Bond Strength Stability of Different Dual-Curing Adhesive Cements towards CAD-CAM Resin Nanoceramic: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
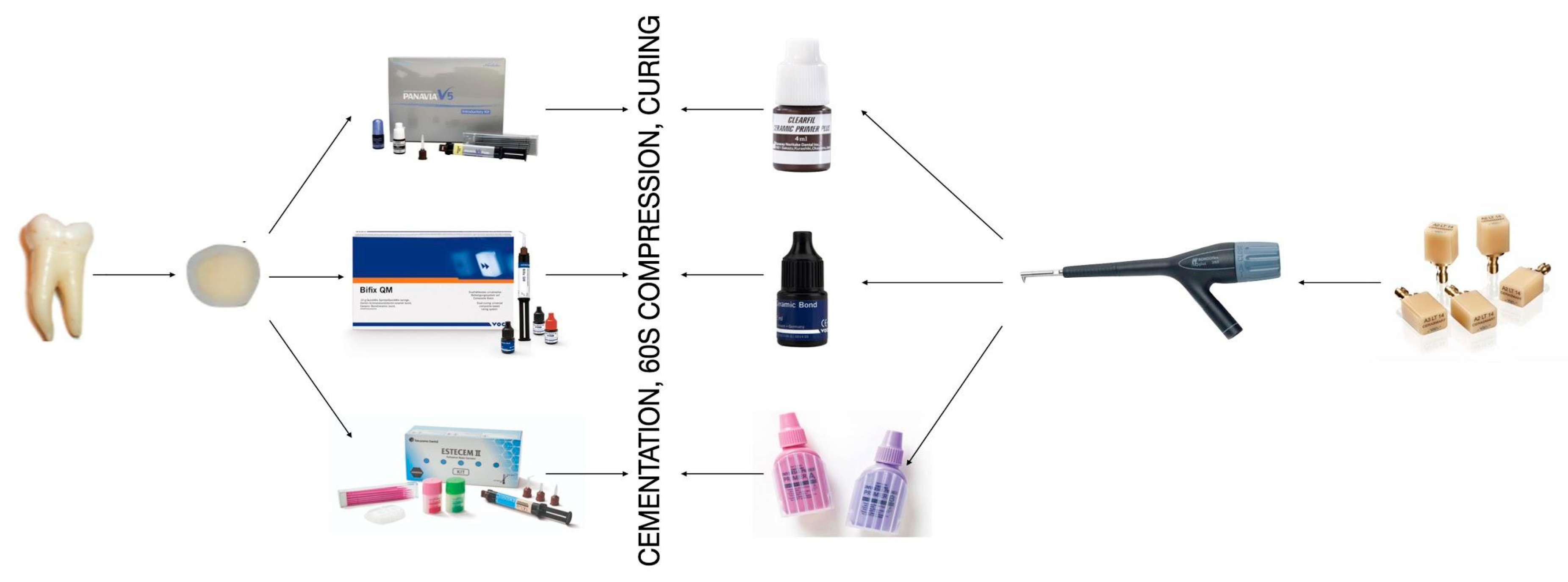
- Group 1 (G1):
- Clearfil Ceramic Primer (Kuraray) applied for 20 s with a microbrush and gently air dried.
- Group 1 (G2):
- Bifix Ceramic Bond (VOCO GmbH) applied for 20 s with a microbrush, and gently air dried.
- Group 1 (G3):
- Primer A + Primer B mixed before application in equal proportions (1:1) (Tokuyama), applied for 20 s with a microbrush and gently air dried after 10 s.
- (G1)
- V5: V5 tooth primer application on the dentinal surface for 20 s, followed by gentle air dry. Application of Clearfil Universal Bond Quick dualized with a 1:1 ratio of Clearfil DC Activator (Kuraray) for 20 s and then gently air dried.
- (G2)
- QM: Application of Futurabond U (VOCO GmbH) for 20 s, then gently air dried.
