Abstract
Adult spinal deformity (ASD) is highly prevalent in persons older than 65 years, affecting more than 30% of the total population. There are many important reports that describe excellent postoperative results for ASD surgery. However, there is no report that describes a chronological evaluation of gait ability and spinal balance after ASD surgery. The present prospective study aimed to determine the recovery time of gait and spinal balance ability after adult spinal deformity (ASD) surgery. Patients with ASD (n = 25: mean age, 73.0 years) who underwent corrective surgery and preoperative and postoperative gait and spinal balance ability evaluation. Spinal radiographs and gait analysis data (static balance; single-leg standing, dynamic balance; time-up and go test, gait ability; 10 m walk velocity) were acquired preoperatively, 1 month, 6 months, and 12 months after surgery. The radiographic parameters of the spine and pelvis (lumbar lordosis; LL, pelvic tilt; PT, sagittal vertical axis; SVA, pelvic incidence; PI) were measured. The mean postoperative SVA, LL, PT, and PI-LL became 30.0 mm, 50.1 degrees, 14.1 degrees, and 0.35 degrees, respectively. Preoperatively, all spinal balance and gait ability were worse than the normal threshold (one-leg standing; 14.2 s vs. 15.0 s, time-up and go test; 13.9 s vs. 13.5 s, 10-m walk speed; 0.91 m/s vs. 1.00 m/s). At 12 months after surgery, all spinal balance and gait ability became normal or improved (single-leg standing; 14.7 s, time-up and go test; 11.0 s, 10-m walk speed; 1.09 m/s). The ODI at one-year follow-up improved from 46.8 ± 12.6% to 27.8 ± 18.1%. In conclusion, gait and spinal balance analysis revealed that ASD patients could not recover gait and spinal balance ability one month after surgery. At 12 months after surgery, gait ability and dynamic spinal balance became better than preoperative levels. However, the static spinal balance was at the same level as that of preoperative status.
1. Introduction
In the world, the population is rapidly increasing because of increased longevity, improved medical care, and declining natality [1,2]. These global population shifts have affected the prevalence of musculoskeletal diseases such as adult spinal deformity (ASD). ASD is highly prevalent in persons older than 65 years, affecting more than 30% of the total population [3,4]. ASD is caused by spinal malalignment, which results in not only severe low back pain and neurological dysfunction but also reflux esophagitis, cosmetic disorders, and mental disorders [5,6].
A large number of reports support the effectiveness of surgical treatment over conservative treatment in severe cases [7,8]. The goal of ASD surgery is to restore the global spinal balance without any complications, especially sagittal alignment [9,10]. However, it needs several months for the elderly ASD patients to adopt a new posture. The rehabilitation after ASD surgery is very important to regain normal daily life activity for the ASD patients to avoid falls because of spinal imbalance [11]. There are many important reports that describe excellent postoperative results for ASD surgery [12,13].
The systematic review revealed that complex rehabilitation reduces short and long-term disability and fear-avoidance behavior following lumbar fusion surgery [14], and the rehabilitation for ASD results in significant functional improvements [15]. Recently, gait analysis, including a timed up and go test (TUG), was reported as a very useful tool to evaluate patients’ dynamic balance [16,17,18]. However, there is no report that describes a chronological evaluation of gait ability and spinal balance after ASD surgery. We made a hypothesis that patients’ gait ability and posture balance will recover gradually and independently after surgery. With those results, the rehabilitation staff can provide patients with appropriate rehabilitation programs according to the recovery of gait ability and posture balance. The present prospective study aimed to determine their recovery times for gait and spinal balance ability after ASD surgery.
2. Materials and Methods
2.1. Patient Population
The study was approved by our institutional review board (No.287). We have obtained fully informed consent from the patients for this study. From June 2017 to August 2019, 25 female patients with ASD who underwent corrective surgery at our hospital were included in the study (Table 1, Figure 1). Inclusion criteria for this study were patients aged 60 years or older with the presence of at least one of the following: the sagittal vertical axis (SVA) 95 mm or more, pelvic tilt (PT) 30 degrees or greater, and/or coronal Cobb angle 30 degrees or greater [4]. Exclusion criteria were spinal deformities resulting from neuromuscular disease, spinal infection, or tumor. The surgeries were performed in the two stages, first OLIF L1 to L5 (or S1), secondly posterior corrective fusion basically from T10 to pelvis. We also evaluated hospital stay, % home return, open/MIS surgery, upper instrumented vertebra (UIV), and complications. BMI: Body mass index.

Table 1.
Patient demographic.
