Poly(lactic acid)-Based Electrospun Fibrous Structures for Biomedical Applications
Abstract
:1. Introduction
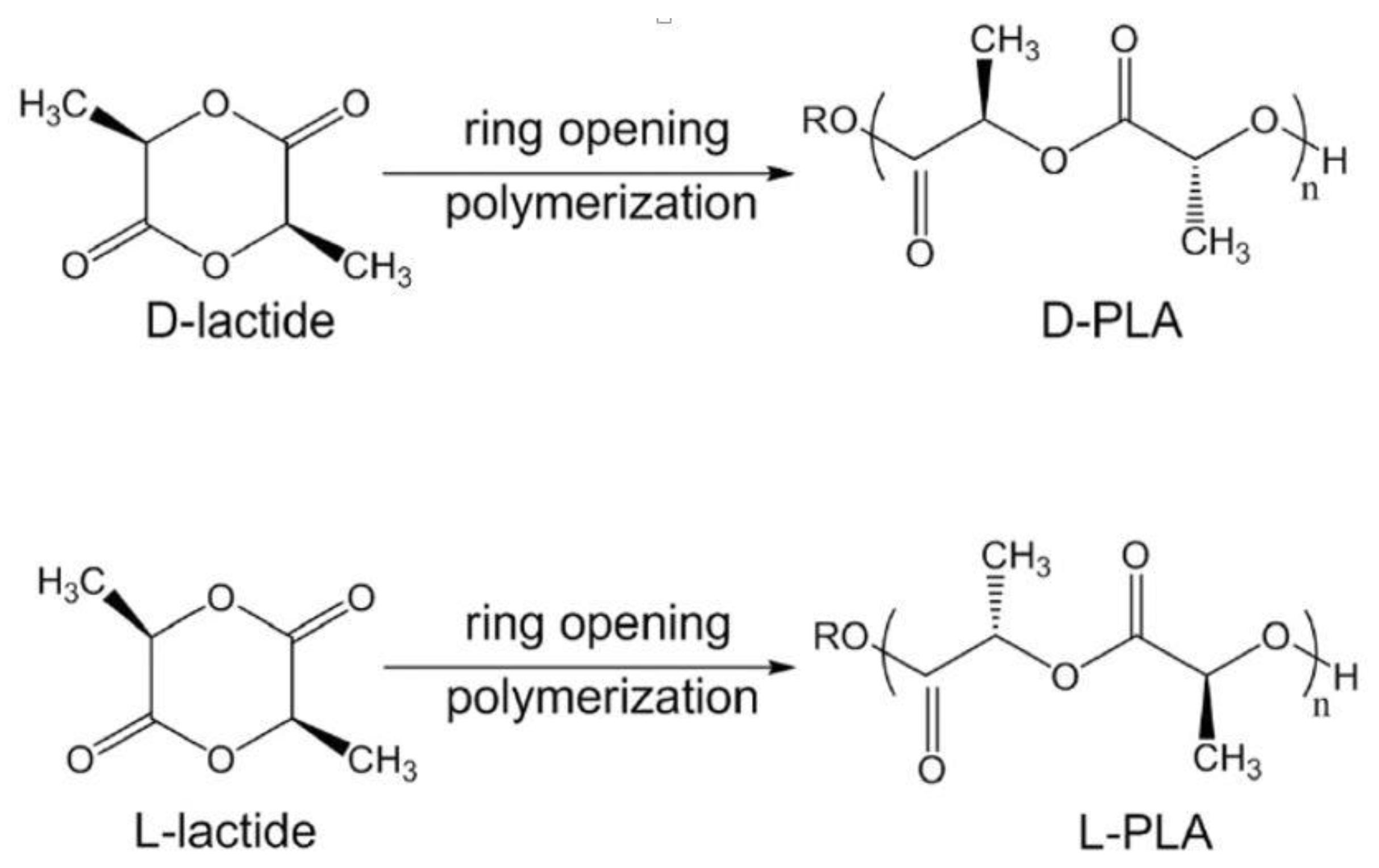
2. PLA Synthesis
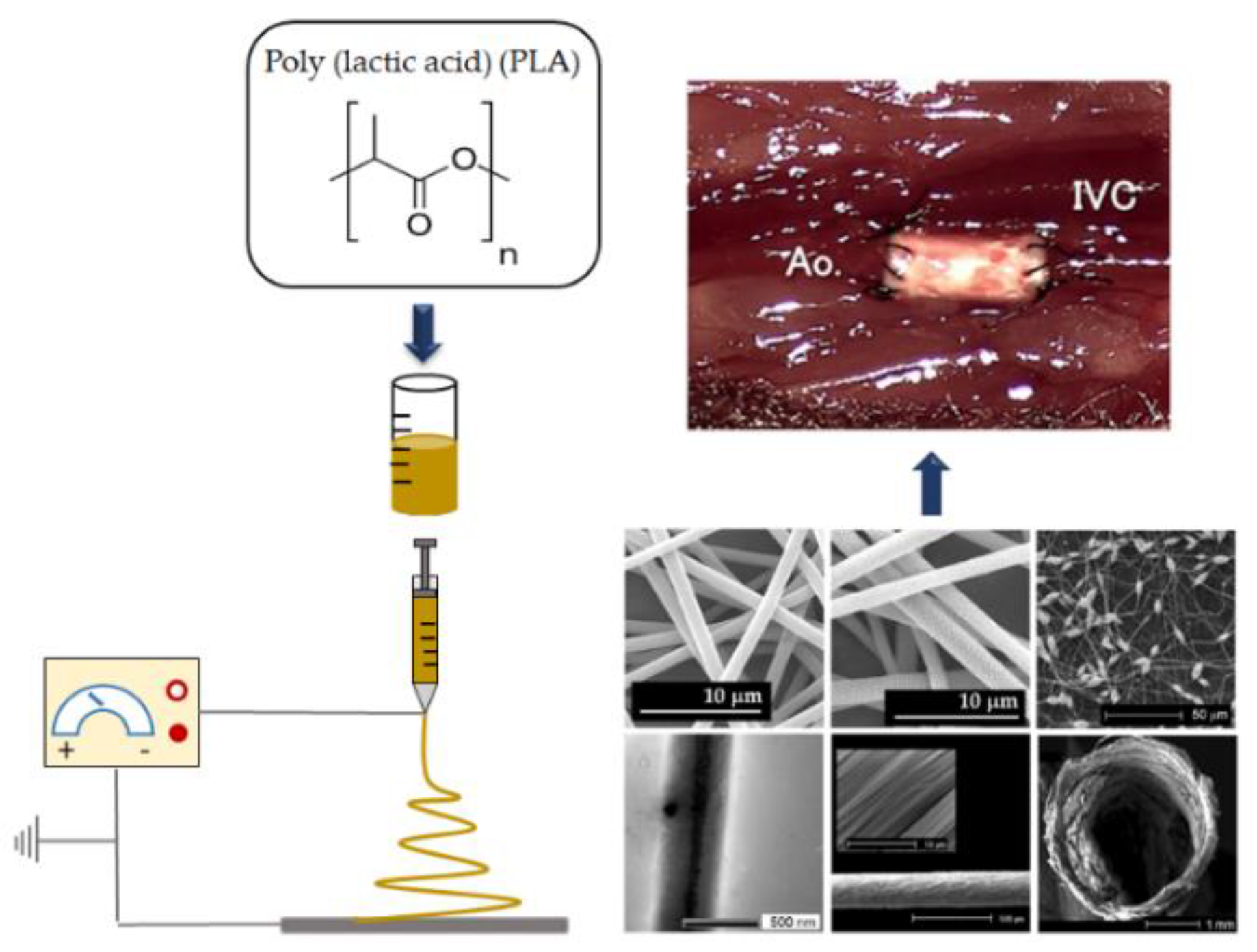
3. PLA Unique Features for Biomedical Applications
4. Electrospinning of PLA Fibers
4.1. PLA Electrospinnability
4.1.1. Solution Parameters
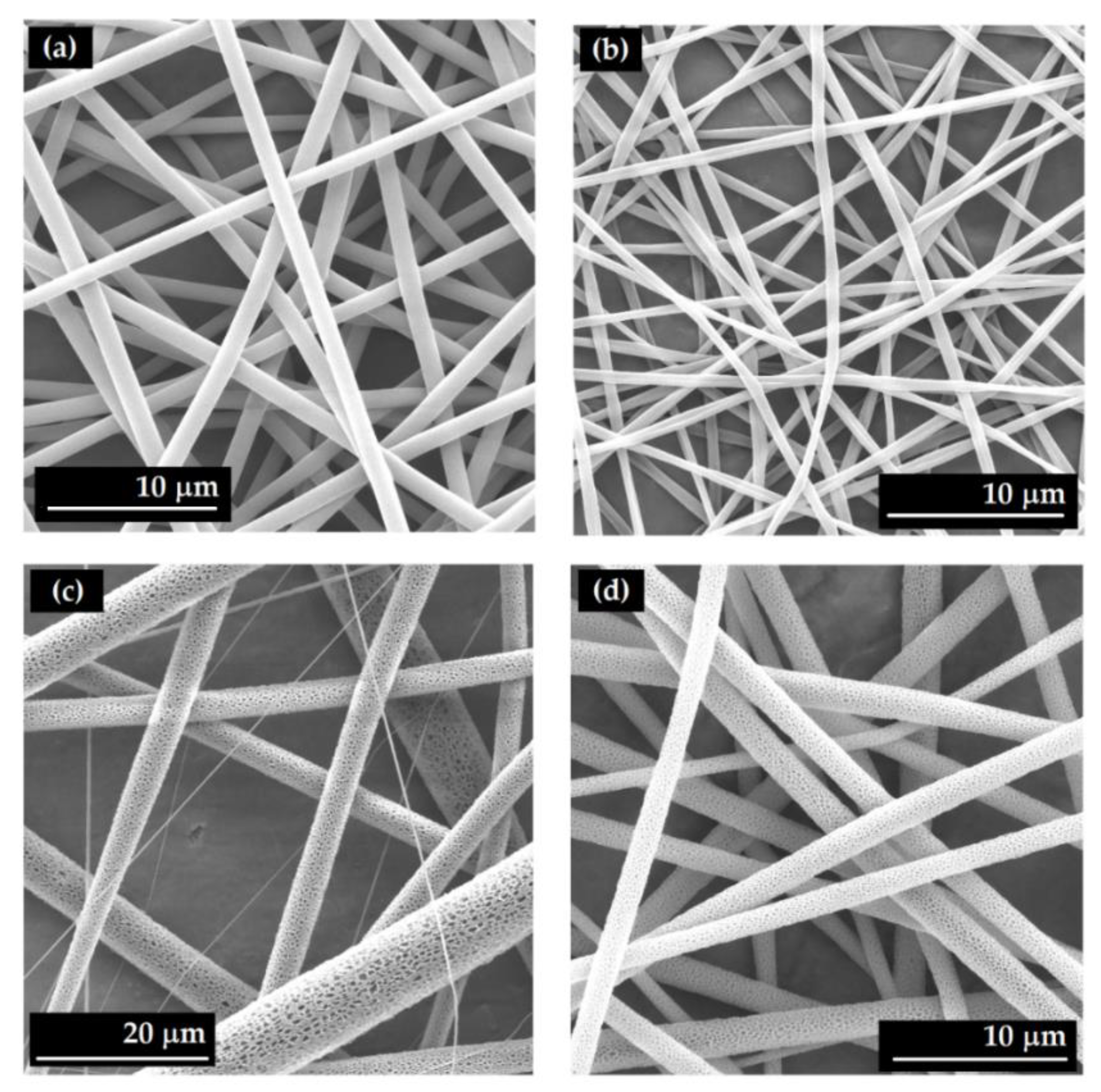
Solvent Systems
Concentration
4.1.2. Processing Parameters
5. Engineering of PLA-Based Electrospun Structures for Biomedical Applications
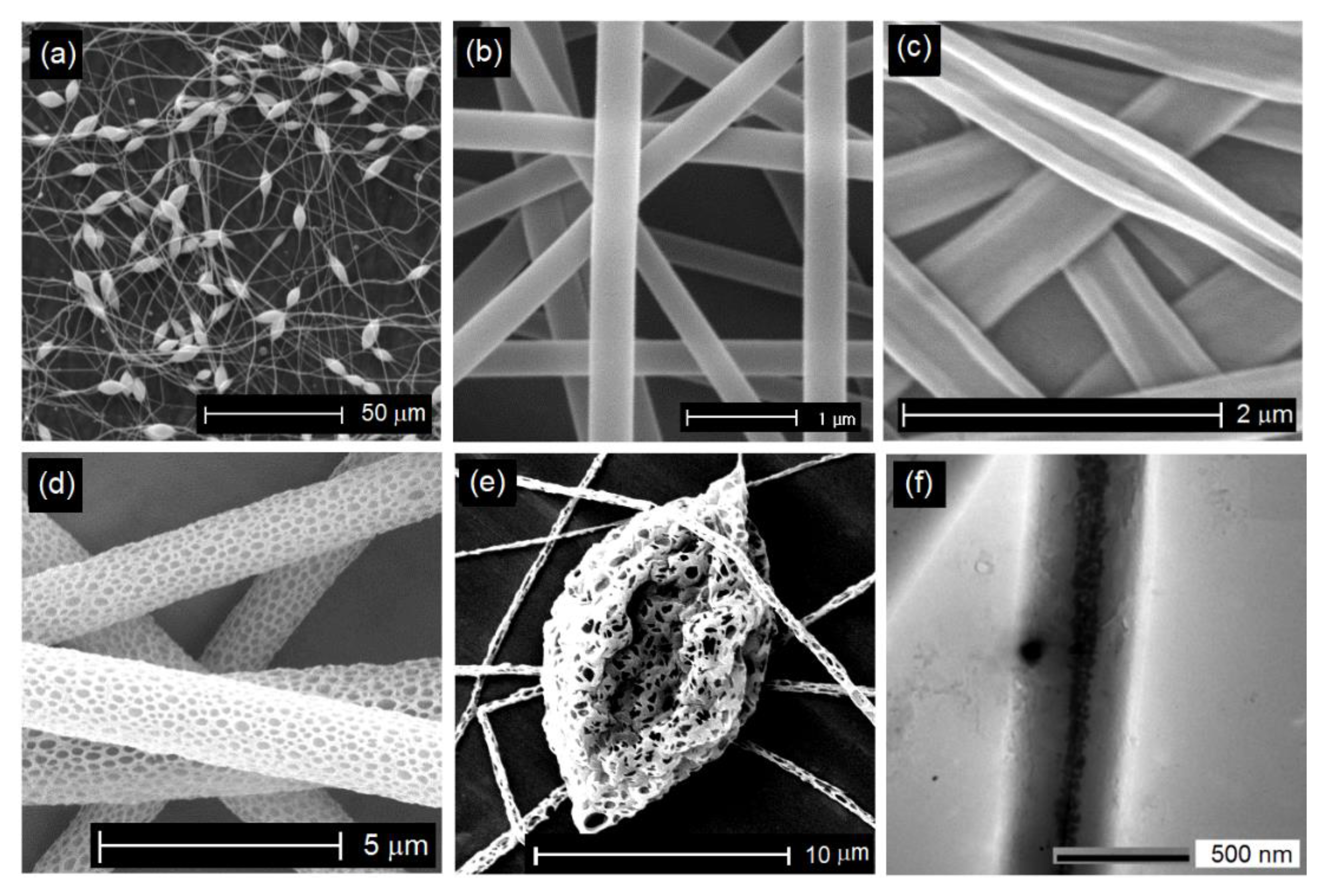
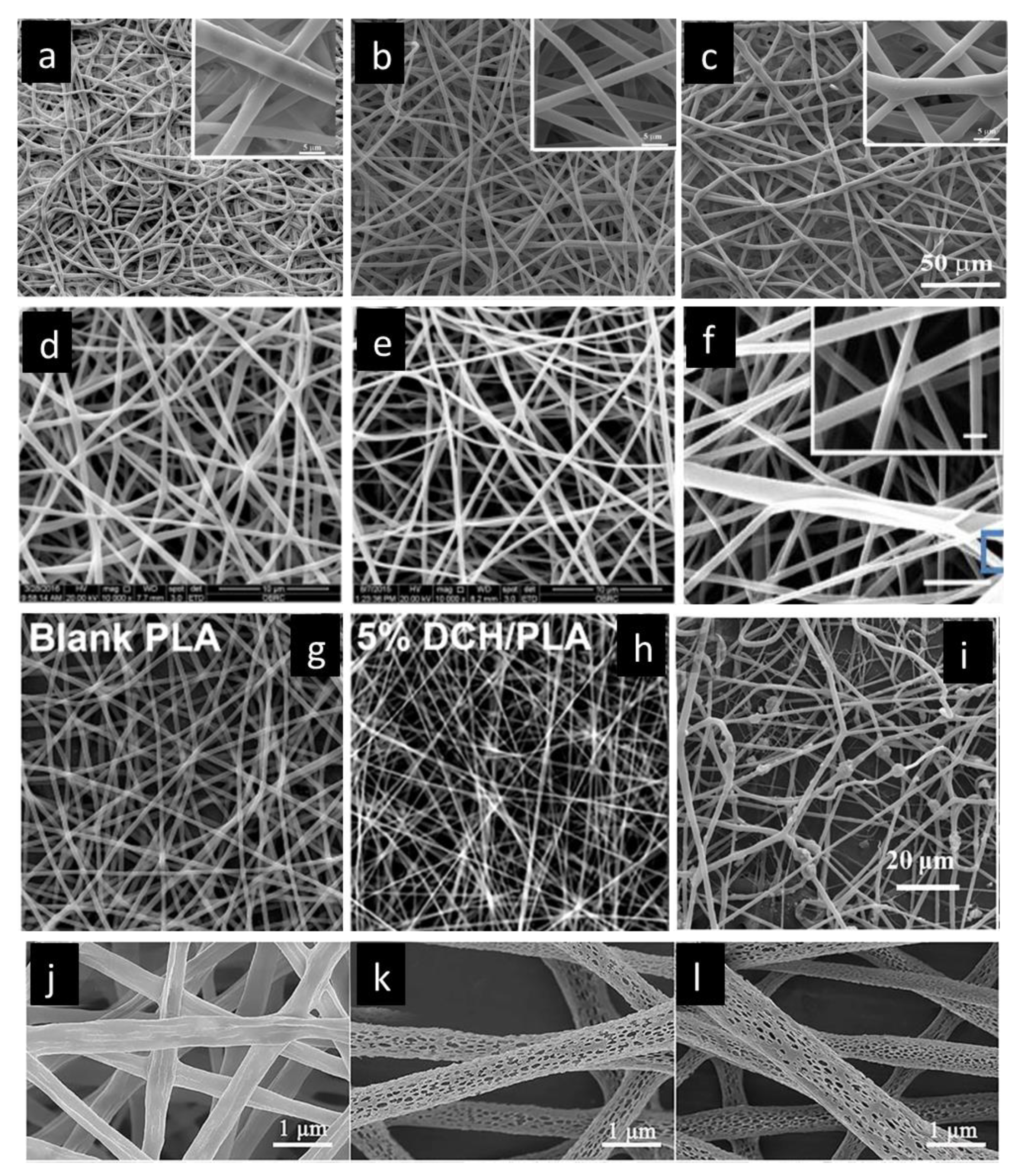
5.1. Control of Morphology
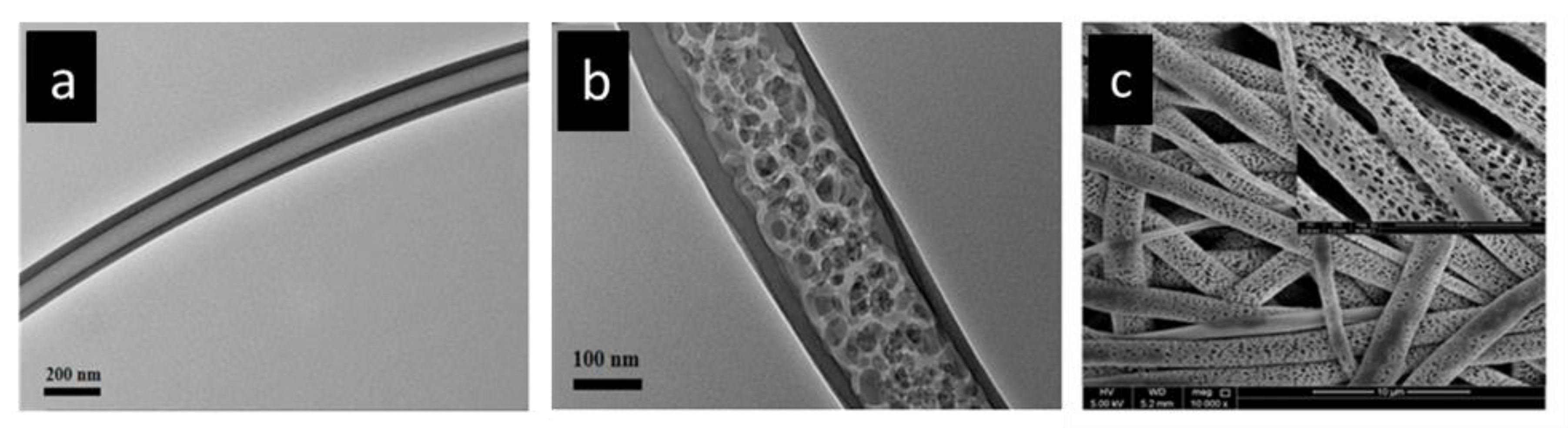
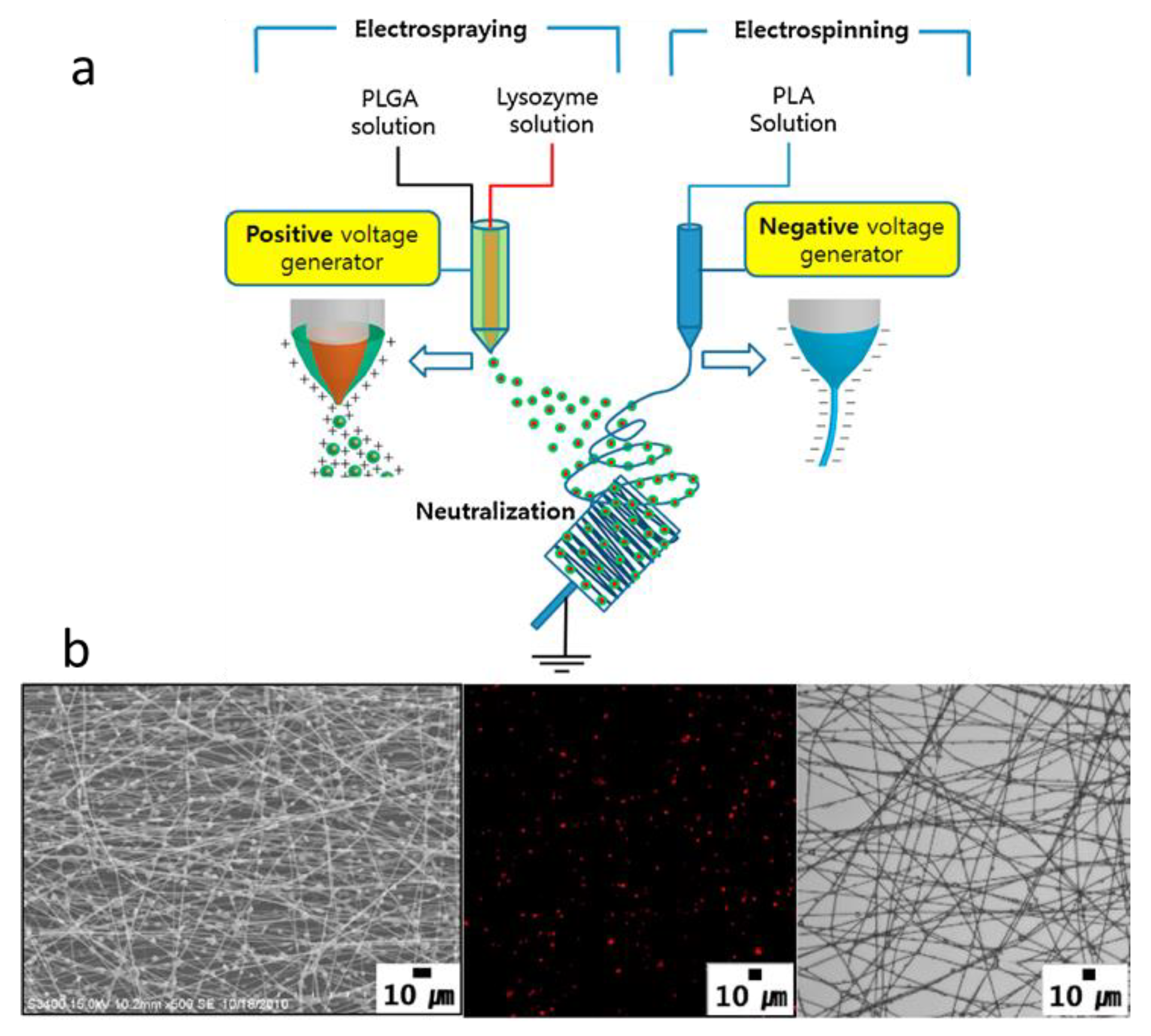
Core-Shell Structure
5.2. Control of the Architecture of PLA-Based Nanofibrous Structures
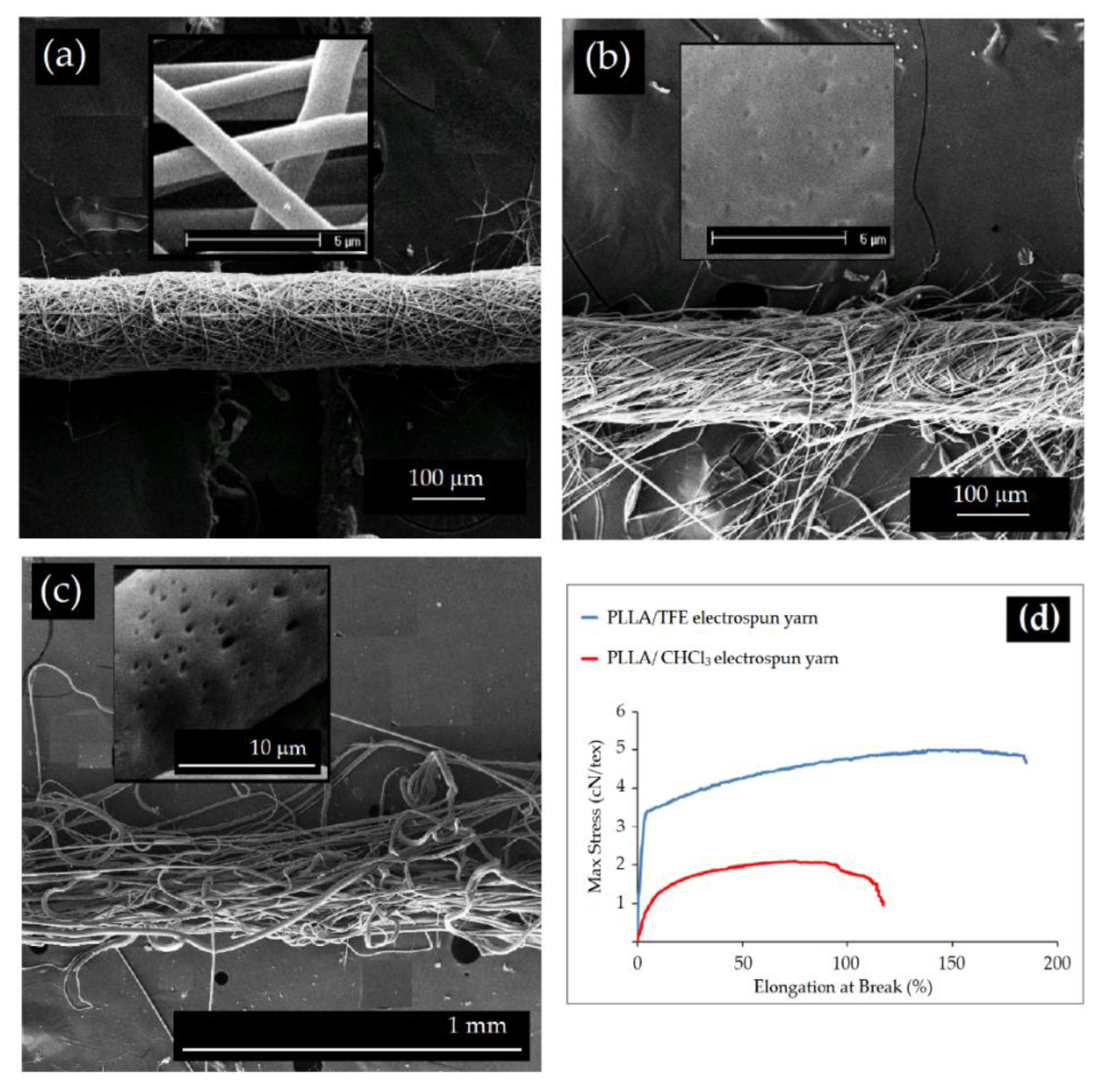
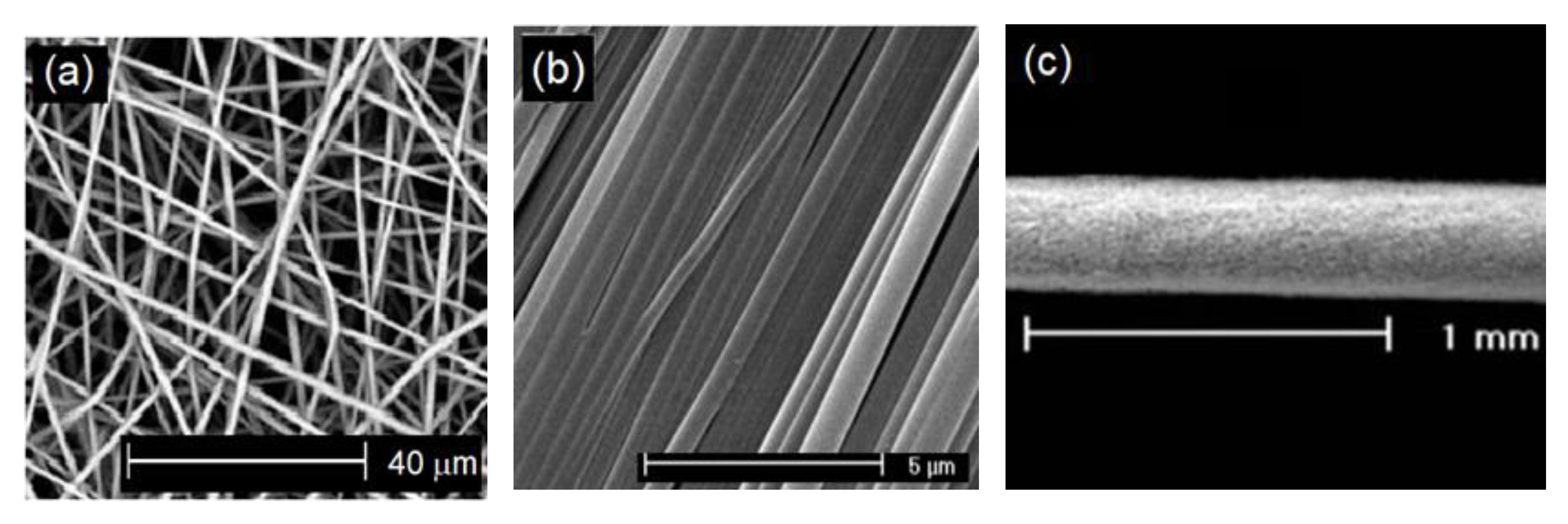
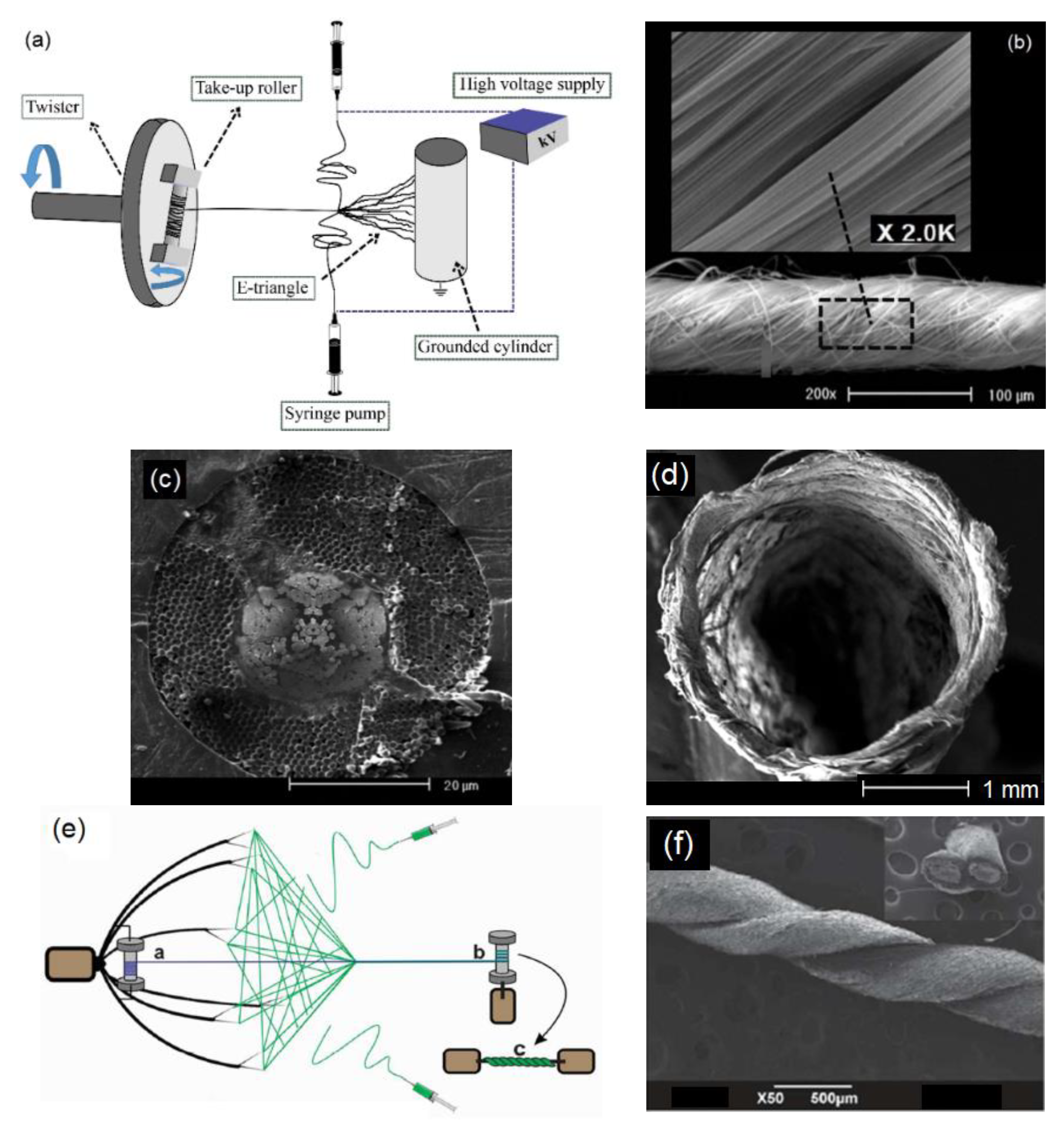
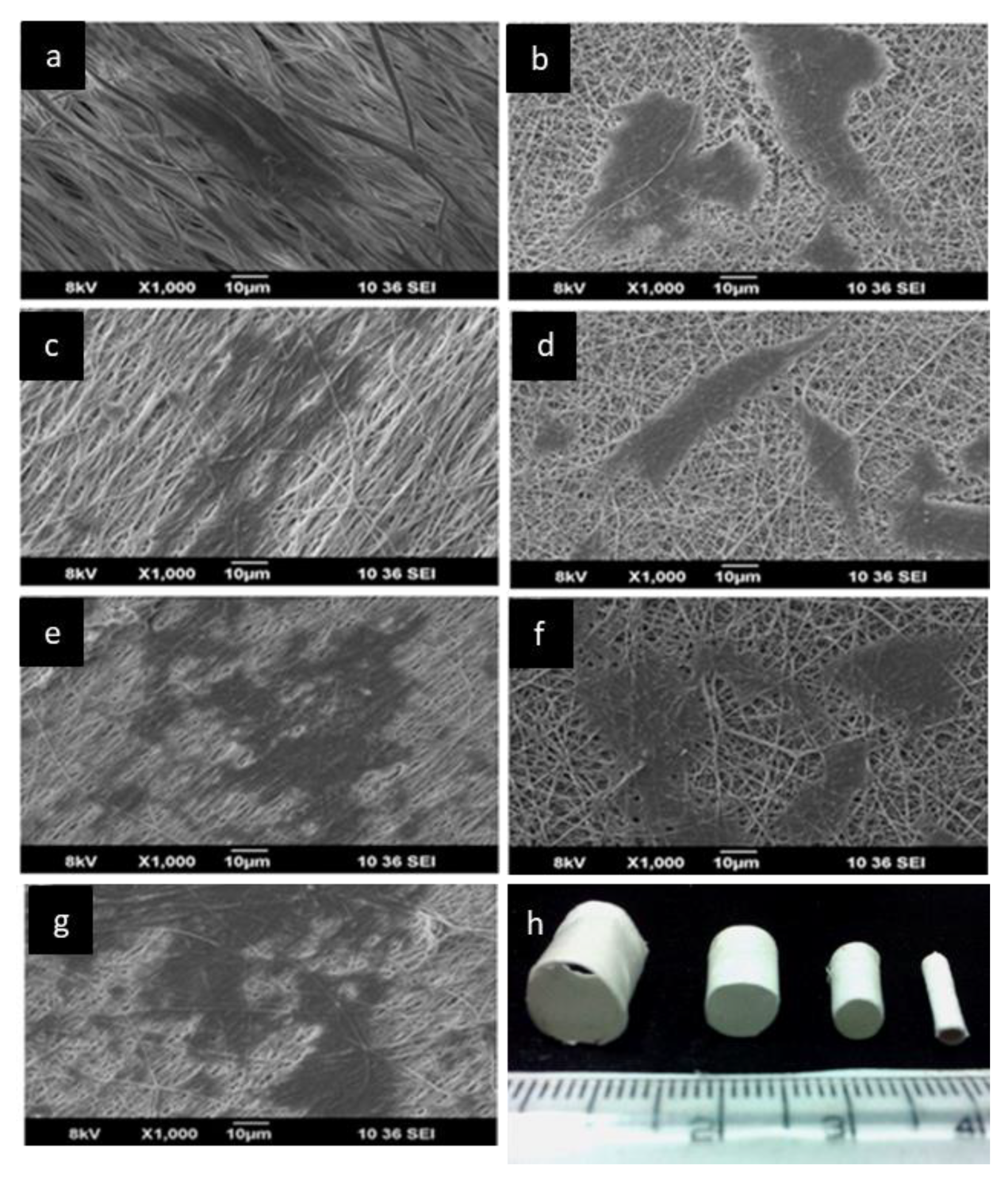
5.3. PLA-Based Electrospun Yarns
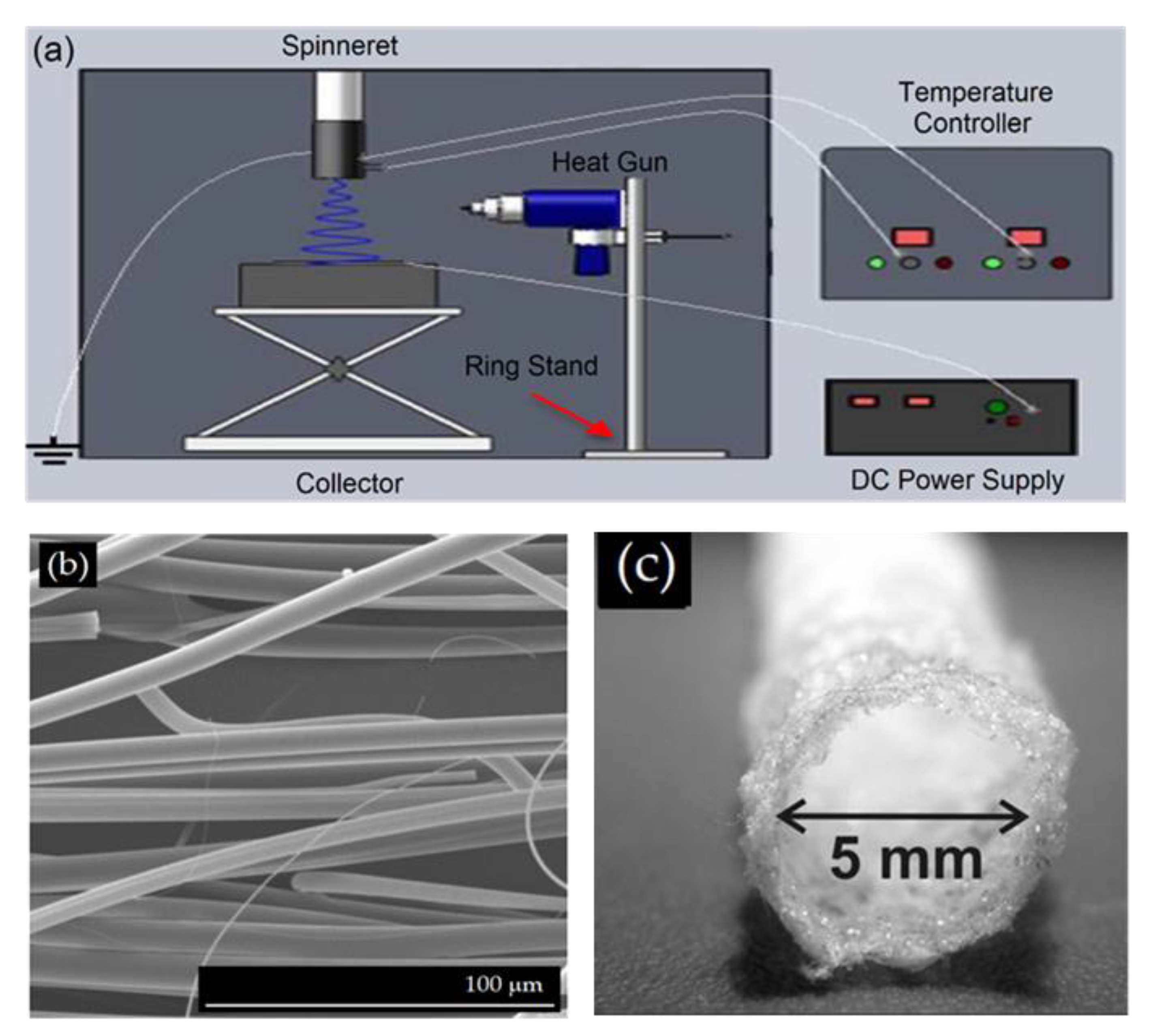
6. Melt Electrospinning
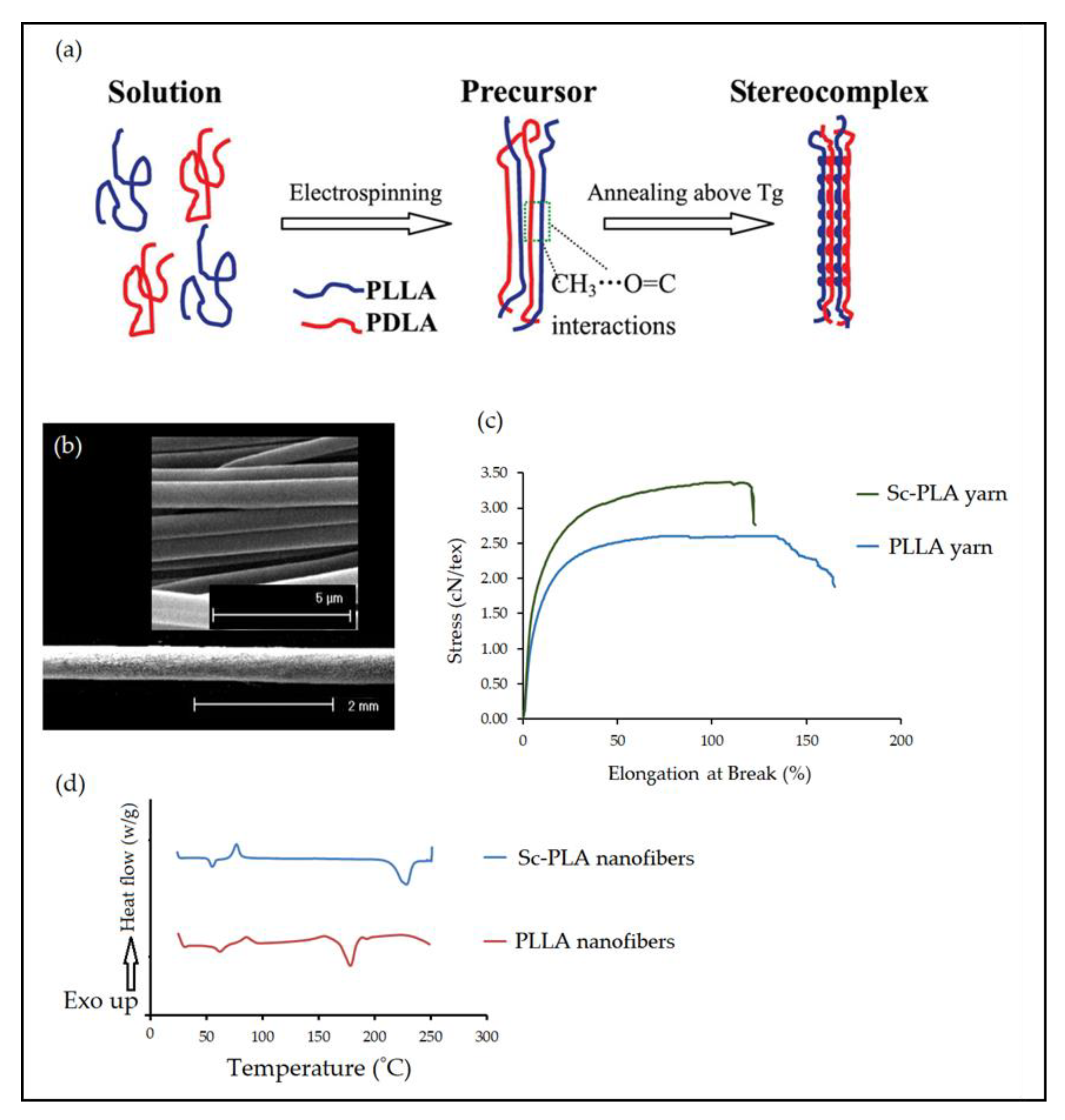
7. Electrospinning of PLA Stereocomplex Nanofibers
8. Biomedical Applications of PLA-Based Nanofibrous Structures
8.1. Wound Healing
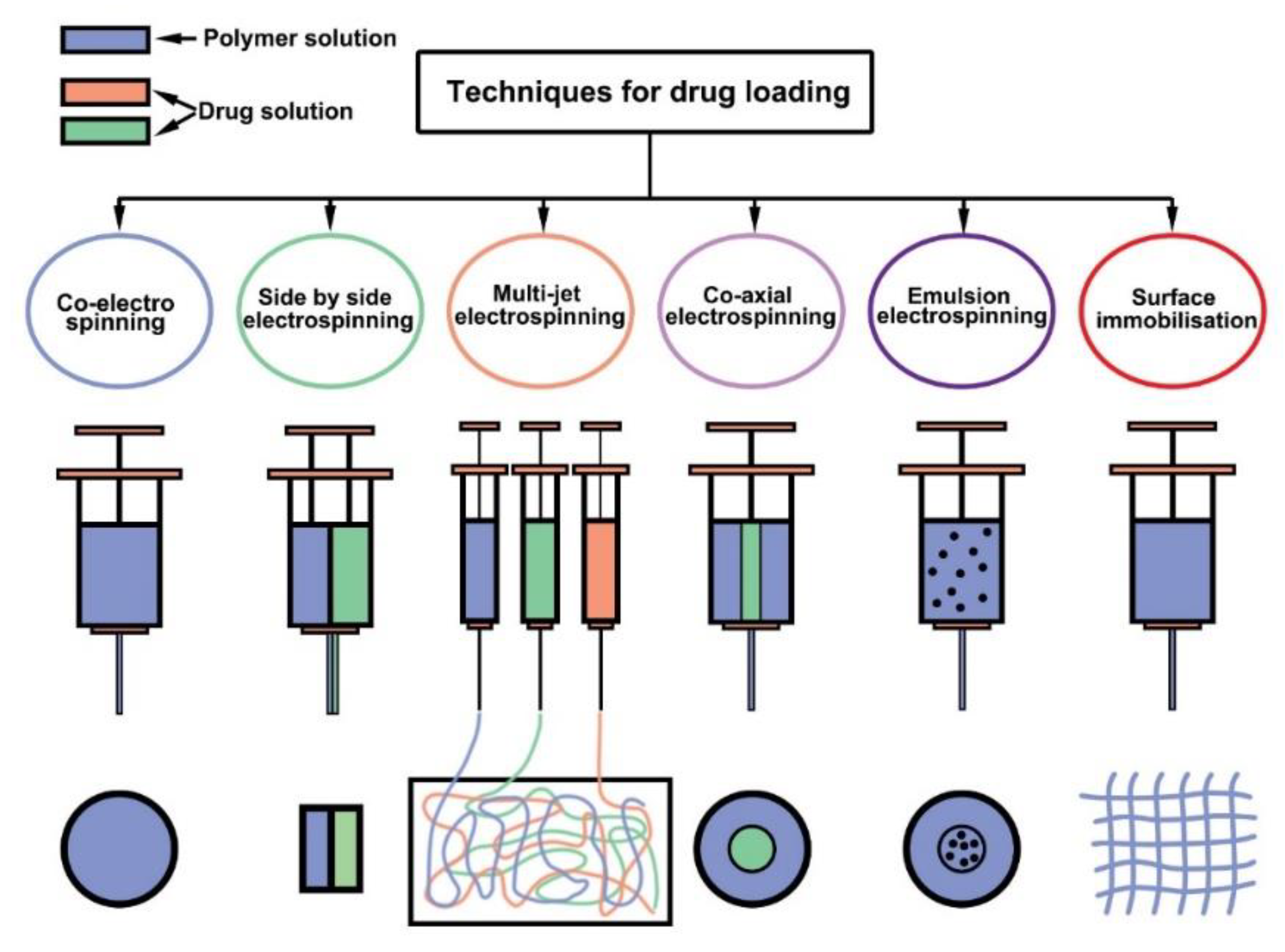
8.2. Drug Delivery
8.3. Tissue Engineering
8.3.1. PLA Electrospun Structures for Musculoskeletal Tissue Engineering
8.3.2. PLA Scaffolds for Neural Tissue Engineering
8.3.3. PLA Scaffolds for Cardiovascular Tissue Engineering
9. Conclusions and Future Trends
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, X.; Li, L.; Yang, D.; Nie, J.; Ma, G. Electrospun Core–Shell Fibrous 2D Scaffold with Biocompatible Poly(Glycerol Sebacate) and Poly-L-Lactic Acid for Wound Healing. Adv. Fiber Mater. 2020, 2, 105–117. [Google Scholar] [CrossRef] [Green Version]
- Alves, P.E.; Soares, B.G.; Lins, L.C.; Livi, S.; Santos, E.P. Controlled delivery of dexamethasone and betamethasone from PLA electrospun fibers: A comparative study. Eur. Polym. J. 2019, 117, 1–9. [Google Scholar] [CrossRef]
- Fattahi, F.-S.; Khoddami, A.; Avinc, O. Poly(lactic acid) (PLA) Nanofibers for Bone Tissue Engineering. J. Text. Polym. 2019, 7, 47. [Google Scholar]
- Azimi, B.; Maleki, H.; Zavagna, L.; De la Ossa, J.G.; Linari, S.; Lazzeri, A.; Danti, S. Bio-Based Electrospun Fibers for Wound Healing. J. Funct. Biomater. 2020, 11, 67. [Google Scholar] [CrossRef]
- Tyler, B.; Gullotti, D.; Mangraviti, A.; Utsuki, T.; Brem, H. Polylactic acid (PLA) controlled delivery carriers for biomedical applications. Adv. Drug Deliv. Rev. 2016, 107, 163–175. [Google Scholar] [CrossRef]
- Fang, Y.; Zhu, X.; Wang, N.; Zhang, X.; Yang, D.; Nie, J.; Ma, G. Biodegradable core-shell electrospun nanofibers based on PLA and γ-PGA for wound healing. Eur. Polym. J. 2019, 116, 30–37. [Google Scholar] [CrossRef]
- Bi, H.; Feng, T.; Li, B.; Han, Y. In Vitro and In Vivo Comparison Study of Electrospun PLA and PLA/PVA/SA Fiber Membranes for Wound Healing. Polymers 2020, 12, 839. [Google Scholar] [CrossRef] [Green Version]
- Maleki, H.; Gharehaghaji, A.A.; Toliyat, T.; Dijkstra, P.J. Drug release behavior of electrospun twisted yarns as implantable medical devices. Biofabrication 2016, 8, 35019. [Google Scholar] [CrossRef]
- Maleki, H.; Mathur, S.; Klein, A. Antibacterial Ag containing core-shell polyvinyl alcohol-poly(lactic acid) nanofibers for biomedical applications. Polym. Eng. Sci. 2020, 60, 1221–1230. [Google Scholar] [CrossRef]
- Li, W.; Fan, X.; Wang, X.; Shang, X.; Wang, Q.; Lin, J.; Hu, Z.; Li, Z. Stereocomplexed micelle formation through enantiomeric PLA-based Y-shaped copolymer for targeted drug delivery. Mater. Sci. Eng. C 2018, 91, 688–695. [Google Scholar] [CrossRef]
- Maleki, H.; Rahbar, R.S.; Nazir, A. Improvement of physical and mechanical properties of electrospun poly(lactic acid) nanofibrous structures. Iran. Polym. J. 2020, 29, 841–851. [Google Scholar] [CrossRef]
- Maleki, H.; Barani, H. Stereocomplex electrospun fibers from high molecular weight of poly(L-lactic acid) and poly(D-lactic acid). J. Polym. Eng. 2019, 40, 136–142. [Google Scholar] [CrossRef]
- Jiang, F.; Yan, D.; Lin, J.; Kong, H.; Yao, Q. Implantation of multiscale silk fibers on poly(lactic acid) fibrous membrane for biomedical applications. Mater. Today Chem. 2021, 21, 100494. [Google Scholar] [CrossRef]
- Deeraj, B.D.S.; Jayan, J.S.; Saritha, A.; Joseph, K. Electrospun biopolymer-based hybrid composites. In Hybrid Natural Fiber Composites; Elsevier: Amsterdam, The Netherlands, 2021; pp. 225–252. [Google Scholar]
- Pisani, S.; Genta, I.; Dorati, R.; Modena, T.; Chiesa, E.; Bruni, G.; Benazzo, M.; Conti, B. A Design of Experiment (DOE) approach to correlate PLA-PCL electrospun fibers diameter and mechanical properties for soft tissue regeneration purposes. J. Drug Deliv. Sci. Technol. 2022, 68, 103060. [Google Scholar] [CrossRef]
- Padmakumar, S.; Joseph, J.; Neppalli, M.H.; Mathew, S.E.; Nair, S.V.; Shankarappa, S.A.; Menon, D. Electrospun Polymeric Core–sheath Yarns as Drug Eluting Surgical Sutures. ACS Appl. Mater. Interfaces 2016, 8, 6925–6934. [Google Scholar] [CrossRef] [PubMed]
- Sharifisamani, E.; Mousazadegan, F.; Bagherzadeh, R.; Latifi, M. PEG-PLA-PCL based electrospun yarns with curcumin control release property as suture. Polym. Eng. Sci. 2020, 60, 1520–1529. [Google Scholar] [CrossRef]
- Awad, N.K.; Niu, H.; Ali, U.; Morsi, Y.S.; Lin, T. Electrospun fibrous scaffolds for small-diameter blood vessels: A review. Membranes 2018, 8, 15. [Google Scholar] [CrossRef] [Green Version]
- Sukchanta, A.; Kummanee, P.; Nuansing, W. Development and study on mechanical properties of small diameter artificial blood vessel by using electrospinning and 3d printing. Proc. J. Phys. Conf. Ser. 2021, 2145, 12037. [Google Scholar] [CrossRef]
- Hajikhani, M.; Emam-Djomeh, Z.; Askari, G. Fabrication and characterization of mucoadhesive bioplastic patch via coaxial polylactic acid (PLA) based electrospun nanofibers with antimicrobial and wound healing application. Int. J. Biol. Macromol. 2021, 172, 143–153. [Google Scholar] [CrossRef]
- Croitoru, A.-M.; Karaçelebi, Y.; Saatcioglu, E.; Altan, E.; Ulag, S.; Aydoğan, H.K.; Sahin, A.; Motelica, L.; Oprea, O.; Tihauan, B.-M. Electrically Triggered Drug Delivery from Novel Electrospun Poly(Lactic Acid)/Graphene Oxide/Quercetin Fibrous Scaffolds for Wound Dressing Applications. Pharmaceutics 2021, 13, 957. [Google Scholar] [CrossRef]
- Echeverría, C.; Muñoz-Bonilla, A.; Cuervo-Rodríguez, R.; López, D.; Fernández-García, M. Antibacterial PLA fibers containing Thiazolium groups as wound dressing materials. ACS Appl. Bio Mater. 2019, 2, 4714–4719. [Google Scholar] [CrossRef] [PubMed]