- (G3)
- ES: Estelink Bond A + Estelink Bond B mixed before application in equal proportions (1:1) (Tokuyama) application for 20 s, then gently air dried.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.F.A.; Bonfante, E.A. A New Classification System for All-Ceramic and Ceramic-like Restorative Materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef] [Green Version]
- Awada, A.; Nathanson, D. Mechanical Properties of Resin-Ceramic CAD/CAM Restorative Materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef]
- Frankenberger, R.; Hartmann, V.E.; Krech, M.; Krämer, N.; Reich, S.; Braun, A.; Roggendorf, M. Adhesive Luting of New CAD/CAM Materials. Int. J. Comput. Dent. 2015, 18, 9–20. [Google Scholar] [PubMed]
- Sjögren, G.; Molin, M.; van Dijken, J.W.V. A 10-Year Prospective Evaluation of CAD/CAM-Manufactured (Cerec) Ceramic Inlays Cemented with a Chemically Cured or Dual-Cured Resin Composite. Int. J. Prosthodont. 2004, 17, 241–246. [Google Scholar]
- Vrochari, A.D.; Eliades, G.; Hellwig, E.; Wrbas, K.-T. Curing Efficiency of Four Self-Etching, Self-Adhesive Resin Cements. Dent. Mater. 2009, 25, 1104–1108. [Google Scholar] [CrossRef]
- Scotti, N.; Comba, A.; Cadenaro, M.; Fontanive, L.; Breschi, L.; Monaco, C.; Scotti, R. Effect of Lithium Disilicate Veneers of Different Thickness on the Degree of Conversion and Microhardness of a Light-Curing and a Dual-Curing Cement. Int. J. Prosthodont. 2016, 29, 384–388. [Google Scholar] [CrossRef] [Green Version]
- Caughman, W.F.; Chan, D.C.; Rueggeberg, F.A. Curing Potential of Dual-Polymerizable Resin Cements in Simulated Clinical Situations. J. Prosthet. Dent. 2001, 86, 101–106. [Google Scholar] [CrossRef]
- Khoroushi, M.; Ghasemi, M.; Abedinzadeh, R.; Samimi, P. Comparison of Immediate and Delayed Light-Curing on Nano-Indentation Creep and Contraction Stress of Dual-Cured Resin Cements. J. Mech. Behav. Biomed. Mater. 2016, 64, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L.; Stansbury, J.W.; Burke, F.J.T. Self-Adhesive Resin Cements—Chemistry, Properties and Clinical Considerations: SELF-ADHESIVE CEMENTS. J. Oral Rehabil. 2011, 38, 295–314. [Google Scholar] [CrossRef] [PubMed]
- Furuichi, T.; Takamizawa, T.; Tsujimoto, A.; Miyazaki, M.; Barkmeier, W.; Latta, M. Mechanical Properties and Sliding-Impact Wear Resistance of Self-Adhesive Resin Cements. Oper. Dent. 2016, 41, E83–E92. [Google Scholar] [CrossRef] [Green Version]
- Betancourt, D.E.; Baldion, P.A.; Castellanos, J.E. Resin-Dentin Bonding Interface: Mechanisms of Degradation and Strategies for Stabilization of the Hybrid Layer. Int. J. Biomater. 2019, 2019, 5268342. [Google Scholar] [CrossRef] [PubMed]
- Breschi, L.; Maravic, T.; Cunha, S.R.; Comba, A.; Cadenaro, M.; Tjäderhane, L.; Pashley, D.H.; Tay, F.R.; Mazzoni, A. Dentin Bonding Systems: From Dentin Collagen Structure to Bond Preservation and Clinical Applications. Dent. Mater. 2018, 34, 78–96. [Google Scholar] [CrossRef] [Green Version]
