Immediate Effect of Customized Foot Orthosis on Plantar Pressure and Contact Area in Patients with Symptomatic Hallux Valgus
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Insoles
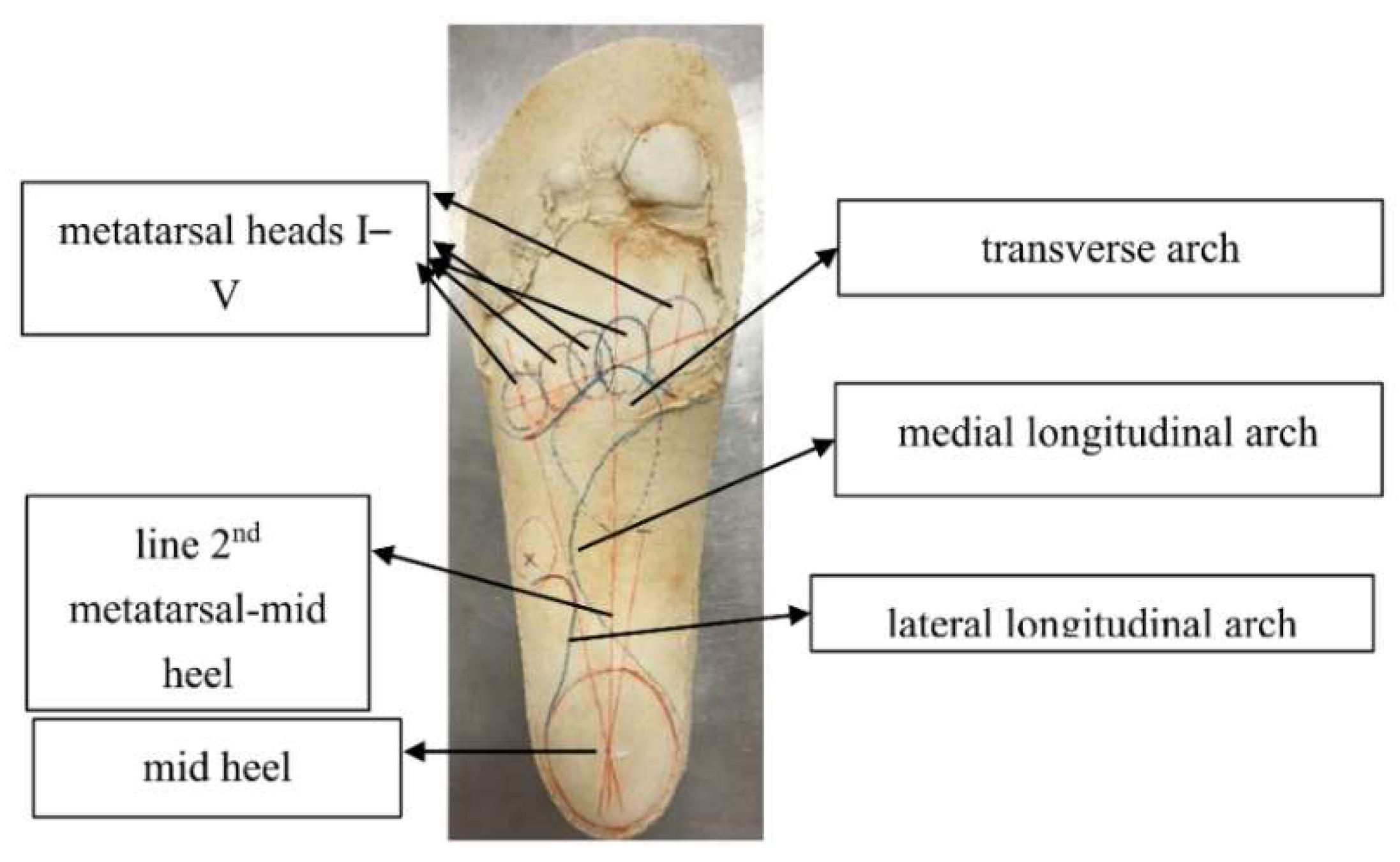
2.4. Data Processing
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Peak Pressure (KPa) | Peak Force (%BW) | Pressure-Time Integral (Kpa*s) | Force-Time Integral (%BW*s) | Contact Area (cm2) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| FO | FI | FO | FI | FO | FI | FO | FI | FO | FI | |
| T1 | 291.52 ± 175.6 s | 280.79 ± 182.38 s | 14.61 ± 10.04 s | 13.59 ± 9.21 s | 30.48 ± 16.1 s | 28.86 ± 14.84 s | 2.32 ± 1.57 s | 2.15 ± 1.49 s | 5.05 ± 2.41 s | 5.19 ± 2.38 s |
| T2 | 156.57 ± 83.11 m | 137.23 ± 62.08 m | 5.09 ± 3.09 s | 4.6 ± 2.92 s | 18.74 ± 6.74 s | 18.71 ± 7.44 s | 0.71 ± 0.42 s | 0.67 ± 0.45 s | 2.95 ± 1 s | 2.86 ± 1.11 s |
| T3 | 137.33 ± 57.3 s | 143.02 ± 84.86 s | 3.89 ± 1.86 s | 4.38 ± 2.77 s | 16.7 ± 6.62 s | 18.45 ± 10.45 s | 0.56 ± 0.27 s | 0.62 ± 0.45 s | 2.63 ± 1.21 s | 2.86 ± 0.87 s |
| T45 | 115.36 ± 76.04 m | 96.06 ± 42.98 m | 3.09 ± 2.44 s | 2.83 ± 2.04 s | 13.71 ± 6.54 s | 13.35 ± 6.73 s | 0.46 ± 0.36 s | 0.43 ± 0.36 s | 2.39 ± 1.37 s | 2.26 ± 1.36 s |
| M1 | 294.81 ± 190.29 s | 294.93 ± 189.12 s | 22.45 ± 11.6 s | 23.03 ± 12.08 s | 36.45 ± 23.7 s | 35.03 ± 18.55 s | 4.27 ± 2.37 s | 4.51 ± 2.51 s | 8.96 ± 2.38 m | 9.46 ± 2.22 m |
| M2 | 320.32 ± 200.48 s | 342.62 ± 227.03 s | 16.15 ± 7.51 s | 17.65 ± 9.66 s | 42.39 ± 22.51 s | 45.31 ± 25.17 s | 3.22 ± 1.62 m | 3.7 ± 2.03 m | 5.32 ± 1.15 *l | 5.69 ± 1.42 *l |
| M3 | 359.88 ± 147.3 s | 345.62 ± 132.21 s | 20.53 ± 6.86 s | 22.14 ± 7.88 s | 49.63 ± 20.53 s | 51.38 ± 21.77 s | 4.1 ± 1.38 m | 4.68 ± 1.65 m | 5.64 ± 1.32 *l | 6.15 ± 1.42 *l |
| M4 | 219.74 ± 79.13 s | 203.69 ± 68.98 s | 12.79 ± 3.49 s | 12.52 ± 2.93 s | 33.94 ± 11.62 s | 34.53 ± 14.45 s | 2.51 ± 0.5 s | 2.61 ± 0.75 s | 5.32 ± 1.4 m | 5.56 ± 1.47 m |
| M5 | 146.11 ± 53.7 s | 140.03 ± 63.36 s | 8.46 ± 3.34 s | 8.37 ± 4.77 s | 24.59 ± 11.6 s | 23.85 ± 10.35 s | 1.68 ± 0.74 s | 1.88 ± 1.39 s | 5.6 ± 1.75 s | 5.85 ± 2.16 s |
| MH | 279.2 ± 148.18 *l | 362.61 ± 169.11 *l | 44.14 ± 16.89 s | 46.45 ± 16.42 s | 37.66 ± 15.36 *l | 50.16 ± 23.51 *l | 9.92 ± 3.96 s | 10.92 ± 4.23 s | 18.69 ± 3.92 *l | 15.36 ± 3.51 *l |
