Effect of Washing Condition on the Fracture Strength, and the Degree of Conversion of 3D Printing Resin
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Materials
2.2. Experimental Groups
2.3. Experimental Method
2.4. Statistical Analysis
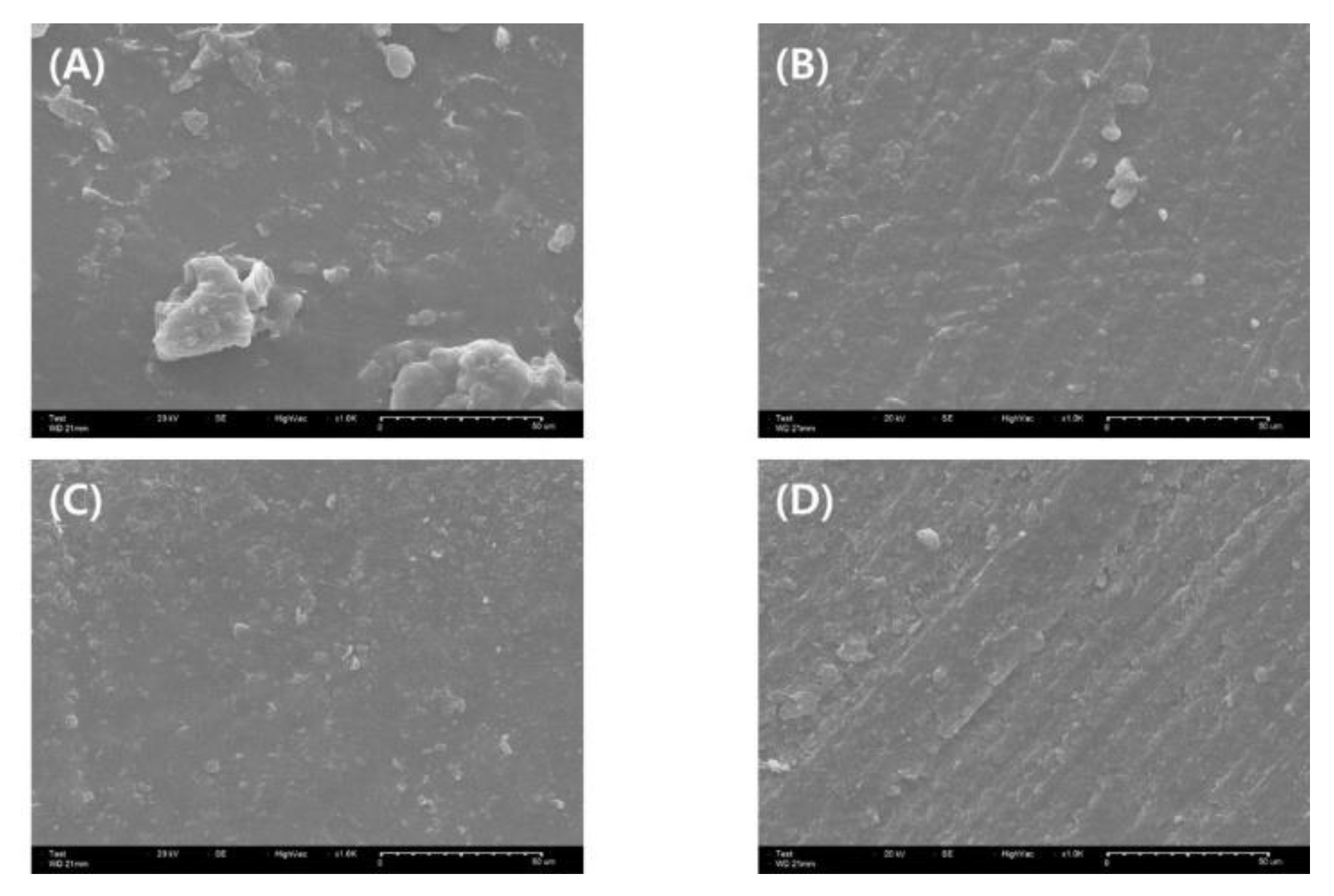
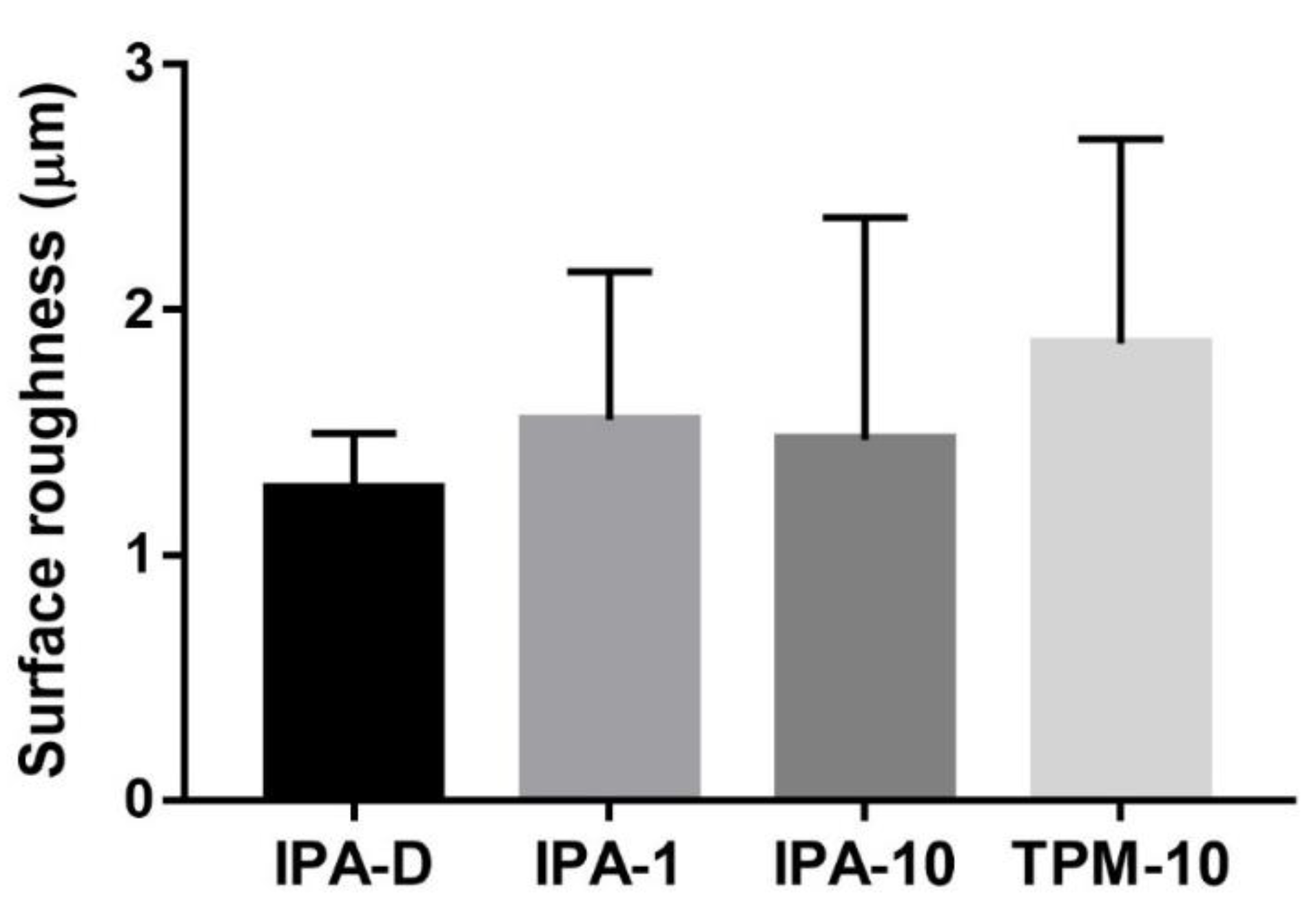
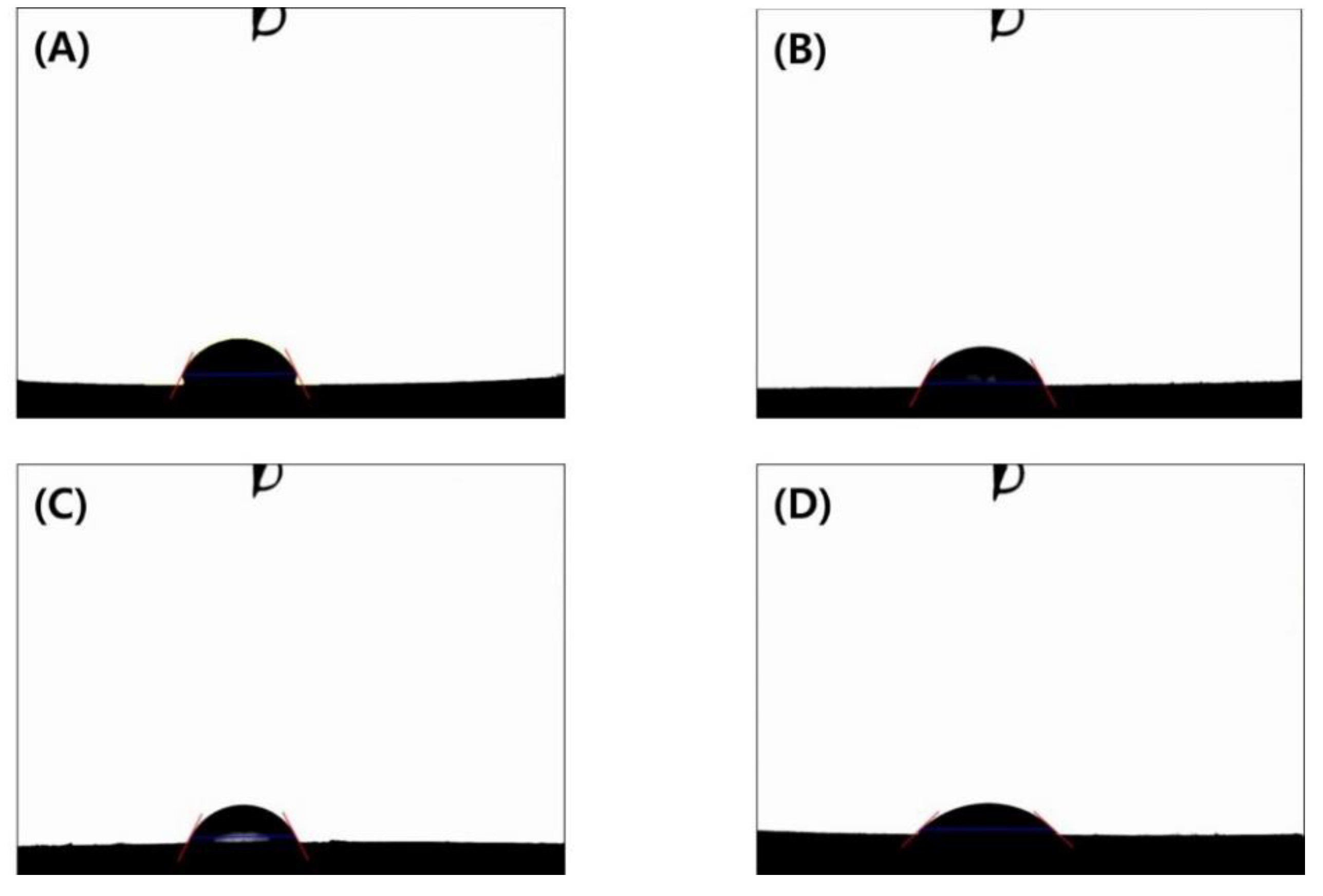
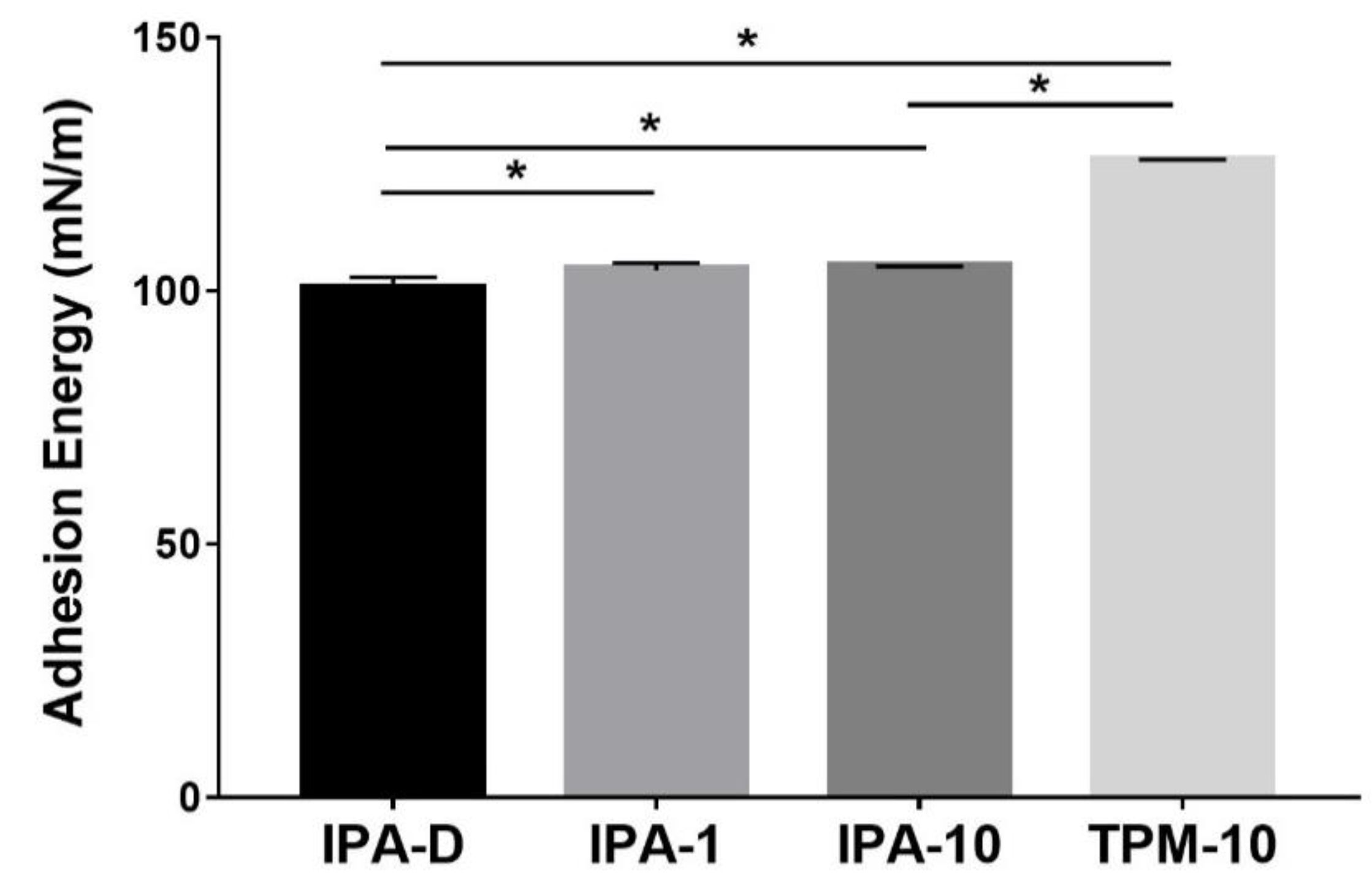
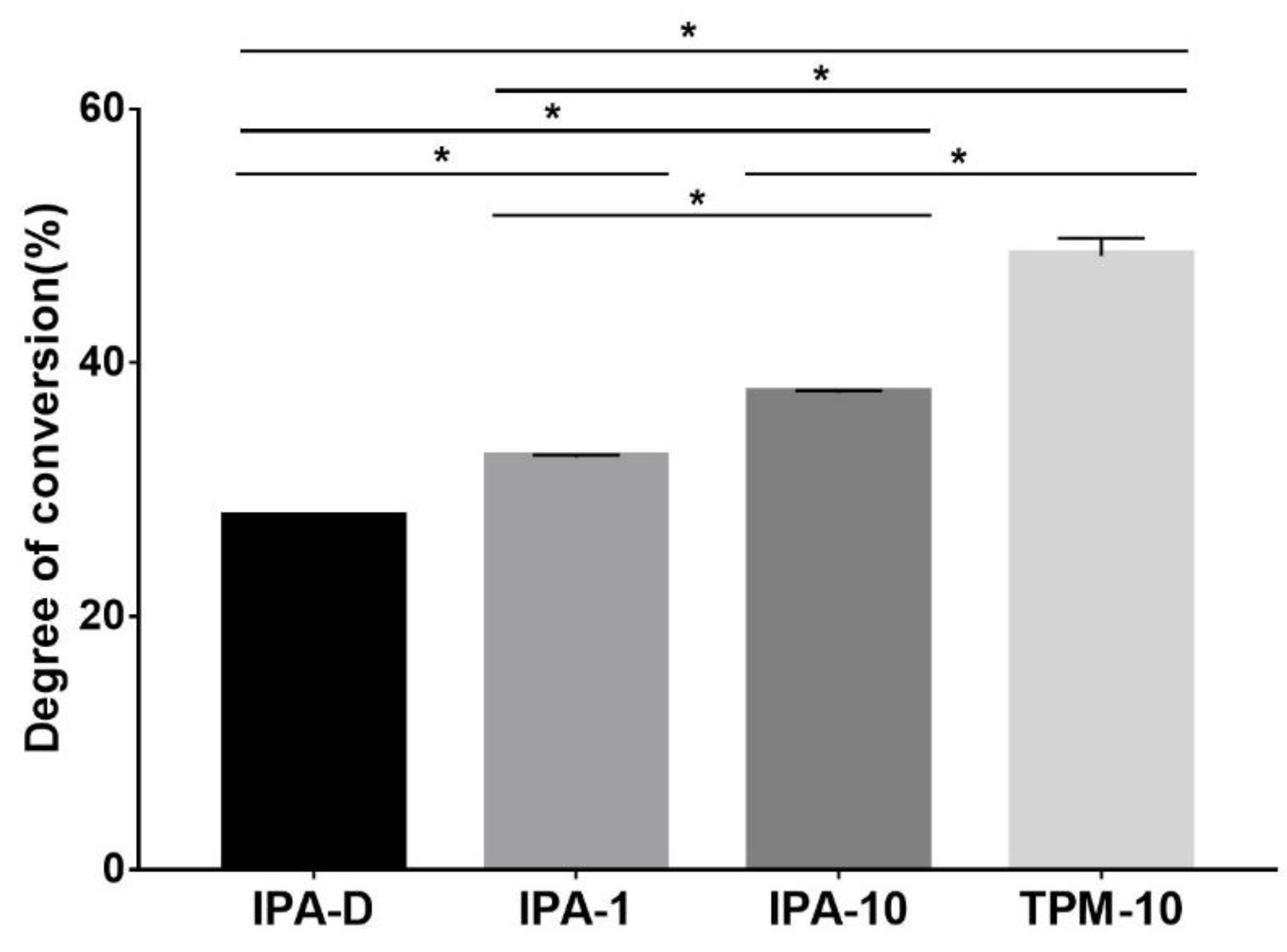
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Schönhoff, L.M.; Mayinger, F.; Eichberger, M.; Reznikova, E.; Stawarczyk, B. 3D printing of dental restorations: Mechanical properties of thermoplastic polymer materials. J. Mech. Behav. Biomed. Mater. 2021, 119, 104544. [Google Scholar] [CrossRef] [PubMed]
- Pillai, S.; Upadhyay, A.; Khayambashi, P.; Farooq, I.; Sabri, H.; Tarar, M.; Lee, K.T.; Harb, I.; Zhou, S.; Wang, Y.; et al. Dental 3D-Printing: Transferring Art from the Laboratories to the Clinics. Polymers 2021, 13, 157. [Google Scholar] [CrossRef] [PubMed]
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry—State of the art. Operat. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Bud, E.S.; Bocanet, V.