Prediagnosis of Heart Failure (HF) Using Deep Learning and the Korotkoff Sound
Abstract
:1. Introduction
- An innovative method for the prediagnosis of HF based on KS and DL networks has been proposed, analyzed, and validated in four types of DL networks.
- The impact of signal segmentation and feature extraction methods on KS-based HF prediagnosis is thoroughly investigated in this paper.
- The pre-trained neural network model is transferred to the KS-based HF prediagnosis task, which improved the model’s training efficiency and ensured the reliability of this paper’s conclusion.
2. Related Works
3. Materials and Methods
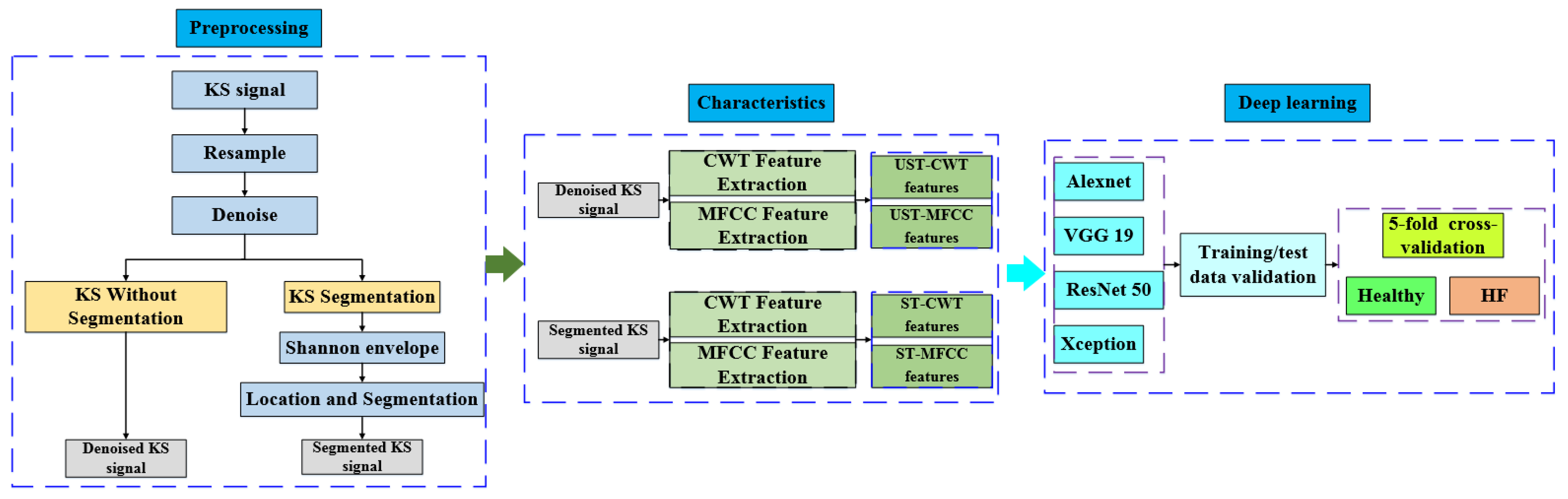
3.1. System Overview
3.2. Database Acquisition
3.3. Data Processing
3.3.1. Wiener Filtering
3.3.2. Shannon Envelope
3.3.3. Location and Segmentation
3.4. Feature Graph Generation
3.4.1. CWT Time-Frequency Characteristics
3.4.2. Mel Frequency Cepstrum Coefficient
3.5. Deep Learning (DL) Network
3.5.1. AlexNet
3.5.2. VGG19
3.5.3. ResNet
3.5.4. Xception
3.5.5. Data Augmentation
3.5.6. Transfer Learning
3.6. Evaluation Metrics
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Statistics. 2022. Available online: https://www.who.int/data/gho/publications/world-health-statistics (accessed on 20 May 2022).