- Scotti, N.; Cavalli, G.; Gagliani, M.; Breschi, L. New Adhesives and Bonding Techniques. Why and When? Int. J. Aesthetic Dent. 2017, 12, 524–535. [Google Scholar]
- da Rosa, W.L.; Piva, E.; da Silva, A.F. Bond Strength of Universal Adhesives: A Systematic Review and Meta-Analysis. J. Dent. 2015, 43, 765–776. [Google Scholar] [CrossRef]
- Yoshihara, K.; Nagaoka, N.; Sonoda, A.; Maruo, Y.; Makita, Y.; Okihara, T.; Irie, M.; Yoshida, Y.; Van Meerbeek, B. Effectiveness and Stability of Silane Coupling Agent Incorporated in ‘Universal’ Adhesives. Dent. Mater. 2016, 32, 1218–1225. [Google Scholar] [CrossRef] [Green Version]
- Sano, H.; Chowdhury, A.F.M.A.; Saikaew, P.; Matsumoto, M.; Hoshika, S.; Yamauti, M. The Microtensile Bond Strength Test: Its Historical Background and Application to Bond Testing. Jpn. Dent. Sci. Rev. 2020, 56, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Pashley, D.H.; Tay, F.R.; Yiu, C.; Hashimoto, M.; Breschi, L.; Carvalho, R.M.; Ito, S. Collagen Degradation by Host-Derived Enzymes during Aging. J. Dent. Res. 2004, 83, 216–221. [Google Scholar] [CrossRef]
- Poitevin, A.; De Munck, J.; Van Landuyt, K.; Coutinho, E.; Peumans, M.; Lambrechts, P.; Van Meerbeek, B. Influence of Three Specimen Fixation Modes on the Micro-Tensile Bond Strength of Adhesives to Dentin. Dent. Mater. J. 2007, 26, 694–699. [Google Scholar] [CrossRef] [Green Version]
- El Zohairy, A.A.; De Gee, A.J.; Mohsen, M.M.; Feilzer, A.J. Microtensile Bond Strength Testing of Luting Cements to Prefabricated CAD/CAM Ceramic and Composite Blocks. Dent. Mater. 2003, 19, 575–583. [Google Scholar] [CrossRef]
- Braga, R.R.; Meira, J.B.C.; Boaro, L.C.C.; Xavier, T.A. Adhesion to Tooth Structure: A Critical Review of “Macro” Test Methods. Dent. Mater. 2010, 26, e38–e49. [Google Scholar] [CrossRef]
- Li, J.; Li, H.; Yun, X.; Fok, A.S.L. A Comparison of Bond Strengths Measured Using Cantilever Bending and Micro-Tensile Methods. Dent. Mater. 2011, 27, 1246–1251. [Google Scholar] [CrossRef]
- Placido, E.; Meira, J.B.C.; Lima, R.G.; Muench, A.; de Souza, R.M.; Ballester, R.Y. Shear versus Micro-Shear Bond Strength Test: A Finite Element Stress Analysis. Dent. Mater. 2007, 23, 1086–1092. [Google Scholar] [CrossRef]
- Turp, V.; Sen, D.; Tuncelli, B.; Özcan, M. Adhesion of 10-MDP Containing Resin Cements to Dentin with and without the Etch-and-Rinse Technique. J. Adv. Prosthodont. 2013, 5, 226–233. [Google Scholar] [CrossRef] [Green Version]
- Yoshihara, K.; Hayakawa, S.; Nagaoka, N.; Okihara, T.; Yoshida, Y.; Van Meerbeek, B. Etching Efficacy of Self-Etching Functional Monomers. J. Dent. Res. 2018, 002203451876360. [Google Scholar] [CrossRef]
- Yoshihara, K.; Nagaoka, N.; Okihara, T.; Kuroboshi, M.; Hayakawa, S.; Maruo, Y.; Nishigawa, G.; De Munck, J.; Yoshida, Y.; Van Meerbeek, B. Functional Monomer Impurity Affects Adhesive Performance. Dent. Mater. 2015, 31, 1493–1501. [Google Scholar] [CrossRef]