| LH | 243.57 ± 97.25 *l | 305.39 ± 100.66 *l | 37.65 ± 10.1 m | 40.01 ± 11.77 m | 33.16 ± 10.04 *l | 40.59 ± 14.85 *l | 8.43 ± 2.28 m | 9.33 ± 3.19 m | 18.92 ± 4.38 *l | 16.5 ± 3.86 *l |
| Toes | 324.76 ± 154.52 m | 304.99 ± 171.78 m | 26.25 ± 11.81 s | 24.9 ± 12.8 s | 27.48 ± 9.89 s | 26.38 ± 10.15 s | 4.05 ± 1.7 s | 3.89 ± 1.96 s | 12.7 ± 4.58 s | 12.88 ± 4.56 s |
| FF | 461.24 ± 214.32 s | 458.58 ± 229.21 s | 152.22 ± 166.81 s | 170.07 ± 183.12 s | 44.89 ± 19.66 s | 44.13 ± 18.84 s | 15.77 ± 4.39 m | 17.38 ± 5.48 m | 30.32 ± 6.54 m | 32.13 ± 7.64 m |
| MF | 166.49 ± 108.98 m | 144.41 ± 88.91 m | 23.30 ± 9.62 *l | 15.1 ± 6.24 *l | 27.98 ± 12.3 *m | 25.75 ± 16.58 *m | 6.65 ± 3.78 * l | 4.02 ± 2.11 *l | 25.83 ± 13.22 *l | 18.12 ± 10.9 *l |
| Heel | 290.27 ± 146.21 * l | 376.17 ± 170.03 *l | 81.98 ± 24.94 m | 91.31 ± 32.2 m | 36.29 ± 12.55 *l | 47.65 ± 21.58 *l | 18.34 ± 5.83 m | 20.26 ± 7.18 m | 37.29 ± 8.06 *l | 31.6 ± 7.24 *l |
References
- Mann, R.A.; Coughlin, M.J. Adult Hallux Valgus. In Surgery of the Foot and Ankle; Coughlin, M.J., Mann, R.A., Eds.; St. Louis Mosby: Maryland Heights, MU, USA, 1999; Volume 1, pp. 150–175. [Google Scholar]
- Hessert, M.J.; Vyas, M.; Leach, J.; Hu, K.; Lipsitz, L.A.; Novak, V. Foot pressure distribution during walking in young and old adults. BMC Geriatr. 2005, 5, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Razak, A.H.; Zayegh, A.; Begg, R.K.; Wahab, Y. Foot plantar pressure measurement system: A review. Sensors 2012, 12, 9884–9912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hida, T.; Okuda, R.; Yasuda, T.; Jotoku, T.; Shima, H.; Neo, M. Comparison of plantar pressure distribution in patients with hallux valgus and healthy matched controls. J. Orthop. Sci. 2017, 22, 1054–1059. [Google Scholar] [CrossRef] [PubMed]
- Farzadi, M.; Safaeepour, Z.; Mousavi, M.E.; Saeedi, H. Effect of medial arch support foot orthosis on plantar pressure distribution in females with mild-to-moderate hallux valgus after one month of follow-up. Prosthet. Orthot. Int. 2015, 39, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Khodaei, B.; Saeedi, H.; Jalali, M.; Farzadi, M.; Norouzi, E. Comparison of plantar pressure distribution in CAD-CAM and prefabricated foot orthoses in patients with flexible flatfeet. Foot 2017, 33, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Nouman, M.; Leelasamran, W.; Chatpun, S. Effectiveness of total contact orthosis for plantar pressure redistribution in neuropathic diabetic patients during different walking activities. Foot Ankle Int. 2017, 38, 901–908. [Google Scholar] [CrossRef]
