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).