1. Introduction
The digital workflow in dentistry has had its number of clinical applications increased by recent advances in computer-aided design and computer-aided manufacturing (CAD-CAM) technology [
1]. Along with the rising of dental optical scanners, the intraoral morphology of patients can be registered and translated into digital data that can be stored easily and manufactured into dental models when required [
2]. In prosthodontics, a digital impression can be made using an intraoral scanner. Consequently, dental casts and prostheses can be digitally created and manufactured for clinical use.
The manufacturing process in digital dentistry may be classified into two categories: subtractive manufacturing (milling machines) and additive manufacturing (3D printing). The latter was defined as a process by which an object can be constructed one layer at a time. There are several categories of 3D-printing available in the market, such as material extrusion, vat polymerization, power bed fusion, sheet lamination, material jetting, binder jetting, and direct energy deposition. Basically, in vat polymerization 3D-printing, a slicing software is used to divide a STL file of an object into multiple layers in two-dimensional planes. These layers will be exported as a new type of file generally known as “sliced file”, which is readable by the 3D printer. The layers of the object will then be successively built up on top of each other until the object is manufactured completely. This type of technology is described to lead to minimal material waste and to produce dental casts with highly detailed and clinically acceptable geometries [
3].
The group of additive manufacturing devices that use vat polymerization 3D-printing include different printing technologies, such as stereolithography (SLA) and digital light processing (DLP), which are among the most commonly used in dentistry. Basically, SLA and DLP printers use the same process for printing, but they differ in the procedure in that light is delivered to cure the 3D-printed object. SLA is the oldest and has been one of the most commonly used method in general 3D-printing. This type of 3D printer projects an ultraviolet (UV) laser beam that rapidly moves into a reservoir filled with light-cured liquid resin to build by drawing the details of each layer of the object. The first cured layer is attached to the printing bed (building platform), rather than to the resin reservoir. Once the first layer is completed, the building platform rises slightly in order to form consecutive new layers on top of the previous ones. This process repeats continuously until the object is fully manufactured. DLP, in turn, is an alternative method to deliver light during 3D-printing. Instead of using a laser beam to scan each layer at a time, the DLP printer projects a silhouette of the entire first layer simultaneously and cures it with light. This enables a relatively faster printing procedure, as compared to SLA [
3,
4].
Although milling has been widely used to fabricate definitive prostheses with a series of materials such as zirconia and lithium disilicate, there are some drawbacks inherent to the process, such as inability to reproduce fine details and relatively higher cost if compared with 3D-printing. The advantages of the latter include the production of desired objects with a minimum amount of material, low waste of the material, and the ability to create multiple products at a time [
4]. Nonetheless, 3D-printed models also present a unique set of limitations (e.g., resolution of the optical scanner, quality of the light-cured resin, etc.).
The accuracy of the resultant models depends on several factors related either to CAD or CAM, in which errors may occur. This includes the parameters involved in the manufacturing and postprocessing procedures, as it does the data acquisition and image processing of the oral hard and soft tissues [
5]. However, recent articles have described 3D-printing as clinically acceptable to produce dental devices such as crowns, surgical guides, and dental casts, with clinical results comparable to the respective milled and conventionally produced devices [
1,
4]. A recent article found similar accuracy results between 3D-printed models using specific technologies and conventional stone casts [
3].
Accurate impressions, as well as conventional or 3D-printing procedures, are prerequisites to manufacture satisfactory dental casts. These, in turn, can be used in the fabrication or adjustment of definitive prostheses or restorations with adequate fit. Unlike conventional stone casts, 3D-printed dental casts can be produced from 3D reconstructed models composed by digital meshes. For this purpose, optical scans from a dental arch can be digitally processed on a CAD software, in order to turn the structure of the digital mesh into a dental model shape by creating and editing a closed mesh area.
The acquisition of 3D-printing devices by dental clinics, as well as by schools of dentistry in universities for research and educational purposes, is the first step in moving dentistry towards the digital era, which may offer benefits to patients and improve their satisfaction and acceptance towards dental treatments significantly. According to the recent literature, digital technologies and workflows in dentistry can simplify and make procedures predictable. Moreover, digital workflows lead to advantages for dental patients as compared with conventional procedures, such as higher quality, better reproducibility of the prosthesis, and faster treatment times [
4,
6].
