Geometrical Planning of the Medial Opening Wedge High Tibial Osteotomy—An Experimental Approach
Abstract
:1. Introduction
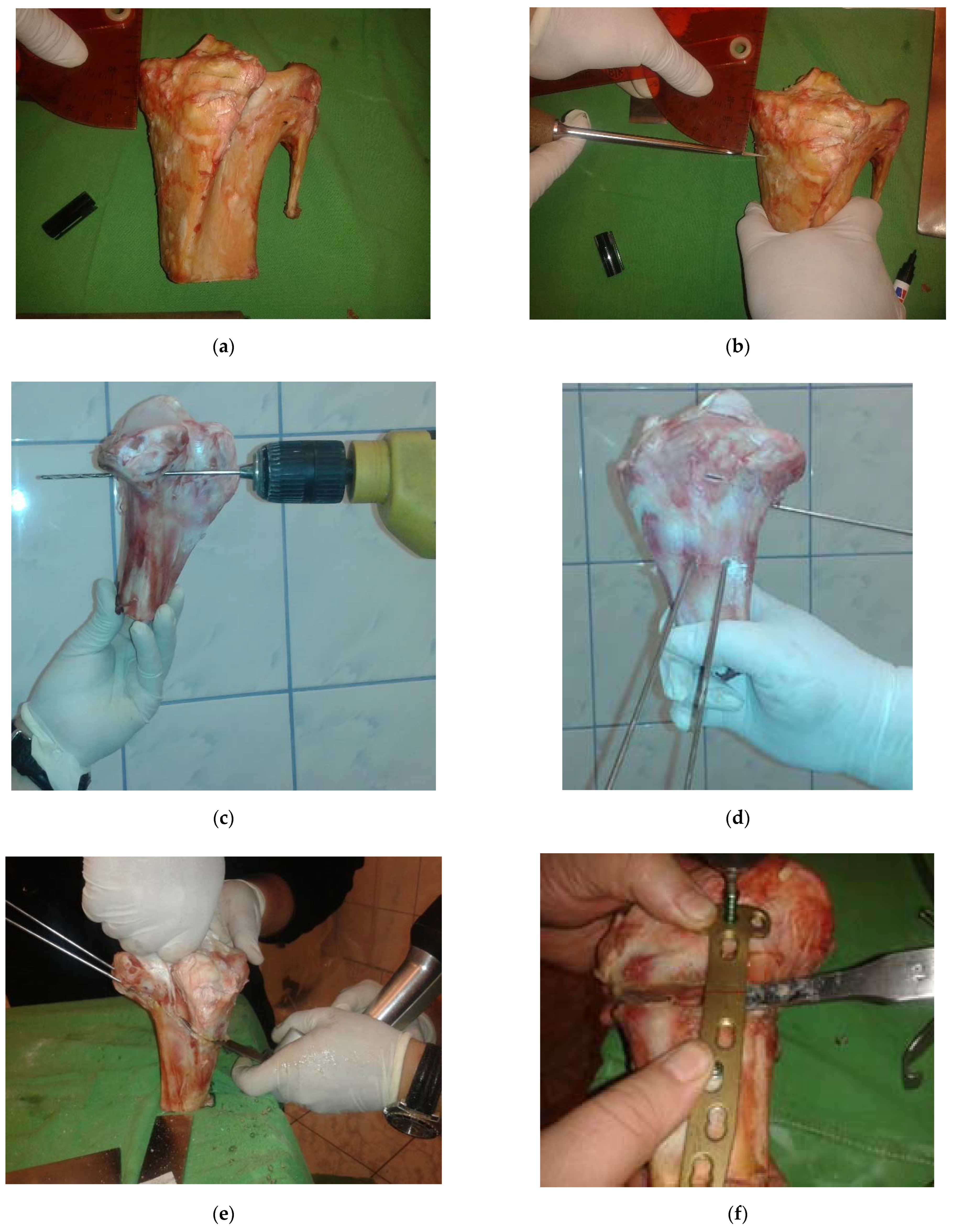
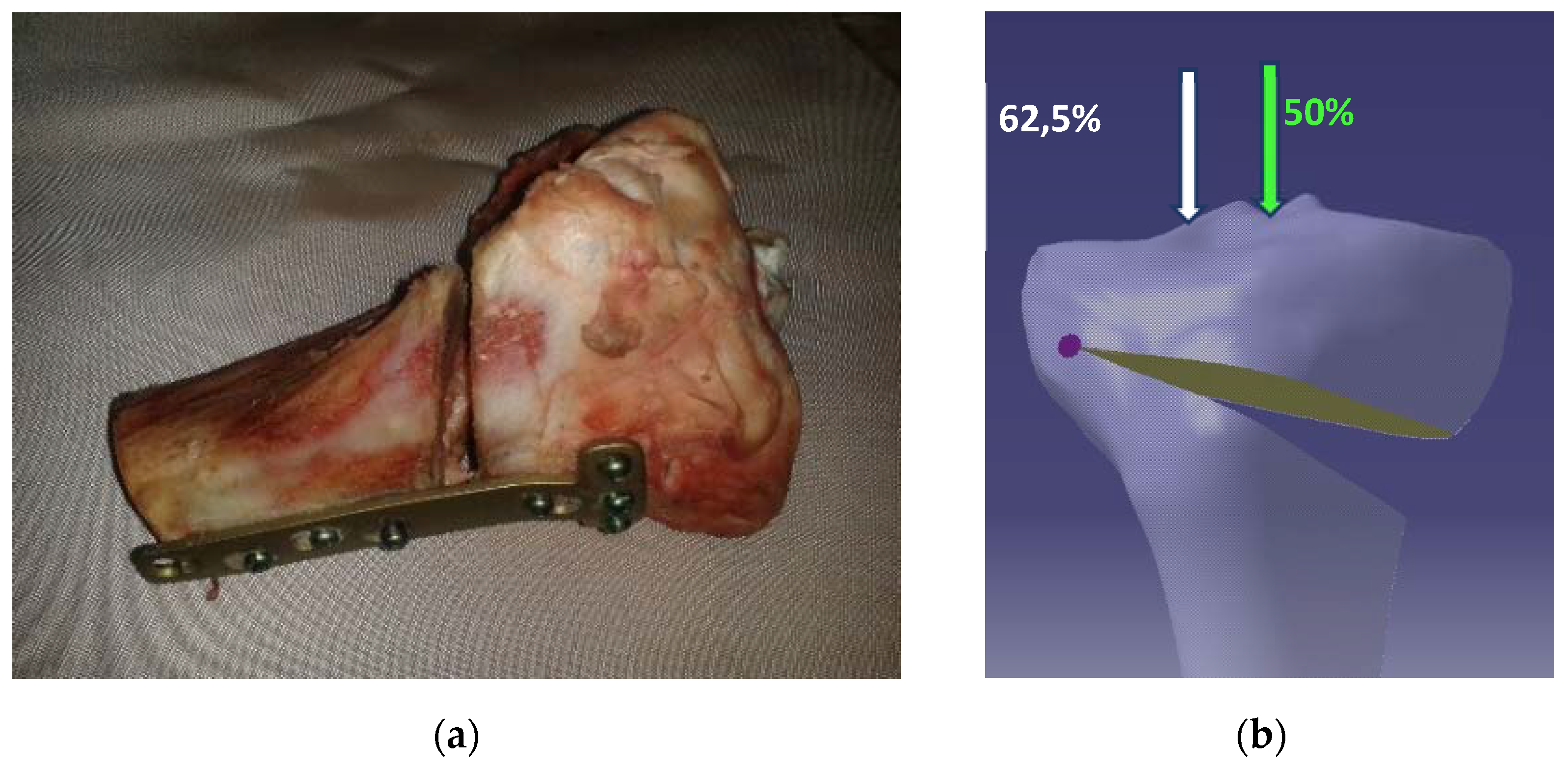
2. Materials and Methods
2.1. Experimental Research on the Study of the Postoperative Behavior of the Tibia-Osteosynthesis Plate Assembly following the Opening Osteotomy
2.1.1. Specimens
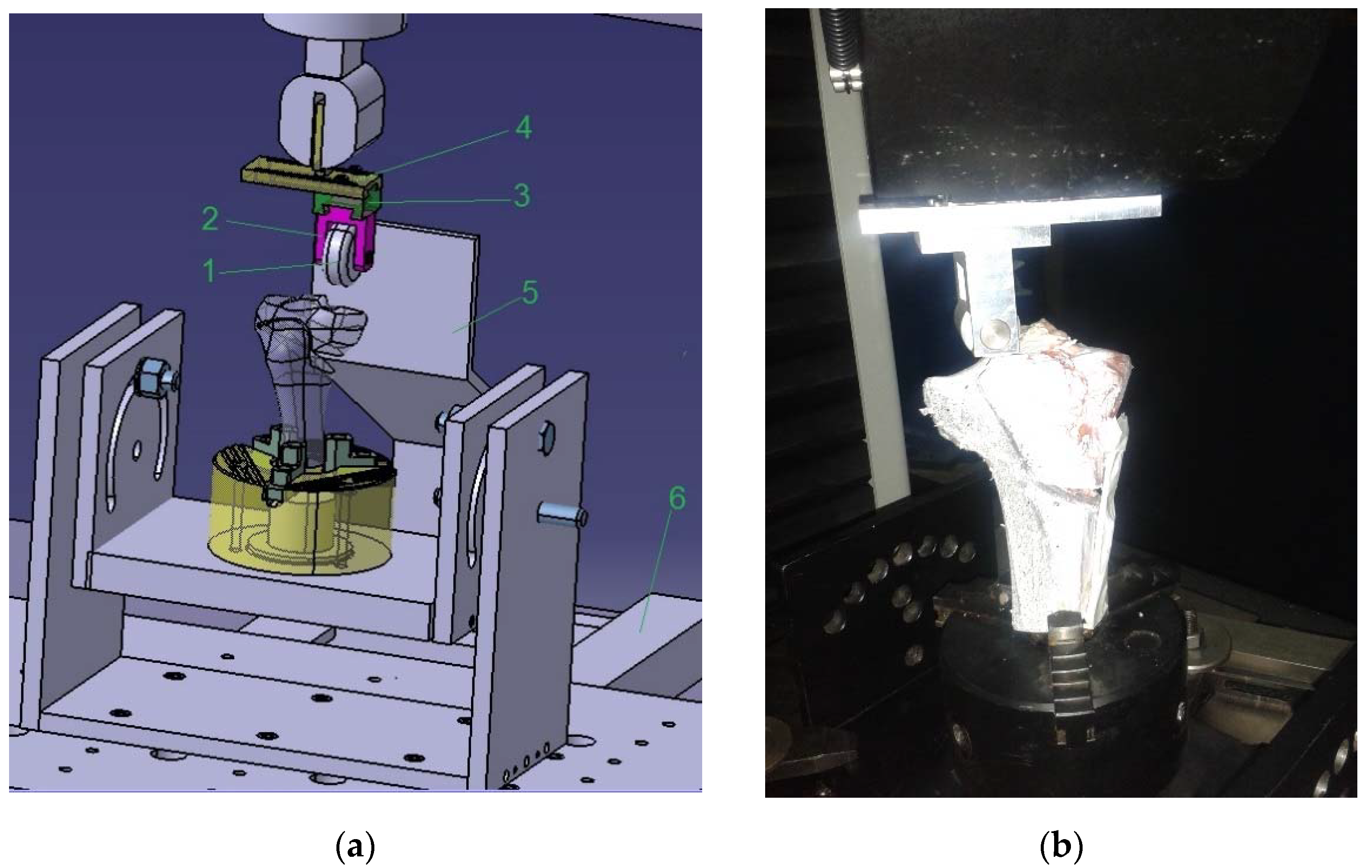
2.1.2. Experimental Stand
- maximum load capacity of 300 kN
- recording of the force with a precision corresponding to class ASME 4-E or DIN 51,221 Class 1
- speed of the mobile crosshead ranging from 0.001 to 500 mm/min
- machine plate surfaces of 1403 × 851 mm
- Bluehill 2.0 software
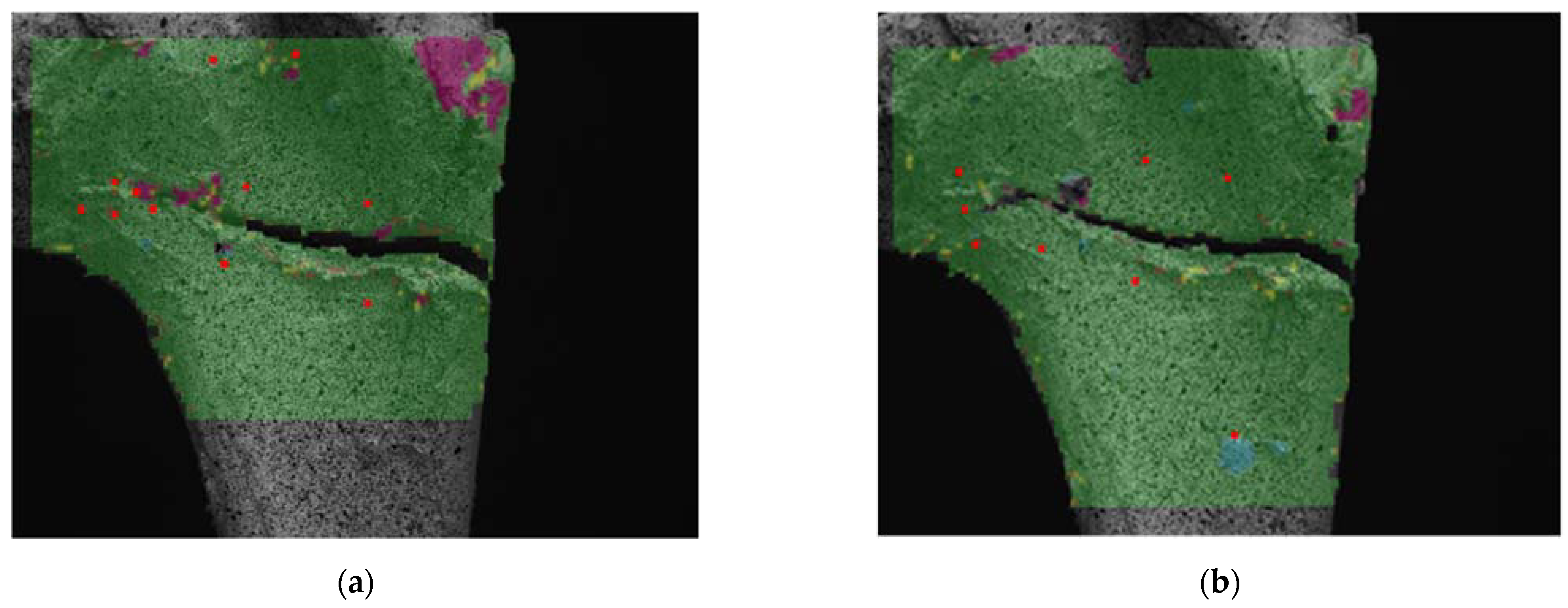
3. Results
Experimental Results Regarding the Study of the Postoperative Behavior of the Tibia-Osteosynthesis Plaque Assembly after Performing an Opening Osteotomy
- The predominant strains are the compression strains (minor strain ε2, the maximum values being 20% for medial loading and 10.6% for offset loading).
- The major strain ε1 has the maximum values of 7.21% in the case of medial loading and 3.96% in the case of offset loading.
