Sinus Floor Augmentation—Associated Surgical Ciliated Cysts: Case Series and a Systematic Review of the Literature
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria for Selecting Studies and Cases in the Systematic Review
- SuCC was diagnosed after the sinus floor augmentation procedure, based on a clinical and radiographic evaluation;
- Absence of clinical and/or radiographic evidence of any antral pathology at the time of the sinus floor augmentation procedure;
- SuCC was confirmed by microscopic evaluation.
2.2. Exclusion Criteria of Studies from the Systematic Literature Search
2.3. Search Methods for Detection of Studies for the Systematic Review
2.4. Data Collection and Analysis for the Systematic Review
3. Results
3.1. Case Description
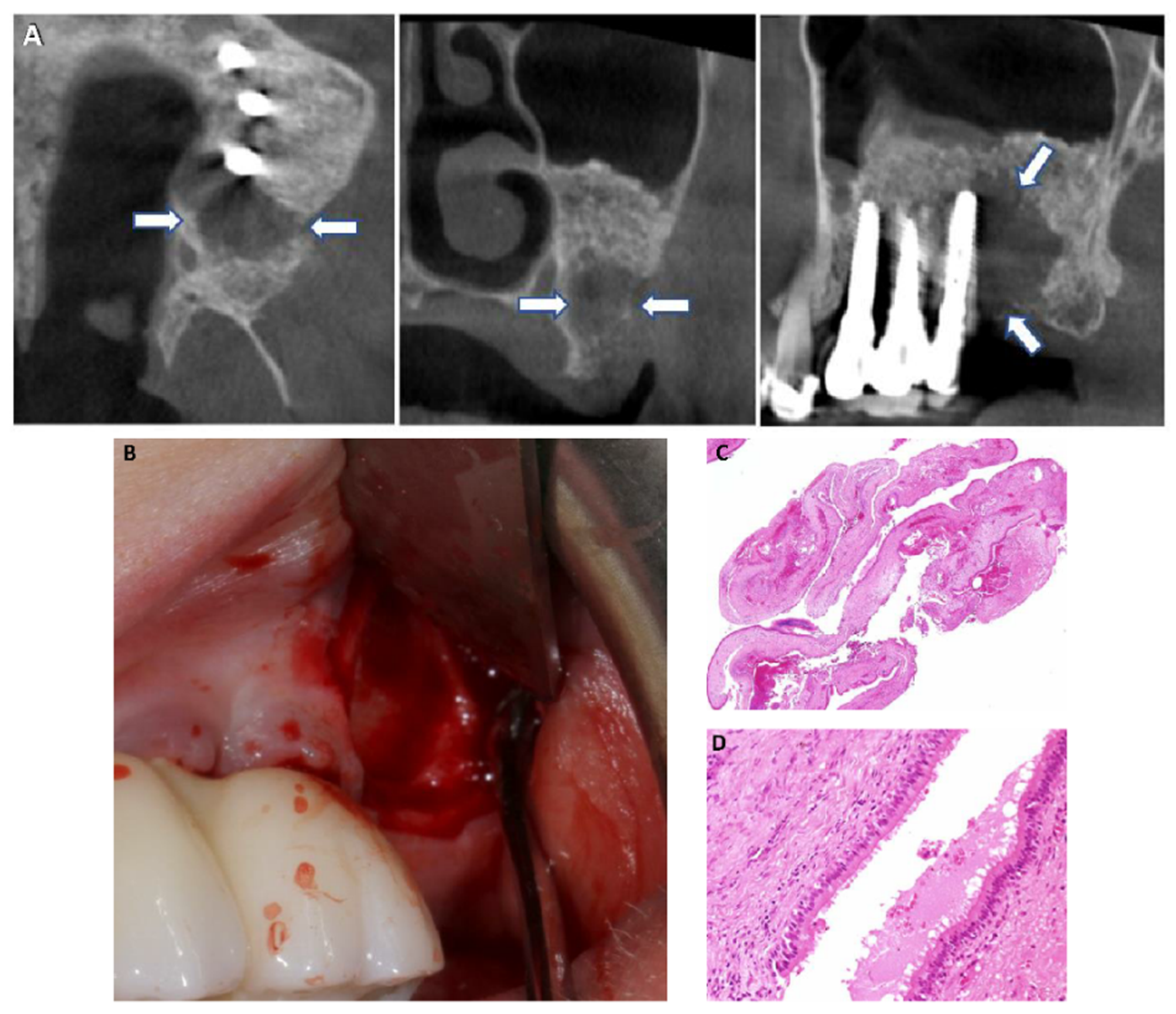
3.1.1. Case 1
3.1.2. Case 2
3.1.3. Case 3
3.1.4. Case 4
3.2. Results of the Systematic Review
3.3. Results of the Case Series—Our New Cases and Cases from the Literature Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nishioka, M.; Pittella, F.; Hamagaki, M.; Okada, N.; Takagi, M. Prevalence of postoperative maxillary cyst significantly higher in Japan. Oral. Med. Pathol. 2005, 10, 9–13. [Google Scholar] [CrossRef]
- Bourgeois, S.L., Jr.; Nelson, B.L. Surgical ciliated cyst of the mandible secondary to simultaneous Le Fort I osteotomy and genioplasty: Report of case and review of the literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 100, 36–39. [Google Scholar] [CrossRef]
- An, J.; Zhang, Y. Surgical ciliated cyst of the medial canthal region after the management of a midfacial fracture: A case report. J. Craniofac. Surg. 2014, 25, 701–702. [Google Scholar] [CrossRef]
