Effects of Mini-Implant-Assisted Rapid Palatal Expansion on Incisive Canal Morphology and Tooth–Canal Relationship
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
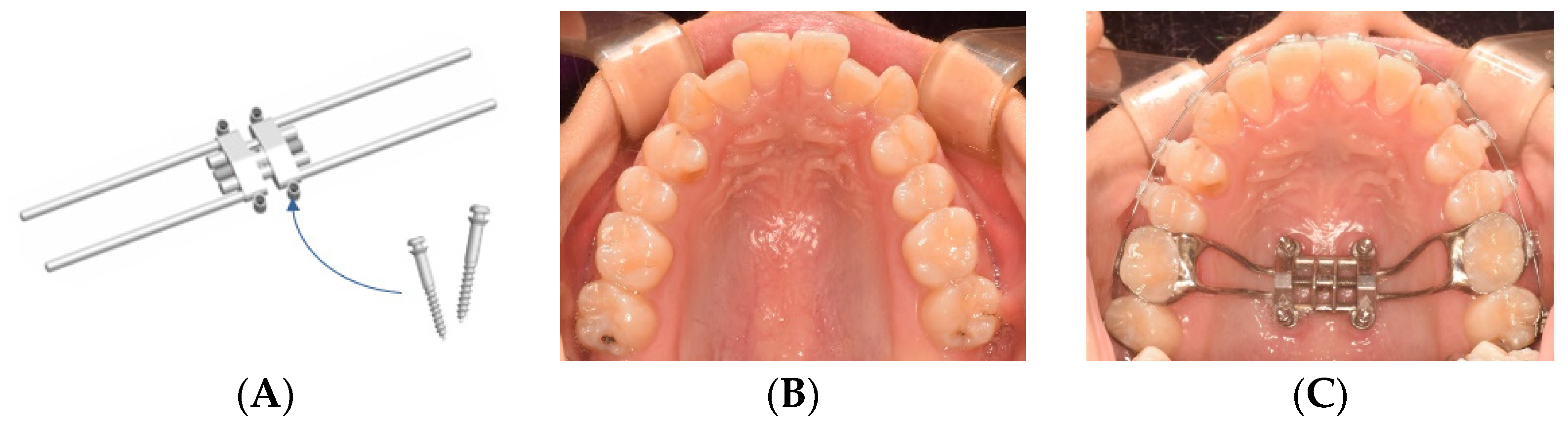
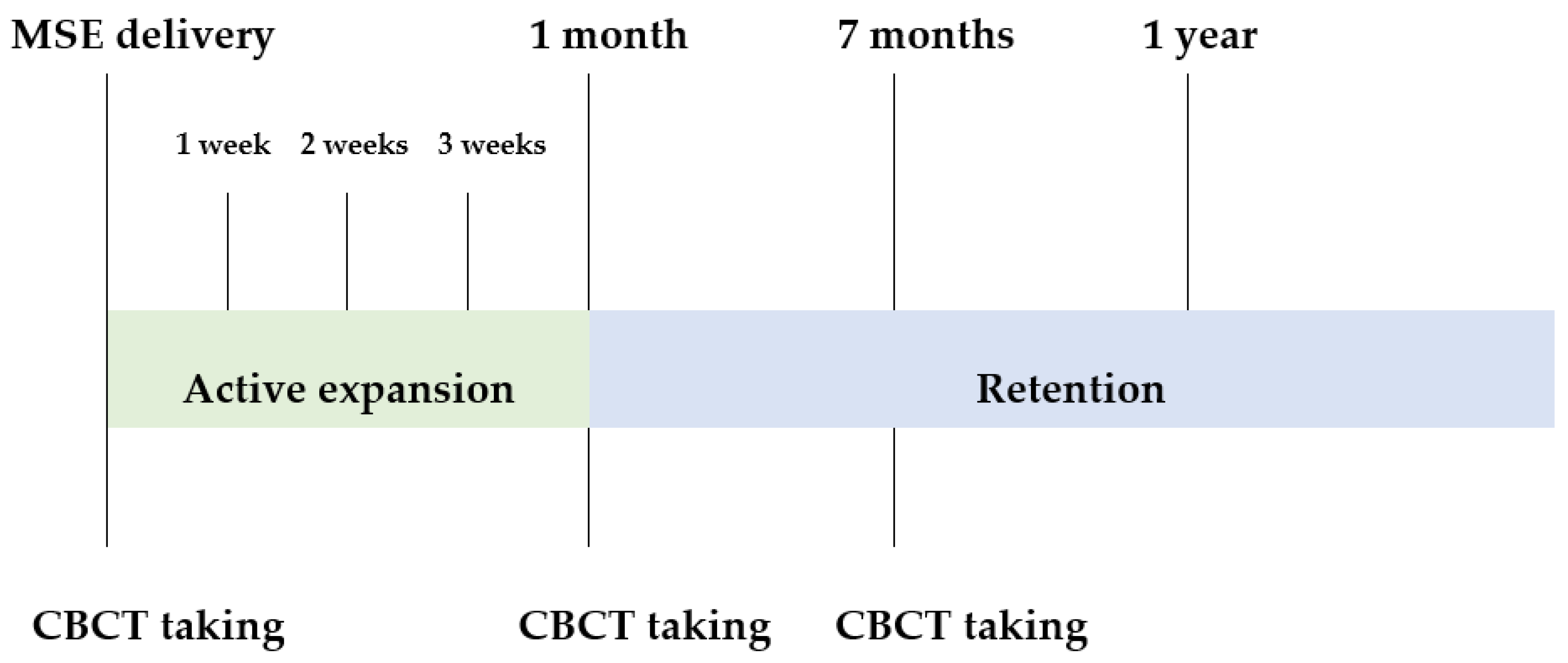
2.2. Materials and Treatment Protocol
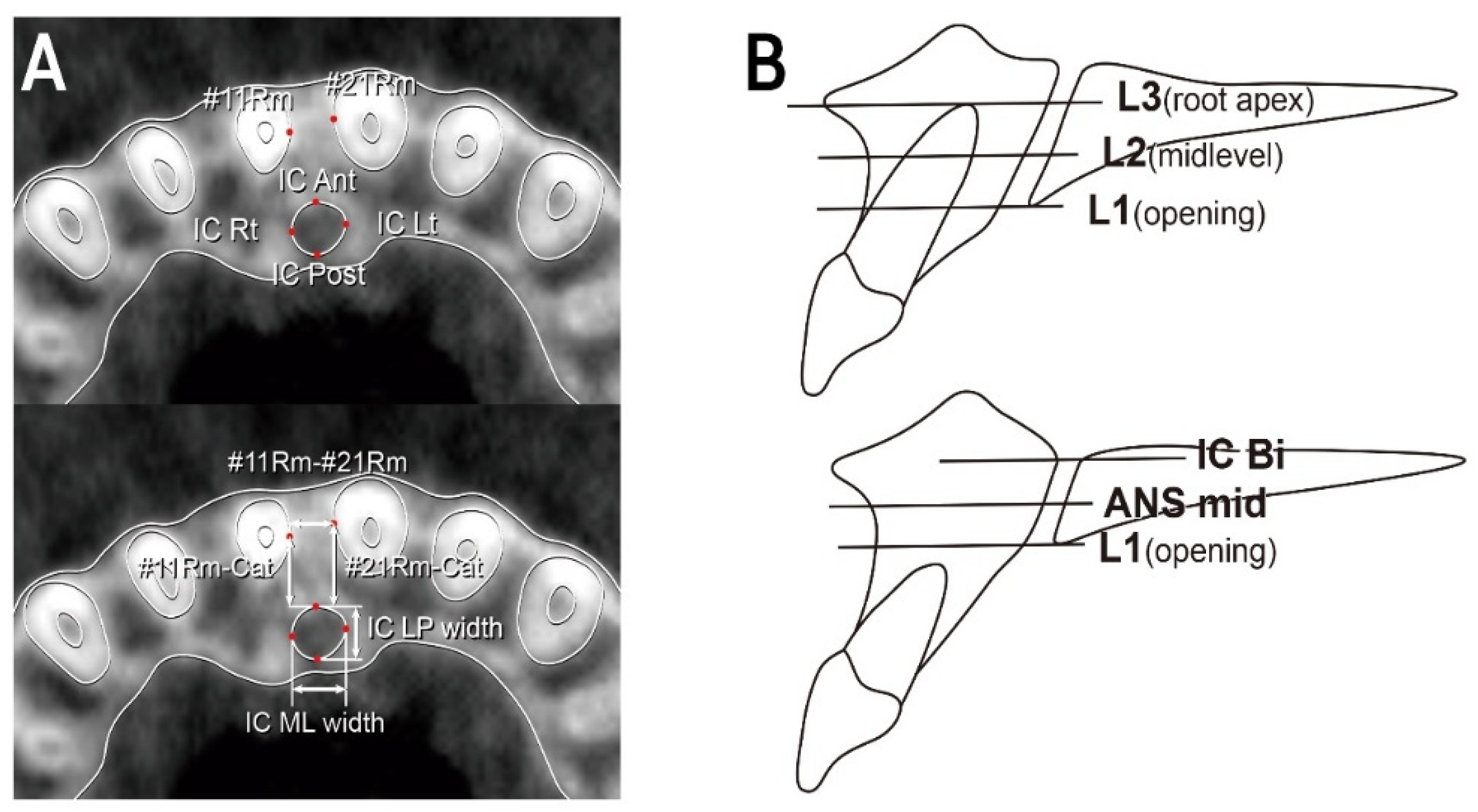
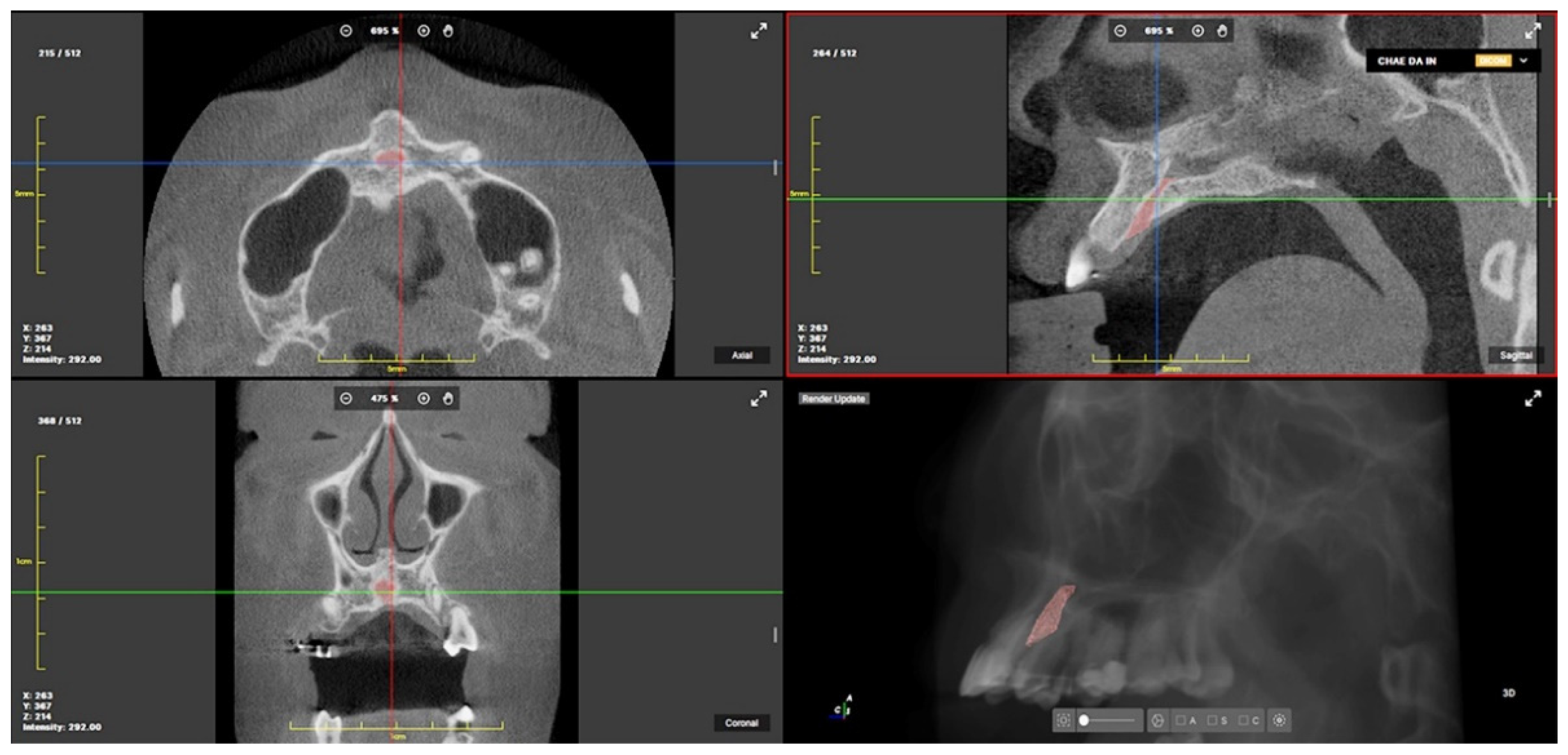
2.3. CBCT Landmarks, Reference Planes and Measurements
2.4. Statistical Evaluation
3. Results
3.1. Changes in IC Dimensions and Tooth–Canal Relationship before and after MARPE Treatment
3.2. Change in the Positional Relationship between the Maxillary Central Incisors after MARPE Treatment (Table 4)
| Measurements | T0 | T1 | p Value |
|---|---|---|---|
| #11Cr-#21Cr (n = 30) | 9.74 ± 1.44 | 9.43 ± 0.80 | 0.258 |
| #11Rm-#21Rm(L1) (n = 20) | 2.88 ± 1.06 | 4.86 ± 1.84 | 0.000 *** |
| #11Rm-#21Rm(L2) (n = 20) | 3.25 ± 1.15 | 5.44 ± 1.75 | 0.000 *** |
| #11Rm-#21Rm(L3) (n = 20) | 3.95 ± 1.12 | 5.84 ± 1.66 | 0.000 *** |
| #11Rt-#21Rt (n = 30) | 7.17 ± 1.55 | 8.94 ± 1.68 | 0.000 *** |
3.3. Volume Change in the IC after MARPE Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bennardo, F.; Barone, S.; Vocaturo, C.; Nucci, L.; Antonelli, A.; Giudice, A. Usefulness of Magnetic Mallet in Oral Surgery and Implantology: A Systematic Review. J. Pers. Med. 2022, 12, 108. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A. Maxillary Transverse Deficiency. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2000, 117, 567–570. [Google Scholar] [CrossRef]
- Vandersea, B.A.; Ruvo, A.T.; Frost, D.E. Maxillary Transverse Deficiency–Surgical Alternatives to Management. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 351–368. [Google Scholar] [CrossRef] [PubMed]
- Haas, A.J. Rapid Expansion of the Maxillary Dental Arch and Nasal Cavity by Opening the Midpalatal Suture. Angle Orthod. 1961, 31, 73–90. [Google Scholar] [CrossRef]
