Abstract
The aim of this paper is to compare von Mises stress levels and displacements between two possible designs of a class II Kennedy unilateral removable partial denture. Finite element analysis was used to compare two unilateral class II Kennedy removable partial dentures replacing a mandibular second premolar, and first and second molars and with the same design, except a distal implant. The 3D model was created for a mandibular RPD with three artificial teeth and double ball attachment on the abutment teeth and a horizontal ball attachment for the implant, using Autodesk Inventor 2022 software. On the saddle, significant differences appear only when force is applied on the second molar. Association with implant increases von Mises stresses on the acrylic saddle, where displacements values are similar, and decreases von Mises stresses on the muco-osseous support, where displacements values are also similar. Regarding metal reinforcement of the denture, von Mises stress values are greater for forces applied on the second premolar in the implant situation, and smaller for forces applied on the first and second molars. Association with implant decreases von Mises stresses on the metal reinforcement of the denture only if the force is applied distally, on the two molars; in this case, the metal reinforcement is more stressed above the mesial double ball attachment, where displacements values are similar. Regarding the artificial teeth, adding a distal implant does not significantly influence the stress and displacements values, except on the second premolar where the von Mises stresses values are greater, where displacements values are similar. Although an association with an implant increases the risk of fracture for the denture, the results demonstrate that in the posterior area of the edentulous space, the denture exerts less pressure on the mucosa and subjacent bone, protecting the area against resorption.
1. Introduction
Association between removable partial dentures (RPD) and implants is gathering more and more interest in clinical practice in dentistry, especially for class I and II Kennedy situations, aiming to avoid displacement of the distal parts of the classical dentures toward mucosal support and to improve masticatory efficiency and comfort [1,2,3,4]. The extensive coverage of the major connectors used for classic class II Kennedy RPDs can be avoided using a unilateral removable partial denture, but in the absence of the cross-arch stabilization these connectors are offering, the denture can be easily dislodged during functions [5]. Proper design with splinting abutments using crowns with milled oral surfaces and interlocks and, if possible, posterior implant support is required in order to avoid complications. There are studies in the literature demonstrating that using an extra-coronal resilient attachment can reduce the stress on the terminal abutment because it distributes more loads onto the distal edentulous ridge [6]. Excessive movements of a unilateral RPD cause bone resorption, which, in turn, contributes to accelerating the loss and amplifying denture movements. It is necessary to identify and evaluate methods to prevent these movements.
The aim of this study is to investigate the von Mises stress distribution in two similar unilateral RPD designs, in order to assess whether adding a posterior implant in the distal part of the edentulous ridge improves the functionality of the denture and, subsequently, contributes to a decrease in the rhythm of the bone resorption. The null hypothesis was that stress distribution in two unilateral RPDs could be similar if supported by a posterior implant in the distal part and without the implant.
2. Materials and Methods
In this study, two cases of a mandibular class II Kennedy edentulous patients with PM2, M1 and M2 teeth missing were considered. For the first patient, a mandibular unilateral removable partial denture was made, in order to replace all the three missing teeth. The two anterior abutment teeth were covered using two splinted metal-ceramic surveyed crowns, with two oral milled shoulders and one interlock in between them. To retain the denture, a prefabricated unique sagittal attachment was used, with two balls (Rhein83, Bologna, Italy), one horizontal and the other sagittal. All the metallic parts of the assembly (splinted crowns with attachment, metal housing of the attachment and metal reinforcement of the saddle) were casted from Cr-Co Remanium GM 380 (Dentaurum, Ispringen, Germany). The acrylic saddles were made of thermo-polymerizable acrylic material Acry-Pole (Ruthinium Dental Manufacturing S.p.A., Badia Polesine, Rovigo, Italy) and the artificial acrylic teeth were made from Acry-Rock (Ruthinium Dental Manufacturing S.p.A., Badia Polesine, Rovigo, Italy). For the second patient, a similar mandibular unilateral removable partial denture was made, but using a posterior implant, on the position of the second molar, also with the same extra-coronal ball attachment and a metal housing positioned horizontally on top of the implant. This second denture design converted the distal extension denture base from a tooth- and tissue-supported prosthesis to a tooth- and implant-supported prosthesis. The used implant (Alpha-Bio Tec, Petach Tikwa, Israel) has the following dimensions: 3.75 mm diameter and 8 mm length. For both cases, the mandibular bone was considered to have an outer layer (1.2 mm thickness) of cancellous bone, while the rest of them were type III trabecular bone [7,8].
