The Medical Outcomes Distribution and the Interpretation of Clinical Data Based on C4.5 Algorithm for the RCC Patients in Taiwan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Measurements
2.3. Statistical Analysis
C4.5 Decision Tree Algorithm and Performance Evaluation
- Precision (positive predictive value (PPV)): ;
- Recall (also known as sensitivity, or true positive rate (TPR)): ;
- F-measure (also known as F1 score, which is the harmonic mean of precision and recall): ;
- ROC area: A ROC area is an area under the ROC curve (AUC), one of the common evaluators for machine learning algorithms. A ROC curve is a plot of the false positive rate (x-axis) versus the true positive rate (y-axis) for a number of different candidate threshold values between 0 and 1;
- PRC area: A PRC area is the area under the PRC curve, another common performance evaluator for machine learning methods. A PRC curve is a plot of the precision (y-axis) and the recall (x-axis) for different thresholds similar to the ROC curve.
3. Results
3.1. The Medical Outcomes and Related Factors
3.1.1. The Description of the Sample Data
3.1.2. The Inferential Statistical Outcomes
3.1.3. C4.5 Decision Tree Algorithm
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bach, P.B.; Carson, S.S.; Leff, A. Outcomes and resource utilization for patients with prolonged critical illness managed by university-based or community-based subspecialists. Am. J. Respir. Crit. Care Med. 1998, 158, 1410–1415. [Google Scholar] [CrossRef]
- Wu, Y.; Kao, K.; Hsu, K.; Hsieh, M.; Tsai, Y. Predictors of successful weaning from prolonged mechanical ventilation in Taiwan. Respir. Med. 2009, 103, 1189. [Google Scholar] [CrossRef] [Green Version]
- Su, J.; Lin, C.-Y.; Chen, P.-J.; Lin, F.J.; Chen, S.-K.; Kuo, H.-T. Experience with a step-down respiratory care center at a tertiary referral medical center in Taiwan. J. Crit. Care 2006, 21, 156–161. [Google Scholar] [CrossRef]
- Yang, P.-H.; Hung, J.-Y.; Yang, C.-J.; Tsai, J.-R.; Wang, T.-H.; Lee, J.-C.; Huang, M.-S. Successful weaning predictors in a respiratory care center in Taiwan. Kaohsiung J. Med. Sci. 2008, 24, 85–91. [Google Scholar] [CrossRef] [Green Version]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- Naved, S.A.; Siddiqui, S.; Khan, F.H. APACHE-II score correlation with mortality and length of stay in an intensive care unit. J. Coll. Physicians Surg. Pak. 2011, 21, 4. [Google Scholar]