- Misch, C.M.; Misch, C.E.; Resnik, R.R.; Ismail, Y.H.; Appel, B. Post-operative maxillary cyst associated with a maxillary sinus elevation procedure: A case report. J. Oral Implantol. 1991, 17, 432–437. [Google Scholar] [PubMed]
- Shear, M.; Speight, P.M. (Eds.) Cysts of the Oral and Maxillofacial Regions, 4th ed.; Blackwell Munksgaard: Singapore, 2007; pp. 167–170. [Google Scholar]
- Leung, Y.Y.; Wong, W.Y.; Cheung, L.K. Surgical ciliated cysts may mimic radicular cysts or residual cysts of maxilla: Report of 3 cases. J. Oral Maxillofac. Surg. 2012, 70, e264–e269. [Google Scholar] [CrossRef] [PubMed]
- Gutmann, J.L. Evidence-Based/Guest Editorial. J. Endod. 2009, 35, 1093. [Google Scholar] [CrossRef] [PubMed]
- Mileman, P.A.; Van den Hout, W.B. Evidence-based diagnosis and clinical decision making. Dentomaxillofac. Radiol. 2009, 38, 1–10. [Google Scholar] [CrossRef]
- Rosenberg, W.; Donald, A. Evidence based medicine: An approach to clinical problem-solving. BMJ 1995, 310, 1122–1126. [Google Scholar] [CrossRef]
- Sutherland, S.E.; Matthews, D.C. Conducting systematic reviews and creating clinical practice guidelines in dentistry: Lessons learned. JADA 2004, 135, 747–753. [Google Scholar] [PubMed]
- ICH GCP. ICH Harmonised Guideline Integrated Addendum to ICH E6(R1): Guideline for Good Clinical Practice ICH E6(R2) ICH Consensus Guideline. Available online: https://ichgcp.net/ (accessed on 20 May 2020).
- PRISMA Guidelines. Available online: http://www.prisma-statement.org (accessed on 1 December 2020).
