Technology Behavior Model—Impact of Extended Reality on Patient Surgery
Abstract
:1. Introduction
2. Literature Review
2.1. Virtual Surgery
2.2. Eye Tracking
2.3. Image
3. Materials and Framework
3.1. Technology Acceptance Model
3.2. Theory of Planned Behavior
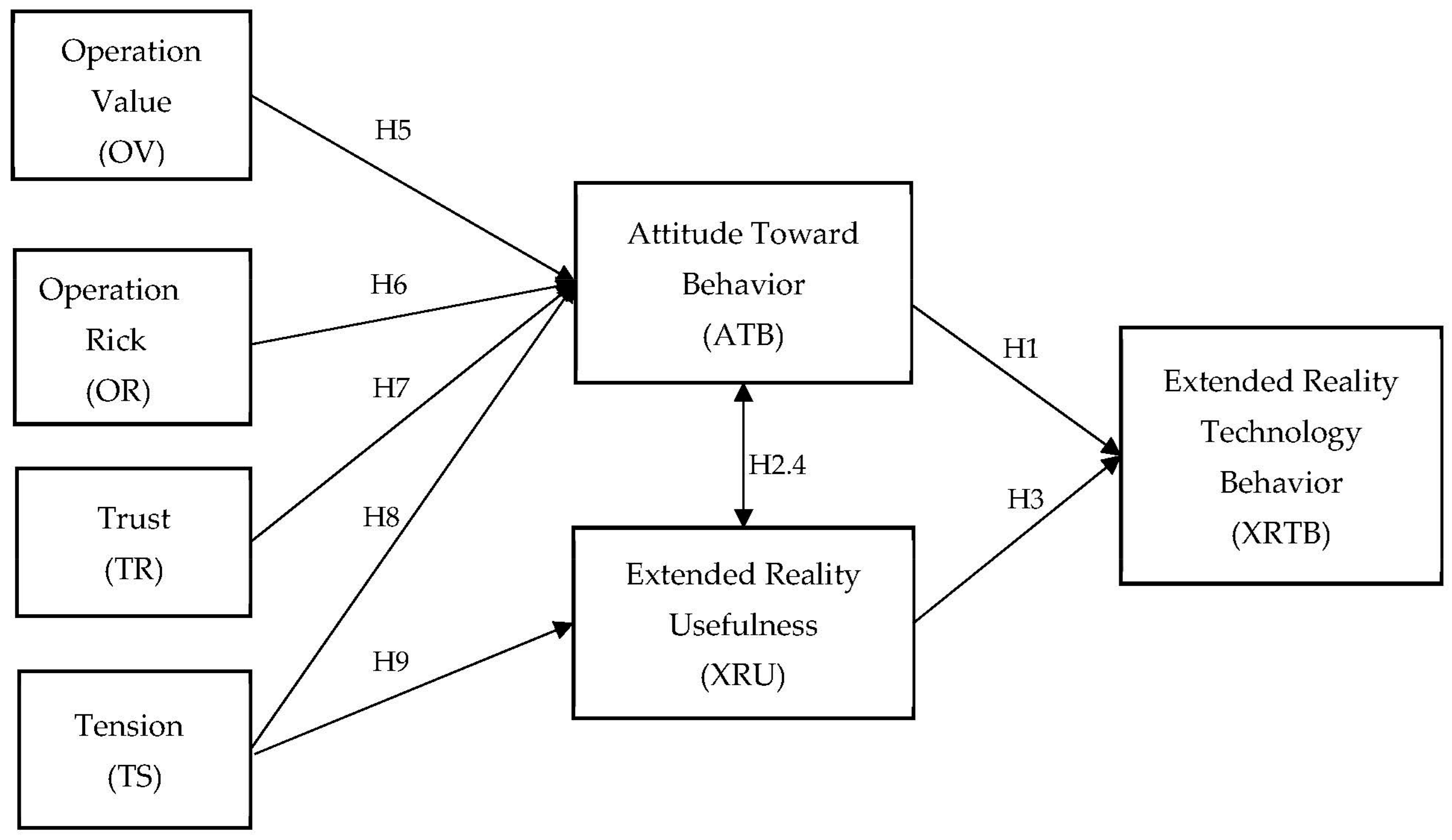
3.3. Technology Behavior Model
3.4. Determinants
3.4.1. Attitude toward Behavior (ATB)
3.4.2. Extended Reality Usefulness (XRU)
3.4.3. Operation Value (OV)
3.4.4. Operation Risk (OR)
3.4.5. Trust (TR)
3.4.6. Tension (TS)
3.5. Theoretical Framework
4. Methodology
5. Data Analysis
5.1. Demographic Analysis
5.2. Statistical Analysis
5.2.1. Common-Method Bias
5.2.2. Assessing the Outer Measurement Model
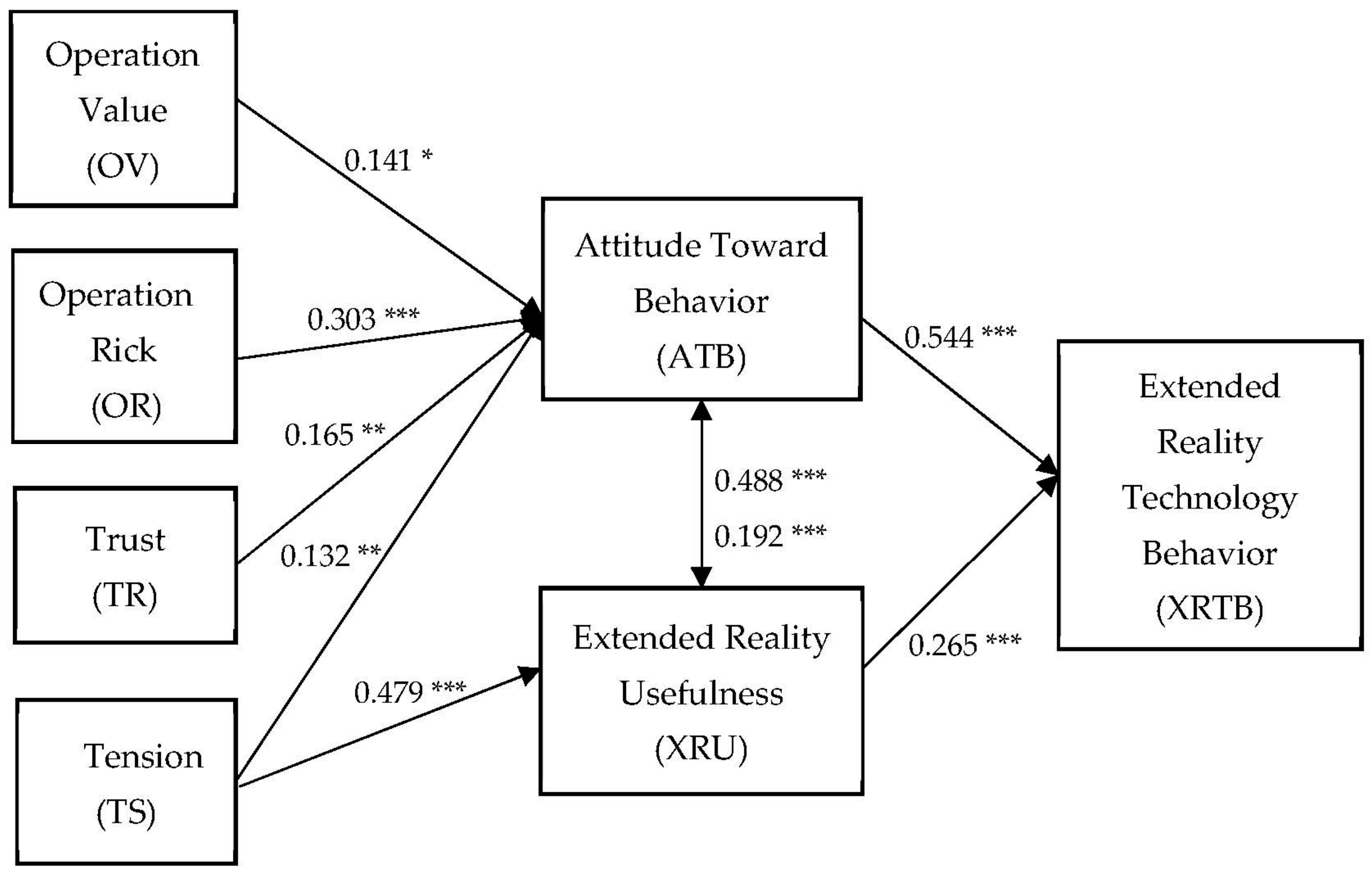
5.2.3. Structural Model
5.2.4. Predictive Relevance and Effect Size
5.2.5. Importance Performance Map
6. Findings and Discussion
7. Conclusions and Future Works
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ayers, B.; Kilic, A. Extended Reality Platforms: A Technological Solution Still Finding the Right Problem. Ann. Thorac. Surg. 2022, 113, 691. [Google Scholar] [CrossRef] [PubMed]
- Costantino, A.; Caprioli, F.; Elli, L.; Roncoroni, L.; Stocco, D.; Doneda, L.; Nandi, N.; Conforti, F.S.; Noviello, D.; Penagini, R.; et al. Determinants of patient trust in gastroenterology televisits: Results of machine learning analysis. Inform. Med. Unlocked 2022, 29, 100867. [Google Scholar] [CrossRef]
- Klinker, K.; Wiesche, M.; Krcmar, H. Smart glasses in health care: A patient trust perspective. In Proceedings of the 53rd Hawaii International Conference on System Sciences, Maui, HI, USA, 7–10 January 2020. [Google Scholar]
- Cho, H.E.; Billig, J.I.; Byrnes, M.E.; Haase, S.C.; Waljee, J.F.; Chung, K.C. Trust and Distrust in Opioid Decision-Making: A Qualitative Assessment of Patient-Doctor Relationship. J. Hand. Surg. Am. 2022, 47, 151–159.e1. [Google Scholar] [CrossRef]
- Dario, P.; Hannaford, B.; Menciassi, A. Smart surgical tools and augmenting devices. IEEE Trans. Robot. Autom. 2003, 19, 782–792. [Google Scholar] [CrossRef]
- Gong, X.; JosephNg, P.S. Technology Behavior Model—Beyond Your Sight with Extended Reality in Surgery. Appl. Syst. Innov. 2022, 5, 35. [Google Scholar] [CrossRef]
- DePalma, L.J.; Olsen, L.D.; Evans, J.H. Patient narratives of hope in stem cell technologies: Trust in biomedicine and the body’s natural ability to heal itself. Health 2021, 13634593211046834. [Google Scholar] [CrossRef]
- Hu, H.; Gong, H.; Wu, X.; Wu, X. Effect of patient-provider communication on patient risk awareness: The moderating role of trust based on scenario experiment. Psych J. 2022. [Google Scholar] [CrossRef] [PubMed]
- Gagandeep, S.; Tejasvi, K.; Nihal, M.; Shubham, J.; Anatoliy, V.; Vadim, S.; Prateek, P.; Sunil, M. Long-term solutions in neurosurgery using extended reality technologies. Neurosurg. Focus 2021, 51, E2. [Google Scholar] [CrossRef]
- Lareyre, F.; Chaudhuri, A.; Adam, C.; Carrier, M.; Mialhe, C.; Raffort, J. Applications of Head-Mounted Displays and Smart Glasses in Vascular Surgery. Ann. Vasc. Surg. 2021, 75, 497–512. [Google Scholar] [CrossRef]
