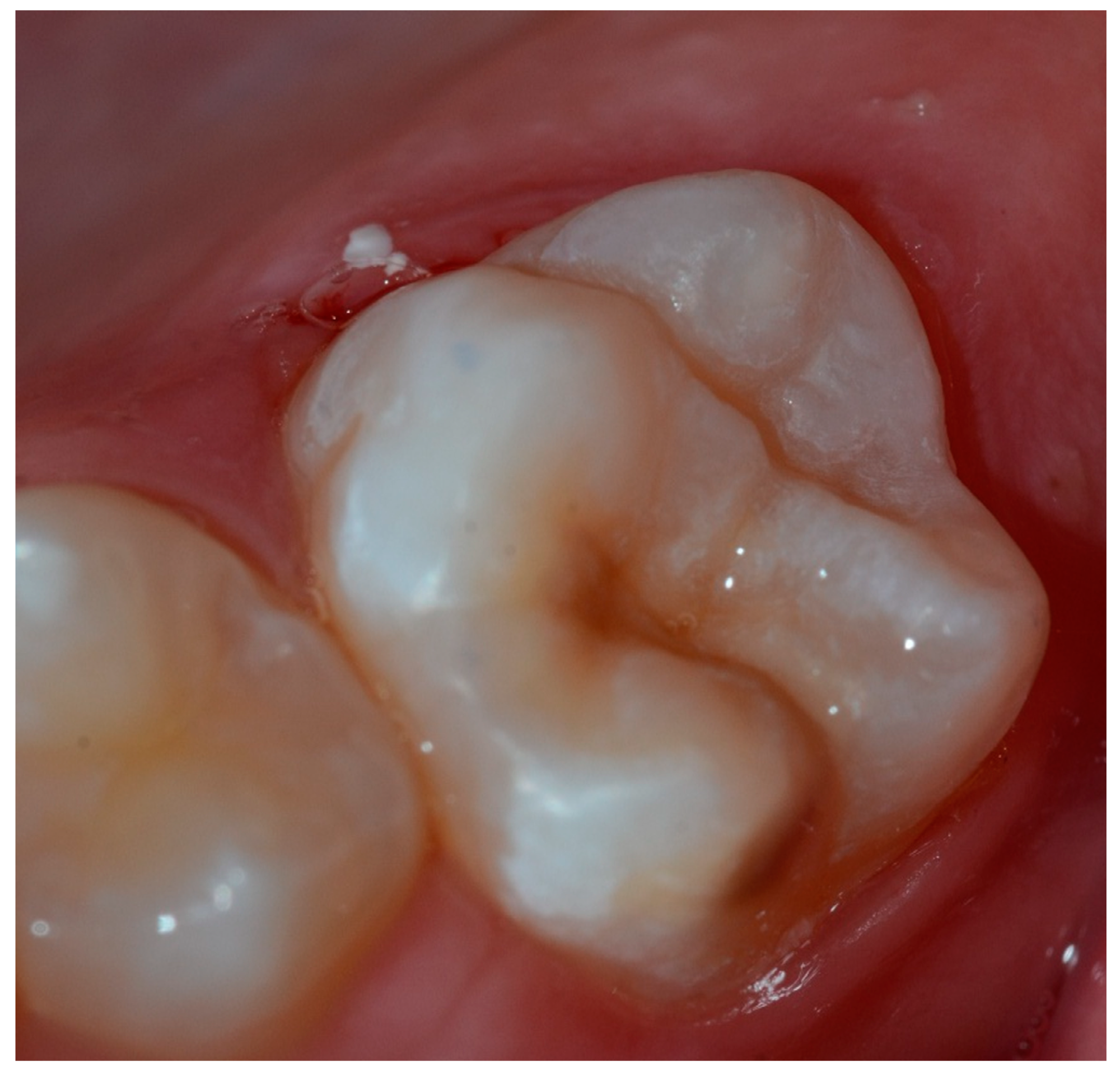
Hypersensitivity in Molar Incisor Hypomineralization: Superficial Infiltration Treatment
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Weerhrijm, K. Molar Incisor Hypomineralisation (MIH). Eur. J. Paediatr. Dent. 2003, 3, 114–120. [Google Scholar]
- Tirlet, G.; Chabouis, H.F.; Attal, J.P. Infiltration, a new therapy for masking enamel white spots: A 19- month follow-up case series. Eur. J. Esthet. Dent. 2013, 8, 180–190. [Google Scholar] [PubMed]
- Steffen, R.; Krämer, N.; Bekes, K. The Würzburg MIH concept: The MIH treatment need index (MIH TNI): A new index to assess and plan treatment in patients with molar incisior hypomineralisation (MIH). Eur. Arch. Paediatr. Dent. 2017, 18, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Hartsock, L.A.; Burnheimer, J.; Modesto, A.; Vieira, A.R. A Snapshot of the Prevalence of Molar Incisor Hypomineralization and Fluorosis in Pittsburgh, Pennsylvania, USA. Pediatr. Dent. 2020, 42, 36–40. [Google Scholar] [PubMed]
- Jälevik, B. Prevalence and Diagnosis of Molar-Incisor-Hypomineralisation (MIH): A systematic review. Eur. Arch. Paediatr. Dent. 2010, 11, 59–64. [Google Scholar] [CrossRef]
- Jälevik, B.; Norén, J.G. Enamel hypomineralization of permanent first molars: A morphological study and survey of possible aetiological factors. Int. J. Paediatr. Dent. 2000, 10, 278–289. [Google Scholar] [CrossRef]
- Apponi, R.; Presti, S.; Spinas, E.; Giannetti, L. Biological genetic and aetiology aspects in molar incisor hypomineralization. J. Biol. Regul. Homeost. Agents 2020, 34, 1219–1222. [Google Scholar]
- Da Costa-Silva, C.M.; Ambrosano, G.M.; Jeremias, F.; De Souza, J.F.; Mialhe, F.L. Increase in severity of molar- incisor hypomineralization and its relationship with the colour of enamel opacity: A prospective cohort study. Int. J. Paediatr. Dent. 2011, 21, 333–341. [Google Scholar] [CrossRef]
- Denis, M.; Atlan, A.; Vennat, E.; Tirlet, G.; Attal, J.P. White defects on enamel: Diagnosis and anatomopathology: Two essential factors for proper treatment (part 1). Int. Orthod. 2013, 11, 139–165. [Google Scholar] [CrossRef] [Green Version]
- Farah, R.A.; Monk, B.C.; Swain, M.V.; Drummond, B.K. Protein content of molar-incisor hypomineralisation enamel. J. Dent. 2010, 38, 591–596. [Google Scholar] [CrossRef]
- Crombie, F.A.; Manton, D.J.; Palamara, J.E.; Zalizniak, I.; Cochrane, N.J.; Reynolds, E.C. Characterisation of developmentally hypomineralised human enamel. J. Dent. 2013, 41, 611–618. [Google Scholar] [CrossRef]
- Bullio Fragelli, C.M.; Jeremias, F.; Feltrin de Souza, J.; Paschoal, M.A.; de Cássia Loiola Cordeiro, R.; Santos-Pinto, L. Longitudinal Evaluation of the Structural Integrity of Teeth Affected by Molar Incisor Hypomineralisation. Caries Res. 2015, 49, 378–383. [Google Scholar] [CrossRef]
