1. Introduction
Nasopalatine duct cysts (NPDCs), also known as incisive canal cysts, are the most common non-odontogenic developmental cysts, with a prevalence of about 1% in the general population [
1,
2,
3]. Their etiology is unknown, but the possible causes may include local trauma, infection and spontaneous proliferation. NPDCs are usually diagnosed in 40- to 60-year-old patients [
3,
4,
5], but they can also be discovered in younger patients [
6,
7,
8]. The literature generally reports a greater predisposition of men developing an NPDC, with a male-to-female ratio of up to three to one [
4,
6].
Nasopalatine cysts are asymptomatic in 25 to 50% of cases and are mostly discovered incidentally on panoramic X-rays performed during routine dental treatments [
2,
3,
7,
8]. Symptoms, if present, are subtle, therefore making the lesion tolerable by patients over long periods of time. The most frequent clinical signs and symptoms consist of median palatal swelling just behind the incisive papilla; fluctuant swelling and bluish appearance of the mucosa if the cyst is close to the surface; pain, burning sensation or paresthesia in the anterior part of the palate caused by compression of the nasopalatine nerve by the cyst; drainage of cystic contents into the oral cavity, perceived by the patient as salty fluid flow; and formation of a fistula [
3,
7,
8].
An NPDC grows slowly, which can be explained by the intermittent drainage of cystic contents into the oral cavity [
8]. There appears to be no correlation between the age of the patient and the size of the cyst or symptomatology [
3,
7]. The lesion classically presents radiologically as a well-defined heart-shaped unilocular radiolucency of homogeneous content that is located between central incisors, centered on the maxillary incisive canal.
We report here a rare case of an aggressive NPDC extending to the nasal cavity in a fully edentulous patient. The cyst presented clinically in the form of a paramedian vestibular lump in quadrant I and prevented the patient from wearing his dentures.