Different 3D-printing techniques can be used to produce models. The common devices in dentistry that use light to polymerize resin are stereolithography apparatus (SLA), digital light processing (DLP), liquid crystal display (LCD), and PolyJet 3D inkjet printing technology (PolyJet) [
7]. There is a gap in the literature on trueness and precision of dental devices for clinical use. So far, only a few studies have effectively compared accuracy of the manufactured dental models by different printing technologies with the corresponding digital files [
8,
9,
10]. In addition, these studies present different outcomes concerning the clinical relevance of the deviation between printing equipment.
Considering the current relevance of this matter with the rise of 3D-printing technologies in dentistry, the purpose of this study was to investigate and compare the accuracy (trueness and precision) of different 3D-printing technologies (SLA, DLP, LCD, and PolyJet).
2. Materials and Methods
For the purpose of this in vitro study, a cone beam computer tomography (CBCT) was performed on a resin dental model with tomographic hyperdensity (tomographicable model; BoneModels; Castellon; Spain), shaped according to a human maxilla. Digital Imaging and Communications in Medicine (DICOM) files obtained were then converted into an STL file using a CBCT software (Nemo Studio; Nemotec SL, Madrid, Spain).
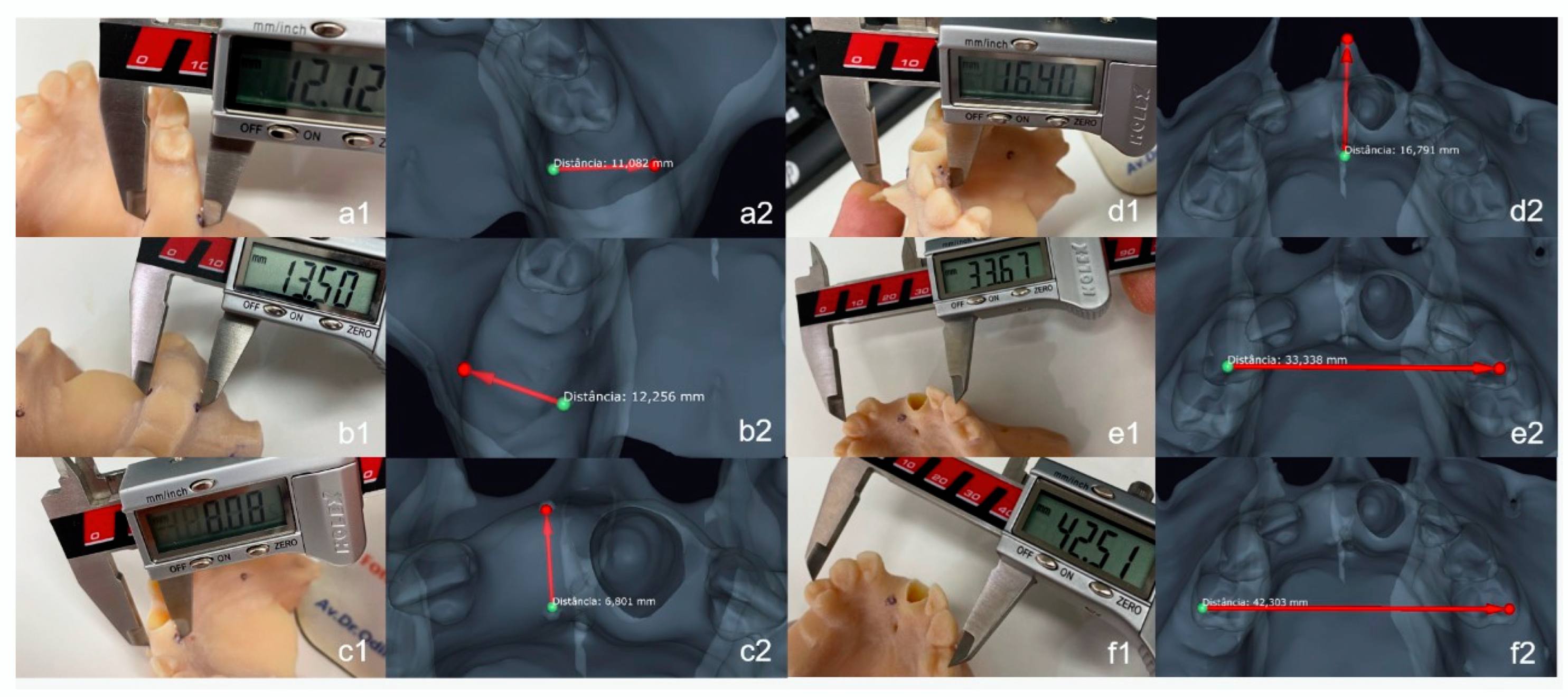
The resulting STL file was imported and virtually measured using a 3D analysis software (DentalCAD 2.4 Matera, Exocad GmbH, Darmstadt, Germany). Digital small marks with 1 mm in diameter were added to specific places on the buccal and palatal plates of the maxillary ridge (simulating buccal–lingual width measurements of edentulous area commonly performed during dental implant planning) to ensure reproducibility of the linear measurements of the buccal–lingual width of the alveolar ridge, performed for trueness analysis, following a previously described methodology [
1].
Figure 1 shows in a smaller STL file of a dental crown how the digital markers were created using the CAD software of this study and how the digital linear measurements were performed. Briefly, the middle point of the upper limit of the mesh area of each digital mark was considered the point at which to start and finish each linear measurement, as this point was also planned to support the tip of the digital caliper on all 3D-printed dental casts. Furthermore, cross-section views of the mesh area containing the measurement were also created by the CAD software and used to orientate all digital linear measurements. Digital linear measurements were used as control values to be compared with the measurements performed directly on the 3D-printed dental casts.