- Bennett, J.E.; Kontis, V.; Mathers, C.D.; Guillot, M.; Rehm, J.; Chalkidou, K.; Kengne, A.P.; Carrillo-Larco, R.M.; Bawah, A.A.; Dain, K.; et al. NCD Countdown 2030: Pathways to achieving Sustainable Development Goal target 3.4. Lancet 2020, 396, 918–934. [Google Scholar] [CrossRef]
- Ohta, Y.; Kitao, S.; Yunaga, H.; Fujii, S.; Mukai, N.; Yamamoto, K.; Ogawa, T. Myocardial delayed enhancement CT for the evaluation of heart failure: Comparison to MRI. Radiology 2018, 288, 682–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanna, G.D.; Canonico, M.E.; Santoro, C.; Esposito, R.; Masia, S.L.; Galderisi, M.; Parodi, G.; Nihoyannopoulos, P. Echocardiographic longitudinal strain analysis in heart failure: Real usefulness for clinical management beyond diagnostic value and prognostic correlations? A comprehensive review. Curr. Heart Fail. Rep. 2021, 18, 290–303. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M.; Sanchis-Gomar, F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur. J. Prev. Cardiol. 2020, 27, 906–908. [Google Scholar] [CrossRef]
- Eeftinck Schattenkerk, D.W.; Van Lieshout, J.J.; Van Den Meiracker, A.H.; Wesseling, K.R.; Blanc, S.; Wieling, W.; Van Montfrans, G.A.; Settels, J.J.; Wesseling, K.H.; Westerhof, B.E.; et al. Nexfin noninvasive continuous blood pressure validated against Riva-Rocci/Korotkoff. Am. J. Hypertens. 2009, 22, 378–383. [Google Scholar] [CrossRef] [Green Version]
- Padwal, R.; Campbell, N.R.; Schutte, A.E.; Olsen, M.H.; Delles, C.; Etyang, A.; Cruickshank, J.K.; Stergiou, G.; Rakotz, M.K.; Wozniak, G.; et al. Optimizing observer performance of clinic blood pressure measurement: A position statement from the Lancet Commission on Hypertension Group. J. Hypertens. 2019, 37, 1737. [Google Scholar] [CrossRef]
- Gosse, P.; Durandet, P.; Roudaut, R. The QKD interval as an easy assessment of pulse wave velocity: Validation of the method. J. Hypertens. 1991, 9, S447. [Google Scholar]
- Takahashi, O.; Shimbo, T.; Rahman, M.; Musa, R.; Kurokawa, W.; Yoshinaka, T.; Fukui, T. Validation of the auscultatory method for diagnosing peripheral arterial disease. Fam. Pract. 2006, 23, 10–14. [Google Scholar] [CrossRef]
- Hussain, L.; Awan, I.A.; Aziz, W.; Saeed, S.; Ali, A.; Zeeshan, F.; Kwak, K.S. Detecting congestive heart failure by extracting multimodal features and employing machine learning techniques. BioMed Res. Int. 2020, 2020, 4281243. [Google Scholar] [CrossRef]
- Kabir, M.A.; Shahnaz, C. Denoising of ECG signals based on noise reduction algorithms in EMD and wavelet domains. Biomed. Signal Process. Control 2012, 7, 481–489. [Google Scholar] [CrossRef]
- Misal, A.; Sinha, G.R. Denoising of PCG signal by using wavelet transforms. Adv. Comput. Res. 2012, 4, 46–49. [Google Scholar]
- Liang, H.; Lukkarinen, S.; Hartimo, I. Heart sound segmentation algorithm based on heart sound envelogram. In Proceedings of the Computers in Cardiology 1997, Lund, Sweden, 7–10 September 1997; IEEE: Piscataway, NJ, USA, 1997; pp. 105–108. [Google Scholar]
- Springer, D.B.; Tarassenko, L.; Clifford, G.D. Logistic regression-HSMM-based heart sound segmentation. IEEE Trans. Biomed. Eng. 2015, 63, 822–832. [Google Scholar] [CrossRef]