- Haas, A.J. The Treatment of Maxillary Deficiency by Opening the Midpalatal Suture. Angle Orthod. 1965, 35, 200–217. [Google Scholar] [CrossRef]
- Sandikçiolu, M.; Hazar, S. Skeletal and Dental Changes after Maxillary Expansion in the Mixed Dentition. Am. J. Orthod. Dentofacial Orthop. 1997, 111, 321–327. [Google Scholar] [CrossRef]
- Liu, S.; Xu, T.; Zou, W. Effects of Rapid Maxillary Expansion on the Midpalatal Suture: A Systematic Review. Eur. J. Orthod. 2015, 37, 651–655. [Google Scholar] [CrossRef] [Green Version]
- Christie, K.F.; Boucher, N.; Chung, C.-H. Effects of Bonded Rapid Palatal Expansion on the Transverse Dimensions of the Maxilla: A Cone-Beam Computed Tomography Study. Am. J. Orthod. Dentofac. Orthop. 2010, 137 (Suppl. S4), S79–S85. [Google Scholar] [CrossRef]
- Baysal, A.; Karadede, I.; Hekimoglu, S.; Ucar, F.; Ozer, T.; Veli, I.; Uysal, T. Evaluation of Root Resorption Following Rapid Maxillary Expansion Using Cone-Beam Computed Tomography. Angle Orthod. 2012, 82, 488–494. [Google Scholar] [CrossRef] [Green Version]
- Garib, D.G.; Henriques, J.F.C.; Janson, G.; de Freitas, M.R.; Fernandes, A.Y. Periodontal Effects of Rapid Maxillary Expansion with Tooth-Tissue-Borne and Tooth-Borne Expanders: A Computed Tomography Evaluation. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2006, 129, 749–758. [Google Scholar] [CrossRef]
- Suri, L.; Taneja, P. Surgically Assisted Rapid Palatal Expansion: A Literature Review. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 290–302. [Google Scholar] [CrossRef]
- Wilmes, B.; Nienkemper, M.; Drescher, D. Application and Effectiveness of a Mini-Implant-and Tooth-Borne Rapid Palatal Expansion Device: The Hybrid Hyrax. World J. Orthod. 2010, 11, 323–330. [Google Scholar]
- Carlson, C.; Sung, J.; McComb, R.W.; Machado, A.W.; Moon, W. Microimplant-Assisted Rapid Palatal Expansion Appliance to Orthopedically Correct Transverse Maxillary Deficiency in an Adult. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 716–728. [Google Scholar] [CrossRef] [PubMed]