- Han, Y.S. Postoperative maxillary cyst developing after sinus augmentation for dental implants: A rare case report. Implant Dent. 2018, 27, 260–263. [Google Scholar] [CrossRef]
- Kim, J.J.; Freire, M.; Yoon, J.H.; Kim, H.K. Postoperative maxillary cyst after maxillary sinus augmentation. J. Craniofac. Surg. 2013, 24, e521–e522. [Google Scholar] [CrossRef]
- Yamamoto, S.; Maeda, K.; Kouchi, I.; Hirai, Y.; Taniike, N.; Imai, Y.; Takenobu, T. Surgical ciliated cyst following maxillary sinus floor augmentation: A case report. J. Oral Implantol. 2017, 43, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, R.; Ceccaldi, J.; Bertrand, J.C. Postoperative maxillary cyst following sinus bone graft: Report of a case. Int. J. Oral Maxillofac. Implants 2000, 15, 583–586. [Google Scholar]
- Danesh-Sani, S.A.; Loomer, P.M.; Wallace, S.S. A comprehensive clinical review of maxillary sinus floor elevation: Anatomy, techniques, biomaterials and complications. Br. J. Oral Maxillofac. Surg. 2016, 54, 724–730. [Google Scholar] [CrossRef]
- Starch-Jensen, T.; Jensen, J.D. Maxillary Sinus floor augmentation: A review of selected treatment modalities. J. Oral Maxillofac. Res. 2017, 8, e3. [Google Scholar] [CrossRef]
- Boffano, P.; Forouzanfar, T. Current concepts on complications associated with sinus augmentation procedures. J. Craniofac. Surg. 2014, 25, 210–212. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Cholakis, A.K.; Piattelli, A. Histologic evaluation of sinus grafting materials after peri-implantitis-induced failure: A case series. Int. J. Oral Maxillofac. Implants 2017, 32, e69–e75. [Google Scholar] [CrossRef] [PubMed]
- Kubo, I. A buccal cyst occurred after a radical operation of the maxillary sinus. JAP J. Otolaryngol. 1927, 33, 896. [Google Scholar]
- Gregory, G.T.; Shafer, W.G. Surgical ciliated cysts of the maxilla: Report of cases. J. Oral Surg. 1958, 16, 251–253. [Google Scholar]
- Basu, M.K.; Rout, P.G.; Rippin, J.W.; Smith, A.J. The post-operative maxillary cyst. Experience with 23 cases. Int. J. Oral Maxillofac. Surg. 1988, 17, 282–284. [Google Scholar] [CrossRef]
- Sugar, A.W.; Walker, D.M.; Bounds, G.A. Surgical ciliated (postoperative maxillary) cysts following mid-face osteotomies. Br. J. Oral Maxillofac. Surg. 1990, 28, 264–267. [Google Scholar] [CrossRef]
- Cai, M.; Shen, G.; Lu, X.; Wang, X. Two mandibular surgical ciliated cysts after Le Fort I osteotomy and genioplasty. Br. J. Oral Maxillofac. Surg. 2015, 53, 1040–1042. [Google Scholar] [CrossRef] [PubMed]
- Gardner, D.G.; Gullane, P.G. Mucoceles of the maxillary sinus. Oral Surg. Oral Med. Oral Pathol. 1986, 62, 538–543. [Google Scholar] [CrossRef]
- Nolan, P.J.; Freeman, K.; Kraut, R.A. Correlation between Schneiderian membrane perforation and sinus lift graft outcome: A retrospective evaluation of 359 augmented sinus. J. Oral Maxillofac. Surg. 2014, 72, 47–52. [Google Scholar] [CrossRef]
- Shlomi, B.; Horowitz, I.; Kahn, A.; Dobriyan, A.; Chaushu, G. The effect of sinus membrane perforation and repair with Lambone on the outcome of maxillary sinus floor augmentation: A radiographic assessment. Int. J. Oral Maxillofac. Implants 2004, 19, 559–562. [Google Scholar]
- Van den Bergh, J.P.; Ten Bruggenkate, C.M.; Disch, F.J.; Tuinzing, D.B. Anatomical aspects of sinus floor elevations. Clin. Oral Implants Res. 2000, 11, 256–265. [Google Scholar] [CrossRef]
- Insua, A.; Monje, A.; Chan, H.-L.; Wang, H.-L. Association of inflammatory status and maxillary sinus Schneiderian membrane thickness. Clin. Oral Investig. 2018, 22, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Anavi, Y.; Allon, D.M.; Avishai, G.; Calderon, S. Complications of maxillary sinus augmentations in a selective series of patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 34–38. [Google Scholar] [CrossRef]
