The Efficacy of Tele-Rehabilitation Program for Improving Upper Limb Function among Adults Following Elbow Fractures: A Pilot Study
Abstract
:1. Background
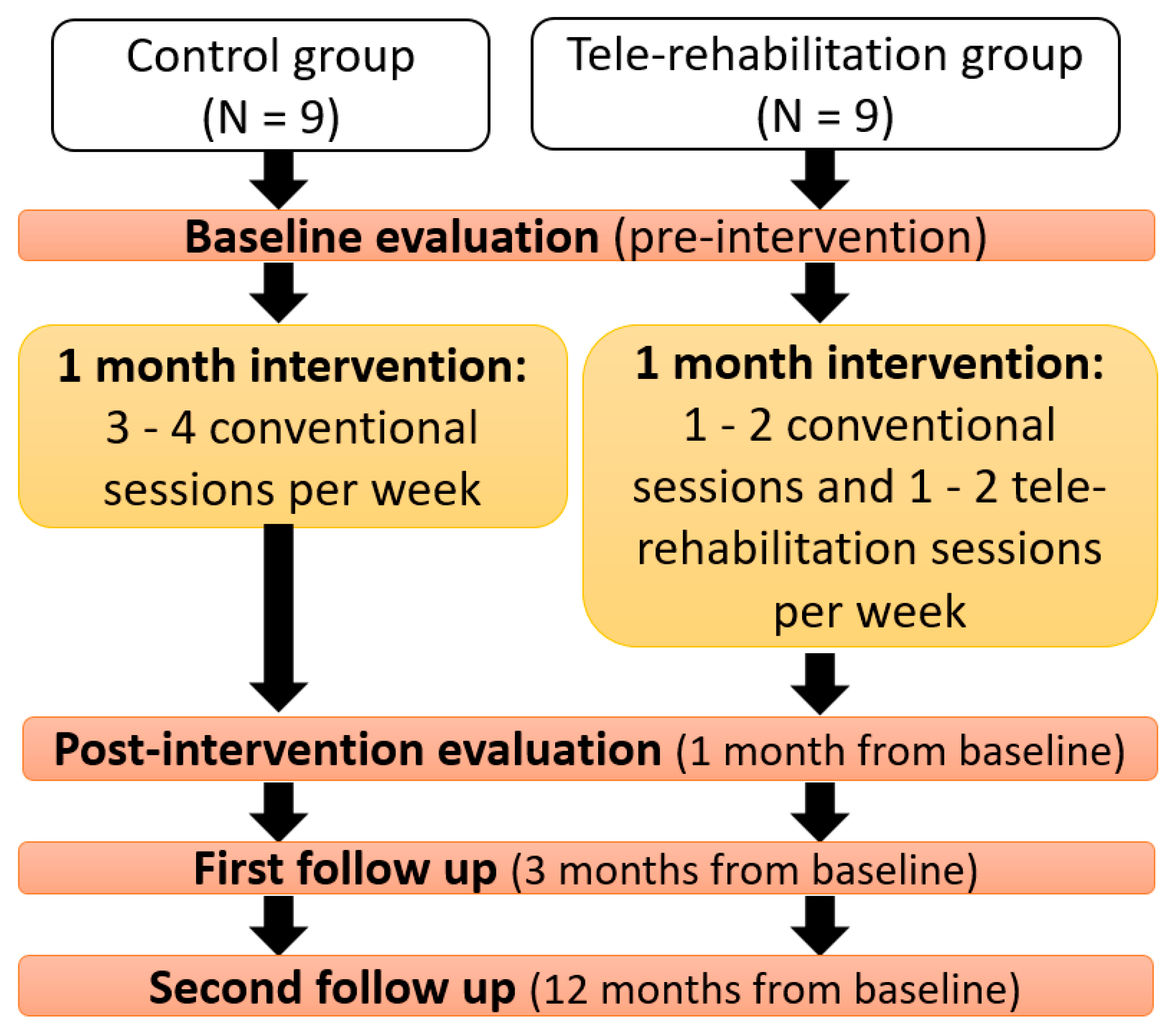
2. Methods
2.1. Participants
2.2. Study Tools and Protocol
2.2.1. Evaluation
- The Disabilities of Arm, Shoulder and Hand (DASH; [28]), a self-assessment functional questionnaire used following an upper extremity injury. The questionnaire includes 30 items concerning functioning and severity of the symptoms in the past week. The patient is asked to rate the difficulty level of performing 21 physical activities on a Likert scale (from 1 = no difficulty to 5 = unable to perform) and the influence of the physical injury on the social functioning (1 = not at all to 5 = extreme). The final score ranges from 0 to 100, with a higher score indicating poorer functioning and more severe symptoms. DASH has a high repeatability in subjects with elbow injuries (ICC = 0.92; [29]). It has also been found that the tool is sensitive to post-treatment status changes compared to the pretreatment condition [29].