- Brunetto, D.P.; Sant’Anna, E.F.; Machado, A.W.; Moon, W. Non-Surgical Treatment of Transverse Deficiency in Adults Using Microimplant-Assisted Rapid Palatal Expansion (MARPE). Dent. Press J. Orthod. 2017, 22, 110–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.J.; Park, Y.-C.; Lee, K.-J.; Cha, J.-Y.; Tahk, J.H.; Choi, Y.J. Skeletal and Dentoalveolar Changes after Miniscrew-Assisted Rapid Palatal Expansion in Young Adults: A Cone-Beam Computed Tomography Study. Korean J. Orthod. 2017, 47, 77–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, H.-M.; Park, Y.-C.; Lee, K.-J.; Kim, K.-H.; Choi, Y.J. Stability of Dental, Alveolar, and Skeletal Changes after Miniscrew-Assisted Rapid Palatal Expansion. Korean J. Orthod. 2017, 47, 313–322. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.-J.; Park, Y.-C.; Park, J.-Y.; Hwang, W.-S. Miniscrew-Assisted Nonsurgical Palatal Expansion before Orthognathic Surgery for a Patient with Severe Mandibular Prognathism. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 830–839. [Google Scholar] [CrossRef]
- Lee, D.-W.; Park, J.H.; Moon, W.; Seo, H.Y.; Chae, J.-M. Effects of Bicortical Anchorage on Pterygopalatine Suture Opening with Microimplant-Assisted Maxillary Skeletal Expansion. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 502–511. [Google Scholar] [CrossRef]
- Cunha, A.C.; da Lee, H.; Nojima, L.I.; da C. G. Nojima, M.; Lee, K.-J. Miniscrew-Assisted Rapid Palatal Expansion for Managing Arch Perimeter in an Adult Patient. Dent. Press J. Orthod. 2017, 22, 97–108. [Google Scholar] [CrossRef]
- Chung, C.J.; Choi, Y.J.; Kim, K.-H. Approximation and Contact of the Maxillary Central Incisor Roots with the Incisive Canal after Maximum Retraction with Temporary Anchorage Devices: Report of 2 Patients. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 493–502. [Google Scholar] [CrossRef] [Green Version]
