Cardiac Radiofrequency Ablation Simulation Using a 3D-Printed Bi-Atrial Thermochromic Model
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
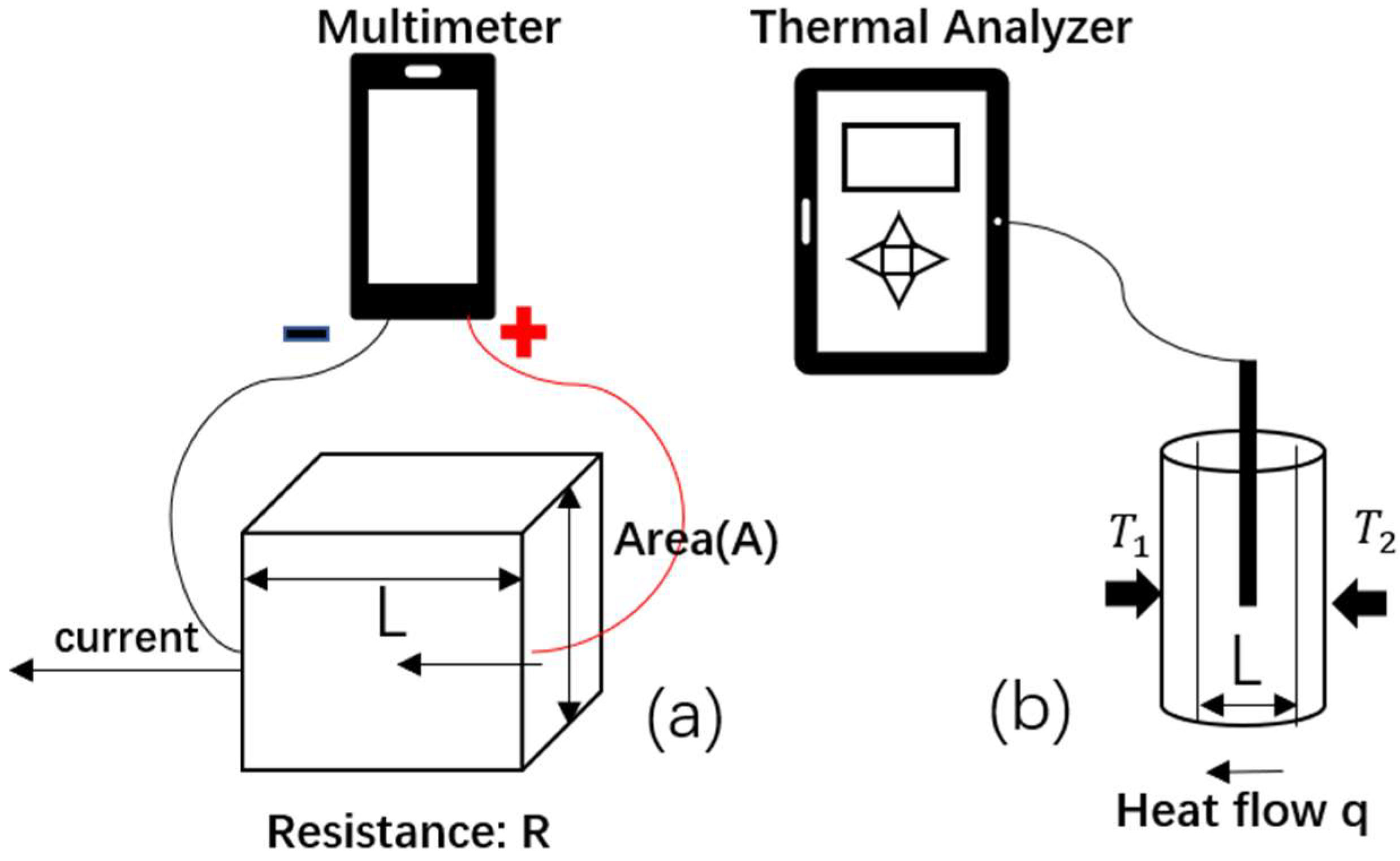
2.1. Layfomm-40 Conductivity Analysis
2.2. Thermochromic Paint Formulation and RFA-Sensitivity
2.3. Inreasing X-ray Visibility
2.4. Atrial Model and Simulator Build-Up
2.5. X-ray Imaging, Mapping, and Ablation
3. Results
3.1. Layfomm-40 Conductivity Analysis
3.2. Thermochromic Paint Formulation and RFA-Sensitivity
3.3. Increasing X-ray Visibility
3.4. Atrial Model and Simulator Build-Up
3.5. X-ray Imaging, Mapping, and Ablation
4. Discussion
5. Conclusions
6. Future Work
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hong, K.L.; Borges, J.; Glover, B. Catheter Ablation for the Management of Atrial Fibrillation: Current Technical Perspectives. Open Heart 2020, 7, e001207. [Google Scholar] [CrossRef] [PubMed]
- De Ponti, R.; Marazzi, R.; Doni, L.A.; Tamborini, C.; Ghiringhelli, S.; Salerno-Uriarte, J.A. Simulator Training Reduces Radiation Exposure and Improves Trainees’ Performance in Placing Electrophysiologic Catheters during Patient-based Procedures. Heart Rhythm. 2012, 9, 1280–1285. [Google Scholar] [CrossRef] [PubMed]
- Rossi, L.; Penela, D.; Doni, L.; Marazzi, R.; Napoli, V.; Napoli, L.; Vilotta, M.; Villani, G.Q.; De Ponti, R. Development of Simulation Combining a Physical Heart Model and Three-dimensional System for Electrophysiology Training. Pacing Clin. Electrophysiol. 2018, 41, 1461–1466. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Barbhaiya, C.R.; Balindger, S.; John, R.M.; Epstein, L.M.; Koplan, B.A.; Tedrow, U.B.; Stevenson, W.G.; Michaud, G.F. Better Lesion Creation and Assessment during Catheter Ablation. J. Atr. Fibrillation 2015, 8, 1189. [Google Scholar] [CrossRef] [PubMed]
- Bu-Lin, Z.; Bing, H.; Sheng-Li, K.; Huang, Y.; Rong, W.; Jia, L. A Polyacrylamide Gel Phantom for Radiofrequency Ablation. Int. J. Hyperth. 2008, 24, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Negussie, A.H.; Partanen, A.; Mikhail, A.S.; Xu, S.; Abi-Jaoudeh, N.; Maruvada, S.; Wood, B.J. Thermochromic Tissue-mimicking Phantom for Optimisation of Thermal Tumour Ablation. Int. J. Hyperth. 2016, 32, 239–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yap, Y.L.; Tan, Y.S.; Tan, H.K.; Peh, Z.K.; Low, X.Y.; Yeong, W.Y.; Tan, C.S.; Laude, A. 3D Printed Bio-Models for Medical Applications. Rapid Prototyp. J. 2017, 23, 227–235. [Google Scholar] [CrossRef]