- The Patient-Rated Elbow Evaluation (PREE; [30]), a self-assessment questionnaire following elbow injuries which evaluates the level of pain and level of function of the affected limb on a Likert scale between 0–10 (0 = no pain and no functional limitations to 10 = the highest pain or highest disability). The questionnaire has three parts: 5 questions are related to the level of pain; 11 questions regarding the ability to perform specific tasks with the elbow, e.g., combing the hair; and 4 questions related to usual daily life activities (dressing, eating, etc.). High scores reflect higher pain and disability. This questionnaire was translated from English to Hebrew as part of this study in a re-translation procedure and expert validation.
- Patient satisfaction questionnaire, about self-management of the home program, a self-completion questionnaire compiled by Dr. Debbie Rand from the Department of Occupational Therapy at Tel Aviv University and adapted for this study. The questionnaire consists of 7 questions. Four items used a Likert scale between 1 and 5 (1 = not at all and 5 = very much): satisfaction from the intervention, level of motivation evoked by the intervention, subjective motor improvement of the injured hand, and the duration of the practice. The other 3 items regarded the assistance needed to use the intervention at home (needs help all the time, occasionally needs help, or do not need help at all) [31].
- The System Usability Scale (SUS; [32]), a questionnaire filled out by the subjects in the tele-rehabilitation group, intended to examine the degree of convenience of using technological systems. This questionnaire consists of 10 statements on the Likert scale (1 = strongly disagrees to 5 = strongly agrees). The scoring is performed as follows: uneven items (1, 3, 5, 7, 9) are deducted by one point from the subject selection, and even items (2, 4, 6, 8, 10) subtract the subject choice from five. The sum of the items is multiplied by 2.5, and a score is obtained on a scale between 0 and 100. A higher score indicates a more positive opinion about the comfort of the system.
2.2.2. Intervention
2.3. Data Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- MacDermid, J.C.; Vincent, J.I.; Kieffer, L.; Kieffer, A.; Demaiter, J.; MacIntosh, S. A Survey of Practice Patterns for Rehabilitation Post Elbow Fracture. Open Orthop. J. 2012, 6, 429–439. [Google Scholar] [CrossRef] [PubMed]
- Everding, N.G.; Maschke, S.D.; Hoyen, H.A.; Evans, P.J. Prevention and treatment of elbow stiffness: A 5-year update. J. Hand Surg. Am. 2013, 38, 2496–2507. [Google Scholar] [CrossRef] [PubMed]
- Harding, P.; Rasekaba, T.; Smirneos, L.; Holland, A.E. Early mobilisation for elbow fractures in adults. Cochrane Database Syst. Rev. 2011, 6, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Fusaro, I.; Orsini, S.; Stignani Kantar, S.; Sforza, T.; Benedetti, M.G.; Bettelli, G.; Rotini, R. Elbow rehabilitation in traumatic pathology. Musculoskelet. Surg. 2014, 98, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Fradet, L.; Liefhold, B.; Rettig, O.; Bruckner, T.; Akbar, M.; Wolf, S.I. Proposition of a protocol to evaluate upper-extremity functional deficits and compensation mechanisms: Application to elbow contracture. J. Orthop. Sci. 2015, 20, 321–330. [Google Scholar] [CrossRef]
- Chinchalkar, S.J.; Szekeres, M. Rehabilitation of elbow trauma. Hand Clin. 2004, 20, 363–374. [Google Scholar] [CrossRef]