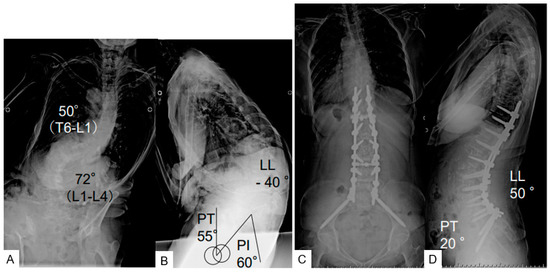
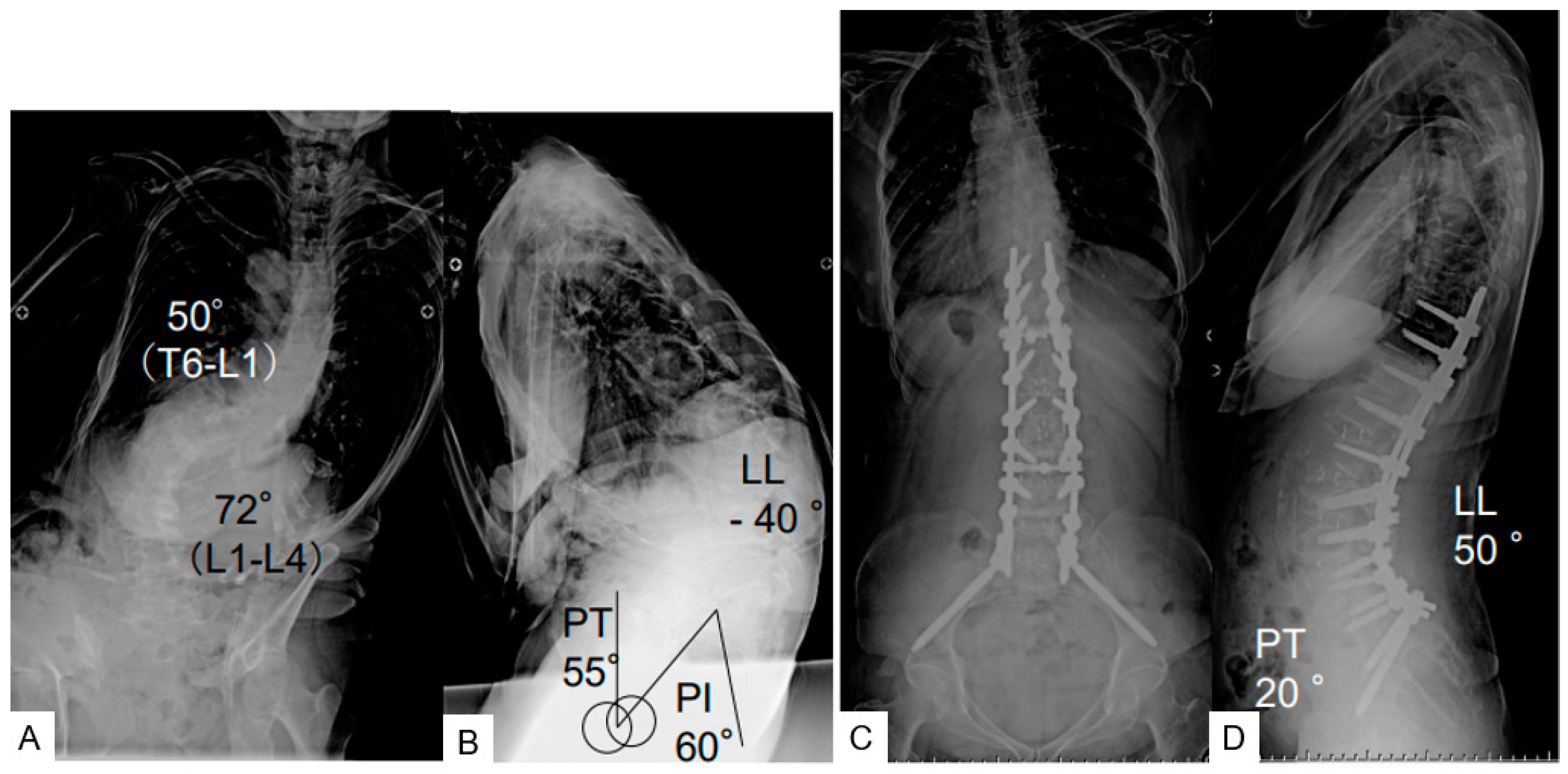
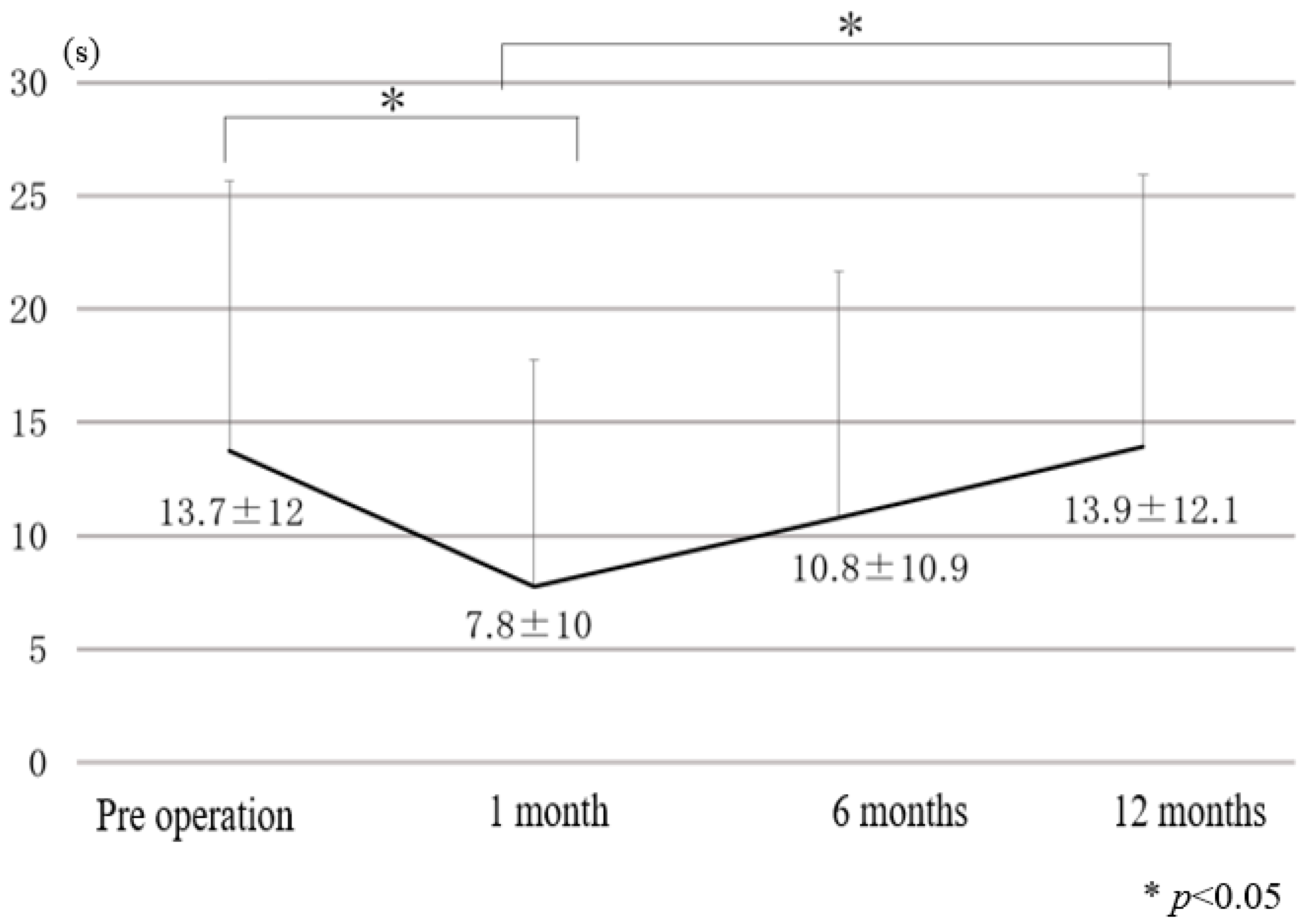
Figure 1.