- Papadaniil, C.D.; Hadjileontiadis, L. Efficient heart sound segmentation and extraction using ensemble empirical mode decomposition and kurtosis features. IEEE J. Biomed. Health Inform. 2013, 18, 1138–1152. [Google Scholar] [CrossRef]
- Chen, W.; Sun, Q.; Chen, X.; Xie, G.; Wu, H.; Xu, C. Deep learning methods for heart sounds classification: A systematic review. Entropy 2021, 23, 667. [Google Scholar] [CrossRef]
- Khare, S.K.; Bajaj, V. Time–frequency representation and convolutional neural network-based emotion recognition. IEEE Trans. Neural Netw. Learn. Syst. 2020, 32, 2901–2909. [Google Scholar] [CrossRef]
- Arias-Vergara, T.; Klumpp, P.; Vasquez-Correa, J.C.; Nöth, E.; Orozco-Arroyave, J.R.; Schuster, M. Multi-channel spectrograms for speech processing applications using deep learning methods. Pattern Anal. Appl. 2021, 24, 423–431. [Google Scholar] [CrossRef]
- El-Segaier, M.; Lilja, O.; Lukkarinen, S.; Sörnmo, L.; Sepponen, R.; Pesonen, E. Computer-based detection and analysis of heart sound and murmur. Ann. Biomed. Eng. 2005, 33, 937–942. [Google Scholar] [CrossRef]
- Varghees, V.N.; Ramachandran, K.I. A novel heart sound activity detection framework for automated heart sound analysis. Biomed. Signal Process. Control 2014, 13, 174–188. [Google Scholar] [CrossRef]
- Acharya, U.R.; Fujita, H.; Adam, M.; Lih, O.S.; Sudarshan, V.K.; Hong, T.J.; Koh, J.E.W.; Hagiwara, Y.; Chua, C.K.; Poo, C.K.; et al. Automated characterization and classification of coronary artery disease and myocardial infarction by decomposition of ECG signals: A comparative study. Inf. Sci. 2017, 377, 17–29. [Google Scholar] [CrossRef]
- Narin, A.; Isler, Y.; Ozer, M. Investigating the performance improvement of HRV Indices in CHF using feature selection methods based on backward elimination and statistical significance. Comput. Biol. Med. 2014, 45, 72–79. [Google Scholar] [CrossRef]
- Watrous, R.L. Computer-aided auscultation of the heart: From anatomy and physiology to diagnostic decision support. In Proceedings of the 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006; IEEE: Piscataway, NJ, USA, 2006; pp. 140–143. [Google Scholar]
- Shuvo, S.B.; Ali, S.N.; Swapnil, S.I.; Al-Rakhami, M.S.; Gumaei, A. CardioXNet: A novel lightweight deep learning framework for cardiovascular disease classification using heart sound recordings. IEEE Access 2021, 9, 36955–36967. [Google Scholar] [CrossRef]
- Son, G.Y.; Kwon, S. Classification of heart sound signal using multiple features. Appl. Sci. 2018, 8, 2344. [Google Scholar]
- Jin, K.; Neubeck, L.; Koo, F.; Ding, D.; Gullick, J. Understanding prevention and management of coronary heart disease among Chinese immigrants and their family carers: A socioecological approach. J. Transcult. Nurs. 2020, 31, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Benmira, A.; Perez-Martin, A.; Schuster, I.; Veye, F.; Triboulet, J.; Berron, N.; Aichoun, I.; Coudray, S.; Laurent, J.; Bereksi-Reguig, F.; et al. An ultrasound look at Korotkoff sounds: The role of pulse wave velocity and flow turbulence. Blood Press. Monit. 2017, 22, 86–94. [Google Scholar] [CrossRef]
- Mondal, A.; Saxena, I.; Tang, H.; Banerjee, P. A noise reduction technique based on nonlinear kernel function for heart sound analysis. IEEE J. Biomed. Health Inform. 2017, 22, 775–784. [Google Scholar] [CrossRef]