- Gutiérrez, M.F.; Sutil, E.; Malaquias, P.; de Paris Matos, T.; de Souza, L.M.; Reis, A.; Perdigão, J.; Loguercio, A.D. Effect of Self-Curing Activators and Curing Protocols on Adhesive Properties of Universal Adhesives Bonded to Dual-Cured Composites. Dent. Mater. 2017, 33, 775–787. [Google Scholar] [CrossRef]
- Lührs, A.-K.; Pongprueksa, P.; De Munck, J.; Geurtsen, W.; Van Meerbeek, B. Curing Mode Affects Bond Strength of Adhesively Luted Composite CAD/CAM Restorations to Dentin. Dent. Mater. 2014, 30, 281–291. [Google Scholar] [CrossRef]
- Inokoshi, M.; Nozaki, K.; Takagaki, T.; Okazaki, Y.; Yoshihara, K.; Minakuchi, S.; Van Meerbeek, B. Initial Curing Characteristics of Composite Cements under Ceramic Restorations. J. Prosthodont. Res. 2021, 65, 39–45. [Google Scholar] [CrossRef]
- Tichy, A.; Hosaka, K.; Abdou, A.; Nakajima, M.; Tagami, J. Degree of Conversion Contributes to Dentin Bonding Durability of Contemporary Universal Adhesives. Oper. Dent. 2020, 45, 556–566. [Google Scholar] [CrossRef]
- Saboia, V.P.A.; Silva, F.C.F.A.; Nato, F.; Mazzoni, A.; Cadenaro, M.; Mazzotti, G.; Giannini, M.; Breschi, L. Analysis of Differential Artificial Ageing of the Adhesive Interface Produced by a Two-Step Etch-and-Rinse Adhesive. Eur. J. Oral Sci. 2009, 117, 618–624. [Google Scholar] [CrossRef]
- Mazzoni, A.; Angeloni, V.; Apolonio, F.M.; Scotti, N.; Tjäderhane, L.; Tezvergil-Mutluay, A.; Di Lenarda, R.; Tay, F.R.; Pashley, D.H.; Breschi, L. Effect of Carbodiimide (EDC) on the Bond Stability of Etch-and-Rinse Adhesive Systems. Dent. Mater. 2013, 29, 1040–1047. [Google Scholar] [CrossRef]
- Comba, A.; Maravić, T.; Villalta, V.; Tozzola, S.; Mazzitelli, C.; Checchi, V.; Mancuso, E.; Scotti, N.; Tay, F.R.; Breschi, L.; et al. Effect of an Ethanol Cross-Linker on Universal Adhesive. Dent. Mater. 2020, 36, 1645–1654. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, M.V.; de Almeida Neves, A.; Mine, A.; Coutinho, E.; Van Landuyt, K.; De Munck, J.; Van Meerbeek, B. Current Aspects on Bonding Effectiveness and Stability in Adhesive Dentistry. Aust Dent. J. 2011, 56 (Suppl. S1), 31–44. [Google Scholar] [CrossRef]
- Mazzoni, A.; Pashley, D.H.; Tay, F.R.; Gobbi, P.; Orsini, G.; Ruggeri, A.; Carrilho, M.; Tjäderhane, L.; Di Lenarda, R.; Breschi, L. Immunohistochemical Identification of MMP-2 and MMP-9 in Human Dentin: Correlative FEI-SEM/TEM Analysis. J. Biomed. Mater. Res. Part A 2009, 88A, 697–703. [Google Scholar] [CrossRef]
- Mazzoni, A.; Angeloni, V.; Comba, A.; Maravic, T.; Cadenaro, M.; Tezvergil-Mutluay, A.; Pashley, D.H.; Tay, F.R.; Breschi, L. Cross-Linking Effect on Dentin Bond Strength and MMPs Activity. Dent. Mater. 2018, 34, 288–295. [Google Scholar] [CrossRef]
- Nishitani, Y.; Yoshiyama, M.; Wadgaonkar, B.; Breschi, L.; Mannello, F.; Mazzoni, A.; Carvalho, R.M.; Tjaderhane, L.; Tay, F.R.; Pashley, D.H. Activation of Gelatinolytic/Collagenolytic Activity in Dentin by Self-Etching Adhesives. Eur. J. Oral Sci. 2006, 114, 160–166. [Google Scholar] [CrossRef]