- Brach, P.; Goitz, R.J. Elbow Arthroscopy: Surgical Techniques and Rehabilitation. J. Hand Ther. 2006, 19, 228–237. [Google Scholar] [CrossRef]
- Paschos, N.K.; Mitsionis, G.I.; Vasiliadis, H.S.; Georgoulis, A.D. Comparison of early mobilization protocols in radial head fractures. J. Orthop. Trauma 2013, 27, 134–139. [Google Scholar] [CrossRef]
- Blackmore, S.M.; Michlovitz, S. The Elbow: Current Practice and Research. The Next Step. J. Hand Ther. 2006, 19, 67–70. [Google Scholar] [CrossRef]
- Mellema, J.J.; Lindenhovius, A.L.C.; Jupiter, J.B. The posttraumatic stiff elbow: An update. Curr. Rev. Musculoskelet. Med. 2016, 9, 190–198. [Google Scholar] [CrossRef] [Green Version]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 625–638. [Google Scholar] [CrossRef]
- Agostini, M.; Moja, L.; Banzi, R.; Pistotti, V.; Tonin, P.; Venneri, A.; Turolla, A. Telerehabilitation and recovery of motor function: A systematic review and meta-analysis. J. Telemed. Telecare 2015, 21, 202–213. [Google Scholar] [CrossRef] [Green Version]
- Grona, S.L.; Bath, B.; Busch, A.; Rotter, T.; Trask, C.; Harrison, E. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: A systematic review. J. Telemed. Telecare 2018, 24, 341–355. [Google Scholar] [CrossRef]
- Malliaras, P.; Cridland, K.; Hopmans, R.; Ashton, S.; Littlewood, C.; Page, R.; Harris, I.; Skouteris, H.; Haines, T. Internet and Telerehabilitation-Delivered Management of Rotator Cuff-Related Shoulder Pain (INTEL Trial): Randomized Controlled Pilot and Feasibility Trial. JMIR mHealth uHealth 2020, 8, e24311. [Google Scholar] [CrossRef]
- Jansson, M.M.; Rantala, A.; Miettunen, J.; Puhto, A.P.; Pikkarainen, M. The effects and safety of telerehabilitation in patients with lower-limb joint replacement: A systematic review and narrative synthesis. J. Telemed. Telecare 2020, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef]
- de la Iglesia, D.H.; Mendes, A.S.; González, G.V.; Jiménez-Bravo, D.M.; de Paz Santana, J.F. Connected elbow exoskeleton system for rehabilitation training based on virtual reality and context-aware. Sensors 2020, 20, 858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padilla-Castañeda, M.A.; Sotgiu, E.; Barsotti, M.; Frisoli, A.; Orsini, P.; Martiradonna, A.; Laddaga, C.; Bergamasco, M. An Orthopaedic Robotic-Assisted Rehabilitation Method of the Forearm in Virtual Reality Physiotherapy. J. Healthc. Eng. 2018, 2018, 1–20. [Google Scholar]
- Lade, H.; McKenzie, S.; Steele, L.; Russell, T.G. Validity and reliability of the assessment and diagnosis of musculoskeletal elbow disorders using telerehabilitation. J. Telemed. Telecare 2012, 18, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Sanford, J.A.; Griffiths, P.C.; Richardson, P.; Hargraves, K.; Butterfield, T.; Hoenig, H. The effects of in-home rehabilitation on task self-efficacy in mobility-impaired adults: A randomized clinical trial. J. Am. Geriatr. Soc. 2006, 54, 1641–1648. [Google Scholar] [CrossRef] [PubMed]
- Prvu Bettger, J.; Green, C.L.; Holmes, D.J.N.; Chokshi, A.; Mather, R.C.; Hoch, B.T.; de Leon, A.J.; Aluisio, F.; Seyler, T.M.; Del Gaizo, D.J.; et al. Effects of Virtual Exercise Rehabilitation In-Home Therapy Compared with Traditional Care After Total Knee Arthroplasty: VERITAS, a Randomized Controlled Trial. J. Bone Jt. Surg. Am. 2020, 102, 101–109. [Google Scholar] [CrossRef] [Green Version]
