Abstract
Although mobile hemodialysis treatments have been found to be an effective alternative to current in-center and home-based hemodialysis treatments, many barriers to its successful implementation remain. These barriers include the lack of considering user-centered monitoring protocols. This study investigates 24 patients’ and 12 care partners’ expectations for monitoring procedures for a mobile hemodialysis device. Individual semi-structured interviews were conducted at three locations within the Veterans Affairs Health Care System: Seattle, WA; Nashville, TN; and Louisville, KY. All interviews were transcribed and analyzed using inductive or deductive content analysis approaches. We identified 10 categories of indicators suggesting patients’ needs to receive dialysis treatment and 11 categories of indicators suggesting patients’ successful dialysis treatment. Furthermore, we identified six categories of patients’ and care partners’ design expectations for monitoring procedures. The findings from this study have the potential to guide the development of a monitoring system to help ensure users’ acceptance of future mobile hemodialysis devices.
1. Introduction
1.1. In-Center, Home, and Mobile Hemodialysis Systems
End-stage renal disease (ESRD) is a medical condition of permanent kidney failure that requires a patient to either have a kidney transplant or adhere to long-term dialysis treatments [1]. Dialysis allows ESRD patient to extend their survival by using a machine that filters salt, waste, and fluids from the patient’s blood when their kidneys are no longer able to function normally. Hemodialysis filters a patient’s blood outside the patient’s body using a dialysis machine. The dialysis machine removes, cleans, and returns the patient’s blood to their body [2]. The most frequently used mode of managing ESRD in the United States requires a patient to adhere to thrice-weekly in-center hemodialysis treatments during which the patient spends multiple hours connected to a stationary dialysis machine [3]. Despite its status as the dominant mode of treatment, in-center hemodialysis has been found to negatively impact patients’ quality of life. For instance, this mode of treatment has been found to impair the patient’s ability to travel, work, and sleep; to impair their mental health; and to restrict or completely foreclose social and physical activities [4,5,6,7].
To overcome the limitations of current in-center treatments, home-based hemodialysis treatments have been recommended [8,9]. Home hemodialysis allows a dialysis patient to perform hemodialysis treatments in the comfort of their home. At home, the patient can use either a conventional in-center hemodialysis machine or a hemodialysis machine particularly designed for home use [10]. With direct access to their own personal machine, patients undergoing home hemodialysis have the opportunity to perform both longer and more frequent treatments, compared to the limited treatment opportunity at dialysis centers that stems from sharing a dialysis machine with other patients that is located a distance away from the patient’s home [2,11]. Evidence suggests that frequent home hemodialysis treatments not only reduces the risk of mortality but also improve health outcomes and quality of life [12,13,14]. In addition, performing home hemodialysis improves patients’ independence and employment potential [9,15]. Despite these advantages, home-based dialysis remains severely underused in the United States. In 2018, only 1.8% of all ESRD dialysis patients performed hemodialysis in their homes [16], indicating only a small number of patients successfully adopt home hemodialysis treatments. Challenges to adoption have been linked to the designs of current home hemodialysis devices. Home hemodialysis devices in the United States are large, heavy, and stationary devices with limited portability, restricting patients’ mobility during treatment. Currently, patients on home hemodialysis spend multiple hours several times a week connected to a stationary device, with a subsequent loss of independent living [17,18].
To overcome the limitations of current home hemodialysis treatment, researchers have begun envisioning and designing a mobile dialysis device [17,19,20,21,22]. Mobile dialysis treatments allow an ESRD patient to undergo continuous dialysis treatments that more closely resemble normal kidney functioning [17]. Such treatment modifications provide the patient with increased freedom of treatment timing and location by allowing the patient to wear a dialysis device during their daily routines [22]. Research has shown that treatment using a mobile dialysis device is an effective alternative to current dialysis technology [19]. The Center for Dialysis Innovation (CDI) at the University of Washington is developing a mobile hemodialysis device called the Ambulatory Kidney to Improve Vitality [22]. The AKTIV aims to improve the lives of patients with ESRD by providing them with increased mobility and confidence in self-managing their dialysis treatments.
1.2. Importance of Self-Management through Symptom-Related Monitoring
Symptom-related monitoring has been known to help support patients’ self-management of health. The self-management of health is defined as “patients’ positive efforts to oversee and participate in their health care to optimize health, prevent complications, control symptoms, marshal medical resources, and minimize the intrusion of the disease into their preferred lifestyles” [23] (p. 386). Patients’ knowledge regarding their own physical conditions and treatment through self-management of symptom monitoring can impact their health-related quality of life [24]. Effective self-management of ESRD patients is crucial for improving patients’ health outcomes [25] but is complicated and requires support [26].
To help support patients’ successful self-management of treatment, it is important to incorporate an effective monitoring system into the designs of mobile dialysis devices [27,28,29,30]. For example, successful dietary monitoring can help prevent poor health outcomes of ESRD patients [31,32,33], and treatment adherence monitoring can be used to support or improve adherence [34]. Remote monitoring from the dialysis center of patients’ biometrics can also help facilitate timely prescription changes, thereby improving patients’ outcomes [35], and reducing unnecessary hospitalizations, resulting in a reduced health care cost [36].
We note that currently there are no established monitoring systems available that support ESRD patients’ self-management and symptom monitoring behaviors [27]. The lack of patient monitoring leads to patients accepting significant responsibility in terms of their self-management of treatment [10]. This responsibility has been found to be burdensome on the patient and among the leading barriers to patients’ successful adoption of treatment outside of dialysis centers [37].
To ensure the AKTIV mobile dialysis device is embraced by users, particularly ESRD patients themselves, CDI has incorporated human factors engineering design principles into their design process [17]. Human factors engineering emphasizes the importance of incorporating users’ perspectives in a design process to help ensure product outcomes that meet users’ needs [38,39]. This is particularly true during the very early concept development of new medical devices to help inform a design process that fulfills users’ expectations [40,41,42]. We previously found that patients and care partners would ideally like to have a monitoring system that displays treatment information related to their mobile hemodialysis treatments [43]. Similarly, Impellicceiri [44] explored how to design a mobile dialysis monitoring system that allows patients to take an active role in their dialysis treatment. Xi and colleagues [45] found out that a supportive monitoring system can help facilitate successful hemodialysis treatments but did not report or characterize such procedures. Failing to consider the diverse perspectives of users during early idea generation and concept development of new medical systems can negatively impact the production and longevity of the device. For example, hinder access to users’ actual expectations and intended use scenarios, increase research and production cost, impact usability, and risk patients’ safety [40,42,46,47,48,49].
1.3. Study Aims
The overall goal of this study is to characterize the early design requirements for a system that monitors patients’ mobile hemodialysis treatments. To the best of our knowledge, no studies currently exist that explore users’ perspectives, particularly those of patients and care partners, on a hemodialysis monitoring system. We have considered both patients and care partners because many ESRD patients require assistance from a care partner. A dialysis care partner is an individual who provides support to a patient with ESRD. The individual is often either a close friend or a family member of an ESRD patient that voluntarily assists the patient in attending their dialysis therapies, health care needs, and activities of daily living [50]. The individual may be living in the same household as the ESRD patient; the individual may also be living elsewhere and providing medical care to the patient during home visits [51].
In order to best support patients in their self-management of treatment, it is important to identify and monitor the changes that occur in patients both before and after treatment. In this paper, to characterize the initial design requirements of a mobile dialysis monitoring system that helps support patients’ self-management and symptom monitoring behaviors, we first explored patients’ and care partners’ awareness of symptoms of ESRD before and after a patient receives a dialysis treatment (Section 3.1). We then explored patients’ and care partners’ design expectations for mobile dialysis monitoring features (Section 3.2). Engaging users and characterizing procedures according to users’ individual needs may help break down barriers to successful mobile-hemodialysis therapies [52]. This understanding may help guide a design process of a mobile hemodialysis device towards a product that ultimately meets users’ needs and satisfies them in the long term.
2. Materials and Methods
2.1. Participants
A total of 36 participants were recruited and interviewed: 24 patients and 12 care partners. Although there are no established criteria for recruiting participants for qualitative studies, studies show that it is common to recruit between 1 and 30 participants for in-depth interviews [53]. Furthermore, we found that data saturation can be achieved with 12 participants [54]. Considering these suggestions, we decided to recruit 12 participants from each of the three geographically different locations in the United States to account for variability that might exist among the three locations. This resulted in a total number of 36 participants that were equally recruited among the study locations with eight patients and four care partners from each location.