- Lin, T.; Huang, L.; Hannaford, B.; Tran, C.; Raiti, J.; Zaragoza, R.; Feng, T.; Wagner, L.; James, J. Empathics system. In Proceedings of the 13th ACM International Conference on PErvasive Technologies Related to Assistive Environments, Corfu, Greece, 30 June–3 July 2020; pp. 1–4. [Google Scholar]
- Lungu, A.J.; Swinkels, W.; Claesen, L.; Tu, P.; Egger, J.; Chen, X. A review on the applications of virtual reality, augmented reality and mixed reality in surgical simulation: An extension to different kinds of surgery. Expert. Rev. Med. Devices 2021, 18, 47–62. [Google Scholar] [CrossRef]
- Sadeghi, A.H.; Mathari, S.E.; Abjigitova, D.; Maat, A.; Taverne, Y.; Bogers, A.; Mahtab, E.A.F. Current and Future Applications of Virtual, Augmented, and Mixed Reality in Cardiothoracic Surgery. Ann. Thorac. Surg. 2022, 113, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Pei, H.; Huang, X.; Ding, M. Image visualization: Dynamic and static images generate users’ visual cognitive experience using eye-tracking technology. Displays 2022, 73, 102175. [Google Scholar] [CrossRef]
- Korečko, Š.; Hudák, M.; Sobota, B.; Sivý, M.; Pleva, M.; Steingartner, W. Experimental Performance Evaluation of Enhanced User Interaction Components for Web-Based Collaborative Extended Reality. Appl. Sci. 2021, 11, 3811. [Google Scholar] [CrossRef]
- van der Linde-van den Bor, M.; Frans-Rensen, S.A.; Slond, F.; Liesdek, O.C.D.; de Heer, L.M.; Suyker, W.J.L.; Jaarsma, T.; Weldam, S.W.M. Patients’ voices in the development of pre-surgical patient education using virtual reality: A qualitative study. PEC Innov. 2022, 1, 100015. [Google Scholar] [CrossRef]
- Xi, N.; Bampouni, E.; Hamari, J. How Does Extended Reality Influence Consumer Decision Making? The Empirical Evidence from A Laboratory Experiment. In Proceedings of the 55th Hawaii International Conference on System Sciences, Maui, HI, USA, 4–7 January 2022. [Google Scholar]
- Mikami, B.S.; Hynd, T.E.; Lee, U.Y.; DeMeo, J.; Thompson, J.D.; Sokiranski, R.; Doll, S.; Lozanoff, S. Extended reality visualization of medical museum specimens: Online presentation of conjoined twins curated by Dr. Jacob Henle between 1844–1852. Transl. Res. Anat. 2022, 27, 100171. [Google Scholar] [CrossRef]
- Hu, L.; Chen, M.; Liu, P.X.; Xu, S. A vortex method of 3D smoke simulation for virtual surgery. Comput. Methods Programs Biomed. 2021, 198, 105813. [Google Scholar] [CrossRef]
- Klaib, A.F.; Alsrehin, N.O.; Melhem, W.Y.; Bashtawi, H.O.; Magableh, A.A. Eye tracking algorithms, techniques, tools, and applications with an emphasis on machine learning and Internet of Things technologies. Expert. Syst. Appl. 2021, 166, 114037. [Google Scholar] [CrossRef]
- Tesfamikael, H.H.; Fray, A.; Mengsteab, I.; Semere, A.; Amanuel, Z. Simulation of Eye Tracking Control based Electric Wheelchair Construction by Image Segmentation Algorithm. J. Innov. Image Proc. 2021, 3, 21–35. [Google Scholar] [CrossRef]
- Kapp, S.; Barz, M.; Mukhametov, S.; Sonntag, D.; Kuhn, J. ARETT: Augmented Reality Eye Tracking Toolkit for Head Mounted Displays. Sensors 2021, 21, 2234. [Google Scholar] [CrossRef]
- Qian, K.; Arichi, T.; Price, A.; Dall’Orso, S.; Eden, J.; Noh, Y.; Rhode, K.; Burdet, E.; Neil, M.; Edwards, A.D.; et al. An eye tracking based virtual reality system for use inside magnetic resonance imaging systems. Sci. Rep. 2021, 11, 16301. [Google Scholar] [CrossRef]