- Wang, S.; Noh, Y.; Brown, J.; Roujol, S.; Li, Y.; Wang, S.; Housden, R.; Ester, M.C.; Al-Hamadani, M.; Rajani, R.; et al. Development and Testing of an Ultrasound-Compatible Cardiac Phantom for Interventional Procedure Simulation Using Direct Three-Dimensional Printing. 3D Print. Addit. Manuf. 2020, 7, 269–278. [Google Scholar] [CrossRef]
- Talalwa, L.; Natour, G.; Bauer, A.; Drzezga, A.; Gordji-Nejad, A.; Beer, S. T 1-mapping and Dielectric Properties Evaluation of A 3D Printable Rubber-Elastomeric Polymer as Tissue Mimicking Materials for MRI Phantoms. Mater. Res. Express 2020, 7, 115306. [Google Scholar] [CrossRef]
- Talalwa, L.; Gordji-Nejad, A.; Natour, G.; Drzezga, A.; Bauer, A.; Beer, S. Evaluation of 3D Printable Rubber-Elastomeric Polymer as Phantom Material for Hybrid PET/MRI. In Proceedings of the IEEE Nuclear Science Symposium and Medical Imaging Conference (NSS/MIC), Manchester, UK, 26 October–2 November 2019; pp. 1–3. [Google Scholar] [CrossRef]
- Nguyen, D.K.; Bach, Q.-V.; Lee, J.-H.; Kim, I.-T. Synthesis and Irreversible Thermochromic Sensor Applications of Manganese Violet. Materials 2018, 11, 1693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, F.; Hu, L. Temperature Sensitive Colour-changed Composites. In Advanced High Strength Natural Fibre Composites in Construction; Fan, M., Fu, F., Eds.; Woodhead Publishing: Cambridge, UK, 2017; pp. 405–423. [Google Scholar] [CrossRef]
- Raghavan, K.; Porterfield, J.E.; Kottam, A.T.G.; Feldman, M.D.; Escobedo, D.; Valvano, J.W.; Pearce, J.A. Electrical conductivity and permittivity of murine myocardium. IEEE Trans. Bio-Med. Eng. 2009, 56, 2044–2053. [Google Scholar] [CrossRef] [PubMed]
- Thermal Conductivity » IT’IS Foundation. Available online: https://itis.swiss/virtual-population/tissue-properties/database/thermal-conductivity (accessed on 8 November 2021).