2. Case Presentation
A 61-year-old patient consulted the Oral Surgery and Implantology Unit of Geneva University Hospitals for a painful swelling of the anterior maxillary vestibule that was present for about two weeks and prevented him from wearing his complete upper denture. The patient smoked (30 pack-year history) and had type 2 diabetes, hypertension and hypercholesterolemia. The patient was taking metformin, atorvastatin and amlodipine.
The extra-oral clinical examination was unremarkable. The intraoral examination showed a completely edentulous maxilla and mandible, and vestibular and palatal swelling around the edentulous sites of teeth #11, 12 and 13. On palpation, the affected area was soft, elastic and painful.
An OPG X-ray revealed a radiotransparent lesion located in the area of the incisors and canines (
Figure 1).
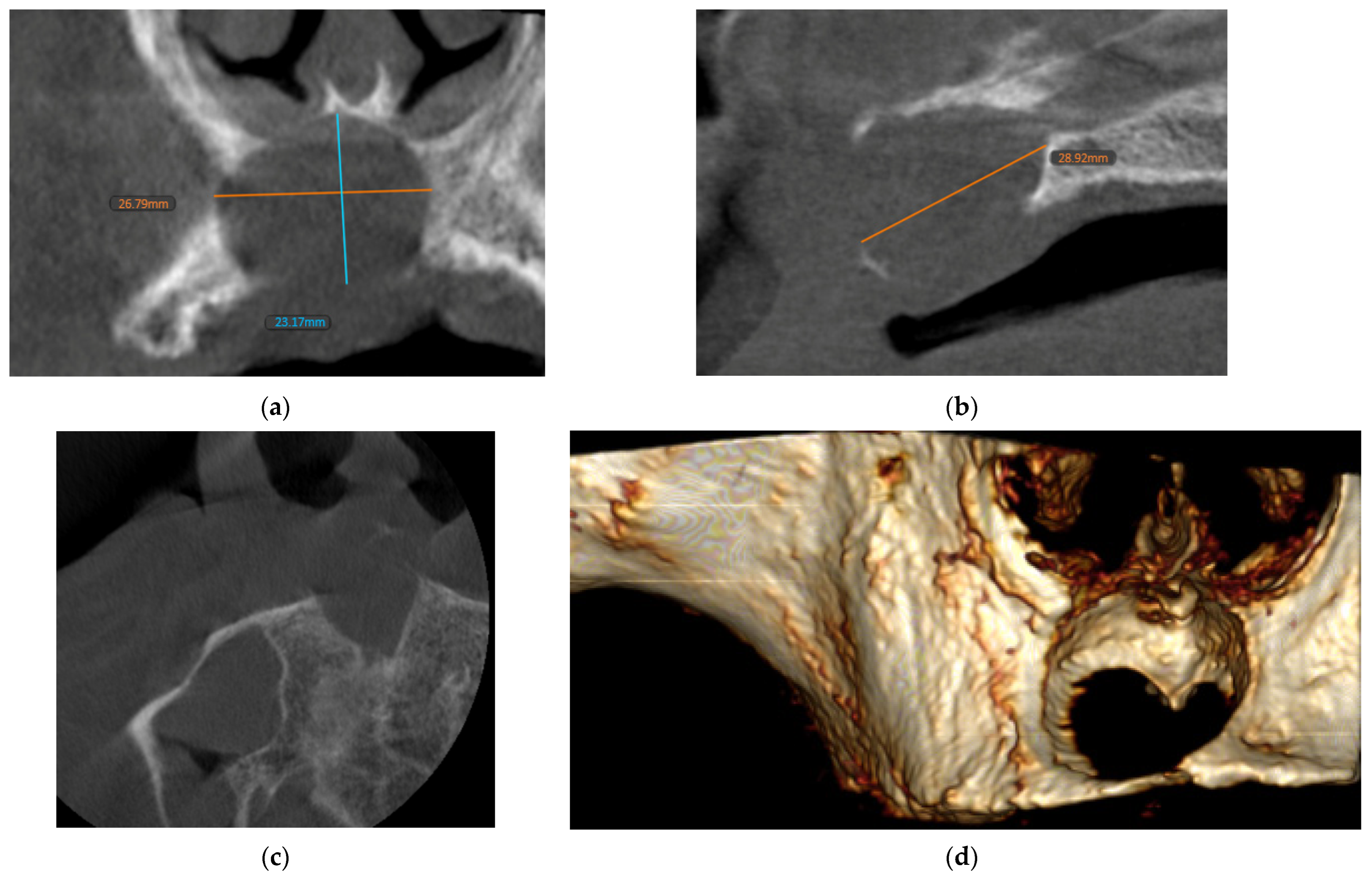
Despite the lesion’s well-defined borders, the analysis of the images was impeded by projection artifacts. A supplementary cone beam computed tomography (CBCT) exam was performed, which showed an expansile lytic lesion with well-delimited contours in the right paramedian region of the maxilla (
Figure 2).
No visible signs of calcification were found within the lesion or periosteal reaction. The lesion had extended to the vestibular side, and, to a lesser degree, to the palatal side, and involved the anterior part of the right nasal cavity floor. In this area, the cortices were extremely expanded, thin, resorbed in places, and could no longer be distinguished.
The lesion extended from sites #13 to 21, and measured about 29 mm × 27 mm × 23 mm. The cystic lesion occupied the region of the incisive canal, which was visible only in its cranial part, opposite to the nasal cavity floor, and was no longer visible elsewhere.
Radiological semiology led to a differential diagnosis of a residual odontogenic cyst, an NPDC or an unicystic ameloblastoma. The lesion was totally enucleated (
Figure 3).