- Deng, S.W.; Han, J.Q. Adaptive overlapping-group sparse denoising for heart sound signals. Biomed. Signal Process. Control 2018, 40, 49–57. [Google Scholar] [CrossRef]
- Lopac, N.; Hržić, F.; Vuksanović, I.P.; Lerga, J. Detection of Non-Stationary GW Signals in High Noise From Cohen’s Class of Time–Frequency Representations Using Deep Learning. IEEE Access 2021, 10, 2408–2428. [Google Scholar] [CrossRef]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef]
- Noman, F.; Salleh, S.H.; Ting, C.M.; Samdin, S.B.; Ombao, H.; Hussain, H. A Markov-switching model approach to heart sound segmentation and classification. IEEE J. Biomed. Health Inform. 2019, 24, 705–716. [Google Scholar] [CrossRef] [Green Version]
- Nogueira, D.M.; Ferreira, C.A.; Gomes, E.F.; Jorge, A. Classifying heart sounds using images of motifs, MFCC and temporal features. J. Med. Syst. 2019, 43, 1–13. [Google Scholar] [CrossRef]
- Potes, C.; Parvaneh, S.; Rahman, A.; Rahman, B. Ensemble of feature-based and deep learning-based classifiers for detection of abnormal heart sounds. In Proceedings of the 2016 Computing in Cardiology Conference (CinC), Vancouver, BC, Canada, 11–14 September 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 621–624. [Google Scholar]
- Rubin, J.; Abreu, R.; Ganguli, A.; Nelaturi, S.; Matei, I.; Sricharan, K. Classifying heart sound recordings using deep convolutional neural networks and mel-frequency cepstral coefficients. In Proceedings of the 2016 Computing in Cardiology Conference (CinC), Vancouver, BC, Canada, 11–14 September 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 813–816. [Google Scholar]
- Zhang, W.; Han, J.; Deng, S. Abnormal heart sound detection using temporal quasi-periodic features and long short-term memory without segmentation. Biomed. Signal Process. Control 2019, 53, 101560. [Google Scholar] [CrossRef]
- He, Y.; Li, W.; Zhang, W.; Zhang, S.; Pi, X.; Liu, H. Research on segmentation and classification of heart sound signals based on deep learning. Appl. Sci. 2021, 11, 651. [Google Scholar] [CrossRef]
- Gjoreski, M.; Gradišek, A.; Budna, B.; Gams, M.; Poglajen, G. Machine learning and end-to-end deep learning for the detection of chronic heart failure from heart sounds. IEEE Access 2020, 8, 20313–20324. [Google Scholar] [CrossRef]
- Gosse, P.; Guillo, P.; Ascher, G.; Clementy, J. Assessment of arterial distensibility by monitoring the timing of Korotkoff sounds. Am. J. Hypertens. 1994, 7, 228–233. [Google Scholar] [CrossRef]
- Constans, J.; Germain, C.; Gosse, P.; Taillard, J.; Tiev, K.; Delevaux, I.; Mouthon, L.; Schmidt, C.; Granel, F.; Soria, P.; et al. Arterial stiffness predicts severe progression in systemic sclerosis: The ERAMS study. J. Hypertens. 2007, 25, 1900–1906. [Google Scholar] [CrossRef]
- Gosse, P.; Cremer, A.; Papaioannou, G.; Yeim, S. Arterial stiffness from monitoring of timing of Korotkoff sounds predicts the occurrence of cardiovascular events independently of left ventricular mass in hypertensive patients. Hypertension 2013, 62, 161–167. [Google Scholar] [CrossRef] [Green Version]