The participants were recruited from three dialysis centers within the Veterans Affairs (VA) Health Care System in the United States. The centers were located in Seattle, WA; Louisville, KY; and Nashville, TN. At each location, we partnered with a local research coordinator who approached potential participants while they were either receiving dialysis treatment as a patient or accompanying someone receiving dialysis treatment as a care partner. The research coordinators approached individuals and identified them as potential participants by first asking them if they were at the dialysis center to receive dialysis treatment as a patient or accompanying a patient as a care partner. At this screening step of the recruitment process, the research coordinators ensured that patients and care partners were not recruited as dyads but instead as individuals. Then, the research coordinators used a diversity recruiting matrix that considered participants’ age, gender, and race. We required that the care partners did not provide care for the patients enrolled in this study. Instead, the care partners should be providing care to other patients with kidney disease. The care partners should also not have kidney diseases requiring dialysis themselves. This was to avoid the possibility that the patients and their care partners might provide similar responses during the interviews, thereby inducing bias. Our decision to recruit patients and care partners individually and not as dyads was further guided by the goal of our study; to explore individual expectations rather than shared experiences, and to optimize data diversity with respect to our research constraints [55]. During our recruitment process, the participants were informed of the goal of the study and given the opportunity to ask questions they might have regarding their study commitment. Prior to participation, the participants were asked to provide informed consent and informed that at any given time throughout the study period, they had the opportunity to forgo their participation. Each patient successfully recruited was added to the recruitment matrix. At the end of the study, each participant was provided with a 30 U.S. dollar cash card as compensation for their participation. Such study compensation may help relieve participants of their financial sacrifices, acknowledge participants’ contributions to medical sciences, and accelerate the process of reaching the optimal number of study participants [56].
Table 1 shows the characteristics of the study participants. The participants were between the ages of 45 and 86 years old, with a mean age of 65.08 years (SD = 8.82). Of the participants, 25 identified as male, and 11 identified as female. In terms of ethnic demographics, 18 identified as Black (50%), 11 as White (31%), and 7 as Other (e.g., Asian, Hispanic; 19%), and most of our participants indicated their highest level of education to be a high school degree. We also gathered participants’ familiarity with mobile medical devices where the participants scored a median of 2 on a scale from 1 to 5, where 1 indicates being “very unfamiliar” and 5 indicates being “very familiar” with using mobile medical devices. We defined familiarity as the level of previous experience with mobile medical devices [57]. The five-point Likert familiarity scale was selected for its midpoint reliability and validity [58], and for being simplistic while still maintaining validity and reliability for the interval data [59].

Table 1.
Characteristics of the participants.
2.2. Interview Procedure
This study was conducted across three locations within the VA Health Care System in the United States; Seattle, WA; Louisville, KY; and Nashville, TN. Three research coordinators, one located at each of the three sites, conducted interviews at their respective locations. The interviewers had clinical backgrounds in dialysis practice and trained as research coordinators with interview training. The interviewers distributed a pre-interview survey and followed an interview guide that was developed and subsequently reviewed and revised by the authors of this paper. The interviews were conducted over a four-month period during the summer of 2019. Prior to conducting the interviews, the three research coordinators at each of the three VA study sites met in an online virtual meeting room and refined the flow of the interview questions, and established interview protocols to ensure interview consistency among the three study sites. The interview guide was nearly identical for the patients and the care partners. The main difference was that some questions asked the care partners to reflect on their patient partners’ experiences instead of their own.
Patients and care partners were all individually interviewed in two stages that occurred during two different interview sessions. First, the research coordinators administered a paper-based pre-interview survey to the participant during one of their visits to the dialysis center. The survey included demographic and background questions, as well as open-ended questions about participants’ experiences with dialysis, familiarity with mobile medical devices, and a question asking the participants to describe the designs of the most ideal mobile dialysis device. The reason for having a pre-interview survey prior to the in-person interview is twofold. First, the survey was intended to limit the risk of interview fatigue during the interview [60]. Second, as there are currently no mobile hemodialysis devices on the market, we aimed to encourage the participants to begin thinking about the most ideal design for a mobile dialysis device prior to the interview.
The second interview stage included an in-person interview where the participant was asked rating questions and in-depth open-ended questions. Each participant was given a choice of where to conduct the interview: at their home, at their respective VA research location, or at the dialysis clinic where they were recruited (provided privacy could be ensured at the clinic). All patients and care partners chose to be interviewed at their respective dialysis centers. The participants were asked to reflect on current and prior dialysis procedures. They were asked about any physical signs indicating the need for dialysis treatment or the successful removal of excess water, solutes, and toxins from the blood. We asked the participants the following questions: “How do you know if you (or your patient partner) need(s) to receive dialysis?” (Section 3.1.1) and “How do you know when dialysis was performed well?” (Section 3.1.2).
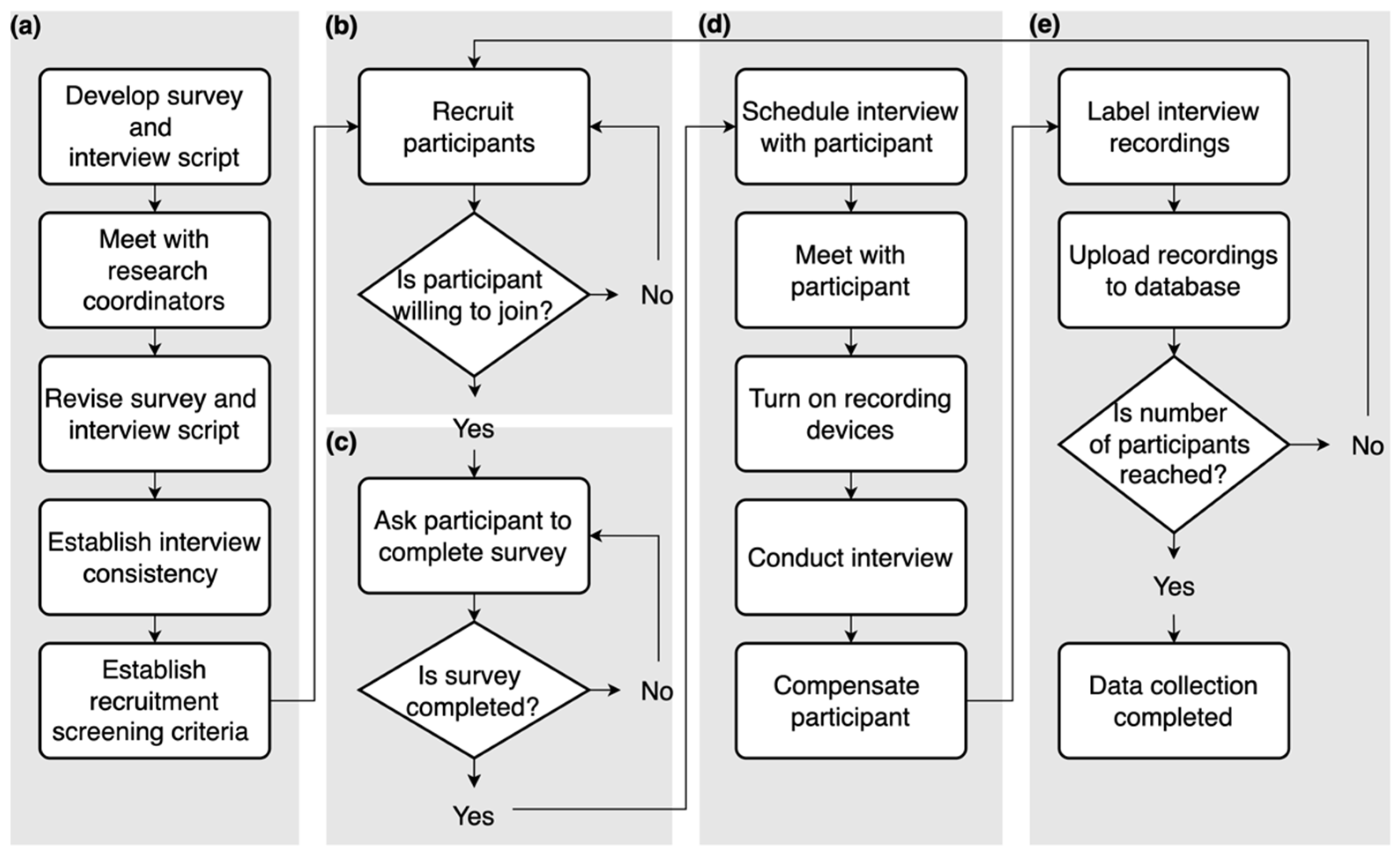
The combined duration of a participant’s pre-interview survey along with the in-person interview was approximately 80 min on average. All interviews were audio-recorded by the research coordinator and labeled using participants’ study identification (ID) numbers to ensure anonymity. After the completion of each interview, the research coordinator uploaded the recording to a secure online database where it was later accessed by a research team member and sent to Verbal-Ink, an online transcription service. Figure 1 displays the detailed interview process. This study was approved by the Institutional Review Board at the University of Washington.