This file was imported into the corresponding slicing software programs of each of the following 3D printers: Objet30 Dental Prime (Stratasys, Minneapolis, MN, USA); Form 2 (Formlabs, Somerville, MA, USA); Sonic Mini (Phrozen, Hsinchu, Taiwan); Photon (Anycubic, Shenzhen, China); and Miicraft 125 (Miicraft, Jena, Germany). All 3D printers were previously calibrated and all 3D-printing parameters adjusted according to the 3D printer and resin manufacturer’s instructions (
Table 1). Before starting the study, representative test specimens with known dimensions provided by the manufacturers were printed with all 3D printers and measured to confirm successful calibration. A total of 15 dental casts were manufactured with each 3D printer. Dental models manufactured with Stratasys were 3D-printed using a light-curing resin of the same brand (VeroDent Plus MED690), whereas all other models were fabricated with an independent light-curing resin brand (Prizma 3D Model, Makertech Labs, Tatuí, Brazil). This resin brand produces different resin bottles specifically designed for either SLA, LCD, or DLP technology. Therefore, the appropriate bottle of Prizma 3D Model resin was chosen for each 3D printer technology. The light-cured resins of this work were composed mainly of monomers and oligomers and was specifically developed to produce dental casts. After 3D-printing, all models were washed and postcured for 10 minutes in a standard UV light-curing chamber. The following measurements were performed with the aid of the locating marks: left posterior buccal–lingual width; right posterior buccal–lingual width; and anterior buccal–lingual width. Furthermore, the distance between the following anatomical structures were also recorded: anterior nasal spine and infraorbital foramen; tip of cusps of teeth 13 and 23; and tips of cusps of teeth 14 and 24.
The manufactured models were physically measured in the corresponding lengths for trueness and reproducibility. A digital caliper with precision of two decimal places was used to measure all of the described widths (
Figure 2), following a previous methodology used to assess trueness and precision of dental 3D-printers [
1]. Briefly, to ensure reproducibility of measurements, the caliper tips were positioned accurately on top of the manufactured marks that were used to guide the digital measurements on the software, as explained above. These measurements were also performed twice by two trained observers at intervals of two weeks to eliminate the memory bias, recorded in millimeters and compared to the control measurements that were previously digitally performed on the reference STL file using the software program. Median and standard error values were obtained for the five 3D printers and compared in the statistical analysis.