- Peranidze, K.; Safronova, T.V.; Kildeeva, N.R. Fibrous Polymer-Based Composites Obtained by Electrospinning for Bone Tissue Engineering. Polymers 2022, 14, 96. [Google Scholar] [CrossRef] [PubMed]
- Ciarfaglia, N.; Laezza, A.; Lods, L.; Lonjon, A.; Dandurand, J.; Pepe, A.; Bochicchio, B. Thermal and dynamic mechanical behavior of poly(lactic acid)(PLA)-based electrospun scaffolds for tissue engineering. J. Appl. Polym. Sci. 2021, 138, 51313. [Google Scholar] [CrossRef]
- Lopresti, F.; Pavia, F.C.; Ceraulo, M.; Capuana, E.; Brucato, V.; Ghersi, G.; Botta, L.; La Carrubba, V. Physical and biological properties of electrospun poly(d, l-lactide)/nanoclay and poly(d, l-lactide)/nanosilica nanofibrous scaffold for bone tissue engineering. J. Biomed. Mater. Res. Part A 2021, 109, 2120–2136. [Google Scholar] [CrossRef] [PubMed]
- Herrero-Herrero, M.; Gómez-Tejedor, J.-A.; Vallés-Lluch, A. PLA/PCL electrospun membranes of tailored fibres diameter as drug delivery systems. Eur. Polym. J. 2018, 99, 445–455. [Google Scholar] [CrossRef] [Green Version]
- Viscusi, G.; Lamberti, E.; Vittoria, V.; Gorrasi, G. Coaxial electrospun membranes of poly(ε-caprolactone)/poly(lactic acid) with reverse core-shell structures loaded with curcumin as tunable drug delivery systems. Polym. Adv. Technol. 2021, 32, 4005–4013. [Google Scholar] [CrossRef]
- Gritsch, L.; Conoscenti, G.; La Carrubba, V.; Nooeaid, P.; Boccaccini, A.R. Polylactide-based materials science strategies to improve tissue-material interface without the use of growth factors or other biological molecules. Mater. Sci. Eng. C 2019, 94, 1083–1101. [Google Scholar] [CrossRef]
- Ghafari, R.; Scaffaro, R.; Maio, A.; Gulino, E.F.; Lo Re, G.; Jonoobi, M. Processing-structure-property relationships of electrospun PLA-PEO membranes reinforced with enzymatic cellulose nanofibers. Polym. Test. 2020, 81, 106182. [Google Scholar] [CrossRef]
- Singhvi, M.S.; Zinjarde, S.S.; Gokhale, D.V. Polylactic acid: Synthesis and biomedical applications. J. Appl. Microbiol. 2019, 127, 1612–1626. [Google Scholar] [CrossRef] [Green Version]
- Singhvi, M.; Gokhale, D. Biomass to biodegradable polymer (PLA). RSC Adv. 2013, 3, 13558–13568. [Google Scholar] [CrossRef]
- Jin, F.L.; Hu, R.R.; Park, S.J. Improvement of thermal behaviors of biodegradable poly(lactic acid) polymer: A review. Compos. Part B Eng. 2019, 164, 287–296. [Google Scholar] [CrossRef]
- Bayer, I.S. Thermomechanical properties of polylactic acid-graphene composites: A state-of-the-art review for biomedical applications. Materials 2017, 10, 748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polonio-Alcalá, E.; Rabionet, M.; Gallardo, X.; Angelats, D.; Ciurana, J.; Ruiz-Martínez, S.; Puig, T. PLA electrospun scaffolds for three-dimensional triple-negative breast cancer cell culture. Polymers 2019, 11, 916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xue, J.; Wu, T.; Dai, Y.; Xia, Y. Electrospinning and Electrospun Nanofibers: Methods, Materials, and Applications. Chem. Rev. 2019, 119, 5298–5415. [Google Scholar] [CrossRef] [PubMed]
- Maleki, H.; Semnani Rahbar, R.; Saadatmand, M.M.; Barani, H. Physical and morphological characterisation of poly(L-lactide) acid-based electrospun fibrous structures: Tunning solution properties. Plast. Rubber Compos. 2018, 47, 438–446. [Google Scholar] [CrossRef]
- Maleki, H.; Gharehaghaji, A.; Moroni, L.; Dijkstra, P.J. Influence of the solvent type on the morphology and mechanical properties of electrospun PLLA yarns. Biofabrication 2013, 5, 035014. [Google Scholar] [CrossRef]
- Maleki, H.; Gharehaghaji, A.A.; Criscenti, G.; Moroni, L.; Dijkstra, P.J. The influence of process parameters on the properties of electrospun PLLA yarns studied by the response surface methodology. J. Appl. Polym. Sci. 2015, 132, 41388. [Google Scholar] [CrossRef]
- Scaffaro, R.; Lopresti, F.; Botta, L. Preparation, characterization and hydrolytic degradation of PLA/PCL co-mingled nanofibrous mats prepared via dual-jet electrospinning. Eur. Polym. J. 2017, 96, 266–277. [Google Scholar] [CrossRef]
- Lopresti, F.; Carfì Pavia, F.; Vitrano, I.; Kersaudy-Kerhoas, M.; Brucato, V.; La Carrubba, V. Effect of hydroxyapatite concentration and size on morpho-mechanical properties of PLA-based randomly oriented and aligned electrospun nanofibrous mats. J. Mech. Behav. Biomed. Mater. 2020, 101, 103449. [Google Scholar] [CrossRef]
- Scaffaro, R.; Lopresti, F. Properties-morphology relationships in electrospun mats based on polylactic acid and graphene nanoplatelets. Compos. Part A Appl. Sci. Manuf. 2018, 108, 23–29. [Google Scholar] [CrossRef]
- Alharbi, H.F.; Luqman, M.; Khalil, K.A.; Elnakady, Y.A.; Abd-Elkader, O.H.; Rady, A.M.; Alharthi, N.H.; Karim, M.R. Fabrication of core-shell structured nanofibers of poly(lactic acid) and poly(vinyl alcohol) by coaxial electrospinning for tissue engineering. Eur. Polym. J. 2018, 98, 483–491. [Google Scholar] [CrossRef]
- Da Silva, T.N.; Gonçalves, R.P.; Rocha, C.L.; Archanjo, B.S.; Barboza, C.A.G.; Pierre, M.B.R.; Reynaud, F.; de Souza Picciani, P.H. Controlling burst effect with PLA/PVA coaxial electrospun scaffolds loaded with BMP-2 for bone guided regeneration. Mater. Sci. Eng. C 2019, 97, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Zhou, R.; Zhou, F.; Streubel, P.N.; Chen, S.; Duan, B. Electrospun thymosin Beta-4 loaded PLGA/PLA nanofiber/ microfiber hybrid yarns for tendon tissue engineering application. Mater. Sci. Eng. C 2020, 106, 110268. [Google Scholar] [CrossRef] [PubMed]
- Maleki, H.; Gharehaghaji, A.A.; Dijkstra, P.J. Electrospinning of continuous poly(L-lactide) yarns: Effect of twist on the morphology, thermal properties and mechanical behavior. J. Mech. Behav. Biomed. Mater. 2017, 71, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Habibi Jouybari, M.; Hosseini, S.; Mahboobnia, K.; Boloursaz, L.A.; Moradi, M.; Irani, M. Simultaneous controlled release of 5-FU, DOX and PTX from chitosan/PLA/5-FU/g-C3N4-DOX/g-C3N4-PTX triaxial nanofibers for breast cancer treatment in vitro. Colloids Surf. B Biointerfaces 2019, 179, 495–504. [Google Scholar] [CrossRef]
- Huang, C.; Thomas, N.L. Fabricating porous poly(lactic acid) fibres via electrospinning. Eur. Polym. J. 2018, 99, 464–476. [Google Scholar] [CrossRef] [Green Version]
- Asghar, A.L.I.; Jeddi, A. Fabrication and characterization of hollow electrospun PLA structure through a modified electrospinning method applicable as vascular graft. Bull. Mater. Sci. 2021, 44, 158. [Google Scholar] [CrossRef]
- Qi, Z.; Yu, H.; Chen, Y.; Zhu, M. Highly porous fibers prepared by electrospinning a ternary system of nonsolvent/solvent/poly(l-lactic acid). Mater. Lett. 2009, 63, 415–418. [Google Scholar] [CrossRef]