- El Tahlawi, M.; Abdelbaset, M.; Gouda, M.; Hussein, I. Can we predict the presence of coronary lesions from blood pressure measurement? A new clinical method. Hypertens. Res. 2015, 38, 260–263. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, T.; Miura, S.; Suematsu, Y.; Kuwano, T.; Sugihara, M.; Ike, A.; Iwata, A.; Nishikawa, H.; Saku, K. A relative difference in systolic blood pressure between arms by synchronal measurement and conventional cardiovascular risk factors are associated with the severity of coronary atherosclerosis. Heart Vessel. 2016, 31, 863–870. [Google Scholar] [CrossRef]
- Jia, S.; Wu, Y.; Wang, W.; Lin, W.; Chen, Y.; Zhang, H.; Xia, S.; Zhou, H. An Exploratory Study on the Relationship between Brachial Arterial Blood Flow and Cardiac Output. J. Healthc. Eng. 2021, 2021, 1251199. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar]
- Suzuki, K.; Washio, T.; Tsukamoto, S.; Kato, K.; Iwamoto, E.; Ogoh, S. Habitual cigarette smoking attenuates shear-mediated dilation in the brachial artery but not in the carotid artery in young adults. Physiol. Rep. 2020, 8, e14369. [Google Scholar] [CrossRef] [Green Version]
- Yao, G.H.; Deng, Y.; Liu, Y.; Xu, M.J.; Zhang, C.; Deng, Y.B.; Ren, W.D.; Li, Z.A.; Tang, H.; Zhang, Q.B.; et al. Echocardiographic measurements in normal Chinese adults focusing on cardiac chambers and great arteries: A prospective, nationwide, and multicenter study. J. Am. Soc. Echocardiogr. 2015, 28, 570–579. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Pan, F.; Zheng, D.; He, P.; Murray, A. Does the position or contact pressure of the stethoscope make any difference to clinical blood pressure measurements: An observational study. Medicine 2014, 93, e301. [Google Scholar] [CrossRef]
- Pan, F.; Chen, F.; Liu, C.; Yang, Z.; Liu, Z.; Zheng, D. Quantitative Comparison of Korotkoff Sound Waveform Characteristics: Effects of Static Cuff Pressures and Stethoscope Positions. Ann. Biomed. Eng. 2018, 46, 1736–1744. [Google Scholar] [CrossRef] [Green Version]
- Saini, M. Proposed algorithm for implementation of Shannon energy envelope for heart sound analysis. Int. J. Electron. Commun. Technol. 2016, 7, 15–19. [Google Scholar]
- Giordano, N.; Knaflitz, M. A novel method for measuring the timing of heart sound components through digital phonocardiography. Sensors 2019, 19, 1868. [Google Scholar] [CrossRef] [Green Version]
- Rajani Kumari, L.V.; Padma Sai, Y.; Balaji, N. R-peak identification in ECG signals using pattern-adapted wavelet technique. IETE J. Res. 2021, 1–10. [Google Scholar] [CrossRef]
- Rajput, J.S.; Sharma, M.; Kumar, T.S.; Acharya, U.R. Automated Detection of Hypertension Using Continuous Wavelet Transform and a Deep Neural Network with Ballistocardiography Signals. Int. J. Environ. Res. Public Health 2022, 19, 4014. [Google Scholar] [CrossRef]
- Sharma, M.; Dhiman, H.S.; Acharya, U.R. Automatic identification of insomnia using optimal antisymmetric biorthogonal wavelet filter bank with ECG signals. Comput. Biol. Med. 2021, 131, 104246. [Google Scholar] [CrossRef]
- Lalitha, S.; Geyasruti, D.; Narayanan, R.; Shravani, M. Emotion detection using MFCC and cepstrum features. Procedia Comput. Sci. 2015, 70, 29–35. [Google Scholar] [CrossRef] [Green Version]
- Tiwari, V. MFCC and its applications in speaker recognition. Int. J. Emerg. Technol. 2010, 1, 19–22. [Google Scholar]