- Chung, C.J.; Nguyen, T.; Lee, J.-H.; Kim, K.-H. Incisive Canal Remodelling Following Maximum Anterior Retraction Reduces Apical Root Resorption. Orthod. Craniofac. Res. 2021, 24 (Suppl. S1), 59–65. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.-A.; Kim, S.-J.; Choi, Y.J.; Kim, K.-H.; Chung, C.J. Morphologic Evaluation of the Incisive Canal and Its Proximity to the Maxillary Central Incisors Using Computed Tomography Images. Angle Orthod. 2016, 86, 571–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mraiwa, N.; Jacobs, R.; Van Cleynenbreugel, J.; Sanderink, G.; Schutyser, F.; Suetens, P.; van Steenberghe, D.; Quirynen, M. The Nasopalatine Canal Revisited Using 2D and 3D CT Imaging. Dentomaxillofac. Radiol. 2004, 33, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Jacobs, R.; Martens, W.; Hu, Y.; Adriaensens, P.; Quirynen, M.; Lambrichts, I. Macro- and Micro-Anatomical, Histological and Computed Tomography Scan Characterization of the Nasopalatine Canal. J. Clin. Periodontol. 2009, 36, 598–603. [Google Scholar] [CrossRef] [Green Version]
- Song, W.-C.; Jo, D.-I.; Lee, J.-Y.; Kim, J.-N.; Hur, M.-S.; Hu, K.-S.; Kim, H.-J.; Shin, C.; Koh, K.-S. Microanatomy of the Incisive Canal Using Three-Dimensional Reconstruction of MicroCT Images: An Ex Vivo Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 108, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Zong, C.; Tang, B.; Hua, F.; He, H.; Ngan, P. Skeletal and Dentoalveolar Changes in the Transverse Dimension Using Microimplant-Assisted Rapid Palatal Expansion (MARPE) Appliances. Semin. Orthod. 2019, 25, 46–59. [Google Scholar] [CrossRef] [Green Version]
- Salmoria, I.; de Souza, E.C.; Furtado, A.; Franzini, C.M.; Custodio, W. Dentoskeletal Changes and Their Correlations after Micro-Implant-Assisted Palatal Expansion (MARPE) in Adults with Advanced Midpalatal Suture Ossification. Clin. Oral Investig. 2022, 26, 3021–3031. [Google Scholar] [CrossRef]
- Sfogliano, L. A Three-Dimensional Analysis to Investigate the Midface Changes with MSE. Master’s Thesis, University of California, Los Angeles (UCLA), Los Angeles, CA, USA, 2019. [Google Scholar]