- Natarajan, L.; New, J.; Dasari, A.; Yu, S.; Manan, M.A. Surface morphology of electrospun PLA fibers: Mechanisms of pore formation. RSC Adv. 2014, 4, 44082–44088. [Google Scholar] [CrossRef]
- Li, L.; Hashaikeh, R.; Arafat, H.A. Development of eco-efficient micro-porous membranes via electrospinning and annealing of poly(lactic acid). J. Membr. Sci. 2013, 436, 57–67. [Google Scholar] [CrossRef]
- Li, Y.; Lim, C.T.; Kotaki, M. Study on structural and mechanical properties of porous PLA nanofibers electrospun by channel-based electrospinning system. Polymer 2015, 56, 572–580. [Google Scholar] [CrossRef]
- Rezabeigi, E.; Sta, M.; Swain, M.; McDonald, J.; Demarquette, N.R.; Drew, R.A.L.; Wood-Adams, P.M. Electrospinning of porous polylactic acid fibers during nonsolvent induced phase separation. J. Appl. Polym. Sci. 2017, 134, 44862. [Google Scholar] [CrossRef]
- Li, T.; Ding, X.; Tian, L.; Hu, J.; Yang, X.; Ramakrishna, S. The control of beads diameter of bead-on-string electrospun nanofibers and the corresponding release behaviors of embedded drugs. Mater. Sci. Eng. C 2017, 74, 471–477. [Google Scholar] [CrossRef]
- Maleki, H.; Barani, H. Morphological and mechanical properties of drawn poly(l-lactide) electrospun twisted yarns. Polym. Eng. Sci. 2017, 58, 1091–1096. [Google Scholar] [CrossRef]
- Banitaba, S.N.; Amini, G.; Gharehaghaji, A.A.; Jeddi, A.A.A. Fabrication of hollow nanofibrous structures using a triple layering method for vascular scaffold applications. Fibers Polym. 2017, 18, 2342–2348. [Google Scholar] [CrossRef]
- Li, X.; Liu, Y.; Peng, H.; Ma, X.; Fong, H. Effects of hot airflow on macromolecular orientation and crystallinity of melt electrospun poly(L-lactic acid) fibers. Mater. Lett. 2016, 176, 194–198. [Google Scholar] [CrossRef]
- Mazalevska, O.; Struszczyk, M.H.; Krucinska, I. Design of vascular prostheses by melt electrospinning—Structural characterizations. J. Appl. Polym. Sci. 2013, 129, 779–792. [Google Scholar] [CrossRef]
- Nazari, T.; Garmabi, H. The effects of processing parameters on the morphology of PLA/PEG melt-electrospun fibers. Polym. Int. 2017, 67, 178–188. [Google Scholar] [CrossRef]
- Yu, S.-X.; Zheng, J.; Yan, X.; Wang, X.-X.; Nie, G.-D.; Tan, Y.-Q.; Zhang, J.; Sui, K.-Y.; Long, Y.-Z. Morphology control of PLA microfibers and spheres via melt electrospinning. Mater. Res. Express 2018, 5, 45019. [Google Scholar] [CrossRef]
- Lee, H.; Ahn, S.; Choi, H.; Cho, D.; Kim, G. Fabrication, characterization, and in vitro biological activities of melt-electrospun PLA micro/nanofibers for bone tissue regeneration. J. Mater. Chem. B 2013, 1, 3670–3677. [Google Scholar] [CrossRef]
- Chrzanowska, O.; Struszczyk, M.H.; Krucinska, I. Small diameter tubular structure design using solvent-free textile techniques. J. Appl. Polym. Sci. 2014, 131, 40147. [Google Scholar] [CrossRef]
- Bai, H.; Deng, S.; Bai, D.; Zhang, Q.; Fu, Q. Recent Advances in Processing of Stereocomplex-Type Polylactide. Macromol. Rapid Commun. 2017, 38, 1700454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurokawa, N.; Hotta, A. Thermomechanical properties of highly transparent self-reinforced polylactide composites with electrospun stereocomplex polylactide nanofibers. Polymer 2018, 153, 214–222. [Google Scholar] [CrossRef]
- Ikada, Y.; Jamshidi, K.; Tsuji, H.; Hyon, S.H. Stereocomplex formation between enantiomeric poly(lactides). Macromolecules 1987, 20, 904–906. [Google Scholar] [CrossRef]
- Tsuji, H.; Nakano, M.; Hashimoto, M.; Takashima, K.; Katsura, S.; Mizuno, A. Electrospinning of Poly(lactic acid) Stereocomplex Nanofibers. Biomacromolecules 2006, 7, 3316–3320. [Google Scholar] [CrossRef]
- Paneva, D.; Spasova, M.; Stoyanova, N.; Manolova, N.; Rashkov, I. Electrospun fibers from polylactide-based stereocomplex: Why? Int. J. Polym. Mater. Polym. Biomater. 2019, 70, 270–286. [Google Scholar] [CrossRef]
- Jing, Y.; Quan, C.; Liu, B.; Jiang, Q.; Zhang, C. A Mini Review on the Functional Biomaterials Based on Poly(lactic acid) Stereocomplex. Polym. Rev. 2016, 56, 262–286. [Google Scholar] [CrossRef]
- Ishii, D.; Ying, T.H.; Mahara, A.; Yamaoka, T.; Lee, W.; Iwata, T.; Murakami, S. In Vivo Tissue Response and Degradation Behavior of PLLA and Stereocomplexed PLA Nanofibers In Vivo Tissue Response and Degradation Behavior of PLLA and Stereocomplexed PLA Nanofibers. Biomacromolecules 2009, 10, 237–242. [Google Scholar] [CrossRef]
- Moradkhannejhad, L.; Abdouss, M.; Nikfarjam, N.; Shahriari, M.H.; Heidary, V. The effect of molecular weight and content of PEG on in vitro drug release of electrospun curcumin loaded PLA/PEG nanofibers. J. Drug Deliv. Sci. Technol. 2020, 56, 101554. [Google Scholar] [CrossRef]
- Fattahi, F.S.; Khoddami, A.; Avinc, O. Poly(Lactic Acid) Nano-fibers as Drug-delivery Systems: Opportunities and Challenges. Nanomed. Res. J. 2019, 4, 130–140. [Google Scholar] [CrossRef]
- Santoro, M.; Shah, S.R.; Walker, J.L.; Mikos, A.G. Poly(lactic acid) nanofibrous scaffolds for tissue engineering. Adv. Drug Deliv. Rev. 2016, 107, 206–212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Xu, H.; Zhang, M.; Yu, D.G. Electrospun Medicated Nanofibers for Wound Healing: Review. Membranes 2021, 11, 770. [Google Scholar] [CrossRef] [PubMed]
- Pankongadisak, P.; Sangklin, S.; Chuysinuan, P.; Suwantong, O.; Supaphol, P. The use of electrospun curcumin-loaded poly(L-lactic acid) fiber mats as wound dressing materials. J. Drug Deliv. Sci. Technol. 2019, 53, 101121. [Google Scholar] [CrossRef]
- Nguyen, T.T.T.; Ghosh, C.; Hwang, S.G.; Tran, L.D.; Park, J.S. Characteristics of curcumin-loaded poly(lactic acid) nanofibers for wound healing. J. Mater. Sci. 2013, 48, 7125–7133. [Google Scholar] [CrossRef]
- Li, J.; Hu, Y.; He, T.; Huang, M.; Zhang, X.; Yuan, J.; Wei, Y.; Dong, X.; Liu, W.; Ko, F.; et al. Electrospun Sandwich-Structure Composite Membranes for Wound Dressing Scaffolds with High Antioxidant and Antibacterial Activity. Macromol. Mater. Eng. 2017, 303, 1700270. [Google Scholar] [CrossRef]
- Ilomuanya, M.O.; Adebona, A.C.; Wang, W.; Sowemimo, A.; Eziegbo, C.L.; Silva, B.O.; Adeosun, S.O.; Joubert, E.; De Beer, D. Development and characterization of collagen-based electrospun scaffolds containing silver sulphadiazine and Aspalathus linearis extract for potential wound healing applications. Appl. Sci. 2020, 2, 881. [Google Scholar] [CrossRef] [Green Version]
- Cui, S.; Sun, X.; Li, K.; Gou, D.; Zhou, Y.; Hu, J.; Liu, Y. Polylactide nanofibers delivering doxycycline for chronic wound treatment. Mater. Sci. Eng. C 2019, 104, 109745. [Google Scholar] [CrossRef]
