Biomechanical Assessment of Mobile-Bearing Total Knee Endoprostheses Using Musculoskeletal Simulation
Abstract
1. Introduction
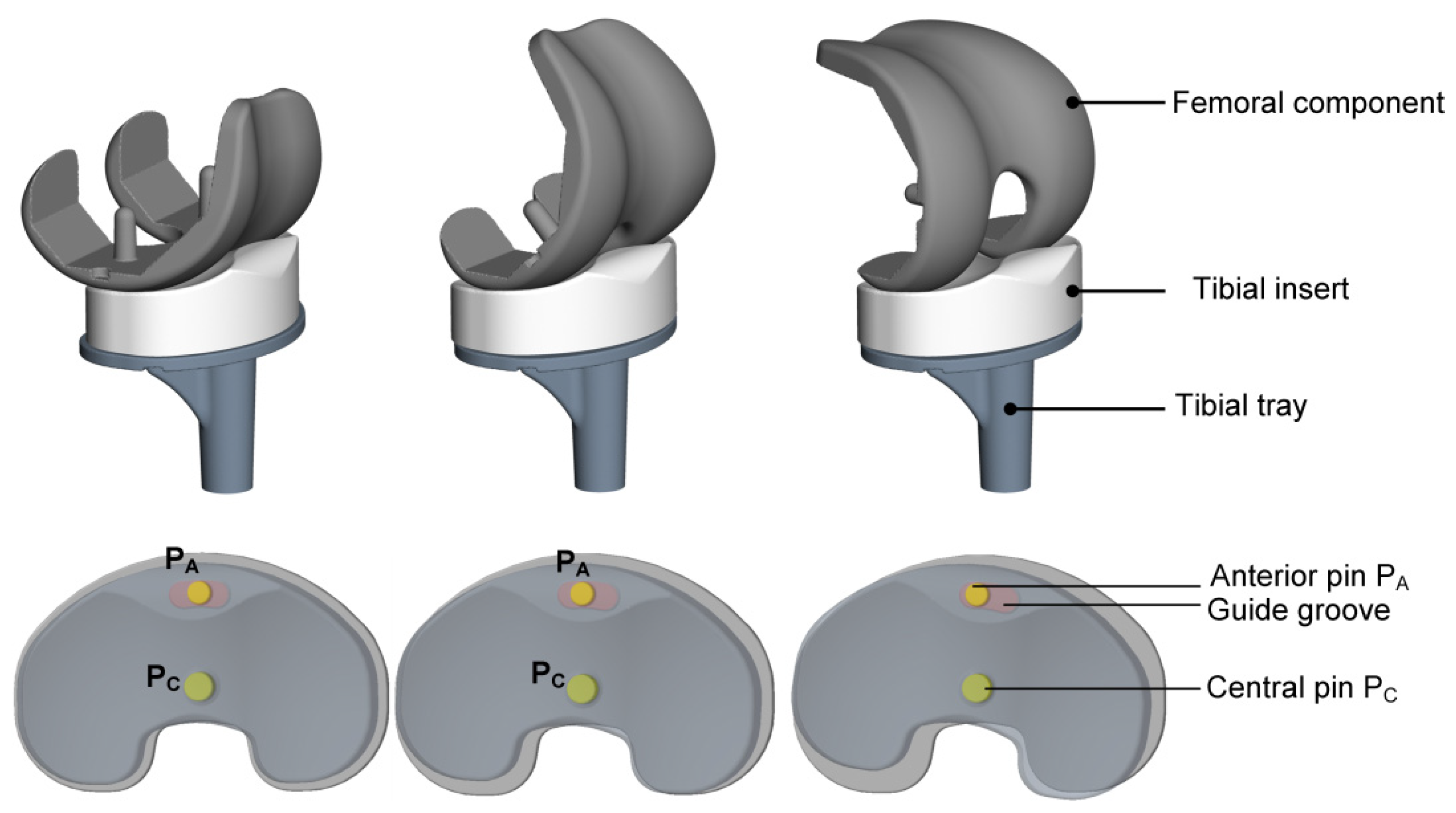
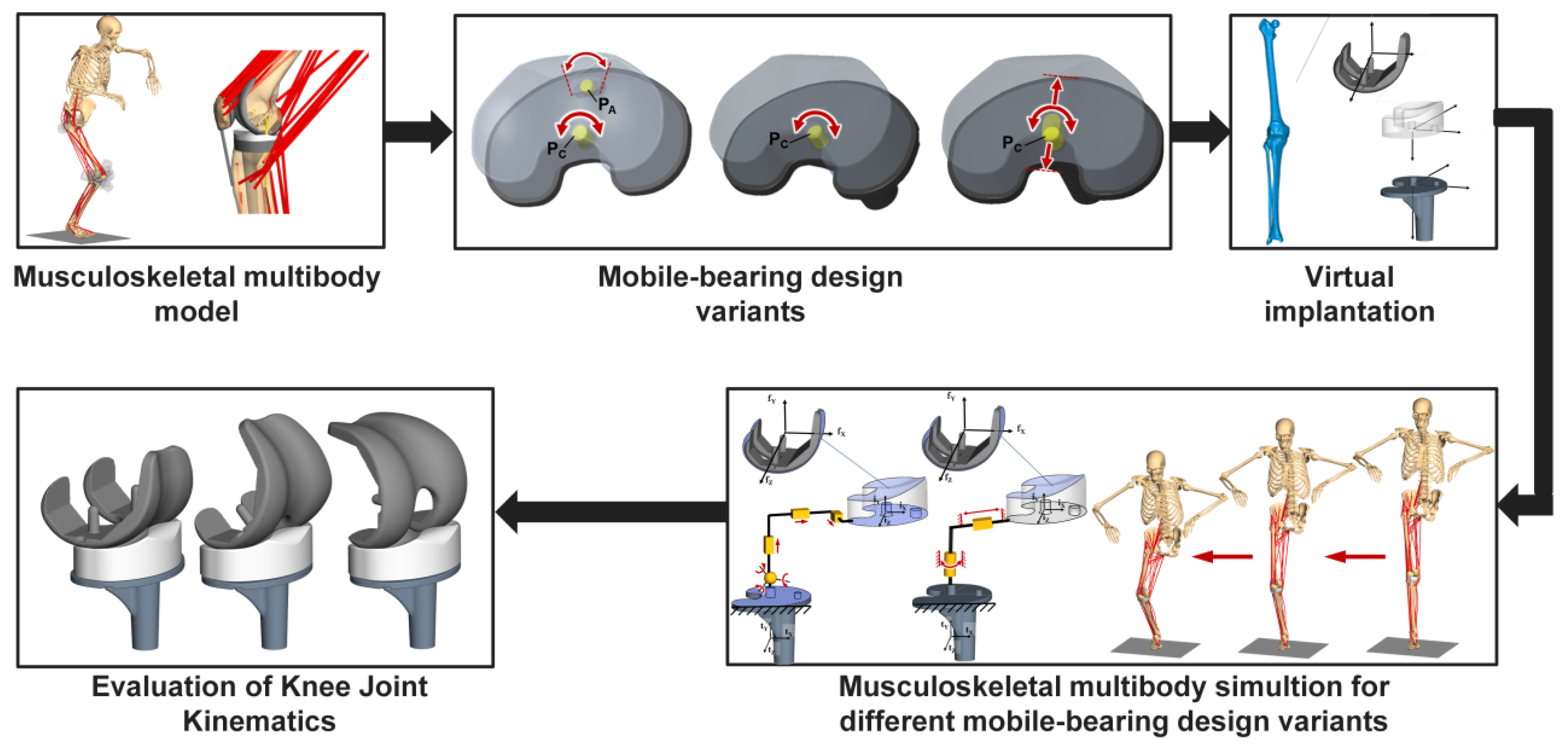
2. Materials and Methods
2.1. Musculoskeletal Multibody Simulation Model of the Knee Joint for Different Mobile-Bearing Design Variants
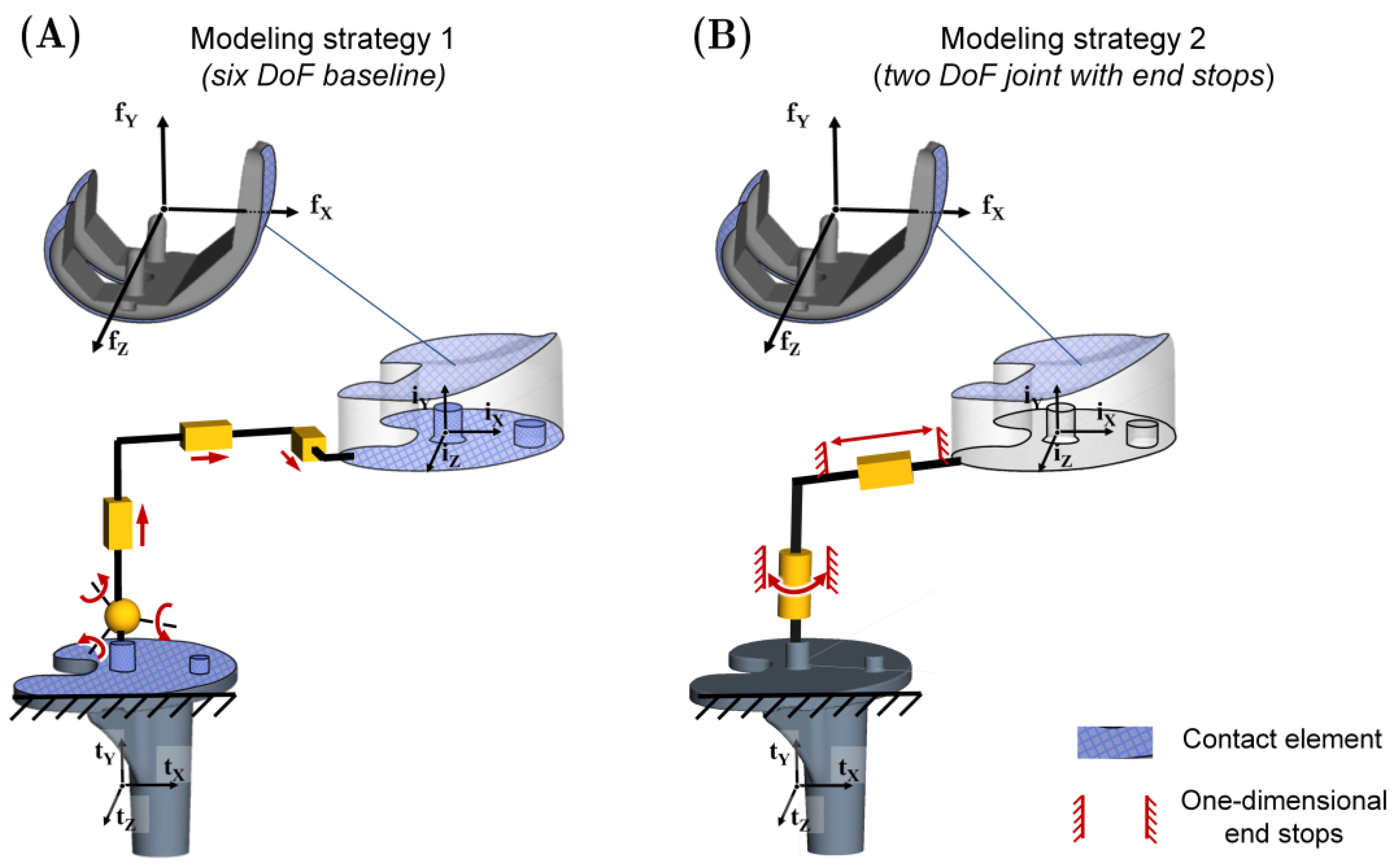
2.2. Description of the Different Modeling Strategies to Consider Mobile-Bearing Total Knee Replacements
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, J.G.; Wixson, R.L.; Tsai, D.; Stulberg, S.D.; Chang, R.W. Functional outcome and patient satisfaction in total knee patients over the age of 75. J. Arthroplast. 1996, 11, 831–840. [Google Scholar] [CrossRef]
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D.J. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef]
- Gibon, E.; Goodman, M.J.; Goodman, S.B. Patient Satisfaction After Total Knee Arthroplasty: A Realistic or Imaginary Goal? Orthop. Clin. N. Am. 2017, 48, 421–431. [Google Scholar] [CrossRef]
- Baker, P.N.; van der Meulen, J.H.; Lewsey, J.; Gregg, P.J. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J. Bone Jt. Surg. Br. 2007, 89, 893–900. [Google Scholar] [CrossRef]
- Mannion, A.F.; Kämpfen, S.; Munzinger, U.; Kramers-de Quervain, I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res. Ther. 2009, 11, R139. [Google Scholar] [CrossRef]
- Kessler, O.; Lacatusu, E.; Sommers, M.B.; Mayr, E.; Bottlang, M. Malrotation in total knee arthroplasty: Effect on tibial cortex strain captured by laser-based strain acquisition. Clin. Biomech. 2006, 21, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Mitsugi, N.; Mochida, Y.; Taki, N.; Akamatsu, Y.; Aratake, M.; Ota, H.; Ishii, K.; Harigane, K.; Ideno, T.; et al. Mid- term results of stryker® scorpio plus mobile bearing total knee arthroplasty. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2012, 4, 38. [Google Scholar] [CrossRef]