- Karargyris, A.; Kashyap, S.; Lourentzou, I.; Wu, J.T.; Sharma, A.; Tong, M.; Abedin, S.; Beymer, D.; Mukherjee, V.; Krupinski, E.A.; et al. Creation and validation of a chest X-ray dataset with eye-tracking and report dictation for AI development. Sci. Data 2021, 8, 92. [Google Scholar] [CrossRef] [PubMed]
- Dimigen, O.; Ehinger, B.V. Regression-based analysis of combined EEG and eye-tracking data: Theory and applications. J. Vis. 2021, 21, 3. [Google Scholar] [CrossRef] [PubMed]
- Palaniappan, P.; Meyer, S.; Radler, M.; Kamp, F.; Belka, C.; Riboldi, M.; Parodi, K.; Gianoli, C. X-ray CT adaptation based on a 2D-3D deformable image registration framework using simulated in-room proton radiographies. Phys. Med. Biol. 2022, 67, 045003. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Zhang, Q.; Sun, Y.; Shen, Y.; Wang, X. Grayscale medical image segmentation method based on 2D&3D object detection with deep learning. BMC Med. Imaging 2022, 22, 33. [Google Scholar]
- Miyashita, Y.; Sawahata, Y.; Komine, K. Perceptual Assessment of Image and Depth Quality of Dynamically Depth-compressed Scene for Automultiscopic 3D Display. IEEE Trans. Vis. Comput. Graph 2022, 1–15. [Google Scholar] [CrossRef]
- Ye, R.Z.; Noll, C.; Richard, G.; Lepage, M.; Turcotte, E.E.; Carpentier, A.C. DeepImageTranslator: A free, user-friendly graphical interface for image translation using deep-learning and its applications in 3D CT image analysis. SLAS Technol. 2022, 27, 76–84. [Google Scholar] [CrossRef]
- Dhou, S.; Alkhodari, M.; Ionascu, D.; Williams, C.; Lewis, J.H. Fluoroscopic 3D Image Generation from Patient-Specific PCA Motion Models Derived from 4D-CBCT Patient Datasets: A Feasibility Study. J. Imaging 2022, 8, 17. [Google Scholar] [CrossRef]
- Chen, Q.Q.; Sun, Z.H.; Wei, C.F.; Wu, E.Q.; Ming, D. Semi-supervised 3D Medical Image Segmentation Based on Dual-task Consistent joint Learning and Task-Level Regularization. IEEE/ACM Trans. Comput. Biol. Bioinform. 2022. [Google Scholar] [CrossRef]
- Jang, J.; Ko, Y.; Shin, W.S.; Han, I. Augmented Reality and Virtual Reality for Learning: An Examination Using an Extended Technology Acceptance Model. IEEE Access 2021, 9, 6798–6809. [Google Scholar] [CrossRef]
- Unal, E.; Uzun, A.M. Understanding university students’ behavioral intention to use Edmodo through the lens of an extended technology acceptance model. Br. J. Educ. Technol. 2020, 52, 619–637. [Google Scholar] [CrossRef]
- Yuen, K.F.; Cai, L.; Qi, G.; Wang, X. Factors influencing autonomous vehicle adoption: An application of the technology acceptance model and innovation diffusion theory. Technol. Anal. Strateg. Manag. 2020, 33, 505–519. [Google Scholar] [CrossRef]
- Murillo, G.G.; Novoa-Hernández, P.; Rodríguez, R.S. Technology Acceptance Model and Moodle: A systematic mapping study. Inf. Dev. 2020, 37, 617–632. [Google Scholar] [CrossRef]
- Alsharida, R.A.; Hammood, M.M.; Al-Emran, M. Mobile Learning Adoption: A Systematic Review of the Technology Acceptance Model from 2017 to 2020. Int. J. Emerg. Technol. Learn. 2021, 16, 147–162. [Google Scholar] [CrossRef]