- Zhang, S.; Ye, J.; Sun, Y.; Kang, J.; Liu, J.; Wang, Y.; Li, Y.; Zhang, L.; Ning, G. Electrospun fibrous mat based on silver (I) metal-organic frameworks-polylactic acid for bacterial killing and antibiotic-free wound dressing. Chem. Eng. J. 2020, 390, 124523. [Google Scholar] [CrossRef]
- Ghorbani, S.; Eyni, H.; Tiraihi, T.; Asl, L.S.; Soleimani, M.; Atashi, A.; Beiranvand, S.P.; Warkiani, M.E. Combined effects of 3D bone marrow stem cell-seeded wet-electrospun polylactic acid scaffolds on full-thickness skin wound healing. Int. J. Polym. Mater. Polym. Biomater. 2018, 67, 905–912. [Google Scholar] [CrossRef]
- Han, Y.; Jiang, Y.; Li, Y.; Wang, M.; Fan, T.; Liu, M.; Ke, Q.; Xu, H.; Yi, Z. An aligned porous electrospun fibrous scaffold with embedded asiatic acid for accelerating diabetic wound healing. J. Mater. Chem. B 2019, 7, 6125–6138. [Google Scholar] [CrossRef]
- Mouro, C.; Gomes, A.P.; Gouveia, I.C. Double-layer PLLA/PEO_Chitosan nanofibrous mats containing Hypericum perforatum L. as an effective approach for wound treatment. Polym. Adv. Technol. 2021, 32, 1493–1506. [Google Scholar] [CrossRef]
- Fan, T.; Daniels, R. Preparation and Characterization of Electrospun Polylactic Acid (PLA) Fiber Loaded with Birch Bark Triterpene Extract for Wound Dressing. AAPS PharmSciTech 2021, 22, 205. [Google Scholar] [CrossRef] [PubMed]
- Mohiti-Asli, M.; Saha, S.; Murphy, S.V.; Gracz, H.; Pourdeyhimi, B.; Atala, A.; Loboa, E.G. Ibuprofen loaded PLA nanofibrous scaffolds increase proliferation of human skin cells in vitro and promote healing of full thickness incision wounds in vivo. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015, 105, 327–339. [Google Scholar] [CrossRef]
- Li, H.; Williams, G.R.; Wu, J.; Lv, Y.; Sun, X.; Wu, H.; Zhu, L.M. Thermosensitive nanofibers loaded with ciprofloxacin as antibacterial wound dressing materials. Int. J. Pharm. 2017, 517, 135–147. [Google Scholar] [CrossRef]
- Li, W.; Tan, X.; Luo, T.; Shi, Y.; Yang, Y.; Liu, L. Preparation and characterization of electrospun PLA/PU bilayer nanofibrous membranes for controlled drug release applications. Integr. Ferroelectr. 2017, 179, 104–119. [Google Scholar] [CrossRef]
- Li, W.; Wu, D.; Zhu, S.; Liu, Z.; Luo, B.; Lu, L.; Zhou, C. Sustained release of plasmid DNA from PLLA/POSS nanofibers for angiogenic therapy. Chem. Eng. J. 2019, 365, 270–281. [Google Scholar] [CrossRef]
- Zou, F.; Sun, X.; Wang, X. Elastic, hydrophilic and biodegradable poly(1, 8-octanediol-co-citric acid)/polylactic acid nanofibrous membranes for potential wound dressing applications. Polym. Degrad. Stab. 2019, 166, 163–173. [Google Scholar] [CrossRef]
- Pedersbæk, D.; Frantzen, M.T.; Fojan, P. Electrospinning of Core-Shell Fibers for Drug Release Systems. J. Self-Assem. Mol. Electron. 2017, 5, 17–30. [Google Scholar] [CrossRef] [Green Version]
- Yang, C.; Yan, Z.; Lian, Y.; Wang, J.; Zhang, K. Graphene oxide coated shell-core structured chitosan/PLLA nanofibrous scaffolds for wound dressing. J. Biomater. Sci. Polym. Ed. 2020, 31, 622–641. [Google Scholar] [CrossRef]
- Augustine, R.; Zahid, A.A.; Hasan, A.; Wang, M.; Webster, T.J. CTGF loaded electrospun dual porous core-shell membrane for diabetic wound healing. Int. J. Nanomed. 2019, 14, 8573. [Google Scholar] [CrossRef] [Green Version]
- Pilehvar-Soltanahmadi, Y.; Dadashpour, M.; Mohajeri, A.; Fattahi, A.; Sheervalilou, R.; Zarghami, N. An Overview on Application of Natural Substances Incorporated with Electrospun Nanofibrous Scaffolds to Development of Innovative Wound Dressings. Mini-Rev. Med. Chem. 2017, 18, 414–427. [Google Scholar] [CrossRef] [PubMed]
- Kontogiannopoulos, K.N.; Assimopoulou, A.N.; Tsivintzelis, I.; Panayiotou, C.; Papageorgiou, V.P. Electrospun fiber mats containing shikonin and derivatives with potential biomedical applications. Int. J. Pharm. 2011, 409, 216–228. [Google Scholar] [CrossRef] [PubMed]
- Pillay, V.; Dott, C.; Choonara, Y.E.; Tyagi, C.; Tomar, L.; Kumar, P.; du Toit, L.C.; Ndesendo, V.M.K. A Review of the Effect of Processing Variables on the Fabrication of Electrospun Nanofibers for Drug Delivery Applications. J. Nanomater. 2013, 2013, 22. [Google Scholar] [CrossRef] [Green Version]
- Fayemi, O.E.; Ekennia, A.C.; Katata-Seru, L.; Ebokaiwe, A.P.; Ijomone, O.M.; Onwudiwe, D.C.; Ebenso, E.E. Antimicrobial and Wound Healing Properties of Polyacrylonitrile-Moringa Extract Nanofibers. ACS Omega 2018, 3, 4791–4797. [Google Scholar] [CrossRef] [PubMed]
- Felgueiras, H.P.; Amorim, M.T.P. Functionalization of electrospun polymeric wound dressings with antimicrobial peptides. Colloids Surf. B Biointerfaces 2017, 156, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Chereddy, K.K.; Lopes, A.; Koussoroplis, S.; Payen, V.; Moia, C.; Zhu, H.; Sonveaux, P.; Carmeliet, P.; des Rieux, A.; Vandermeulen, G.; et al. Combined effects of PLGA and vascular endothelial growth factor promote the healing of non-diabetic and diabetic wounds. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1975–1984. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Nielsen, L.H.; Kłodzińska, S.N.; Nielsen, H.M.; Qu, H.; Christensen, L.P.; Rantanen, J.; Yang, M. Ciprofloxacin-loaded sodium alginate/poly(lactic-co-glycolic acid) electrospun fibrous mats for wound healing. Eur. J. Pharm. Biopharm. 2018, 123, 42–49. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Qiu, Y.; Wang, H.; Chen, Y.; Jin, S.; Chen, S. Preparation of Nanofibers with Renewable Polymers and Their Application in Wound Dressing. Int. J. Polym. Sci. 2016, 2016, 4672839. [Google Scholar] [CrossRef] [Green Version]
- Thenmozhi, S.; Dharmaraj, N.; Kadirvelu, K.; Kim, H.Y. Electrospun nanofibers: New generation materials for advanced applications. Mater. Sci. Eng. B 2017, 217, 36–48. [Google Scholar] [CrossRef]
- Tocco, I.; Zavan, B.; Bassetto, F.; Vindigni, V. Nanotechnology-based therapies for skin wound regeneration. J. Nanomater. 2012, 2012, 714134. [Google Scholar] [CrossRef] [Green Version]
- Pásztor, N.; Rédai, E.; Szabó, Z.-I.; Sipos, E. Preparation and Characterization of Levofloxacin-Loaded Nanofibers as Potential Wound Dressings. Acta Med. Marisiensis 2017, 63, 66–69. [Google Scholar] [CrossRef] [Green Version]
- Scaffaro, R.; Lopresti, F.; D’Arrigo, M.; Marino, A.; Nostro, A. Efficacy of poly(lactic acid)/carvacrol electrospun membranes against Staphylococcus aureus and Candida albicans in single and mixed cultures. Appl. Microbiol. Biotechnol. 2018, 102, 4171–4181. [Google Scholar] [CrossRef] [PubMed]
- Scaffaro, R.; Lopresti, F.; Marino, A.; Nostro, A. Antimicrobial additives for poly(lactic acid) materials and their applications: Current state and perspectives. Appl. Microbiol. Biotechnol. 2018, 102, 7739–7756. [Google Scholar] [CrossRef]