- Asaumi, R.; Kawai, T.; Sato, I.; Yoshida, S.; Yosue, T. Three-Dimensional Observations of the Incisive Canal and the Surrounding Bone Using Cone-Beam Computed Tomography. Oral Radiol. 2010, 26, 20–28. [Google Scholar] [CrossRef]
- Song, K.-T.; Park, J.H.; Moon, W.; Chae, J.-M.; Kang, K.-H. Three-Dimensional Changes of the Zygomaticomaxillary Complex after Mini-Implant Assisted Rapid Maxillary Expansion. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 653–662. [Google Scholar] [CrossRef]
- Wennström, J.L.; Lindhe, J.; Sinclair, F.; Thilander, B. Some Periodontal Tissue Reactions to Orthodontic Tooth Movement in Monkeys. J. Clin. Periodontol. 1987, 14, 121–129. [Google Scholar] [CrossRef]
- Baek, E.S.; Hwang, S.; Choi, Y.J.; Roh, M.R.; Nguyen, T.; Kim, K.-H.; Chung, C.J. Quantitative and Perceived Visual Changes of the Nasolabial Fold Following Orthodontic Retraction of Lip Protrusion. Angle Orthod. 2018, 88, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, V.; Davidovitch, Z. On a Path to Unfolding the Biological Mechanisms of Orthodontic Tooth Movement-V. 2009. Available online: https://journals.sagepub.com/doi/full/10.1177/0022034509338914 (accessed on 12 September 2022).
- Chung, C.J.; Jang, W.; Piers, C.; Lee, D.-W.; Hwang, S.; Kim, K.-H.; Proffit, W.R.; Nguyen, T. Differential Alveolar Bone Modeling after Orthodontic Retraction. J. Am. Dent. Assoc. 2019, 150, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, V.; Davidovitch, Z. Cellular, Molecular, and Tissue-Level Reactions to Orthodontic Force. Am. J. Orthod. Dentofacial Orthop. 2006, 129, 469.e1–469.e32. [Google Scholar] [CrossRef] [PubMed]