- Tang, S.F.; Chen, C.P.; Lin, S.C.; Wu, C.K.; Chen, C.K.; Cheng, S.P. Reduction of plantar pressures in leprosy patients by using custom made shoes and foot orthosis. Clin. Neurol. Neurosurg. 2015, 129 (Suppl. 1), S12–S15. [Google Scholar] [CrossRef]
- Bonanno, D.R.; Ledchumanasarma, K.; Landorf, K.B.; Munteanu, S.E.; Murley, G.S.; Menz, H.B. Effects of a contoured foot orthosis and flat insole on plantar pressure and tibial acceleration while walking in defence boots. Sci. Rep. 2019, 9, 1688. [Google Scholar] [CrossRef]
- Stolwijk, N.M.; Louwerens, J.W.; Nienhuis, B.; Duysens, J.; Keijsers, N.L. Plantar pressure with and without custom insoles in patients with common foot complaints. Foot Ankle Int. 2011, 32, 57–65. [Google Scholar] [CrossRef]
- Tsujinaka, S.; Shima, H.; Yasuda, T.; Mori, K.; Kizawa, M.; Togei, K.; Neo, M. Comparison of plantar pressure distribution between postoperative hallux valgus feet and healthy feet. Foot Ankle Int. 2019, 40, 578–585. [Google Scholar] [CrossRef]
- Doty, J.F.; Alvarez, R.G.; Ervin, T.B.; Heard, A.; Gilbreath, J.; Richardson, N.S. Biomechanical evaluation of custom foot orthoses for hallux valgus deformity. J. Foot Ankle Surg. 2015, 54, 852–855. [Google Scholar] [CrossRef]
- Mahieu, C.; Salvia, P.; Beyer, B.; Rooze, M.; Feipel, V.; Van Sint Jan, S. Metatarsal arch deformation and forefoot kinematics during gait in asymptomatic subjects. Int. Biomec. 2019, 6, 75–84. [Google Scholar] [CrossRef] [Green Version]
- Nakai, K.; Zeidan, H.; Suzuki, Y.; Kajiwara, Y.; Shimoura, K.; Tatsumi, M.; Nishida, Y.; Bitoh, T.; Yoshimi, S.; Aoyama, T. Relationship between forefoot structure, including the transverse arch, and forefoot pain in patients with hallux valgus. J. Phys. Ther. Sci. 2019, 31, 202–205. [Google Scholar] [CrossRef]
- Suzuki, J.; Tanaka, Y.; Takaoka, T.; Kadono, K.; Takakura, Y. Axial radiographic evaluation in hallux valgus: Evaluation of the transverse arch in the forefoot. J. Orthop. Sci. 2004, 9, 446–451. [Google Scholar] [CrossRef]