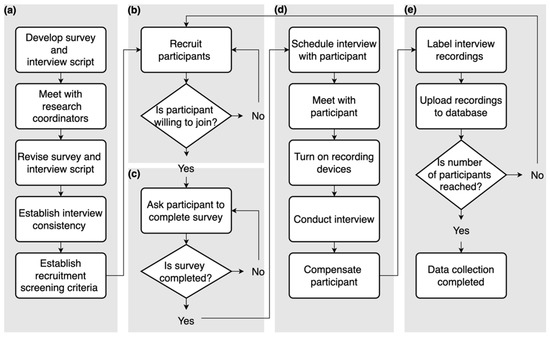
Figure 1.
Flowchart of the interview process. (a) interview preparation; (b) participant recruitment; (c) survey data collection; (d) interview data collection; (e) interview data handling and completion.
2.3. Analysis
Our analysis followed guidelines given by Hsieh and Shannon [61] and MacQueen and colleagues [62] and our prior experience in analyzing textual data [43,57,63,64,65]. We conducted both inductive and deductive content analyses. We used an inductive content analysis approach to analyze patients’ and care partners’ awareness of indicators of ESRD before and after dialysis treatments (Section 3.1). A deductive content analysis approach was used to analyze patients’ and care partners’ design expectations of monitoring procedures related to their mobile hemodialysis treatments (Section 3.2).
For the inductive content analysis, all the transcribed interviews were carefully read by two analysts and authors of this paper to gain knowledge of the interview data prior to starting the analysis process. This was an important step in achieving immersion in the data before the coding process begins [66,67,68,69]. For the inductive content analysis, structural coding was conducted using the software ATLAS.ti (Version 9.1.2 (2087)) [70,71]. In this stage, one analyst used ATLAS.ti to capture large segments of participants’ full responses to the questions of interest to preserve the context of the interview data. Then, each segment was analyzed. Keywords and short phrases uttered by the participants were highlighted and coded using either the direct words as keywords or the direct short phrases as quotations and marked by the participants’ study identification (ID) number. A word was identified as a keyword if it was in the form of an attribute related to the question of interest. For example, we asked the participants, “How do you know if dialysis was performed well?” One participant responded, “my weight goes down and I have more energy”. This response had two keywords, “weight” and “energy”, which were coded as “weight goes down” and “more energy”. The former was later rephrased to “weight loss” to be documented with another participant’s comment. The keywords and quotations were exported from ATLAS.ti to a spreadsheet to form an initial codebook. At this stage of the analysis, a second analyst joined in analyzing the interviews by confirming that all keywords and comments had been correctly captured and identified. In the event of discrepancies, adjustments were collaboratively made by the two analysts. Lastly, the codes were collaboratively organized into categories based on code commonalities. Code commonalities were identified when keywords or phrases were related to the same attribute. An overarching concept was chosen to describe each category where the repetition of keywords was the strategy most frequently used to identify a theme and to form and name each category [72]. However, during our analysis process, we noticed that by focusing only on repetitions, certain important comments made by our participants might have been overlooked. For this reason, we decided to include all responses that included a keyword in the form of an attribute of interest. To represent our results, we first created each category based on our analysis; we then displayed the number of keywords or short phrases, phrases that included a keyword, that fell under each category as a bulleted list connected to the category.
For the deductive content analysis, we followed a more directed analysis approach where we systematically identified attributes in the interviews related to participants’ expectations of monitoring procedures for mobile hemodialysis treatments. This was done to extend our understanding of patients’ and care partners’ needs for monitoring features as we had previously identified monitoring as an important feature of a dialysis device [43]. Our deductive content analysis strategy was performed in three stages. First, the transcribed interviews were carefully read by the first analyst, and structural coding was conducted. Instances related to monitoring were highlighted and coded using the temporary code “monitoring”. Then, the highlighted and coded sections were exported to a spreadsheet where a dual coding process, coding conducted separately by the two analysts, was initiated. In this stage, keywords related to monitoring were extracted from each coded section and sorted into categories separately by two analysts. Then, the second round of coding was conducted. All transcripts were searched using keywords related to monitoring; namely, “monitoring”, “alarm”, “heart rate”, “blood pressure”, “follow-up”, “smartphone”, and “Bluetooth”. In the event of identifying instances that had not previously been coded, the section was highlighted and coded using the aforementioned analysis method. The keywords used for searching the transcripts were chosen because they had either been previously identified in relation to an ideal monitoring feature for a dialysis device [43], or during the first stage of the deductive analysis. Lastly, to ensure all instances had been correctly identified, all transcripts were carefully read by both analysts. During the coding and analysis of the interviews, both analysts had weekly meetings where the coding results were compared, and discrepancies were discussed until a coding agreement was reached. To represent our results, we placed each category based on our analysis in a table and displayed the total number of comments that fell under each category along with an exemplary quotation from either a patient or a care partner.
To ensure the rigor of our qualitative analysis we considered three criteria of trustworthiness: validity, reliability, and generalizability [73]. To ensure validity, or the extent to which inferences made are accurate, the analysts had prolonged engagement with the project and prior experiences with interviewing and analyzing responses from patients and care partners to accurately capture their preferences guiding the designs of dialysis devices [43,57,63,64,65]. Our engagement is in line with human factors principles of accurately presenting users’ information to guide design decisions. The validity of our analysis is further represented by the detailed presentations of participants’ responses and our recruiting method of using a diversity matrix to capture demographic diversity and sample size to reach data saturation [74]. To ensure the reliability of our study or the extent to which the results of the study can be replicated, we aimed to meet two criteria: (i) to limit the possibility of subjective interpretations of participants’ responses, we had two researchers code the interviews and preserved participants’ responses, as codes; and (ii) for the purposes of replication, we provided detailed documentation of our process, from data collection and analysis. Lastly, to ensure the generalizability of our findings or the extent to which our results can be transferred to other patients and care partners, we made inferences based on the descriptive representation of our study population [75].