- Brüllmann, D.; Schulze, R.K.W. Spatial Resolution in CBCT Machines for Dental/Maxillofacial Applications—What Do We Know Today? Dentomaxillofac. Radiol. 2015, 44, 20140204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsutsumi, K.; Chikui, T.; Okamura, K.; Yoshiura, K. Accuracy of linear measurement and the measurement limits of thin objects with cone beam computed tomography: Effects of measurement directions and of phantom locations in the fields of view. Int. J. Oral Maxillofac. Implants. 2011, 26, 91–100. [Google Scholar]
- Kumar, S.A.; Gurunathan, D.; Muruganandham, S.S.; Kumar, S.A. Rapid Maxillary Expansion: A Unique Treatment Modality in Dentistry. J. Clin. Diagn. Res. 2011, 5, 906–911. [Google Scholar]
- Doruk, C.; Sökücü, O.; Biçakçi, A.A.; Yilmaz, U.; Taş, F. Comparison of Nasal Volume Changes during Rapid Maxillary Expansion Using Acoustic Rhinometry and Computed Tomography. Eur. J. Orthod. 2007, 29, 251–255. [Google Scholar] [CrossRef] [Green Version]
- Krogstad, O.; Omland, G. Temporary Paresthesia of the Lower Lip: A Complication of Orthodontic Treatment. A Case Report. Br. J. Orthod. 1997, 24, 13–15. [Google Scholar] [CrossRef]
| Measurement | Definition |
|---|---|
| #11Rm-#21Rm | Mediolateral distance between #11Rm and #21Rm (mm) |
| #11Rm-Cat | Anteroposterior distance between #11Rm and anterior margin of IC (mm) |
| #21Rm-Cat | Anteroposterior distance between #21Rm and anterior margin of IC (mm) |
| IC LP width | Labiopalatal width of IC (mm) |
| IC ML width | Mediolateral width of IC (mm) |
| #11Rt-#21Rt | Mediolateral distance between root apices of #11 and #21 (mm) |
| #11Cr-#21Cr | Mediolateral distance between crown tips of #11 and #21 (mm) |
| IC volume | Volume of IC from oral opening to nasal bifurcation (px, cm3) |
| Measurements (n = 20) | L1 | L2 | L3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | p Value | T0 | T1 | p Value | T0 | T1 | p Value | |
| IC ML width | 3.64 ± 1.47 | 5.82 ± 1.04 | 0.000 *** | 3.71 ± 1.04 | 5.73 ± 1.46 | 0.000 ***† | 3.45 ± 0.84 | 5.77 ± 1.27 | 0.000 *** |
| IC LP width | 3.27 ± 0.69 | 3.60 ± 0.73 | 0.008 ** | 3.09 ± 0.65 | 3.61 ± 0.50 | 0.001 ** | 2.90 ± 0.57 | 3.38 ± 0.62 | 0.004 ** |