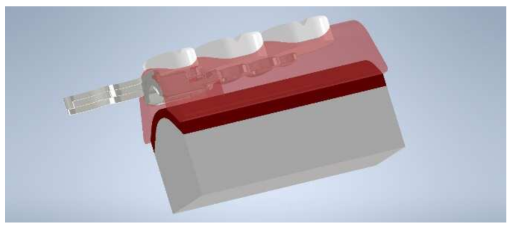
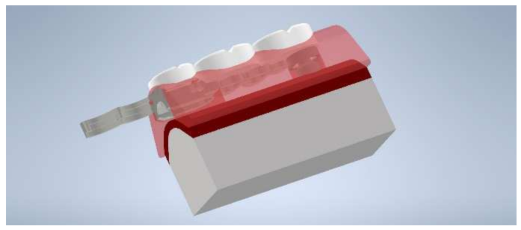
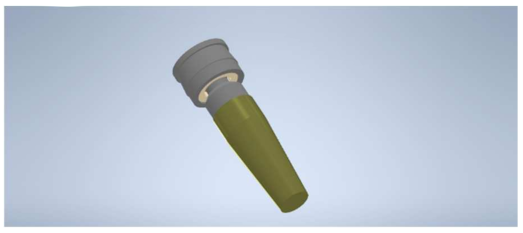
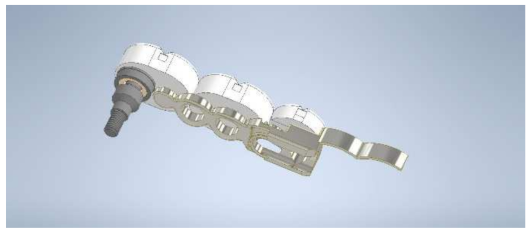
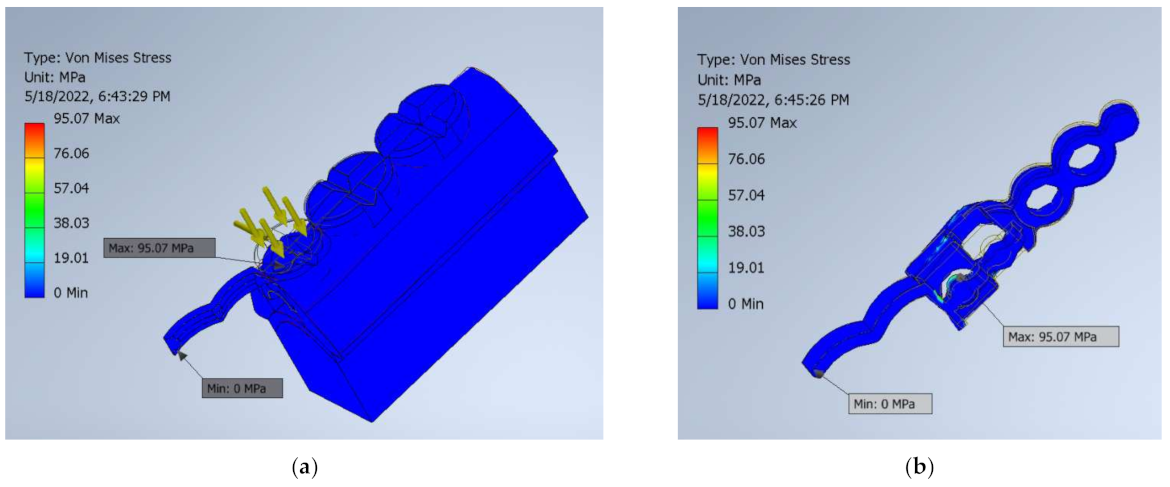
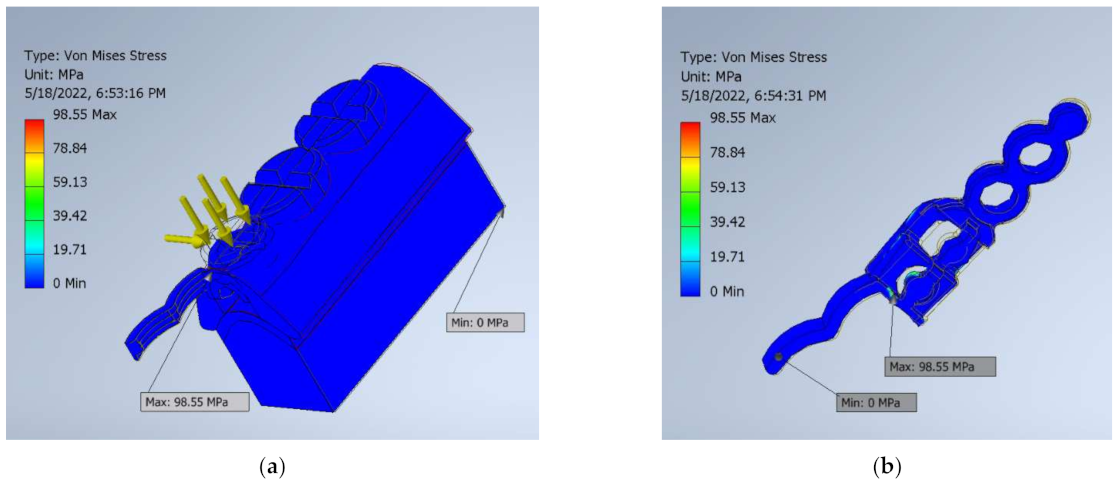
Finite element analysis was used in order to study the stress distribution in these two unilateral denture designs. The 3D models were created using Autodesk Inventor 2022 software (Figure 1, Figure 2, Figure 3 and Figure 4); their characteristics are presented in Table 1. The geometrical form of the second premolar was cylindrical, while