A 79 female, adult spinal deformity, (A): preoperative posteroanterior radiogram, (B): preoperative lateral radiogram, PI 60°, PT 55°, LL −44°, SVA 150 mm, PI-LL 100°, (C): postoperative posteroanterior radiogram, PI 60°, PT 20°, LL 50°, SVA −15 mm, PI-LL 10°, (D): postoperative lateral radiogram.
2.2. Gait Analysis
2.2.1. Gait Ability Test (10-m Walk Test)
The 10-m walk test was used to measure the patient’s gait ability and speed of comfortable walking. The 10-m walk test is a commonly used measure for assessing walking speed [19]. Distances were provided at the beginning and end of the timed walkway to allow participants space to accelerate/decelerate outside the data collection area to help reduce gait variability introduced during these phases [20]. The average walking velocities according to the age are 1.34–1.24 m/s (60–69 years old), 1.26–1.13 m/s (70–79 years old), and 0.97–0.94 m/s (80–99 years old) [21]. The excellent reliability of this test has been reported [22].
2.2.2. Static Balance Test (Single-Leg Stand Test)
Patients were instructed to stand on a single leg, face is straight, both arms are side of the body, with shoes (Figure 2). The test was performed twice and the average values were taken. The average single leg standing time according to the age are 19 s (>70 years), 10 s (70–75 years old), and 6 s (>75 years old) [23].

Figure 2.
Static balance test.
2.2.3. Dynamic Balance Test (Timed Up and Go Test; TUG)
TUG measures the time it takes a subject to stand up from a chair, walk a distance of 3 m, turn, walk back to the chair, and sit down. TUG has a wide variety of clinical use making it a diverse measure that should be considered when choosing an activity-based outcome. The excellent reliability and validity of TUG as a clinical tool has been reported in a systematic review [24]. These data were acquired preoperatively, 1 month, 6 months, and 12 months after surgery. The age-matched normal values of these tests were obtained from previous reports [16,17,18].
2.3. Radiographic Measurements
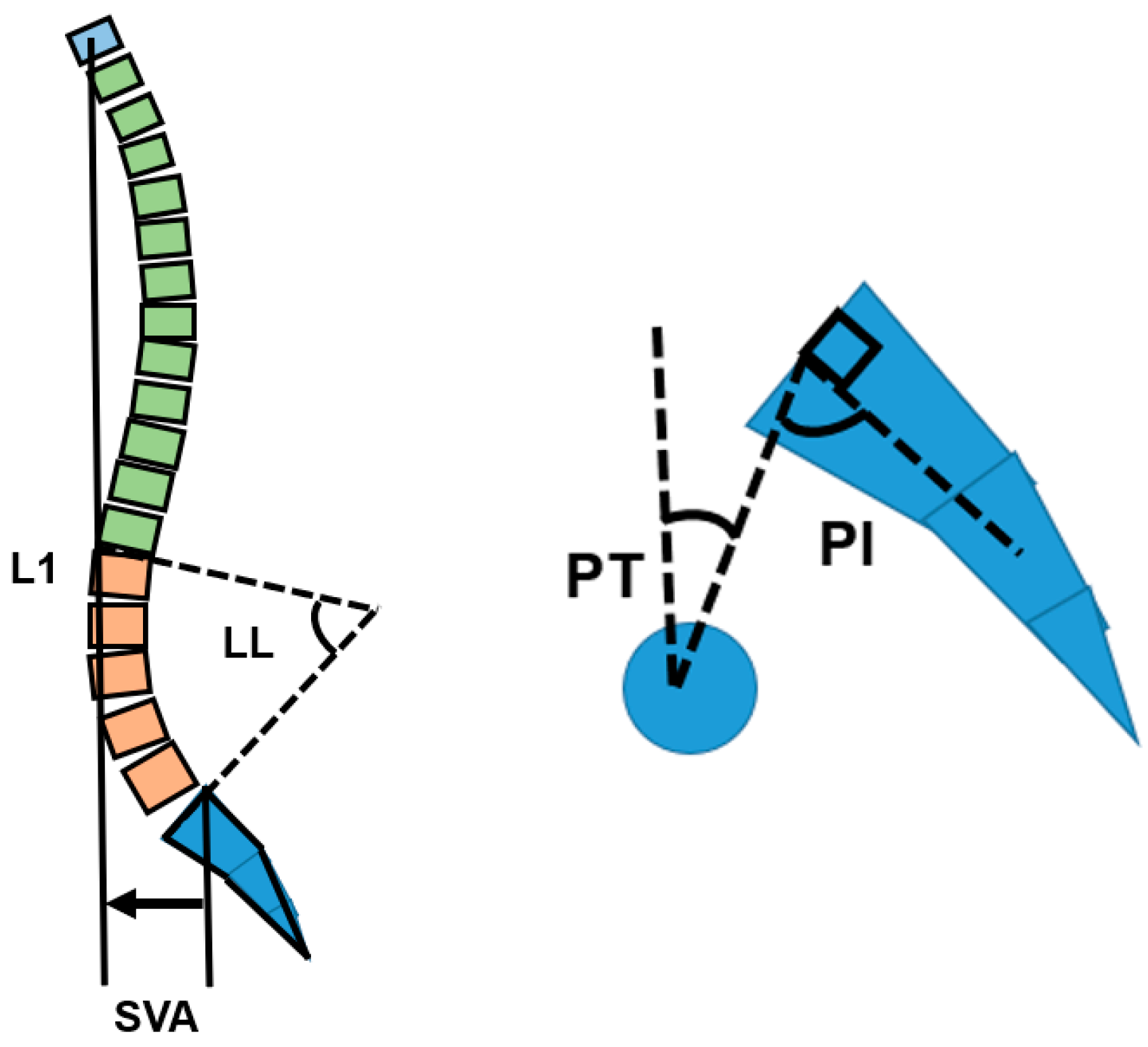
The radiographic parameters of the spine and pelvis (lumbar lordosis; LL, pelvic tilt; PT, sagittal vertical axis; SVA, pelvic incidence; PI) were measured preoperatively and at 12 months postoperatively, (Figure 3) [25]. We evaluated correlations between these parameters and gait ability and spinal balance data.