3. Results
3.1. Indicators of ESRD before and after a Dialysis Treatment
3.1.1. Indicators of ESRD Suggesting Patients’ Need for a Dialysis Treatment
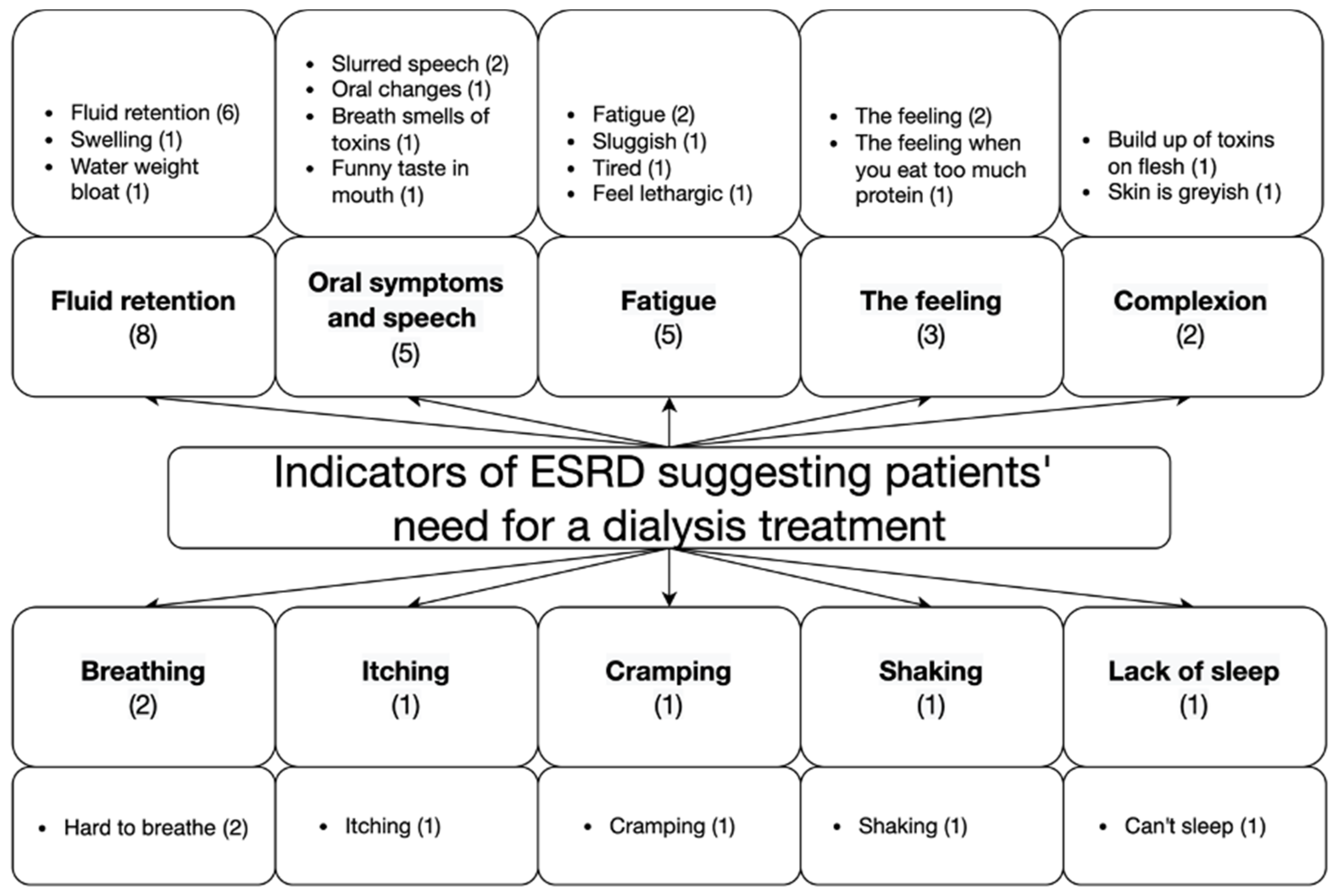
Figure 2 displays the categories and keywords related to patients’ and care partners’ awareness of indicators of ESRD suggesting a patient’s need for dialysis treatment. Most participants mentioned that they knew the treatment was needed based on the scheduled sessions mentioned by a health care provider (20 out of 54 comments). Although some participants specifically stated that they did not recognize or did not have any physical indicators suggesting the need for treatment (5 comments), other participants reported diverse physical signs indicating the need for treatment. Participants reported that they knew the treatment was needed based on fluid retention or swelling (8 comments); oral changes such as slurred speech and foul-smelling breath (5 comments); fatigue (5 comments); a specific feeling indicating patients’ deteriorating health (3 comments); complexion (2 comments); breathing difficulties (2 comments); itching (1 comment); cramping (1 comment); shaking (1 comment); and lack of sleep (1 comment). One care partner from Seattle stated, “Sometimes at night he gets out of breath. He can’t breathe too well. And that means that he’s gathered too much fluid in his body. And sometimes we are up practically all night. Just sit up and once I had to get in the middle of the night and bring him to the emergency room.” A patient from Nashville reported, “Other than being on a schedule, you can feel it when you have too much fluid on you or when you’ve eaten incorrectly and you need to cleanse yourself, and that can be signs of itching. It could be cramping. You can also feel your [waste] build go up if you’ve eaten too much protein. So your body gives you signs that tell you it’s time for another session”.
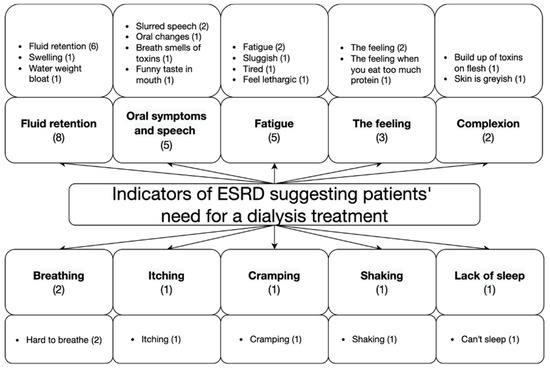
Figure 2.
Categories and keywords related to patients’ and care partners’ awareness of indicators of ESRD suggesting patients’ need for dialysis treatment. The number in parentheses next to each category indicates the number of times a related keyword or comment was mentioned by a participant.
3.1.2. Indicators of ESRD Suggesting a Successful Dialysis Treatment
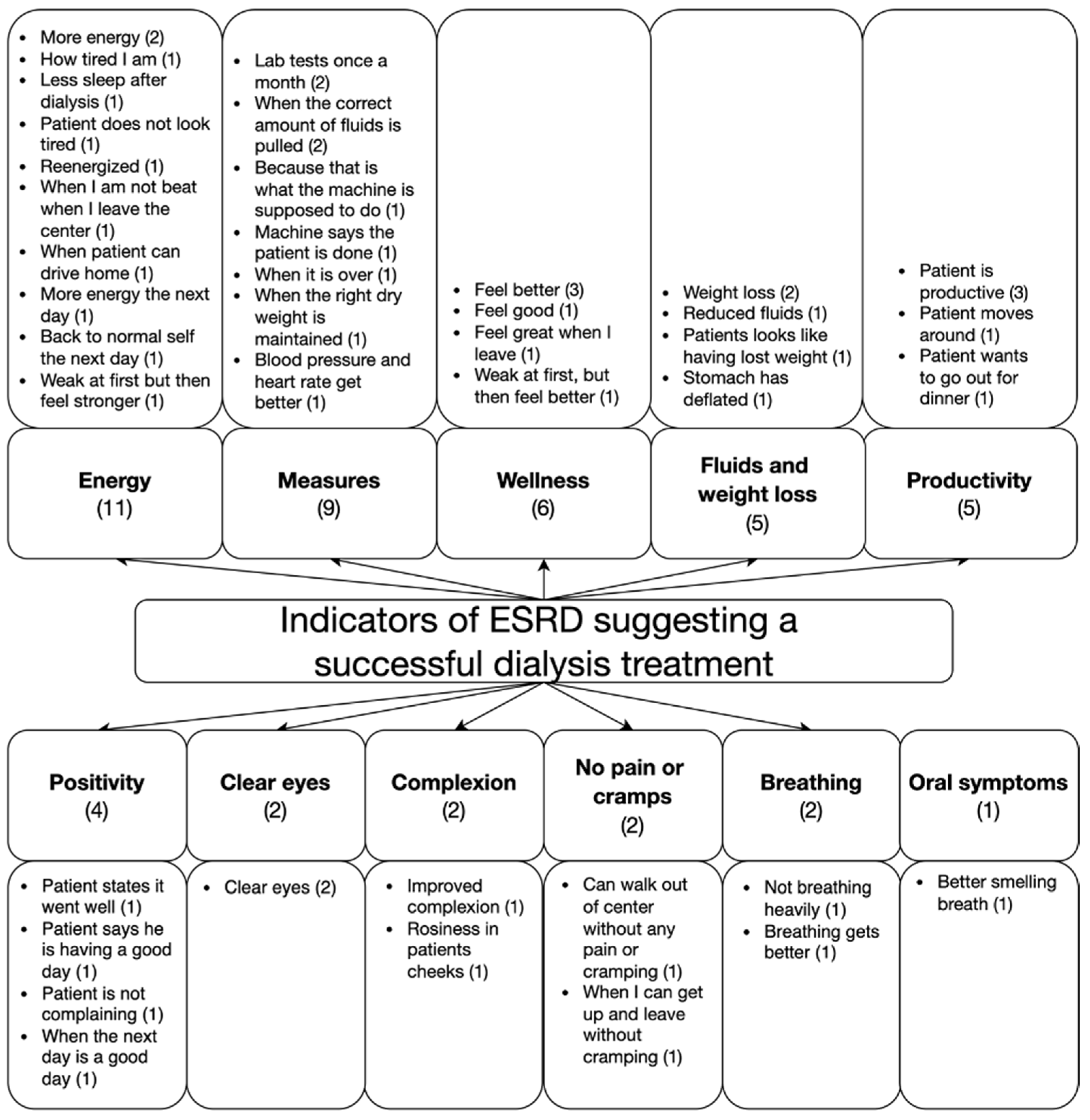
Categories and keywords related to patients’ and care partners’ awareness of indicators of ESRD suggesting a successful dialysis treatment are shown in Figure 3. Although four participants were unable to identify any indicators (4 comments), most of the participants reported observing physical or emotional changes (40 comments). Increased energy was the most frequently observed indicator. One patient from Louisville stated, “Oh, I feel great. I’ve got reenergized, a little bit. To me, it is normal now. When I first started, I felt a little funny, but now it’s normal to feel the way I feel, and I don’t gotta worry about all the toxicity that is in my bloodstream. I know it’s been cleaned out.” Other comments related to indicators of a successful treatment included a feeling of wellness (7 comments), reduced fluids or weight loss (5 comments), increased productivity (5 comments), positivity (4 comments), clear eyes (2 comments), improved complexion (2 comments), a lack of physical pain or cramping (2 comments), improved breathing (2 comments), and better-smelling breath (1 comment).