that of the two molars was elliptic cylindrical; their dimensions were considered equal. In addition, all the cusps were considered to be equally dimensioned and in the same occlusal plane.
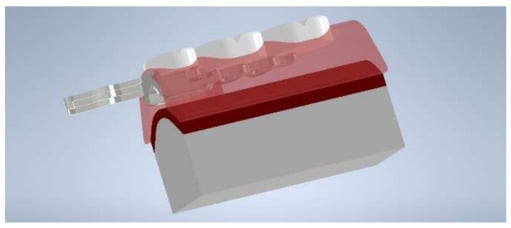
Figure 1.
The 3D Model of the unilateral mandibular RPD.
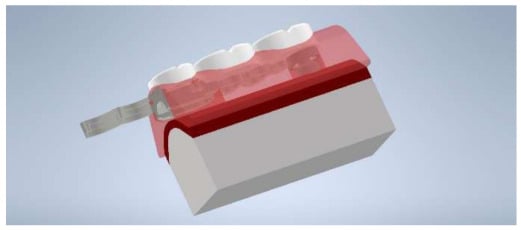
Figure 2.
The 3D Model of the unilateral mandibular RPD with distal implant.
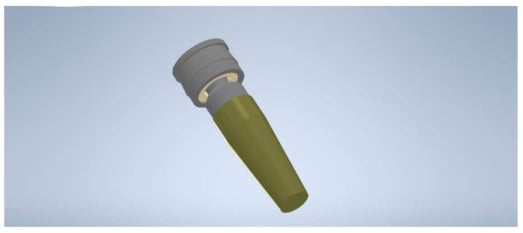
Figure 3.
The 3D Model of the implant and ball attachment, with matrix housing.
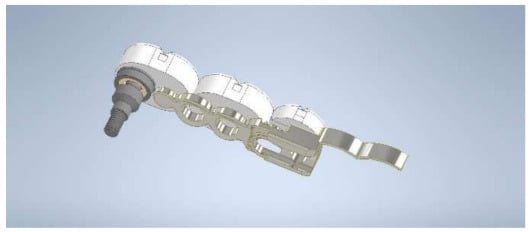
Figure 4.