- Kenawy, E.-R.; Bowlin, G.L.; Mansfield, K.; Layman, J.; Simpson, D.G.; Sanders, E.H.; Wnek, G.E. Release of tetracycline hydrochloride from electrospun poly(ethylene-co-vinylacetate), poly(lactic acid), and a blend. J. Control. Release 2002, 81, 57–64. [Google Scholar] [CrossRef]
- Mao, Z.; Li, J.; Huang, W.; Jiang, H.; Zimba, B.L.; Chen, L.; Wan, J.; Wu, Q. Preparation of poly(lactic acid)/graphene oxide nanofiber membranes with different structures by electrospinning for drug delivery. RSC Adv. 2018, 8, 16619–16625. [Google Scholar] [CrossRef] [Green Version]
- Yuan, Y.; Choi, K.; Choi, S.O.; Kim, J. Early stage release control of an anticancer drug by drug-polymer miscibility in a hydrophobic fiber-based drug delivery system. RSC Adv. 2018, 8, 19791–19803. [Google Scholar] [CrossRef] [Green Version]
- Doustgani, A. Doxorubicin release from optimized electrospun polylactic acid nanofibers. J. Ind. Text. 2016, 47, 71–88. [Google Scholar] [CrossRef]
- Hrib, J.; Sirc, J.; Hobzova, R.; Hampejsova, Z.; Bosakova, Z.; Munzarova, M.; Michalek, J. Nanofibers for drug delivery—Incorporation and release of model molecules, influence of molecular weight and polymer structure. Beilstein J. Nanotechnol. 2015, 6, 1939–1945. [Google Scholar] [CrossRef] [Green Version]
- Bae, H.; Lee, J. Assembly of particle-fiber composites by electrohydrodynamic jetting using counter-charged nozzles: Independent release control. J. Ind. Eng. Chem. 2016, 40, 99–105. [Google Scholar] [CrossRef]
- Wu, S.; Wu, J.; Yue, J.; To, M.K.T.; Pan, H.; Lu, W.W.; Zhao, X. Poly(d,l-lactic acid) electrospun fibers with tunable surface nanotopography for modulating drug release profiles. Mater. Lett. 2015, 161, 716–719. [Google Scholar] [CrossRef]
- Sóti, P.L.; Nagy, Z.K.; Serneels, G.; Vajna, B.; Farkas, A.; Van Der Gucht, F.; Fekete, P.; Vigh, T.; Wagner, I.; Balogh, A.; et al. Preparation and comparison of spray dried and electrospun bioresorbable drug delivery systems. Eur. Polym. J. 2015, 68, 671–679. [Google Scholar] [CrossRef] [Green Version]
- Yaru, W.; Lan, X.; Jianhua, S.; Chenxu, F. Preparation, Characterization and Drug Release of Salicylic Acid Loaded Porous Electrospun Nanofibers. Recent Pat. Nanotechnol. 2018, 12, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Chen, G.; Shuler, F.D.; Wang, C.H.; Xie, J. Local Sustained Delivery of 25-Hydroxyvitamin D3 for Production of Antimicrobial Peptides. Pharm. Res. 2015, 32, 2851–2862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adomavičiute, E.; Pupkevičiute, S.; Juškaite, V.; Žilius, M.; Stanys, S.; Pavilonis, A.; Briedis, V. Formation and investigation of electrospun PLA materials with propolis extracts and silver nanoparticles for biomedical applications. J. Nanomater. 2017, 2017, 8612819. [Google Scholar] [CrossRef] [Green Version]
- Sudakaran, S.V.; Venugopal, J.R.; Vijayakumar, G.P.; Abisegapriyan, S.; Grace, A.N.; Ramakrishna, S. Sequel of MgO nanoparticles in PLACL nanofibers for anti-cancer therapy in synergy with curcumin/β-cyclodextrin. Mater. Sci. Eng. C 2017, 17, 620–628. [Google Scholar] [CrossRef]
- Birhanu, G.; Tanha, S.; Akbari Javar, H.; Seyedjafari, E.; Zandi-Karimi, A.; Kiani Dehkordi, B. Dexamethasone loaded multi-layer poly-l-lactic acid/pluronic P123 composite electrospun nanofiber scaffolds for bone tissue engineering and drug delivery. Pharm. Dev. Technol. 2018, 24, 338–347. [Google Scholar] [CrossRef]
- Jiang, S.; Lv, J.; Ding, M.; Li, Y.; Wang, H.; Jiang, S. Release behavior of tetracycline hydrochloride loaded chitosan/poly(lactic acid) antimicrobial nanofibrous membranes. Mater. Sci. Eng. C 2016, 59, 86–91. [Google Scholar] [CrossRef]
- Nazari, T.; Moghaddam, A.B.; Davoodi, Z. Optimized polylactic acid/polyethylene glycol (PLA/PEG) electrospun fibrous scaffold for drug delivery: Effect of graphene oxide on the cefixime release mechanism. Mater. Res. Express 2019, 6, 115351. [Google Scholar] [CrossRef]
- Ma, H.; Wu, W.; Zhang, H.; Chen, G.; Han, W.; Cao, J. Preparation, structure, and release behavior of PLLA/silk fibroin micro-fiber films with controlled structure. J. Text. Inst. 2018, 110, 298–301. [Google Scholar] [CrossRef]
- Cai, N.; Han, C.; Luo, X.; Chen, G.; Dai, Q.; Yu, F. Fabrication of Core/Shell Nanofibers with Desirable Mechanical and Antibacterial Properties by Pickering Emulsion Electrospinning. Macromol. Mater. Eng. 2017, 302, 1–10. [Google Scholar] [CrossRef]
- Zhang, H.; Niu, Q.; Wang, N.; Nie, J.; Ma, G. Thermo-sensitive drug controlled release PLA core/PNIPAM shell fibers fabricated using a combination of electrospinning and UV photo-polymerization. Eur. Polym. J. 2015, 71, 440–450. [Google Scholar] [CrossRef]
- Zhu, T.; Yang, C.; Chen, S.; Li, W.; Lou, J.; Wang, J. A facile approach to prepare shell/core nanofibers for drug controlled release. Mater. Lett. 2015, 150, 52–54. [Google Scholar] [CrossRef]
- Azimi, B.; Thomas, L.; Fusco, A.; Kalaoglu-Altan, O.I.; Basnett, P.; Cinelli, P.; de Clerck, K.; Roy, I.; Donnarumma, G.; Coltelli, M.B.; et al. Electrosprayed Chitin Nanofibril/Electrospun Polyhydroxyalkanoate Fiber Mesh as Functional Nonwoven for Skin Application. J. Funct. Biomater. 2020, 11, 62. [Google Scholar] [CrossRef] [PubMed]
- Amini, A.R.; Laurencin, C.T.; Nukavarapu, S.P. Bone Tissue Engineering: Recent Advances and Challenges. Crit. Rev. Biomed. Eng. 2012, 40, 363. [Google Scholar] [CrossRef] [Green Version]
- Azimi, B.; Milazzo, M.; Lazzeri, A.; Berrettini, S.; Uddin, M.J.; Qin, Z.; Buehler, M.J.; Danti, S. Electrospinning Piezoelectric Fibers for Biocompatible Devices. Adv. Healthc. Mater. 2020, 9, e1901287. [Google Scholar] [CrossRef]
- Puppi, D.; Chiellini, F.; Piras, A.M.; Chiellini, E. Polymeric materials for bone and cartilage repair. Prog. Polym. Sci. 2010, 35, 403–440. [Google Scholar] [CrossRef]
- Holzwarth, J.M.; Ma, P.X. Biomimetic nanofibrous scaffolds for bone tissue engineering. Biomaterials 2011, 32, 9622–9629. [Google Scholar] [CrossRef] [Green Version]
- Azimi, B.; Bafqi, M.S.S.; Fusco, A.; Ricci, C.; Gallone, G.; Bagherzadeh, R.; Donnarumma, G.; Uddin, M.J.; Latifi, M.; Lazzeri, A.; et al. Electrospun ZnO/Poly(Vinylidene Fluoride-Trifluoroethylene) Scaffolds for Lung Tissue Engineering. Tissue Eng. Part A 2020, 26, 1312–1331. [Google Scholar] [CrossRef]
- Xie, J.; Shen, H.; Yuan, G.; Lin, K.; Su, J. The effects of alignment and diameter of electrospun fibers on the cellular behaviors and osteogenesis of BMSCs. Mater. Sci. Eng. C 2021, 120, 111787. [Google Scholar] [CrossRef]
- Rattier, B.D.; Hoffman, A.S.; Schoen, F.J.; Lemons, J.E. Biomaterials Science: An Introduction to Materials in Medicine. J. Clin. Eng. 1996, 22, 26. [Google Scholar] [CrossRef]