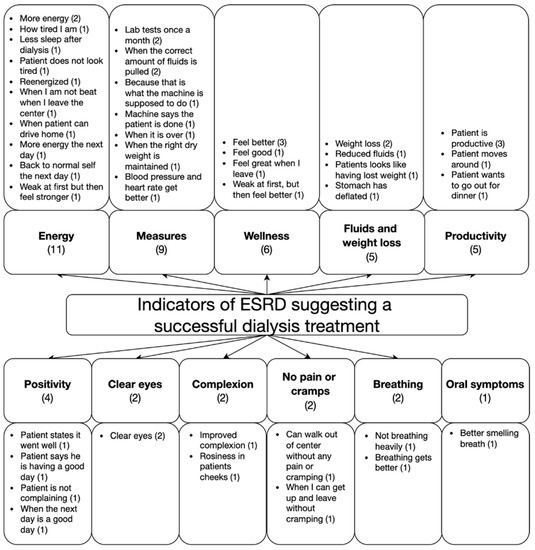
Figure 3.
Categories and keywords related to patients’ and care partners’ awareness of indicators of ESRD suggesting a successful dialysis treatment. The number in parentheses next to each category indicates the number of times a related keyword or comment was mentioned by a participant.
Participants who did not report any physical or emotional signs of successful dialysis treatment instead mostly reported objective measures (9 comments), including parameters displayed on currently used dialysis machines, patients’ weights before and after treatment, and results from regular laboratory tests. One Nashville patient stated, “It’s always performed well because that’s what the machine is supposed to do.” Another patient from Nashville stated, “If I go and weigh, I know if they have pulled correctly or not. Sometimes the machine pulls more than we expect, and at that time they have to pull me back and give me some—what do you call it, saline?”
3.2. Design Expectations for Establishing Mobile Dialysis Monitoring Procedures
A total of 28 comments related to patients’ and care partners’ design expectations for mobile dialysis monitoring were identified. As shown in the first and second categories in Table 2, general features of monitoring were most frequently mentioned (9 comments). Participants also frequently mentioned the need for establishing a monitoring procedure that would take the form of regular follow-up sessions with the patients by a health care worker (5 comments). The participants further mentioned the need for a system that monitors patients’ heart condition and blood pressure (5 comments), includes an alarm that notifies patients of urgent medical, or equipment needs (3 comments), allows another person to monitor the patients during and after dialyzing (3 comments), and uses mobile phones or watches to automatically record and send patients’ information to the dialysis center (3 comments).

Table 2.
Design features along with exemplary quotations from patients and care partners related to mobile dialysis monitoring. The number in parentheses next to each category indicates the number of related comments.
Overall, participants wanted a mobile dialysis device with an interface that would display indicators of patients’ health conditions, such as the current and remaining status of their dialysis treatments, blood pressure, and heart rate, while the patients were connected to the device. Some participants wanted to be able to access these recordings via smart applications that would ideally send these recordings to a dialysis center for remote monitoring of patients’ health conditions. The participants emphasized the need for a regular follow-up procedure to ensure patients’ successful self-management of their mobile dialysis treatments.
4. Discussion
To the best of our knowledge, this study is the first to characterize the design requirements for monitoring procedures for a mobile dialysis device using a human factor engineering approach. To help support patients’ self-monitoring behaviors, we explored patients’ and care partners’ awareness of ESRD symptoms that suggest a patient’s need for dialysis treatment as well as indicators that might suggest a dialysis treatment has been successful. We also explored patients’ and care partners’ design expectations regarding ideal monitoring procedures before patients and care partners begin using a mobile dialysis device.
4.1. Indicators of ESRD before and after a Dialysis Treatment
In exploring patients’ and care partners’ awareness of indicators that suggest a patient’s need for dialysis treatment, we found that patients and care partners notice physical and emotional changes in patients before and after they receive dialysis treatment. While some participants reported actively noticing patients’ physical or emotional changes (e.g., slurred speech, fluid retention, and fatigue), most of the participants indicated passively knowing from the patients’ prescribed treatment schedules when treatments are necessary (Figure 2). In contrast, while few patients referred to objective measures (e.g., patients’ weight, blood pressure, treatment duration) when asked about their awareness of indicators of successful dialysis treatment, most of the participants reported a range of physical, emotional, and cognitive changes in the patients (e.g., increased energy, weight loss, wellness, positivity, and productivity) as indicators of successful dialysis treatment (Figure 3).
The physiological indicators identified in this study may help maintain patients’ confidence in the self-management of their dialysis therapies [28]. Studies show that monitoring target parameters can help support patients’ self-management behaviors, ultimately facilitating the patients’ well-being [29]. Additionally, successful self-management of one’s health is dependent on good communication between a patient and clinician where a patient is able to report their disease indicators and experiences and receive in return information, support, and guidance [24]. These findings have the potential to guide researchers in designing an interface for a mobile dialysis device that incorporates the monitoring of patients’ physiological, emotional, and cognitive changes during their mobile dialysis treatments and helps facilitate communication between a dialysis patient and the patient’s healthcare team.
4.2. Design Expectations for Establishing Mobile Dialysis Monitoring Procedures
Analyzing patients’ expectations for mobile dialysis monitoring procedures, we uncovered that patients and care partners would like device-integrated monitoring features that automatically track patients’ health and treatment-related factors (e.g., heart rate, blood pressure, and levels of dialysis). The patients also expected smart and remote monitoring options that allow for digital and wireless access to patients’ treatment records, thereby extending the interactive communication between dialysis patients and the patients’ healthcare teams. In addition, the participants indicated they would like the ability to track and capture individual target parameters with notifications to both parties when a parameter falls outside of prespecified ranges. Incorporating the monitoring features identified in this study (Table 2) into the designs of mobile dialysis devices has the potential to improve patients’ mobile dialysis experiences while simultaneously yielding better clinical outcomes and reduced treatment costs. Remote monitoring of patients’ physiological indicators and mobile dialysis treatment data such as patients’ vital signs, treatment adherence, and ultrafiltration values may help reduce the risk of repeated or unnecessary hospitalizations [76,77,78].
4.3. Implications and Contributions
Despite the goal of supporting ESRD patients’ independent management of their dialysis therapies, our findings strongly suggest that many patients long for partnership in care via bidirectional monitoring between the patient and the patient’s provider. Bidirectional monitoring would allow a patient to self-manage their therapies while simultaneously being under safety supervision and support. Remote safety supervision and support entails the recording and sharing of patients’ individual health information across geographically diverse regions and allows healthcare workers to access both longitudinal and near-instantaneous recordings of patients’ physiological and treatment measures. Remote supervision through monitoring allows health care workers to identify instances of urgent medical and equipment needs or longitudinal trends suggesting patients’ need for additional education or support. Such remote patient monitoring has the potential to help facilitate medical decision-making and support patients in self-managing their dialysis therapies outside of medical centers [35,79,80,81]. To our knowledge, the expectation has been partially resolved through a health information sharing platform that is currently available on the market [82]. Although the current health information sharing platform shows potential in supporting patients’ successful dialysis by incorporating it into the mobile dialysis system, the platform mainly focuses on in-center treatments and aims to support clinicians’ workflow more than patients’ self-management of treatment. To better support dialysis across different user groups and locations, our findings can be integrated into data management platforms for both the current and future dialysis devices. Such integrations that are tailored according to users’ needs and expectations may strengthen the link between a dialysis community and information technology that in return helps support patients’ successful dialysis experiences.
Building on our previous research, this study deepens our understanding of patients’ and care partners’ preferences and expectations for the design of a mobile dialysis device. Researchers at the Center for Dialysis Innovation at the University of Washington are currently designing and developing the Ambulatory Kidney to Improve Vitality (AKTIV). The AKTIV is a mobile dialysis device that allows patients with ESRD to undergo continuous dialysis treatments outside of dialysis centers [57]. The overall goal of the AKTIV is to improve ESRD patients’ quality of life by providing them with the freedom of treatment location and flexibility in treatment timing. The AKTIV is expected to provide similar or greater levels of benefits than current existing home dialysis treatments as it will be designed to allow the patient a greater number of dialysis hours without restrictions on their mobility. This method of treatment will more closely approximate renal functioning and improve biological variability that occurs with the current thrice-weekly dialysis treatments [2].