- Hwang, B.-H.; Lee, W.-S.; Park, K.-K.; Yang, I.-H.; Han, C.-D. Anterior-posterior glide mobile-bearing total knee arthroplasty: Complications related to prosthesis design. J. Arthroplast. 2011, 26, 1438–1444. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.T.; Kang, M.S.; Lim, Y.H.; Park, J.W.; Wang, L. Short-Term Results of Total Knee Arthroplasty with Anterior-Posterior Glide LCS Mobile-Bearing System. Knee Surg. Relat. Res. 2014, 26, 162–167. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yamazaki, T.; Futai, K.; Tomita, T.; Sato, Y.; Yoshikawa, H.; Tamura, S.; Sugamoto, K. 3D kinematics of mobile-bearing total knee arthroplasty using X-ray fluoroscopy. Int. J. Comput. Assist. Radiol. Surg. 2015, 10, 487–495. [Google Scholar] [CrossRef]
- Maas, A.; Kim, T.K.; Miehlke, R.K.; Hagen, T.; Grupp, T.M. Differences in anatomy and kinematics in Asian and Caucasian TKA patients: Influence on implant positioning and subsequent loading conditions in mobile bearing knees. BioMed Res. Int. 2014, 612838. [Google Scholar] [CrossRef]
- Huang, Z.-M.; Ouyang, G.-L.; Xiao, L.-B. Rotating-platform knee arthroplasty: A review and update. Orthop. Surg. 2011, 3, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Vertullo, C.J.; Easley, M.E.; Scott, W.N.; Insall, J.N. Mobile bearings in primary knee arthroplasty. J. Am. Acad. Orthop. Surg. 2001, 9, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Walker, P.S.; Komistek, R.D.; Barrett, D.S.; Anderson, D.; Dennis, D.A.; Sampson, M. Motion of a mobile bearing knee allowing translation and rotation. J. Arthroplast. 2002, 17, 11–19. [Google Scholar] [CrossRef]
- Chouteau, J.; Lerat, J.-L.; Testa, R.; Moyen, B.; Fessy, M.-H.; Banks, S.A. Mobile-bearing insert translational and rotational kinematics in a PCL-retaining total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 254–259. [Google Scholar] [CrossRef][Green Version]
- Munzinger, U.K.; Boldt, J.G. Mobile-Bearing Knee Prostheses. In European Surgical Orthopaedics and Traumatology; Bentley, G., Ed.; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Jenny, J.-Y.; Saragaglia, D. No Detectable Polyethylene Wear 15 Years After Implantation of a Mobile-Bearing Total Knee Arthroplasty with Electron Beam-Irradiated Polyethylene. J. Arthroplast. 2019, 34, 1690–1694. [Google Scholar] [CrossRef]
- Mulcahy, H.; Chew, F.S. Current concepts in knee replacement: Complications. AJR Am. J. Roentgenol. 2014, 202, W76–W86. [Google Scholar] [CrossRef]