- Alfadda, H.A.; Mahdi, H.S. Measuring Students’ Use of Zoom Application in Language Course Based on the Technology Acceptance Model (TAM). J. Psycholinguist. Res. 2021, 50, 883–900. [Google Scholar] [CrossRef]
- Fussell, S.G.; Truong, D. Using virtual reality for dynamic learning: An extended technology acceptance model. Virtual Real. 2022, 26, 249–267. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior: Frequently asked questions. Hum. Behav. Emerg. Technol. 2020, 2, 314–324. [Google Scholar] [CrossRef]
- Sok, J.; Borges, J.R.; Schmidt, P.; Ajzen, I. Farmer Behaviour as Reasoned Action: A Critical Review of Research with the Theory of Planned Behaviour. J. Agric. Econ. 2020, 72, 388–412. [Google Scholar] [CrossRef]
- McTaggart-Cowan, H.; Bentley, C.; Raymakers, A.; Metcalfe, R.; Hawley, P.; Peacock, S. Understanding cancer survivors’ reasons to medicate with cannabis: A qualitative study based on the theory of planned behavior. Cancer Med. 2021, 10, 396–404. [Google Scholar] [CrossRef]
- Bosnjak, M.; Ajzen, I.; Schmidt, P. The Theory of Planned Behavior: Selected Recent Advances and Applications. Eur. J. Psychol. 2020, 16, 352–356. [Google Scholar] [CrossRef]
- Fan, C.W.; Chen, I.H.; Ko, N.Y.; Yen, C.F.; Lin, C.Y.; Griffiths, M.D.; Pakpour, A.H. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Hum. Vaccin. Immunother. 2021, 17, 3413–3420. [Google Scholar] [CrossRef]
- JosephNg, P.S. EaaS Optimization: Available yet hidden information technology infrastructure inside medium size enterprise. Technol. Forecast. Soc. Chang. 2018, 132, 165–173. [Google Scholar] [CrossRef]
- Hagger, M.S.; Cheung, M.W.; Ajzen, I.; Hamilton, K. Perceived behavioral control moderating effects in the theory of planned behavior: A meta-analysis. Health Psychol. 2022, 41, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.A.; Sheeran, P.; Fong, G.T.; Cheah, C.S.L.; Oremus, M.; Liu-Ambrose, T.; Sakib, M.N.; Butt, Z.A.; Ayaz, H.; Jandu, N.; et al. Biobehavioral Aspects of the COVID-19 Pandemic: A Review. Psychosom. Med. 2021, 83, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef] [PubMed]
- Murillo, R.; Fernandez-Deaza, G.; Zuluaga, M.; Lewison, G.; Usgame-Zubieta, D.; Usgame-Zubieta, I.D.; Manrique, M.M. Cancer Research in the Time of COVID-19: A Colombian Narrative. Front. Public Health 2021, 9, 750755. [Google Scholar] [CrossRef]
- Pittig, A.; Hoyer, J.; Noack, R. Smart-Glass Guided Exposure for Anxiety Disorders: A Proof-of-Concept Study. Cogn. Behav. Pract. 2021, 28, 364–378. [Google Scholar] [CrossRef]
- Bai, L.; Li, Y.; Cen, M.; Hu, F. 3D Instance Segmentation and Object Detection Framework Based on the Fusion of Lidar Remote Sensing and Optical Image Sensing. Remote Sens. 2021, 13, 3288. [Google Scholar] [CrossRef]
- Baldoto Gava Chakr, V.C. Building up trust in the doctor-patient relationship. Andes Pediatr. 2021, 92, 480–482. [Google Scholar] [CrossRef]
- Kapikiran, G.; Bulbuloglu, S.; Saritas, S. The Effect of Video Training before Organ Transplant Surgery on Patient Satisfaction and Anxiety: Head Mounted Display Effect. Clin. Simul. Nurs. 2022, 62, 99–106. [Google Scholar] [CrossRef]
- Rutkowski, S.; Czech, O.; Wrzeciono, A.; Kiper, P.; Szczepanska-Gieracha, J.; Malicka, I. Virtual reality as a chemotherapy support in treatment of anxiety and fatigue in patients with cancer: A systematic review and meta-analysis and future research directions. Complement. Med. 2021, 61, 102767. [Google Scholar] [CrossRef]