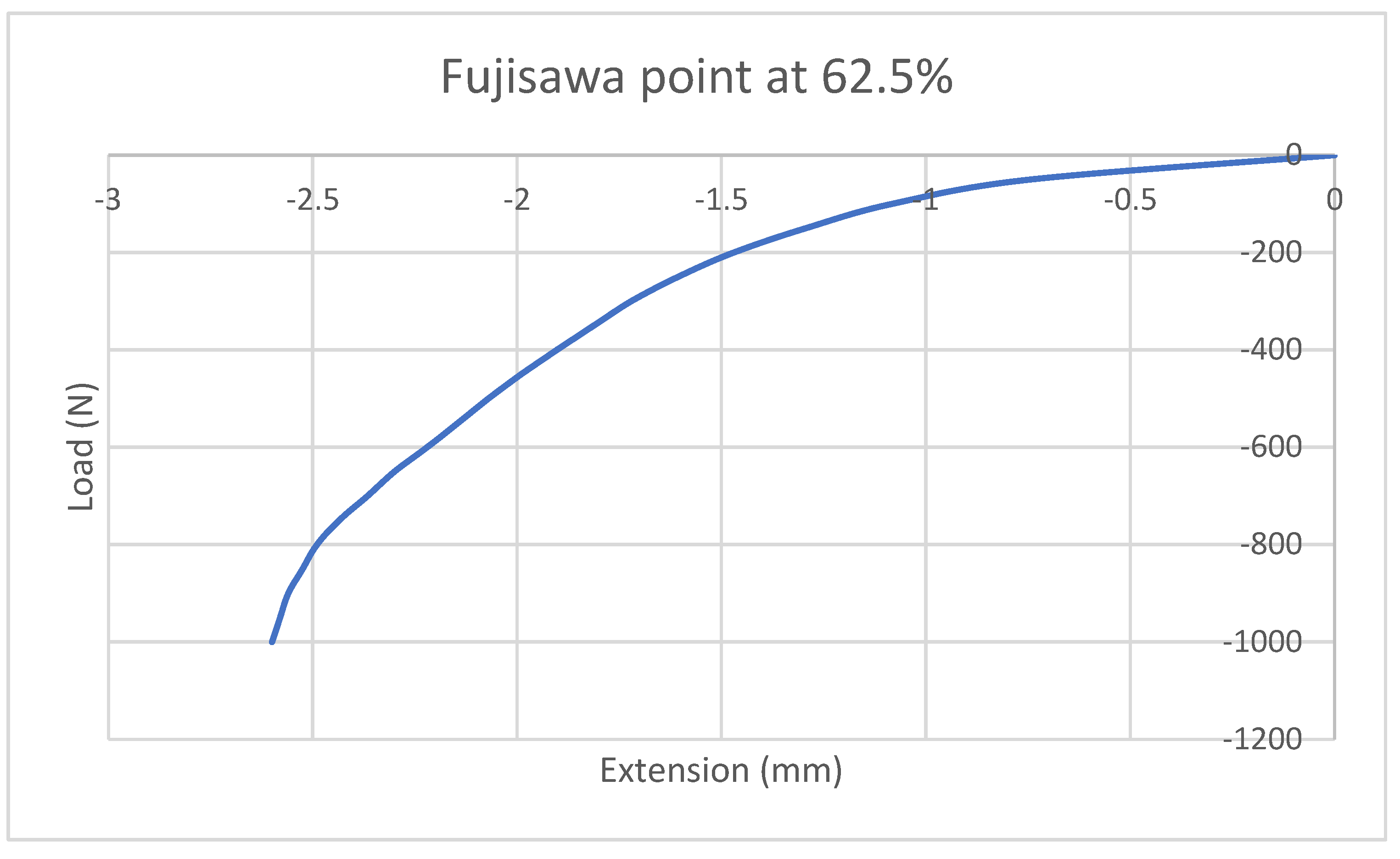
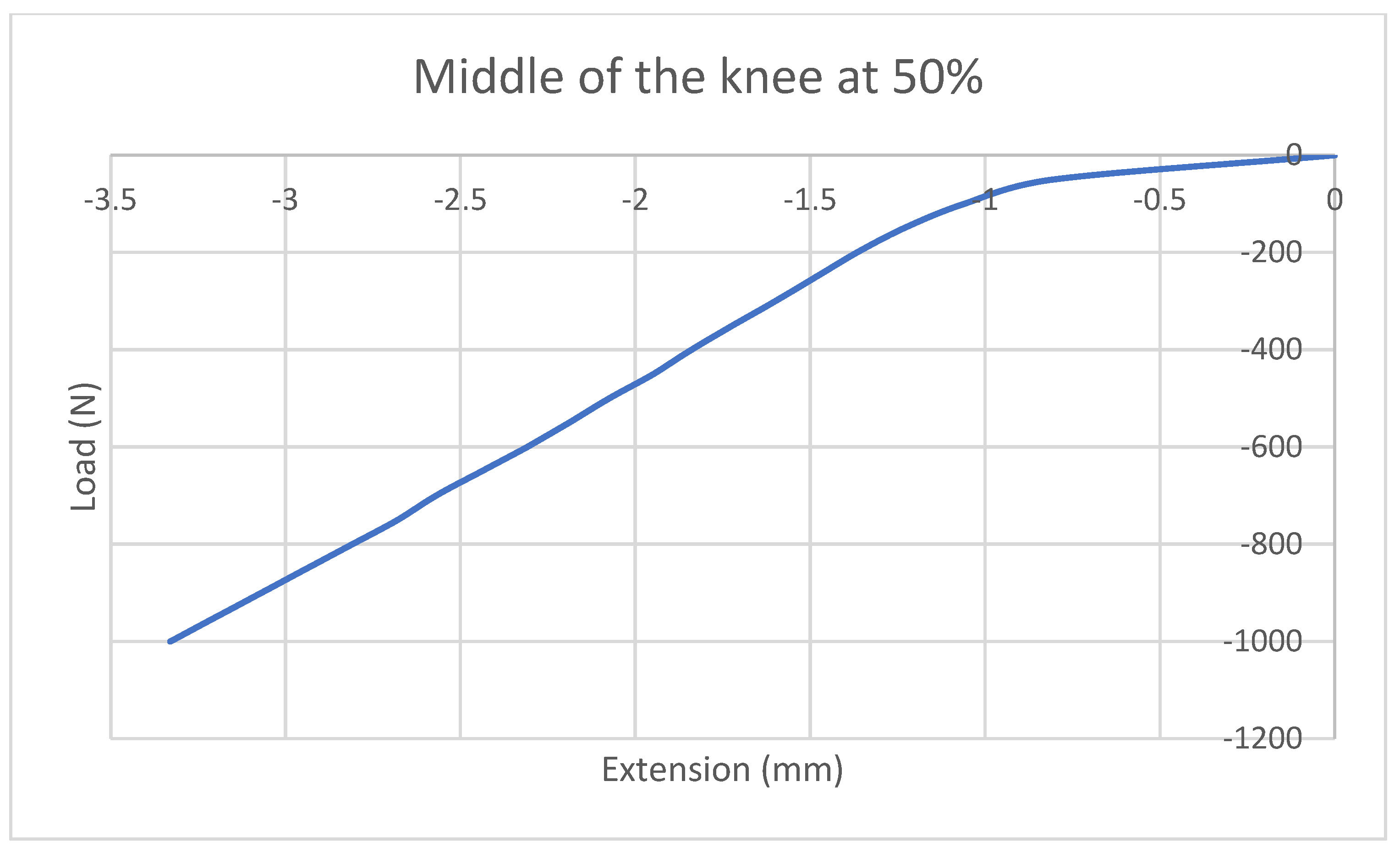
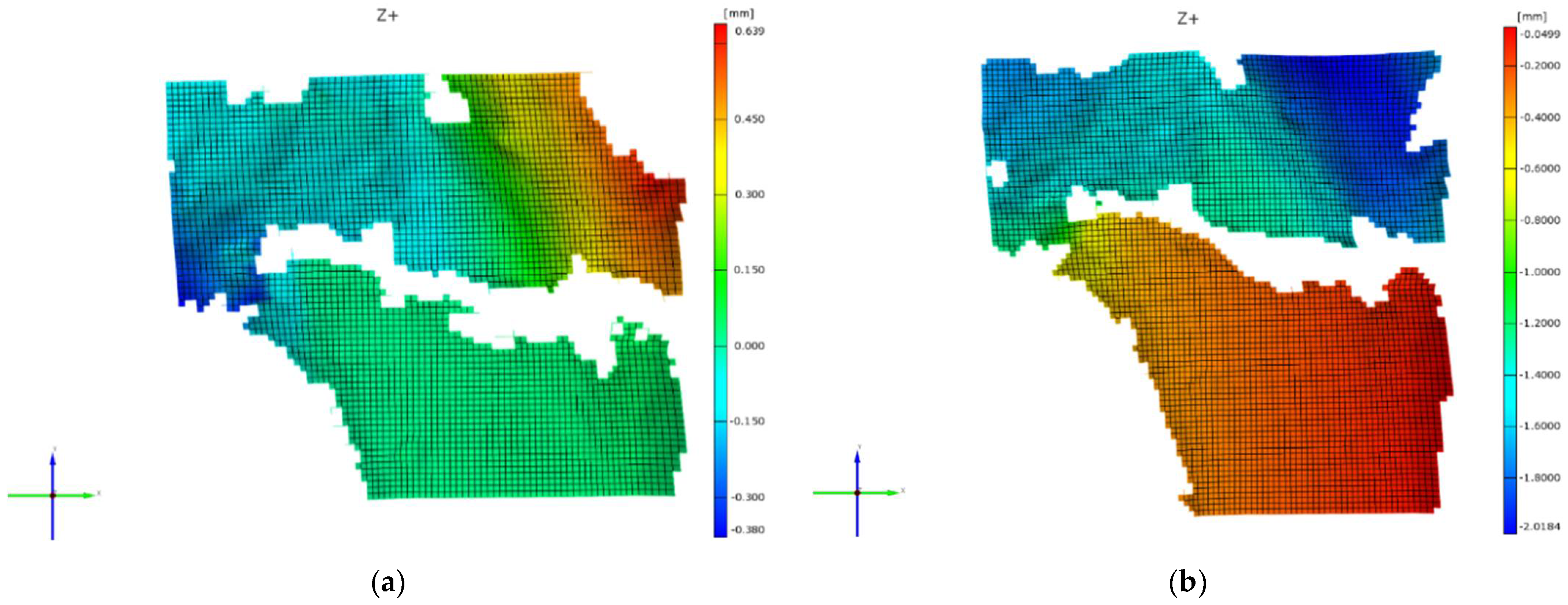
- From the point of view of the displacements that occur, it can be easily seen that the maximum values in the vertical direction (Oy) are reached during the medial loading −2.01 mm, while at offset loading (Fujisawa point) the maximum value of the displacements is 0.639 mm in the positive direction of the Oy axis. This is due to the fact that the stress is applied to the left of the tibial plateau and the stressing force tends to twist the upper part of this plateau in the trigonometric direction.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kutzner, I.; Heinlein, B.; Graichen, F.; Bender, A.; Rohlmann, A.; Halder, A.; Beier, A.; Bergmann, G. Loading of the knee joint during activities of daily living measured in vivo in five subjects. J. Biomech. 2010, 43, 2164–2173. [Google Scholar] [CrossRef] [PubMed]