- Lee, D.-H.; Lee, D.-K.; Shin, Y.-S.; Han, S.-B. Mid-term outcomes of floating platform mobile-bearing total knee arthroplasty under navigational guidance with a minimum 4-year follow-up. J. Arthroplast. 2013, 28, 1801–1805. [Google Scholar] [CrossRef]
- Williams, J.L.; Gomaa, S.T. Kinematics of Rotating Platform Total Knee Replacements: Does the Position of the Rotating Platform Axis Matter? In Proceedings of the 3rd Frontiers in Biomedical Devices Conference, Imaging and Anatomic Interaction; Simulation and Testing, Irvine, CA, USA, 18–20 June 2008; pp. 15–16. [Google Scholar]
- Colwell, C.W.; Chen, P.C.; D’Lima, D. Extensor malalignment arising from femoral component malrotation in knee arthroplasty: Effect of rotating-bearing. Clin. Biomech. 2011, 26, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Capella, M.; Dolfin, M.; Saccia, F. Mobile bearing and fixed bearing total knee arthroplasty. Ann. Transl. Med. 2016, 4, 127. [Google Scholar] [CrossRef]
- Hanusch, B.; Lou, T.N.; Warriner, G.; Hui, A.; Gregg, P. Functional outcome of PFC Sigma fixed and rotating-platform total knee arthroplasty. A prospective randomised controlled trial. Int. Orthop. 2010, 34, 349–354. [Google Scholar] [CrossRef]
- Koh, Y.-G.; Lee, J.-A.; Lee, H.-Y.; Suh, D.-S.; Kim, H.-J.; Kang, K.-T. Effect of sagittal femoral component alignment on biomechanics after mobile-bearing total knee arthroplasty. J. Orthop. Surg. Res. 2019, 14, 400. [Google Scholar] [CrossRef]
- Kang, K.-T.; Koh, Y.-G.; Son, J.; Kwon, O.-R.; Lee, J.-S.; Kwon, S.K. Comparison of Kinematics in Cruciate Retaining and Posterior Stabilized for Fixed and Rotating Platform Mobile-Bearing Total Knee Arthroplasty with respect to Different Posterior Tibial Slope. BioMed Res. Int. 2018, 5139074. [Google Scholar] [CrossRef]
- Futai, K.; Tomita, T.; Yamazaki, T.; Tamaki, M.; Yoshikawa, H.; Sugamoto, K. In vivo kinematics of mobile-bearing total knee arthroplasty during deep knee bending under weight-bearing conditions. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 914–920. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Chen, Z.; Wang, L.; Li, D.; Jin, Z. A patient-specific wear prediction framework for an artificial knee joint with coupled musculoskeletal multibody-dynamics and finite element analysis. Tribol. Int. 2017, 109, 382–389. [Google Scholar] [CrossRef]