- Basco, R.; Hair, J.F.; Ringle, C.M.; Sarstedt, M. Advancing family business research through modeling nonlinear relationships: Comparing PLS-SEM and multiple regression. J. Fam. Bus. Strategy 2021. [Google Scholar] [CrossRef]
- Low, M.P.; Cham, T.H.; Chang, Y.S.; Lim, X.J. Advancing on weighted PLS-SEM in examining the trust-based recommendation system in pioneering product promotion effectiveness. Qual. Quant. 2021, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Mena, J.A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2011, 40, 414–433. [Google Scholar] [CrossRef]
- Dash, G.; Paul, J. CB-SEM vs PLS-SEM methods for research in social sciences and technology forecasting. Technol. Forecast. Soc. Chang. 2021, 173, 121092. [Google Scholar] [CrossRef]
- Yoo, W.; Yu, E.; Jung, J. Drone delivery: Factors affecting the public’s attitude and intention to adopt. Telemat. Inform. 2018, 35, 1687–1700. [Google Scholar] [CrossRef]
- Astrachan, C.B.; Patel, V.K.; Wanzenried, G. A comparative study of CB-SEM and PLS-SEM for theory development in family firm research. J. Fam. Bus. Strategy 2014, 5, 116–128. [Google Scholar] [CrossRef]
- Ali, S.; Javed, H.M.U.; Danish, M. Adoption of green IT in Pakistan: A comparison of three competing models through model selection criteria using PLS-SEM. Env. Sci. Pollut. Res. Int. 2021, 28, 36174–36192. [Google Scholar] [CrossRef]
- Min, J.; Iqbal, S.; Khan, M.A.S.; Akhtar, S.; Anwar, F.; Qalati, S.A. Impact of supervisory behavior on sustainable employee performance: Mediation of conflict management strategies using PLS-SEM. PLoS ONE 2020, 15, e0236650. [Google Scholar] [CrossRef]
- Manley, S.C.; Hair, J.F.; Williams, R.I.; McDowell, W.C. Essential new PLS-SEM analysis methods for your entrepreneurship analytical toolbox. Int. Entrep. Manag. J. 2020, 17, 1805–1825. [Google Scholar] [CrossRef]
- Li, Z.; Wei, Y.; Li, Y.; Wang, Z.; Zhang, J. China’s Provincial Eco-Efficiency and Its Driving Factors-Based on Network DEA and PLS-SEM Method. Int. J. Env. Res Public Health 2020, 17, 8702. [Google Scholar] [CrossRef]
- Hidayanto, A.N.; Anggorojati, B.; Abidin, Z.; Phusavat, K. Data modeling positive security behavior implementation among smart device users in Indonesia: A partial least squares structural equation modeling approach (PLS-SEM). Data Brief 2020, 30, 105588. [Google Scholar]
- Li, X.; Du, J.; Long, H. Mechanism for Green Development Behavior and Performance of Industrial Enterprises (GDBP-IE) Using Partial Least Squares Structural Equation Modeling (PLS-SEM). Int. J. Env. Res Public Health 2020, 17, 8450. [Google Scholar] [CrossRef] [PubMed]
- JosephNg, P. EaaS infrastructure disruptor for MSE. Int. J. Bus. Inf. Syst. 2019, 30, 373–385. [Google Scholar]
- Lin, L.; Huang, Z.; Othman, B.; Luo, Y. Let’s make it better: An updated model interpreting international student satisfaction in China based on PLS-SEM approach. PLoS ONE 2020, 15, e0233546. [Google Scholar] [CrossRef]
- Hair, J.F.; Astrachan, C.B.; Moisescu, O.I.; Radomir, L.; Sarstedt, M.; Vaithilingam, S.; Ringle, C.M. Executing and interpreting applications of PLS-SEM: Updates for family business researchers. J. Fam. Bus. Strategy 2021, 12, 100392. [Google Scholar] [CrossRef]