The 3D Model of the metal reinforcement, artificial teeth and distal implant.

Table 1.
The 3D models characteristics.
The von Mises stress levels and stress distribution that appeared in these two situations were compared using a masticatory force with an axial component of 160 N and a tangential component of 23.5 N [9]. All materials were considered isotropic with linear elasticity and they were homogeneous. The mechanical properties (obtained from the above-mentioned manufacturers and [7,8]) of all materials are presented in Table 2.

Table 2.
The constant mechanical properties of the used materials.
The bracket was considered to be frictionless and constrained on the support surface. The ball attachments were modeled as pin constrained. The lateral, front, back and base faces of the jawbone were considered to be fully constrained. The implant for the second patient was simulated as inserted in M2, through an HDPE cup. All contacts between parts were considered to be bonded. The mesh refinement threshold was 0.75 and the convergence of the results was set to be von Mises stress.
For both analyzed cases, the meshing was carried out using linear tetrahedrons elements, with the average size of 0.1 mm, grading factor 1.5 and maximum turn angle 60 deg. For the model without implant, the meshing contains 38,243 nodes and 22,179 elements. For the model with implant, the meshing contains 59,780 nodes and 34,526 elements.
3. Results
For the classical unilateral RPD design, the highest von Mises stresses (MPa) are presented in Table 3; for the unilateral RPD with distal implant, the highest von Mises stresses (MPa) are presented in Table 4.

Table 3.
The maximum von Mises stress (MPa) for the unilateral RPD.

Table 4.
The maximum von Mises stress (MPa) for the unilateral RPD with distal implant.
On the saddle, significant differences appear only when force is applied on the second molar. Association with the implant increases von Mises stresses on the acrylic saddle, where the displacements values are similar, and decreases von Mises stresses on the muco-osseous support, where the displacements values are also similar. Regarding the metal reinforcement of the denture, von Mises stress values are greater for forces applied on the second premolar in the implant situation, and smaller for forces applied on the first and second molars. Association with the implant decreases von Mises stresses on the metal reinforcement of the denture only if the force is applied distally, on the two molars; in this case, the metal reinforcement is more stressed above the mesial double ball attachment (PM2), where the displacements values are similar (Figure 5 and Figure 6), and the saddle is more stressed on the second molar. Regarding the artificial teeth, adding a distal implant does not significantly influence the stress and displacements values, except on the second premolar, where the von Mises stresses values are greater, and displacements values are similar. Comparing the two clinical situations, association with a distal implant decreases the maximum von Mises stresses values on the two molars, especially on the second one, on the bone area.
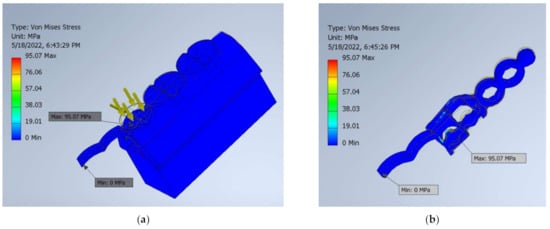
Figure 5.
Maximum von Mises stress in classical unilateral RPD when the forces were applied on the PM2: (a) full analyzed assembly; (b) metallic reinforcement.
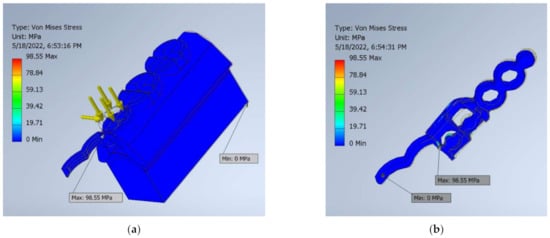
Figure 6.
Maximum von Mises stress in unilateral RPD with implant when the forces were applied on the PM2: (a) full analyzed assembly; (b) metallic reinforcement.