-I.; Muntean, M.H.; Vlasa, A.B.; Sorana, M.; Pacurar, M.D.; Bogdan, R.; Olteanu, C.D.; Bud, A. Accuracy of Three-Dimensional (3D) Printed Dental Digital Models Generated with Three Types of Resin Polymers by Extra-Oral Optical Scanning. J. Clin. Med. 2021, 109, 1908. [Google Scholar] [CrossRef] [PubMed]
- Greco, G.B.; Popi, D.; Di Stefano, D.A. Accuracy of 3-dimensional printing of dental casts: A proposal for quality standardization. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Lee, J.H.; Lee, K.B. Comparison of Intaglio Surface Trueness of Interim Dental Crowns Fabricated with SLA 3D Printing, DLP 3D Printing, and Milling Technologies. Healthcare 2021, 9, 983. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.W.; Shin, S.-Y. Accuracy of dies fabricated by various three dimensional printing systems: A comparative study. J. Dent. Rehabil. Appl. Sci. 2020, 36, 242–253. [Google Scholar] [CrossRef]
- Song, G.; Son, J.W.; Jang, J.H.; Choi, S.H.; Jang, W.H.; Lee, B.N.; Park, C. Comparing volumetric and biological aspects of 3D-printed interim restorations under various post-curing modes. J. Adv. Prosthodont. 2021, 13, 71–78. [Google Scholar] [CrossRef]