- Tidwell, J.K.; Blijdorp, P.A.; Stoelinga, P.J.; Brouns, J.B.; Hinderks, F. Composite grafting of the maxillary sinus for placement of endosteal implants. A preliminary report of 48 patients. Int. J. Oral Maxillofac. Surg. 1992, 21, 204–209. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Timmenga, N.M.; Reintsema, H.; Stegenga, B.; Vissink, A. Maxillary bone grafting for insertion of endosseous implants: Results after 12–124 months. Clin. Oral Implants Res. 2001, 12, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Takagi, M. Clinicopathologic study of the postoperative maxillary cyst. Oral Surg. Oral Med. Oral Pathol. 1986, 62, 544–548. [Google Scholar] [CrossRef]
- Kaneshiro, S.; Nakajuma, T.; Yoshikawa, Y.; Iwasaki, H.; Tokiwa, N. The postoperative maxillary cyst: Report of 71 cases. J. Oral Surg. 1981, 39, 191–198. [Google Scholar] [PubMed]
- Adachi, M.; Miyata, Y.; Ito, Y. Mid-face deformity secondary to a traumatic haemorrhage in a maxillary cyst. Surg. Case Rep. 2016, 2016, rjw013. [Google Scholar] [CrossRef][Green Version]
- Siwach, P.; Joy, T.; Gaikwad, S.; Meshram, V. Postoperative maxillary cyst. Indian J. Dent. Res. 2020, 31, 157–159. [Google Scholar] [CrossRef] [PubMed]


| Case # | Age at Diagnosis (Years) | Sex | Side of Maxillary Sinus | Graft Material | No. of Implants Placed/mo. after Augmentation | Cyst Diagnosis (Years after Augmentation) | Cyst Dimension (Largest Diameter) |
|---|---|---|---|---|---|---|---|
| Present case #1 | 54 | F | Left | Allograft, bovine bone mineral | 3 implants/9 mo. | 2 | 1 cm |
| Present case #2 | 70 | M | Right | Bovine bone mineral | 2 implants/24 mo. | 2 | 1.5 cm |
| Present case #3 | 61 | M | Right | Allograft | 2 implants/6 mo. | 0.9 | 1.5 cm |
| Present cases #4–5 | 46 | F | Bilateral | Bovine bone mineral | 8 implants/ | 2 | 1 cm, 1.5 cm |
| simultaneous | 2 |
| Case # | Authors | Country | Age at Diagnosis (Years) | Sex | Side of Maxillary Sinus | Graft Material | No. of Implants Placed/mo. after Augmentation | Diagnosis (Years after Augmentation) | Cyst Dimension (Largest Diameter) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Misch et al., 1991 [4] | USA | 76 | F | Right | No information | 1 blade implant/simultaneous | 3 | 1 cm |
| 2 | Lockhart et al., 2000 [16] | France | 41 | F | Left | Autogenous bone | No information | 0.5 | 1 cm |
| 3 | Kim et al., 2013 [14] | South Korea | 60 | M | Right | Autogenous bone | 5 implants/5 mo. | 10 | No information |
| 4 | Yamamoto et al., 2017 [15] | Japan | 64 | F | Left | Tricalcium phosphate, hydroxyapatite, | 4 implants/6 mo. | 9 | No information |
| autogenous bone | |||||||||
| 5 | Han, 2018 [13] | South Korea | 63 | M | Left | Allograft, autogenous bone, collagen | 2 implants/simultaneous | 5 | 4.5 cm |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kahn, A.; Matalon, S.; Salem, R.B.; Kats, L.; Chaushu, L.; Vered, M.; Rosen, E. Sinus Floor Augmentation—Associated Surgical Ciliated Cysts: Case Series and a Systematic Review of the Literature. Appl. Sci. 2021, 11, 1903. https://doi.org/10.3390/app11041903
Kahn A, Matalon S, Salem RB, Kats L, Chaushu L, Vered M, Rosen E. Sinus Floor Augmentation—Associated Surgical Ciliated Cysts: Case Series and a Systematic Review of the Literature. Applied Sciences. 2021; 11(4):1903. https://doi.org/10.3390/app11041903
Chicago/Turabian StyleKahn, Adrian, Shlomo Matalon, Rahaf Bassam Salem, Lazar Kats, Liat Chaushu, Marilena Vered, and Eyal Rosen. 2021. "Sinus Floor Augmentation—Associated Surgical Ciliated Cysts: Case Series and a Systematic Review of the Literature" Applied Sciences 11, no. 4: 1903. https://doi.org/10.3390/app11041903
APA StyleKahn, A., Matalon, S., Salem, R. B., Kats, L., Chaushu, L., Vered, M., & Rosen, E. (2021). Sinus Floor Augmentation—Associated Surgical Ciliated Cysts: Case Series and a Systematic Review of the Literature. Applied Sciences, 11(4), 1903. https://doi.org/10.3390/app11041903