- Akinnusi, M.E.; Pineda, L.A.; El Solh, A.A. Effect of obesity on intensive care morbidity and mortality: A meta-analysis. Crit. Care Med. 2008, 36, 151–158. [Google Scholar] [CrossRef] [Green Version]
- Oliveros, H.; Villamor, E. Obesity and mortality in critically ill adults: A systematic review and meta-analysis. Obesity 2008, 16, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Hogue, C.W.; Stearns, J.D.; Colantuoni, E.; Robinson, K.A.; Stierer, T.; Mitter, N.; Pronovost, P.J.; Needham, D.M. The impact of obesity on outcomes after critical illness: A meta-analysis. Intensive Care Med. 2009, 35, 1152. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.M.; Welsh, C.H.; Fish, R.H.; Ancukiewicz, M.; Kramer, A.M. Excess body weight is not independently associated with outcome in mechanically ventilated patients with acute lung injury. Ann. Intern. Med. 2004, 140, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Flabouris, A. Patient referral and transportation to a regional tertiary ICU: Patient demographics, severity of illness and outcome comparison with non-transported patients. Anaesth. Intensive Care 1999, 27, 385. [Google Scholar] [CrossRef] [PubMed]
- Gerber, D.R.; Schorr, C.; Ahmed, I.; Dellinger, R.P.; Parrillo, J. Location of patients before transfer to a tertiary care intensive care unit: Impact on outcome. J. Crit. Care 2009, 24, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Dermot Frengley, J.; Sansone, G.R.; Shakya, K.; Kaner, R.J. Prolonged mechanical ventilation in 540 seriously ill older adults: Effects of increasing age on clinical outcomes and survival. J. Am. Geriatr. Soc. 2014, 62, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Huang, C. How prolonged mechanical ventilation is a neglected disease in chest medicine: A study of prolonged mechanical ventilation based on 6 years of experience in Taiwan. Ther. Adv. Respir. Dis. 2019, 13, 1753466619878552. [Google Scholar] [CrossRef] [PubMed]
- Lamy, J.-B.; Ellini, A.; Ebrahiminia, V.; Zucker, J.-D.; Falcoff, H.; Venot, A. Use of the C4.5 machine learning algorithm to test a clinical guideline-based decision support system. Stud. Health Technol. Inform. 2008, 136, 223. [Google Scholar]
- Khaleel, A.H.; Al-Suhai, G.A.; Hussan, B.M. Application Tool based on C4. 5 Decision Tree for Diagnosing Diabetes Infection Symptoms. J. Commun. Technol. Electron. Comput. Sci. 2019, 22, 7–15. [Google Scholar]