For statistical analyses, Shapiro–Wilk test was initially performed to confirm normal distribution of variables. Interobserver reproducibility and intra-observer reliability of measurements were calculated using the intraclass correlation coefficient (ICC). Trueness was given by relative error calculation and precision was given by median values along with standard error. Pairwise comparisons were performed with Wilcoxon test with post hoc Bonferroni correction for trueness and precision among 3D printers. All statistical analyses were performed with a significance level of 5% using a statistical software program (SPSS v24 for Macintosh; IBM Corp., Chicago, IL, USA).
3. Results
All 3D printers could manufacture the dental casts successfully from the same STL file. Average printing time was 11 hours, and average number of layers was 930 (approximately 130 mL of light-cured resin).
Normality assumption was not confirmed (
p < 0.05), therefore non-parametric tests comparisons were assessed. Both interobserver reproducibility and intra-observer reliability were confirmed as ICC values ranged between 0.87 and 0.96 (
p = 0.01). No significant difference was found in the comparison between observers in all measurements performed with the different models.
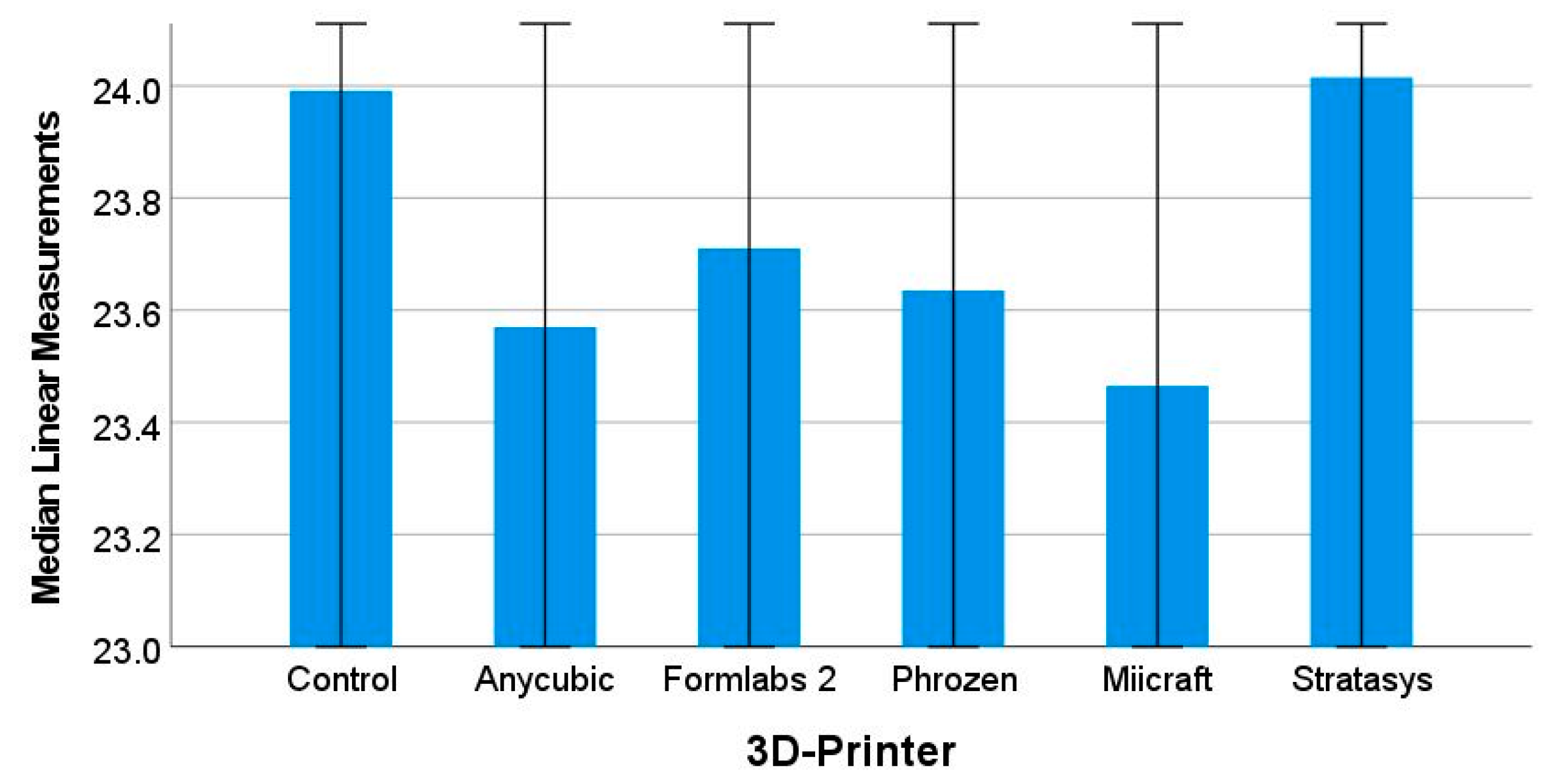
Figure 3 shows the estimated marginal median control and test measurements. The Stratasys 3D printer achieved the greatest accuracy, as the digital caliper measurements of the respective dental casts were the most similar to the control measurements performed in the CAD software.
For the left posterior buccal–lingual width measurement, Anycubic obtained the lowest median and standard error values (12.160 ± 0.075 mm), followed by Stratasys (12.288 ± 0.138 mm), Form 2 (12.306 ± 0.117 mm), Miicraft (12.436 ± 0.066 mm), and Phrozen (12.548 ± 0.039 mm). For the right posterior buccal–lingual width measurement, the Anycubic (13.500 ± 0.067 mm) obtained the lowest values, again followed by Stratasys (13.683 ± 0.114 mm), Form 2 (13.705 ± 0.167 mm), Miicraft (13.840 ± 0.079 mm), and Phrozen (13.930 ± 0.109 mm), respectively. For the anterior buccal–lingual