- Fraysse, F.; Arnold, J.; Thewlis, D. A method for concise reporting of joint reaction forces orientation during gait. J. Biomech. 2016, 49, 3538–3542. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhang, X.; Ardestani, M.M.; Wang, L.; Liu, Y.; Lian, Q.; He, J.; Li, D.; Jin, Z. Prediction of in vivo joint mechanics of an artificial knee implant using rigid multi-body dynamics with elastic contacts. Proc. Inst. Mech. Eng. Part H 2014, 228, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Sutton, P.M.; Holloway, E.S. The young osteoarthritic knee: Dilemmas in management. BMC Med. 2013, 11, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, D.; Ramos, E.; Branco, J. Osteoarthritis. Acta Med. Port. 2014, 28, 99–106. [Google Scholar] [CrossRef] [Green Version]
- Mina, C.; Garrett, W.E.; Pietrobon, R.; Glisson, R.; Higgins, L. High Tibial Osteotomy for Unloading Osteochondral Defects in the Medial Compartment of the Knee. Am. J. Sports Med. 2008, 36, 949–955. [Google Scholar] [CrossRef]
- Messner, K.; Maletius, W. The long-term prognosis for severe damage to weight-bearing cartilage in the knee: A 14-year clinical and radiographic follow-up in 28 young athletes. Acta Orthop. Scand. 1996, 67, 165–168. [Google Scholar] [CrossRef]