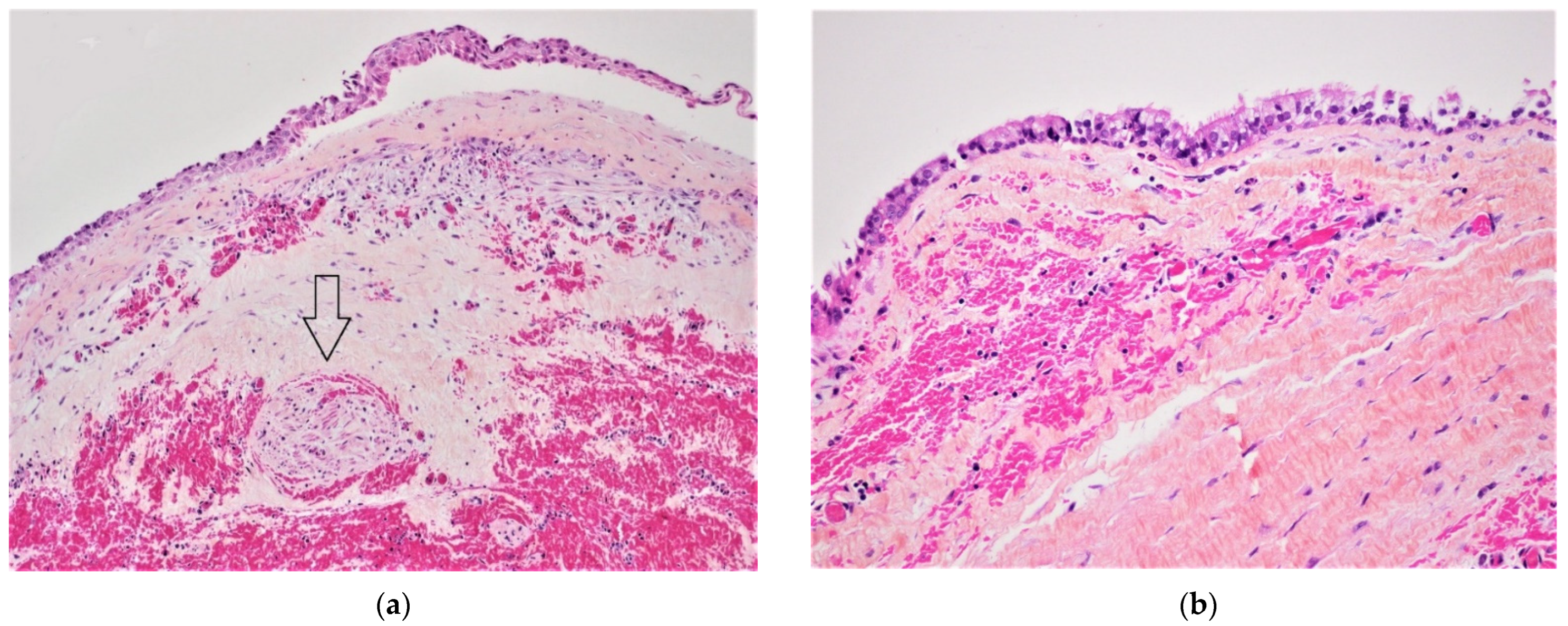
Histopathological examination revealed a fibrous wall lined in part by a thin stratified non-keratinized squamous epithelium and in part by a cuboidal or respiratory-type epithelium with ciliated cells containing a scanty lymphoplasmocytic inflammatory infiltrate. These features allowed for a diagnosis of an NPDC (
Figure 4a,b).
3. Discussion
The nasopalatine canal constitutes a passage through the hard palate and usually contains the nasopalatine nerve and blood vessels, as well as embryonic remains of the nasopalatine duct, which is obliterated at birth [
7,
9]. Although the etiology of NPDCs is unknown, they were initially thought to originate from the epithelium trapped during the fusion of the three processes that make up the palate. Some authors proposed that NPDC result from the spontaneous proliferation of embryonic epithelial tissue remnants in the nasopalatine canal [
5,
6,
7]. Regarding pathogenesis, several factors have been suspected of promoting this proliferation and the development of an NPDC, such as trauma, infection, genetic predisposition or spontaneous onset, but none could be confirmed with complete certainty [
1,
2,
3,
7,
9,
10,
11]. As cysts were found in human fetal nasopalatine ducts, spontaneous cystic degeneration of epithelial rests was also suggested [
1,
2].
NPDCs are located in the nasopalatine canal projects between the roots of the upper central incisors on radiological examination [
12]. The borders of the cysts are generally well-defined and often marked by osteocondensation, unless the cyst is inflamed [
3,
8,
12]. Radiographically, the cysts show as a heart-shaped or pear-shaped image due to the presence of structures more resistant than the spongy bone, such as the nasal spine and the palatine suture. However, the cyst may also appear oval or rounded [
3,
7,
12]. The content of the cyst often produces a homogenous radiotransparent image, although sometimes it can also contain dystrophic calcifications [
12]. An NPDC can affect adjacent structures: it often causes the roots of the central incisors to spread [
12] or, in rare cases, cause root resorption [
3,
12]. At the bone level, it can expand the palatine and, less frequently, the vestibular cortices [
12]. The lamina dura of the adjacent teeth remains intact [
7,
9].