| #11 Rm-Cat | 4.48 ± 1.34 | 4.03 ± 1.17 | 0.008 ** | 4.13 ± 1.47 | 3.95 ± 1.50 | 0.218 | 4.11 ± 1.47 | 3.94 ± 1.45 | 0.299 |
| #21 Rm-Cat | 4.53 ± 1.25 | 4.02 ± 1.15 | 0.013 * | 4.18 ± 1.54 | 3.90 ± 1.31 | 0.129 | 4.07 ± 1.55 | 3.87 ± 1.44 | 0.182 |
| Measurements (n = 10) | L1 | ANS mid | IC Bi | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | p Value | T0 | T1 | p Value | T0 | T1 | p Value | |
| IC ML width | 3.97 ± 2.18 | 5.97 ± 1.10 | 0.028 * | 3.52 ± 1.52 | 5.70 ± 1.28 | 0.000 *** | 4.85 ± 1.53 | 6.73 ± 1.56 | 0.000 *** |
| IC LP width | 2.89 ± 0.72 | 2.98 ± 0.63 | 0.712 | 2.59 ± 0.71 | 2.93 ± 0.88 | 0.004 **† | 3.09 ± 1.109 | 3.37 ± 1.13 | 0.047 *† |
| Measurements | T0 | T1 | p Value |
|---|---|---|---|
| IC volume (px) | 2269.6 ± 838.7 | 3765.8 ± 1096.8 | 0.000 *** |
| IC volume (cm3) | 0.13 ± 0.050 | 0.22 ± 0.064 | 0.000 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, S.-K.; Kim, Y.-R.; Park, J.H.; Kang, K.-H.; Chang, N.-Y.; Chae, J.-M. Effects of Mini-Implant-Assisted Rapid Palatal Expansion on Incisive Canal Morphology and Tooth–Canal Relationship. Appl. Sci. 2022, 12, 10470. https://doi.org/10.3390/app122010470
Choi S-K, Kim Y-R, Park JH, Kang K-H, Chang N-Y, Chae J-M. Effects of Mini-Implant-Assisted Rapid Palatal Expansion on Incisive Canal Morphology and Tooth–Canal Relationship. Applied Sciences. 2022; 12(20):10470. https://doi.org/10.3390/app122010470
Chicago/Turabian StyleChoi, Sung-Kwon, Yu-Rim Kim, Jae Hyun Park, Kyung-Hwa Kang, Na-Young Chang, and Jong-Moon Chae. 2022. "Effects of Mini-Implant-Assisted Rapid Palatal Expansion on Incisive Canal Morphology and Tooth–Canal Relationship" Applied Sciences 12, no. 20: 10470. https://doi.org/10.3390/app122010470
APA StyleChoi, S.-K., Kim, Y.-R., Park, J. H., Kang, K.-H., Chang, N.-Y., & Chae, J.-M. (2022). Effects of Mini-Implant-Assisted Rapid Palatal Expansion on Incisive Canal Morphology and Tooth–Canal Relationship. Applied Sciences, 12(20), 10470. https://doi.org/10.3390/app122010470