- Tousignant, M.; Boissy, P.; Corriveau, H.; Moffet, H. In home telerehabilitation for older adults after discharge from an acute hospital or rehabilitation unit: A proof-of-concept study and costs estimation. Disabil. Rehabil. Assist. Technol. 2006, 1, 209–216. [Google Scholar] [CrossRef]
- Sarsak, H.I. Telerehabilitation services: A successful paradigm for occupational therapy clinical services? Int. Phys. Med. Rehabil. J. 2020, 5, 93–98. [Google Scholar] [CrossRef]
- Turolla, A.; Rossettini, G.; Viceconti, A.; Palese, A.; Geri, T. Musculoskeletal Physical Therapy During the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys. Ther. 2020, 100, 1260–1264. [Google Scholar] [CrossRef] [PubMed]
- Mathiowetz, V. Comparison of Rolyan and Jamar dynamometers for measuring grip strength. Occup. Ther. Int. 2002, 9, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Mathiowetz, V.; Weber, K.; Volland, G.; Kashman, N. Reliability and validity of grip and pinch strength evaluations. J. Hand Surg. Am. 1984, 9, 222–226. [Google Scholar] [CrossRef]
- Jebsen, R.H.; Taylor, N.; Trieschmann, R.B.; Trotter, M.J.; Howard, L.A. An objective and standardized test of hand function. Arch. Phys. Med. Rehabil. 1969, 50, 311–319. [Google Scholar]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder, and head). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Beaton, D.E.; Katz, J.N.; Fossel, A.H.; Wright, J.G.; Tarasuk, V.; Bombardier, C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J. Hand Ther. 2001, 14, 128–142. [Google Scholar] [CrossRef]
- MacDermid, J.C. Outcome evaluation in patients with elbow pathology: Issues in instrument development and evaluation. J. Hand Ther. 2001, 14, 105–114. [Google Scholar] [CrossRef]
- Shochat, G.; Maoz, S.; Stark-Inbar, A.; Blumenfeld, B.; Rand, D.; Preminger, S.; Sacher, Y. Motion-based virtual reality cognitive training targeting executive functions in acquired brain injury community-dwelling individuals: A feasibility and initial efficacy pilot. In Proceedings of the International Conference on Virtual Rehabilitation, ICVR, Montreal, QC, Canada, 19–22 June 2017; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2017; Volume 2017-June. [Google Scholar]
- Brooke, J. SUS: A “Quick and Dirty” Usability Scale. In Usability Evaluation In Industry; CRC Press: Boca Raton, FL, USA, 1996; pp. 207–212. [Google Scholar]
- Carmeli, E.; Peleg, S.; Bartur, G.; Elbo, E.; Vatine, J.J. HandTutorTM enhanced hand rehabilitation after stroke—A pilot study. Physiother. Res. Int. 2011, 16, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Chua, K.S.G.; Kuah, C.W.K. Innovating With Rehabilitation Technology in the Real World: Promises, Potentials, and Perspectives. Am. J. Phys. Med. Rehabil. 2017, 96, S150–S156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dávila, S.A. Therapist’s Management of Fractures and Dislocations of the Elbow. In Rehabilitation of the Hand and Upper Extremity, 2-Volume Set; Elsevier: Amsterdam, The Netherlands, 2011; pp. 1061–1074.e2. [Google Scholar]
- Schmitt, J.S.; Di Fabio, R.P. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J. Clin. Epidemiol. 2004, 57, 1008–1018. [Google Scholar] [CrossRef] [PubMed]
- Angst, F.; Schwyzer, H.K.; Aeschlimann, A.; Simmen, B.R.; Goldhahn, J. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and Its Short Version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society Standardized Shoulder Assessment Form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire. Arthritis Care Res. 2011, 63, S174–S188. [Google Scholar]