- Ramani, R.G.; Sivagami, G. Parkinson disease classification using data mining algorithms. Int. J. Comput. Appl. 2011, 32, 17–22. [Google Scholar]
- Sa’Di, S.; Maleki, A.; Hashemi, R.; Panbechi, Z.; Chalabi, K. Comparison of data mining algorithms in the diagnosis of type II diabetes. Int. J. Comput. Sci. Appl. (IJCSA) 2015, 5, 1–12. [Google Scholar] [CrossRef]
- Wiharto, W.; Kusnanto, H.; Herianto, H. Interpretation of clinical data based on C4. 5 algorithm for the diagnosis of coronary heart disease. Healthc. Inform. Res. 2016, 22, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Quinlan, J.R. C4.5: Programs for Machine Learning; Morgan Kaufmann Publishers: Boston, MA, USA, 1993. [Google Scholar]
- Witten, I.H.; Frank, E.; Hall, M.A. Data Mining: Practical Machine Learning Tools and Techniques, 3rd ed.; Morgan Kaufmann: San Francisco, CA, USA, 2011; p. 191. [Google Scholar]
- Mancuso, P. Obesity and lung inflammation. J. Appl. Physiol. 2010, 108, 722–728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, C.V.; Neville, A.L.; Rhee, P.; Salim, A.; Velmahos, G.C.; Demetriades, D. The impact of obesity on the outcomes of 1153 critically injured blunt trauma patients. J. Trauma Acute Care Surg. 2005, 59, 1048–1051. [Google Scholar] [CrossRef]
- Ciesla, D.J.; Moore, E.E.; Johnson, J.L.; Burch, J.M.; Cothren, C.C.; Sauaia, A. Obesity increases risk of organ failure after severe trauma. J. Am. Coll. Surg. 2006, 203, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Neville, A.L.; Brown, C.V.; Weng, J.; Demetriades, D.; Velmahos, G.C. Obesity is an independent risk factor of mortality in severely injured blunt trauma patients. Arch. Surg. 2004, 139, 983–987. [Google Scholar] [CrossRef] [Green Version]
- Gupta, R.; Knobel, D.; Gunabushanam, V.; Agaba, E.; Ritter, G.; Marini, C.; Barrera, R. The effect of low body mass index on outcome in critically ill surgical patients. Nutr. Clin. Pract. 2011, 26, 593–597. [Google Scholar] [CrossRef] [PubMed]
- Pickkers, P.; de Keizer, N.; Dusseljee, J.; Weerheijm, D.; van der Hoeven, J.G.; Peek, N. Body mass index is associated with hospital mortality in critically ill patients: An observational cohort study. Crit. Care Med. 2013, 41, 1878–1883. [Google Scholar] [CrossRef] [PubMed]
- Donnino, M.W.; Salciccioli, J.D.; Dejam, A.; Giberson, T.; Giberson, B.; Cristia, C.; Gautam, S.; Cocchi, M.N. APACHE II scoring to predict outcome in post-cardiac arrest. Resuscitation 2013, 84, 651–656. [Google Scholar] [CrossRef] [Green Version]