- Catani, F.; Benedetti, M.G.; Bianchi, L.; Marchionni, V.; Giannini, S.; Leardini, A. Muscle activity around the knee and gait performance in unicompartmental knee arthroplasty patients: A comparative study on fixed- and mobile-bearing designs. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1042–1048. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.H.; Zakaria, T.; van der Merwe, W.; D’Angelo, F. Computational modelling of mobile bearing TKA anterior-posterior dislocation. Comput. Methods Biomech. Biomed. Engin. 2016, 19, 549–562. [Google Scholar] [CrossRef]
- Sharma, A.; Komistek, R.D.; Ranawat, C.S.; Dennis, D.A.; Mahfouz, M.R. In vivo contact pressures in total knee arthroplasty. J. Arthroplast. 2007, 22, 404–416. [Google Scholar] [CrossRef]
- Innocenti, B.; Pianigiani, S.; Labey, L.; Victor, J.; Bellemans, J. Contact forces in several TKA designs during squatting: A numerical sensitivity analysis. J. Biomech. 2011, 44, 1573–1581. [Google Scholar] [CrossRef]
- Wen, Y.; Liu, D.; Huang, Y.; Li, B. A meta-analysis of the fixed-bearing and mobile-bearing prostheses in total knee arthroplasty. Arch. Orthop. Trauma Surg. 2011, 131, 1341–1350. [Google Scholar] [CrossRef]
- McEwen, H.M.J.; Barnett, P.I.; Bell, C.J.; Farrar, R.; Auger, D.D.; Stone, M.H.; Fisher, J. The influence of design, materials and kinematics on the in vitro wear of total knee replacements. J. Biomech. 2005, 38, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Zhu, G.-D.; Guo, W.-S.; Zhang, Q.-D.; Liu, Z.-H.; Cheng, L.-M. Finite Element Analysis of Mobile-bearing Unicompartmental Knee Arthroplasty: The Influence of Tibial Component Coronal Alignment. Chin. Med. J. 2015, 128, 2873–2878. [Google Scholar] [CrossRef]
- Anuar, M.A.M.; Todo, M.; Nagamine, R.; Hirokawa, S. Dynamic finite element analysis of mobile bearing type knee prosthesis under deep flexional motion. Sci. World J. 2014, 2014, 586921. [Google Scholar]