- Yoo, M.-J.; Shin, Y.-E. Open Wedge High Tibial Osteotomy and Combined Arthroscopic Surgery in Severe Medial Osteoarthritis and Varus Malalignment: Minimum 5-Year Results. Knee Surg. Relat. Res. 2016, 28, 270–276. [Google Scholar] [CrossRef] [Green Version]
- Schuster, P.; Geßlein, M.; Schlumberger, M.; Mayer, P.; Mayr, R.; Oremek, D.; Frank, S.; Schulz-Jahrsdörfer, M.; Richter, J. Ten-Year Results of Medial Open-Wedge High Tibial Osteotomy and Chondral Resurfacing in Severe Medial Osteoarthritis and Varus Malalignment. Am. J. Sports Med. 2018, 46, 1362–1370. [Google Scholar] [CrossRef]
- Lee, S.-S.; Celik, H.; Lee, D.-H. Predictive Factors for and Detection of Lateral Hinge Fractures Following Open Wedge High Tibial Osteotomy: Plain Radiography Versus Computed Tomography. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 3073–3079. [Google Scholar] [CrossRef]
- Lerner, Z.F.; DeMers, M.; Delp, S.L.; Browning, R.C. How tibiofemoral alignment and contact locations affect predictions of medial and lateral tibiofemoral contact forces. J. Biomech. 2015, 48, 644–650. [Google Scholar] [CrossRef] [Green Version]
- Halder, A.; Kutzner, I.; Graichen, F.; Heinlein, B.; Beier, A.; Bergmann, G. Influence of Limb Alignment on Mediolateral Loading in Total Knee Replacement: In Vivo measurements in five patients. J. Bone Jt. Surg. 2012, 94, 1023–1029. [Google Scholar] [CrossRef]
- Amis, A.A. Biomechanics of high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2012, 21, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Amendola, A.; Bonasia, D.E. Results of high tibial osteotomy: Review of the literature. Int. Orthop. 2009, 34, 155–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Chen, Z.; Gao, Y.; Zhang, J.; Jin, Z. High Tibial Osteotomy: Review of Techniques and Biomechanics. J. Health Eng. 2019, 2019, 8363128. [Google Scholar] [CrossRef]
- Chernchujit, B.; Tharakulphan, S.; Prasetia, R.; Chantarapanich, N.; Jirawison, C.; Sitthiseripratip, K. Preoperative planning of medial opening wedge high tibial osteotomy using 3D computer-aided design weight-bearing simulated guidance: Technique and preliminary result. J. Orthop. Surg. 2019, 27, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomofix Medial High Tibial Plate for Medial Tibial Osteotomy. Available online: http://www.syntes.com/ (accessed on 15 August 2021).