Figure 3.
Spinopelvic parameter, SVA; sagittal vertical axis, LL; lumbar lordosis, PT; pelvic tilt, PI; pelvic incidence.
2.4. Statistical Analysis
All values are expressed as mean ± standard deviation (SD). We performed Shapiro–Wilk normality test histogram for the values. The result was not a normal distribution because of the small number of the patients. The gait ability and spinal balance data from preoperative to postoperative 12 months were examined by Friedman test and Bonferroni correction. The preoperative and postoperative spinopelvic parameters were examined by Wilcoxon signed-rank test. The relationship between spinopelvic parameters and gait analysis data was examined by Spearman’s rank correlation coefficient test. The analysis software was EZR [26] and p < 0.05 was considered statistically significant.
3. Results
3.1. Clinical Evaluation
The ODI at one-year follow-up improved from 46.8 ± 12.6% to 27.8 ± 18.1%. The mean hospital stay of the patients was 32.0 ± 11.3 days. Twenty-one patients returned home directly, and four patients were moved to another rehabilitation center. Sixteen patients underwent posterior Ponte osteotomy, and nine patients underwent percutaneous pedicle screw fixation (Table 2). There was one postoperative deterioration of leg numbness, which was recovered 6 months after surgery.

Table 2.
Clinical results.
3.2. Spine and Pelvic Parameter
The mean preoperative SVA, LL, PT, and PI-LL were 100.5 mm, 8.8 degrees, 35.5 degrees, and 41.1 degrees, respectively. The mean postoperative SVA, LL, PT, and PI-LL became 30.0 mm, 50.1 degrees, 14.1 degrees, and 0.35 degrees, respectively. There were no correlations between the spine and pelvic parameters, gait ability, spinal balance test data (Table 3 and Table 4).

Table 3.
Preoperative and postoperative spine and pelvic parameters.

Table 4.
Correlation between spinopelvic parameters and gait ability and spinal balance.
3.3. Gait Ability and Spinal Balance Test
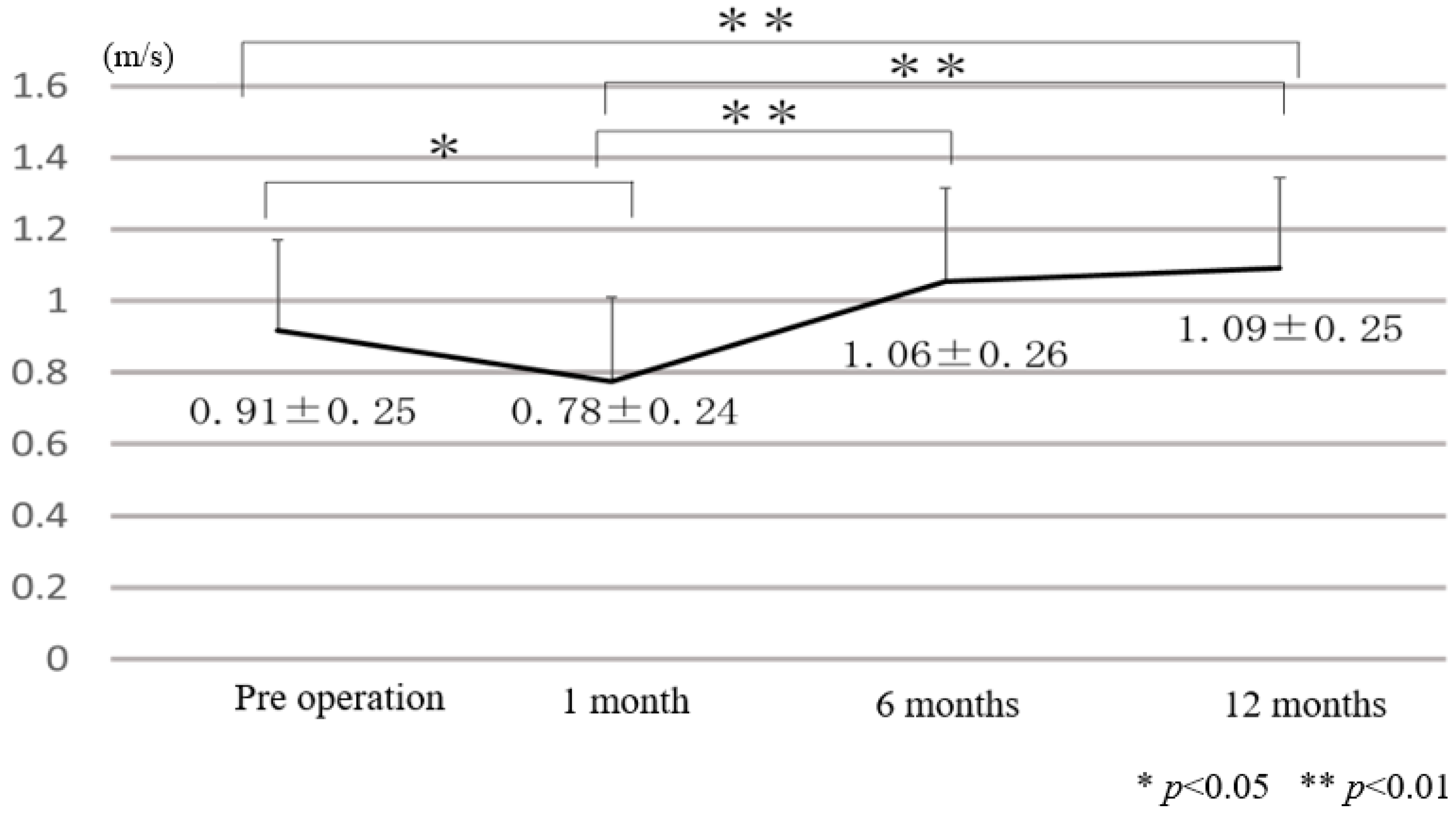
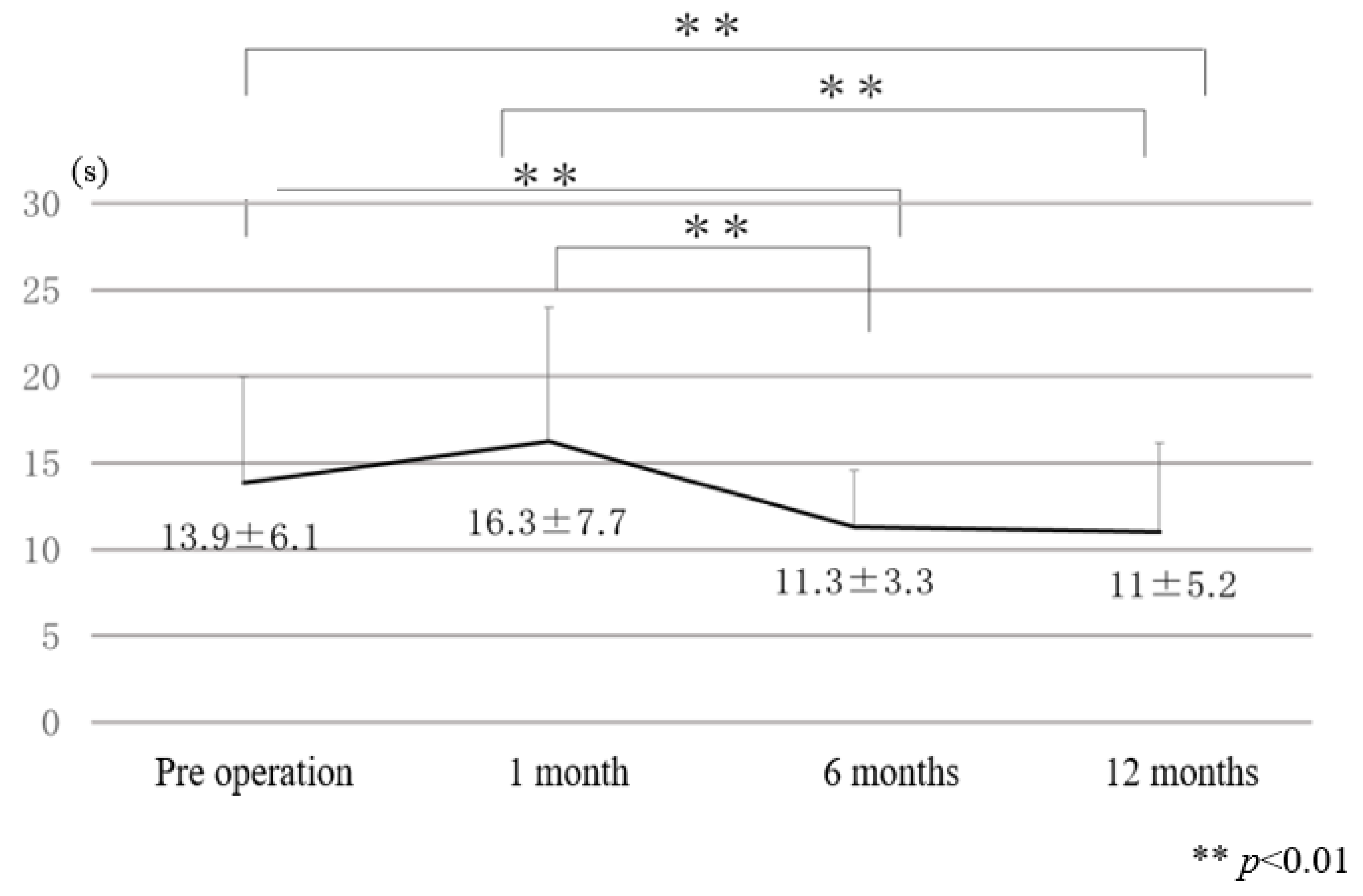
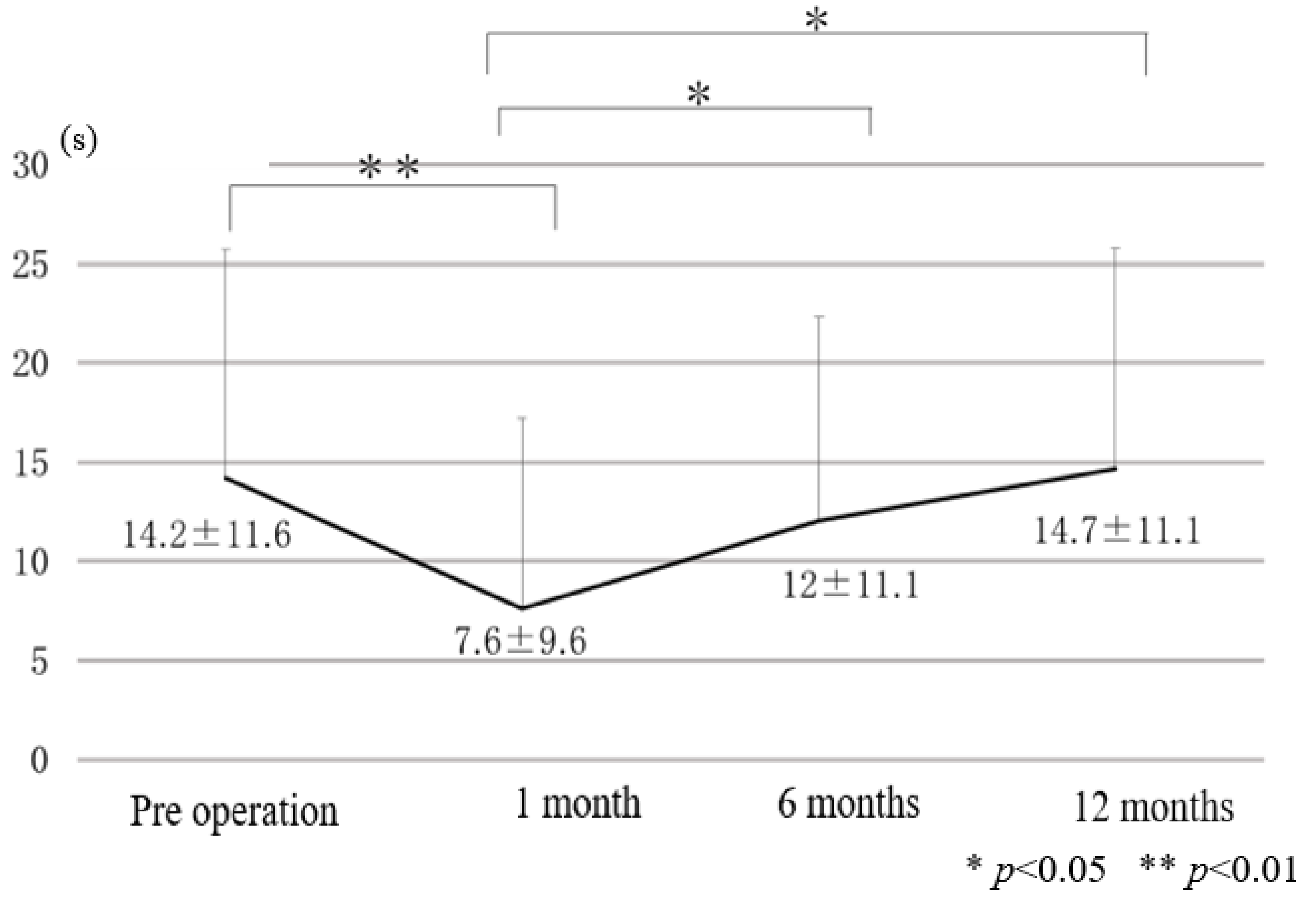
Chronological results of gait ability and spinal balance tests before and after adult spinal deformity surgery are indicated in Figure 4, Figure 5, Figure 6 and Figure 7. Preoperative all gait ability and spinal balance were worse than normal threshold [16,17,18] (one-leg standing time; 14.2 s vs. 15 s, time-up and go test TUG; 13.9 s vs. 13.5 s, 10 m walking speed; 0.91 m/s vs. 1.00 m/s; preoperative data