- Bland, M.D.; Beebe, J.A.; Hardwick, D.D.; Lang, C.E. Restricted Active Range of Motion at the Elbow, Forearm, Wrist, or Fingers Decreases Hand Function. J. Hand Ther. 2008, 21, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Piron, L.; Turolla, A.; Tonin, P.; Piccione, F.; Lain, L.; Dam, M. Satisfaction with care in post-stroke patients undergoing a telerehabilitation programme at home. J. Telemed. Telecare 2008, 14, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; Lannin, N.A.; George, S.; Sherrington, C. Telerehabilitation services for stroke. Cochrane Database Syst. Rev. 2020, 1, 1–78. [Google Scholar] [CrossRef]
- Hopp, F.; Woodbridge, P.; Subramanian, U.; Copeland, L.; Smith, D.; Lowery, J. Outcomes Associated with a Home Care Telehealth Intervention. Telemed. J. e-Health 2006, 12, 297–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tousignant, M.; Boissy, P.; Moffet, H.; Corriveau, H.; Cabana, F.; Marquis, F.; Simard, J. Patients’ satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists’ satisfaction toward technology for post-knee arthroplasty: An embedded study in a randomized trial. Telemed. J. e-Health 2011, 17, 376–382. [Google Scholar] [CrossRef]
- Groth, G.N.; Wulf, M.B. Compliance with Hand Rehabilitation: Health Beliefs and Strategies. J. Hand Ther. 1995, 8, 18–22. [Google Scholar] [CrossRef]
- Crepeau, E.B.; Garren, K.R. I looked to her as a guide: The therapeutic relationship in hand therapy. Disabil. Rehabil. 2011, 33, 872–881. [Google Scholar] [CrossRef] [PubMed]
- Kachooei, A.R.; Moradi, A.; Janssen, S.J.; Ring, D. The influence of dominant limb involvement on DASH and QuickDASH. Hand 2015, 10, 512–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Tele-Rehabilitation Group (N = 9) | Control Group (N = 9) | p | |
|---|---|---|---|
| Age (years) | 33.0 (27.9) | 60.0 (37.0) | 0.185 ¥ |
| Sex | 3 male; 6 female | 4 male; 5 female | 1.000 § |
| Injured hand | 3 Right; 6 Left | 3 Right; 6 Left | 1.000 § |
| Injured hand | 3 D; 6 ND | 3 D; 6 ND | 1.000 § |
| Hand dominance | 7 Right; 2 Left | 8 Right; 1 Left | 1.000 § |
| Fracture type | 4 Ol, 3 DH, 2 Arth | 4 Ol, 3 DH, 2RH, 1 Arth. | 0.469 § |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayer, N.; Portnoy, S.; Palti, R.; Levanon, Y. The Efficacy of Tele-Rehabilitation Program for Improving Upper Limb Function among Adults Following Elbow Fractures: A Pilot Study. Appl. Sci. 2021, 11, 1708. https://doi.org/10.3390/app11041708
Mayer N, Portnoy S, Palti R, Levanon Y. The Efficacy of Tele-Rehabilitation Program for Improving Upper Limb Function among Adults Following Elbow Fractures: A Pilot Study. Applied Sciences. 2021; 11(4):1708. https://doi.org/10.3390/app11041708
Chicago/Turabian StyleMayer, Naomi, Sigal Portnoy, Ram Palti, and Yafa Levanon. 2021. "The Efficacy of Tele-Rehabilitation Program for Improving Upper Limb Function among Adults Following Elbow Fractures: A Pilot Study" Applied Sciences 11, no. 4: 1708. https://doi.org/10.3390/app11041708
APA StyleMayer, N., Portnoy, S., Palti, R., & Levanon, Y. (2021). The Efficacy of Tele-Rehabilitation Program for Improving Upper Limb Function among Adults Following Elbow Fractures: A Pilot Study. Applied Sciences, 11(4), 1708. https://doi.org/10.3390/app11041708