4.4. Limitations
Several limitations of this study should be considered. First, although we aimed to recruit a diverse sample of participants by following a recruitment matrix that considered demographic diversity, our study population was of limited age and gender diversity. All our patient participants were male, and most of the care partners were female. This sampling limitation is largely due to the demographic diversity imbalance within the VA population. The VA population has a higher median age compared to the general ESRD population (64 vs. 41 years old, respectively), and there is a far greater number of men than women (89% vs. 11%, respectively), and is predominantly white race (80%) [83,84,85]. In terms of the broader ESRD patient population, the disease disproportionately affects men more than women (60% vs. 40%, respectively), affects older individuals more than younger people (85% of ESRD patients are at least 45 years old), and affects black individuals more than individuals of other races (78.6% higher than the next group) [84]. Studies suggest that such disproportional distribution of ESRD between individuals may be linked to several factors including physiological differences such as gender hormones [86], socioeconomic status [87], and lifestyle-related factors that induce the risk of obesity, diabetes, and hypertension contributing to the disease development [88]. Given this information, the findings may not reflect the perspectives of all patients with ESRD and their care partners. Mobile hemodialysis experiences with bi-directional monitoring of patients’ vital signs and disease symptoms may be different across different user populations. We acknowledge that our study population may represent minority groups in terms of race and level of education. We highlight the importance of overcoming challenges that may exist in establishing a mobile dialysis care program across different socioeconomic groups. Secondly, while this study explored both patients’ and care partners’ perspectives, it did not include clinicians’ points of view. Clinicians’ opinions are an important consideration when designing a medical device and designing and implementing new monitoring systems and procedures.
5. Conclusions
Characterizing design requirements according to users’ perspectives during the early stages of designing a mobile dialysis device reflects our commitment to a human factors engineering design process. This understanding may help guide design decisions towards an end product that is tailored according to users’ needs and helps support patients’ safe self-management of their therapies using mobile dialysis devices. Future studies should aim to explore the perspectives of the more diverse population of mobile dialysis device users, particularly characterizing clinicians’ perspectives for monitoring systems and associated procedures for mobile dialysis device therapies.
Author Contributions
Conceptualization, A.A.J., J.-E.K. and L.G.K.; methodology, A.A.J. and J.-E.K.; software, A.A.J.; validation, A.A.J., J.-E.K. and L.G.K.; formal analysis, A.A.J.; investigation, A.A.J., J.-E.K. and L.G.K.; resources, J.-E.K. and L.G.K.; data curation, A.A.J. and J.-E.K.; writing—original draft preparation, A.A.J.; writing—review and editing, J.-E.K. and L.G.K.; visualization, A.A.J.; supervision, J.-E.K.; project administration, J.-E.K. and L.G.K.; funding acquisition, J.-E.K. and L.G.K. All authors have read and agreed to the published version of the manuscript.
Funding
The authors gratefully acknowledge a grant from the Northwest Kidney Centers to the Center for Dialysis Innovation (CDI) for support during this study. This work was also supported by Award 101-19-1-2965-0001 from the U.S. Department of Veterans Affairs. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Institutional Review Board Statement
This research was approved by the Institutional Review Board at the University of Washington (protocol code: STUDY00006639) and Veterans Affairs (protocol code: 01763).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank Robin Stillwell for conducting the interviews for this study and Glenda Roberts for reviewing and revising the interview script.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abbasi, M.A.; Chertow, G.M.; Hall, Y.N. End-Stage Renal Disease. BMJ Clin. Evid. 2010, 2010, 2002. [Google Scholar] [PubMed]
- Himmelfarb, J.; Ikizler, T.A. Hemodialysis. N. Engl. J. Med. 2010, 363, 1833–1845. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Saran, R. Global Dialysis Perspective: United States. Kidney360 2020, 1, 1137. [Google Scholar] [CrossRef] [PubMed]
- Delgado, C.; Johansen, K.L. Barriers to Exercise Participation among Dialysis Patients. Nephrol. Dial. Transplant. 2012, 27, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.D.S.; Fernandes, N.D.S.; de Melo, N.P.; Abrita, R.; Grincenkov, F.R.D.S.; Fernandes, N.M.D.S. Beyond Quality of Life: A Cross Sectional Study on the Mental Health of Patients with Chronic Kidney Disease Undergoing Dialysis and Their Caregivers. Health Qual. Life Outcomes 2017, 15, 74. [Google Scholar] [CrossRef]
- Edalat-Nejad, M.; Qlich-Khani, M. Quality of Life and Sleep in Hemodialysis Patients. Saudi J. Kidney Dis. Transplant. 2013, 24, 514. [Google Scholar] [CrossRef]
- Urquhart-Secord, R.; Craig, J.C.; Hemmelgarn, B.; Tam-Tham, H.; Manns, B.; Howell, M.; Polkinghorne, K.R.; Kerr, P.G.; Harris, D.C.; Thompson, S.; et al. Patient and Caregiver Priorities for Outcomes in Hemodialysis: An International Nominal Group Technique Study. Am. J. Kidney Dis. 2016, 68, 444–454. [Google Scholar] [CrossRef]
- Combes, G.; Allen, K.; Sein, K.; Girling, A.; Lilford, R. Taking Hospital Treatments Home: A Mixed Methods Case Study Looking at the Barriers and Success Factors for Home Dialysis Treatment and the Influence of a Target on Uptake Rates. Implement. Sci. 2015, 10, 1–13. [Google Scholar] [CrossRef]
- Young, B.A.; Chan, C.; Blagg, C.; Lockridge, R.; Golper, T.; Finkelstein, F.; Shaffer, R.; Mehrotra, R. ASN Dialysis Advisory Group How to Overcome Barriers and Establish a Successful Home HD Program. Clin. J. Am. Soc. Nephrol. 2012, 7, 2023–2032. [Google Scholar] [CrossRef]
- Moran, J.; Kraus, M. Starting a Home Hemodialysis Program. In Proceedings of the Seminars in Dialysis; Wiley Online Library: Hoboken, NJ, USA, 2007; Volume 20, pp. 35–39. [Google Scholar]
- Bieber, S.D.; Young, B.A. Home Hemodialysis: Core Curriculum 2021. Am. J. Kidney Dis. 2021, 78, 876–885. [Google Scholar] [CrossRef]
- Marshall, M.R.; Byrne, B.G.; Kerr, P.G.; McDonald, S.P. Associations of Hemodialysis Dose and Session Length with Mortality Risk in Australian and New Zealand Patients. Kidney Int. 2006, 69, 1229–1236. [Google Scholar] [CrossRef] [PubMed]
- Mowatt, G.; Vale, L.; MacLeod, A. Systematic Review of the Effectiveness of Home versus Hospital or Satellite Unit Hemodialysis for People with End-Stage Renal Failure. Int. J. Technol. Assess. Health Care 2004, 20, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Saran, R.; Bragg-Gresham, J.L.; Levin, N.W.; Twardowski, Z.J.; Wizemann, V.; Saito, A.; Kimata, N.; Gillespie, B.W.; Combe, C.; Bommer, J. Longer Treatment Time and Slower Ultrafiltration in Hemodialysis: Associations with Reduced Mortality in the DOPPS. Kidney Int. 2006, 69, 1222–1228. [Google Scholar] [CrossRef]
- Mitra, S.; Kharbanda, K.; Ebah, L. Home Haemodialysis: Providing Opportunities to Reimagine Haemodialysis Care. Nephrol. Ther. 2021, 17, S60–S63. [Google Scholar] [CrossRef] [PubMed]
- USRDS. USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; USRDS: Bethesda, MD, USA, 2020. [Google Scholar]
- Himmelfarb, J.; Ratner, B. Wearable Artificial Kidney: Problems, Progress and Prospects. Nat. Rev. Nephrol. 2020, 16, 558–559. [Google Scholar] [CrossRef] [PubMed]
- van Gelder, M.K.; Mihaila, S.M.; Jansen, J.; Wester, M.; Verhaar, M.C.; Joles, J.A.; Stamatialis, D.; Masereeuw, R.; Gerritsen, K.G.F. From Portable Dialysis to a Bioengineered Kidney. Expert Rev. Med. Devices 2018, 15, 323–336. [Google Scholar] [CrossRef]
- Gura, V.; Rivara, M.B.; Bieber, S.; Munshi, R.; Smith, N.C.; Linke, L.; Kundzins, J.; Beizai, M.; Ezon, C.; Kessler, L. A Wearable Artificial Kidney for Patients with End-Stage Renal Disease. JCI insight 2016, 1, e86397. [Google Scholar] [CrossRef]
- Gura, V.; Macy, A.S.; Beizai, M.; Ezon, C.; Golper, T.A. Technical Breakthroughs in the Wearable Artificial Kidney (WAK). Clin. J. Am. Soc. Nephrol. 2009, 4, 1441–1448. [Google Scholar] [CrossRef]
- Ronco, C.; Davenport, A.; Gura, V. Toward the Wearable Artificial Kidney. Hemodial. Int. 2008, 12, S40–S47. [Google Scholar] [CrossRef]
- Winner: The Wearable AKTIV: Artificial Kidney to Improve Vitality. 2022. Available online: https://www.kidneyx.org/PrizeCompetitions/UnivWashington (accessed on 26 September 2022).