4. Discussion
The null hypothesis was that stress distribution in two unilateral RPDs could be similar if supported by a posterior implant in the distal part and without the implant. The results showed that the presence of the implant increases the stress on the partial denture and the risk of fracture, while the implant-supported denture is exerting less pressure on the mucosa and subjacent bone, thus rejecting the hypothesis. Various researchers have tried to find the best solution for solving the unilateral free-end saddle equation. Some authors recommend special care in choosing and positioning the artificial teeth in order to adequately stabilize the abutment tooth and denture base of unilateral RPD [10]. Radović et al. compared stresses under different loads in a unilateral RPD and a classical RPD, both with three artificial teeth (second premolar, first molar and second molar) and found similar physiological values [11]. In our study, on the second premolar, values obtained on the bone are not clinically relevant, considering the fact that the denture is completely supported by the attachment under the second premolar. With regard to the second molar, and also clinically speaking, association with a distal implant decreases the maximum von Mises stresses values on the two molars, especially on the second one, on the bone area. This is the most important area for the long-term success of the prosthetic treatment because it prevents the tilting of the saddle that accentuates during the use of the denture trough bone resorption.
A prior study that aimed to compare a mandibular class I Kennedy removable partial denture (RPD) with ball attachments, in two designs—teeth supported only, and implant and teeth supported—demonstrated that associating an implant for each free-end saddle significantly reduces the maximum von Mises stress and the maximum displacement values in the RPD [12] and decreases the risk of bone resorption. In this study, in the case of unilateral RPDs, association with distal implants increases the risk of fracture for the denture, but it is also decreasing the risk of resorption of the bone, which is important for maintaining the vertical dimension of occlusion, masticatory efficiency and comfort. Another FEA study revealed differences between the stress distribution pattern of implant-supported RPD and that of implant-tissue-supported RPD; the highest maximum displacement value was found in the model tooth-tissue-supported RPD, while the lowest value was in the implant-supported RPD [13].
Another study analyzed how the free-end saddle length influences the behavior of unilateral partial denture supporting structures and found a different stress distribution on the abutment teeth and the attachment, determined by physiological forces; stress level values in the abutment teeth and the attachment were far lower than the marginal ones [14]. In our study, values obtained for the metal reinforcement above the attachment are greater for the implant supported denture only on the second premolar.
Studies found in the literature showed that association between implants and RPDs is beneficial for the teeth and tissues because the implant receives the majority of the load and reduces the stress on the abutment and the displacement of the denture; the amount of stress in the implant and the periodontal ligament of the abutment teeth decreases when the implants are placed in the first molar area [15,16]. The implant position affects the stresses level around implant such that a distal position recorded higher stresses than a mesial implant position [17]. Another benefit of the association between the implant and the mandibular free-end saddle is that it significantly improves masticatory function which occurs, regardless of the position chosen for the implant [18]. In our study, the implant was positioned under the second molar. In line with previous research, this study shows that the placement of the implant had beneficial effects on the bone; the stress on the implant increases as long as the force is applied more distally.
In their 2016 study, Choi et al. recommended that special care be taken in the selection of attachments that are used in implant supported RPDs, aiming to reduce stress levels, and to avoid mechanical problems [19]. The effect of the type of attachment on peri-implant and peri-abutment supporting structures was studied by Mously in 2020; he did not find statistically significant differences between the attachment types [20]. Moreover, a recent study showed that the implant survival rate and patient satisfaction were not affected by the type of the attachments used in removable partial dentures on implants, on Kennedy class II edentulous cases [21]; in our study, a double ball attachment was chosen, especially dedicated for those types of dentures.
A study that aimed to evaluate the prognosis of combining natural teeth and implants in the same removable denture found that tooth-and-implant-supported and solely implant-supported double-crown-retained removable partial dentures, with both abutment types, showed high cumulative survival rate, most of which were approximately 100% [22]. Other authors also found that that the association of teeth and implants to support double crown-retained RDPs has a prognostic advantage [23]. None of the unilateral RDPs compared in our study benefit from cross-arch stabilization, since they do not have a major connector; the presence of the distal implant adds height and contributes to the limitation of such horizontal movements, during the action of the tangential forces, showing maximum values on the shoulder of the housing and on the apex of the implant.