- Johnson, C.; Toh, S.; Campbell, M. Combination of APACHE-II score and an obesity score (APACHE-O) for the prediction of severe acute pancreatitis. Pancreatology 2004, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Syed, S.T.; Gerber, B.S.; Sharp, L.K. Traveling towards disease: Transportation barriers to health care access. J. Community Health 2013, 38, 976–993. [Google Scholar] [CrossRef] [Green Version]
- Schönhofer, B.; Euteneuer, S.; Nava, S.; Suchi, S.; Köhler, D. Survival of mechanically ventilated patients admitted to a specialised weaning centre. Intensive Care Med. 2002, 28, 908–916. [Google Scholar] [CrossRef]


| n | % | |
|---|---|---|
| Gender | ||
| Female | 101 | 42.8 |
| Male | 135 | 57.2 |
| Age | mean ± SD = 74.1 ± 14.6 | |
| ≤64 | 50 | 21.2 |
| 65–74 | 47 | 19.9 |
| 75–84 | 78 | 33.1 |
| ≥85 | 61 | 25.8 |
| BMI | ||
| Under weight (<18.5) | 49 | 20.9 |
| Normal weight (18.5–23.9) | 111 | 47.2 |
| Over weight (24.0–26.9) | 41 | 17.4 |
| Obese (≥27.0) | 34 | 14.5 |
| Source of admission | ||
| Home | 129 | 54.7 |
| Long-term care institution | 107 | 45.3 |
| APACHE II scores | mean ± SD = 24.58 ± 7.70 | |
| <15 | 64 | 27.8 |
| 15–24 | 115 | 50.0 |
| ≥25 | 51 | 22.2 |
| Main Diagnosis | ||
| Cancer | 24 | 10.2 |
| Cardiac disease | 66 | 28.0 |
| Pneumonia | 41 | 17.4 |
| Cerebrovascular accident | 61 | 25.8 |
| Diabetes | 98 | 41.5 |
| Lower respiratory illnesses | 25 | 10.6 |
| Hypertension | 152 | 64.4 |
| CKD | 42 | 17.8 |
| Liver disease | 15 | 6.4 |
| Dementia | 26 | 11.0 |
| Parkinson’s disease | 13 | 5.5 |
| Miscellaneous | 24 | 10.2 |
| Medical Outcomes | ||
| Critical or deceased | 61 | 25.8 |
| RCW | 62 | 26.3 |
| Weaning | 113 | 47.9 |
| Total | 236 | 100.0 |
| Medical Outcome | |||||
|---|---|---|---|---|---|
| n (%) | p Value | ||||
| Critical or Deceased | RCW | Weaning | Total | ||
| Gender | 0.486 | ||||
| Female | 30 (29.7) | 26 (25.7) | 45 (44.6) | 101 (100) | |
| Male | 31 (23.0) | 36 (26.7) | 68 (50.4) | 135 (100) | |
| Age | 0.102 | ||||
| ≤64 | 10 (20.0) | 11 (22.0) | 29 (58.0) | 50 (100) | |
| 65–74 | 13 (27.7) | 6 (12.8) | 28 (59.6) | 47 (100) | |
| 75–84 | 21 (26.9) | 26 (33.3) | 31 (39.7) | 78 (100) | |
| ≥85 | 17 (27.9) | 19 (31.1) | 25 (41.0) | 61 (100) | |
| BMI * | 0.006 | ||||
| Under weight | 13 (26.5) | 12 (24.5) | 24 (49.0) | 49 (100) | |
| Normal weight | 17 (15.3) | 37 (33.3) | 57 (51.4) | 111 (100) | |