- Hu, L.; Xiao, Y.; Fang, M.; Gao, Y.; Huang, L.; Jia, A.; Chen, J. Effects of Type I Collagen Degradation on the Durability of Three Adhesive Systems in the Early Phase of Dentin Bonding. PLoS ONE 2015, 10, e0116790. [Google Scholar] [CrossRef] [PubMed]
- Carrilho, M.R.O.; Geraldeli, S.; Tay, F.; de Goes, M.F.; Carvalho, R.M.; Tjäderhane, L.; Reis, A.F.; Hebling, J.; Mazzoni, A.; Breschi, L.; et al. In Vivo Preservation of the Hybrid Layer by Chlorhexidine. J. Dent. Res. 2007, 86, 529–533. [Google Scholar] [CrossRef]
- Mazzoni, A.; Scaffa, P.; Carrilho, M.; Tjäderhane, L.; Di Lenarda, R.; Polimeni, A.; Tezvergil-Mutluay, A.; Tay, F.R.; Pashley, D.H.; Breschi, L. Effects of Etch-and-Rinse and Self-Etch Adhesives on Dentin MMP-2 and MMP-9. J. Dent. Res. 2013, 92, 82–86. [Google Scholar] [CrossRef] [Green Version]
- Angeloni, V.; Scotti, N. Role of Chlorhexidine on Long-Term Bond Strength of Self-Adhesive Composite Cements to Intraradicular Dentin. J. Adhes. Dent. 2017, 19, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Aida, M.; Odaki, M.; Fujita, K.; Kitagawa, T.; Teshima, I.; Suzuki, K.; Nishiyama, N. Degradation-Stage Effect of Self-Etching Primer on Dentin Bond Durability. J. Dent. Res. 2009, 88, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Carrilho, E.; Cardoso, M.; Marques Ferreira, M.; Marto, C.; Paula, A.; Coelho, A. 10-MDP Based Dental Adhesives: Adhesive Interface Characterization and Adhesive Stability—A Systematic Review. Materials 2019, 12, 790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiraishi, N.; Tochio, N.; Kigawa, T.; Otsuki, M.; Tagami, J. Role of 2-Hydroxyethyl Methacrylate in the Interaction of Dental Monomers with Collagen Studied by Saturation Transfer Difference NMR. J. Dent. 2014, 42, 484–489. [Google Scholar] [CrossRef]
- Yoshihara, K.; Yoshida, Y.; Hayakawa, S.; Nagaoka, N.; Torii, Y.; Osaka, A.; Suzuki, K.; Minagi, S.; Van Meerbeek, B.; Van Landuyt, K.L. Self-Etch Monomer-Calcium Salt Deposition on Dentin. J. Dent. Res. 2011, 90, 602–606. [Google Scholar] [CrossRef] [PubMed]



| Materials | Label | Company | Category | Composition |
|---|---|---|---|---|
| CAD CAM Blocks | Cerasmart | GC Europe, Leuven, Belgium | Resin-based composite | Filler (71% wt): silica (20 nm) and barium-glass (300 nm) nanoparticles |
| Luting Agents | Panavia V5 Cement | Kuraray Europe GmbH, Hattersheim am Main, Germany | Dual-cured adhesive composite cement (automix syringe) | Paste A: Bis-GMA, TEGDMA, Hydrophobic aromatic dimethacrylate, Hydrophilic aliphatic dimethacrylate, Initiators, Accelerators, Silanated barium glass filler, Silanated, fluoroalminosilicate glass filler, Colloidal silica. Paste B: Bis-GMA, Hydrophobic aromatic dimethacrylate, Hydrophilic aliphatic dimethacrylate, Silanated barium glass filler, Silanated aluminum oxide filler, Accelerators, DI-Camphorquinone, Pigments |
| Clearfil Ceramic Primer Plus | Kuraray Europe GmbH, Hattersheim am Main, Germany | Silane Coupling Agent | 3-trimethoxylsilylpropyl methacrylate, MDP, Ethanol | |