- Lu, Z.; Wang, W.; Zhang, J.; Bártolo, P.; Gong, H.; Li, J. Electrospun highly porous poly(L-lactic acid)-dopamine-SiO2 fibrous membrane for bone regeneration. Mater. Sci. Eng. C 2020, 117, 111359. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, M.; Alibolandi, M.; Abnous, K.; Salmasi, Z.; Jaafari, M.R.; Ramezani, M. Fabrication of hybrid scaffold based on hydroxyapatite-biodegradable nanofibers incorporated with liposomal formulation of BMP-2 peptide for bone tissue engineering. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 1987–1997. [Google Scholar] [CrossRef] [PubMed]
- Ye, K.; Liu, D.; Kuang, H.; Cai, J.; Chen, W.; Sun, B.; Xia, L.; Fang, B.; Morsi, Y.; Mo, X. Three-dimensional electrospun nanofibrous scaffolds displaying bone morphogenetic protein-2-derived peptides for the promotion of osteogenic differentiation of stem cells and bone regeneration. J. Colloid Interface Sci. 2019, 534, 625–636. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Cheng, R.; Sun, Z.; Su, W.; Pan, G.; Zhao, S.; Zhao, J.; Cui, W. Flexible bipolar nanofibrous membranes for improving gradient microstructure in tendon-to-bone healing. Acta Biomater. 2017, 61, 204–216. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.K.; Dutta, S.D.; Hexiu, J.; Ganguly, K.; Lim, K.T. Bioactive electrospun nanocomposite scaffolds of poly(lactic acid)/cellulose nanocrystals for bone tissue engineering. Int. J. Biol. Macromol. 2020, 162, 1429–1441. [Google Scholar] [CrossRef]
- Xu, Z.; Liu, P.; Li, H.; Zhang, M.; Wu, Q. In vitro study on electrospun lecithin-based poly(L-lactic acid) scaffolds and their biocompatibility. J. Biomater. Sci. Polym. Ed. 2020, 31, 2285–2298. [Google Scholar] [CrossRef]
- Wang, X.; Yan, H.; Shen, Y.; Tang, H.; Yi, B.; Qin, C.; Zhang, Y. Shape Memory and Osteogenesis Capabilities of the Electrospun Poly(3-Hydroxybutyrate- co-3-Hydroxyvalerate) Modified Poly(l-Lactide) Fibrous Mats. Tissue Eng. Part A 2021, 27, 142–152. [Google Scholar] [CrossRef]
- Magiera, A.; Markowski, J.B.; Menaszek, E.; Pilch, J.; Blazewicz, S. PLA-Based Hybrid and Composite Electrospun Fibrous Scaffolds as Potential Materials for Tissue Engineering. J. Nanomater. 2017, 2017, 9246802. [Google Scholar] [CrossRef]
- Chen, J.; Zhang, T.; Hua, W.; Li, P.; Wang, X. 3D Porous poly(lactic acid)/regenerated cellulose composite scaffolds based on electrospun nanofibers for biomineralization. Colloids Surf. A Physicochem. Eng. Asp. 2020, 585, 124048. [Google Scholar] [CrossRef]
- Xu, T.; Yang, H.; Yang, D.; Yu, Z.-Z. Polylactic Acid Nanofiber Scaffold Decorated with Chitosan Islandlike Topography for Bone Tissue Engineering. ACS Appl. Mater. Interfaces 2017, 9, 21094–21104. [Google Scholar] [CrossRef]
- Abazari, M.F.; Zare Karizi, S.; Hajati-Birgani, N.; Kohandani, M.; Torabinejad, S.; Nejati, F.; Nasiri, N.; Maleki, M.H.; Mohajerani, H.; Mansouri, V. Curcumin-loaded PHB/PLLA nanofibrous scaffold supports osteogenesis in adipose-derived stem cells in vitro. Polym. Adv. Technol. 2021, 32, 3563–3571. [Google Scholar] [CrossRef]
- Wang, S.F.; Wu, Y.C.; Cheng, Y.C.; Hu, W.W. The Development of Polylactic Acid/Multi-Wall Carbon Nanotubes/Polyethylene Glycol Scaffolds for Bone Tissue Regeneration Application. Polymers 2021, 13, 1740. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.H.; Yang, J.C.; Shih, Y.H.; Yang, J.C.; Li, S.H.; Yang, W.C.V.; Chen, C.C. Bio-electrospinning of poly(l-lactic acid) hollow fibrous membrane. Text. Res. J. 2012, 82, 602–612. [Google Scholar] [CrossRef]
- Tian, L.; Prabhakaran, M.P.; Hu, J.; Chen, M.; Besenbacher, F.; Ramakrishna, S. Coaxial electrospun poly(lactic acid)/silk fibroin nanofibers incorporated with nerve growth factor support the differentiation of neuronal stem cells. RSC Adv. 2015, 5, 49838–49848. [Google Scholar] [CrossRef]
- Martin, R.A.; Wendling, M.; Mohrenweiser, B.; Qian, Z.; Zhao, F.; Mullins, M.E. Formation of aligned core/sheath microfiber scaffolds with a poly-L-lactic acid (PLLA) sheath and a conductive poly(3,4-ethylenedioxythiophene) (PEDOT) core. J. Mater. Res. 2019, 34, 1931–1943. [Google Scholar] [CrossRef]
- Kurobe, H.; Maxfield, M.W.; Tara, S.; Rocco, K.A.; Bagi, P.S.; Yi, T.; Udelsman, B.; Zhuang, Z.W.; Cleary, M.; Iwakiri, Y.; et al. Development of small diameter nanofiber tissue engineered arterial grafts. PLoS ONE 2015, 10, e0120328. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Zhang, Y.; Wang, H.; Yin, G.; Dong, Z. Fabrication and properties of the electrospun polylactide/silk fibroin-gelatin composite tubular scaffold. Biomacromolecules 2009, 10, 2240–2244. [Google Scholar] [CrossRef]
- Shalumon, K.T.; Deepthi, S.; Anupama, M.S.; Nair, S.V.; Jayakumar, R.; Chennazhi, K.P. Fabrication of poly(l-lactic acid)/gelatin composite tubular scaffolds for vascular tissue engineering. Int. J. Biol. Macromol. 2015, 72, 1048–1055. [Google Scholar] [CrossRef]
- Luiz, A.; Santos, D.; Duarte, M.A.T.; Pezzin, S.H.; Silva, L.; Domingues, J.A. Preparation of porous poly(lactic acid) fibers by medium field electrospinning for tissue engineering applications. Mater. Res. 2020, 23, 20190468. [Google Scholar] [CrossRef]
- Ravichandran, R.; Venugopal, J.R.; Sundarrajan, S.; Mukherjee, S.; Sridhar, R.; Ramakrishna, S. Minimally invasive injectable short nanofibers of poly(glycerol sebacate) for cardiac tissue engineering. Nanotechnology 2012, 23, 385102. [Google Scholar] [CrossRef]
- Gu, X.; Ding, F.; Yang, Y.; Liu, J. Construction of tissue engineered nerve grafts and their application in peripheral nerve regeneration. Prog. Neurobiol. 2011, 93, 204–230. [Google Scholar] [CrossRef] [PubMed]
- Chiono, V.; Tonda-Turo, C. Trends in the design of nerve guidance channels in peripheral nerve tissue engineering. Prog. Neurobiol. 2015, 131, 87–104. [Google Scholar] [CrossRef] [PubMed]
- Butcher, J.T.; Mahler, G.J.; Hockaday, L.A. Aortic valve disease and treatment: The need for naturally engineered solutions. Adv. Drug Deliv. Rev. 2011, 63, 242–268. [Google Scholar] [CrossRef] [PubMed]
- Eschenhagen, T.; Eder, A.; Vollert, I.; Hansen, A. Physiological aspects of cardiac tissue engineering. Am. J. Physiol. Heart Circ. Physiol. 2012, 303, H133–H143. [Google Scholar] [CrossRef] [Green Version]




| Polymers and Blends | Molecular Weight g.mol−1 | Solvent (s) | Active Compound | Average Fiber Diameter (nm) | Type of Cell | Reference | |
|---|---|---|---|---|---|---|---|
| PLA | Mw = 124,900 | chloroform: DMF (80:20 v/v) | Dexamethasone (14 w/w%) | 311 ± 74 | Emulsion electrospinning | [2] | |
| Betamethasone (14 w/w%) | 254 ± 34 | ||||||
| PLLA | Mn = 200,000 | DMF: DCM (3:7 v/v) | Curcumin (1 w/w%) | 380 ± 113 | Human adult dermal fibroblasts (HDFa) | Emulsion electrospinning | [74] |