- Curtin, R.B.; Mapes, D.L. Health Care Management Strategies of Long-Term Dialysis Survivors. Nephrol. Nurs. J. 2001, 28, 385. [Google Scholar]
- Curtin, R.B.; Mapes, D.; Schatell, D.; Burrows-Hudson, S. Self-Management in Patients with End Stage Renal Disease: Exploring Domains and Dimensions. Nephrol. Nurs. J. 2005, 32, 389–395. [Google Scholar] [PubMed]
- Ormandy, P.; Hulme, C. Measuring Patients’ Preferences and Priorities for Information in Chronic Kidney Disease. Inf. Res. 2013, 18, 588. [Google Scholar]
- Van Biesen, W.; Van Der Veer, S.N.; Murphey, M.; Loblova, O.; Davies, S. Patients’ Perceptions of Information and Education for Renal Replacement Therapy: An Independent Survey by the European Kidney Patients’ Federation on Information and Support on Renal Replacement Therapy. PLoS ONE 2014, 9, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Taber-Hight, E.B.; Miller, B.W. Perceptions of Home Dialysis Training and Experience among US Nephrology Fellows. Am. J. Kidney Dis. 2021, 77, 713–718. [Google Scholar] [CrossRef] [PubMed]
- John, O.; Jha, V. Remote Patient Management in Peritoneal Dialysis: An Answer to an Unmet Clinical Need. Remote patient Manag. Perit. Dial. 2019, 197, 99–112. [Google Scholar]
- Yang, Y.; Chen, H.; Qazi, H.; Morita, P.P. Intervention and Evaluation of Mobile Health Technologies in Management of Patients Undergoing Chronic Dialysis: Scoping Review. JMIR Mhealth Uhealth 2020, 8, e15549. [Google Scholar] [CrossRef]
- Liu, N.; Kim, J.; Jung, Y.; Arisy, A.; Nicdao, M.A.; Mikaheal, M.; Baldacchino, T.; Khadra, M.; Sud, K. Remote Monitoring Systems for Chronic Patients on Home Hemodialysis: Field Test of a Copresence-Enhanced Design. JMIR Hum. factors 2017, 4, e7078. [Google Scholar] [CrossRef]
- Connelly, K.; Siek, K.A.; Chaudry, B.; Jones, J.; Astroth, K.; Welch, J.L. An Offline Mobile Nutrition Monitoring Intervention for Varying-Literacy Patients Receiving Hemodialysis: A Pilot Study Examining Usage and Usability. J. Am. Med. Informatics Assoc. 2012, 19, 705–712. [Google Scholar] [CrossRef]
- Kosa, S.D.; Monize, J.; D’Souza, M.; Joshi, A.; Philip, K.; Reza, S.; Samra, S.; Serrago, B.; Thabane, L.; Gafni, A. Nutritional Mobile Applications for CKD Patients: Systematic Review. Kidney Int. Rep. 2019, 4, 399–407. [Google Scholar] [CrossRef]
- Welch, J.L.; Astroth, K.S.; Perkins, S.M.; Johnson, C.S.; Connelly, K.; Siek, K.A.; Jones, J.; Scott, L.L. Using a Mobile Application to Self-Monitor Diet and Fluid Intake among Adults Receiving Hemodialysis. Res. Nurs. Health 2013, 36, 284–298. [Google Scholar] [CrossRef]
- Kumar, S.; Nilsen, W.J.; Abernethy, A.; Atienza, A.; Patrick, K.; Pavel, M.; Riley, W.T.; Shar, A.; Spring, B.; Spruijt-Metz, D. Mobile Health Technology Evaluation: The MHealth Evidence Workshop. Am. J. Prev. Med. 2013, 45, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Nicdao, M.A.; Kim, J.; Baldacchino, T.; Jung, Y.H.; Mikaheal, M.; Patekar, A.; Sud, K. My Home Hemo’app-a New Telehealth Tool for Remote Monitoring of Patients on Home Haemodialysis. Ren. Soc. Australas. J. 2016, 12, 41–47. [Google Scholar]
- Lew, S.Q. Telehealth in Peritoneal Dialysis: Review of Patient Management. Adv. Perit. Dial. 2018, 34, 32–37. [Google Scholar] [PubMed]
- Cafazzo, J.A.; Leonard, K.; Easty, A.C.; Rossos, P.G.; Chan, C.T. Patient-Perceived Barriers to the Adoption of Nocturnal Home Hemodialysis. Clin. J. Am. Soc. Nephrol. 2009, 4, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.D.; Wickens, C.D.; Liu, Y.; Boyle, L.N. Designing for People: An Introduction to Human Factors Engineering, 3rd ed.; CreateSpace Independent Publishing Platform: Scotts Valley, CA, USA, 2017; ISBN 9781539808008. [Google Scholar]
- Money, A.G.; Barnett, J.; Kuljis, J.; Craven, M.P.; Martin, J.L.; Young, T. The Role of the User within the Medical Device Design and Development Process: Medical Device Manufacturers’ Perspectives. BMC Med. Inform. Decis. Mak. 2011, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Garmer, K.; Liljegren, E.; Osvalder, A.-L.; Dahlman, S. Application of Usability Testing to the Development of Medical Equipment. Usability Testing of a Frequently Used Infusion Pump and a New User Interface for an Infusion Pump Developed with a Human Factors Approach. Int. J. Ind. Ergon. 2002, 29, 145–159. [Google Scholar] [CrossRef]
- Shah, S.G.S.; Robinson, I.; Alshawi, S. Developing Medical Device Technologies from Users’ Perspectives: A Theoretical Framework for Involving Users in the Development Process. Int. J. Technol. Assess. Health Care 2009, 25, 514–521. [Google Scholar] [CrossRef]
- Sculpher, M.; Drummond, M.; Buxton, M. The Iterative Use of Economic Evaluation as Part of the Process of Health Technology Assessment. J. Health Serv. Res. Policy 1997, 2, 26–30. [Google Scholar] [CrossRef]
- Anna Jónsdóttir, A.; Firestone, S.; Kessler, L.; Kim, J.-E. Human Factors Considerations in Designing a Portable Dialysis Device: Understanding Patients’ and Care Partners’ Needs for Increased Mobility. In Proceedings of the Proceedings of the Human Factors and Ergonomics Society Annual Meeting, Baltimore, MD, USA, 3–8 October 2021; SAGE Publications: Los Angeles, CA, USA, 2021; Volume 65, pp. 520–524. [Google Scholar]
- Impellicceiri, S. Designing Medical Devices for Healing Interactions: A Dialysis Case Study. Master’s Thesis, Carnegie Mellon University, Pittsburgh, PA, USA, 2015. [Google Scholar]
- Xi, W.; Singh, P.M.; Harwood, L.; Lindsay, R.; Suri, R.; Brown, J.B.; Moist, L.M. Patient Experiences and Preferences on Short Daily and Nocturnal Home Hemodialysis. Hemodial. Int. 2013, 17, 201–207. [Google Scholar] [CrossRef]
- Chiu, C.C.; Vicente, K.J.; BUFFO-SEQUEIRA, I.; Hamilton, R.M.; McCRINDLE, B.W. Usability Assessment of Pacemaker Programmers. Pacing Clin. Electrophysiol. 2004, 27, 1388–1398. [Google Scholar] [CrossRef]
- Kaufman, D.R.; Patel, V.L.; Hilliman, C.; Morin, P.C.; Pevzner, J.; Weinstock, R.S.; Goland, R.; Shea, S.; Starren, J. Usability in the Real World: Assessing Medical Information Technologies in Patients’ Homes. J. Biomed. Inform. 2003, 36, 45–60. [Google Scholar] [CrossRef]
- Lang, A.R.; Martin, J.L.; Sharples, S.; Crowe, J.A. The Effect of Design on the Usability and Real World Effectiveness of Medical Devices: A Case Study with Adolescent Users. Appl. Ergon. 2013, 44, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Rochford, L.; Rudelius, W. New Product Development Process: Stages and Successes in the Medical Products Industry. Ind. Mark. Manag. 1997, 26, 67–84. [Google Scholar] [CrossRef]
- Bennett, P.N.; Schatell, D.; Shah, K.D. Psychosocial Aspects in Home Hemodialysis: A Review. Hemodial. Int. 2015, 19, S128–S134. [Google Scholar] [CrossRef]