vs. normal threshold). At one month after surgery, dynamic spinal balance (TUG) became worse (16.3 ± 7.7 s) but was not statistically significant. Static spinal balance (one-leg standing) and gait ability (10-m walk test) at one month became significantly worse at 7.6 ± 9.6 s and 0.78 ± 0.24 m/s, respectively. At 12 months after surgery, spinal dynamic balance and gait ability were improved (TUG; 11.0 s vs. 13.9 s, 10-m walk speed; 1.09 m/s vs. 0.91 m/s; 12 months vs. preoperative). However, the static spinal balance was at the same level as preoperative status (single-leg stand test: 14.7 s vs. 14.2 s; 12 months vs. preoperative). Postoperatively, five patients had a fall. The TUGs of those patients were all abnormal values. This section may be divided into subheadings. It should provide a concise and precise description of the experimental results, their interpretation, as well as the experimental conclusions that can be drawn.
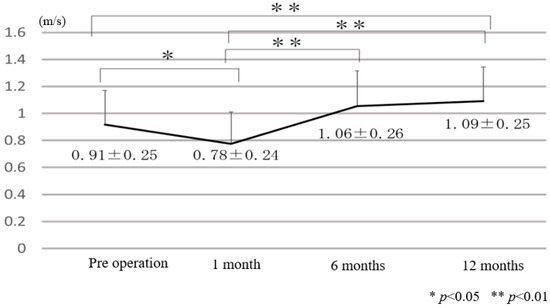
Figure 4.
A 10-m walk velocity.
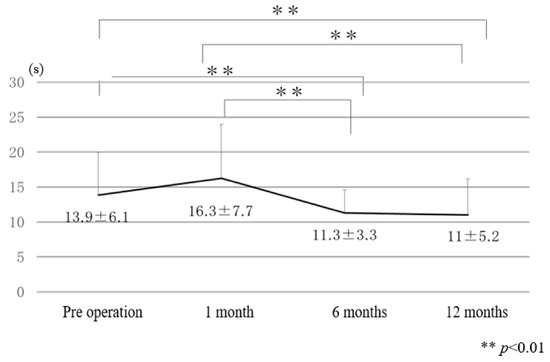
Figure 5.
Timed up and go test.
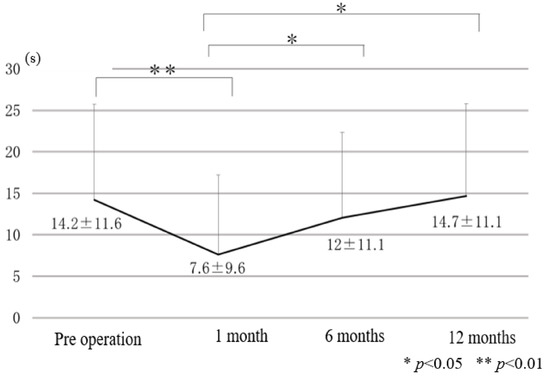
Figure 6.
Single leg standing (right side).
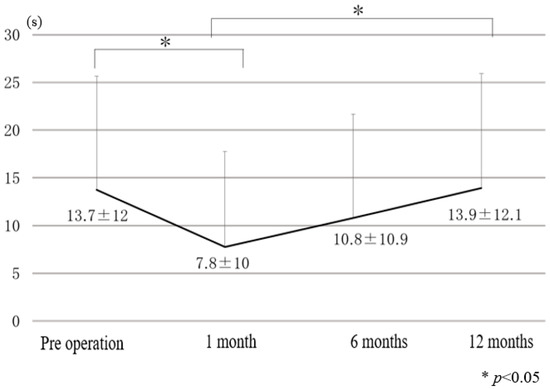
Figure 7.
Single leg standing (left side).