- Martínez, M.d.C.V.; Cervantes, P.A.M. (Eds.) Partial Least Squares Structural Equation Modeling (PLS-SEM) Applications in Economics and Finance; MDPI AG: Basel, Switzerland, 2021. [Google Scholar]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 3rd ed.; SAGE: Los Angeles, CA, USA, 2022. [Google Scholar]
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M.; Danks, N.P.; Ray, S. Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook, 1st ed.; Springer International Publishing: Cham, Switzerland, 2021. [Google Scholar]
- Anggraini, R.D.S.; Patricia, P. Pengaruh Attitude Toward Behavior, Perceived Behavioral Control, dan Subjective Norm terhadap Entrepreneurial Intention Mahasiswa Non-Ekonomi. Ekon. Dan Bisnis 2019, 5, 96–105. [Google Scholar] [CrossRef] [Green Version]
- Alizadehsalehi, S.; Hadavi, A.; Huang, J.C. From BIM to extended reality in AEC industry. Autom. Constr. 2020, 116, 103254. [Google Scholar] [CrossRef]
- Taylor, L.; Dyer, T.; Al-Azzawi, M.; Smith, C.; Nzeako, O.; Shah, Z. Extended reality anatomy undergraduate teaching: A literature review on an alternative method of learning. Ann. Anat. Anat. Anz. 2022, 239, 151817. [Google Scholar] [CrossRef]
- Gong, X.; Wong, A.H.; Daronovna, R.K.; JosephNg, P. Beyond Human Eye in Surgical Smart Glasses. In Proceedings of the 5th International Conference on Algorithms, Computing and Systems, Xi’an, China, 24–26 September 2021; pp. 135–139. [Google Scholar]
- Ratcliffe, J.; Soave, F.; Bryan-Kinns, N.; Tokarchuk, L.; Farkhatdinov, I. Extended Reality (XR) Remote Research: A Survey of Drawbacks and Opportunities. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, New York, NY, USA; 2021; pp. 1–13. [Google Scholar] [CrossRef]
- Kim, A.S.; Cheng, W.C.; Beams, R.; Badano, A. Color Rendering in Medical Extended-Reality Applications. J. Digit. Imaging 2021, 34, 16–26. [Google Scholar] [CrossRef]
- Tabrizi, S.; Trippa, L.; Cagney, D.; Aizer, A.A.; Tanguturi, S.; Ventz, S.; Fell, G.; Bellon, J.R.; Mamon, H.; Nguyen, P.L. Assessment of simulated SARS-CoV-2 infection and mortality risk associated with radiation therapy among patients in 8 randomized clinical trials. JAMA Netw. Open 2021, 4, e213304. [Google Scholar] [CrossRef]
- Turani, A.A.; Alkhateeb, J.H.; Alsewari, A.A. Students Online Exam Proctoring: A Case Study Using 360 Degree Security Cameras. In Proceedings of the 2020 Emerging Technology in Computing, Communication and Electronics (ETCCE), Dhaka, Bangladesh, 21–22 December 2020; pp. 1–5. [Google Scholar]

| Demographic Characteristic | Options | Counts | Percentage (%) |
|---|---|---|---|
| Gender | Male | 164 | 54.67% |
| Female | 136 | 45.33% | |
| Age | 20–35 | 23 | 7.67% |
| 36–45 | 63 | 21.00% | |
| 46–55 | 91 | 30.33% | |
| Older than 56 | 123 | 41.00% | |
| Marital status | Single | 52 | 17.33% |
| Married | 248 | 82.77% | |
| Education | Junior and lower | 11 | 3.67% |
| High school | 47 | 15.67% | |
| Undergraduate | 153 | 51.00% | |
| Postgraduate | 89 | 29.67% | |
| Income | Less than MYR 3000 | 6 | 2.00% |
| MYR 3000–5000 | 89 | 29.67% | |
| MYR 5000–8000 | 118 | 39.33% | |