| PLA | Mn = 200,000 | chloroform: DMAc (80:20 w/w) | Curcumin (0.125 w/w%) | 943 ± 383 | C2C12 myoblast cells | Emulsion electrospinning | [75] |
| PLA/PEG (20 wt%) | Mn = 146,000 | chloroform: acetone (2:1 v/v) | Curcumin (10 wt %) | 430 | MG-63 cells | Blend electrospinning | [70] |
| PLA | Mw = 90 000 | DMAC/acetone (1:1, w/w) | Enrofloxacin (20 w/w%) | 640 | L929 mouse skin fibroblasts (L929 MSFs) | Emulsion electrospinning | [76] |
| PLA /collagen (4% w/v) | Mw = 250,000 | HFIP | Aspalathus linearis /silver sulfadiazine | 154 | Neonatal epidermal keratinocytes | Blend electrospinning | [77] |
| PLA | Mn = 265 kDa | HFIP | Doxycycline (30%) | 424 ± 62 | L929 mouse fibroblast cells | Emulsion electrospinning | [78] |
| PLA | DCM | Silver (I) metal-organic framework | 600 ± 50 | rat full-thickness skin infection mode | Emulsion electrospinning | [79] | |
| PLA | Mw = 160,000 | Chloroform Coagulation bath: aqueous solution of sodium hydroxide (NaOH, pH~13) | 274 ± 76 | Rat bone marrow stem cells | Wet electrospinning | [80] | |
| PLLA | Mw = 300 kDa | DCM and Asiatic acid (AA) | Immortalized human keratinocytes HaCaT Mouse mononuclear macrophage cell line RAW 264.7 | Electrospinning | [81] | ||
| PLLA PEO, Chitosan (CS) | Mw = 217.000 to 225.000, Mw = 100.000, Mw = 50.000–190.000 | Chloroform/DMF 9:1 (v/v), ethanol/distilled water 8:2 (v/v), 14% acetic acid (v/v) | Hypericum perforatum (HP) | PLLA = 186 ± 68 PEO_CS = 141 ± 46 PEO_HP_CS = 88 ± 29 | Normal human dermal fibroblasts (NHDF) | Blend electrospinning | [82] |
| PLA | 1,000,000 (DG-DL400), | DCM/DMF 2:1 (v/v) | 402 ± 106 | L929 cells | Electrospinning | [7] | |
| PLA (L207S) | DCM/DMSO 4:1 (v/v) | Triterpene extract | 927 ± 214 | Emulsion electrospinning | [83] | ||
| PLA | Mw = 70,000 | DMF/ chloroform (1:3) | Ibuprofen (20 wt%) | 478.31 ± 167.61 | HDF & HEK from adult human skin | Electrospinning | [84] |
| P(LLA-CL)/PDEGMA 1:1 | HFIP | Ciprofloxacin 0.9% w/v | 0.32 ± 0.11 | L929 cells | Emulsion electrospinning | [85] | |
| PLA/polyurethane | Mw = 100,000 | Acetone: DMA | Doxorubicin (DOX) | Emulsion electrospinning | [86] | ||
| PLLA and polyhedral oligomeric silsesquioxane (POSS) | Mn = 1 × 105 | DMF: DCM (1:3 v/v) | Plasmid DNA encoding angiopoietin-1 (pAng) | 0.78 ± 0.10 | Human umbilical vein endothelial cells (HUVECs) | Blend electrospinning | [87] |
| PLA/poly(1, 8-octanediol-co-citric acid) (POC) 75:25 | Mw = 1 × 105 | HFIP | Aspirin | 716 ± 122 nm | Blend electrospinning | [88] | |
| γ-PGA (core) PLA (shell) | MwPLA = 500,000 MwPGA = 1,000,000 | CH2CL2 for PLA & CH3COOH for PGA | Rhodamine B and coumarin-6 | 120 ± 31 nm | Mouse embryonic fibroblast cells (NIH/3T3) | Coaxial electrospinning | [6] |
| PCL as core, blends of PCL/PLA as shell | chloroform/methanol was 19:1 | Tetracycline hydrochloride (TCH) | ~1.4 | Coaxial electrospinning | [89] | ||
| PLLA as shell, poly(glycerol sebacate) as core | PLLA, (Mn = 200 KDa) | Chloroform for PLA DCM and DMF (v:v = 3:1) for PGS | 1000 nm | L929 cells, Twenty-four 6-week adult female mice | Coaxial electrospinning | [1] | |
| PLLA as core CS: PEO as shell | (Mw = 500 kDa) | HFIP for PLLA 3%HAc: DMSO:triton X-100 (10:1.0: 0.3) for CS:PEO | Graphene oxide (GO) sheet for coating | 240 ± 132 | Pig iliac endothelial cells (PIECs) for in vitro, Twelve adult female Sprague-Dawley rats for in vivo | Coaxial electrospinning | [90] |
| PLLA as shell, PVA as core | Mn PLA = 125 × 103, Mn PVA = 90 × 103 | DCM/DMF (1:9 ratio) | Connective tissue growth factor (CTGF) | 260 ± 140 | Fibroblasts, keratinocytes and endothelial cells | Coaxial electrospinning | [91] |
| Polymers and Blends | Molecular Weight g.mol−1 | Solvent (s) | Drug | Average Fiber Diameter (μm) | Type of Illness | Techniques for Loading Drugs | Refs. |
|---|---|---|---|---|---|---|---|
| PLA | Mw = 205 kDa | chloroform: | tetracycline hydrochloride | 3 to 6 | Emulsion electrospinning | [105] | |
| PLLA | Mn = 470,000 | DMF:DCM (1:1 v/v) | Rhodamine B | 4.32.5 ± 0.22 | Coaxial electrospinning | [106] | |
| PLA | Mw = 111,000 | DMF:DCM (1:1 v/v) | Doxorubicin in hydrophilic form (Dox-HCl) | 0.32 ± 0.05 | Cancer | Emulsion electrospinning | [107] |
| Doxorubicin in hydrophobic free base form (Dox-base) | 0.30 ± 0.03 | ||||||
| PLA | Mw = 75 kDa | Chloroform | Doxorubicin | 0.1 ± 0.01 | Emulsion electrospinning | [108] | |
| PLA | Trichloromethane (TCM)/acetone 2:1 v/v | Carvacrol | 1.54 ± 1.07 | Emulsion electrospinning | [103] | ||
| PLA | Mw ≈ 100 kDa | DCM/trifluoroacetic acid 2:1 (w/w) | polyethylene glycol (PEG) | 0.28 | Emulsion electrospinning | [109] | |
| PLA 70:30 | Resomer LR708 | DMF/THF (1:1 v/v) | Lysozyme-loaded PVP /PLGA core/sheath nanoparticles | 0.75 ± 0.11 | Assembly of particle-fiber composites by emulsion electrospinning | [110] | |
| PDLLA | Mw = 170 kDa | DCM/Chloroform 9:1 to 1:1 | Rifampicin | Emulsion electrospinning | [111] | ||
| PLA, D isomer < 5% | CHCl3/DMF = 6:1 | caffeine | 0.97 ± 0.35 | Emulsion electrospinning | [112] | ||
| PLA | Mw = 100,000 | DMF: Chloroform 1:9 w/w | Salicylic acid (SA) 4, 8, 12 wt% | 0.69 ± 0.14 | Skin care | Emulsion electrospinning | [113] |
| PLA | Mw = 103~259 kDa | DCM/DMF 4:1 v/v | 25-hydroxy vitamin 3 | 1.2 ± 0.3 | For minimizing the chance of surgical site infection | Emulsion electrospinning | [114] |
| PLA | Mn = 112,890 | chloroform | Propolis ethanolic extract (PEE) 20 wt% | 0.37 ± 0.25 | Antiseptic and antimicrobial activity | [115] | |
| silver nanoparticles (AgNPs) 5 wt% | 0.25 ± 0.25 | ||||||
| PLACL (70:30) | Mw = 150 kDa | 1,1,1,3,3,3-hexafluoro-isopropanol (HFP) | 0.78 ± 0.28 | Breast cancer therapy | [116] | ||
| Aloe Vera (AV) | 0.50 ± 0.17 | ||||||
| AV & magnesium oxide (MgO) nanoparticles | 0.33 ± 0.95 | ||||||
| Av & MgO &curcumin (CUR) | 0.36 ± 0.94 | ||||||
| Av & MgO & β-cyclodextrin (β-CD) | 0.32 ± 0.80 | ||||||
| PLLA/ Pluronic®P123 | Chloroform/DMF 6:1 v/v | Dexamethasone | 0.98 ± 0.41 | Bone defects | Emulsion electrospinning | [117] | |
| PLA/Chitosan 30% | Mw = 35,000 | Chloroform/ethanol (1:1, v/v) & formic acid for CS | Tetracycline hydrochloride loaded | 0.28 ± 0.01 | Emulsion electrospinning | [118] | |
| PLA/PEG | Mn = 120,000 Mw PEG = 6000 | DMF/Chloroform 10:90 v/v | Graphene oxide | 0.38 ± 0.09 | Co-electrospinning | [119] | |
| PLLA/ /silk fibroin as sheath & polyoxyethylene/ as core | Mw = 500,000 | HFIP | l-Ascorbic acid-2-phosphate sodium | coaxial electrospinning | [120] | ||
| PLA/ oleic acid (OA)-coated magnetite iron oxide nanoparticles (OA-MIONs) | Mw = 100 kDa | Chloroform and the DMF) | Vancomycin hydrochloride | Outer diameter of ≈0.64 and an inner diameter of ≈0.28 | Emulsion electrospinning | [121] | |