- Nowacki, B.; Kowol, P.; Koziol, M.; Olesik, P.; Wieczorek, J.; Waclawiak, K. Effect of Post-Process Curing and Washing Time on Mechanical Properties of mSLA Printouts. Materials 2021, 14, 4856. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Kim, D.; Shim, J.-S.; Lee, D.; Shin, S.-H.; Nam, N.-E.; Park, K.-H.; Shim, J.-S.; Kim, J.-E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Zhao, Z.; Zhang, Q.; Qi, H.J.; Fang, D. Mechanics of shape distortion of DLP 3D printed structures during UV post-curing. Soft Matter. 2019, 15, 6151–6159. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Lumkemann, N.; Stawarczyk, B. 3D-printed material for temporary restorations: Impact of print layer thickness and post-curing method on degree of conversion. Int. J. Comput. Dent. 2019, 22, 231–237. [Google Scholar]
- Jindal, P.; Juneja, M.; Bajaj, D.; Siena, F.L.; Breedon, P. Effects of post-curing conditions on mechanical properties of 3D printed clear dental aligners. Rapid Prototyp. J. 2020, 26, 1337–1344. [Google Scholar] [CrossRef]
- Herrera-Gonzalez, A.M.; Caldera-Villalobos, M.; Perez-Mondragon, A.A.; Cuevas-Suarez, C.E.; Gonzalez-Lopez, J.A. Analysis of Double Bond Conversion of Photopolymerizable Monomers by FTIR-ATR Spectroscopy. J. Chem. Educ. 2019, 96, 1786–1789. [Google Scholar] [CrossRef]