| MYR 8000–10000 | 52 | 17.33% | |
| More than MYR 10,000 | 35 | 11.67% |
| Latent Construct | Indicators | Substantive Factor Loading (Ra) | Substantial Variance Square (Ra2) | Method Factor Loading (Rb) | Method Variance Square (Rb2) |
|---|---|---|---|---|---|
| ATB | ATB1 | 0.9259 | 0.857291 | 0.0909 | 0.008263 *** |
| ATB2 | 0.9279 | 0.860998 | −0.1451 | 0.021054 ** | |
| ATB3 | 0.8964 | 0.803533 | 0.0494 | 0.002440 NS | |
| OR | OR1 | 0.9287 | 0.862484 | −0.0553 | 0.003058 NS |
| OR2 | 0.9173 | 0.841439 | 0.2414 | 0.058274 * | |
| OR3 | 0.9324 | 0.86937 | −0.1886 | 0.035570 ** | |
| OV | OV1 | 0.8997 | 0.80946 | 0.0332 | 0.001102 *** |
| OV2 | 0.9404 | 0.884352 | 0.0261 | 0.000681 NS | |
| OV3 | 0.9106 | 0.829192 | −0.0599 | 0.003588 *** | |
| TS | TS1 | 0.9276 | 0.860442 | −0.0753 | 0.005670 *** |
| TS2 | 0.9249 | 0.85544 | 0.0497 | 0.002470 *** | |
| TS3 | 0.9033 | 0.815951 | 0.0255 | 0.000650 NS | |
| AXRS | AXRS1 | 0.8902 | 0.792456 | 0.0588 | 0.003457 *** |
| AXRS2 | 0.9372 | 0.878344 | −0.1275 | 0.016256 ** | |
| AXRS3 | 0.9356 | 0.875347 | 0.0677 | 0.004583 *** | |
| TR | TR1 | 0.9351 | 0.874412 | −0.0022 | 0.000005 NS |
| TR2 | 0.9461 | 0.895105 | −0.0309 | 0.000955 NS | |
| TR3 | 0.9243 | 0.85433 | 0.0336 | 0.001129 *** | |
| XRU | XRU1 | 0.8992 | 0.808561 | −0.1105 | 0.012210 ** |
| XRU2 | 0.9178 | 0.842357 | 0.1067 | 0.011385 ** | |
| XRU3 | 0.9431 | 0.889438 | −0.0039 | 0.000015 NS | |
| AVD | 0.850491 | 0.009182 *** |
| Latent Construct | Items | Loadings | Standard Deviation | RhoA (ρA) | Composite Reliability | Average Variance Extracted (AVE) |
|---|---|---|---|---|---|---|
| ATB | ATB1 | 0.927 | 0.364 | 0.907 | 0.940 | 0.840 |
| ATB2 | 0.925 | |||||
| ATB3 | 0.898 | |||||
| OR | OR1 | 0.930 | 0.36 | 0.926 | 0.947 | 0.857 |
| OR2 | 0.923 | |||||
| OR3 | 0.924 | |||||
| OV | OV1 | 0.901 | 0.363 | 0.907 | 0.941 | 0.841 |
| OV2 | 0.941 | |||||
| OV3 | 0.909 | |||||
| TS | TS1 | 0.923 | 0.363 | 0.910 | 0.942 | 0.844 |
| TS2 | 0.922 | |||||
| TS3 | 0.910 | |||||
| AXRS | AXRS1 | 0.893 | 0.362 | 0.915 | 0.944 | 0.848 |
| AXRS2 | 0.933 | |||||
| AXRS3 | 0.937 | |||||
| TR | TR1 | 0.934 | 0.356 | 0.929 | 0.954 | 0.875 |
| TR2 | 0.945 | |||||
| TR3 | 0.927 | |||||
| XRU | XRU1 | 0.890 | 0.362 | 0.922 | 0.943 | 0.846 |
| XRU2 | 0.925 | |||||
| XRU3 | 0.944 |
| Latent Construct | ATB | OR | OV | TS | AXRS | TR | XRU |
|---|---|---|---|---|---|---|---|
| ATB | |||||||
| OR | 0.743 | ||||||
| OV | 0.649 | 0.678 | |||||
| TS | 0.597 | 0.624 | 0.625 | ||||
| AXRS | 0.772 | 0.642 | 0.654 | 0.684 | |||
| TR | 0.638 | 0.665 | 0.541 | 0.436 | 0.601 | ||
| XRU | 0.662 | 0.650 | 0.570 | 0.519 | 0.642 | 0.622 |
| Latent Construct | Original Sample (O) | Sample Mean (M) | Bias | 2.50% | 97.50% |
|---|---|---|---|---|---|
| ATB -> AXRS | 0.672 | 0.671 | −0.001 | 0.588 | 0.746 |
| ATB -> XRU | 0.488 | 0.488 | 0.000 | 0.370 | 0.597 |
| XRU -> ATB | 0.192 | 0.192 | −0.001 | 0.092 | 0.298 |
| OR -> ATB | 0.350 | 0.348 | −0.002 | 0.245 | 0.466 |
| OR -> AXRS | 0.235 | 0.234 | −0.001 | 0.163 | 0.320 |
| OR -> XRU | 0.171 | 0.170 | −0.001 | 0.109 | 0.246 |
| OV -> ATB | 0.172 | 0.172 | 0.001 | 0.052 | 0.287 |
| OV -> AXRS | 0.115 | 0.116 | 0.001 | 0.036 | 0.200 |
| OV -> XRU | 0.084 | 0.085 | 0.001 | 0.025 | 0.153 |