4. Discussion
Gait disturbance is one of the most severe symptoms for ASD patients. Spinopelvic parameters are very important and useful indicators to check the spinal balance for ASD patients. Miyazaki et al. reported the loss of lumbar lordosis related to loss of leg strength for walking ability in elderly ASD patients [11,27]. However, there is a difference between gait posture and standing posture over a short time [28]. The 10-m walk test is a performance measure used to assess walking speed in meters per second over a short distance, which can be employed to determine functional mobility, gait, and vestibular function. To check for real gait disturbance, the 10-m walk test has been proven to be a simple and excellent test [29]. According to this velocity, household ambulator < 0.40 m/s; limited community ambulator 0.40 to <0.80 m/s; community ambulator ≥ 0.80 m/s. For elderly patients, spinal balance is very important to prevent falls during walking [5]. Falls in elderly patients may cause hip fractures that lead to the deterioration of their ambulatory function, increasing their dependence on assistance with activities of daily living [30]. The single-leg stand time is an easy and quick balance assessment measurement. And a prior cohort study reported that a decrease in one-leg standing time was associated with falling in the elderly [31,32]. On the other hand, TUG is a simple test used to assess a person’s mobility and requires both static and dynamic balance. This test is usually performed to predict the patient’s ability to go outside alone safely [33]. For this study, we regarded TUG as the main evaluation of dynamic spinal balance.
Preoperative data of these three tests indicated that ASD patients had worse results than the normal population, thereby they potentially have a high risk of falls and gait disturbance. Yagi et al. reported that, in comparison to healthy individuals, ASD patients had an asymmetrical gait pattern and impaired gait ability [34]. Gait ability correlated significantly with the gravity line, spinopelvic alignment, lower extremity joint ROM, and lean volume [34]. In our data, there was no correlation between spinopelvic alignment and gait ability. This is mainly because our patients were all candidates for surgery, so the spinopelvic alignment was extremely deteriorated, and there was almost no difference among the data. One month after surgery, all data of gait analysis were worse than preoperative data. This deterioration of spinal balance and walking ability may be due to surgical muscle damage, postoperative bed rest, and poor adaptation to new spinal alignment. This suggests that medical staff should take care of the ASD patient not to fall during the postoperative rehabilitation period.
Six months after surgery, the static and gait ability of the ASD patients became the same level as preoperative status, and the dynamic balance of the ASD patients became better than preoperative status. From these results, it needs 2 to 6 months to regain preoperative spinal balance and walking ability. Twelve months after surgery, all data except static posture balance became better than the preoperative status. The result of 10 m walking speed became 1.09+/−0.25 m/s and this result is more than 1.00 m/s, which indicates the normal speed of stable walking [17]. For the elderly people, it has been reported that there is a strong correlation between 10 m walking speed and TUG [34], which is equivalent to our data. Most importantly, TUG will improve faster than 10 m of walking ability after ASD surgery. Single leg standing time was not improved at 12 months after surgery. Usually, a long spinal fusion is necessary for ASD patients, so the spinal segmental motion is lost. This segmental spinal motion is very important to control the gravity center, and as a result, static spinal balance is lost for the patients with long spinal fusion. According to our chronological evaluation of gait ability and spinal balance after adult spinal deformity surgery, dynamic balance is improved first, walking ability second, then static balance remains at preoperative status at 12 months’ follow-up.
The limitations of this study are a small number of patients, only female patients, and no obese patients. There is no data for dynamic alignment. We neither used force plates to evaluate patients’ balance nor a quantitative muscle power test. The follow-up period is just 12 months.
5. Conclusions
Chronological evaluation of gait and posture balance analysis after ASD surgery revealed that ASD patients could not recover gait and posture balance ability one month after surgery. However, at 12 months after surgery, gait ability and dynamic posture balance became better than preoperative levels, but static posture balance was at the same level as preoperative status. Rehabilitation staff and patient-support personnel should pay special attention to patients’ static balance within 12 months after ASD surgery.
Author Contributions
Conceptualization, T.S. and M.T.; methodology, T.S.; formal analysis, S.A. and K.U.; data curation, Y.F., A.S., K.T., Y.Y. and M.N.; writing—original draft preparation, T.S.; writing—review and editing, H.S. and T.Y.; supervision, N.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Japan Organization of Occupational Health and Safety.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Okayama Rosai Hospital (protocol code 287, 21 September 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to patients’ privacy.
Acknowledgments
This study was supported by the Okayama Spine Group.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fehlings, M.G.; Tetreault, L.; Nater, A. The aging of the global population: The changing epidemiology of disease and spinal disorders. Neurosurgery 2015, 77, S1–S5. [Google Scholar] [CrossRef] [PubMed]
- Lutz, W.; Sanderson, W.; Scherbov, S. The coming acceleration of global population ageing. Nature 2008, 451, 716–719. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Dubey, A.; Gamez, L.; El Fegoun, A.B.; Hwang, K.; Pagala, M.; Farcy, J.P. Adult scoliosis: Prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine 2005, 30, 1082–1085. [Google Scholar] [CrossRef] [PubMed]
- Kebaish, K.M.; Neubauer, P.R.; Voros, G.D.; Khoshnevisan, M.A.; Skolasky, R.L. Scoliosis in adults aged forty years and older: Prevalence and relationship to age, race, and gender. Spine 2011, 36, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Konno, S.; Kikuchi, S.; Nagaosa, Y. The relationship between intramuscular pressure of the paraspinal muscles and low back pain. Spine 1994, 9, 2186–2189. [Google Scholar] [CrossRef] [PubMed]