- Zeidan, H.; Ryo, E.; Suzuki, Y.; Iijima, H.; Kajiwara, Y.; Harada, K.; Nakai, K.; Shimoura, K.; Fujimoto, K.; Takahashi, M.; et al. Detailed analysis of the transverse arch of hallux valgus feet with and without pain using weightbearing ultrasound imaging and precise force sensors. PLoS ONE 2020, 15, e0226914. [Google Scholar] [CrossRef]
- Su, S.; Mo, Z.; Guo, J.; Fan, Y. The effect of arch height and material hardness of personalized insole on correction and tissues of flatfoot. J. Healthc. Eng. 2017, 2017, 8614341. [Google Scholar] [CrossRef] [Green Version]
- Xu, R.; Wang, Z.; Ren, Z.; Ma, T.; Jia, Z.; Fang, S.; Jin, H. Comparative study of the effects of customized 3D printed insole and prefabricated insole on plantar pressure and comfort in patients with symptomatic flatfoot. Med. Sci. Monit. 2019, 25, 3510–3519. [Google Scholar] [CrossRef]
- El-Hilaly, R.; Elshazly, O.; Amer, A. The role of a total contact insole in diminishing foot pressures following partial first ray amputation in diabetic patients. Foot 2013, 23, 6–10. [Google Scholar] [CrossRef]
- Coughlin, M.J.; Carlson, R.E. Treatment of hallux valgus with an increased distal metatarsal articular angle: Evaluation of double and triple first ray osteotomies. Foot Ankle Int. 1999, 20, 762–770. [Google Scholar] [CrossRef]
- Song, C.Y.; Lin, S.F.; Huang, C.Y.; Wu, H.C.; Chen, C.H.; Hsieh, C.L. Validation of the Brief Pain Inventory in patients with low back pain. Spine 2016, 41, E937–E942. [Google Scholar] [CrossRef] [Green Version]
- Song, C.Y.; Chen, C.H.; Chen, T.W.; Chiang, H.Y.; Hsieh, C.L. Assessment of low back pain: Reliability and minimal detectable change of the Brief Pain Inventory. Am. J. Occup. Ther. 2022, 76, 7603205040. [Google Scholar] [CrossRef]
- Price, C.; Parker, D.; Nester, C. Validity and repeatability of three in-shoe pressure measurement systems. Gait Posture 2016, 46, 69–74. [Google Scholar] [CrossRef] [Green Version]
- Patrick, K.; Donovan, L. Test-retest reliability of the Tekscan(R) F-Scan(R) 7 in-shoe plantar pressure system during treadmill walking in healthy recreationally active individuals. Sports Biomech. 2018, 17, 83–97. [Google Scholar] [CrossRef]
- Beling, J.; Wolfe, G.A.; Allen, K.A.; Boyle, J.M. Lower extremity preference during gross and fine motor skills performed in sitting and standing postures. J. Orthop. Sports Phys. Ther. 1998, 28, 400–404. [Google Scholar] [CrossRef]