- Moldovan, M.; Balazsi, R.; Soanca, A.; Roman, A.; Sarosi, C.; Prodan, D.; Vlassa, M.; Cojocaru, I.; Saceleanu, V.; Cristescu, I. Evaluation of the Degree of Conversion, Residual Monomers and Mechanical Properties of Some Light-Cured Dental Resin Composites. Materials 2019, 12, 2109. [Google Scholar] [CrossRef] [Green Version]
- Suvarna, S.; Chhabra, T.; Raghav, D.; Singh, D.; Kumar, P.; Sahoo, S. Residual monomer content of repair autopolymerizing resin after microwave postpolymerization treatment. Eur. J. Prosthodont. 2014, 2, 28–32. [Google Scholar]
- Leloup, G.; Holvoet, P.E.; Bebelman, S.; Devaux, J. Raman scattering determination of the depth of cure of light-activated composites: Influence of different clinically relevant parameters. J. Oral Rehabil. 2002, 29, 510–515. [Google Scholar] [CrossRef]
- Grivet, M.; Morrier, J.J.; Benay, G.; Barsotti, O. Effect of hydrophobicity on in vitro streptococcal adhesion to dental alloys. J. Mater. Sci. Mater. Med. 2000, 11, 637–642. [Google Scholar] [CrossRef] [PubMed]
- Nassar, U.; Meyer, A.E.; Ogle, R.E.; Baier, R.E. The effect of restorative and prosthetic materials on dental plaque. Periodontology 2000 1995, 8, 114–124. [Google Scholar] [CrossRef] [PubMed]