- Giannetti, L.; Murri Dello Diago, A.; Corciolani, E.; Spinas, E. Deep infiltration for the treatment of hypomineralized enamel lesions in a patient with molar incisor hypomineralization: A clinical case. J. Biol. Regul. Homeost. Agents 2018, 32, 751–754. [Google Scholar]
- Giannetti, L.; Murri Dello Diago, A.; Silingardi, G.; Spinas, E. Superficial infiltration to treat white hypomineralized defects of enamel: Clinical trial with 12-month follow-up. J. Biol. Regul. Homeost. Agents 2018, 32, 1335–1338. [Google Scholar] [PubMed]
- Giannetti, L.; Bartoli, G.; Banchelli, F.; Spinas, E.; Murri Dello Diago, A. MIH: A survey amongst dental practitioners in Modena and Reggio Emilia districts. Dent. Cadmos 2018, 86, 172–180. [Google Scholar] [CrossRef]
- Ozgül, B.M.; Saat, S.; Sönmez, H.; Oz, F.T. Clinical evaluation of desensitizing treatment for incisor teeth affected by molar-incisor hypomineralization. J. Clin. Pediatr. Dent. 2013, 38, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Bekes, K.; Heinzelmann, K.; Lettner, S.; Schaller, H.G. Efficacy of desensitizing products containing 8% arginine and calcium carbonate for hypersensitivity relief in MIH-affected molars: An 8-week clinical study. Clin. Oral. Investig. 2017, 21, 2311–2317. [Google Scholar] [CrossRef] [Green Version]
- Lygidakis, N.A.; Wong, F.; Jälevik, B.; Vierrou, A.M.; Alaluusua, S.; Espelid, I. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH). Eur. Arch. Paediatr. Dent. 2010, 11, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Bentley, C.D.; Disney, J.A. A comparison of partial and full mouth scoring of plaque and gingivitis in oral hygiene studies. J. Clin. Periodontol. 1995, 22, 131–135. [Google Scholar] [CrossRef]
- Loe, H.; Silness, J. Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol. Scand. 1963, 21, 533–551. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, T.J.; Drake, R.B.; Naylor, J.E. The plaque control record. J. Periodontol. 1972, 43, 38. [Google Scholar] [CrossRef]
- Schiff, T.; Delgado, E.; Zhang, Y.P.; Cummins, D.; De Vizio, W.; Mateo, L.R. Clinical evaluation of the efficacy of an in-office desensitizing paste containing 8% arginine and calcium carbonate in providing instant and lasting relief of dentin hypersensitivity. Am. J. Dent. 2009, 22, 8a–15a. [Google Scholar] [PubMed]
- Wong, D.L.; Baker, C.M. Pain in children: Comparison of assessment scales. Pediatr. Nurs. 1988, 14, 9–17. [Google Scholar] [PubMed]
- Attal, J.P.; Atlan, A.; Denis, M.; Vennat, E.; Tirlet, G. White spots on enamel: Treatment protocol by superficial or deep infiltration (part 2). Int. Orthod. 2014, 12, 1–31. [Google Scholar] [CrossRef] [Green Version]
- Jia, L.; Stawarczyk, B.; Schmidlin, P.R.; Attin, T.; Wiegand, A. Effect of caries infiltrant application on shear bond strength of different adhesive systems to sound and demineralized enamel. J. Adhes. Dent. 2012, 14, 569–574. [Google Scholar] [PubMed] [Green Version]