| PLA as core N-Isopropyl acrylamide (NIPAM) as shell | Mw = 10 kDa | Dichloromethane for PLA, deionized water for NIPAM | Combretastatin A4 (CA4) in core, N,N–Methylenebisacrylamide (MBA) in shell | Core = 0.5, Shell = 0.3 | Tissue engineering | UV photo-polymerization combined with blend electrospinning | [122] |
| PLA as shell PVP as core | Mw = 240,000 | Trichloromethane (TCM)/DCM 3:1 v/v | Flurbiprofen axetil (FA) | 0.7 ± 0.01 | Pharmaceutical science | Coaxial electrospinning | [123] |
| Polymers and Blends | Solvent (s) | Additive | Scaffold Properties | Tissue | Refs. |
|---|---|---|---|---|---|
| PLLA, average Mw = 138,000 | HFIP | Diameter of aligned nanofiber: 0.58 ± 0.10 µm, Diameter of random nanofiber: 0.59 ± 0.10, Alignment improved the ability to promote proliferation, migration and facilitating the osteogenic differentiation of BMSCs | Bone | [130] | |
| PLLA, PL 65 | DCM: DMF (95:5 w/w) | Dopamine and SiO2 nanoparticles to be coated on the surface of fibers | Highly porous with a rougher surface, good Hydrophilicity, mechanical properties, biocompatibility and improved cell attachment and proliferation | Bone | [132] |
| PLLA | CHCl3 | The scaffold was coated with hydroxyapatite nanoparticles and immobilized with BMP-2 loaded liposomes | Improved cellular attachment and proliferation due to nanoHA | Bone | [133] |
| PLLA/gelatin (25/75 wt%) | HFIP | Nano-hydroxyapatite (nHA) | nHA/PLA/GEL scaffold r immobilized with peptides have Interconnected and multilevel porous structures similar to native ECM | Bone | [134] |
| PLLA Mw = 50 kDa | DCM: DMF (2:1 w/w) | Nano-hydroxyapatite (nHA) | Bipolar nanofibrous membrane of nHA and PLLA represented a novel treatment modality for enhancing the tendon–bone healing | Bone | [135] |
| PLA | CHCl3: DMF (3:1) | Cellulose nanocrystals (4%) | Enhancement in the mechanical and thermal properties, cell viability, mineralization and expression of osteogenic gene markers for composite fibers | Bone | [136] |
| PLLA /lecithin | DCM | Dimeter: 0.15–3 µm | Bone | [137] | |
| PLLA/ Poly(3-hydroxybutyrate-co-3-hydroxyvalerate) PHBV (7:3) | TCM: DMF (9:1 v/v) | Diameter 2.89 ± 0.51 µm, Significantly promote the osteogenic commitment in BMSCs | Bone | [138] | |
| PLA, (Mw: 90,000–120,000 g/mol), Gelatin (Mw: 40,000–100,000 g/mol) | DCM: DMF (3:1 w/w), Acetic acid for gelatin | Multiwalled carbon nanotubes (MWCN) 1%(wt) | Fiber diameter: 300 nm Material porosity: 0.87 Wettability: 51.4 ± 1.4 (°) Tensile strength: 12.3 ± 1.9 MPa Young’s Modulus: 898 ± 91 MPa | Bone | [139] |
| PLA 4043D, celluloseacetate (CA) | HFIP for PLA and DMAc/acetone, 2:1 w/w for CA | Introduction of regenerated cellulose in the scaffolds improved superabsorbent property and mechanical strength | Bone | [140] | |
| PLA Mw: 150 000 g/mol and CS (DA 90%) | TFA | PLA scaffolds with CS island-nanotopology surfaces were favorable for the spread of cells and the CS accelerated the mineralization of HA, as well as endowed the scaffold with a better ability to form bone | Bone | [141] | |
| PLLA (Mw = 240,000 g/mol) and PHB (Mw = 300,000 g/mol) | Chloroform and DMF | Curcumin 5% | Smooth and bead-free fibers with porosity and well-interconnected pore, Tensile strength: 33.23 ± 0.12 MPa, Curcumin improves viability, cell attachment, and protein adsorption | Bone | [142] |
| PLA 180~210 kDa and PEG | DCM | MWCNTs and Dexamethasone | The presence of PEG improved the ductility of nanofibers, MWCNTs could adsorb DEX to facilitate the even distribution of DEX in the nanofibers | Bone | [143] |
| PLLA (Mw = 140 kDa), PEG (Mw = 35 kDa), PEO (Mw = 900 kDa) | DMF/DCM | PC12 cells | Aligned, cell-containing, micro-scale hollow fibers were prepared, PC12 cells showed attachment, proliferation, and finally differentiation, in the tubular scaffold with the addition of the neuron growth factor | Nerve | [144] |
| PLA as shell Silk fibroin (SF) as core | 1,1,1,3,3,3-Hexafluoro-2-propanol (HFP) for PLA, water for SF | Nerve Growth Factor | 0.22 ± 0.04 | Nerve | [145] |
| PLA as shell poly(3,4-ethylenedioxythiophene) (PEDOT): polystyrene sulfonate (PSS) as core | Chloroform for PLA and oleic acid for PEDOT | A novel, highly aligned core/sheath fiber structure with a conductive polymer core and an insulating the sheath was successfully produced and characterized | [146] | ||
| PLA | HFIP | Histologic analysis of explanted TEVG grafts showed the presence of CD31-positive endothelial monolayer and F4/80-positive macrophages after 4, 8, and 12 months in vivo. Cells positive for α- smooth muscle actin was observed within TEVG, demonstrating the presence of smooth muscle cells (SMCs). A neo-extracellular matrix consisting mostly of collagen types I and III were observed at 12 months post-implantation | Vascular grafts | [147] | |
| PLA MW = 1.0 × 105 kg/mol (outer layer), Silk Fibroen gelatin (inner layer) | chloroform: acetone (2:1 v/v) for PLA, Formic acid for SF and gelatine | The electrospun PLA/SF-gelatin composite tubular scaffolds possess a porous structure, adequate strength and excellent biocompatibility | Blood vessels | [148] | |
| PLA (MW ∼ 350,000), gelatin (MW ∼ 15,000) | Formic acid, chloroform and acetone in (2:2:1) | the presence of gelatin enhanced cell attachment and proliferation of PLA scaffolds. Aligned nanofibers highly supported the SMCs and improved the proliferation of cells | Vascular | [149] | |
| PLLA MW = 2.78 × 105 g.mol−1, | Chloroform | sodium lauryl ether sulfate (SLES) surfactant | A three-dimensional fiber network with a highly porous surface was obtained by Medium Field Electrospinning (MFES), | Tissue engineering | [150] |
| PLLA as sheath & poly(glycerol sebacate) (PGS) as core | 1,1,1,3,3,3-hexafluoro-2-propanol (HFP) | 1.32 ± 0.16 | Cardiac tissue engineering | [151] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maleki, H.; Azimi, B.; Ismaeilimoghadam, S.; Danti, S. Poly(lactic acid)-Based Electrospun Fibrous Structures for Biomedical Applications. Appl. Sci. 2022, 12, 3192. https://doi.org/10.3390/app12063192
Maleki H, Azimi B, Ismaeilimoghadam S, Danti S. Poly(lactic acid)-Based Electrospun Fibrous Structures for Biomedical Applications. Applied Sciences. 2022; 12(6):3192. https://doi.org/10.3390/app12063192
Chicago/Turabian StyleMaleki, Homa, Bahareh Azimi, Saeed Ismaeilimoghadam, and Serena Danti. 2022. "Poly(lactic acid)-Based Electrospun Fibrous Structures for Biomedical Applications" Applied Sciences 12, no. 6: 3192. https://doi.org/10.3390/app12063192
APA StyleMaleki, H., Azimi, B., Ismaeilimoghadam, S., & Danti, S. (2022). Poly(lactic acid)-Based Electrospun Fibrous Structures for Biomedical Applications. Applied Sciences, 12(6), 3192. https://doi.org/10.3390/app12063192