| Over weight | 15 (36.6) | 8 (19.5) | 18 (43.9) | 41 (100) | |
| Fatty | 16 (47.1) | 5 (14.7) | 13 (38.2) | 34 (100) | |
| Source of admission * | 0.011 | ||||
| Home | 43 (33.3) | 33 (25.6) | 53 (41.1) | 129 (100) | |
| Long-term care institution | 18 (16.8) | 29 (27.1) | 60 (56.1) | 107 (100) | |
| APACHE II scores * | 0.028 | ||||
| <15 | 11 (17.2) | 17 (26.6) | 36 (56.3) | 64 (100) | |
| 15–24 | 24 (20.9) | 33 (28.7) | 58 (50.4) | 115 (100) | |
| ≥25 | 21 (41.2) | 12 (23.5) | 18 (35.3) | 51 (100) | |
| Cancer | 0.364 | ||||
| Yes | 9 (37.5) | 6 (25.0) | 9 (37.5) | 24 (100) | |
| No | 52 (24.5) | 56 (26.4) | 104 (49.1) | 212 (100) | |
| Cardiac disease | 0.158 | ||||
| Yes | 20 (30.3) | 21 (31.8) | 25 (37.9) | 66 (100) | |
| No | 41 (24.1) | 41 (24.1) | 88 (51.8) | 170 (100) | |
| Pneumonia | 0.512 | ||||
| Yes | 8 (19.5) | 13 (31.7) | 20 (48.8) | 41 (100) | |
| No | 53 (27.2) | 49 (25.1) | 93 (47.7) | 195 (100) | |
| CVA | 0.812 | ||||
| Yes | 14 (23.0) | 16 (26.2) | 31 (50.8) | 61 (100) | |
| No | 47 (26.9) | 46 (26.3) | 82 (46.9) | 175 (100) | |
| Diabetes * | 0.023 | ||||
| Yes | 28 (28.6) | 33 (33.7) | 37 (37.8) | 98 (100) | |
| No | 33 (23.9) | 29 (21.0) | 76 (55.1) | 138 (100) | |
| Lower respiratory illnesses | 0.375 | ||||
| Yes | 4 (16.0) | 6 (24.0) | 15 (60.0) | 25 (100) | |
| No | 57 (27.0) | 56 (26.5) | 98 (46.4) | 211 (100) | |
| Hypertension | 0.051 | ||||
| Yes | 45 (29.6) | 43 (28.3) | 64 (42.1) | 152 (100) | |
| No | 16 (19.0) | 19 (22.6) | 49 (58.3) | 84 (100) | |
| CKD | 0.211 | ||||
| Yes | 14 (33.3) | 13 (31.0) | 15 (35.7) | 42 (100) | |
| No | 47 (24.2) | 49 (25.3) | 98 (50.5) | 194 (100) | |
| Liver disease | 0.171 | ||||
| Yes | 4 (26.7) | 1 (6.7) | 10 (66.7) | 15 (100) | |
| No | 57 (25.8) | 61 (27.6) | 103 (46.6) | 221 (100) | |
| Dementia | 0.591 | ||||
| Yes | 6 (23.1) | 9 (34.6) | 11 (42.3) | 26 (100) | |
| No | 55 (26.2) | 53 (25.2) | 102 (48.6) | 210 (100) | |
| Parkinson’s disease | 0.088 | ||||
| Yes | 0 (0) | 5 (38.5) | 8 (61.5) | 13 (100) | |
| No | 61 (27.4) | 57 (25.6) | 105 (47.7) | 223 (100) | |
| Miscellaneous | 0.364 | ||||
| Yes | 9 (37.5) | 6 (25.0) | 9 (37.5) | 24 (100) | |
| No | 52 (24.5) | 56 (26.4) | 104 (49.1) | 212 (100) | |
| OR | 95% C.I. | p Value | |
|---|---|---|---|
| Medical Outcomes | |||
| Critical or deceased | Reference | ||
| RCW | 8.092 | 4.092–16.000 | <0.001 |
| Weaning | 2.200 | 1.171–4.133 | 0.014 |
| Diabetes | |||
| No | Reference | ||
| Yes | 0.622 | 0.372–1.044 | 0.072 |