- Guess, T.M.; Thiagarajan, G.; Kia, M.; Mishra, M. A subject specific multibody model of the knee with menisci. Med. Eng. Phys. 2010, 32, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Srinivas, G.R.; Deb, A.; Kumar, M.N. A study on polyethylene stresses in mobile-bearing and fixed-bearing total knee arthroplasty (TKA) using explicit finite element analysis. J. Long Term Eff. Med. Implants 2013, 23, 275–283. [Google Scholar] [CrossRef]
- Kebbach, M.; Darowski, M.; Krueger, S.; Schilling, C.; Grupp, T.M.; Bader, R.; Geier, A. Musculoskeletal Multibody Simulation Analysis on the Impact of Patellar Component Design and Positioning on Joint Dynamics after Unconstrained Total Knee Arthroplasty. Materials 2020, 13, 2365. [Google Scholar] [CrossRef]
- Fregly, B.J.; Besier, T.F.; Lloyd, D.G.; Delp, S.L.; Banks, S.A.; Pandy, M.G.; D’Lima, D.D. Grand challenge competition to predict in vivo knee loads. J. Orthop. Res. 2012, 30, 503–513. [Google Scholar] [CrossRef]
- Carbone, V.; Fluit, R.; Pellikaan, P.; van der Krogt, M.M.; Janssen, D.; Damsgaard, M.; Vigneron, L.; Feilkas, T.; Koopman, H.F.J.M.; Verdonschot, N. TLEM 2.0—A comprehensive musculoskeletal geometry dataset for subject-specific modeling of lower extremity. J. Biomech. 2015, 48, 734–741. [Google Scholar] [CrossRef]
- Thelen, D.G.; Won Choi, K.; Schmitz, A.M. Co-simulation of neuromuscular dynamics and knee mechanics during human walking. J. Biomech. Eng. 2014, 136, 021033. [Google Scholar] [CrossRef]
- Lampe, F.; Sufi-Siavach, A.; Bohlen, K.E.; Hille, E.; Dries, S.P.M. One year after navigated total knee replacement, no clinically relevant difference found between fixed bearing and mobile bearing knee replacement in a double-blind randomized controlled trial. Open Orthop. J. 2011, 5, 201–208. [Google Scholar] [CrossRef]
- Walker, P.S.; Sathasivam, S. Design forms of total knee replacement. Proc. Inst. Mech. Eng. Part H 2000, 214, 101–119. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A. Biomechanics and Motor Control of Human Movement, 4th ed.; Wiley: Hoboken, NJ, USA, 2009. [Google Scholar]
- Blankevoort, L.; Kuiper, J.H.; Huiskes, R.; Grootenboer, H.J. Articular contact in a three-dimensional model of the knee. J. Biomech. 1991, 24, 1019–1031. [Google Scholar] [CrossRef]