- Dugdale, T.W.; Noyes, F.R.; Styer, D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin. Orthop. Relat. Res. 1992, 274, 248–264. [Google Scholar] [CrossRef]
- Fujisawa, Y.; Masuhara, K.; Shiomi, S. The Effect of High Tibial Osteotomy on Osteoarthritis of the Knee. An arthroscopic study of 54 knee joints. Orthop. Clin. N. Am. 1979, 10, 585–608. [Google Scholar] [CrossRef]
- Jakob, R.P.; Jacobi, M. Die zuklappende Tibiakopfosteotomie in der Behandlung der unikompartimentären Arthrose. Closing wedge osteotomy of the tibial head in treatment of single compartment arthrosis. Orthopade 2004, 33, 143–152. [Google Scholar] [CrossRef]
- Yin, Y.; Li, S.; Zhang, R.; Guo, J.; Hou, Z.; Zhang, Y. What is the relationship between the “Fujisawa point” and postoperative knee valgus angle? A theoretical, computer-based study. Knee 2019, 27, 183–191. [Google Scholar] [CrossRef]
- Kuriyama, S.; Morimoto, N.; Shimoto, T.; Takemoto, M.; Nakamura, S.; Nishitani, K.; Ito, H.; Matsuda, S.; Higaki, H. Clinical efficacy of preoperative 3D planning for reducing surgical errors during open-wedge high tibial osteotomy. J. Orthop. Res. 2019, 37, 898–907. [Google Scholar] [CrossRef] [PubMed]
- Black, M.S.; D’Entremont, A.; McCormack, R.G.; Hansen, G.; Carr, D.; Wilson, D. The effect of wedge and tibial slope angles on knee contact pressure and kinematics following medial opening-wedge high tibial osteotomy. Clin. Biomech. 2018, 51, 17–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, S.J.; Bae, D.K. Computer-Assisted Navigation in High Tibial Osteotomy. Clin. Orthop. Surg. 2016, 8, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Coventry, M.B.; Ilstrup, D.M.; Wallrichs, S.L. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J. Bone Jt. Surg. 1993, 75, 196–201. [Google Scholar] [CrossRef]
- Hernigou, P.; Medevielle, D.; Debeyre, J.; Goutallier, D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J. Bone Jt. Surg. 1987, 69, 332–354. [Google Scholar]
- Fletcher, J.W.A.; Williams, S.; Whitehouse, M.R.; Gill, H.S.; Preatoni, E. Juvenile bovine bone is an appropriate surrogate for normal and reduced density human bone in biomechanical testing: A validation study. Sci. Rep. 2018, 8, 10181. [Google Scholar] [CrossRef]
- Sisljacic, V.; Jovanovic, S.; Mrcela, T.; Nikolic, V.; Radic, R.; Wertheimerc, V.; Tanja Kovac, T.; Mrcela, M. Applicability of bovine tibia as a model in research on various osteosynthesis techniques. Period. Biol. 2010, 112, 59–62. [Google Scholar]
- Cofaru, N.F.; Roman, M.D.; Cofaru, I.I.; Oleksik, V.S.; Fleaca, S.R. Medial Opening Wedge High Tibial Osteotomy in Knee Osteoarthritis—A Biomechanical Approach. Appl. Sci. 2020, 10, 8972. [Google Scholar] [CrossRef]
- Koh, Y.-G.; Son, J.; Kim, H.-J.; Kwon, S.K.; Kwon, O.-R.; Kim, H.J.; Kang, K.-T. Multi-objective design optimization of high tibial osteotomy for improvement of biomechanical effect by using finite element analysis. J. Orthop. Res. 2018, 36, 2956–2965. [Google Scholar] [CrossRef] [Green Version]