- Maceira, A.M.; Cosín-Sales, J.; Roughton, M.; Prasad, S.K.; Pennell, D.J. Right Atrial Dimensions and Volume Estimation by Steady State Free Precession Cardiovascular Magnetic Resonance. J. Cardiovasc. Magn. Reson. 2013, 15, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masnok, K.; Watanabe, N. Role of Catheter Contact Force on Biophysical Properties of the Ablation Lesion Formation in Radiofrequency Catheter Cardiac Ablation. In Proceedings of the IEEE Region 10 Symposium (TENSYMP), Jeju-si, Korea, 23–25 August 2021; pp. 1–4. [Google Scholar] [CrossRef]
- Russell, W.M.S.; Burch, R.L. The Principles of Humane Experimental Technique; Methuen: London, UK, 1959. [Google Scholar]









| Ablation Temperature (°C)/Power (Watts) | 50 °C | 60 | 70 | 80 |
|---|---|---|---|---|
| 30 W | NA | NA | NA | NA |
| 40 | NA | NA | 2.7 | 2.4 |
| 50 | NA | 2.3 | 1.3 | 1.6 |
| 60 | NA | 1.4 | 1.8 | 3.3 |
| 70 | NA | 2.4 | 3.2 | 3.3 |
| 80 | NA | 1.9 | 3.0 | 3.2 |
| 90 | NA | 2.5 | 3.2 | 3.5 |
| UAP:BaSO4 | 15:1 | 15:2 | 5:1 | 15:4 | 3:1 | 5:2 | Myocardium |
|---|---|---|---|---|---|---|---|
| % Contrast | 5.56 | 15.6 | 23.6 | 28.2 | 35.5 | 40.0 | 21.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.; Saija, C.; Choo, J.; Ou, Z.; Birsoan, M.; Germanos, S.; Rothwell, J.; Vakili, B.; Kotadia, I.; Xu, Z.; et al. Cardiac Radiofrequency Ablation Simulation Using a 3D-Printed Bi-Atrial Thermochromic Model. Appl. Sci. 2022, 12, 6553. https://doi.org/10.3390/app12136553
Wang S, Saija C, Choo J, Ou Z, Birsoan M, Germanos S, Rothwell J, Vakili B, Kotadia I, Xu Z, et al. Cardiac Radiofrequency Ablation Simulation Using a 3D-Printed Bi-Atrial Thermochromic Model. Applied Sciences. 2022; 12(13):6553. https://doi.org/10.3390/app12136553
Chicago/Turabian StyleWang, Shu, Carlo Saija, Justin Choo, Zhanchong Ou, Maria Birsoan, Sarah Germanos, Joshua Rothwell, Behrad Vakili, Irum Kotadia, Zhouyang Xu, and et al. 2022. "Cardiac Radiofrequency Ablation Simulation Using a 3D-Printed Bi-Atrial Thermochromic Model" Applied Sciences 12, no. 13: 6553. https://doi.org/10.3390/app12136553
APA StyleWang, S., Saija, C., Choo, J., Ou, Z., Birsoan, M., Germanos, S., Rothwell, J., Vakili, B., Kotadia, I., Xu, Z., Rolet, A., Namour, A., Yang, W. S., Williams, S. E., & Rhode, K. (2022). Cardiac Radiofrequency Ablation Simulation Using a 3D-Printed Bi-Atrial Thermochromic Model. Applied Sciences, 12(13), 6553. https://doi.org/10.3390/app12136553