- Mabboux, F.; Ponsonnet, L.; Morrier, J.J.; Jaffrezic, N.; Barsotti, O. Surface free energy and bacterial retention to saliva-coated dental implant materials—An in vitro study. Colloids Surf. B Biointerfaces 2004, 39, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kwon, T.Y. In vitro study of Streptococcus mutans adhesion on composite resin coated with three surface sealants. Restor. Dent. Endod. 2017, 42, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Komalsingsakul, A.; Senawongse, P. Effect of the surface roughness of composite resins on the water contact angle and biofilm formation. Mahidol. Dent. J. 2019, 39, 75–84. [Google Scholar]
- Gönülol, N.; Yılmaz, F. The effects of finishing and polishing techniques on surface roughness and color stability of nanocomposites. J. Dent. 2012, 40, e64–e70. [Google Scholar] [CrossRef]
- Attia, M.A.; Shokry, T.E.; Abdel-Aziz, M. Effect of different surface treatments on the bond strength of milled polyetheretherketone posts. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef] [PubMed]
- Araújo, P.H.H.; Sayer, C.; Giudici, R.; Poço, J.G.R. Techniques for reducing residual monomer content in polymers: A review. Polym. Eng. Sci. 2002, 42, 1442–1468. [Google Scholar] [CrossRef]
- Leber, A.P. Human exposures to monomers resulting from consumer contact with polymers. Chem. Biol. Interact. 2001, 135, 215–220. [Google Scholar] [CrossRef]
- Ponting, D.J.; Ortega, M.A.; Niklasson, I.B.; Karlsson, I.; Seifert, T.; Steen, J.; Luthman, K.; Karlberg, A.T. Development of New Epoxy Resin Monomers—A Delicate Balance between Skin Allergy and Polymerization Properties. Chem. Res. Toxicol. 2018, 32, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Görukmez, E.; Şen Yilmaz, B.; Ramoglu, S.I. Is a Single Rinse Effective on Evacuating the Residual Monomers After Orthodontic Bonding? An In Vivo Study. Bezmiâlem Sci. 2021, 9, 127. [Google Scholar] [CrossRef]
- Seo, D.-S. Influence of the washing process on the aligning capability of a nematic liquid crystal on polymer surfaces. Liquid Cryst. 2000, 27, 789–793. [Google Scholar] [CrossRef]
- Guerra, R.M.; Duran, I.; Ortiz, P. FTIR monomer conversion analysis of UDMA-based dental resins. J. Oral Rehabil. 1996, 23, 632–637. [Google Scholar] [CrossRef] [PubMed]


| Photopolymer Resin | |
|---|---|