- Luo, C.-A.; Hua, S.-Y.; Lin, S.-C.; Chen, C.-M.; Tseng, C.-S. Stress and stability comparison between different systems for high tibial osteotomies. BMC Musculoskelet. Disord. 2013, 14, 110. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.C.-S.; Chen, C.-F.; Lee, O.K. Benefits of opposite screw insertion technique in medial open-wedge high tibial osteotomy: A virtual biomechanical study. J. Orthop. Transl. 2019, 20, 31–36. [Google Scholar] [CrossRef]
- Kwuna, J.D.; Kima, H.J.; Parkb, J.; Parka, I.H.; Kyung, H.S. Open wedge high tibial osteotomy using three-dimensional printed models: Experimental analysis using porcine bone. Knee 2016, 24, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Kyung, H.-S.; Lee, B.-J.; Kim, J.-W.; Yoon, S.-D. Biplanar Open Wedge High Tibial Osteotomy in the Medial Compartment Osteoarthritis of the Knee Joint: Comparison between the Aescula and TomoFix Plate. Clin. Orthop. Surg. 2015, 7, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Russu, O.M.; Strnad, G.; Jakab-Farkas, L.; Cazacu, R.; Feier, A.; Gergely, I.; Trambitas, C.; Petrovan, C. Electrochemical Synthesis of Nanostructured Oxide Layers on Threaded Surfaces of Medical Implants. Rev. Chim. 2018, 69, 1636–1639. [Google Scholar] [CrossRef]
- Andor, B.; Patrascu, J.M.; Florescu, S.; Cojocaru, D.; Sandesc, M.; Borcan, F.; Boruga, O.; Bolintineanu, S. Comparison of Different Knee Implants Used on Patients with Osteoarthritis Control Study. Mater. Plast. 2016, 53, 119–125. [Google Scholar]
- Todor, A.; Vermesan, D.; Haragus, H.; Patrascu, J.M., Jr.; Timar, B.; Cosma, D.I. Cross-cultural adaptation and validation of the Romanian International Knee Documentation Committee—subjective knee form. Peer. J. 2020, 8, e8448. [Google Scholar] [CrossRef]
- Ogawa, H.; Matsumoto, K.; Akiyama, H. Coronal tibiofemoral subluxation is correlated to correction angle in medial opening wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3482–3490. [Google Scholar] [CrossRef]
- Ioniţescu, M.; Vermeşan, D.; Andor, B.; Dumitrascu, C.; Al-Qatawneh, M.; Bloanca, V.; Dumitrascu, A.; Prejbeanu, R. Potential New Treatments for Knee OA: A Prospective Review of Registered Trials. Appl. Sci. 2021, 11, 11049. [Google Scholar] [CrossRef]
- Agneskirchner, J.D.; Freiling, D.; Hurschler, C.; Lobenhoffer, P. Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2005, 14, 291–300. [Google Scholar] [CrossRef]
- Nha, K.W.; Oh, S.M.; Ha, Y.W.; Nikumbha, V.P.; Seo, J.H.; Oh, M.J.; Lim, C.O.; Kim, J.G. A Retrospective Comparison of Union Rates After Open Wedge High Tibial Osteotomies with and Without Synthetic Bone Grafts (Hydroxyapatite and β-tricalciumphosphate) at 2 Years. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 2621–2630. [Google Scholar] [CrossRef]
- Stoffel, K.; Stachowiak, G.; Kuster, M. Open wedge high tibial osteotomy: Biomechanical investigation of the modified Arthrex Osteotomy Plate (Puddu Plate) and the TomoFix Plate. Clin. Biomech. 2004, 19, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Jacquet, C.; Marret, A.; Myon, R.; Ehlinger, M.; Bahlouli, N.; Wilson, A.; Kley, K.; Rossi, J.-M.; Parratte, S.; Ollivier, M. Adding a protective screw improves hinge’s axial and torsional stability in High Tibial Osteotomy. Clin. Biomech. 2020, 74, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.W.; Lim, D.; Seo, H.; Lee, M.C.; Lee, O.-S.; Lee, Y.S. Role of an anatomically contoured plate and metal block for balanced stability between the implant and lateral hinge in open-wedge high-tibial osteotomy. Arch. Orthop. Trauma. Surg. 2018, 138, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, J.M.; Luites, L.W.H.; Wymenga, A.B.; van Heerwaarden, R.J. Early full weight bearing is safe in open-wedge high tibial osteotomy RSA analysis of postoperative stability compared to delayed weight bearing. Acta Orthop. 2010, 81, 193–198. [Google Scholar] [CrossRef]