The limits of this study are that it is based on a numerical simulation, since it was not the authors’ intention to perform a clinical trial; however, the finite element analysis method is well used in dental medicine and offers good results for analyzing the design and performance of dentures. Conserving the height of the bone, the vertical dimension of occlusion and the chewing ability of the patient for a long term has a huge importance for a good quality of life, therefore further clinical studies are necessary to confirm that positioning a distal implant to support a class II Kennedy unilateral RPD proves to be a valuable treatment solution.
5. Conclusions
The results of this study show that, although association with an implant increases the risk of fracture for the unilateral removable partial denture in the posterior area of the edentulous space, the denture exerts less pressure on the mucosa and subjacent bone, protecting the area against resorption.
Author Contributions
Conceptualization, O.C.A. and M.H.T., methodology, O.C.A. and L.A.T., software, I.D.T. and M.H.T., validation, O.C.A. and M.N.D., investigation, L.A.T. and I.D.T., resources, M.N.D.; writing—original draft preparation, O.C.A. and L.A.T., writing—review and editing, M.N.D., I.D.T. and M.H.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alam-Eldein, A.; Abd El Fattah, F.; Shakal, E. Comparative study of two different designs of partial over denture supported with distal implant for the treatment of mandibular Kennedy class II cases. Tanta Dent. J. 2013, 10, 39–47. [Google Scholar] [CrossRef] [Green Version]
- Anantharaju, A.; Joseph, B.; Kusum, C.K.; Nooji, D. Connectors and attachments in oral rehabilitation. J. NTR Univ. Health Sci. 2013, 2, 222–226. [Google Scholar] [CrossRef]
- Ramchandran, A.; Agrawal, K.K.; Chand, P.; Ramashanker; Singh, R.D.; Gupta, A. Implant-assisted removable partial denture: An approach to switch Kennedy Class I to Kennedy Class III. J. Indian Prosthodont. Soc. 2016, 16, 408–411. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Ayukawa, Y.; Ogino, Y.; Nakagawa, A.; Horikawa, T.; Yamaguchi, E.; Takaki, K.; Koyano, K. Clinical effectiveness of implant support for distal extension removable partial dentures: Functional evaluation using occlusal force measurement and masticatory efficiency. Int. J. Implant Dent. 2021, 7, 101. [Google Scholar] [CrossRef] [PubMed]
- Uludag, B.; Celik, G. Technical tips for improved retention and stabilization of a unilateral removable partial denture. J. Oral Implantol. 2007, 33, 344–346. [Google Scholar] [CrossRef]
- Wang, H.Y.; Zhang, Y.M.; Yao, D.; Chen, J.H. Effects of rigid and nonrigid extracoronal attachments on supporting tissues in extension base partial removable dental prostheses: A nonlinear finite element study. J. Prosthet. Dent. 2011, 105, 338–346. [Google Scholar] [CrossRef]
- Wang, S.; Shen, Y.; Fuh, L.; Peng, S.; Tsai, M.; Huang, H.; Hsu, J. Relationship between Cortical Bone Thickness and Cancellous Bone Density at Dental Implant Sites in the Jawbone. Diagnostics 2020, 10, 710. [Google Scholar] [CrossRef]
- Misch, C.E. Contemporary Implant Dentistry, 3rd ed.; Mosby Elsevier: St. Louis, MO, USA, 2008; pp. 68–91. [Google Scholar]
- De Las Casas, E.B.; De Almeida, A.F.; Cimini Junior, C.A.; Gomes, P.T.V.; Cornacchia, T.P.; Saffar, J.M. Determination of tangential and normal components of oral forces. J. Appl. Oral Sci. 2007, 15, 70–76. [Google Scholar] [CrossRef]
- Jin, X.; Sato, M.; Nishiyama, A.; Ohyama, T. Influence of loading positions of mandibular unilateral distal extension removable partial dentures on movements of abutment tooth and denture base. J. Med. Dent. Sci. 2004, 51, 155–163. [Google Scholar]