- Wismans, J.; Veldpaus, F.; Janssen, J.; Huson, A.; Struben, P. A three-dimensional mathematical model of the knee-joint. J. Biomech. 1980, 13, 677–685. [Google Scholar] [CrossRef]
- Hippmann, G. An Algorithm for Compliant Contact Between Complexly Shaped Bodies. Multibody Syst. Dyn. 2004, 12, 345–362. [Google Scholar] [CrossRef]
- Golish, S.R.; Mihalko, W.M. Principles of biomechanics and biomaterials in orthopaedic surgery. J. Bone Jt. Surg. Am. 2011, 93, 207–212. [Google Scholar] [CrossRef]
- Kurt, S.M. UHMWPE Biomaterials Handbook; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Shoifi Abubakar, M.; Nakamura, S.; Kuriyama, S.; Ito, H.; Ishikawa, M.; Furu, M.; Tanaka, Y.; Matsuda, S. Influence of Posterior Cruciate Ligament Tension on Knee Kinematics and Kinetics. J. Knee Surg. 2016, 29, 684–689. [Google Scholar] [CrossRef]
- Morra, E.A.; Heim, C.S.; Greenwald, A.S. Preclinical computational models: Predictors of tibial insert damage patterns in total knee arthroplasty: AAOS exhibit selection. J. Bone Jt. Surg. Am. 2012, 94, e137. [Google Scholar] [CrossRef]
- Kwon, O.-R.; Kang, K.-T.; Son, J.; Kwon, S.-K.; Jo, S.-B.; Suh, D.-S.; Choi, Y.-J.; Kim, H.-J.; Koh, Y.-G. Biomechanical comparison of fixed- and mobile-bearing for unicomparmental knee arthroplasty using finite element analysis. J. Orthop. Res. 2014, 32, 338–345. [Google Scholar] [CrossRef]
- Zhang, J.-Y.; Wang, J.; Tian, D.-M.; Jiang, D.-P.; Li, J.-J.; Hu, Y.-C. Spherical center and rotating platform hinged knee prosthesis: Finite-element model establishment, verification and contact analysis. Knee 2020, 27, 731–739. [Google Scholar] [CrossRef]
- Kim, T.K.; Phillips, M.; Bhandari, M.; Watson, J.; Malhotra, R. What Differences in Morphologic Features of the Knee Exist Among Patients of Various Races? A Systematic Review. Clin. Orthop. Relat. Res. 2017, 475, 170–182. [Google Scholar] [CrossRef]
- Mahfouz, M.; Abdel Fatah, E.E.; Bowers, L.S.; Scuderi, G. Three-dimensional morphology of the knee reveals ethnic differences. Clin. Orthop. Relat. Res. 2012, 470, 172–185. [Google Scholar] [CrossRef] [PubMed]
- Kutzner, I.; Heinlein, B.; Graichen, F.; Bender, A.; Rohlmann, A.; Halder, A.; Beier, A.; Bergmann, G. Loading of the knee joint during activities of daily living measured in vivo in five subjects. J. Biomech. 2010, 43, 2164–2173. [Google Scholar] [CrossRef]