It was often stated that NPDCs have limited growth potential. However, some cases of expansive NPDCs are described in the literature. NPDCs can on occasion expand into neighboring anatomic regions, such as the nasal space [
13,
14,
15,
16,
17,
18,
19,
20].
A differential diagnosis based on radiologic findings should consider several possibilities. A large nasopalatine canal is the most frequent characteristic of an NPDC. The average diameter of the nasopalatine canal is 3 mm. In the absence of symptomatology, a canal with a diameter not exceeding 6 mm is considered normal [
3,
8,
9,
12]. A cyst of the incisive papilla can appear as a radiotransparent oval that is well delimited by a border of peripheral osteocondensation and projects between the apices of the central incisors, but clinical examination enables distinguishing it from an NPDC. A periapical granuloma or a periapical radicular cyst associated with a central incisor may take on the appearance of an NPDC, but they are also characterized by an enlarged desmodontal space and a negative vitality test of adjacent teeth. An additional intra-oral apical X-ray with a slightly modified incident angle should demonstrate a lesion centered on the apex of the responsible tooth, if it is a periapical cyst, while the center of the lesion is shifted in the case of an NPDC [
12]. A dentigerous cyst associated with a mesiodens can give clinical symptoms similar to those of an NPDC, but radiography (discovery of a mesiodens) can guide a diagnosis [
9]. Ameloblastomas are rarely present in this localization; a primary bone tumor and an odontogenic keratocyst should also be included among the possible lesions [
7]. Other clinical differential diagnosis includes a nasolabial cyst, salivary gland tumor (benign and possibly malignant) and schwannoma.
In the presented case, the differential diagnosis considered a residual cyst because of the clinical history of dental extractions and because of the radiological findings. A residual cyst persists after the lack of or an incomplete excision of the initial, usually radicular, cyst after extraction of the affected tooth [
12,
21]. Residual cysts account for about 10% of odontogenic cysts, with a prevalence of about 2% [
21]. They are usually asymptomatic and discovered incidentally [
9]. If they become superinfected, they can cause swelling and pain [
12,
22]. They can be found in all locations [
12,
21]. The center of such a cyst corresponds to where the apex of the affected tooth was previously located [
12]. The boundaries of a residual cyst are rounded, generally well defined and surrounded by a border of peripheral osteocondensation. If superinfection develops, the borders may become poorly defined [
12,
22,
23]. The content of such a cyst appears homogeneously radiotransparent [
12]. Residual cysts can affect adjacent structures in ways similar to NPDCs: they can cause displacement or root resorption of adjacent teeth, and expansion and thinning, or lysis of the cortices [
15]. A definitive diagnosis requires histological examination. Histologically, NPDCs are variable lined by squamous, ciliated (respiratory) and cuboidal epithelium. A characteristic feature helping the diagnosis of NPDC is the presence of nerve bundles and arterial vessels in the cyst wall.
The treatment of choice for an NPDC is palatine enucleation, even in asymptomatic cases, due to the risk of superinfection and possible complications associated with the removal of a very large cyst [
3,
7,
9]. A biopsy should be done before the enucleation to confirm the diagnosis. In the present case, the patient refused the biopsy, preferring the enucleation straight away and he agreed that according to the diagnosis, additional surgery would be necessary. Some authors advocate prior marsupialization for large cysts to reduce the risk of the formation of a naso-antral communication or devitalization of the central incisors [
3,
9]. The main postoperative complication is paresthesia in the anterior palatine region caused by iatrogenic damage to the nasopalatine nerve. It is observed in less than 10% of cases [
3,
8]. It is generally agreed that NPDCs have a low recurrence rate; reports of recurrence range from 0% to 11% [
24].
In this case, the cyst manifested itself clinically in the form of a vestibular lump, which caused discomfort and prevented the patient from wearing his full denture. Radiologically, the cyst was quite aggressive because of its size and its relationship to the surrounding structures it was crossing the maxilla from side to side in the vestibular–palatal plane and extended to the nasal floor. Another peculiarity was that it extended more on the vestibular side, while classically, NPDCs develop mainly on the palatal side. Since the patient had been toothless for years, the differential diagnosis included a residual cyst, even though there were no associated root remnants. We used a slightly modified surgical procedure compared with the classical approach: flaps were raised on both the palatal and vestibular sides instead of the one-sided palatal approach. The specific surgical risk in this case was the accidental creation of naso-antral communication, but the lesion was enucleated without complications.