| Panavia Tooth Primer | Kuraray Europe GmbH, Hattersheim am Main, Germany | Self-etching tooth primer | MDP, HEMA, Hydrophilic aliphatic dimethacrylate, Accelerators, Water | |
| Clearfil Universal Bond Quick | Kuraray Europe GmbH, Hattersheim am Main, Germany | Universal Adhesive | HEMA, bisphenol A diglycidylmethacrylate (BIS-GMA), 10-methacryloyoxydecyl dihydrogen phosphate (MDP), hydrophilic amide monomers, colloidal silica, silane, sodium fluoride, and CQ in ethanol and water | |
| Clearfil DC Activator | Kuraray Europe GmbH, Hattersheim am Main, Germany | Dual Curing Activator | Ethanol, initiators, and accelerators | |
| Bifix QM Cement | VOCO GmbH, Cuxhaven, Germany | Dual-cured adhesive composite cement (automix syringe) | Bis-GMA, benzoylperoxide, amines, barium-aluminiumboro-silicate glasse (71-73% wt) | |
| Ceramic Bond | VOCO GmbH, Cuxhaven, Germany | Silane Coupling Agent | Phosphoric acid ester, trimethoxysilane and acetone | |
| Futurabond U | VOCO GmbH, Cuxhaven, Germany | Universal Adhesive | “Modified” 10-MDP, Dymethacrylate resins, HEMA, Ethanol, Water, Carboxylic acid ester, Iniators | |
| Estecem | Tokuyama Dental Italy, Montecchio Precalcino, Italy | Dual-cured adhesive composite cement (automix syringe) | Paste A: Bis-GMA, TEGDMA, Bis-MPEPP, silica-zirconia filler (wt 74%) Paste B: Bis-GMA, TEGDMA, Bis-MPEPP, silica-zirconia filler, CQ, peroxide. | |
| Tokuyama Universal Primer | Tokuyama Dental Italy, Montecchio Precalcino, Italy | Silane Coupling Agent | Primer A: MTU-6, γ-MPS, Bis-GMA, TEGDMA, ethanol Primer B: 3D-SR, MAC-10, UDMA, acetone | |
| Estelink | Tokuyama Dental Italy, Montecchio Precalcino, Italy | Universal Adhesive | Bond A: 3D-SR monomer, HEMA, Bis-GMA, TEGDMA, acetone Bond B: Borate, peroxide, acetone, isopropyl alcohol, water |
| Panavia V5 | Bifix QM | Estelite | |
|---|---|---|---|
| T = 0 | 32.45 ± 7.71 (42 A, 1 CC, 2 CD, 10 M) | 25.75 ± 7.65 (36 A, 5 CC, 4 CD, 8 M) | 26.39 ± 6.69 (37 A, 3 CC, 2 CD, 5 M) |
| T = 12 | 35.55 ± 6.18 (34 A, 5 CC, 1 CD, 7 M) | 27.75 ± 6.46 (27 A, 6 CC, 1 CD, 8 M) | 26.32 ± 6.09 (29 A, 10 CC, 4 CD, 9 M) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vergano, E.A.; Baldi, A.; Comba, A.; Italia, E.; Ferrero, G.; Femiano, R.; Femiano, F.; Scotti, N. Bond Strength Stability of Different Dual-Curing Adhesive Cements towards CAD-CAM Resin Nanoceramic: An In Vitro Study. Appl. Sci. 2021, 11, 3971. https://doi.org/10.3390/app11093971
Vergano EA, Baldi A, Comba A, Italia E, Ferrero G, Femiano R, Femiano F, Scotti N. Bond Strength Stability of Different Dual-Curing Adhesive Cements towards CAD-CAM Resin Nanoceramic: An In Vitro Study. Applied Sciences. 2021; 11(9):3971. https://doi.org/10.3390/app11093971
Chicago/Turabian StyleVergano, Edoardo Alberto, Andrea Baldi, Allegra Comba, Edoardo Italia, Giorgio Ferrero, Rossella Femiano, Felice Femiano, and Nicola Scotti. 2021. "Bond Strength Stability of Different Dual-Curing Adhesive Cements towards CAD-CAM Resin Nanoceramic: An In Vitro Study" Applied Sciences 11, no. 9: 3971. https://doi.org/10.3390/app11093971