- Witjes, S.; Gouttebarge, V.; Kuijer, P.P.F.M.; van Geenen, R.C.I.; Poolman, R.W.; Kerkhoffs, G.M.M.J. Return to Sports and Physical Activity After Total and Unicondylar Knee Arthroplasty: A Systematic Review and Meta-Analysis. Sports Med. 2016, 46, 269–292. [Google Scholar] [CrossRef] [PubMed]
- Mündermann, A.; Dyrby, C.O.; D’Lima, D.D.; Colwell, C.W.; Andriacchi, T.P. In vivo knee loading characteristics during activities of daily living as measured by an instrumented total knee replacement. J. Orthop. Res. 2008, 26, 1167–1172. [Google Scholar] [CrossRef]
- Vitalis, L.; Russu, O.; Zuh, S.; Pop, T.S. Recommendations for Sport and Physical Activity after total Hip and Knee Arthroplasty: A Systematic Review. Acta Med. Transilv. 2021, 26, 63–66. [Google Scholar] [CrossRef]
- Shabani, B.; Bytyqi, D.; Batailler, C.; Servien, E.; Lustig, S. Sports After Knee Arthroplasty. In The Sports Medicine Physician; Piedade, S.R., Imhoff, A.B., Clatworthy, M., Cohen, M., Espregueira-Mendes, J., Eds.; Springer: Cham, Switzerland, 2019. [Google Scholar]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kebbach, M.; Soodmand, I.; Krueger, S.; Grupp, T.M.; Woernle, C.; Bader, R. Biomechanical Assessment of Mobile-Bearing Total Knee Endoprostheses Using Musculoskeletal Simulation. Appl. Sci. 2022, 12, 182. https://doi.org/10.3390/app12010182
Kebbach M, Soodmand I, Krueger S, Grupp TM, Woernle C, Bader R. Biomechanical Assessment of Mobile-Bearing Total Knee Endoprostheses Using Musculoskeletal Simulation. Applied Sciences. 2022; 12(1):182. https://doi.org/10.3390/app12010182
Chicago/Turabian StyleKebbach, Maeruan, Iman Soodmand, Sven Krueger, Thomas M. Grupp, Christoph Woernle, and Rainer Bader. 2022. "Biomechanical Assessment of Mobile-Bearing Total Knee Endoprostheses Using Musculoskeletal Simulation" Applied Sciences 12, no. 1: 182. https://doi.org/10.3390/app12010182
APA StyleKebbach, M., Soodmand, I., Krueger, S., Grupp, T. M., Woernle, C., & Bader, R. (2022). Biomechanical Assessment of Mobile-Bearing Total Knee Endoprostheses Using Musculoskeletal Simulation. Applied Sciences, 12(1), 182. https://doi.org/10.3390/app12010182