- Radović, K.; Čairović, A.; Todorović, A.; Stančić, I.; Grbović, A. Comparative analysis of unilateral removable partial denture and classical removable partial denture by using finite element method. Srp. Arh. Za Celok. Lek. 2010, 138, 706–713. [Google Scholar] [CrossRef]
- Andrei, O.C.; Dăguci, C.; Ţierean, M.H.; Farcaşiu, T.A.; Farcaşiu, C.; Tănăsescu, L.A. Compared stress levels of removable partial dentures with attachments with and without distal implants—A finite element analysis. In Proceedings of the 2015 E-Health and Bioengineering Conference (EHB), Iasi, Romania, 19–21 November 2015; pp. 1–4. [Google Scholar] [CrossRef]
- Eom, J.W.; Lim, Y.J.; Kim, M.J.; Kwon, H.B. Three-dimensional finite element analysis of implant-assisted removable partial dentures. J. Prosthet. Dent. 2017, 117, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Patrnogić, V.; Todorović, A.; Sćepanović, M.; Radović, K.; Vesnić, J.; Grbović, A. Free-end saddle length influence on stress level in unilateral complex partial denture abutment teeth and retention elements. Vojn. Pregl. 2013, 70, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Mousa, M.A.; Abdullah, J.Y.; Jamayet, N.B.; El-Anwar, M.I.; Ganji, K.K.; Alam, M.K.; Husein, A. Biomechanics in Removable Partial Dentures: A Literature Review of FEA-Based Studies. Biomed Res. Int. 2021, 2021, 5699962. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.; de Araújo, R.M.; Ramanzine, N.P.; Santos, N.R.; Dal Piva, A.O.; Borges, A.L.; da Silva, J.M. Mechanical behavior of implant assisted removable partial denture for Kennedy class II. J. Clin. Exp. Dent. 2020, 12, e38–e45. [Google Scholar] [CrossRef] [PubMed]
- ELsyad, M.A.; El Ghany Kabil, A.A.; El Mekawy, N. Effect of Implant Position and Edentulous Span Length on Stresses Around Implants Assisting Claspless Distal Extension Partial Overdentures: An In Vitro Study. J. Oral Implantol. 2017, 43, 100–106. [Google Scholar] [CrossRef]
- Jensen, C.; Speksnijder, C.M.; Raghoebar, G.M.; Kerdijk, W.; Meijer, H.; Cune, M.S. Implant-supported mandibular removable partial dentures: Functional, clinical and radiographical parameters in relation to implant position. Clin. Implant Dent. Relat. Res. 2017, 19, 432–439. [Google Scholar] [CrossRef]
- Choi, J.; Lee, J.; Song, K.; Park, J.; Kim, K.; Seo, J. Complication and management of implant-assisted removable partial denture with distal extension: A clinical report. J. Dent. Rehabil. Appl. Sci. 2016, 32, 338–344. [Google Scholar] [CrossRef] [Green Version]
- Mously, H.A. Effect of Two Implant-supported Partial Overdenture Attachment Design on the Periodontal Health. J. Contemp. Dent. Pract. 2020, 21, 68–72. [Google Scholar] [CrossRef]
- Putra Wigianto, A.Y.; Goto, T.; Iwawaki, Y.; Ishida, Y.; Watanabe, M.; Ichikawa, T. Treatment outcomes of implant-assisted removable partial denture with distal extension based on the Kennedy classification and attachment type: A systematic review. Int. J. Implant Dent. 2021, 7, 111. [Google Scholar] [CrossRef]
- Lian, M.; Zhao, K.; Feng, Y.; Yao, Q. Prognosis of Combining Remaining Teeth and Implants in Double-Crown-Retained Removable Dental Prostheses: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 281–297. [Google Scholar] [CrossRef] [Green Version]
- Rammelsberg, P.; Bernhart, G.; Lorenzo Bermejo, J.; Schmitter, M.; Schwarz, S. Prognosis of implants and abutment teeth under combined tooth-implant-supported and solely implant-supported double-crown-retained removable dental prostheses. Clin. Oral Implant. Res. 2014, 25, 813–818. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).