- Astuti, W.; Sediono, W.; Aibinu, A.M.; Akmeliawati, R.; Salami, M.J.E. Adaptive Short Time Fourier Transform (STFT) Analysis of seismic electric signal (SES): A comparison of Hamming and rectangular window. In Proceedings of the 2012 IEEE Symposium on Industrial Electronics and Applications, Bandung, Indonesia, 23–26 September 2012; IEEE: Piscataway, NJ, USA, 2012; pp. 372–377. [Google Scholar]
- Hinton, G.E.; Salakhutdinov, R.R. Reducing the dimensionality of data with neural networks. Science 2006, 313, 504–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. Imagenet classification with deep convolutional neural networks. Commun. ACM 2017, 60, 84–90. [Google Scholar] [CrossRef] [Green Version]
- Bansal, M.; Kumar, M.; Sachdeva, M.; Mittal, A. Transfer learning for image classification using VGG19: Caltech-101 image data set. J. Ambient Intell. Humaniz. Comput. 2021, 1–12. [Google Scholar] [CrossRef]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep residual learning for image recognition. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778. [Google Scholar]
- Chollet, F. Xception: Deep learning with depthwise separable convolutions. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Honolulu, HI, USA, 21–26 July 2017; pp. 1251–1258. [Google Scholar]
- Touvron, H.; Cord, M.; Douze, M.; Massa, F.; Sablayrolles, A.; Jégou, H. Training data-efficient image transformers & distillation through attention. In Proceedings of the International Conference on Machine Learning, PMLR 2021, Virtual Event, 18–24 July 2021; pp. 10347–10357. [Google Scholar]
- Gajendran, M.K.; Khan, M.Z.; Khattak MA, K. ECG Classification using Deep Transfer Learning. In Proceedings of the 2021 4th International Conference on Information and Computer Technologies (ICICT), Kahului, HI, USA, 11–14 March 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 1–5. [Google Scholar]
- Olivas, E.S.; Guerrero JD, M.; Martinez-Sober, M.; Magdalena-Benedito, J.R.; Serrano, L. (Eds.) Handbook of Research on Machine Learning Applications and Trends: Algorithms, Methods, and Techniques: Algorithms, Methods, and Techniques; IGI Global: Hershey, PA, USA, 2009. [Google Scholar]
- Zheng, Y.; Guo, X.; Qin, J.; Xiao, S. Computer-assisted diagnosis for chronic heart failure by the analysis of their cardiac reserve and heart sound characteristics. Comput. Methods Programs Biomed. 2015, 122, 372–383. [Google Scholar] [CrossRef]
- Yang, Y.; Guo, X.M.; Wang, H.; Zheng, Y.N. Deep Learning-Based Heart Sound Analysis for Left Ventricular Diastolic Dysfunction Diagnosis. Diagnostics 2021, 11, 2349. [Google Scholar] [CrossRef]
- Zheng, Y.; Guo, X.; Wang, Y.; Qin, J.; Lv, F. A multi-scale and multi-domain heart sound feature-based machine learning model for ACC/AHA heart failure stage classification. Physiol. Meas. 2022, 43, 065002. [Google Scholar] [CrossRef]








| Subjects | Female Ratio % | Ages Years | BMI Kg/m2 | LVEF % | SBP mm Hg | DBP mm Hg | NT-proBNP pg/mL | Numbers - |
|---|---|---|---|---|---|---|---|---|
| Healthy | 50 | 42 ± 22 | 24.8 ± 2.1 | 65 ± 7.5 | 111 ± 15 | 73 ± 10 | 513~11,950 | 116 |
| HF patients | 40 | 61 ± 17 | 24.5 ± 3.2 | 40 ± 6.83 | 129 ± 35 | 77 ± 20 | <125 | 249 |
| Classifier | Acc (%) | Se (%) | Sp (%) | AUC | Tc (min) |
|---|---|---|---|---|---|
| AlexNet | 87.0 | 91.8 | 80.2 | 0.947 | 3 |