- Lee, B.-S.; Jo, B.-K.; Bin, S.-I.; Kim, J.-M.; Lee, C.-R.; Kwon, Y.-H. Hinge Fractures Are Underestimated on Plain Radiographs After Open Wedge Proximal Tibial Osteotomy: Evaluation by Computed Tomography. Am. J. Sports Med. 2019, 47, 1370–1375. [Google Scholar] [CrossRef]
- Schröter, S.; Gonser, C.E.; Konstantinidis, L.; Helwig, P.; Albrecht, D. High Complication Rate After Biplanar Open Wedge High Tibial Osteotomy Stabilized with a New Spacer Plate (Position HTO Plate) Without Bone Substitute. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 644–652. [Google Scholar] [CrossRef]
- Schröter, S.; Hoffmann, T.; Döbele, S.; Welke, B.; Hurschler, C.; Schwarze, M.; Stöckle, U.; Freude, T.; Ateschrang, A. Biomechanical properties following open wedge high tibial osteotomy: Plate fixator combined with dynamic locking screws versus standard locking screws. Clin. Biomech. Bristol. Avon. 2018, 60, 108–114. [Google Scholar] [CrossRef]
- Na, Y.G.; Kwak, D.-S.; Chong, S.; Kim, T.K. Factors affecting stability after medial opening wedge high tibial osteotomy using locking plate: A cadaveric study. Knee 2019, 26, 1313–1322. [Google Scholar] [CrossRef]

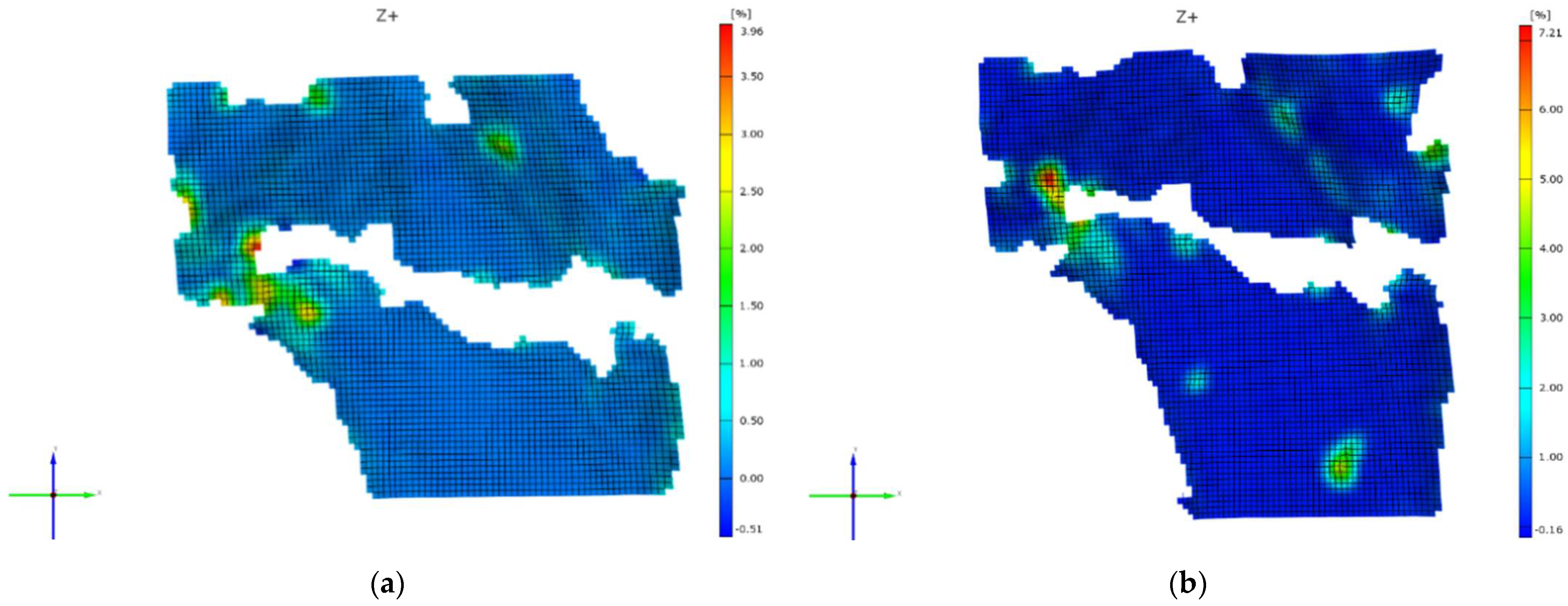
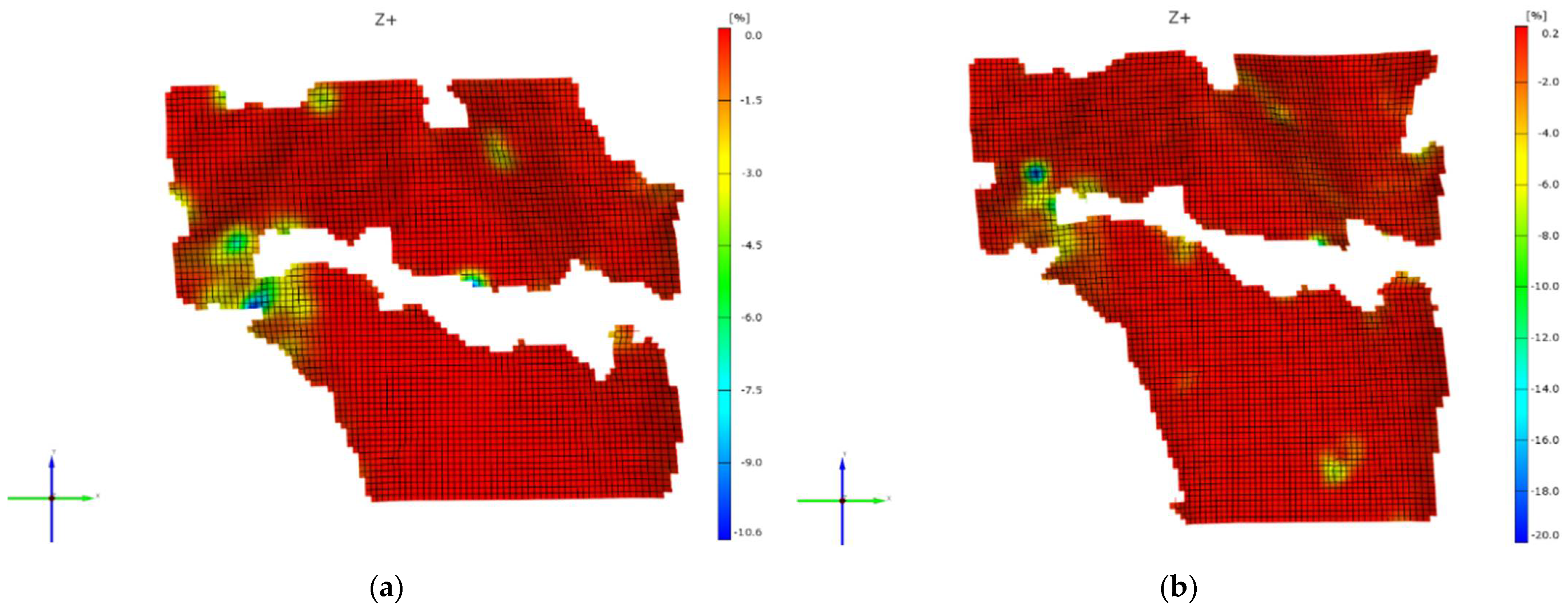


| Stages of the Loading Stroke (Percent) | Medial Loading (Percent) | Offset Loading (Fujisawa Point) (Percent) | |
|---|---|---|---|
| Major strain ε1 | 25 | 5.624 | 2.99 |
| 50 | 6.165 | 3.31 | |
| 75 | 6.509 | 3.75 | |
| 100 | 7.21 | 6.96 | |
| Minor strain ε2 (modulus) | 25 | 13.84 | 5.478 |
| 50 | 16.8 | 5.514 | |
| 75 | 19.411 | 5.953 | |
| 100 | 20 | 10.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cofaru, N.F.; Oleksik, V.; Cofaru, I.I.; Simion, C.M.; Roman, M.D.; Lebada, I.C.; Fleaca, S.R. Geometrical Planning of the Medial Opening Wedge High Tibial Osteotomy—An Experimental Approach. Appl. Sci. 2022, 12, 2475. https://doi.org/10.3390/app12052475
Cofaru NF, Oleksik V, Cofaru II, Simion CM, Roman MD, Lebada IC, Fleaca SR. Geometrical Planning of the Medial Opening Wedge High Tibial Osteotomy—An Experimental Approach. Applied Sciences. 2022; 12(5):2475. https://doi.org/10.3390/app12052475
Chicago/Turabian StyleCofaru, Nicolae Florin, Valentin Oleksik, Ileana Ioana Cofaru, Carmen Mihaela Simion, Mihai Dan Roman, Ioana Codruta Lebada, and Sorin Radu Fleaca. 2022. "Geometrical Planning of the Medial Opening Wedge High Tibial Osteotomy—An Experimental Approach" Applied Sciences 12, no. 5: 2475. https://doi.org/10.3390/app12052475
APA StyleCofaru, N. F., Oleksik, V., Cofaru, I. I., Simion, C. M., Roman, M. D., Lebada, I. C., & Fleaca, S. R. (2022). Geometrical Planning of the Medial Opening Wedge High Tibial Osteotomy—An Experimental Approach. Applied Sciences, 12(5), 2475. https://doi.org/10.3390/app12052475