| BMI | |||
| Normal weight | Reference | ||
| Under weight | 0.779 | 0.372–1.630 | 0.507 |
| Over weight | 1.198 | 0.587–2.445 | 0.620 |
| Obese * | 2.426 | 1.106–5.318 | 0.027 |
| Source of admission | |||
| Home ** | 2.104 | 1.257–3.523 | 0.005 |
| Long-term care institution | Reference | ||
| Apache II scores | |||
| <15 | Reference | ||
| 15–24 | 0.291 | 0.758–2.524 | 0.291 |
| ≥25 ** | 2.640 | 1.283–5.433 | 0.008 |
| R2 = 0.116 | |||
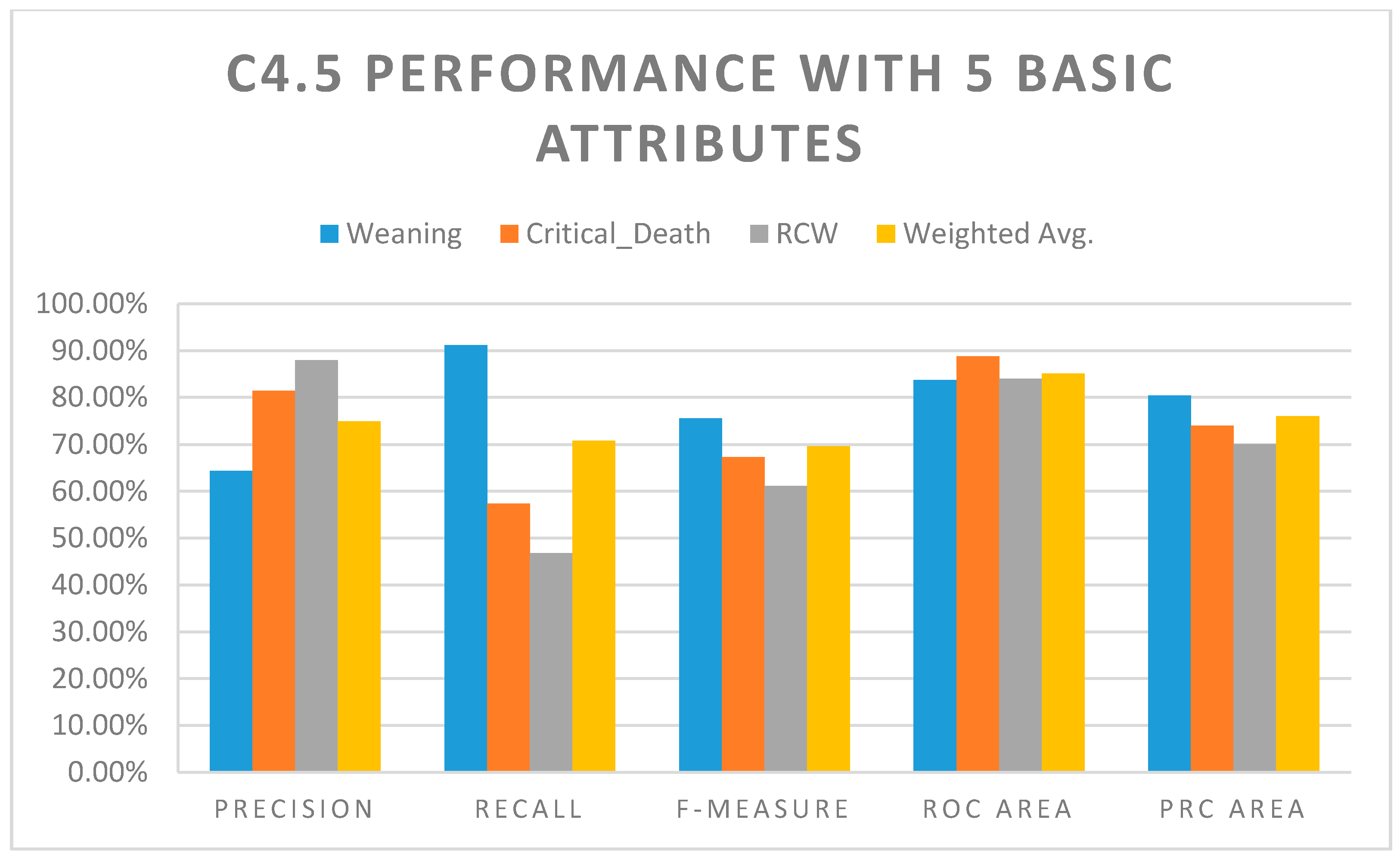
| Class | Precision | Recall | F-Measure | ROC Area | PRC Area |
|---|---|---|---|---|---|
| Weaning | 64.40% | 91.20% | 75.50% | 83.70% | 80.40% |
| Critical Death | 81.40% | 57.40% | 67.30% | 88.80% | 74.00% |
| RCW | 87.90% | 46.80% | 61.10% | 84.00% | 70.10% |
| Weighted Avg. | 74.90% | 70.80% | 69.60% | 85.10% | 76.00% |
| Class | Precision | Recall | F-Measure | ROC Area | PRC Area |
|---|---|---|---|---|---|
| Weaning | 75.50% | 92.90% | 83.30% | 88.70% | 83.60% |
| Critical Death | 86.00% | 60.70% | 71.20% | 88.90% | 78.90% |
| RCW | 81.50% | 71.00% | 75.90% | 90.60% | 81.10% |
| Weighted Avg. | 79.80% | 78.80% | 78.20% | 89.20% | 81.70% |
| Model | Precision | Recall | F-Measure | ROC Area | PRC Area |
|---|---|---|---|---|---|
| Model I (5 basic attributes) | 74.90% | 70.80% | 69.60% | 85.10% | 76.00% |
| Model II (5 basic + 12 disease attributes) | 79.80% | 78.80% | 78.20% | 89.20% | 81.70% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-C.; Liu, J.-H.; Ho, C.-S. The Medical Outcomes Distribution and the Interpretation of Clinical Data Based on C4.5 Algorithm for the RCC Patients in Taiwan. Appl. Sci. 2021, 11, 2566. https://doi.org/10.3390/app11062566
Lee H-C, Liu J-H, Ho C-S. The Medical Outcomes Distribution and the Interpretation of Clinical Data Based on C4.5 Algorithm for the RCC Patients in Taiwan. Applied Sciences. 2021; 11(6):2566. https://doi.org/10.3390/app11062566
Chicago/Turabian StyleLee, Hsi-Chieh, Ju-Hsia Liu, and Ching-Sung Ho. 2021. "The Medical Outcomes Distribution and the Interpretation of Clinical Data Based on C4.5 Algorithm for the RCC Patients in Taiwan" Applied Sciences 11, no. 6: 2566. https://doi.org/10.3390/app11062566
APA StyleLee, H.-C., Liu, J.-H., & Ho, C.-S. (2021). The Medical Outcomes Distribution and the Interpretation of Clinical Data Based on C4.5 Algorithm for the RCC Patients in Taiwan. Applied Sciences, 11(6), 2566. https://doi.org/10.3390/app11062566