- Abe, M. Study of utility of outer longitudinal arch pad in toe. J. Niigata Univ. Health Welf. 2015, 15, 2–7. [Google Scholar]
- Matsuya, A.; Abe, K. Examination of the optimum height of the metatarsal pad by sole pressure. J. Niigata Med. Welf. Soc. 2012, 12, 25. [Google Scholar]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef] [Green Version]
- Galica, A.M.; Hagedorn, T.J.; Dufour, A.B.; Riskowski, J.L.; Hillstrom, H.J.; Casey, V.A.; Hannan, M.T. Hallux valgus and plantar pressure loading: The Framingham foot study. J. Foot Ankle Res. 2013, 6, 42. [Google Scholar] [CrossRef] [Green Version]
- Yokozuka, M.; Okazaki, K.; Sakamoto, Y.; Takahashi, K. Correlation between functional ability, toe flexor strength, and plantar pressure of hallux valgus in young female adults: A cross-sectional study. J. Foot Ankle Res. 2020, 13, 44. [Google Scholar] [CrossRef]
- Cheng, K.W.; Peng, Y.; Chen, T.L.; Zhang, G.; Cheung, J.C.; Lam, W.K.; Wong, D.W.; Zhang, M. A Three-dimensional printed foot orthosis for flexible flatfoot: An exploratory biomechanical study on arch support reinforcement and undercut. Materials 2021, 14, 5297. [Google Scholar] [CrossRef] [PubMed]
- Redmond, A.C.; Landorf, K.B.; Keenan, A.M. Contoured prefabricated foot orthoses demonstrate comparable mechanical properties to contoured, customised foot orthoses: A plantar pressure study. J. Foot Ankle Res. 2009, 2, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aminian, G.; Safaeepour, Z.; Farhoodi, M.; Pezeshk, A.F.; Saeedi, H.; Majddoleslam, B. The effect of prefabricated and proprioceptive foot orthoses on plantar pressure distribution in patients with flexible flatfoot during walking. Prosthet. Orthot. Int. 2012, 37, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Tsung, B.Y.; Zhang, M.; Mak, A.F.; Wong, M.W. Effectiveness of insoles on plantar pressure redistribution. J. Rehabil. Res. Dev. 2004, 41, 767–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bus, S.A.; Ulbrecht, J.S.; Cavanagh, P.R. Pressure relief and load redistribution by custom-made insoles in diabetic patients with neuropathy and foot deformity. Clin. Biomech. 2004, 19, 629–638. [Google Scholar] [CrossRef]
- Dissaneewate, T.; Rungsri, T.N.; Cheunchokasan, P.; Leelasamran, W. Comparison between the plantar pressure effects of toe separators and insoles in patients with hallux valgus at a one-month follow-up. Foot Ankle Surg. 2022, 28, 93–99. [Google Scholar] [CrossRef]