- Ghanim, A.; Silva, M.J.; Elfrink, M.E.C.; Lygidakis, N.A.; Marino, R.J.; Weerheijm, K.L.; Manton, D.J. Molar incisor hypomineralisation (MIH) training manualfor clinical field surveys and practice. Eur. Arch. Paediatr. Dent. 2017, 18, 225–242. [Google Scholar] [CrossRef]
- Restrepo, M.; Jeremias, F.; Santos-Pinto, L.; Cordeiro, R.C.; Zuanon, A.C. Effect of Fluoride Varnish on Enamel Remineralization in Anterior Teeth with Molar Incisor Hypomineralization. J. Clin. Pediatr. Dent. 2016, 40, 207–210. [Google Scholar] [CrossRef]
- Mastroberardino, S.; Campus, G.; Strohmenger, L.; Villa, A.; Cagetti, M.G. An Innovative Approach to Treat Incisors Hypomineralization (MIH): A Combined Use of Casein Phosphopeptide- Amorphous Calcium Phosphate and Hydrogen Peroxide-A Case Report. Case Rep. Dent. 2012, 2012, 379593. [Google Scholar] [CrossRef] [PubMed]
- Pasini, M.; Giuca, M.R.; Scatena, M.; Gatto, R.; Caruso, S. Molar incisor hypomineralization treatment with casein phosphopeptide and amorphous calcium phosphate in children. Minerva Stomatol. 2018, 67, 20–25. [Google Scholar] [PubMed]
- Paris, S.; Schwendicke, F.; Seddig, S.; Müller, W.D.; Dörfer, C.; Meyer-Lueckel, H. Micro-hardness and mineral loss of enamel lesions after infiltration with various resins: Influence of infiltrant composition and application frequency in vitro. J. Dent. 2013, 41, 543–548. [Google Scholar] [CrossRef]
- Taher, N.M.; Alkhamis, H.A.; Dowaidi, S.M. The influence of resin infiltration system on enamel microhardness and surface roughness: An in vitro study. Saudi Dent. J. 2012, 24, 79–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Etiology Causes | |
|---|---|
| Born prematurely/problem during childbirth | 76% |
| Fluoride intake | 13% |
| Asthma | 28.60% |
| Bronchitis | 33.40% |
| Pneumonia | 15% |
| Respiratory tract infections | 31.90% |
| Celiac disease | 26% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murri Dello Diago, A.; Cadenaro, M.; Ricchiuto, R.; Banchelli, F.; Spinas, E.; Checchi, V.; Giannetti, L. Hypersensitivity in Molar Incisor Hypomineralization: Superficial Infiltration Treatment. Appl. Sci. 2021, 11, 1823. https://doi.org/10.3390/app11041823
Murri Dello Diago A, Cadenaro M, Ricchiuto R, Banchelli F, Spinas E, Checchi V, Giannetti L. Hypersensitivity in Molar Incisor Hypomineralization: Superficial Infiltration Treatment. Applied Sciences. 2021; 11(4):1823. https://doi.org/10.3390/app11041823
Chicago/Turabian StyleMurri Dello Diago, Alberto, Milena Cadenaro, Rossana Ricchiuto, Federico Banchelli, Enrico Spinas, Vittorio Checchi, and Luca Giannetti. 2021. "Hypersensitivity in Molar Incisor Hypomineralization: Superficial Infiltration Treatment" Applied Sciences 11, no. 4: 1823. https://doi.org/10.3390/app11041823
APA StyleMurri Dello Diago, A., Cadenaro, M., Ricchiuto, R., Banchelli, F., Spinas, E., Checchi, V., & Giannetti, L. (2021). Hypersensitivity in Molar Incisor Hypomineralization: Superficial Infiltration Treatment. Applied Sciences, 11(4), 1823. https://doi.org/10.3390/app11041823