- Chan, C.T.; Wallace, E.; Golper, T.A.; Rosner, M.H.; Seshasai, R.K.; Glickman, J.D.; Schreiber, M.; Gee, P.; Rocco, M. V Exploring Barriers and Potential Solutions in Home Dialysis: An NKF-KDOQI Conference Outcomes Report. Am. J. Kidney Dis. 2019, 73, 363–371. [Google Scholar] [CrossRef]
- Wilkie, M.; Barnes, T. Shared Hemodialysis Care: Increasing Patient Involvement in Center-Based Dialysis. Clin. J. Am. Soc. Nephrol. 2019, 14, 1402–1404. [Google Scholar] [CrossRef]
- Bengtsson, M. How to Plan and Perform a Qualitative Study Using Content Analysis. NursingPlus Open 2016, 2, 8–14. [Google Scholar] [CrossRef]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough? An Experiment with Data Saturation and Variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Eisikovits, Z.; Koren, C. Approaches to and Outcomes of Dyadic Interview Analysis. Qual. Health Res. 2010, 20, 1642–1655. [Google Scholar] [CrossRef]
- Pandya, M.; Desai, C. Compensation in Clinical Research: The Debate Continues. Perspect. Clin. Res. 2013, 4, 70. [Google Scholar] [CrossRef]
- Kim, J.; Kessler, L.; Mccauley, Z.; Niiyama, I.; Boyle, L.N.; Kim, J. Human Factors Considerations in Designing a Personalized Mobile Dialysis Device: An Interview Study. Appl. Ergon. 2020, 85, 103003. [Google Scholar] [CrossRef] [PubMed]
- O’Muircheartaigh, C.A.; Krosnick, J.A.; Helic, A. Middle Alternatives, Acquiescence, and the Quality of Questionnaire Data; Harris School of Public Policy Studies, University of Chicago: Chicago, IL, USA, 2000. [Google Scholar]
- Cox, E.P. The Optimal Number of Response Alternatives for a Scale: A Review. J. Mark. Res. 1980, 17, 407–422. [Google Scholar] [CrossRef]
- Lavrakas, P.J. Encyclopedia of Survey Research Methods; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2008. [Google Scholar]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- MacQueen, K.M.; McLellan, E.; Kay, K.; Milstein, B. Codebook Development for Team-Based Qualitative Analysis. Field Methods 1998, 10, 31–36. [Google Scholar] [CrossRef]
- Mccauley, Z.; Niiyama, I.; Kessler, L.; Kim, J. User-Centered Design for a Customized Mobile Dialysis Device for Patients with ESRD: An Interview Study. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2019, 63, 762–766. [Google Scholar] [CrossRef]
- Jónsdóttir, A.A.; Kessler, L.G.; Rim, S.-Y.; Kim, J.-E. What Patients and Care Partners Want in a Wearable Dialysis Device: A Mixed-Methods Study. IISE Trans. Healthc. Syst. Eng. 2022, 12, 101–110. [Google Scholar] [CrossRef]
- Jónsdóttir1, A.A.; Kessler, L.; Rim, S.Y.; Kim, J.-E. Users’ Needs in Designing a Mobile Dialysis Device. Insights from an Interview in a Mixed Methods Study. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2020, 64, 746–749. [Google Scholar] [CrossRef]
- Tesch, R. Qualitative Research: Analysis Types and Software; Routledge: London, UK, 2013. [Google Scholar]
- Miles, M.B.; Huberman, M. Qualitative Data Analysis: An Expanded Sourcebook, 2nd ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 1994. [Google Scholar]
- Morgan, D.L. Qualitative Content Analysis: A Guide to Paths Not Taken. Qual. Health Res. 1993, 3, 112–121. [Google Scholar] [CrossRef]
- Morse, J.M.; Field, P.A. Nursing Research: The Application of Qualitative Approaches; Nelson Thornes: Cheltenham, UK, 1995. [Google Scholar]
- Muhr, T. ATLAS.Ti: The Knowledge Workbench: Visual Qualitative Data, Analysis, Management, Model Building: Short User’s Manual; Scientific Software Development: Berlin, Germany, 1997. [Google Scholar]
- Muhr, T. A Brief History of ATLAS. Available online: https://atlasti.com/about-atlas-ti (accessed on 26 September 2022).
- Ryan, G.W.; Bernard, H.R. Techniques to Identify Themes. Field Methods 2003, 15, 85–109. [Google Scholar] [CrossRef]
- Morse, J.M. Critical Analysis of Strategies for Determining Rigor in Qualitative Inquiry. Qual. Health Res. 2015, 25, 1212–1222. [Google Scholar] [CrossRef]
- Fusch, P.I.; Ness, L.R. Are We There yet? Data Saturation in Qualitative Research. Qual. Rep. 2015, 20, 1408–1416. [Google Scholar] [CrossRef]
- Maxwell, J.A.; Chmiel, M. Notes toward a Theory of Qualitative Data Analysis. SAGE Handb. Qual. Data Anal. 2014, 1, 21–34. [Google Scholar]
- Erickson, K.F.; Winkelmayer, W.C.; Chertow, G.M.; Bhattacharya, J. Physician Visits and 30-Day Hospital Readmissions in Patients Receiving Hemodialysis. J. Am. Soc. Nephrol. 2014, 25, 2079. [Google Scholar] [CrossRef] [PubMed]
- Martino, F.; Adıbelli, Z.; Mason, G.; Nayak, A.; Ariyanon, W.; Rettore, E.; Crepaldi, C.; Rodighiero, M.; Ronco, C. Home Visit Program Improves Technique Survival in Peritoneal Dialysis. Blood Purif. 2014, 37, 286–290. [Google Scholar] [CrossRef]
- Slinin, Y.; Guo, H.; Li, S.; Liu, J.; Ensrud, K.; Gilbertson, D.T.; Collins, A.J.; Ishani, A. Association of Provider–Patient Visit Frequency and Patient Outcomes on Hemodialysis. J. Am. Soc. Nephrol. 2012, 23, 1560. [Google Scholar] [CrossRef]
- Krishna, V.N.; Managadi, K.; Smith, M.; Wallace, E. Telehealth in the Delivery of Home Dialysis Care: Catching up with Technology. Adv. Chronic Kidney Dis. 2017, 24, 12–16. [Google Scholar] [CrossRef]
- Minatodani, D.E.; Chao, P.J.; Berman, S.J. Home Telehealth: Facilitators, Barriers, and Impact of Nurse Support among High-Risk Dialysis Patients. Telemed. e-Health 2013, 8, 573–578. [Google Scholar] [CrossRef]
- Whitlow, M.; Wallace, E. Remote Patient Monitoring: An Important Tool in Advancing Home Dialysis. Kidney Med. 2019, 1, 327–328. [Google Scholar] [CrossRef]
- Stuard, S.; Amato, C.; Nash, S. Connected Health at Fresenius Medical Care|FMCNA. Available online: https://fmcna.com/insights/amr/2021/connected-health-fresenius-medical-care/ (accessed on 26 September 2022).
- U.S. Department of Veterans Affairs National Center for Veterans Analysis and Statistics. Available online: https://www.va.gov/vetdata/veteran_population.asp (accessed on 8 March 2022).
- USRDS. USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; USRDS: Bethesda, MD, USA, 2021. [Google Scholar]
- Watnick, S.; Crowley, S.T. ESRD Care Within the US Department of Veterans Affairs: A Forward-Looking Program With an Illuminating Past. Am. J. Kidney Dis. 2014, 63, 521–529. [Google Scholar] [CrossRef]
- Kummer, S.; von Gersdorff, G.; Kemper, M.J.; Oh, J. The Influence of Gender and Sexual Hormones on Incidence and Outcome of Chronic Kidney Disease. Pediatr. Nephrol. 2012, 27, 1213–1219. [Google Scholar] [CrossRef]
- Klag, M.J.; Whelton, P.K.; Randall, B.L.; Neaton, J.D.; Brancati, F.L.; Stamler, J. End-Stage Renal Disease in African-American and White Men: 16-Year MRFIT Findings. JAMA 1997, 277, 1293–1298. [Google Scholar] [CrossRef] [PubMed]
- McCullough, K.P.; Morgenstern, H.; Saran, R.; Herman, W.H.; Robinson, B.M. Projecting ESRD Incidence and Prevalence in the United States through 2030. J. Am. Soc. Nephrol. 2019, 30, 127–135. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).