| Monomers | Methacrylic oligomers |
| Crosslinking agent | Phosphine oxide |
| Dipping with IPA (IPA-D) | 1 min with IPA (IPA-1) | 10 min with IPA (IPA-10) | 10 min with TPM (TPM-10) | |
|---|---|---|---|---|
| Uncured | 10 | 10 | 10 | 10 |
| Cured | 10 | 10 | 10 | 10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, W.; Kook, G.-S.; Kang, J.-H.; Kim, Y.; Yun, Y.; Lee, S.-K.; Park, S.-W.; Lim, H.-P.; Yun, K.-D.; Park, C. Effect of Washing Condition on the Fracture Strength, and the Degree of Conversion of 3D Printing Resin. Appl. Sci. 2021, 11, 11676. https://doi.org/10.3390/app112411676
Jang W, Kook G-S, Kang J-H, Kim Y, Yun Y, Lee S-K, Park S-W, Lim H-P, Yun K-D, Park C. Effect of Washing Condition on the Fracture Strength, and the Degree of Conversion of 3D Printing Resin. Applied Sciences. 2021; 11(24):11676. https://doi.org/10.3390/app112411676
Chicago/Turabian StyleJang, Woohyung, Gyeong-Soo Kook, Jin-Ho Kang, Yeseul Kim, Yina Yun, Seon-Ki Lee, Sang-Won Park, Hyun-Pil Lim, Kwi-Dug Yun, and Chan Park. 2021. "Effect of Washing Condition on the Fracture Strength, and the Degree of Conversion of 3D Printing Resin" Applied Sciences 11, no. 24: 11676. https://doi.org/10.3390/app112411676