| VGG19 | 89.0 | 91.5 | 85.5 | 0.965 | 9 |
| ResNet50 | 89.8 | 91.1 | 87.9 | 0.962 | 6 |
| Xception | 93.4 | 94.3 | 92.2 | 0.979 | 55 |
| Classifier | Acc (%) | Se (%) | Sp (%) | AUC | Tc (min) |
|---|---|---|---|---|---|
| AlexNet | 90.4 | 94.4 | 84.8 | 0.951 | 3 |
| VGG19 | 93.0 | 94.8 | 90.5 | 0.976 | 9 |
| ResNet50 | 95.0 | 91.1 | 97.7 | 0.983 | 6 |
| Xception | 95.0 | 98.6 | 89.9 | 0.988 | 55 |
| Classifier | Acc (%) | Se (%) | Sp (%) | AUC | Tc (min) |
|---|---|---|---|---|---|
| AlexNet | 90.9 | 94.9 | 85.2 | 0.966 | 3 |
| VGG19 | 91.1 | 96.4 | 83.6 | 0.968 | 9 |
| ResNet50 | 92.2 | 90.5 | 93.4 | 0.974 | 6 |
| Xception | 94.3 | 95.7 | 92.4 | 0.979 | 55 |
| Classifier | Acc (%) | Se (%) | Sp (%) | AUC | Tc (min) |
|---|---|---|---|---|---|
| AlexNet | 89.3 | 93.9 | 82.8 | 0.956 | 3 |
| VGG19 | 93.0 | 97.5 | 86.5 | 0.979 | 9 |
| ResNet50 | 95.4 | 92.0 | 97.8 | 0.988 | 6 |
| Xception | 96.0 | 97.5 | 93.8 | 0.989 | 55 |
| Authors | Data Set | Number of Subjects | Method | Performance |
|---|---|---|---|---|
| Zheng et al. (2015) [67] | Collected by HS acquisition system | 88 healthy volunteers and 64 CHF patients | LS-SVM | Acc 95.39% Se 96.59% Sp 93.75% |
| Potes et al. (2016) [34] | Physionet databases | 2575 normal signals and 665 abnormal signals | AdaBoost and CNN | Acc 86.0% Se 94.2% Sp 77.8% |
| Gjoreski et al. (2020) [38] | six (A to F) PhysioNet Challenge datasets & measured HS by digital stethoscope | 3153 signals from PhysioNet Challenge datasets and 110 healthy people, 51 CHF recorded by digital stethoscope | Machine-Learning and end-to-end DeepLearning | Acc 92.9% Se 82.3% Sp 96.2% |
| Yang et al. (2021) [68] | Acquired from the First Affiliated Hospital of Chongqing Medical University | 41 healthy volunteers and 30 left ventricular diastolic dysfunction patients | VGG-16, VGG-19, ResNet-18, ResNet-50, DenseNet-121, and AlexNet | Acc 98.7% Se 98.6% Sp 98.8% |
| Zheng et al. (2022) [69] | Dataset from First Affiliated Hospital and the University-Town Hospital of Chongqing Medical University | 51 healthy volunteers and 224 CHF patients | LS-SVM | Acc 82% Se 82.1% Sp 95.5% |
| Our method | Dataset of measured KS from the Fourth People’s Hospital of Zhejiang University | 116 healthy subjects and 249 CHF patients | DeepLearning(DL) | Acc 96.0% Se 97.5% Sp 93.8% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, H.; Wang, R.; Zhou, H.; Xia, S.; Jia, S.; Wu, Y. Prediagnosis of Heart Failure (HF) Using Deep Learning and the Korotkoff Sound. Appl. Sci. 2022, 12, 10322. https://doi.org/10.3390/app122010322
Zhang H, Wang R, Zhou H, Xia S, Jia S, Wu Y. Prediagnosis of Heart Failure (HF) Using Deep Learning and the Korotkoff Sound. Applied Sciences. 2022; 12(20):10322. https://doi.org/10.3390/app122010322
Chicago/Turabian StyleZhang, Huanyu, Ruwei Wang, Hong Zhou, Shudong Xia, Sixiang Jia, and Yiteng Wu. 2022. "Prediagnosis of Heart Failure (HF) Using Deep Learning and the Korotkoff Sound" Applied Sciences 12, no. 20: 10322. https://doi.org/10.3390/app122010322
APA StyleZhang, H., Wang, R., Zhou, H., Xia, S., Jia, S., & Wu, Y. (2022). Prediagnosis of Heart Failure (HF) Using Deep Learning and the Korotkoff Sound. Applied Sciences, 12(20), 10322. https://doi.org/10.3390/app122010322