| TS -> ATB | 0.158 | 0.156 | −0.002 | 0.064 | 0.257 |
| TS -> AXRS | 0.163 | 0.163 | 0.000 | 0.092 | 0.243 |
| TS -> XRU | 0.291 | 0.289 | −0.002 | 0.187 | 0.401 |
| TR -> ATB | 0.220 | 0.224 | 0.003 | 0.123 | 0.322 |
| TR -> AXRS | 0.148 | 0.150 | 0.002 | 0.082 | 0.219 |
| TR -> XRU | 0.108 | 0.109 | 0.002 | 0.058 | 0.168 |
| XRU -> AXRS | 0.265 | 0.266 | 0.001 | 0.136 | 0.389 |
| Hyp | PLS Paths | Original Sample (O) | Sample Mean (M) | Standard Deviation (STDEV) | T Statistics (O/STDEV) | p Values | 2.5% | 97.5% | Remarks |
|---|---|---|---|---|---|---|---|---|---|
| H1 | ATB -> AXRS | 0.543 | 0.542 | 0.061 | 8.943 | 0.000 *** | 0.418 | 0.656 | YES |
| H2 | ATB -> XRU | 0.488 | 0.488 | 0.058 | 8.417 | 0.000 *** | 0.373 | 0.601 | YES |
| H3 | XRU -> AXRS | 0.265 | 0.266 | 0.064 | 4.152 | 0.000 *** | 0.139 | 0.391 | YES |
| H4 | XRU -> ATB | 0.192 | 0.192 | 0.053 | 3.625 | 0.000 *** | 0.090 | 0.296 | YES |
| H5 | OV -> ATB | 0.141 | 0.142 | 0.056 | 2.539 | 0.011 * | 0.033 | 0.252 | YES |
| H6 | OR -> ATB | 0.303 | 0.302 | 0.052 | 5.802 | 0.000 *** | 0.201 | 0.405 | YES |
| H7 | TR -> ATB | 0.165 | 0.167 | 0.054 | 3.063 | 0.002 ** | 0.064 | 0.275 | YES |
| H8 | TS -> ATB | 0.132 | 0.130 | 0.048 | 2.766 | 0.006 ** | 0.036 | 0.222 | YES |
| H9 | TS -> XRU | 0.479 | 0.477 | 0.058 | 8.279 | 0.000 *** | 0.358 | 0.585 | YES |
| Endogenous Construct | SSO | SSE | Q2 (=1−SSE/SSO) | Predictive Relevance |
|---|---|---|---|---|
| ATB | 3600.000 | 1694.572 | 0.529 | Q2 > 0 |
| OR | 900.000 | 298.145 | 0.669 | Q2 > 0 |
| OV | 900.000 | 323.752 | 0.640 | Q2 > 0 |
| TS | 900.000 | 319.077 | 0.645 | Q2 > 0 |
| AXRS | 6300.000 | 3140.999 | 0.501 | Q2 > 0 |
| TR | 900.000 | 271.190 | 0.699 | Q2 > 0 |
| XRU | 5400.000 | 2721.810 | 0.496 | Q2 > 0 |
| AXRS | PLS-SEM | Linear Model Benchmark | ||||
|---|---|---|---|---|---|---|
| Q2_Predict | RMSE | MAE | Q2_Predict | RMSE | MAE | |
| AXRS1 | 0.443 | 0.778 | 0.652 | 0.576 | 0.678 | 0.549 |
| AXRS3 | 0.404 | 0.833 | 0.687 | 0.45 | 0.8 | 0.654 |
| AXRS2 | 0.384 | 0.796 | 0.663 | 0.526 | 0.698 | 0.579 |
| Predictor Construct/ Dependent Construct | ATB | OR | OV | TS | AXRS | TR | XRU |
|---|---|---|---|---|---|---|---|
| ATB | 0.349 | 0.489 | |||||
| OR | 0.407 | 0.021 | |||||
| OV | 0.226 | 0.120 | |||||
| TS | 0.266 | 0.213 | |||||
| TR | 0.221 | 0.120 | |||||
| XRU | 0.211 | 0.135 |
| Importance (Total Effect) | Importance (Total Effect) | Performances (Index Value) |
|---|---|---|
| ATB | 0.543 | 71.566 |
| OR | 0.165 | 76.395 |
| OV | 0.076 | 65.287 |
| TS | 0.249 | 65.264 |
| TR | 0.090 | 70.847 |
| XRU | 0.369 | 68.576 |
| Mean Value | 0.249 | 69.656 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
JosephNg, P.S.; Gong, X. Technology Behavior Model—Impact of Extended Reality on Patient Surgery. Appl. Sci. 2022, 12, 5607. https://doi.org/10.3390/app12115607
JosephNg PS, Gong X. Technology Behavior Model—Impact of Extended Reality on Patient Surgery. Applied Sciences. 2022; 12(11):5607. https://doi.org/10.3390/app12115607
Chicago/Turabian StyleJosephNg, Poh Soon, and Xiaoxue Gong. 2022. "Technology Behavior Model—Impact of Extended Reality on Patient Surgery" Applied Sciences 12, no. 11: 5607. https://doi.org/10.3390/app12115607