- Venkadesan, M.; Yawar, A.; Eng, C.M.; Dias, M.A.; Singh, D.K.; Tommasini, S.M.; Haims, A.H.; Bandi, M.M.; Mandre, S. Stiffness of the human foot and evolution of the transverse arch. Nature 2020, 579, 97–100. [Google Scholar] [CrossRef] [Green Version]
- Koller, U.; Willegger, M.; Windhager, R.; Wanivenhaus, A.; Trnka, H.J.; Schuh, R. Plantar pressure characteristics in hallux valgus feet. J. Orthop. Res. 2014, 32, 1688–1693. [Google Scholar] [CrossRef] [Green Version]
- Kwan, M.Y.; Yick, K.L.; Yip, J.; Tse, C.Y. The immediate effects of hallux valgus orthoses: A comparison of orthosis designs. Gait Posture 2021, 90, 283–288. [Google Scholar] [CrossRef]
- Huang, Y.P.; Peng, H.T.; Wang, X.; Chen, Z.R.; Song, C.Y. The arch support insoles show benefits to people with flatfoot on stance time, cadence, plantar pressure and contact area. PLoS ONE 2020, 15, 0237382. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.-Y.; Peng, H.-T.; Chang, C.-K.; Wang, F.-T.; Yen, C.-H.; Wang, T.-Y.; Chuang, H.-C.; Chiu, F.-Y.; Song, C.-Y. Immediate Effect of Customized Foot Orthosis on Plantar Pressure and Contact Area in Patients with Symptomatic Hallux Valgus. Appl. Sci. 2022, 12, 7593. https://doi.org/10.3390/app12157593
Chen H-Y, Peng H-T, Chang C-K, Wang F-T, Yen C-H, Wang T-Y, Chuang H-C, Chiu F-Y, Song C-Y. Immediate Effect of Customized Foot Orthosis on Plantar Pressure and Contact Area in Patients with Symptomatic Hallux Valgus. Applied Sciences. 2022; 12(15):7593. https://doi.org/10.3390/app12157593
Chicago/Turabian StyleChen, Hsin-Yu, Hsien-Te Peng, Chin-Kang Chang, Fu-Ting Wang, Chia-Hao Yen, Tsung-Yang Wang, Hsiang-Chun Chuang, Fang-Yao Chiu, and Chen-Yi Song. 2022. "Immediate Effect of Customized Foot Orthosis on Plantar Pressure and Contact Area in Patients with Symptomatic Hallux Valgus" Applied Sciences 12, no. 15: 7593. https://doi.org/10.3390/app12157593
APA StyleChen, H.-Y., Peng, H.-T., Chang, C.-K., Wang, F.-T., Yen, C.-H., Wang, T.-Y., Chuang, H.-C., Chiu, F.-Y., & Song, C.-Y. (2022). Immediate Effect of Customized Foot Orthosis on Plantar Pressure and Contact Area in Patients with Symptomatic Hallux Valgus. Applied Sciences, 12(15), 7593. https://doi.org/10.3390/app12157593