width, Anycubic obtained the lowest values (8.065 ± 0.046 mm), followed by Form 2 (8.190 ± 0.033 mm), Miicraft (8.285 ± 0.060 mm), Stratasys (8.298 ± 0.132 mm), and Phrozen (8.370 ± 0.056 mm). The larger measurement was the maximum horizontal width and lowest measurement values was the anterior buccal–lingual width. The lowest value of trueness was obtained for anterior nasal spine: nasopalatine foramen measurement for Miicraft printer (0.128 mm). The highest value of trueness was obtained for anterior buccal–lingual width measurement for Phrozen (0.230 mm). The lowest values of precision were reached by Form 2 (0.002 mm) and Miicraft (0.002 mm) for maximum horizontal width. The highest value of precision was obtained by Anycubic (0.035 mm) for the anterior nasal spine: nasopalatine foramen measurement. Friedmann test revealed no significant differences among all 3D printers for trueness and precision (p > 0.05). However, pairwise Wilcoxon test comparisons revealed statistically significant differences between Stratasys versus Anycubic printers (p = 0.025) and Anycubic versus Form 2 (p = 0.048).
4. Discussion
This study aimed to compare the accuracy of three different 3D-printing technologies used to manufacture dental models, SLA, DLP, and LCD 3D printers, in creating a final manufactured product (dental models). For this purpose, trueness and precision analyses were performed with a model resin commercially available generally available in the market. Our main outcome was a discrepancy between the referential measures on the original digital files that were manufactured and the physical measures on the manufactured models [
11]. This is the first in vitro study to address the aforementioned differences between the 3D printers. Nevertheless, the present findings are consistent with previous studies that also compared 3D-printing technologies [
4,
5]. However, the clinical relevance of the accuracy differences found herein may not be clear, since several other studies confirmed that the 3D-printing methodologies lead to clinically acceptable outcomes, which were better than those observed in conventional cast models [
11,
12].