- Hosogane, N.; Watanabe, K.; Yagi, M.; Kaneko, S.; Toyama, Y.; Matsumoto, M. Scoliosis is Risk Factor for Gastroesophageal Reflex Disease in Adult Spinal Deformity. Clin. Spine Surg. 2017, 30, E480–E484. [Google Scholar] [CrossRef] [PubMed]
- Everett, C.R.; Patel, R.K. A systematic literature review of nonsurgical treatment in adult scoliosis. Spine 2007, 32, S130–S134. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.S.; Shaffrey, C.I.; Berven, S.; Glassman, S.; Hamill, C.; Horton, W.; Ondra, S.; Schwab, F.; Shainline, M.; Fu, K.M.; et al. Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery 2009, 65, 86–93. [Google Scholar]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Dimnet, J. Classification of the normal variation in the sagittal alignment of the lumbar spine and pelvis in the standing position. Spine 2005, 30, 346–353. [Google Scholar] [CrossRef]
- Schwab, F.; Lafage, V.; Patel, A.; Farcy, J.P. Sagittal plane consideration and the pelvis in the adult patient. Spine 2009, 34, 1828–1833. [Google Scholar] [CrossRef]
- Miyazaki, J.; Murata, S.; Horie, J.; Uematsu, A.; Hortobágyi, T.; Suzuki, S. Lumbar lordosis angle (LLA) and leg strength predict walking ability in elderly males. Arch. Gerontol. Geriatr. 2013, 56, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Togawa, D.; Hasegawa, T.; Yamato, Y.; Yoshida, G.; Kobayashi, S.; Yasuda, T.; Oe, S.; Banno, T.; Arima, H.; Mihara, Y.; et al. Postoperative Disability After Long Corrective Fusion to the Pelvis in Elderly Patients With Spinal Deformity. Spine 2018, 43, E804–E812. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Fujiwara, Y.; Uotani, K.; Maste, P.; Yamauchi, T. C-Arm-Free Circumferential Minimally Invasive Surgery for Adult Spinal Deformity: Technical Note. World Neurosurg. 2020, 143, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, J.; McGregor, A.; Jones, F.; Mullane, J.; Hurley, M. Rehabilitation Following Lumbar Fusion Surgery: A Systematic Review and Meta-Analysis. Spine 2016, 41, E28–E36. [Google Scholar] [CrossRef] [PubMed]
- Theologis, A.A.; Lau, D.; Dalle-Ore, C.; Tsu, A.; Deviren, V.; Ames, C.P. Costs and utility of post-discharge acute inpatient rehabilitation following adult spinal deformity surgery. Spine Deform. 2021, 9, 817–822. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar]
- Shimada, H.; Suzuki, T.; Suzukawa, M.; Makizako, H.; Doi, T.; Yoshida, D.; Tsutsumimoto, K.; Anan, Y.; Uemura, K.; Ito, T.; et al. Performance-based assessments and demand for personal care in older Japanese people: A cross-sectional study. BMJ Open 2013, 3, e002424. [Google Scholar] [CrossRef] [Green Version]
- Michikawa, T.; Nishiwaki, Y.; Takebayashi, T.; Toyama, Y. One-leg standing test for elderly populations. J. Orthop Sci. 2009, 14, 675–685. [Google Scholar] [CrossRef]
- Bohannon, R.W. Comfortable and maximum walking speed of adults aged 20–79 years: Reference values and determinants. Age Ageing 1997, 26, 15–19. [Google Scholar] [CrossRef] [Green Version]
- Salbach, N.M.; Mayo, N.E.; Higgins, J.; Ahmed, S.; Finch, L.E.; Richards, C.L. Responsiveness and predictability of gait speed and other disability measures in acute stroke. Arch. Phys. Med. Rehabil. 2001, 82, 1204–1212. [Google Scholar] [CrossRef]
- Perera, S.; Mody, S.H.; Woodman, R.C.; Studenski, S.A. Meaningful change and responsiveness in common physical performance measures in older adults. J. Am. Geriatr. Soc. 2006, 54, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Peters, D.M.; Fritz, S.L.; Krotish, D.E. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J. Geriatr. Phys. Ther. 2013, 36, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Seichi, A.; Hoshino, Y.; Doi, T.; Akai, M.; Tobimatsu, Y.; Kita, K.; Iwaya, T. Determination of the optimal cutoff time to use when screening elderly people for locomotive syndrome using the one-leg standing test (with eyes open). J. Orthop Sci. 2014, 19, 620–626. [Google Scholar] [CrossRef]
- Christopher, A.; Kraft, E.; Olenick, H.; Kiesling, R.; Doty, A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review. Disabil. Rehabil. 2021, 43, 1799–1813. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Ungar, B.; Blondel, B.; Buchowski, J.; Coe, J.; Deinlein, D.; DeWald, C.; Mehdian, H.; Shaffrey, C.; Tribus, C.; et al. Scoliosis Research Society-Schwab adult spinal deformity classification: A validation study. Spine 2012, 37, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinaki, M.; Brey, R.H.; Hughes, C.A.; Larson, D.R.; Kaufman, K.R. Balance disorder and increased risk of falls in osteoporosis and kyphosis: Significance of kyphotic posture and muscle strength. Osteoporos. Int. 2005, 16, 1004–1010. [Google Scholar] [CrossRef]
- Arima, H.; Yamato, Y.; Hasegawa, T.; Togawa, D.; Kobayashi, S.; Yasuda, T.; Banno, T.; Oe, S.; Matsuyama, Y. Discrepancy Between Standing Posture and Sagittal Balance During Walking in Adult Spinal Deformity Patients. Spine 2016, 42, 25–30. [Google Scholar] [CrossRef]
- iWalk Guide Online Resources 14. Quick Look-Up Sheet: Reference Values for 10mWT & 6MWT © University of Toronto, Toronto, Canada 1 Quick Look-Up Sheet: Reference Values for 10-metre Walk Test and 6-Minute Walk Test. Available online: https://www.physicaltherapy.utoronto.ca/wp-content/uploads/ (accessed on 3 December 2021).
- Pouwels, S.; Lalmohamed, A.; Leufkens, B.; de Boer, A.; Cooper, C.; van Staa, T.; de Vries, F. Risk of hip/femur fracture after stroke: A population-based case-control study. Stroke 2009, 40, 3281–3285. [Google Scholar] [CrossRef] [Green Version]
- Shimada, H.; Suzukawa, M.; Tiedemann, A.; Kobayashi, K.; Yoshida, H.; Suzuki, T. Which neuromuscular or cognitive test is the optimal screening tool to predict falls in frail community-dwelling older people? Gerontology 2009, 55, 532–538. [Google Scholar] [CrossRef]
- Kozinc, Ž.; Löfler, S.; Hofer, C.; Carraro, U.; Šarabon, N. Diagnostic Balance Tests for Assessing Risk of Falls and Distinguishing Older Adult Fallers and Non-Fallers: A Systematic Review with Meta-Analysis. Diagnostics 2020, 10, 667. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Yagi, M.; Ohne, H.; Konomi, T.; Fujiyoshi, K.; Kaneko, S.; Takemitsu, M.; Machida, M.; Yato, Y.; Asazuma, T. Walking balance and compensatory gait mechanisms in surgically treated patients with adult spinal deformity. Spine J. 2017, 17, 409–417. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).