There were no significant differences in trueness and precision among all 3D printers (Friedmann test,
p > 0.05). Discussing this finding in relation with previous similar studies [
13,
14] is a challenge, as these studies were not able to standardize the materials used and the method of calibration of the 3D printers. Nevertheless, the absence of significant differences among 3D printers suggests that low-cost devices might perform at similar levels of trueness of highly priced devices, provided that the correct materials and methods are applied. On the other hand, pairwise comparisons showed that the PolyJet technology was significantly better in trueness and had greater reproducibility and reliability of measurements, especially compared to the 3D printer that showed the greatest deviation in median values from the control ones, which was the Anycubic Photon. This finding is in agreement with a previous study on dental models, which found greater accuracy for dental models 3D-printed using the PolyJet technology [
13].
While this study solely assessed 3D-printing accuracy, other factors such as the cost relationship among 3D printers are important in 3D-printing comparisons for dentistry. For instance, the DLP technology enables fast light-curing 3D-printing and ensures high precision [
15]. One of its biggest drawbacks of this technology is that it is relatively expensive and limited in size of the printing bed. The LCD technique, in turn, is also based on light-curing, but it uses liquid crystals instead of a light projector [
16]. Compared to other 3D-printing technologies, LCD is more inexpensive and has good resolution, but it is known to have a shorter lifespan [
17]. Factors such as time taken to 3D-print dental devices, cost, and production rates are important for comparison in research to assess whether the clinician can implement 3D-printing in its practice [
18,
19]. The more automated the 3D-printing procedure is, the more acceptability from clinicians the procedure can achieve. In this context, some models of DLP 3D-printers that have user-friendly interfaces but that were not tested herein have also been used in studies validating dental techniques, such as The Hunter Printer (Flashforge, China) [
19,
20]. Research and website validating 3D-printing software parameters for each light-cured resin can also be a useful tool to help the clinician and dental professionals to standardize the procedure used to manufacture dental devices in their practice.
Compared with conventional stone casts, 3D-printed models have been described to be equally accurate [
3]. Although this could not be assessed herein, it is noteworthy that the advantages of 3D-printing over conventional methods are not limited to accuracy, but also includes faster procedures and better communication with professionals such as the dental technologist [
18]. On the other hand, dental professionals should be aware and have knowledge on the correct usage and disposal procedures of light-cured resins. Professionals should work in well-ventilated areas and use protective gloves. Post-cure using UV light is usually recommended by the manufacturer. Such a procedure should follow proper wash before the printed object is handled without gloves. To wash the 3D-printed before post-curing with a UV light chamber, the professional should use a manufacturer’s recommended solvent, such as isopropyl or rubbing alcohol. Alterations in post-processing procedures could also affect the results of 3D-printing trueness and precision, and therefore the procedure should be as standardized as possible. To standardize the 3D-printing methods used herein, all measurements were conducted right after post-processing procedures. Storing 3D-printed objects and light-curing resins also should be performed properly. Professionals should keep UV curable resins sealed tightly in their containers, out of direct sunlight and within a temperature range as suggested by the manufacturer. Differences in precision and accuracy between 3D printers and 3D-printing technologies have also been reported [
3]. This finding is in agreement with the present study, insofar as significant pairwise differences were detected by statistical analysis.
One of the limitations of this in vitro study performed solely on dental models is that the impact of clinical factors commonly encountered in CBCT exams, such as low resolution of the 3D image reconstruction, could not be addressed. Furthermore, other variables that could affect 3D-printing outcomes such as orientation in the printing bed, different resin types, and shape of the object to be printed were not compared herein. Therefore, future observational clinical studies could address the impact of different CAM systems and materials on trueness, 3D deviation, and precision of dental models. The current fast technological development also requires ongoing research projects to test not only trueness and precision, but also time, cost, and production rates of new 3D printers.
In conclusion, the present findings suggest that the 3D-printing methods may have small significant discrepancies when compared to the original digital files, which may not be clinically relevant. Pairwise comparison showed only two significant differences between the cheapest 3D printer (Anycubic Photon) and two high-end 3D-printers (Objet30, Stratasys, p = 0.025; and Form 2, Formlabs, p = 0.048). In addition, there were no significant discrepancies among median measurements of each printing method (within 3D printer analysis), which suggests that, for dental casts, all 3D printers analyzed performed similarly.